Abstract
Although CD8 T-cell vaccines do not have the record of success of humoral-mediated vaccines, they do not receive the same degree of effort. Many diseases, including malaria, tuberculosis, and acquired immune deficiency syndrome (AIDS) have not yielded to vaccines, and intrinsic barriers may impede approaches limited solely to generating antibodies. Moreover, population growth and modernization are driving an increased pace of new emerging global health threats (human immunodeficiency virus [HIV] is a recent example), which will create unpredictable challenges for vaccinologists. Vaccine-elicited CD8 T cells may contribute to protective modalities, although their development will require a more thorough understanding of CD8 T-cell biology, practices for manufacturing and delivering CD8 T-cell-eliciting vectors that have acceptable safety profiles, and, ultimately, the political will and faith of those that make vaccine research funding decisions.
Great Debates
What are the most interesting topics likely to come up over dinner or drinks with your colleagues? Or, more importantly, what are the topics that don't come up because they are a little too controversial? In Immune Memory and Vaccines: Great Debates, Editors Rafi Ahmed and Shane Crotty have put together a collection of articles on such questions, written by thought leaders in these fields, with the freedom to talk about the issues as they see fit. This short, innovative format aims to bring a fresh perspective by encouraging authors to be opinionated, focus on what is most interesting and current, and avoid restating introductory material covered in many other reviews.
The Editors posed 13 interesting questions critical for our understanding of vaccines and immune memory to a broad group of experts in the field. In each case, several different perspectives are provided. Note that while each author knew that there were additional scientists addressing the same question, they did not know who these authors were, which ensured the independence of the opinions and perspectives expressed in each article. Our hope is that readers enjoy these articles and that they trigger many more conversations on these important topics.
The adaptive immune system has evolved specialized components to protect different topological compartments. Antibodies (humoral immunity) protect extracellular spaces, CD4 T cells patrol phagosomal infections, and CD8 T cells eliminate the majority of intracellular infections (including viruses and some bacteria, fungi, and parasites). As far as we know, this strategy has been maintained since the emergence of vertebrates during the Cambrian explosion, meaning that an organism with a humoral immune system, but lacking a surrogate for CD8 T cells, has not yet been defined (Hirano et al. 2011). So it appears that CD8 T cells serve essential functions that have necessitated their maintenance across 525 million years of vertebrate radiation.
CD8 T cells play a role in clearing primary and suppressing persistent intracellular infections. But that does not mean memory CD8 T cells serve a purpose after an infection is cleared. One could envisage, for example, that anamnestic protective duties are deferred to the humoral response, and that neutralizing antibodies might supplant any need for CD8 T-cell memory. So, did God make a mistake, or might memory CD8 T cells fill a niche or a need that antibodies do not? And, more importantly, can this be exploited for vaccines? We will consider these weighty issues below.
EVIDENCE THAT MEMORY CD8 T CELLS PROTECT AGAINST REINFECTION
Investigations of antibodies and their functions dominated the field of immunology (and related Nobel Prizes awarded from 1901 to 1987!) for most of its history. In contrast, the identification and understanding of CD8 T cells and their functions is quite recent (Masopust et al. 2007). CD8 T-cell responses may control primary intracellular infections before antibody responses have gotten a chance to mature, undergo affinity maturation, and mediate the class switching, which favors broader anatomic coverage. But do CD8 T cells protect from reinfection?
Abundant evidence in experimental animal models shows memory CD8 T-cell-mediated pathogen control (Harty et al. 2000). Some of this evidence result from “what-can-happen” experiments, wherein CD8 T cells are not needed if antibody memory was also established, as would typically be the case physiologically. For instance, memory CD8 T cells contribute to vaccinia control in the absence of B cells (Xu et al. 2004). But for those of us that have B cells, the antibody would likely play a dominant role (Spriggs et al. 1992). Of course, there are many ways to show what can happen under reductionist circumstances that have little relationship with reality.
But might there be pathogens that appear less vulnerable to antibody-mediated protection? One pathogen that periodically appears on the news is Listeria monocytogenes (LM), which may cause outbreaks associated with unwashed vegetables or unsavory fast food enterprises. LM spreads from cell to cell without needing an extracellular phase (Pamer 2004). Thus, in this disease, CD8 T cells patrol an anatomic niche that neutralizing antibodies cannot access. In other words, CD8 T-cell memory would serve you better than humoral immunity for protection against LM reexposure. But a particularly strong rationale for maintaining CD8 T-cell memory may be for dealing with serological variants. CD8 T cells recognize a broader antigenic repertoire than neutralizing antibodies (the latter typically limited to outer surface determinants, including potentially variable glycan moieties) (Moutaftsi et al. 2010; Doores 2015). In circumstances of heterosubtypic infection, which occurs in a variety of infections not least of which includes influenza virus, cross-reactive CD8 T cells can mean the difference between life and death where antibody (which can be specific to a fault) has failed us (Grant et al. 2016).
IS THERE A NEED FOR A CD8 T-CELL VACCINE?
If cheap, safe, and effective humoral vaccines existed to protect us against all major pathogens, then we would not need a CD8 T-cell vaccine—at least for infectious diseases; there are other potential targets for a CD8 T-cell vaccine, including cancer. But there are seemingly intractable pathogens that cause significant morbidity and mortality for which vaccines do not exist (Koff et al. 2013). Collectively, these pathogens can kill people of all ages, including the most economically productive demographic segments of society. So in addition to causing direct human misery, these diseases are an absolutely tremendous financial burden. The pathogens that have gotten the most attention include HIV, tuberculosis (TB), and malaria. Humoral approaches have not saved us yet. And, quite frankly, those approaches have attracted the lion’s share of the effort (Gray et al. 2016). In other words, we have more examples of failure from humoral vaccines than we do from CD8 T-cell vaccines. However, we will come back to a discussion of what a CD8 T-cell vaccine would take, and we can make our own conclusions about the practicality.
The history of vaccines has been a slow but steady success story (Plotkin 2014). Vaccines have likely done more to help humanity than all other medical interventions, and research in this area has provided a high return on investment. A success in the last decade is the human papillomavirus (HPV) vaccine, which is interesting because it is based on an innovative platform (virus-like particles) and protects against viral-induced cancer (Garland et al. 2016). The collective experience in vaccinology would support the conclusions that development takes time and that it can sometimes be aided by new technology or approaches. Importantly, the pursuit of new approaches need not exclude research in improving on the status quo. Indeed, vaccines can be developed that elicit both humoral and CD8 T-cell immunity (in fact, the very effective yellow fever and smallpox vaccines unknowingly accomplished this long ago).
Any discussion of vaccine development must acknowledge the alarming pace at which new infectious diseases are emerging (Morens and Fauci 2013). HIV has taught us that some of these emerging pathogens can cause a global pandemic and high rates of mortality. Fortunately, it did not spread with the same efficiency as, for example, influenza virus (Taubenberger and Morens 2010). Like HIV, Hendra virus, Marburg and Ebola viruses, SARS and MERS coronaviruses, and Hanta viruses also cause high mortality and morbidity. Also worrisome are the flaviruses, which include not only familiar foes, Dengue and yellow fever virus, but newly spreading diseases caused by Chikungunya and Zika virus. The microbial world is not static. Global population growth, modernization, and habitat encroachment has created an incubator for the emergence of pathogens. We do not know what is coming, and efforts to understand the diverse immunological strategies that control or prevent infections might help in our preparation. Indeed, HIV has shown that vaccine development dependent on conventional humoral immunity can be slow and fraught with challenges. Perhaps CD8 T-cell vaccines will be an aid in our practical defense against coming plagues.
SAFETY, MANUFACTURING, AND DELIVERY
A need for vaccines that elicit CD8 T-cell responses (perhaps in addition to humoral responses) is not sufficient to spur development and licensing. They must be deemed safe, producible at a reasonable cost, and deliverable to the masses. Safety issues will depend on the risk profile of a vaccine and risk tolerance, which may vary by pathogenicity and exposure risk. CD8 T cells often mount the most robust responses against live replicating pathogens. In general, sterile or subunit immunization strategies that elicit optimal CD8 T-cell responses have not been discerned. CD8 T cells may just fundamentally sense the difference between real infections that cause cell injury and death (accompanied by a plethora of danger signals) versus antigens delivered in the context of a single adjuvant or Toll-like receptor (TLR) ligand.
Can we accept the development of new live replicating vaccines in the modern era? Or must we develop a better understanding of memory CD8 T-cell ontogeny and function, and translate that knowledge into modalities that replace crude replicating vaccines without sacrificing essential features of immunogenicity, or find one empirically (Amanna et al. 2012). On this topic, it is important to note that safety includes the perception of safety. Some vaccine candidates could be excluded from trial (or even basic science funding) on the basis that they might cause problems, and it is plausible that some safe and efficacious ideas have gotten triaged before being given a chance (Bhan and Green 2011; Hoffman et al. 2015). This problem will be difficult to overcome, although the advancement of therapeutic cancer vaccines, which likely will have a lower safety bar than prophylactic vaccines, could possibly impact the vector pipeline.
More mundane but very real issues include vaccine manufacturing and delivery. Regardless of the mode of protection, it must be considered whether vector production is scalable. An extreme example of the potential challenges would be the use of irradiated sporozoites dissected out of mosquito salivary glands that serve as an effective (and seemingly CD8 T-cell-dependent) malaria vaccine (Seder et al. 2013; Ishizuka et al. 2016). This is not to say that these challenges cannot, in principle, be overcome. But it does make some options, even in the preclinical pipeline, less appealing and perhaps less fundable.
All things being equal, heterologous (as opposed to homologous) prime boost (HPB) vaccination strategies magnify the magnitude of memory CD8 T-cell populations (Lu 2009). Size matters in settings where the absolute number of memory CD8 T cells (at the time of pathogen exposure) correlates with protection. However, HPB requires preparation of more than one totally distinct modality. Each modality multiplies the regulatory compliance, testing, and safety barriers. And if there were a need for many different HPB vaccines for many diseases, it is possible that we would run out of serologically distinct vectors. This of course depends on modality (e.g., this would not be an issue with DNA-based vaccines). Moreover, HPB, just like homologous boosted vaccines, require more than one immunization, which stresses compliance and the cost of administration. And in a related issue, it requires storage of more than one vaccine preparation. Particularly with live-replicating vaccines, storage can be nontrivial, perhaps requiring an unbroken cold chain that imposes additional challenges.
Whereas safety, manufacturing, and delivery create thorny issues, perhaps for CD8 T-cell vaccines in particular, the good news is that we have the technology to solve these issues today given sufficient political will.
NEW TECHNOLOGY, IMMUNOLOGICAL CONCEPTS, AND APPROACHES
The possibility must be noted that CD8 T cells may not yet have revealed all their tricks to scientists. Clearly, they are more than killers engaged solely in hand-to-hand combat, and may have widespread and potent sensing and alarm functions that broaden antimicrobial effects (Ariotti et al. 2014; Schenkel et al. 2014). Their location is important, and the recently described resident memory T-cell (TRM) lineage may be critical for rapid responses. Indeed, demonstration of rapid TRM-mediated protection is quite recent, and the vaccine community is still assimilating this knowledge (Carbone 2015). Louis Picker and colleagues proposed the bold concept of using chronic cytomegalovirus as an HIV vaccine vector and tested this concept in rhesus macaques for protection against simian immunodeficiency virus (SIV) (Hansen et al. 2011). A remarkable efficacy signal has been observed, and the mechanism is potentially reliant on completely unexpected means of T-cell recognition (Hansen et al. 2016). What else remains unknown?
Important gaps in our knowledge include a quantitative understanding of CD8 T-cell-mediated immunosurveillance efficiency. What parameters (e.g., magnitude, function, location) relate to protective efficacy? How many CD8 T cells are required to find a rare infected founder cell within 1 day? Within 1 hour? How do CD8 T-cells’ target-scanning rates vary by tissue or by pathogen? For instance, within the reproductive mucosa, would interaction between a vaccine-elicited HIV-specific T cell and an infected target result in productive recognition? How long does an infected founder cell take to present HIV peptides on its major histocompatibility complex (MHC) I molecules? To produce HIV that infects neighboring cells? To migrate, perhaps to draining lymphoid organs that have high densities of infectable targets? What do we really know about the exact early events, temporally and spatially, of HIV transmission? Perhaps not enough to make informed predictions about what optimal cell-mediated immunity would look like.
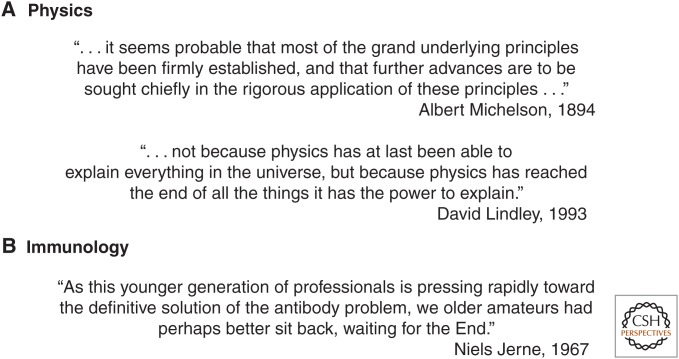
The basic point here is that there is a lot we do not know. So thinking that something is impossible, predicated on the conventional knowledge of today that is woefully incomplete, is risky (see Fig. 1). But our ignorance opens the possibility and thus opportunity to discover new technology or approaches that will solve today’s problems.
Figure 1.
Previous announcements of the end of scientific fields have been premature. (A) Quotes predicting the end of physics. (B) Even in the comparatively young field of immunology, past thought leaders believed too soon that we had essentially figured everything out. See Silverstein (2001) for a colorful accounting of premature predictions on the end of immunology.
CONCLUDING REMARKS
We have presented arguments that CD8 T cells might contribute to vaccine-mediated protection against current and future unmet infectious challenges. Importantly, CD8 T-cell responses do not necessarily prevent humoral responses, and approaches that leverage both arms of the immune system may have their place. Ultimately, bringing new licensed vaccines to market that elicit robust CD8 T-cell memory will require a real need for a vaccine, failure of humoral-only approaches (assuming that they are tried first), and the political willpower to pursue research on modalities that do not completely compromise immunogenicity for the sake of safety.
Footnotes
Editors: Shane Crotty and Rafi Ahmed
Additional Perspectives on Immune Memory and Vaccines: Great Debates available at www.cshperspectives.org
REFERENCES
- Amanna IJ, Raué HP, Slifka MK. 2012. Development of a new hydrogen peroxide–based vaccine platform. Nat Med 18: 974–979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariotti S, Hogenbirk MA, Dijkgraaf FE, Visser LL, Hoekstra ME, Song JY, Jacobs H, Haanen JB, Schumacher TN. 2014. T cell memory. Skin-resident memory CD8+ T cells trigger a state of tissue-wide pathogen alert. Science 346: 101–105. [DOI] [PubMed] [Google Scholar]
- Bhan A, Green SK. 2011. Balancing safety, efficacy and cost: Improving rotavirus vaccine adoption in low- and middle-income countries. J Glob Health 1: 148–153. [PMC free article] [PubMed] [Google Scholar]
- Carbone FR. 2015. Tissue-resident memory T cells and fixed immune surveillance in nonlymphoid organs. J Immunol (Baltim Md 1950) 195: 17–22. [DOI] [PubMed] [Google Scholar]
- Doores KJ. 2015. The HIV glycan shield as a target for broadly neutralizing antibodies. FEBS J 282: 4679–4691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland SM, Kjaer SK, Muñoz N, Block SL, Brown DR, DiNubile MJ, Lindsay BR, Kuter BJ, Perez G, Dominiak-Felden G, et al. 2016. Impact and effectiveness of the quadrivalent human papillomavirus vaccine: A systematic review of 10 years of real-world experience. Clin Infect Dis Off Publ Infect Dis Soc Am 63: 519–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant EJ, Quiñones-Parra SM, Clemens EB, Kedzierska K. 2016. Human influenza viruses and CD8+ T cell responses. Curr Opin Virol 16: 132–142. [DOI] [PubMed] [Google Scholar]
- Gray GE, Laher F, Lazarus E, Ensoli B, Corey L. 2016. Approaches to preventative and therapeutic HIV vaccines. Curr Opin Virol 17: 104–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen SG, Ford JC, Lewis MS, Ventura AB, Hughes CM, Coyne-Johnson L, Whizin N, Oswald K, Shoemaker R, Swanson T, et al. 2011. Profound early control of highly pathogenic SIV by an effector memory T-cell vaccine. Nature 473: 523–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen SG, Wu HL, Burwitz BJ, Hughes CM, Hammond KB, Ventura AB, Reed JS, Gilbride RM, Ainslie E, Morrow DW, et al. 2016. Broadly targeted CD8+ T cell responses restricted by major histocompatibility complex E. Science 351: 714–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harty JT, Tvinnereim AR, White DW. 2000. CD8+ T cell effector mechanisms in resistance to infection. Annu Rev Immunol 18: 275–308. [DOI] [PubMed] [Google Scholar]
- Hirano M, Das S, Guo P, Cooper MD. 2011. The evolution of adaptive immunity in vertebrates. Adv Immunol 109: 125–157. [DOI] [PubMed] [Google Scholar]
- Hoffman SL, Vekemans J, Richie TL, Duffy PE. 2015. The march toward malaria vaccines. Vaccine 33: D13–D23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishizuka AS, Lyke KE, DeZure A, Berry AA, Richie TL, Mendoza FH, Enama ME, Gordon IJ, Chang LJ, Sarwar UN, et al. 2016. Protection against malaria at 1 year and immune correlates following PfSPZ vaccination. Nat Med 22: 614–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koff WC, Burton DR, Johnson PR, Walker BD, King CR, Nabel GJ, Ahmed R, Bhan MK, Plotkin SA. 2013. Accelerating next-generation vaccine development for global disease prevention. Science 340: 1232910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu S. 2009. Heterologous prime-boost vaccination. Curr Opin Immunol 21: 346–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masopust D, Vezys V, Wherry EJ, Ahmed R. 2007. A brief history of CD8 T cells. Eur J Immunol 37: S103–S110. [DOI] [PubMed] [Google Scholar]
- Morens DM, Fauci AS. 2013. Emerging infectious diseases: Threats to human health and global stability. PLoS Pathog 9: e1003467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moutaftsi M, Tscharke DC, Vaughan K, Koelle DM, Stern L, Calvo-Calle M, Ennis F, Terajima M, Sutter G, Crotty S, et al. 2010. Uncovering the interplay between CD8, CD4 and antibody responses to complex pathogens. Future Microbiol 5: 221–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pamer EG. 2004. Immune responses to Listeria monocytogenes. Nat Rev Immunol 4: 812–823. [DOI] [PubMed] [Google Scholar]
- Plotkin S. 2014. History of vaccination. Proc Natl Acad Sci 111: 12283–12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schenkel JM, Fraser KA, Beura LK, Pauken KE, Vezys V, Masopust D. 2014. T cell memory. Resident memory CD8 T cells trigger protective innate and adaptive immune responses. Science 346: 98–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seder RA, Chang LJ, Enama ME, Zephir KL, Sarwar UN, Gordon IJ, Holman LA, James ER, Billingsley PF, Gunasekera A, et al. 2013. Protection against malaria by intravenous immunization with a nonreplicating sporozoite vaccine. Science 341: 1359–1365. [DOI] [PubMed] [Google Scholar]
- Silverstein AM. 2001. The end of immunology? Nat Immunol 2: 893–895. [DOI] [PubMed] [Google Scholar]
- Spriggs MK, Koller BH, Sato T, Morrissey PJ, Fanslow WC, Smithies O, Voice RF, Widmer MB, Maliszewski CR. 1992. β2-Microglobulin–, CD8+ T-cell-deficient mice survive inoculation with high doses of vaccinia virus and exhibit altered IgG responses. Proc Natl Acad Sci 89: 6070–6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taubenberger JK, Morens DM. 2010. Influenza: The once and future pandemic. Public Health Rep Wash DC 1974 125: 16–26. [PMC free article] [PubMed] [Google Scholar]
- Xu R, Johnson AJ, Liggitt D, Bevan MJ. 2004. Cellular and humoral immunity against vaccinia virus infection of mice. J Immunol (Baltim Md 1950) 172: 6265–6271. [DOI] [PubMed] [Google Scholar]