Abstract
Background
Green, blue, and purple tattoo pigments are often the colors most resistant to laser removal. Recently, the first ever production picosecond‐domain laser with a 785 nm wavelength was developed to improve the rate of clearance of green, blue, and purple tattoo inks.
Methods
Twenty‐two tattoos from 15 subjects with skin phototypes II–IV were enrolled in the study. A total of four treatments were administered using a single 785 nm picosecond‐domain laser wavelength. Blinded assessment of digital, cross‐polarized photographs taken approximately 8 weeks following the last treatment was performed using an 11‐point clearance scale.
Results
Fourteen subjects with 21 tattoos completed all study visits. The 21 tattoos contained the following pigments: black (n = 15), green (n = 13), blue (n = 8), yellow (n = 5), purple (n = 4), and red (n = 3). Treatments were performed with a 2‐4‐mm beam diameter and fluences ranging from 1.1 to 3.1 J/cm2. Blinded assessment of photographs found 85%, 81%, 74%, 61%, 11%, and 5% clearance from baseline photos for purple, blue, green, black, red, and yellow pigments, respectively. Treatments were well tolerated with typical erythema, edema and one case of pinpoint bleeding. No scarring was noted.
Conclusion
This first study of a new 785 nm picosecond‐domain laser demonstrates safe and effective removal of multicolor tattoos. Although clearance was shown for a multitude of colors including black, the 785 nm laser wavelength has special affinity to purple, blue and green tattoo pigments. Lasers Surg. Med. 50:704–710, 2018. © 2018 The Authors. Lasers in Surgery and Medicine Published by Wiley Periodicals, Inc.
Keywords: tattoo, picosecond, removal, treatment, 785 nm
INTRODUCTION
Picosecond‐domain lasers have added to the treatment options for laser tattoo removal, joining the Q‐switched, nanosecond‐domain devices that have been the mainstay for laser tattoo removal using selective photothermolysis 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27. The shorter pulse‐durations offered by picosecond‐domain lasers were developed to remove tattoos in fewer treatments, as compared to nanosecond‐domain devices. Difficulty comparing picosecond‐domain lasers to nanosecond‐domain devices results from differences in available fluences, beam diameters, and peak powers between the two types of devices. Exact comparisons of these devices need to compare maximally tolerated fluences for each color within a given tattoo 15, 23. A dramatic demonstration of a qualitative difference between nanosecond‐domain and picosecond‐domain lasers in clearing tattoo pigments is the ability to remove yellow tattoo inks in a few treatments with picosecond‐domain devices 22, 23, despite tremendous difficulty removing yellow ink with nanosecond‐domain devices 15.
The new picosecond‐domain lasers not only offer shorter pulse‐durations than earlier‐generation, nanosecond‐domain lasers, but many also offer laser‐pumped lasers that deliver the three main wavelengths used to treat multi‐color tattoos: 1064 nm infrared laser energy predominantly for removing black ink, 532 nm green light to remove red, yellow, and orange ink, and 755 nm red light to remove blue, green, and purple inks 16, 17, 20, 21, 22, 23, 24, 26, 27. The highest energy will come from the primary wavelength generated from a device, since conservation of energy dictates that there will be loss when converting from one wavelength to another. In this study, we investigate the first production 785 nm, titanium:sapphire (Ti:sapphire) laser for removing multicolored tattoos, assessing both the safety and efficacy of this device. This wavelength is generated by converting the 532 nm second harmonic of the primary 1064 nm picosecond‐domain laser into 785 nm laser light using a laser‐pumped, laser handpiece.
MATERIALS AND METHODS
Subjects
This is a prospective study demonstrating the safety and efficacy of a new picosecond‐domain Ti‐sapphire laser for the treatment of decorative professional tattoos. The study was reviewed and approved by an Institutional Review Board (IRB) for treatment of human subjects. Subjects were included if they had decorative tattoos that were previously untreated and were required to have at least black, blue, or green tattoo ink. Enrollment was open to males and females ages 18–70 and all Fitzpatrick skin types (I–VI). Some subjects had more than one tattoo treated, yielding a total of 22 multicolor tattoos from 15 subjects treated in this study. Five males and 10 females enrolled into the study. Two subjects had skin type II, 9 had skin type III and 4 had skin type IV. No subjects with Fitzpatrick skin types I, V, or VI presented for inclusion into the study. The ages of the subjects ranged from 20 to 57 years, averaging 36.
A breakdown of the tattoos treated are as follows: one subject had three tattoos treated, five subjects had two tattoos treated, and nine subjects had a single tattoo treated. The subject that had three tattoos treated was a female 30 years old, with Fitzpatrick skin type IV. Of the five subjects who had two tattoos treated in the study, one was male and four were female, their ages ranged from 30 to 45 and averaged 39 years, and three were Fitzpatrick skin type III, while one had skin type II, and the other had skin type IV. Although the most common tattoo color in this study was black (n = 15), 13 tattoos had green ink, eight tattoos had blue ink, five tattoos had yellow ink, four tattoos had purple ink, and three tattoos had red ink.
Laser
A prototype handpiece housing a 785 nm Ti‐sapphire laser was used for this study. The Ti‐sapphire laser was pumped with picosecond‐domain 532 nm pulses delivered from a commercially available Nd:YAG picosecond‐domain laser system incorporating a potassium titanyl phosphate (KTP) frequency doubling crystal (PicoWay®, Syneron‐Candela Corporation, Wayland, MA) enabling the delivery of three wavelengths: 1064 nm, 532 nm, and 785 nm, from a single device. The Ti‐sapphire laser delivered up to 120 mJ pulses at 785 nm with a pulse‐duration of 300 ps. Laser beam diameters included a 2‐, 3‐, and 4‐mm beam selected via lens cartridges. The highest fluences available was 3.1 J/cm2, delivered with a 2‐mm spot size. The laser repetition rate was adjustable from 1 to 10 Hz, but treatments were done at 3 Hz.
Laser Treatment
For most subjects, anesthesia was injected intra‐dermally using 0.5% lidocaine with 1:200,000 epinephrine or 1% plain lidocaine, depending upon the subject's concurrent medications. One subject requested topical lidocaine cream (L.M.X. 4, Ferndale Laboratories, Inc. Ferndale, MI) while three subjects elected to be treated without any anesthesia (Table 1). A hydrogel dressing (Vigilon, CR Bard, Inc., Covington, CA) was applied over the tattoo, and the laser treatment was delivered through it to protect the epidermis and minimize the risk of scarring, as well as to prevent the hazard of aerosolized blood and skin impacting the treatment provider throughout the laser treatment.
Table 1.
Summary of Treatment Parameters and Pain Scores at Each Treatment Visit
| Parameter | Tx1 | Tx2 | Tx3 | Tx4 |
|---|---|---|---|---|
| Treatment | ||||
| Mean fluence (J/cm2) (range) | 1.4 (1.2–1.6) | 2.6 (1.1–3.0) | 3.0 (2.0–3.1) | 2.0 (2.0–2.0) |
| Spot size range (mm) | 3 | 2–4 | 2–3 | 3 |
| Tattoos treated | 22 | 22 | 20 | 20 |
| Median No. of pulses (range) | 261 (34–952) | 221 (43–1,149) | 296 (60–1,547) | 364 (68–1,538) |
| Anesthesia/Pain | ||||
| Lidocaine injection, n | 14 | 14 | 13 | 13 |
| Median pain (range) | 0.3 (0–5) | 0.5 (0–3) | 1.0 (0–5) | 0.0 (0–4) |
| LMX, n | 3 | 3 | 3 | 3 |
| Median pain (range) | 1.0 (1–1) | 3.0 (3–3) | 4.0 (4–4) | 3.0 (3–3) |
| None, n | 5 | 5 | 4 | 4 |
| Median pain (range) | 6.0 (5–7) | 6.5 (6–7) | 7.0 (6–7) | 6.0 (5–7) |
All tattoos, regardless of color, were treated with the Ti‐sapphire 785 nm, picosecond‐domain laser. Although other wavelengths may have been considered more optimal for various tattoo pigments, such as black, 785 nm was intentionally administered to all colors to assess the their responses to the 785 nm wavelength. In practice, the 785 nm Ti‐sapphire laser would typically be selected for blue, green and purple tattoo ink, and the 1064 nm wavelength would be used for black ink, while the 532 nm laser would be reserved for yellow and red ink. All subjects received four treatments by the principal investigator, with treatments administered at 6–10 week intervals. Fluences that resulted in immediate whitening of the treated area without pinpoint bleeding were selected by the treating physician. As tattoos were removed, subsequent treatments required higher fluences to achieve this endpoint (Table 1). The 4th and final treatment was administered using a lower average fluence, because the treating physician chose to use a 3‐mm beam diameter as opposed to a 2‐mm beam, to ensure adequate depth of penetration of laser energy for the final treatment, assuming more superficial pigment had been removed by the prior treatments. Treatments were performed while viewing the tattoo using a cross‐polarizing headlamp that fit over protective laser goggles to better visualize tattoos (v600, Syris Scientific, Gray, ME). Eye protection was worn by all personnel and the patient in the treatment room.
Blinded Evaluation of Digital Images
Digital photographs (D80, Nikon Corporation, Melville, NY) were taking by the treating physician. Typically, two fixed focal lengths were used depending upon the size of the tattoo. Photographs were taken with a cross‐polarized flash (Canfield Scientific, Fairfield, NJ) to limit surface reflections. With cross‐polarization, the view of the tattoo is enhanced over what is seen visually, making them look more prominent than they are with the unaided eye. Photographs were taken at baseline, and 8‐weeks following the fourth, and final, treatment session. Baseline and follow‐up photographs were randomized and placed in a PowerPoint presentation, and graded by three blinded independent reviewers using an 11‐point clearance scale (0 = no clearance, 1 = 10%, 2 = 20%, 3 = 30% clearance to 10 = 100% or total clearance). If the baseline image was incorrectly identified by a reviewer, the reviewer's evaluation would be given a negative score (i.e., a score of 3 would be recorded as a −3).
Side Effects
Immediately following each treatment session erythema, edema, crusting, purpura, blistering, and pin‐point bleeding were evaluated by the treating physician using a 4‐point scale where 0 = absent, 1 = mild, 2 = moderate and 3 = severe forms of each treatment effect listed above. Hypopigmentation, hyperpigmentation and scarring were evaluated 8‐weeks following the final treatment. Pigmentary alterations or scarring were rated on a 4‐point scale with: 0 = none, 1 = mild, 2 = moderate, and 3 = severe hyperpigmentation, hypopigmentation, or scarring.
RESULTS
Fifteen subjects enrolled in the study presenting with 22 tattoos. One female subject with one tattoo dropped from the study after receiving two treatments due to scheduling difficulties. One tattoo completely cleared after two treatments. The remaining 20 tattoos received four treatments with the 785 nm picosecond‐domain laser.
Blinded Evaluation of Digital Images
Comparison of baseline and final cross‐polarized images revealed improvement scores of 8.5 ± 1.2 (85%), 8.1 ± 1.6 (81%), 7.4 ± 1.7 (74%), 6.1 ± 1.8 (61%), 1.1 ± 0.8 (11%), and 0.5 ± 0.5 (5%), for purple, blue, green, black, red, and yellow inks respectively using a 0–10 scale (Figs. 1 and 2). No reviewer misidentified any baseline image as a treatment image, which is typical for laser tattoo removal studies.
Figure 1.
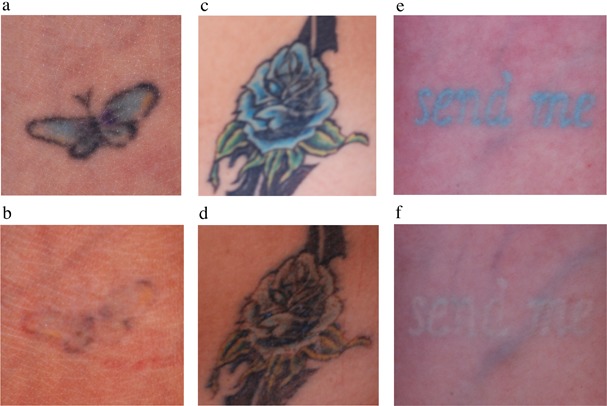
Cross‐polarized, digital images taken before (a,c,e) laser treatment and after (b,d,f) the 4th treatment. Purple, blue, and green pigment cleared almost completely, while some residual yellow and black ink are clearly visible. Cross‐polarized photography enhances visibility of tattoos over conventional lighting or non‐polarized flash photography.
Figure 2.
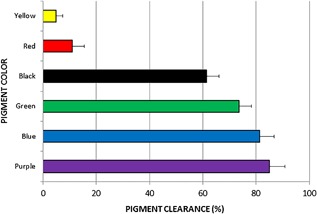
Average clearance for each tattoo color treated with the 785 nm wavelength are shown following the 4th treatment. Purple ink was the most completely removed followed by blue, green, black, red, and yellow (Error bars show sem).
Side Effects
Pinpoint bleeding was noted in one subject following a single treatment (1.7%), edema was seen after 50% of the treatments, and erythema in 81% of treatments. No purpura, blistering, or crusting was seen immediately after treatment, although these are common side‐effects of tattoo treatment days following treatment. No scarring, hyperpigmentation or hypopigmentation was noted during any 8‐week follow‐up visit.
Pain during treatment generally scaled with laser fluence and the anesthesia used (Table 1). The maximum median pain score was 7 for the group of subjects who elected no anesthesia and occurred during the third treatment in which the highest fluence was used. For the lidocaine group, the maximum median pain score was 1, occurring during the third treatment when the maximum fluence was used.
DISCUSSION
This study demonstrates that the new picosecond‐domain, 785 nm, Ti‐sapphire, laser‐pumped laser effectively removes blue, green, and purple tattoos; and as expected, is less effective at removing other colors that are more appropriately addressed by the 1064 and 532 nm wavelengths also available from the device used in this study. In the current study: purple, blue, and green ink improved 85%, 81%, and 74%, respectively, after four treatments, demonstrating the ability to the new 785 nm, Ti:Sapphire, laser‐pumped laser to remove these pigments in a similar fashion to the 755 nm alexandrite laser. Figure 3 shows a comparison of tattoo clearance in the current study to a similar study done by the same investigators, but treating with the 1064 nm and 532 nm wavelengths delivered by the same device as was used in this study 23. As expected, red and yellow inks were not well treated with the 785 nm laser wavelength and would have presumably been removed better using 532 nm. Black ink would also have more likely cleared more completely if treated with the 1064 nm Nd:YAG laser.
Figure 3.
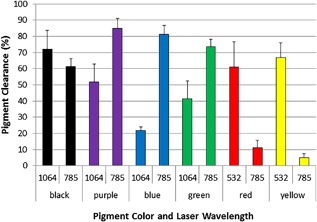
Average clearances for each tattoo color treated with the 785 nm wavelength compared to an earlier study that using the same device but with the 1064 nm and 532 nm wavelengths. Clearance was determined by blinded reviewers following the 4th treatment using an identical scale in each study. Purple, blue, and green inks show the most benefit from 785 nm treatment, while black ink was cleared more effectively by 1064 nm and red and yellow by 532 nm, as expected (Error bars show sem).
Bencini et al. studied 352 tattoos and found that 96% contained black ink, and 71% were only black, with 23% contained red, 9% had yellow ink, and 26% contained green, blue, or violet ink. White ink was present in 5% of tattoos 25, and most likely present in another 5% where it was used to create colors such as light blue or pink. The importance of knowing what colors commonly occur in tattoos, is that this knowledge directs laser surgeons toward what wavelengths are most crucial to laser tattoo removal. Because black and red are the most common tattoo pigments by far, it is most critical to have higher available fluences at 1,064 nm and 532 nm to treat these most common pigments. The Nd:YAG laser emitting at 1064 nm is more effective at removing black tattoo ink, as compared to the 755 nm alexandrite and 532 nm KTP lasers. Because the 1,064 nm Nd:YAG wavelength is the longest available, it is also the least likely wavelength to target epidermal melanin pigment causing hypopigmentation, an unwanted side effect when treating tattoos. Black ink also tends to require more treatments compared to the other inks. Thus, the most desirable primary laser wavelength used for treating tattoos should be 1064 nm because the primary wavelength is the wavelength with the greatest available total energy. Converting the primary wavelength to 532 nm using a KTP frequency‐doubling crystal, or as is the case with the current study, to 785 nm using a Ti:Sapphire crystal, results in a loss of energy during the conversion process. However, having three wavelengths available to target all colors in a tattoo is critical as evidenced in the Bencini et al. study 25 which showed that over a quarter of tattoos contain green, purple, or blue ink that has traditionally been targeted by the 755 nm alexandrite laser, and was shown here to respond to the 785 nm Ti:Sapphire laser as well.
The Ti:Sapphire laser used in the current study has a very short, 300 ps, pulse‐duration enabling high peak powers. Typically, Q‐switched alexandrite laser have relatively long pulse‐durations in the 50–100 ns range, compared to 5–10 ns for Q‐switched, Nd:YAG lasers delivering 1064 and 532 nm laser energy 8, 9, 10, 11, 12, 13, 17. The new picosecond‐domain, 755 nm lasers represent a major shortening of the pulse‐duration from 50 to 100 ns to approximately 500–900 ps 20, 21. This shorter pulse‐duration should deliver better tattoo removal for green, blue and purple inks, as compared to earlier‐generation, nanosecond‐domain devices. Saedi et al. and Brauer et al. demonstrated a greater than 75% clearance of most blue and black tattoos treated in their studies in 1–5 treatments. However, Saedi et al. used a 4‐point scale to rate photographs without giving a score of no improvement a unique zero value, and the scale used to gauge improvement for the Brauer et al. study was not detailed; so, direct comparisons to the results of the current study are not possible 20, 21.
Almost 2 decades ago, Herd et al. compared an early picosecond‐domain, Ti:sapphire laser to a 752 nm Q‐switched alexandrite laser and found the former to be more effective 17. Their study demonstrated the promise of picosecond‐domain lasers, and more specifically the Ti:sapphire laser, but has little relevance to relative comparisons of modern Q‐switched versus nanosecond‐domain lasers currently on the market. In addition, the long time between the development of the first prototype Ti‐sapphire and other picosecond‐domain lasers to the first production versions of these devices speaks to the technical challenges of bringing this technology to the clinic.
The development of a convenient and cost‐effective, laser‐pumped, Ti:Sapphire laser handpiece enables generation of a 3rd wavelength of laser energy from this single device for treating blue, green, and purple tattoo inks. The handpiece simply screws onto the distal end of the articulated arm of the laser device. It is effectiveness at treating blue, green, and purple tattoos was demonstrated in this study. Laser‐pumped lasers have advantages over dye‐cartridge handpieces that attach to Q‐switched or nanosecond‐domain lasers and deliver alternate wavelengths as well 10. These dye handpieces have much more limited lifetimes, and more importantly, as they are not true lasers they do not deliver specific wavelengths of light, but rather a range of wavelengths. This potential for wavelengths drift from dye handpieces attached to Q‐switched and nanosecond‐domain lasers can present an ocular hazard as well as potentially delivering variable clinical results. In addition, as the handpieces age with use, their output can decrease necessitating their replacement. The first true laser‐pumped laser handpieces were utilized with a Q‐switched alexandrite laser, enabling conversion of the primary 755 nm wavelength to both 1064 nm and 532 nm laser energy 10. This laser‐pumped laser technology was applied here to create the first production Ti:Sapphire, 785 nm, 300 picosecond pulse‐duration laser, and was shown to be effective at removing blue, green, and purple tattoos.
Lorgeou et al. compared a nanosecond‐domain laser to two picosecond‐domain lasers using a split tattoo design, where one‐half of a tattoo was treated with one of two picosecond‐domain lasers, and the other with a Q‐switched, nanosecond‐domain laser. They found that the picosecond‐domain lasers were more effective; 26 however, the nanosecond‐domain device they used is significantly underpowered compared to most Q‐switched, nanosecond‐domain lasers currently on the market. To make adequate comparisons between the two modalities, a split‐tattoo design as used by Lorgeou et al 26. using the state‐of‐the‐art Q‐switched lasers currently on the market would need to be done while using the maximally tolerated fluences (MTFs) with each device 23.
Pinto et al. compared a modern, high‐powered, Q‐switched, nanosecond‐domain laser to a high‐powered picosecond‐domain laser using a split‐tattoo design and administering two treatments at 6 week intervals to untreated and previously treated black tattoos. They treated using MTFs with each device using whitening as a clinical endpoint. These investigators also used a 4‐point scale without a separate score for no improvement. They found no difference in clearance between the Q‐switched lasers and picosecond‐domain lasers 27. A more granular scale, or more importantly, more treatment sessions may have been able to unmask differences between these devices; however, this study using adequate fluences and modern devices and showed no difference between the devices after two treatments. The difference in pulse‐duration between the two lasers used by Pinto et al. was approximately 10‐fold shorter for the picosecond‐domain device 27. This difference is much greater when comparing Q‐switched alexandrite lasers to their picosecond counterparts, where the difference in pulse‐durations is 100‐fold or more for alexandrite, or Ti:sapphire, picosecond‐domain lasers compared to Q‐switched alexandrite lasers. Although no difference was found when treating black ink with pulse durations that vary 10‐fold by Pinto et al., 27 dramatic responses were seen when treating yellow tattoos that were typically unresponsive to Q‐switched, 532 nm lasers, with a picosecond‐domain 532 nm lasers having a pulse‐duration that was approximately 10‐fold shorter. The picosecond‐domain lasers cleared yellow tattoos in only a few treatments despite little‐to‐no response from their nanosecond‐domain counterparts 22, 23. Thus the relationship between pulse‐duration, tattoo ink composition, age of tattoo, and the biology of individual patients needs to be further explored to fully understand the optimal clinical situations where the advantages of picosecond‐domain lasers are the greatest. The ability to have three or more wavelengths of true laser energy is an obvious advantage of most picosecond‐domain devices currently on the market, as well as the multi‐functionality of offering additional settings and handpieces which enable laser treatments for rejuvenation of photodamage and treatment of acne scarring 28, 29.
Further study of tattoo inks should enable better laser and ink designs aimed at optimizing tattoo removal and tattoo safety. Hogsberg et al. studied various tattoo inks and characterized their chemical structure, which included organic crystals, inorganic crystals, and graphite and measured particle size with black inks having the smallest size at 40 nm, followed by blue inks at 100 nm, with still other colors reaching 200 nm in diameter. White inks, containing titanium dioxide were 1000 nm in size 30. These white particles are often mixed with other colors to lighten them. Light blue, light purple, light green, and pink are examples of pigments created by mixing white with blue, purple, green, or red pigments. This creates a risk of gray discoloration which commonly occurs when treating white pigments, which can be very resistant to removal. It remains to be seen if even shorter pulse‐durations will be less wavelength dependent as has been postulated and able to remove all colors equally, as this is not the case for current picosecond‐domain lasers.
Future developments, such as even shorter pulse‐durations enabling higher peak powers, as well as higher‐powered lasers, should enable even more rapid clearance of tattoos going forward. Further research should yield insights into laser‐tattoo interactions and the biology of tattoo removal, including attention to re‐designed tattoo inks with both safety and removability in mind.
ACKNOWLEDGMENTS
Dr. Bernstein is a consultant for Syneron‐Candela and has equity in Syneron‐Candela. Drs. Bhawalkar and Schomacker were employees of Syneron‐Candela at the time this study was completed. Research funding for this project and loan of equipment were provided by Syneron‐Candela.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
REFERENCES
- 1. Taylor CR, Gange RW, Dover JS, Flotte TJ, Gonzalez E, Michaud N, Anderson RR. Treatment of tattoos by Q‐switched ruby laser. A dose‐response study. Arch Dermatol 1990; 126:893–899. [PubMed] [Google Scholar]
- 2. Scheibner A, Kenny G, White W, Wheeland RG. A superior method of tattoo removal using the Q‐switched ruby laser. J Dermatol Surg Oncol 1990; 16:1091–1098. [DOI] [PubMed] [Google Scholar]
- 3. Ashinoff R, Geronemus RG. Rapid response of traumatic and medical tattoos to treatment with the Q‐switched ruby laser. Plast Reconstr Surg. 1993; 91:841–845. [DOI] [PubMed] [Google Scholar]
- 4. Kilmer SL, Anderson RR. Clinical use of the Q‐switched ruby and the Q‐switched Nd:YAG (1064 nm and 532 nm) lasers for treatment of tattoos. J Dermatol Surg Oncol. 1993; 19:330–338. [DOI] [PubMed] [Google Scholar]
- 5. Levine VJ, Geronemus RG. Tattoo removal with the Q‐switched ruby laser and the Q‐switched Nd:YAG laser: a comparative study. Cutis 1995; 55:291–296. [PubMed] [Google Scholar]
- 6. Kilmer SL, Lee MS, Grevelink JM, Flotte TJ, Anderson RR. The Q‐switched Nd:YAG laser effectively treats tattoos. A controlled, dose‐response study. Arch Dermatol. 1993; 129:971–978. [PubMed] [Google Scholar]
- 7. Jones A, Roddey P, Orengo I, Rosen T. The Q‐switched ND:YAG laser effectively treats tattoos in darkly pigmented skin. Dermatol Surg 22:999–1001, 1996. [DOI] [PubMed] [Google Scholar]
- 8. Fitzpatrick RE, Goldman MP. Tattoo removal using the alexandrite laser. Arch Dermatol 1994; 130:1508–1514. [PubMed] [Google Scholar]
- 9. Alster TS. Q‐switched alexandrite laser treatment (755nm) of professional and amateur tattoos. J Am Acad Dermatol 1995; 33:69–73. [DOI] [PubMed] [Google Scholar]
- 10. Bernstein EF, Bhawalkar J, Clifford J, Hsia J. Treatment of tattoos with a 755‐nm Q‐switched alexandrite laser and novel 1064 nm and 532 nm Nd:YAG laser handpieces pumped by the alexandrite treatment beam. J Drugs Dermatol 2010; 9:1333–1339. [PubMed] [Google Scholar]
- 11. Stafford TJ, Lizek R, Tan OT. Role of the Alexandrite laser for removal of tattoos. Lasers Surg Med 1995; 17:32–38. [DOI] [PubMed] [Google Scholar]
- 12. Leuenberger ML, Mulas MW, Hata TR, Goldman MP, Fitzpatrick RE, Grevelink JM. Comparison of the Q‐switched alexandrite, Nd:YAG, and ruby lasers in treating blue‐black tattoos. Dermatol Surg 1999; 25:10–14. [DOI] [PubMed] [Google Scholar]
- 13. Bukhari IA. Removal of amateur blue‐black tattoos in Arabic women of skin type (III‐IV) with Q‐switched alexandrite laser. J Cosmet Dermatol 2005; 4:107–101. [DOI] [PubMed] [Google Scholar]
- 14. Zelickson BD, Mehregan DA, Zarrin AA, Coles C, Hartwig P, Olson S, Leaf‐Davis J. Clinical, histologic, and ultrastructural evaluation of tattoos treated with three laser systems. Lasers Surg Med 1994; 15:364–372. [DOI] [PubMed] [Google Scholar]
- 15. Bernstein EF, Civiok JM. A continuously variable beam‐diameter, high fluence, Q‐switched Nd:YAG laser for tattoo removal: comparison of the maximum beam diameter to a standard 4‐mm diameter treatment beam. Lasers Surg Med 2013; 45:621–627. [DOI] [PubMed] [Google Scholar]
- 16. Ross V, Naseef G, Lin G, Kelly M, Michaud N, Flotte TJ, Raythen J, Anderson RR. Comparison of responses of tattoos to picosecond and nanosecond Q‐switched neodymium: YAG lasers. Arch Dermatol 1998; 134:167–171. [DOI] [PubMed] [Google Scholar]
- 17. Herd RM, Alora MB, Smoller B, Arndt KA, Dover JS. A clinical and histologic prospective controlled comparative study of the picosecond titanium:sapphire (795 nm) laser versus the Q‐switched alexandrite (752 nm) laser for removing tattoo pigment. J Am Acad Dermatol 1999; 40:603–606. [DOI] [PubMed] [Google Scholar]
- 18. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 1983; 220:524–527. [DOI] [PubMed] [Google Scholar]
- 19. Anderson AA, Parrish JA. Microvasculature can be selectively damaged using dye lasers: a basic theory and experimental evidence in human skin. Lasers Surg Med 1981; 3:263–276. [DOI] [PubMed] [Google Scholar]
- 20. Saedi N, Metelitsa A, Petrell K, Arndt KA, Dover JS. Treatment of tattoos with a picosecond alexandrite laser: a prospective trial. Arch Dermatol 2012; 148(12):1360–1363. [DOI] [PubMed] [Google Scholar]
- 21. Brauer JA, Reddy KK, Anolik R, et al. Successful and rapid treatment of blue and green tattoo pigment with a novel picosecond laser. Arch Dermatol 2012; 148(7):820–823. [DOI] [PubMed] [Google Scholar]
- 22. Alabdulrazzaq H, Brauer JA, Bae YS, Geronemus RG. Clearance of yellow tattoo ink with a novel 532‐nm picosecond laser. Lasers Surg Med 2015; 47(4):285–288. [DOI] [PubMed] [Google Scholar]
- 23. Bernstein EF, Schomacker KT, Basilavecchio LD, Plugis JM, Bhawalkar JD. A novel dual‐wavelength, Nd:YAG, picosecond‐domain laser safely and effectively removes multicolor tattoos. Lasers Surg Med 2015; 47:542–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kauvar ANB, Keaney TC, Alster T. Laser treatment of professional tattoos with a 1064/532‐nm dual‐wavelength picosecond laser. Dermatol Surg 2017; 43:1434–1440. [DOI] [PubMed] [Google Scholar]
- 25. Bencini PL, Cazzaniga S, Tourlaki A, Glaimberti MG. Removal of tattoos by Q‐switched laser: variables influencing outcome and sequelae in a large cohort of treated patients. Arch Dermatol 2012; 148:1364–1369. [DOI] [PubMed] [Google Scholar]
- 26. Lorgeou A, Perrillat Y, Gral N, Lagrange S, Lacour JP, Passeron T. Comparison of two picosecond lasers to a nanosecond laser for treating tattoos: a prospective randomized study on 49 patients. J Eur Acad Dermatol Venereol 2017; 32:265–270. [DOI] [PubMed] [Google Scholar]
- 27. Pinto F, Große‐Büning S, Karsai S, et al. Neodymium‐doped yttrium aluminium garnet (Nd:YAG) 1064‐nm picoseond laser vs Nd:YAG 1064‐nm nanosecond laser in tattoo removal: a randomized controlled single‐blind clinical trial. Br J Dermatol 2017; 176:457–464. [DOI] [PubMed] [Google Scholar]
- 28. Brauer JA, Kazlouskaya V, Alabdulrazzaq H, et al. Use of a picosecond pulse duration laser with specialized optic for treatment of facial acne scarring. JAMA Dermatol 2015; 151(3):278–284. [DOI] [PubMed] [Google Scholar]
- 29. Bernstein EF, Schomacker KT, Bhawalkar JD. A novel fractional 1064 nm and 532 nm picosecond‐domain laser incorporating a holographic beam‐splitter improves facial photodamage. J Drugs Dermatol 2017; 16:1077–1082. [PubMed] [Google Scholar]
- 30. Hogsbert T, Loeschner K, Loft D, Serup J. Light and electron microscopic analysis of tattoos treated by q‐switched ruby laser. J Invest Dermatol 1991; 97:131–136. [DOI] [PubMed] [Google Scholar]


