Summary
Compared to its neighbors, Sri Lanka performs well in terms of health. Health care is provided for free in the public sector, yet households' out‐of‐pocket health expenditures are steadily increasing. We explore whether this increase can be explained by supply shortages and insufficient public health care financing or whether it is rather the result of an income‐induced demand for supplementary and higher quality services from the private sector. We focus on total health care expenditures and health care expenditures for specific services such as expenses on private outpatient treatments and expenses on laboratory and other diagnostic services. Overall, we find little indication that limited supply of public health care per se pushes patients into the private sector. Yet income is identified as one key driver of rising health care expenditures, ie, as households get richer, they spend an increasing amount on private services suggesting a dissatisfaction with the quality offered by the public sector. Hence, quality improvements in the public sector seem to be necessary to ensure sustainability of the public health care sector. If the rich and the middle class increasingly opt out of public health care, the willingness to pay taxes to finance the free health care policy will certainly shrink.
Keywords: free health care policy, health care demand, health care supply, Sri Lanka
If the health system is so good, why did the Health Minister go to Singapore for treatment? (Anura Kumara Dissanayake, Chief Opposition Whip, Sri Lanka).
1. INTRODUCTION
Sri Lanka is one of the best health performers in the South Asian region. On average, only 30 women die for 100 000 live births in Sri Lanka, this compares to 178 and 174 women in Pakistan and India, respectively.1 The infant mortality rate is estimated at 8 per 1000 children, which is significantly lower than Pakistan's rate of 66 and India's rate2 of 38. These better health indicators are often related to the good accessibility of health care services, government‐funded free health care facilities in public hospitals, and high levels of female education.3, 4, 5 Patients can in principle visit any government hospital in the country without restriction. Almost all the medical facilities provided by the government are supposed to be freely available for every citizen including all inpatient, outpatient, and community health services.
Yet substantial changes have been witnessed in terms of health care financing in Sri Lanka. According to our own calculations based on household survey data, the share of out‐of‐pocket health expenditures in total households' expenditures has increased from about 2% in 1990/1991 to almost 3.5% in 2012/2013. Rannan‐Eliya and Sikurajapathy3 report that the households' out‐of‐pocket health care expenditures represented about 33% of national health expenditure in 1953, 41% in 1980, and 48% in 2005. In contrast, the share of public funding for inpatient care, ancillary health services such as laboratory and imaging services and medical goods dispensed to outpatient have decreased6 steadily between 1990 and 2009. Govindaraj and colleagues,6 for example, report that the share of public expenditure in ancillary outpatient health care services declined significantly from 7% in 1990 to 3% in 2009. Expenditures for medical goods declined from 28% in 1990 to 18% in 2009.
Against this background, the main objective of this study is to address the puzzle of increasing households' out‐of‐pocket health expenditures in a context of a free health care policy. Precisely, we examine whether the declining trend of public health care financing can explain the increasing trend of out‐of‐pocket health expenditures and the seemingly increasing substitution of public by private health care services. This substitution is also subject of intense debates in Sri Lankan politics. Recently, the chief opposition whip attacked the Minister of Health stating “Pharmacies are mushrooming around hospitals because the free health service is not as free as it seems. There are hospitals and there are doctors, but the medication has to be bought from outside.”7
We do not only focus on total health care expenditures but also examine health care expenditures for specific services such as expenses on private outpatient treatments, expenses on laboratory and other diagnostic services, expenses on medicines and other pharmaceutical products, expenses on private hospitals, and expenses on specialist consultations. We use 6 waves of household survey data covering the period 1990 to 2013 and add to these data sets detailed information on public sector health care supply on the district level for the same period.
Our study is closely related to other papers that have explored the determinants of out‐of‐pocket health care expenditures in high‐income countries such as in the United States,8, 9 Australia,10 and Germany,11 but also in low‐ and middle‐income countries such as China,12 India,13, 14 Sri Lanka,15 and Nigeria.16 This literature has also shown that out‐of‐pocket health care expenditures can impose a significant financial burden on households resulting in catastrophic health expenditures and medical impoverishment (see, for example, previous studies17, 18, 19). Several studies highlight next to demand side factors also the importance of supply side factors such as availability of hospital beds and doctors.15, 20, 21
The remainder of this paper is organized as follows. The next section provides the institutional setting and documents the puzzle described above in more detail. It introduces in particular Sri Lanka's free health care policy and the trends in out‐of‐pocket health care expenditures. Section 3 presents the data used in this study and discusses descriptive statistics in relation to health care expenditures and potential covariates. Section 4 discusses the used empirical specifications. Section 5 presents the main results, and Section 6 discusses them. Section 7 concludes.
2. BACKGROUND
2.1. The health care system in Sri Lanka
Health care in any public hospital or health clinic is free. Public hospitals are divided into 3 main levels: primary, secondary, and tertiary. Primary hospitals that are located all over the island provide basic outpatient health care. Secondary hospitals that are mainly located in semiurban areas provide basic outpatient and some inpatient health care. Tertiary hospitals are mainly located in the larger cities and provide basic outpatient as well as specialized health care. In total, there are 622 public hospitals that consist of 488 primary hospitals, 69 secondary hospitals, and 65 tertiary hospitals.22 Public health care is financed through general tax revenues. Yet there are regularly shortages of medicines, laboratory and other diagnostic facilities, long queues for specialized health clinics and surgeries and overcrowded inpatient wards.23
Private health care is provided by a limited number of large private hospitals as well as private health clinics that are mostly run by public sector doctors as a dual practice service. There are 125 private hospitals that are mainly located in the Western province.24 Private health clinics are located in every part of the island. They usually provide basic outpatient services after the regular working hours, as most doctors work full time in public hospitals. According to Amarasinghe and colleagues,24 87% of private health care expenditures are funded through household out‐of‐pocket payments and only 5% and 7% are funded by private health insurance schemes and employee‐funded health schemes.
Every year, the government allocates funds in the order of 1.3% to 1.6% of GDP to public health care.25 This was 1.3% in 1990; it peaked at 1.6% in 2006 and then gradually decreased back to 1.3% in 2013. The bulk of the funding is allocated to the Ministry of Health (62%) and provincial departments of health (DOHs) (31%). The Ministry of Health provides health care services mainly through tertiary hospitals. Provincial hospitals (DOHs) in turn provide their services through primary and secondary hospitals. The highest share of public sector health expenditure is still allocated to inpatient care although it decreased from 83% in 1990 to 75% in 2013.
2.2. Trends in out‐of‐pocket health care expenditures
The data show an increasing trend of private health care usage and of out‐of‐pocket health care expenditures.23, 26 Kumara and Samaratunga15 find that on average, more than 60% of households incur out‐of‐pocket health care expenditures. In particular, households with elderly members and small children, and members with chronic health problems are at a high risk to incur significant out‐of‐pocket health care expenditures. Figure 1 shows that share of household out‐of‐pocket health care expenditures in total household expenditures significantly increased over the years.
Figure 1.
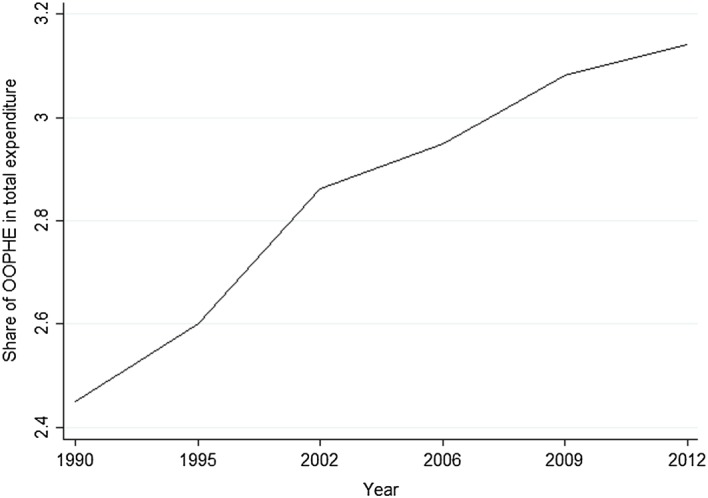
The share of out‐of‐pocket health care expenditure (OOPHE) in total expenditure by Sri Lankan households between 1990/1991 and 2012/2013
Households spent around 2% of their total expenditure on out‐of‐pocket health expenses in 1990/1991. Until 2012/2013, this share increased to around 3%, ie, by 50%. Note that this has been a period of sustained economic growth with a real annual GDP per capita growth rate of roughly 4.6%.27 Figure 2 shows that income growth alone does not seem to explain the rise in per capita out‐of‐pocket health care expenditures. Out‐of‐pocket health care expenditures rose much faster than household income. Whereas between 1990 and 2012 per capita household consumption expenditures increased by about 50%, per capita out‐of‐pocket health care expenditures increased by about 150%.
Figure 2.
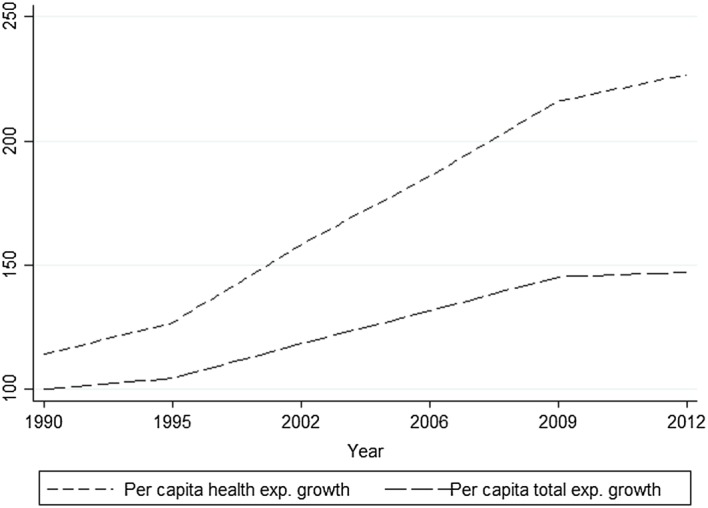
Household per capita health expenditure growth and per capita total expenditure growth between 1990/1991 and 2012/2013
3. DATA AND DESCRIPTIVE STATISTICS
3.1. Data sources
To analyze why out‐of‐pocket health care payments have risen under free health care policy, we use several data sources. First, we use data from Household Income and Expenditure Surveys (HIESs) conducted by the Department of Census and Statistics of Sri Lanka. HIES is a nationally representative cross‐sectional household survey started in 1980 and which since then has been conducted roughly every 5 years. Since 2006/2007, it is even conducted every 3 years in order to monitor the rapid changes of income and expenditure patterns in Sri Lanka.28 This study uses 6 waves of HIES data collected in 1990/1991, 1995/1996, 2002, 2006/2007, 2009/2010, and 2012/2013, respectively. Although HIES is aimed to cover all 25 districts of Sri Lanka, several northern and eastern districts had been excluded from the surveys in 1990/1991, 1995/1996, 2002, 2006/2007, and 2009/2010 due to the civil conflict that ended only in 2009. HIES has detailed information on household expenditure including food consumption, nonfood consumption, and out‐of‐pocket expenditures for health care. Health expenditures are recorded separately by expenditure category on a monthly basis. In addition, the survey records individual and household socio‐demographic information. We aggregated all information at the district level to obtain a district level panel set.
Second, in order to capture the trends and patterns of the public sector health care supply and demand, we use data from the Annual Health Statistics compiled by the Sri Lankan Ministry of Health. It gathers public sector health data on morbidity, mortality, resource availability, and services provision annually. We use in particular district level Annual Health Statistics data on public sector health care supply (number of hospital beds, number of doctors) and utilization (number of outpatients attendance, number of inpatient stays).
Third, we use administrative death registry data provided by the registrar general's department of the Ministry of Public Administration and Home Affairs.29 It covers the entire Sri Lankan population and registers every death case that has occurred in Sri Lanka. Based on this data, we calculated annual death rates at the district level.
Hence, we combine 3 sources of data at the district level and obtain a panel data set over 25 districts covering 6 points in time: 1990/1991, 1995/1996, 2002, 2006/2007, 2009/2010, and 2012/2013. The core of our analysis relies on a balanced panel where 8 northern and eastern districts are excluded from our analysis. It covers 17 districts with in total 102 observations. As a robustness check, we however replicate most of our results with the unbalanced panel of all 25 districts. The expenditure data are expressed in 2012/2013 Colombo prices.
3.2. Descriptive statistics
Figure 3 shows the trend of different categories of health care expenditures over time (in constant prices): expenses on private outpatient medical practitioners, payments for lab tests and other diagnostic services, spending on medicine and other pharmaceutical products, fees for specialist consultations, and expenses on private hospitals. According to Figure 3, payments for private outpatient health care services constitute the largest share of out‐of‐pocket health expenditures. Per capita monthly average expenses on private outpatient treatments increased in real terms from about 120 Rupees to almost 150 Rupees between 1990 and 2012. The increase for some subcategories was much stronger.
Figure 3.
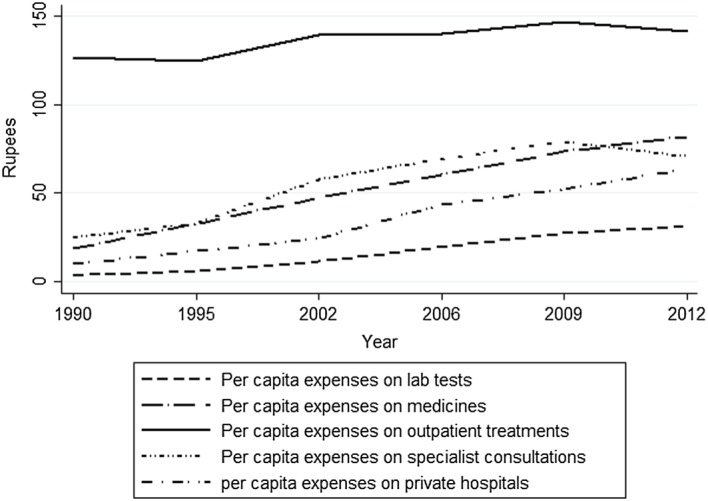
Monthly per capita out‐of‐pocket health care expenditure by different categories
Figure 4 depicts the trends and patterns of indicators reflecting the (potential) demand for health care services: The share of children aged 0 to 5 in the total population and the share of the adult population (aged 65 and above), the death rate per 1000 population, the number of outpatient visits per 100 000 population in public hospitals and clinics, and the number of inpatient visits per 100 000 population in public hospitals. The data on the changes in the age structure document the still ongoing demographic transition that has repercussions on the health care needs and expenditures. The data also show that the outpatient and inpatient attendance rates in public hospitals significantly increased over time as did expenditures for private health care.
Figure 4.
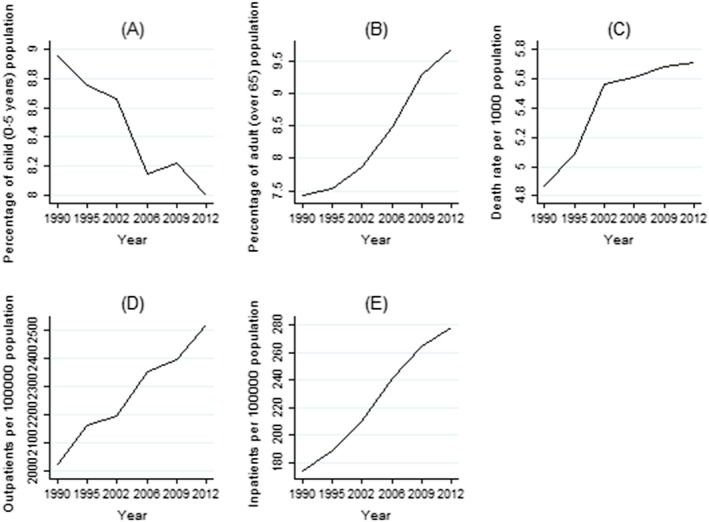
Trend and patterns of demand side variables
Figure 5 illustrates trends and patterns of supply side indicators including the number of hospital beds per 1000 population and the number of doctors per 100 000 population in public hospitals. Figure 5A and 5B shows that both, hospital beds and doctors, steadily increased over the years. We assume that these variables are good proxies of the available resources in the public health sector, although they do not necessarily reflect quality improvements of care.
Figure 5.
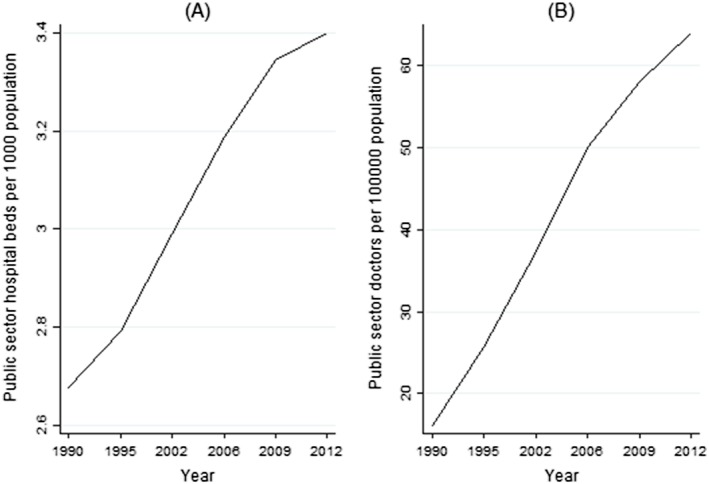
Trends and patterns of supply side variables
In the next sections, we will explore the relation between private health care expenditures and the supply and demand for health care in more detail using multivariate regression analysis and regression‐based factor decompositions in order to identify the underlying forces of rising private health expenditures.
4. EMPIRICAL SPECIFICATIONS
4.1. Regression model
To identify the drivers of rising out‐of‐pocket health care expenditures over time, we start with random‐effects regressions using the district panel data set. We focus on total out‐of‐pocket health care expenditures as well as on its different components. The model can be written as follows.
| (1) |
where lnY it stands for the log of the different health care expenditure categories in district i in period t. X mit is a vector of m potential demand side and supply side determinants, and β m is the vector of the associated coefficients to be estimated. District level random effects are denoted μ i. δ t denotes year‐specific effects that control for all time‐specific effects that are uniform across districts, such as the changes in the public health care policies and general trends in the health status. ε it stands for the district‐specific error term. Given the short panel and the small number of observation units, we prefer a random‐effects model over a fixed‐effects model. The data do not contain enough variation within districts over time that would allow us to identify the coefficients β m in a district fixed‐effects framework. It implies of course to make the strong assumption that μ i is uncorrelated with each explanatory variable in all time periods. To check the robustness of the estimates, we also estimate Equation (1) on the household level controlling for district fixed effects.
4.2. Factor decomposition
To disentangle the contribution of each factor captured by Equation (1) to rising out‐of‐pocket health expenditures, we use a regression‐based decomposition method proposed by Fields,30 which is an extension of Shorrocks.31 Formally, this decomposition can be written as follows:
| (2) |
where , , , and .
Note that and are estimates of the district and time effects, 1{⋅} is an index function, and is the residual from the estimation of (1). Applying the inequality decomposition, we obtain the proportional contribution S k (y) of the kth determinant to the variance in ln Y. In principle, the decomposition can also use other inequality measures defined over ln Y, such as variance, the squared coefficient of variation, the Gini index, or the Theil index.30, 32 The proportional contribution is calculated as follows.
| (3) |
where y stands for ln Y it.
The sum of all factors in (3) adds up to unity, ie,
| (4) |
Using estimated regression coefficients of Equation (1), this decomposition estimates the contribution from each explanatory variable to the total variance in the dependent variables across districts and over time. It is important to note that this decomposition includes a residual component that cannot be attributed to a specific factor. Moreover, it can only deal with linear parameter specifications, ie, interaction terms cannot be included.32, 33
5. RESULTS
In this section, we report the findings for total household health care expenditures per capita and all its subcategories. We always start with the results from the estimation of Equation (1) (Table 1) and then present the results from the factor decomposition based on Equation (2) (Table 2). Note that we include all explanatory variables in the decomposition analysis including the residual to ensure that the proportional contributions add up to unity even though some of the explanatory variables are not statistically significant in the regression analysis. Finally, we relate the results from the regression and the decomposition to the trend in each single explanatory variable to identify the main contributors to rising health care expenditures over time.
Table 1.
Random effect model regression results using district panel data
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| THEXP | PMPEXP | LABEXP | MEXP | SCEXP | PHEXP | |
| ln (per capita total expenditure) | 1.7391*** (0.1702) | 0.8181*** (0.2072) | 2.6574*** (0.5868) | 1.6917*** (0.3753) | 2.0233*** (0.5288) | 4.8657*** (1.0890) |
| ln (percentage of child (0‐5 y) population) | −0.5433 (0.3374) | −0.3270 (0.3498) | −0.6222 (1.0333) | −0.6364 (0.6362) | −1.2943 (0.9449) | 0.2053 (2.0670) |
| ln (percentage of adult (over 65) population | 0.1261 (0.1578) | −0.1072 (0.1917) | 0.8299 (0.5439) | 0.5562 (0.3473) | 0.2218 (0.4903) | 1.3179 (1.0097) |
| ln (number of hospital beds per 1000 population) | −0.2474 (0.2481) | 0.2181 (0.2734) | −0.2694 (0.7933) | −1.0424** (0.4963) | −1.7420** (0.7211) | 1.2518 (1.5425) |
| ln (number of doctors per 100 000 population) | −0.0216 (0.1031) | −0.1166 (0.1104) | −0.2523 (0.3232) | 0.5036** (0.2007) | 0.0126 (0.2947) | 0.3327 (0.6370) |
| ln (number of outpatient attendance per 100 000 population) | 0.0858 (0.2069) | −0.5460** (0.2231) | 0.9823 (0.6529) | 0.1734 (0.4055) | 0.6489 (0.5950) | 1.2589 (1.2823) |
| n (number of inpatient stays per 100 000 population) | −0.2037 (0.2408) | 0.0503 (0.2732) | −0.3804 (0.7892) | 0.0208 (0.4958) | 1.0285 (0.7160) | −3.3380** (1.5140) |
| ln (annual death rate per 1000 population) | −0.1149 (0.1451) | 0.0697 (0.1519) | 0.7463* (0.4470) | −0.0768 (0.2762) | 0.3769 (0.4082) | −1.2098 (0.8897) |
| year 1995/1996 (dummy) | 0.3102*** (0.1164) | 0.2187* (0.1168) | 0.5483 (0.3467) | 0.6239*** (0.2125) | 0.3721 (0.3178) | 0.0768 (0.7042) |
| year 2002 (dummy) | 0.3002* (0.1580) | 0.1498 (0.1634) | 1.2936*** (0.4814) | 0.9324*** (0.2971) | 0.5638 (0.4401) | 0.8264 (0.9644) |
| year 2006/2007 (dummy) | 0.2177 (0.1479) | 0.1539 (0.1606) | 1.7025*** (0.4656) | 0.5293* (0.2915) | 0.6733 (0.4235) | 0.2990 (0.9118) |
| year 2009/2010 (dummy) | 0.1309 (0.1728) | 0.1119 (0.1879) | 1.5099*** (0.5453) | 0.3067 (0.3412) | 0.0247 (0.4960) | −0.3006 (1.0670) |
| year 2012/2013 (dummy) | 0.2597 (0.1827) | 0.0814 (0.2045) | 1.8466*** (0.5889) | 0.6771* (0.3710) | 0.3925 (0.5343) | 0.3347 (1.1365) |
| Constant | −10.7508*** (2.3811) | 0.4171 (2.7159) | −26.4533*** (7.8401) | −14.4978*** (4.9290) | −27.4374*** (7.1091) | −33.2039** (14.9962) |
| Observations | 102 | 102 | 102 | 102 | 102 | 102 |
| R‐squared (overall) | 0.770 | 0.512 | 0.732 | 0.788 | 0.572 | 0.417 |
| Number of districts | 17 | 17 | 17 | 17 | 17 | 17 |
Standard errors in parentheses.
Source: Authors estimation based on HIES 1990/1991, HIES 1995/1996, HIES 2002, HIES 2006/2007, HIES 2009/2010, HIES 2012/2013, Annual Health Statistics, Administrative data.
P < .1.
P < .05.
P < .01.
Table 2.
Factor decomposition with district fixed effects
| Variable | Contribution to Disparities in Outcome | |||||
|---|---|---|---|---|---|---|
| THEXP | PMPEXP | LABEXP | MEXP | SCEXP | PHEXP | |
| Per capita expenditure | 56.31 | 11.43 | 14.29 | 10.26 | 14.17 | 40.72 |
| Child rate | 5.23 | 0.91 | 0.63 | 2.79 | 5.70 | 0.93 |
| Adult rate | 1.53 | −1.23 | 12.10 | 0.18 | −6.66 | −0.47 |
| No. of beds | 0.82 | 3.76 | 8.76 | −5.58 | −14.44 | 2.11 |
| No. of doctors | −0.36 | −12.60 | −18.82 | 22.70 | −4.97 | 16.76 |
| Outpatients | 0.50 | 10.44 | 2.75 | 0.19 | 1.59 | 0.24 |
| Inpatients | −10.10 | −0.39 | 0.65 | −0.23 | 0.55 | −13.06 |
| Death rate | 3.45 | 4.84 | 10.16 | 1.65 | 8.56 | −2.90 |
| Others | 42.62 | 76.25 | 69.48 | 68.04 | 95.50 | 55.67 |
| Total | 100 | 100 | 100 | 100 | 100 | 100 |
Source: Authors estimation based on HIES 1990/1991, HIES 1995/1996, HIES 2002, HIES 2006/2007, HIES 2009/2010, HIES 2012/2013, Annual Health Statistics, Administrative data.
5.1. Total household health care expenditures
Column 1 of Table 1 shows that district‐level total out‐of‐pocket health care expenditures are strongly correlated with district‐level household total expenditure per capita that we use as a proxy for household income per capita (“income” hereafter). This aggregate also includes health care expenditures, since we use it as a proxy for total household income per capita, yet our results hold if we re‐estimate them excluding health care expenditures from total expenditures to address concerns regarding endogeneity. According to our estimates, an increase in income by 1% is associated with an increase in health care expenditures by 1.7%. This elasticity implies that income alone is associated with an increase in health care expenditures between 1990 and 2013 of 93%. Since care in the public sector is free of charge, this increase should largely reflect an increase of spending for private health care with rising income. All other coefficients are insignificant according to conventional levels of significance, which is at least partly due to the limited number of data points we have. Yet, looking at the effect size alone and its sign, it can be noted that changes in the population age composition and health care supply in a district matter for determining total health care expenditures. Whereas a higher share of children under 5 reduces households' health care expenditures, a higher share of elderly people (above 65) increases them. An increase in the number of beds in public hospitals per 1000 by 1% (controlling for inpatient attendance) reduces district‐level households' health care expenditures by 0.25%. Note that these results and those that follow are not significantly different from those that we obtain if we include also the northern and eastern districts that were the strongest hit by the civil war and for which no data are available for the years 1990/1991, 1995/1996, 2002, 2006/2007, and 2009/2010.
The results from the decomposition in column 1 of Table 2 show that about 56% of the total variance in health care expenditures across districts and over time can be explained by differences in per capita income. The age composition explains about 7%. In contrast, public sector inpatient attendance actually reduced the variability of total health care expenditure data across districts and time. All other factors make only minor contributions to the explanation in the total variance either because they vary little across districts and time or because they have only a small effect on health care expenditures (ie, small β m) or both. About 43% of the total variance remains in the residual.
Linking both, the regression coefficients and the relative contributions from the decomposition with the changes over time, our explanatory variables suggest that the increase in per capita health care expenditures is to a large extent driven by income growth that Sri Lankans experienced over the past 25 years. Health care supply measured through the number of beds per population (holding constant usage) has offset part of this increase. In other words, there is little indication that a deterioration of the quantity of health care supply in the public sector has driven the increase in health care expenditures over time. However, quality issues may of course play a role.
5.2. Expenditures for private outpatient medical practitioners
Column 2 of Table 1 shows that the expenditures for private outpatient medical practitioners are again strongly correlated with income and with outpatient attendance in the public sector. Income shows a positive elasticity of 0.82 and outpatient attendance in the public sector a negative elasticity. This is what we would expect: The higher the usage of outpatient care in the public sector, the lower usage of outpatient care in the private sector. More doctors in the public sector also imply lower expenditures for private outpatient care, but the effect is small and statistically not significant.
The decomposition results in column 2 of Table 2 suggests that income now makes with only 11% a much smaller contribution to the variance in the expenditures for private outpatient medical practitioners. Outpatient care in the public sector makes a comparable contribution. The number of doctors reduces even the inequality in outpatient health care expenditures in the private sector.
As before, comparing these results with the trends observed for the various explanatory variables, we can conclude that the rise of private outpatient care over time is mainly driven by income growth, but this effect seems to be compensated by a very large extent by an increase in the number of doctors in the public system and the capacity of the public sector to provide outpatient care. Figure 3 also shows that private outpatient care increased very slowly over time and is compared to all other cost categories, rather a moderate driver of total health care expenditures per capita over time.
5.3. Expenditures for lab tests and other diagnostic services in private health care facilities
Column 3 in Table 1 shows that expenditures for lab tests and other diagnostic services in private health care facilities are also strongly and positively correlated with income. They are also positively correlated with the death rate suggesting that population ageing is an important driver of these expenses. This interpretation is supported by the signs of the coefficients of the child ratio and the elderly ratio, respectively, even though both coefficients are not statistically significant according to conventional levels of significance.
The decomposition in column 3 in Table 2 indicates that income explains about 14% in the overall inequality in expenditures for lab tests and other diagnostic services. About 22% are due to population ageing and changes in the death rate. Differences in the number of doctors per population had again an equalizing effect.
Combining these findings with the trends documented in Section 3 suggests that the rise in expenditures for lab tests and other diagnostic services is due to income growth and population ageing.
5.4. Expenditures for medicines and other pharmaceutical products
Column 4 in Table 1 shows that expenditures for medicines and other pharmaceutical products are again mostly driven by income. But they also seem to depend on health care supply characteristics. The number of hospital beds per population is negatively associated with expenditures for medicines and other pharmaceutical products that is plausible because medicines and other pharmaceutical products are in principle provided freely in public sector hospitals. Yet these expenditures increase with the number of doctors, which seems also plausible, as they prescribe medicines and pharmaceuticals also in their private consulting hours, and people need to buy them then at private pharmacies by paying out of pocket.
Looking at the results in column 4 in Table 2, we can see that indeed about 10% of the inequality in expenditures for medicines and other pharmaceutical products are explained by our proxy for income per capita, about 23% are explained by differences in the number of medical doctors across time and districts. Conversely, the number of beds in public sector hospitals reduces the variance in expenditures for medicines and other pharmaceutical products.
Taking these results and the trends in the explanatory variables shown in Section 3, it can be concluded that the documented rise in expenditures for medicines and other pharmaceutical products illustrated in Figure 3 is driven mainly by income growth and the increase in the number of doctors.
5.5. Expenditures for private specialist consultations
Column 5 in Table 1 indicates that expenditures for specialist consultations are also mainly driven by income. A 1% increase in income leads to a 2% increase in expenditures on health specialists. This is plausible because specialist consultations that are more commonly referred as “specialist channeling” are quite expensive compared to standard general practice outpatient treatments. Richer people are more likely to use these private services, as they may value the higher service level (less overcrowding) and shorter waiting times. The other variable that seems important is the supply of hospital beds. More beds per 1000 population are associated with lower expenditures for specialists, suggesting that with larger capacities in the public sector, the supply of specialist consultations in the public sector increases as well.
From the decomposition results shown in column 5 in Table 2, one can see that the contributions to the overall inequality in expenditures for specialist consultations from per capita income and the number of hospital beds per 1000 population exactly offset each other. The share of children and the death rate also increase the inequality in expenditures for specialist consultations. All remaining variables make only marginal contributions.
Taken together the regression results and the decomposition, it can be concluded that the increase in expenditures on specialist consultations over the years can be mainly attributed to the income growth, also this effect was partly offset by an increase in the number of public sector facilities and hence more specialist consultations in the public sector.
5.6. Expenditures for private inpatient hospital attendance
As a last cost category, we focus on expenditures for private hospitals. According to column 6 of Table 1, income shows the strongest association. An increase of income by 1% is associated with an increase of expenditures for private hospital attendance of almost 5%, ie, the increase in income between 1990 and 2013 alone is associated with an increase in expenditures for private inpatient care by 262%. A sizeable income elasticity is expected for this cost category since private inpatient care is in the given context “extremely” expensive and only high‐income households can afford to stay in private hospitals. Also, as expected, inpatient attendance in the public sector is associated with lower expenditures for private hospital attendance. Differences in the share of elderly persons may again be another important factor, but the corresponding coefficient and also all others are not or only borderline significant.
The decomposition results in column 6 of Table 2 show that income alone explains 41% of the inequality in expenditures for private hospital attendance. Public inpatient care has an equalizing effect by reducing the variance in expenditures. The decomposition also reveals that the number of doctors increases the variance in expenditures for private inpatient care. As most doctors in the public sector provide health care services in their after hour work in private hospitals, more doctors in general may also come with higher private hospital expenditures.
Combining regression and decomposition results with the trends shown in Figure 3 suggests that the rise in private hospital expenditures is mainly due to income growth and the increase in the number of doctors. Expenditures for private inpatient care are reduced as more public sector inpatient care is used.
5.7. Household level estimates
We also re‐estimated the above model with the household level data, ie, also exploiting the variation across households within districts. The results are shown in Table 3. As for the subcategories expenditures are zero for many households, we use a 2‐part model for estimation.34, 35 The income elasticity of health care demand is somewhat lower than if estimated on the district level. It is still larger than one for total household health care expenditures per capita and private outpatient medical practitioners, but it is smaller than one for all other categories. This is due to the fact that in household level estimates, all households have the same weight irrespective of the size of their health care expenditures whereas district averages are “biased” towards households with higher expenditure levels and richer households spend larger shares of their income on these types of health care expenditures. We find lower total household health expenditures per capita in female headed households and higher expenditures in households with household heads that have at least attended primary or secondary education. The sign reverses for households with university level education. Households in urban areas spend less on health care expenditures in general but more on medicines and specialists. On the household level, we find that health care expenditures increase in both, a higher proportion of children in the household and a higher proportion of elderly in the household. Health care expenditures per capita also increase with household size, and they increase with the district‐specific annual death rate.
Table 3.
Marginal effects from 2‐part model estimation using household data
| Variable | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| THEXP | PMPEXP | LABEXP | MEXP | SCEXP | PHEXP | |
| ln (per capita total expenditure) | 1.6289*** (0.0178) | 1.1197*** (0.0164) | 0.1300 (0.0000) | 0.5379*** (0.0106) | 0.2083*** (0.0056) | 0.0574*** (0.0014) |
| Age of the household head (years) | 0.0127*** (0.0008) | 0.0060*** (0.0008) | 0.0014 (0.0000) | 0.0060*** (0.0005) | 0.0021*** (0.0002) | 0.0001 (0.0001) |
| Gender of the household head (1 = male, 0 = female) | −0.0516** (0.0204) | −0.0414** (0.0204) | 0.0045 (0.0000) | −0.0208 (0.0141) | −0.0021 (0.0057) | 0.0039 (0.0033) |
| Household head only attended up to primary school (dummy) | 0.0459** (0.0220) | 0.0238 (0.0223) | 0.0057 (0.0000) | 0.0353** (0.0162) | −0.0101 (0.0069) | 0.0010 (0.0038) |
| Household head only attended up to secondary school (dummy) | 0.1278*** (0.0235) | 0.1167*** (0.0238) | 0.0242 (0.0000) | 0.0266 (0.0174) | 0.0427*** (0.0078) | −0.0077* (0.0041) |
| Household head only attended above university level (dummy) | −0.4237*** (0.0628) | −0.4271*** (0.0619) | 0.0061 (0.0000) | −0.0818** (0.0407) | 0.0299** (0.0141) | −0.0216*** (0.0079) |
| Ethnic Sinhalese household head (dummy) | 0.2692 (0.1785) | 0.3622** (0.1796) | 0.0107 (0.0000) | 0.0634 (0.1202) | 0.0301 (0.0450) | 0.0049 (0.0218) |
| Ethnic Tamil household head (dummy) | 0.1514 (0.1838) | 0.3460* (0.1847) | −0.0075 (0.0000) | −0.1120 (0.1243) | −0.0306 (0.0484) | −0.0125 (0.0229) |
| Ethnic Muslim household head (dummy) | 0.3496 (0.2141) | 0.5910*** (0.2131) | −0.0023 (0.0000) | −0.0648 (0.1459) | 0.0004 (0.0644) | −0.0044 (0.0232) |
| Buddhist (religion) household head (dummy) | 0.6749 (0.5741) | 0.5002 (0.5846) | 0.8230 (0.0000) | 0.0825 (0.4081) | 1.0439*** (0.0586) | 0.3273*** (0.0238) |
| Hindu (religion) household head (dummy) | 0.6556 (0.5726) | 0.4511 (0.5835) | 0.8110 (0.0000) | 0.1310 (0.4077) | 1.0298*** (0.0650) | 0.3413*** (0.0247) |
| Islam (religion) household head (dummy) | 0.6137 (0.5856) | 0.3664 (0.5961) | 0.8219 (0.0000) | 0.1585 (0.4149) | 1.0378*** (0.0745) | 0.3358*** (0.0244) |
| Christian (religion) household head (dummy) | 0.7069 (0.5735) | 0.4940 (0.5840) | 0.8358 (0.0000) | 0.1756 (0.4078) | 1.0446*** (0.0519) | 0.3403*** (0.0231) |
| Urban households (dummy) | −0.3183*** (0.0224) | −0.4839*** (0.0223) | 0.0137 (0.0000) | 0.1558*** (0.0149) | 0.0348*** (0.0056) | 0.0007 (0.0031) |
| Proportion of child (0‐5 y) within household | 2.0859*** (0.0673) | 2.1782*** (0.0666) | 0.0130 (0.0000) | 0.2551*** (0.0470) | 0.0970*** (0.0192) | 0.0108 (0.0109) |
| Proportion of adults (over 65 y) within household | 0.9973*** (0.0537) | 0.6054*** (0.0530) | 0.0408 (0.0000) | 0.3550*** (0.0356) | 0.0574*** (0.0134) | 0.0269*** (0.0074) |
| Household size (members) | 0.1611*** (0.0053) | 0.1395*** (0.0052) | 0.0150 (0.0000) | 0.0530*** (0.0035) | 0.0243*** (0.0013) | 0.0074*** (0.0006) |
| ln (number of hospital beds per 1000 population) | −0.1587*** (0.0411) | 0.1927*** (0.0412) | 0.0190 (0.0000) | −0.2763*** (0.0294) | 0.0025 (0.0116) | −0.0235*** (0.0063) |
| ln (number of doctors per 100 000 population) | −0.0010 (0.0008) | 0.0001 (0.0008) | −0.0003 (0.0000) | −0.0001 (0.0006) | −0.0006*** (0.0002) | −0.0002 (0.0001) |
| ln (number of outpatient attendance per 100 000 population) | 0.0000 (0.0000) | −0.0001*** (0.0000) | −0.0000 (0.0000) | 0.0002*** (0.0000) | 0.0000 (0.0000) | −0.0000 (0.0000) |
| ln (number of inpatient stays per 100000 population) | −0.0019*** (0.0006) | −0.0035*** (0.0006) | −0.0002 (0.0000) | 0.0006 (0.0004) | −0.0003 (0.0002) | 0.0001 (0.0001) |
| ln (annual death rate per 1000 population) | 1.0112*** (0.1191) | 1.1430*** (0.1215) | 0.0628 (0.0000) | −0.2441** (0.1008) | 0.1248*** (0.0400) | 0.0091 (0.0184) |
| Observations | 106 023 | 106 029 | 106 029 | 106 029 | 106 029 | 106 029 |
| District FE | Yes | Yes | Yes | Yes | Yes | Yes |
| Year FE | Yes | Yes | Yes | Yes | Yes | Yes |
Robust standard errors in parentheses.
Source: Authors estimation based on HIES 1990/1991, HIES 1995/1996, HIES 2002, HIES 2006/2007, HIES 2009/2010, HIES 2012/2013, Annual Health Statistics, Administrative data.
P < .1.
P < .05.
P < .01.
6. DISCUSSION
The analysis showed that household income per capita, which we approximated by total household expenditures per capita, are by far the most important driver of differences in total household health expenditures across districts and over time. We find an income elasticity of 1.7% for the aggregate of all health care expenditure categories. Results from the separate health care cost categories show that the elasticities for lab tests and other diagnostic services, for specialist consultations and for private hospitals are even larger. The elasticity for private outpatient medical practitioners is somewhat smaller. Hence, overall, this implies that expenses for health care increase over proportionally with income. Yet, if the elasticity is estimated using the household sample instead of the district sample, the income elasticity of health care demand is somewhat lower, still larger than 1 for total household health care expenditures per capita and expenses on private outpatient medical practitioners, but not anymore larger than 1 for all other sub categories.
The consumers' strive for higher quality implies that “health care” has a lot in common with what is called in “Economic Theory” a luxury good. The question whether health care is a luxury or a necessity has always been of interest and previous studies found mixed results.36, 37, 38 While many studies estimated an income elasticity of health care demand in developed countries, there are only a small number of studies that deal with developing countries. Similar to our findings, a study by Khan and Mahumud,39 for instance, found that citizens of selected Southeast Asian countries consider private health care as a luxury good. Xu and colleagues40 reported that private health care (out‐of‐pocket expenditure) is considered as a luxury good (income elasticity of 1.098) in low‐income countries and a necessity (income elasticity of 0.842‐0.869) in the middle‐income countries. The fact that per capita income is the main contributor to total out‐of‐pocket health care expenditures is in line with some previous studies.41, 42 Our finding is in contrast with the findings by Hayashi and Oyama32 who found per capita income contributes little to the variance in health care expenditures in Japan. However, it should be noted that their analysis was based on both public and private health care expenditures not just private health care expenditures as in our case.
Our analysis also showed that the growth of public health care supply proxied by the number of beds dampened the increase in expenditures for purchasing medicines and for specialist consultations. Interestingly, an increase in the number of doctors rather tends to increase expenditures for some cost categories, such as medicines and private inpatient care. This may reflect the supplier‐induced demand as doctors conduct dual practice in both fixed salary‐based public hospitals and patient fee‐based private facilities.43, 44, 45 Nonclinical aspects of quality such as better interpersonal communication by doctors and other health staffs and after hours of consultation (in the late afternoon and on weekends) seem to have further pushed the demand to the private sector as soon as patients can afford. Yet there is no systematic relationship between health care expenditures and outpatient and inpatient per population usage rates; hence, overcrowding in the public sector as such does not seem to be an important driver of private health care expenditures. In other words, it is more a quality than a quantity constraint.
We also found that changes in the population age composition and the crude death rate have influenced the household health care expenditures across districts and over time. Our results suggest that, for instance, expenses for medical laboratory tests and other diagnostic services increased with the share of older persons. Older persons have to take regular medical tests and spend more on these services. Older persons are more likely to suffer from chronic diseases such as heart ailments, diabetics, and hypertension and therefore need to take regular monitoring checkups. Our results are in line with previous studies that identified population ageing as one of the main determinants of out‐of‐pocket health care expenditure.46, 47, 48 The positive association with the crude death rate is another reflection of the link between morbidity and health care expenditures.49, 50
Yet we are aware of the fact that these variables may not fully capture all relevant aspects of health care quality and quantity in the public sector.
7. CONCLUSION
Our results show that despite the free health care policy, people purchase many health care services from the private sector. The increase in income over the past 2 decades allows people to buy higher quality, in form of supplementary private services, characterized not necessarily only by higher clinical quality, but also other quality aspects such as shorter waiting times, better interpersonal communication by doctors and other health staff, and cleanliness and availability of luxurious private facilities (individual room and bed, TVs, and unrestricted visiting time).51, 52
If these trends continue, they may erode the willingness to pay of the middle class and the rich to pay taxes for public health care services as they increasingly may opt out of the public health care system. This may act as a threat to the sustainability of free public health care. From a policy perspective, the government may consider improving nonclinical aspects of public health care quality by adopting quality improvement strategies. The results have general implications for emerging countries with a free health care policy.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGEMENTS
Asankha Pallegedara gratefully acknowledges financial support from the Alexander von Humboldt Foundation. The authors thank the Department of Census and Statistics of Sri Lanka for providing the HIES data and Ministry of Health and Nutrition of Sri Lanka for providing Annual Health Statistics data.
Pallegedara A, Grimm M. Have out‐of‐pocket health care payments risen under free health care policy? The case of Sri Lanka. Int J Health Plann Mgmt. 2018;33:e781–e797. 10.1002/hpm.2535
REFERENCES
- 1. WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division . Trends in Maternal Mortality: 1990 to 2015 Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. 2015. http://www.who.int/gho/maternal_health/countries/en/. Published 2015. Accessed September 19, 2017.
- 2. United Nations Children's Fund (UNICEF) . The State of the World's Children 2016: A fair chance for every child. New York: UNICEF; 2016. http://apps.who.int/iris/bitstream/10665/194254/1/9789241565141_eng.pdf?ua=1. Accessed September 20, 2017. [Google Scholar]
- 3. Rannan‐Eliya RP, Sikurajapathy L. Sri Lanka: “Good Practice” in Expanding Health Care Coverage. Research Studies Series, Number 3 Colombo: Institute for Health Policy; 2008. [Google Scholar]
- 4. Caldwell JC. Routes to low mortality in poor countries. Pop Dev Rev. 1986;12(2):171‐220. [Google Scholar]
- 5. Caldwell JC, Gajanayake I, Caldwell P, Peiris I. Sensitization to illness and the risk of death: an explanation for Sri Lanka's approach to good health for all. Soc Sci Med. 1989;28(4):365‐379. [DOI] [PubMed] [Google Scholar]
- 6. Govindaraj R, Navaratne K, Cavagnero E, Seshadri SR. Health Care in Sri Lanka : What Can the Private Health Sector Offer?. Health, Nutrition and Population (HNP) Discussion Paper Series no. 89554. Washington, DC: World Bank; 2014. [Google Scholar]
- 7. Asian Mirror . If the health system is so good, why did the health minister go to Singapore for treatment: Anura Kumara Dissanayake hits out at Rajitha. August 24, 2017. http://www.asianmirror.lk/news/item/25031-if-the-health-system-is-so-good-why-did-the-health-minister-go-to-singapore-for-treatment-anura-kumara-dissanayake-hits-out-at-rajitha. Accessed September 29, 2017.
- 8. Hwang W, Weller W, Ireys H, Anderson G. Out‐of‐pocket medical spending for care of chronic conditions. Health Aff. 2001;20(6):267‐278. [DOI] [PubMed] [Google Scholar]
- 9. Waters HR, Anderson GF, Mays J. Measuring financial protection in health in the United States. Health Policy. 2004;69(3):339‐349. [DOI] [PubMed] [Google Scholar]
- 10. Carpenter A, Islam MM, Yen L, McRae I. Affordability of out‐of‐pocket health care expenses among older Australians. Health Policy. 2015;119(7):907‐914. [DOI] [PubMed] [Google Scholar]
- 11. Bock JO, Matschinger H, Brenner H, et al. Inequalities in out‐of‐pocket payments for health care services among elderly Germans—results of a population‐based cross‐sectional study. Int J Equity Health. 2014;13(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. You X, Kobayashi Y. Determinants of out‐of‐pocket health expenditure in China. Appl Health Econ Health Policy. 2011;9(1):39‐49. [DOI] [PubMed] [Google Scholar]
- 13. Garg CC, Karan AK. Reducing out‐of‐pocket expenditures to reduce poverty: a disaggregated analysis at rural‐urban and state level in India. Health Policy Plan. 2009;24(2):116‐128. [DOI] [PubMed] [Google Scholar]
- 14. Mukherjee S, Haddad S, Narayana D. Social class related inequalities in household health expenditure and economic burden: evidence from Kerala, South India. Int J Equity Health. 2011;10(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kumara AS, Samaratunge R. Patterns and determinants of out‐of‐pocket health care expenditure in Sri Lanka: evidence from household surveys. Health Policy Plan. 2016;31(8):970‐983. [DOI] [PubMed] [Google Scholar]
- 16. Onwujekwe OE, Uzochukwu BS, Obikeze EN, et al. Investigating determinants of out‐of‐pocket spending and strategies for coping with payments for healthcare in southeast Nigeria. BMC Health Serv Res. 2010;10(1):67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wagstaff A, Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam, 1993‐98. Health Econ. 2003;12(11):921‐934. [DOI] [PubMed] [Google Scholar]
- 18. Van Minh H, Phuong NTK, Saksena P, James CD, Xu K. Financial burden of household out‐of pocket health expenditure in Viet Nam: findings from the National Living Standard Survey 2002–2010. Soc Sci Med. 2013;96:258‐263. [DOI] [PubMed] [Google Scholar]
- 19. Perera M, Gunatilleke G, Bird P. Falling into the medical poverty trap in Sri Lanka: what can be done? Int J Health Serv. 2007;37(2):379‐398. [DOI] [PubMed] [Google Scholar]
- 20. Shahrawat R, Rao KD. Insured yet vulnerable: out‐of‐pocket payments and India's poor. Health Policy Plan. 2012;27(3):213‐221. [DOI] [PubMed] [Google Scholar]
- 21. Séne LM, Cissé M. Catastrophic out‐of‐pocket payments for health and poverty nexus: evidence from Senegal. Int J Health Econ Manag. 2015;15(3):307‐328. [DOI] [PubMed] [Google Scholar]
- 22. Ministry of Health Sri Lanka (MOH) . Annual Health Bulletin 2014. Colombo: MOH; 2016. [Google Scholar]
- 23. Withanachchi N, Uchida Y. Healthcare rationing: a guide to policy directions in Sri Lanka. Health Policy. 2006;78(1):17‐25. [DOI] [PubMed] [Google Scholar]
- 24. Amarasinghe S, De Alwis S, Saleem S, Ranna‐Eliya R, Dalpatadu S. IHP Technical Reports Series, Number 2: Private Health Sector Review 2012. Colombo: Institute for Health Policy; 2015. [Google Scholar]
- 25. Amarasinghe SN, Thowfeek FR, Anuranga C, Dalpatadu KCS, Rannan‐Eliya RP. Sri Lanka Health Accounts: National Health Expenditure 1990–2014. Health Expenditure Series No.4 Colombo: Institute for Health Policy; 2015. [Google Scholar]
- 26. Thresia CU. Rising private sector and falling ‘good health at low cost’: health challenges in China, Sri Lanka, and Indian state of Kerala. Int J Health Serv. 2013;43(1):31‐48. [DOI] [PubMed] [Google Scholar]
- 27. World Bank . World Development Indicators: GDP per Capita (Current US$). Washington DC: World Bank; http://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=LK%26year_low_desc=false. Accessed March 15, 2017. [Google Scholar]
- 28. Department of Census and Statistics of Sri Lanka (DCS) . Household Income and Expenditure Survey, 2012/2013 Final Report. Colombo: DCS; 2015.
- 29. Department of Census and Statistics of Sri Lanka (DCS) . Vital Statistics – Deaths. http://nada.statistics.gov.lk/index.php/catalog/Demography. Accessed December 15, 2016.
- 30. Fields GS. Accounting for Income Inequality and its Change: A new Method, With Application to the Distribution of Earnings in the United States In: Polachek SW, ed. Worker Well‐Being and Public Policy. Research in Labor Economics Vol.22 Bingley: Emerald Group Publishing Limited; 2003:1‐38. [Google Scholar]
- 31. Shorrocks AF. Inequality decomposition by factor components. Econometrica. 1982;50(1):193‐211. [Google Scholar]
- 32. Hayashi M, Oyama A Factor decomposition of inter‐prefectural health care expenditure disparities in Japan. Working paper No. CIRJE‐F‐948. Tokyo: CIRJE, Faculty of Economics, University of Tokyo; 2014.
- 33. Wan G. Accounting for income inequality in China: a regression‐based approach. J Comp Econ. 2004;32(2):348‐363. [Google Scholar]
- 34. Duan N, Manning WG, Morris CN, Newhouse JP. A comparison of alternative models for the demand for medical care. J Bus Econ Stat. 1984;1(2):115‐126. [Google Scholar]
- 35. Grytten J, Holst D, Laake P. Accessibility of dental services according to family income in a non‐insured population. Soc Sci Med. 1993;37(12):1501‐1508. [DOI] [PubMed] [Google Scholar]
- 36. Getzen T. Health care is an individual necessity and a national luxury: applying multilevel decision models to the analysis of health care expenditures. J Health Econ. 2000;19(2):259‐270. [DOI] [PubMed] [Google Scholar]
- 37. Gerdtham UG, Jonsson B. International Comparisons of Health Expenditure: Theory, Data, and Econometric Analysis In: Culyer AJ, Newhouse JP, eds. Handbook of Health Economics. Vol.1A Amsterdam: North‐Holland; 2000. [Google Scholar]
- 38. Costa‐Font J, Gemmill M, Rubert G. Biases in the healthcare luxury good hypothesis?: a meta‐regression analysis. J R Stat Soc a Stat Soc. 2011;174(1):95‐107. [Google Scholar]
- 39. Khan JA, Mahumud RA. Is healthcare a ‘Necessity’ or ‘Luxury’? An empirical evidence from public and private sector analyses of South‐East Asian countries? Heal Econ Rev. 2015;5(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Xu K, Saksena P, Holly A. The Determinants of Health Expenditure: A Country Level Panel Data Analysis. Geneva: World Health Organisation (WHO); 2011:2011. [Google Scholar]
- 41. Martín JJM, Puerto Lopez del Amo Gonzalez M, Dolores Cano Garcia M. Review of the literature on the determinants of healthcare expenditure. Appl Econ. 2011;43(1):19‐46. [Google Scholar]
- 42. Murthy VN, Okunade AA. The core determinants of health expenditure in the African context: some econometric evidence for policy. Health Policy. 2009;91(1):57‐62. [DOI] [PubMed] [Google Scholar]
- 43. Auster RD, Oaxaca RL. Identification of supplier induced demand in the health care sector. J Hum Resour. 1981;16(3):327‐342. [PubMed] [Google Scholar]
- 44. Dranove D, Wehner P. Physician‐induced demand for childbirths. J Health Econ. 1994;13(1):61‐73. [DOI] [PubMed] [Google Scholar]
- 45. Delattre E, Dormont B. Fixed fees and physician‐induced demand: a panel data study on French physicians. Health Econ. 2003;12(9):741‐754. [DOI] [PubMed] [Google Scholar]
- 46. Karatzas G. On the determination of the US aggregate health care expenditure. Appl Econ. 2000;32(9):1085‐1099. [Google Scholar]
- 47. Di Matteo L. The macro determinants of health expenditure in the United States and Canada: assessing the impact of income, age distribution and time. Health Policy. 2005;71(1):23‐42. [DOI] [PubMed] [Google Scholar]
- 48. Crivelli L, Filippini M, Mosca L. Federalism and regional health care expenditures: an empirical analysis for the Swiss cantons. Health Econ. 2006;15(5):535‐541. [DOI] [PubMed] [Google Scholar]
- 49. Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditure: a red herring? Health Econ. 1999;8(6):485‐496. [DOI] [PubMed] [Google Scholar]
- 50. Felder S, Meier M, Schmitt H. Health care expenditure in the last months of life. J Health Econ. 2000;19(5):679‐695. [DOI] [PubMed] [Google Scholar]
- 51. Russell S. Treatment‐seeking behaviour in urban Sri Lanka: trusting the state, trusting private providers. Soc Sci Med. 2005;61(7):1396‐1407. [DOI] [PubMed] [Google Scholar]
- 52. Rannan‐Eliya RP, Wijemanne N, Liyanage IK, et al. The quality of outpatient primary care in public and private sectors in Sri Lanka—how well do patient perceptions match reality and what are the implications? Health Policy Plan. 2015;30(suppl_1):i59‐i74. [DOI] [PubMed] [Google Scholar]


