Short abstract
Background and objectives
The interest of older adults in using patient portals is rising, yet subject to functional and usability barriers. This study aims to gain insight into registration rates and experiences of older adult patients using a patient portal, one year after implementation in an academic hospital.
Methods
Registration rates for one year were collected via automated data extraction. Older adult patients’ experiences were collected through a survey, available via the portal in the last three months of the year.
Results
Older adults were a large user group of the patient portal and appreciated its functionalities. In one year, 10,679 older adult patients (aged 56+) registered, which constituted 47% of total portal registrations. The 131 older adult survey respondents had a mean age of 64.5 years and 40% indicated that they liked to review their medical information and appointments via the portal. Yet, older adults experienced user interaction issues and had higher expectations of content within the portal and patient/provider communication through the portal. Of the survey respondents, 22% experienced usability issues at login and in viewing test results, 15% commented on late or no responses by providers on patients’ sent messages and 24% expected the portal to provide medical history information.
Implications: Patient portal designs should be optimized to usability needs of older adults. Portals preferably include medical history information, physicians’ notes and require prompt responses of providers.
Keywords: Patient portal, technology acceptance, usability, user interaction, patient provider communication, elderly
Introduction
Over the past few decades, there has been a significant proliferation in the implementation and use of electronic health records (EHRs) creating vast opportunities for improvement in the efficiency and quality of patient care as well as reduction in healthcare costs.1 Driven by a multitude of social and economic factors, most notably financially-overstretched healthcare systems and patients’ wishes for a more active role in the management of their disease, patient portals are increasingly being seen as powerful tools for health promotion. A patient portal is often tethered to the EHR of the hospital and most portals offer the same set of basic functions to patients, such as a secure means to schedule appointments, view laboratory results, request medication prescriptions and send secure messages to a healthcare team.2–4 Older adults, aged 50 years and above, typically need healthcare services related to multi and comorbidity problems and for this reason can benefit in particular from the use of a portal. Access to their medical record content and interaction with their providers via a portal can support them specifically in maintaining wellness and independence during the management of their medical condition(s).5
Despite the potential benefits of patient portals, previous research has identified several factors as barriers that have thus far hampered their use, including privacy concerns,6–8 unresponsiveness to messages sent to physicians,8 a mismatch between patients’ expectations and the actual functionalities of a portal6 as well as health literacy and usability problems.9 Further, examples of specific barriers mentioned by older adults are that they have limited access to technology or internet, are not aware that their hospital offers a portal and they are satisfied with the current, face-to-face care communication.2,9–12 These reported barriers suggest that older adult patients use portals less often compared to middle-aged or younger adults. However, a number of studies have indicated that there is a rise in older adults’ interest in using portals to manage personal health information.5,9 A recent systematic review by Sakaguchi-Tang et al. indicates that older adults perceive portals as useful and have an intention to use these portals.13 A 2016 study by Walker et al. likewise reported the growing interest of older people (aged 75+) and their families in online resources such as medication lists, provider rosters, clinicians’ encounter notes and guides to community resources.9
Yet, most studies in the review by Sakaguchi-Tang et al. focused on older adults’ intention to use portals, instead of actual activation rates and use of portals by older adults. Four of the included studies evaluated the older patients’ use experience, and only one study reported on actual activation rates of portals among the older adult patient population.13 Our study contributes to these previous studies on older adults and patient portals by examining actual registration rates of older adult patients one year after a portal’s implementation in a large academic hospital in The Netherlands. It further explores positive or negative experiences of this portal’s use amongst older adult patients with an activated account. A deeper understanding of older adults’ portal usage could be helpful to physicians and other care givers in using portals while providing care for older adults. These insights could likewise enable policy makers to adjust portals to better suit the needs of older adults. Therefore, this study aims to expand the knowledge on (a) enrollment to patient portals amongst the older adult patient population and on (b) experienced factors that contribute to or inhibit portal use by older adults.
Design and methods
Context: Patient portal ‘Mijn Dossier’
As part of the implementation of a new EHR system, the Academic Medical Center (AMC) in Amsterdam launched a tethered patient portal, named ‘Mijn Dossier’ (MyChart) on 25 October 2015. The portal provided the following main functionalities to patients at the time of implementation: (a) patient/provider communication through secure messaging; (b) viewing of medical correspondence; (c) viewing and editing of medical conditions, over the counter medication and allergies list; (d) requesting medication prescriptions; (e) viewing test results, which were automatically shown in the portal 7 days after being recorded in the EHR; pathology, radiology and sexual transmitted diseases test results were automatically shown in the portal 21 days after being recorded in the EHR; (f) viewing and cancelling appointments, or requesting a new appointment. From the date of launch onwards, information on these six aspects, if registered in the EHR, was visible in MyChart; information prior to that date, such as a patient’s historical medical record, was not visible. Patients were informed on MyChart by means of flyers distributed amongst the outpatient clinics and a ‘MyChart page’ at the website of the hospital, including a short video on MyChart and a ‘questions and answers’ section. At the first two weeks of the implementation, MyChart was promoted by the implementation team at the entrance of the outpatient clinics. Patients received a letter with an activation code within the hospital to register to MyChart, which was provided by hospital staff (administration or physicians). Once the activation code was given, the patient could activate his/her account at home. After activation, patients could login by means of a two-factor-authentication method, using a username and password as well as a login code that was sent via a mobile text message. A continuous web support team for patients was available to answer questions from patients regarding the use of the portal. Researcher GW coordinated the implementation and web support activities.
Data collection
Older adults’ patient portal registration rates
Registrations rates were collected from the EHR database. The vendor of the EHR system provided a report on the MyChart ‘status type’ of patients who had had a hospital visit between 25 October 2015 and 25 October 2016. Descriptions of status types are explained in Table 1. Due to the report settings of the EHR vendor, the age clusters in the report ranged from 56 to 105 years, with increments of 10 years. For this reason, the age range of the registration rates differs from the survey respondents’ age range (50+).
Table 1.
Status types of MyChart, including description
| Status type | Description |
|---|---|
| Active | Patient has activated his/her MyChart account |
| Expired | Patient received activation code, but has not activated his/her MyChart account (code has expired) |
| Declined | Patient has indicated he/she does not want to use MyChart |
Survey on older adults’ patient portal experiences
The MyChart web support team created an online survey in Dutch with open-ended questions (Online Appendix A). Patients could provide compliments and/or suggestions on main functionalities of MyChart, including the registration and login process, the messaging feature and viewing/editing of medical information. The survey served to gain insight in how MyChart’s functionalities could be improved. The management team of MyChart in the AMC set the survey’s requirements: it had to be non-obtrusive regarding a patient’s regular MyChart use, thus short in length and not excessively present or marketed while a patient used MyChart. A patient communication advisor and two eHealth specialists of the AMC pre-tested and approved the survey. Consent by patients for scientific research was included in the terms and conditions of MyChart and this study was approved by the Medical Ethical Committee of the AMC.
From the beginning of October 2016 until the end of December 2016, the survey was accessible via a message on the homepage of MyChart after a patient had logged in. Patients could only answer the questions if they had had experiences with (basic) functionalities and could choose to complete the survey anonymously or with their patient ID. Blank returned surveys and anonymous survey data not providing demographics were excluded. We included data from patients with a patient ID to obtain data on gender and age of the patients. Data from patients aged 50 years old and above was anonymized for identity and used for data analysis.
Data analysis
A coding frame was inductively constructed from the data.14 Researcher KM carried out an initial reading of the data and identified specific text segments related to the research objectives. He labelled the text segments to create themes that constituted the preliminary findings and performed an initial coding of the data with those themes. Researcher GW was given the evaluation objectives, the coding themes and the raw data. GW performed an independent parallel session of coding of the raw data. KM and GW conferred to compare, discuss, refine and reduce overlap and redundancy among the themes to develop a more robust coding frame. GW and KM then performed a second round of coding the data. When any disagreement about the coding occurred, researcher LP was involved to discuss the coding to ensure data integrity. The process continued until 100% agreement was reached. In subsequent analysis, it was examined whether both positive and negative aspects regarding MyChart use were reported in individual responses.
Results
Registration rates of older adults
Figure 1 and Online Appendix B show the registration rates of MyChart of older adult patients per age cluster; in total 10,679 older adults activated their MyChart account in one year, this is 47% of all 22,724 patients who activated a patient portal account and 20% of all 53,215 older adults who had a visit in the hospital between 25 October 2015 and 25 October 2016. In the age clusters 56–65 years and 66–75 years, the activated accounts (9,347) outnumber the number of patients who declined to create an account (4,813). However, in the categories above 76 years of age, the number of patients who have declined to create an account (1,858) moderately outnumber the activated accounts (1,332).
Figure 1.
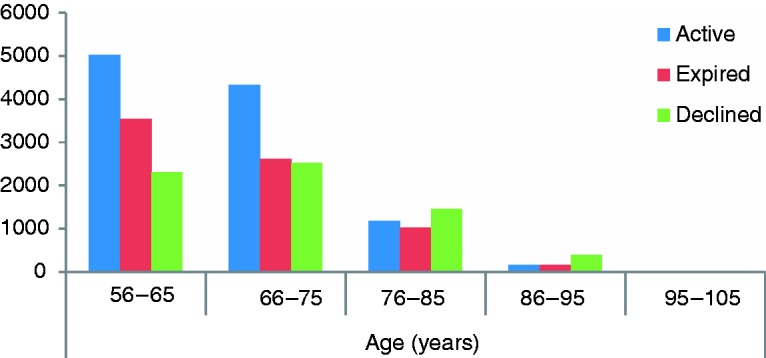
Registration rates for MyChart of patients aged 56 years and above (25 Oct 2015–25 Oct 2016).
Survey demographics
Between October 2016 and December 2016, 406 MyChart users responded to the survey (response rate is approximately 15%), of which 203 responded with a patient ID. Forty returned surveys were excluded due to either being blank on all questions or containing special request texts such as questions directed to the treatment team. Of the remaining 163 responses, 32 were excluded as they were replies from patients younger than 50 years old. The remaining 131 responses were used for data analysis. Demographics of these respondents are shown in Table 2.
Table 2.
Demographics of older adult AMC survey respondents (n=131)
| Age (years) | |
|---|---|
| Mean (±SD) | 64.5 (±8.4) |
| Min–Max | 50–90 |
| Female (n) | 50 |
| Male (n) | 81 |
Older adult patient experiences
Six themes were identified: (a) usefulness of the portal (positive/negative); (b) usability of the portal (positive/negative); (c) attitude and beliefs towards patient portals in general (positive/negative); (d) mismatch of portal terminology with health literacy level of the patient; (e) mismatch of portal content with prior knowledge of the patient on the portal; and (f) coordination of care communication between the patient and the provider (no problem/problem). Figure 2 and Online Appendix C indicate the number of times a theme was mentioned in the responses by patients.
Figure 2.
Number of times of reported patient experiences per theme, per age cluster.
Usefulness
Fifty-three respondents (40%) pointed out that MyChart was useful to them. For example, respondents appreciated that they could review their laboratory results and retrieve information about their health condition: ‘Nice to have a look at home or elsewhere, safe feeling up till now’ (female, 52).
They also stated the relevance of MyChart in the follow-up and planning of their health condition, most notably concerning their upcoming appointments. Eleven respondents (8%) expressed dissatisfaction with the usefulness of MyChart. Main complaints revolved around incompleteness of the information presented in the portal or the considerable time it takes before the test results are shown in the portal once the results are issued from the laboratory: ‘It takes much too long before the results are shown in MyChart’ (male, 61).
Usability
Nineteen respondents (15%) expressed positive comments on usability, mainly using expressions as ‘user friendly’, ‘use is easy’ and ‘clear’. However, usability problems were reported by 29 respondents (22%). For example, respondents were dissatisfied that they could not review all test results on one page; instead each result had to be opened on a different page, rendering it impossible to have an overview of the pattern of test values over time: ‘Is it possible to put all lab results in one overview, then you would not need to click on each single result’ (male, 55).
The two-factor-authentication login system generated praise and criticism. Some respondents were explicitly asking for a simpler mode of access so as to minimize the numbers of passwords and codes to be remembered and entered on a (mobile) device: ‘Now this is too much to remember or type and then there is also an extra notification per telephone all double double’ (female, 55).
Of the respondents who reported usability problems, 9 (35%) still assessed MyChart as useful.
Attitude and beliefs
Out of 15 respondents (11%) who had a negative attitude towards patient portals in general, only 1 acknowledged the usefulness of MyChart, while 9 were clear in their disinterest; reporting that MyChart was not useful to them: ‘Records are not well maintained. This has absolutely no use!!!!!’ (male, 73).
In contrast, only 1 respondent of the 35 respondents (27%) with a positive view of patient portals in general, was still skeptical as to the use of MyChart in its current development stage.
It is very good that a start has been made with providing information to patients on their own treatment. However, much more information can be provided in MyChart, so that eventually it will become a full record to consult as a patient (male, 61).
Mismatch of portal terminology and content with patient’s health literacy and prior knowledge
Seventeen respondents (13%) indicated their inability to fully understand the terminology used in MyChart. Some deemed the use of terminology too medical. Others had difficulties with the abbreviations that were used in medical correspondence or with understanding the laboratory test values in the absence of normal range values as a reference: ‘The terminology used in the results of blood tests is difficult to understand for a regular patient’ (male, 70).
Of these 17 respondents who had difficulties in understanding the terminology used in MyChart, five had a positive attitude towards MyChart, compared to 35 of total respondents with a positive overall attitude.
Insufficient prior knowledge of what MyChart entailed was a problem for 31 respondents (24%). They had higher expectations of MyChart based on their idea of what functionalities a patient portal should provide. For example, they expected their physicians’ notes and historical medical information to be available in MyChart; as well as their medical images: ‘My doctor always makes extensive notes in the system during a consult. Unfortunately, I cannot see those’ (male, 68).
Coordination of care communication
Twenty-two respondents (17%) had explicit comments on communication with the medical staff, with 19 (15%) of them indicating a negative experience. Physicians’ unresponsiveness to respondents’ messages sent via MyChart was a clear source of dissatisfaction: ‘Not every doctor looks at the record and it sometimes takes days or even longer before a message is answered or sometimes there is no answer at all’ (female, 73).
Nevertheless, this unresponsiveness did not seem to alter the perception of the usefulness of MyChart, since 12 (9%) of the 19 (15%) respondents still considered MyChart to be useful. Three respondents (2%) reported receiving timely replies to their questions and being satisfied with this: ‘Contact with specialists is good’ (female, 51).
Discussion
Over 10,600 older adult patients activated their account one year after the implementation of MyChart, 20% of all older adult patients with a hospital visit in that year. An important finding was that older adult patients with an activated account constituted 47% of all patients with a registered MyChart account. Compared to the overall Dutch population of people aged 50+ (39%),15–16 the percentage of registered older users for MyChart seems to indicate that older adults are particularly interested in the patient portal. Other studies on patient portal registration by older adults are scarce, yet they do report that older adults currently form a large user group of patient portals. For example, a Dutch study on the usage of patient portals of 22 hospitals reports that patients aged 60–79 years account for 31–40% of users.17 MyChart offered similar functionalities compared to the portals of these other hospitals in The Netherlands.17 An American database study by Gordon et al. reports that 77% of all patients aged 65–79 years of Kaiser Permanente Northern California health plan registered to their patient portal.18
The results of the survey indicate that main contributors to patient portal use by older adults were those who experienced usefulness of the portal in question, as well as a positive attitude and belief towards patient portals in general. Main inhibitors were that patients had higher expectations of MyChart based on their idea of what functionalities a patient portal should provide, unresponsiveness of physicians to messages sent by patients via MyChart and experienced usability problems. Regarding the latter, consistent with previous literature this study acknowledges the importance of usability in relation to adoption of technology, especially for older adult target groups.19–21 A main usability problem of MyChart concerned the two-factor-authentication method. Most respondents reported that it was difficult to use this method to login and suggested simpler means. An interesting finding is that about one third of patients with login problems still reported the portal to be useful to them. Lower registration rates of MyChart from 76 years upwards might, likewise, be related to login usability problems experienced by this group. The rate of patients with an expired activation code (those who received an activation code but did not activate their account in time) is higher in relation to the rate of activated accounts from 76 years upwards. A possible explanation is that this population might find the activation and login process too difficult and thus do not attempt to register or discard their registration attempt, which leads to their code expiring.
A patient’s health literacy level is an aspect that is considered to be a strong influential factor as to the patient’s interest and ability to use a patient portal.22–23 A literature review on portals and engagement confirms that patients with higher health literacy were more likely to adopt the patient portal, while those with low health (and computer) literacy would either lack the interest to use it or would use it ineffectively.23 Another finding was that patients interacted better with the patient portal if medical abbreviations and terminology were replaced by lay language.23 Most studies on health literacy and patient portal use do not examine specific age groups. The exceptions are a study by Taha et al. that reported that numeracy (dis)abilities of older adults impact their (mis)understanding of medical content, for example of test results, and a study by Walker et al. explaining that difficulties in older adults’ portal usage can be related to health literacy issues.9,24 Some older adult patients in our study mentioned that they experienced difficulties in understanding the medical terminology used in MyChart. Nevertheless, almost one-third of these patients had a positive perception of the usefulness of the portal. A possible explanation for this could be that respondents were mostly health (and computer) literate, since they were users of the portal. Patients with lower health literacy levels might not have used the portal and as such could not have responded to the survey.
The majority of respondents in our study were adamant in pointing out their discontent regarding the absence of replies of their physician to their questions asked via MyChart, yet most of them still valued the usefulness of the portal on the whole. In other words, although the portal did not facilitate or strengthen patient/provider communication, older adult patients still valued MyChart since they could review their medical data and check appointments. The previous review on patient portals and patient engagement reports that a provider’s endorsement and continued engagement with the portal is of importance to encourage patients into adopting a portal.23 Of the eight articles reviewed on this matter, none addressed the older adult patient population specifically. The principal findings of our study suggest that the experienced usefulness of the portal seems to provide enough reason for older adult patients to use the patient portal, despite the current lack of provider endorsement and engagement for the portal we investigated.
Trends are showing that patient portals and digital health tools are increasingly being used in continuing care and communication with patients with chronic diseases. For example, a growth of patient-reported outcome measures (PROMs) linked to EHRs is seen; to gather these PROMs it is preferred that patients report their health outcomes via a tethered portal.25 Consequently, patient portals are transforming from a tool used mainly as a reference for patients to review their medical data and check appointments to an interactive tool in which patients need to actively register data on their medical health status in the portal. As this study shows, such interactive use of portals by older adults, a population in which the prevalence of chronic diseases is higher compared to younger adults, could yet be jeopardized by non-engagement of portal use at the provider side or by experienced usability problems of older adults. Future research directions should therefore concentrate on how to incorporate the benefits of patient portal functionalities as experienced by patients into the work processes of healthcare delivery teams. In addition, future research should focus on which designs, including presentation and visualization of medical data, and training efforts to support older adults in their user interactions with portals. They can focus as well on training efforts to support healthcare providers in their interaction with patients via patient portals.
Limitations
In this study, patient registration rates are based on quantitative reports of the EHR system. Yet, hospital staff had to provide an activation code before a patient could activate an account. At the introduction of the portal this process might have been imperfect, as the staff was still getting acquainted with how to operate the system, which might have negatively influenced the registration rates. Similar to previous studies, our study uses registration data to report on initial usage rates of the portal; frequency of use is not measured.
Using a monthly average of unique users of MyChart, we estimated the response rate of the survey at 15%. This might cause bias in our study regarding representativeness of our sample for the total older adult user population of MyChart.26 Nevertheless, 80% of the survey respondents were older adult patients, compared to 47% of older adult patients registered at the portal.
We did not analyse the anonymous data and for this reason we might have missed relevant insights mentioned in this dataset. However, since this data did not include the age of the patient, we were not able to use this data set. We chose to use the data set in which we were certain the patients were aged 50 years and above, in order to give a detailed insight into the experiences of these older adult patients’ current use of a patient portal.
Conclusion
Activation rates of a patient portal amongst the older adult patient population were high; patients aged 56 to 75 years old form a large user population of this patient portal. The main factor that contributes to older adult patients’ portal use, experienced by all age groups, is the opportunity to review medical record information and check the planning of upcoming appointments. Factors that inhibit portal use by older adult patients are difficulties in user interaction, annoyances regarding the difference in EHR data versus. medical record data presented in the portal, and a lack of a timely response from providers on patients’ questions asked via the portal.
Implications
To increase adoption of patient portals by older adult patients, usability needs of these patients should be addressed in patient portal designs to further optimize user friendliness of portals for this apparently large user group. Ensuring privacy and security by means of the two-factor authentication standard is essential; yet to avoid non-adoption by older adults due to login issues they might experience, we encourage investigating new secure and user-friendly authentication options that may better suit an older population, for example by using biometrics during authentication (i.e. a photo of a patient’s face, a record of a patient’s voice or an image of a patient’s fingerprint). As an addition to current standard functionalities and content of patient portals, additional content should preferably include medical history data and physicians’ notes, to meet the older adult patients’ expectations. Effective patient/provider communication via a patient portal requires prompt responses of providers on questions asked by patients via the portal. Since there might be a lack of time for the physician to do so and the physician might prefer to speak to and/or see the patient in responding to questions, physicians and patients can discuss preferred communication means and response time regarding questions asked via the portal by patients during the first consultation.
Supplemental Material
Supplemental material for Older adults using a patient portal: registration and experiences, one year after implementation by Gaby Anne Wildenbos, Karim Maasri, Monique Jaspers and Linda Peute in Digital Health
Acknowledgements
The Authors would like to thank the project team of the AMC of ‘Mijn Dossier’ for their cooperation in conducting the survey. We would like to thank the technical support staff of the EHR vendor for their assistance in creating a report regarding the registration data of ‘Mijn Dossier’.
Conflict of interests
The Authors declare that there is no conflict of interest.
Contributorship
Prof. Dr MWJ is head of the research laboratory of Human Factors and Usability Studies at the Department of Medical Informatics at the Academic Medical Center of Amsterdam, where this research took place. Dr LP is an expert in Human Factor methods in Health Informatics. GW is a PhD student and expert in Human Factor methods for mobile devices. KM is a Master Medical Informatics student and Medical Doctor. Study conception was created by MWJ, LP and GW; design was created by LP and GW. Acquisition of data was performed by GW. Analysis and interpretation of data was performed by KM, GW and LP. Drafting of manuscript was performed by GW, KM and LP was involved in writing the manuscript from the first version onwards. MWJ was further involved in critical revision of the manuscript.
Ethical approval
This study was approved by the Medical Ethical Committee of the Academic Medical Center in Amsterdam. Consent by patients for scientific research was included in the terms and conditions of ‘Mijn Dossier’ of the Academic Medical Center in Amsterdam.
Funding
This work was supported by the Department of Medical Informatics of the Academic Medical Center in Amsterdam. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Guarantor
MWJ
Peer review
This manuscript was reviewed by Dr. Romaric Marcilly, Centre d’Investigation Clinique, France, and one other individual who has chosen to remain anonymous.
Supplemental Material
Supplemental Material for this article is available online.
References
- 1.Chaudhry B., Wang J, Wu S, et al. Systematic Review: Impact of Health Information Technology on Quality, Efficiency, and Costs of Medical Care. Ann Intern Med. 2006; 144(10): 742. DOI: 10.7326/0003-4819-144-10-200605160-00125 [DOI] [PubMed] [Google Scholar]
- 2.Goel MS, Brown A, Williams AJ, et al. Patient reported barriers to enrolling in a patient portal. J Am Med Inform Assoc 2011; 18(1): i8–12. DOI: 10.1136/amiajnl-2011-000473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sarkar U., Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: Evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18(3): 318–321. DOI: 10.1136/jamia.2010.006015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith SG, O’Conor R, Aitken W, et al. Disparities in registration and use of an online patient portal among older adults: Findings from the LitCog Cohort. J Am Med Inform Assoc 2015; 22(4): 888–895. DOI: 10.1093/jamia/ocv025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner AM, Osterhage K, Hartzler A, et al. Use of Patient Portals for Personal Health Information Management: The Older Adult Perspective. In: AMIA Annual Symposium Proceedings 2015; 1234–1241. [PMC free article] [PubMed]
- 6.Greenhalgh T, Hinder S, Stramer K, et al. Adoption, non-adoption, and abandonment of a personal electronic health record: Case Study of HealthSpace. BMJ 2010; 341: c5814. DOI: 10.1136/bmj.c5814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pyper C, Amery J, Watson M, et al. Patients’ experiences when accessing their on-line electronic patient records in primary care. Br J Gen Pract 2004; 54(498): 38–43. [PMC free article] [PubMed] [Google Scholar]
- 8.Ralston JD. Patients’ experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. BMJ 2004; 328(7449): 1159. DOI: 10.1136/bmj.328.7449.1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walker J, Crotty BH, O’Brien J, et al. Addressing the challenges of aging: How elders and their care partners seek information. Gerontologist 2016; 57(5): 955–962. DOI: 10.1093/geront/gnw060. [DOI] [PubMed] [Google Scholar]
- 10.Mishuris RG, Stewart M, Fix GM, et al . Barriers to patient portal access among veterans receiving home-based primary care: A qualitative study. Health Expectations 2015; 18(6) 2296–2305. DOI: 10.1111/hex.12199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Latulipe C, Gatto A, Nguyen HT, et al. Design Considerations for Patient Portal Adoption by Low-Income, Older Adults. In: Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems Seoul, Republic of Korea, April 18–23 2015, pp. 3859–3868. New York: ACM Press, 2015. DOI: 10.1145/2702123.2702392. [DOI] [PMC free article] [PubMed]
- 12.Tieu L, Sarkar U, Schillinger D, et al . Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: A qualitative study. J Med Internet Res 2015; 17(12): e275. DOI: 10.2196/jmir.4847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakaguchi-Tang DK, Bosold AL, Choi YK, et al. Patient portal use and experience among older adults: Systematic review. JMIR Med Inform 2017; 5(4): e38. DOI: 10.2196/medinform.8092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Evaluation 2006; 27(2): 237–246. DOI: 10.1177/1098214005283748 [Google Scholar]
- 15.National Institute for Public Health and the Environment. Bevolking, Cijfers & Context, Vergrijzing. https://www.volksgezondheidenzorg.info/onderwerp/bevolking/cijfers-context/vergrijzing (accessed: 12 July 2018).
- 16.Central Bureau of Statistics. Bevolking op 1 januari en gemiddeld; geslacht, leeftijd en regio. www.statsline.cbs.nl (accessed: 12 July 2018).
- 17.Pluut B, Peters E, Sinnige J, et al. Het gebruik van patiëntportalen: een verkennende studie [The use of patient portals: an explorative study]. https://www.nictiz.nl/SiteCollectionDocuments/Whitepapers/Whitepaper_het_gebruik_van_pati%C3%ABntportalen.pdf (accessed 15 February 2018).
- 18.Gordon NP, Hornbrook MC. Differences in access to and preferences for using patient portals and other eHealth technologies based on race, ethnicity, and age: a database and survey study of seniors in a large health plan.” J Med Internet Res 2016; 18(3): e50. DOI:10.2196/jmir.5105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Czaja SJ., Zarcadoolas C, Vaughon WL, et al. The usability of electronic personal health record systems for an underserved adult population. Hum Factors 2015; 57(3): 491–506. DOI: 10.1177/0018720814549238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gao C, Zhou L, Liu Z, et al. Mobile application for diabetes self-management in China: do they fit for older adults? Int J Med Inf 2017; 101: 68–74. DOI: 10.1016/j.ijmedinf.2017.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Or C, Tao D. Usability study of a computer-based self-management system for older adults with chronic diseases. JMIR Res Protoc 2012; 1(2): e13. DOI: 10.2196/resprot.2184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc 2008; 15(1): 1–7. DOI: 10.1197/jamia.M2562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Irizarry T, DeVito Dabbs A, Curran CR. Patient portals and patient engagement: A state of the science review. J Medl Internet Res 2015; 17(6); e148. DOI: 10.2196/jmir.4255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Taha J, Sharit J, Czaja SJ. The impact of numeracy ability and technology skills on older adults’ performance of health management tasks using a patient portal. J App Gerontology 2014; 33(4): 416–436. DOI: 10.1177/0733464812447283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu AW, Kharrazi H, Boulware LE, et al. Measure once, cut twice—adding patient-reported outcome measures to the electronic health record for comparative effectiveness research. J Clin Epidem 2013; 66(8): S12–20. DOI: 10.1016/j.jclinepi.2013.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fincham JE. Response rates and responsiveness for surveys, standards, and the Journal. Am J Pharml Educ 2008; 72(2): 43. DOI: 10.5688/aj720243 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for Older adults using a patient portal: registration and experiences, one year after implementation by Gaby Anne Wildenbos, Karim Maasri, Monique Jaspers and Linda Peute in Digital Health



