Abstract
Context:
Magnesium (Mg) is an intracellular cation which takes part in various functions including smooth muscle contractility. Studies have shown that serum Mg level has no significant effect on asthma severity. There are only sparse data on the effect of serum Mg level on asthma control.
Aims:
The aim of this study was to evaluate the effect of serum Mg level on asthma control.
Settings and Design:
This hospital-based cross-sectional study was conducted at the Department of Respiratory Medicine, Kasturba Medical College, Manipal.
Subjects and Methods:
Our participants were adult asthma patients over 18 years of age. Asthma control was assessed using a questionnaire. Serum Mg level was estimated. The study was approved by the Institutional Ethics Committee, and informed consent was obtained from the participants.
Statistical Analysis Used:
Welch's ANOVA test was used to analyze the correlation between serum Mg level and level of control of asthma.
Results:
We screened 256 patients who met the inclusion criteria. After 96 patients were removed based on exclusion criteria, 160 patients were grouped into three based on the level of symptom control. Forty-eight patients belonged to the “well controlled” group, 59 in “partly controlled” group, and the remaining 53 in “uncontrolled” group. The mean serum Mg level (mg/dl) was 2.08 ± 0.37, 2.07 ± 0.28, and 1.83 ± 0.34 in well, partly, and uncontrolled groups, respectively. As the level of control of asthma decreased from well controlled to uncontrolled, the level of mean serum Mg also decreased.
Conclusions:
Serum Mg levels have a positive correlation with the level of symptom control in asthma. In uncontrolled asthma, serum Mg is significantly low. Hence, it might be useful as a biomarker in assessing control or severity of asthma.
KEY WORDS: Asthma, bronchodilator agents, magnesium
INTRODUCTION
Magnesium (Mg) is one among the most abundant cations in the human body with normal serum value ranges of 1.5–2.3 mg/dl.[1] It has a vital role in cellular metabolism, cardiac contractility, and muscle contractility. Among these, the effect of Mg on smooth muscle warrants further attention. Mg is involved in mechanisms such as inhibition of vascular and bronchial smooth muscle contraction and inhibition of acetylcholine release from cholinergic nerves.[2] It is also engaged in the promotion of nitric oxide and prostacyclin generation and smooth muscle stabilization.[3] Hence, Mg has a significant role in causing muscle relaxation. Hypomagnesemia leads to muscle contraction and hypermagnesemia to muscle relaxation.[4] There are studies documenting usefulness of Mg in treating acute asthma.[5,6,7] There are several studies on serum Mg levels in asthma patients which show that hypomagnesemia is commonly seen in asthmatics.[8,9,10,11] However, there are no studies that correlate the asthma symptom control and serum Mg level. We aimed at estimating the serum Mg levels and asthma control.
SUBJECTS AND METHODS
This study was of prospective hospital-based cross-sectional design. Our participants were from the Department of Respiratory Medicine, Kasturba Medical College, Manipal, which is a tertiary care center in Karnataka state of India. The study period was from September 2014 to March 2016. The Institutional Ethics Committee approved the study. We included patients who have asthma aged >18 years and attended the outpatient and emergency department. We diagnosed asthma based on symptoms and spirometry evaluation depicting reversible airflow obstruction (postbronchodilator forced expiratory volume in the 1st s (FEV1) >12% and 200 ml). Exclusion criteria included the following: chronic obstructive pulmonary disease, diabetes mellitus, cardiac diseases, and chronic renal and liver diseases. We excluded pregnant women, alcoholics, those on diuretics, having diarrhea, smokers, and those who underwent gastric resection or abdominal surgery.
We obtained a written informed consent before the study. We recorded the demographic details, the relevant history, and physical findings. Asthma control was assessed based on a questionnaire.[12] Symptom level over the past 4 weeks was assessed based on the following questions:
Daytime asthma symptoms more than twice/week?
Any nighttime waking due to asthma?
Reliever needed for symptoms more than twice/week?
Any activity limitation due to asthma?
We included those who answered negative to all of the questions in “well controlled” group; those who had one or two affirmatives in “partly controlled” group; and those who answered yes to three or four questions in the “uncontrolled” group. We recorded spirometry values before and after administering bronchodilator. We collected 2 mL of venous blood for estimation of Mg level in serum. Mg was estimated by the end point calorimetric method using xylidyl blue (Cobas 6000, Roche Diagnostics Limited, Switzerland).
Statistical analysis
We correlated the serum Mg levels of the patients with the level of control of asthma by comparing the serum Mg value across all the three groups. The sample size was estimated by the G*Power 3.17 tool for statistical power analysis.[13] Power analysis was conducted in G*Power using an alpha of 0.05, power of 0.80, and a medium effect size (f = 0.25). Based on these assumptions, the desired sample size needed was 159 (rounded to 160 in our study). Welch's ANOVA test was used to analyze the correlation between serum Mg level and level of control of asthma and to ascertain whether the difference in the level of Mg between these three groups was statistically significant (P < 0.05). The analysis was performed using the statistical package for the social sciences (SPSS) version 22.0 (IBM Corp., Armonk, NY, USA).
RESULTS
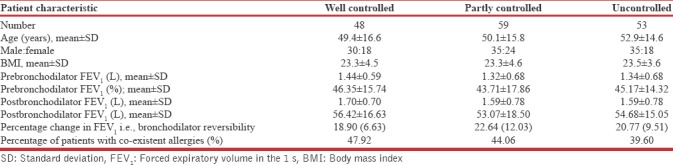
We screened a total of 256 patients for eligibility who met the inclusion criteria. Among these 256 patients, 49 patients were excluded at the onset on the basis of significant smoking history. Among the remaining 207 patients, 18 patients were unable to perform acceptable spirometry as per ATS guidelines. The remaining reasons for exclusion were diabetics (14), patients on diuretic therapy (7), chronic liver disease/alcoholics (6), and chronic renal failure (2) [Figure 1]. A total of 160 patients were included in the study. There were 99 males and 61 females. We grouped them into three based on the level of symptom control [Table 1]. Majority of the patients belonged to the “partly controlled” group (n = 59) followed by “uncontrolled” group (n = 53) and “well controlled” group (n = 48). Males were the predominant gender in all groups. The mean age was 49.4 ± 16.6 in “well controlled,” 50.1 ± 15.8 in partly controlled, 52.9 ± 14.6 years in “uncontrolled group,” respectively. The median age across the three groups was 51, 53, and 52 years and the age range was 59, 65, and 55 years in well controlled, partly controlled, and uncontrolled groups, respectively. Prebronchodilator FEV1 in litres was 1.44 ± 0.59 in “well controlled,” 1.32 ± 0.68 in “partly controlled,” and 1.34 ± 0.68 in “uncontrolled group.” After administering bronchodilator, there was an increase in FEV1 of 18.90% ± 6.63% in well controlled, 22.64% ± 12.03% in partly controlled, and 20.77% ± 9.51% in “uncontrolled” group. Among the 160 patients, the total number of patients with history of coexisting allergies such as rhinitis or conjunctivitis was 70 (43.8%). The distribution of patients with these comorbid allergies was 23 (47.92%), 26 (44.06%), and 21 (39.60%) in well controlled, partly controlled, and uncontrolled groups, respectively.
Figure 1.
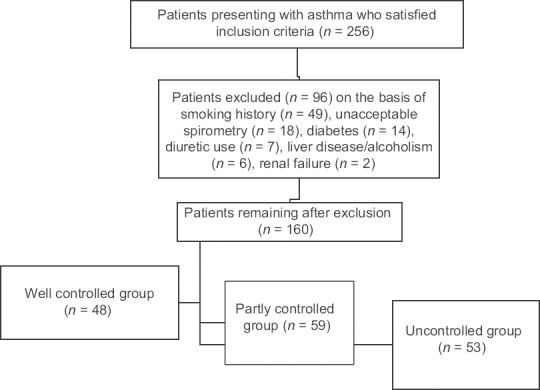
Consort diagram of the study
Table 1.
Baseline patient characteristics
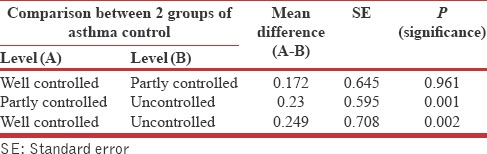
The mean serum Mg level (mg/dl) was 2.08 ± 0.37, 2.07 ± 0.28, and 1.83 ± 0.34 in well, partly, and uncontrolled groups, respectively [Table 2]. The serum Mg levels for the three different groups were analyzed using Welch's ANOVA test [Table 3]. The “well controlled” group had significantly higher mean serum Mg values compared to the “uncontrolled” group (P = 0.002). Similarly, the partly controlled group had significantly higher serum Mg values compared to the “uncontrolled” group (P = 0.001). However, the difference between mean serum Mg levels between well controlled and partly controlled groups was not statistically significant (P = 0.961). These findings indicated a positive correlation between Mg and asthma control.
Table 2.
Descriptive values of serum magnesium (mg/dl) across the three groups of asthma based on symptom control
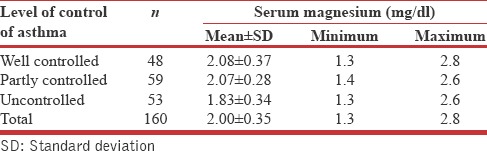
Table 3.
Comparative analysis of serum magnesium levels across the three groups of asthma based on symptom control by Welch ANOVA test
On correlation of spirometry results with serum Mg values, a weak positive correlation coefficient was noted for prebronchodilator FEV1 and postbronchodilator FEV1 (+0.071 and + 0.073, respectively).
DISCUSSION
The relation between Mg and asthma is well established over the years. Among these, the most well-known association is the therapeutic utility of MgSO4 in acute severe asthma. Asthma is characterized by airway obstruction. Increased airway smooth muscle tone is the main mechanism leading to this obstruction. Mg is an essential macro element, which takes part in smooth and skeletal muscle contraction and neurosynaptic function.[14,15] It has an inhibitory effect on acetylcholine secretion.[16] Several studies have established this inhibitory action as the basis for MgSO4 use in acute asthma.
However, other aspects dealing with Mg and asthma are less straightforward. Serum Mg level in asthma is one such studied aspect. Emelyanov et al. studied the serum Mg level in bronchial asthma patients and demonstrated that the bronchial hyperresponsiveness is inversely proportional to the serum level of this cation.[17] Other studies from Egypt and India have also shown concordant results.[18,19] Majority of the recent studies emphasize the fact that hypomagnesemia is prevalent in asthma.[8,9,10,11] Hence, accepting that hypomagnesemia is prevalent in asthma, in this study, we aimed to evaluate serum Mg levels and its relation to asthma control. As per the Global Initiative for Asthma guidelines, asthma is divided into well controlled, partly controlled, and uncontrolled, based on a questionnaire related to symptoms.[12] Studies comparing asthma control to serum Mg levels are relatively rare.
The participants in our study were divided into three groups based on asthma symptom control. The serum Mg levels in these participants were measured. We attempted to eliminate the factors which may affect serum Mg levels by excluding participants with comorbidities such as diabetes mellitus, cardiac diseases, chronic renal and liver diseases, pregnant females, alcoholics, participants who were on diuretics, and those having diarrhea. Thus, we aimed to establish a more accurate relationship between Mg and asthma control.
We observed that serum Mg had a positive correlation with the level of control in asthma. The participants with well-controlled asthma had a higher serum Mg compared to the other two groups. In uncontrolled asthma, serum Mg was significantly low.
Our study had many limitations. A significant share of total body Mg is intracellular, estimation of which is difficult.[20] Serum Mg levels may not correlate with intracellular levels. Furthermore, normal controls were not included. Serial values were not measured in longitudinal follow-up to see if a patient loses control, whether there is a fall in serum Mg levels, or if a patient gains control whether serum Mg levels increases. The study population is unrepresentative of the regular asthmatic population since the mean age of the study population is 50 years. Laboratory values such as absolute eosinophil count and serum IgE values and whether patients had atopic/nonatopic asthma were not further evaluated.
Maintaining of the serum Mg level in normal or high serum ranges might help in achieving good asthma control. MgSO4 has been used in managing severe exacerbations of asthma. This study raises the possibility that in addition to being used as a therapeutic adjunct in managing severe acute asthma, Mg might also play an important role in preventing asthma attacks.
Whether regular dietary supplementation of Mg might help in achieving asthma control needs further study. Foods such as whole grains and dark-green, leafy vegetables are rich sources of Mg. Some ready-to-eat breakfast cereals are fortified with Mg.[21] The physiology of Mg in the human body, intracellular stores, and correlation with serum levels needs to be further understood. Alternative methods of estimation of Mg level such as red blood cell storage might be useful. The possible side effects as well as complications of overdose also need to be understood.
CONCLUSIONS
Serum Mg levels have a direct correlation with the level of control in asthma. Maintaining normal serum Mg values by regularly consuming a healthy Mg-rich diet could help in achieving better control of asthma. Whether there is a role for regularly measuring serum Mg as a marker for asthma control needs further validation. There is a need for studies to understand the physiology involved in storage and distribution of intracellular Mg as well as possible adverse effects associated with Mg supplementation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Jahnen-Dechent W, Ketteler M. Magnesium basics. Clin Kidney J. 2012;5:i3–i14. doi: 10.1093/ndtplus/sfr163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodrigo G, Rodrigo C, Burschtin O. Efficacy of magnesium sulfate in acute adult asthma: A meta-analysis of randomized trials. Am J Emerg Med. 2000;18:216–21. doi: 10.1016/s0735-6757(00)90024-x. [DOI] [PubMed] [Google Scholar]
- 3.Song WJ, Chang YS. Magnesium sulfate for acute asthma in adults: A systematic literature review. Asia Pac Allergy. 2012;2:76–85. doi: 10.5415/apallergy.2012.2.1.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Swaminathan R. Magnesium metabolism and its disorders. Clin Biochem Rev. 2003;24:47–66. [PMC free article] [PubMed] [Google Scholar]
- 5.Ciarallo L, Brousseau D, Reinert S. Higher-dose intravenous magnesium therapy for children with moderate to severe acute asthma. Arch Pediatr Adolesc Med. 2000;154:979–83. doi: 10.1001/archpedi.154.10.979. [DOI] [PubMed] [Google Scholar]
- 6.Singh AK, Gaur S, Kumar R. A randomized controlled trial of intravenous magnesium sulphate as an adjunct to standard therapy in acute severe asthma. Iran J Allergy Asthma Immunol. 2008;7:221–9. [PubMed] [Google Scholar]
- 7.Kaye P, O'Sullivan I. The role of magnesium in the emergency department. Emerg Med J. 2002;19:288–91. doi: 10.1136/emj.19.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shaikh MN, Malapati BR, Gokani R, Patel B, Chatriwala M. Serum magnesium and Vitamin D levels as indicators of asthma severity. Pulm Med 2016. 2016:1643717. doi: 10.1155/2016/1643717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SH, Song WJ, Park HW, Kim SH, Park HK, Kim SH, et al. Serum micronutrients levels and clinical features of elderly asthmatics. Allergy Asthma Respir Dis. 2017;5:223–7. [Google Scholar]
- 10.Ali AA, Bakr RM, Yousif M, Foad RE. Assessment of serum magnesium level in patients with bronchial asthma. Egypt J Chest Dis Tuberc. 2015;64:535–9. [Google Scholar]
- 11.Hashimoto Y, Nishimura Y, Maeda H, Yokoyama M. Assessment of magnesium status in patients with bronchial asthma. J Asthma. 2000;37:489–96. doi: 10.3109/02770900009055475. [DOI] [PubMed] [Google Scholar]
- 12.(*NEW) 2017 GINA Report: Global Strategy for Asthma Management and Prevention. Global Initiative for Asthma – GINA. [Last accessed on 2018 Jan 30]. Available from: http://www.ginasthma.org/2017-gina-report-global-strategy-for-asthma-management-and-prevention/
- 13.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 14.de Baaij JH, Hoenderop JG, Bindels RJ. Magnesium in man: Implications for health and disease. Physiol Rev. 2015;95:1–46. doi: 10.1152/physrev.00012.2014. [DOI] [PubMed] [Google Scholar]
- 15.Saris NE, Mervaala E, Karppanen H, Khawaja JA, Lewenstam A. Magnesium. An update on physiological, clinical and analytical aspects. Clin Chim Acta. 2000;294:1–26. doi: 10.1016/s0009-8981(99)00258-2. [DOI] [PubMed] [Google Scholar]
- 16.Fox C, Ramsoomair D, Carter C. Magnesium: Its proven and potential clinical significance. South Med J. 2001;94:1195–201. [PubMed] [Google Scholar]
- 17.Emelyanov A, Fedoseev G, Barnes PJ. Reduced intracellular magnesium concentrations in asthmatic patients. Eur Respir J. 1999;13:38–40. doi: 10.1183/09031936.99.13103899. [DOI] [PubMed] [Google Scholar]
- 18.Mohammad HA, Abdulfttah MT, Abdulazez AO, Mahmoud AM, Emam RM. A study of electrolyte disturbances in patients with chronic stable asthma and with asthma attacks. Egypt J Chest Dis Tuberc. 2014;63:529–34. [Google Scholar]
- 19.Das SK, Haldar AK, Ghosh I, Saha SK, Das A, Biswas S, et al. Serum magnesium and stable asthma: Is there a link? Lung India. 2010;27:205–8. doi: 10.4103/0970-2113.71944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatipoglu N, Hatipoglu H, Turel O, Aydogmus C, Engerek N, Erkal S, et al. Serum magnesium concentration in children with asthma. Eurasian J Pulmonol. 2014;16:36–9. [Google Scholar]
- 21.Rude RK. Magnesium. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler TR, editors. Modern Nutrition in Health and Disease. 11th ed. Baltimore, Mass: Lippincott Williams & Wilkins; 2012. pp. 159–75. [Google Scholar]


