See the article by Brown et al. pp. 1374-1382.
Health disparities are differences in health among different groups of people. Generally related to socioeconomic factors, they culminate in differential outcomes among people suffering from similar conditions. Health disparities span all of health care—from management of chronic conditions (hypertension) to more acute conditions (cancer). An often-cited result is a widening gap in life expectancy between groups. Beyond survival, health disparities have a profound impact on general well-being. Multiple factors contribute to health disparities, including income inequality, which has increased dramatically and has been associated with a widening gap in life expectancy.1 Wealthier individuals have greater flexibility when considering options. The relationship between health care outcomes and income is likely more complicated than available monetary resources. Education has consistently correlated with health outcomes. New technology created a demand for skilled labor demanding higher wages while simultaneously decreasing demand for less skilled labor. Better jobs afforded by advanced education provide access to higher quality insurance. Education (in conjunction with financial potential) may increase access to and adaptation of healthful behaviors—smoking cessation, weight loss, etc—and improves compliance with complex therapies. Rising income inequalities promote geographic segregation of high- and low-income populations, resulting in differential diffusion of positive and negative influences. Health care access and type of insurance are other determinants of disparities. The article by Brown et al in this issue reports that the type of insurance correlates with treatment and outcome in glioblastoma patients.2
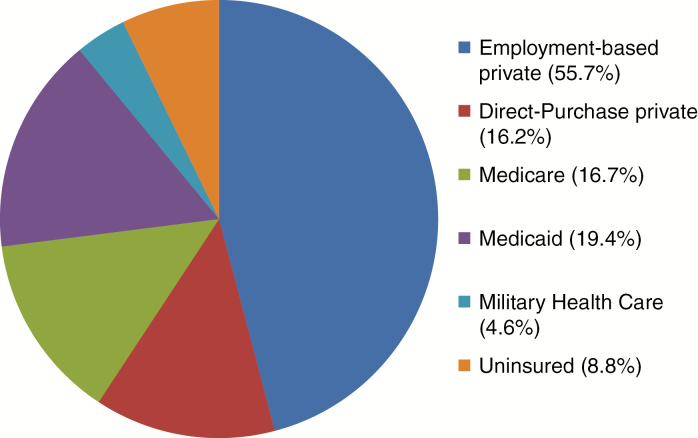
In the United States, health insurance is categorized into Medicare, Medicaid, and “private insurance.” In addition 8.8% of the population is uninsured3 (Fig. 1). People aged >65 are covered by Medicare, which is broken down into 3 “parts.” Part A covers inpatient acute and skilled nursing care and hospice. This is available to most without additional cost who paid Medicare taxes. Part B covers outpatient care, including physician services and medical supplies. Part D covers prescription medications. Participants in Parts B and D pay a premium depending on their income. Medicaid provides coverage for low-income families, children, pregnant women, and the disabled. Eligibility and extent of coverage is established by the state. Consequently, coverage varies widely. Private insurance is purchased by individuals or provided by an employer. Policies vary widely, including covered services, patient-associated costs, and extent of health care access.
Fig. 1.
Proportion of patients covered by main insurance categories. Obtained from the US Census Bureau, Health Insurance Coverage in the United States: 2016. Individuals may have more than one type of insurance.
A by-product of rising health care costs is increased “cost sharing” between the insured and the insurer. This includes higher premiums, deductibles, and co-pays. Cost sharing impacts all forms of coverage except Medicaid and results in another tier of patients—the underinsured. Out-of-pocket spending accounted for 11% of health expenditures ($352.5 billion) in 2016, a 3.9% increase, exceeding the average annual growth in 2008–2015 (2.0%).4 The high cost associated with glioma management results in significant financial burden even if only a small proportion of cost is shared by the patient. For many, the problem is further compounded by frequent loss of employment associated with disability. Consequently, patients may experience significant financial toxicity, often having to choose between treatment and other essential life costs (food, utilities, etc).5 Either way, underinsurance potentially culminates in adverse outcomes for patients with gliomas.
In an effort to control insurance premiums, insurers restrict access to smaller networks of hospitals and physicians. Often excluded are tertiary programs. Data suggest that glioma outcomes at high-volume referral programs, historically in academic programs, are superior to those at less experienced centers.6 Specialized centers have increased access to clinical trials and more rapidly adapt novel technology and therapies. As insurance networks shrink, so does access to more experienced care, resulting in potentially worse outcomes. Patients seeking care outside of approved networks assume even greater responsibility for the financial burden associated with treatment.
In an attempt to improve health care access and delivery and decrease cost, the Affordable Care Act (ACA) was signed by President Obama in 2010. Among other mandates, the ACA required employers to provide “affordable” insurance to employees and individuals to purchase insurance or pay a penalty. To assist low-income individuals, Medicaid was expanded to cover all individuals with incomes up to 138% of the federal poverty level. In 2012 the Supreme Court reversed this provision, allowing states to opt out of Medicaid expansion. Consequently, Medicaid eligibility remained unchanged in multiple states (18 states in 2017). Analysis has demonstrated that a large number of previously uninsured individuals obtained coverage, including a significant proportion through Medicaid in states that chose to expand coverage. However, some physicians remain reluctant to accept Medicaid patients because of low reimbursement. ACA addressed this issue by improving reimbursement to primary care physicians. This benefit did not extend to specialties. Consequently, the impact of Medicaid expansion is nonuniform and potentially remains a barrier to access.
ACA created marketplaces through which individuals could purchase insurance. Plans available on the exchange must meet certain criteria. Marketplace plans must cover at least 60% of total medical expenses on average. As such, patients with plans providing the lowest allowable level of coverage (also the lowest premium) are still responsible for 40% of medical expenses. Policies providing more comprehensive coverage are available at greater expense. Marketplace plans did not resolve cost sharing, as patients remain responsible for deductibles and co-pays. Analyses of the impact of the changes predict decreased costs to patients, although they remain high.7
The findings reported by Brown et al2 in their review of the National Cancer Database are consistent with previous reports—insurance impacts treatment and outcomes. Insurance is a surrogate for other socioeconomic factors that cannot be addressed in a registry review. Furthermore, not all private and Medicare policies are alike in terms of cost sharing and treatment access. Within these groups there is likely to be differences in outcomes. The review could not address disease-related financial toxicity and the resulting adverse impact on quality of life. A recent survey by the Federal Reserve Board reported that 46% of adults could not cover a $400 emergency expense. The magnitude of cost sharing far exceeds this value. In fact, 46% of respondents who experienced an unexpected medical expense were in debt as a result.8 Insurance is a critical element to individual well-being. The current trend of increasing cost sharing even among privately insured patients is problematic. Ultimately, the cost of care drives the challenges we face as a society. While it is critical to address how we pay for it, the discussion must also include cost containment. Although the merits of the ACA are debated, it is a first step toward addressing the significant shortcomings of health care in the US. The discussion must continue, as the quality and quantity of coverage still falls well short of that of which we are capable.
Conflict of interest/authorship statement
I have no conflict of interest related to the topic. I am accountable for all aspects of the submission.
References
- 1. Bor J, Cohen GH, Galea S. Population health in an era of rising income inequality: USA, 1980-2015. Lancet. 2017;389(10077):1475–1490. [DOI] [PubMed] [Google Scholar]
- 2. Brown DA, Himes BT, Kerezoudis P, et al. Insurance correlates with improved access to care and outcome among glioblastoma patients. Neuro Oncol. 2018;20(10):1374–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Health Insurance Coverage in the United States: 2016. https://www.census.gov/content/dam/Census/library/publications/2017/demo/p60-260.pdf Accessed July 15, 2018. [Google Scholar]
- 4. National Health Expenditure Accounts. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nationalhealthaccountshistorical.html Accessed July 15, 2018. [Google Scholar]
- 5. Kent EE, Forsythe LP, Yabroff KR, et al. Are survivors who report cancer-related financial problems more likely to forgo or delay medical care?Cancer. 2013;119(20):3710–3717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Curry WT Jr, Carter BS, Barker FG II. Racial, ethnic, and socioeconomic disparities in patient outcomes after craniotomy for tumor in adult patients in the United States, 1988-2004. Neurosurgery. 2010;66(3):427–437; discussion 437. [DOI] [PubMed] [Google Scholar]
- 7. Dusetzina SB, Keating NL. Mind the gap: why closing the doughnut hole is insufficient for increasing medicare beneficiary access to oral chemotherapy. J Clin Oncol. 2016;34(4):375–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Report on the Economic Well-Being of U.S. Households in 2015. https://www.federalreserve.gov/2015-report-economic-well-being-us-households-201605.pdf Accessed July 15, 2018. [Google Scholar]