Abstract
Melatonin exhibits extraordinary diversity in terms of its functions and distribution. When discovered, it was thought to be uniquely of pineal gland origin. Subsequently, melatonin synthesis was identified in a variety of organs and recently it was shown to be produced in the mitochondria. Since mitochondria exist in every cell, with a few exceptions, it means that every vertebrate, invertebrate, and plant cell produces melatonin. The mitochondrial synthesis of melatonin is not photoperiod-dependent, but it may be inducible under conditions of stress. Mitochondria-produced melatonin is not released into the systemic circulation, but rather is used primarily in its cell of origin. Melatonin’s functions in the mitochondria are highly diverse, not unlike those of sirtuin 3 (SIRT3). SIRT3 is an NAD+-dependent deacetylase which regulates, among many functions, the redox state of the mitochondria. Recent data proves that melatonin and SIRT3 post-translationally collaborate in regulating free radical generation and removal from mitochondria. Since melatonin and SIRT3 have cohabitated in the mitochondria for many eons, we predict that these molecules interact in many other ways to control mitochondrial physiology. It is predicted that these mutual functions will be intensely investigated in the next decade and importantly, we assume that the findings will have significant applications for preventing/delaying some age-related diseases and aging itself.
Keywords: reactive oxygen species, oxidative stress, molecular pathways, sirtuins, antioxidant enzymes, oxidative phosphorylation
1. Introduction
Genetic diversity often exceeds that which is predicted based on the number of genes that have been sequenced [1,2]. This suggests that epigenetic processes may account for the greater molecular heterogeneity than that which is apparent in organisms [3,4]. Within recent decades, unraveling the mechanisms whereby the large variety of epigenetic modifications (post-translational modifications) are achieved has been a major area of research [5,6,7].
Sirtuins are a class of histone deacetylates that are homologues of a translational repressor, the first of which was originally discovered in yeast (Saccharomyces cerevisiae) and named mating-type regulator 1 (MAR1) [8,9]. Almost a decade later, Rine and colleagues [10] extended the findings of Klar et al. [8,9] when they identified four deacetylases in S. cerevisiae; they abandoned the name mating-type regulator and renamed the enzymes silent information regulators; since they had identified four such enzymes they were named SIR1-4.
In the last 25 years, the associated enzymes, now called sirtuins (SIRT), have been major agents of intensive investigative endeavor and they have been linked to a wide variety of physiological processes [11,12,13]. The actions include longevity-promoting effects [14,15], for their ability to inhibit cancer [16,17] and, more recently, because of their involvement in circadian rhythm regulation [18,19,20].
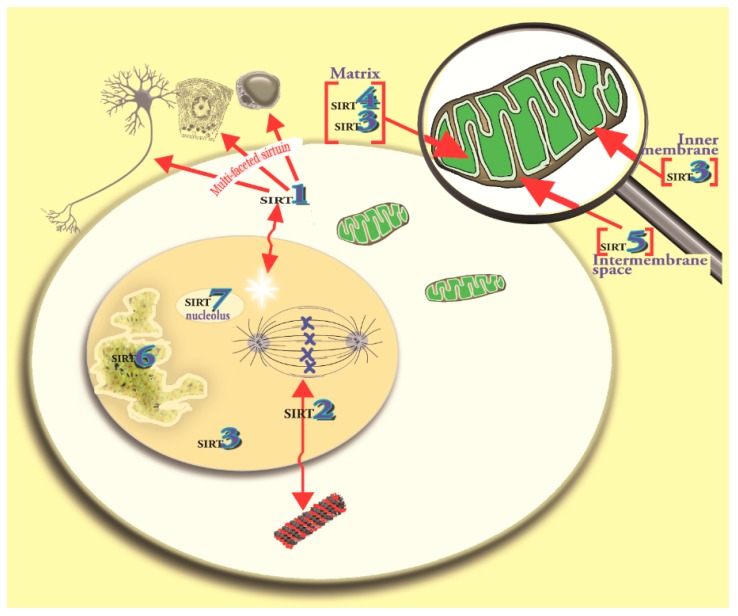
The sirtuin family in mammalian cells now includes seven members (SIRT1–7); they are collectively known as the cellular acylome [21]. Each sirtuin has a well-conserved NAD+-binding domain. The sirtuins have a variety of enzymatic activities and functions and they are differentially distributed at the subcellular level (Figure 1) [1,22]. One major function of sirtuins is to act as sensors of energy availability and, during each reaction, they consume molecules of NAD+ [5,23]. The best-known members of the sirtuin family that function as metabolic sensors include SIRT1, which is primarily located in the nucleus of cells and SIRT3 which is concentrated in the mitochondria [24,25]. Mitochondrial SIRT3 [12,26] is susceptible to regulation by exogenously-supplied melatonin; this is consistent with melatonin being a mitochondria-targeted antioxidant [27,28,29,30].
Figure 1.
This figure identifies the primary location of sirtuins 1–7 in eukaryotes. Sirtuins are NAD+-dependent deacetylates which account for post-translational modifications of molecules within cells; sirtuins have a wide variety of functions including the promotion of longevity and the prevention in age-related diseases. For the purposes of the current report, specific interest is directed to mitochondrial SIRT3, the activity of which has been shown to be modulated by melatonin. SIRT3 is primarily located in the mitochondria where it co-localizes with melatonin. Both these molecules are involved in redox regulation and, as shown in this report, they are functionally intertwined. Single arrowheads identify structure; double headed arrows identify movement of molecules.
Of the seven sirtuins, three (SIRT3, SIRT4 and SIRT5) are located, although not exclusively, in the mitochondria, attesting to their potential involvement in their regulation of metabolism and especially of respiratory changes and oxidative phosphorylation [31,32,33]. Evidence has accumulated showing that melatonin, which exists in mitochondria along with SIRT3, influences the deacetylation of this sirtuin [28]. Since SIRT3 is known to modulate the redox state of the mitochondria, as does melatonin, we surmised these actions may be interrelated. Those relationships are discussed in this report.
2. Melatonin: Harnessing Free Radicals
The discovery of melatonin as a free radical scavenger 25 years ago [34] was preceded by reports that the indole protected against DNA damage as a result of being exposed to a chemical carcinogen [35] and was alleged to be a life-promoting molecule, as was SIRT3. Given that both these processes were believed to be related to oxidative stress [36,37], the initial studies designed to test the radical trapping ability of melatonin were undertaken. The hydroxyl radical (•OH), the most destructive of the oxygen-based toxic species, was generated by exposing a solution of hydrogen peroxide (H2O2) to ultraviolet light. A spin trapping agent, 5,5′-dimethylpyrroline N-oxide (DMPO), was added to the solution with or without the addition of melatonin; DMPO captures the •OH with the formation of an adduct, DMPO-•OH [38]. In the absence of melatonin in the solution, this adduct was abundant; however, when melatonin was added to the solution adduct formation was almost zero indicating melatonin had scavenged the •OH and reduced their availability to form a DMPO-•OH. When melatonin was compared to two other known •OH scavengers, glutathione or mannitol, melatonin proved superior as a radical quencher in this pure chemical system. The presence of the DMPO-•OH adduct was verified using high performance liquid chromatography with an electrochemical detector (HPLC-EC) and further confirmed with electron spin resonance spectroscopy (ESR) [39]. Given that these studies were performed using a cell-free system, it was obvious that the radical scavenging actions did not require membrane melatonin receptors (or any other receptor/binding site) which had been described [40,41] to exist in many cells.
The discovery that melatonin was a highly-efficient •OH scavenger was met with considerable skepticism by mainstream free radical biologists. They were resistant for several reasons. The first reason seemed to be was that they simply did not believe the data. Previously, there had been no hint that melatonin or related molecules had radical scavenging potential. Also, they argued that because of its very high reactivity, the •OH interacts (is scavenged by) with any molecule in its vicinity. In our study, however, we had compared melatonin with two confirmed •OH scavengers, i.e., glutathione and mannitol, both of which showed less reactivity to the free radical than did melatonin. Within a year after the initial publication, the radical scavenging capability of melatonin was confirmed in another chemical system using other methods [42].
Another reason that was used for rejecting the idea of the radical scavenging capability of melatonin was that there was little evidence that it functions in the detoxification and the reduction of oxidative stress in vivo or in cultured cells. This deficiency was soon rectified, however, since within two years melatonin was documented to reduce oxidative stress in vivo due to glutathione depletion [43], ionizing radiation exposure [44], paraquat toxicity [45], lipopolysaccharide [46,47], kainic acid [48], and ischemic/reperfusion injury [49]. The cellular damage in each of these situations is known to involve toxic free radicals and strongly support the idea that melatonin can protect a variety of molecules against oxidative stress in vivo.
The repeated independent verification of the capability of melatonin to function as a free radical scavenger [50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68] and to hold oxidative stress in check has solidified the idea that this intrinsically-produced indole is a legitimate in vivo agent that limits oxidative damage. An additional small percentage of the total number of published reports substantiating the ability of melatonin to limit oxidative stress under conditions that would have otherwise had disastrous consequences are summarized in Table 1 [69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100].
Table 1.
Experimental evidence that melatonin reduces oxidative stress and related events in cells, animals, and humans. Listed here are representative publications where melatonin was used to diminish oxidative damage and/or associated physiological/molecular changes following exposure to a variety of different chemical toxins/processes that normally lead to oxidative mutilation of critical molecules, cellular apoptosis, and compromised organ function. As mentioned, these are representative reports; there are many more. If the reader has a specific interest in a toxin/melatonin interaction, it (they) could be easily found in an appropriate literature search. Also, for many of the subjects listed, there are numerous publications documenting the protective function of melatonin, e.g., in ischemia/reperfusion injury, heavy metal toxicity, etc. The reports are in chronological order.
| Toxin/Process | Tissue Protected | Reference |
|---|---|---|
| Carbon tetrachloride | Liver | [69] |
| Hyperbaric oxygen | Lung and brain | [70] |
| 2-Nitropropane | Lipid and DNA | [71] |
| Cerulein | Pancreas | [72] |
| Quinolinic acid | Brain | [73] |
| δ-Aminolevulinic acid | Lipid and DNA | [74] |
| Neonatal asphyxia (human) | Lipid | [75] |
| Ochratoxin A | Liver and kidney | [76] |
| Ultraviolet radiation | Leucocytes | [77] |
| Respiratory distress syndrome (human) | Lung | [78] |
| 1-Methyl-4-phenyl-1,2,3,6-tetrahydro pyridine | Brain | [79] |
| Organ transplantation | Liver | [80] |
| Diquat | Lipid | [81] |
| Cerebral hypoperfusion | Brain | [82] |
| Aspirin (human) | Gastrointestinal tract | [83] |
| Opisthorchis viverrini (liver fluke) | Liver | [84] |
| Methamphetamine | Brain | [85] |
| Doxorubicin | Heart | [86] |
| Cobra toxin | Multiple tissues | [87] |
| Strenuous exercise | Skeletal muscle | [88] |
| Ionizing radiation | Oral mucosa | [89] |
| Ischemia/reperfusion | Heart | [90] |
| Cadmium | Brain | [91] |
| Phosphine | Heart | [92] |
| Neonatal sepsis (human) | Neonate | [93] |
| ST-segment elevation, myocardial infarction (human) | Heart | [94] |
| Ischemia/reperfusion | Brain | [95] |
| p-Cresol | Mesenchymal stem cells | [96] |
| Arsenic trioxide | Liver | [97] |
| Type 2 diabetes | Cardiovascular system | [98] |
| Hexavalent chromium | Spermatogonia | [99] |
| Ischemia/reperfusion | Lung | [100] |
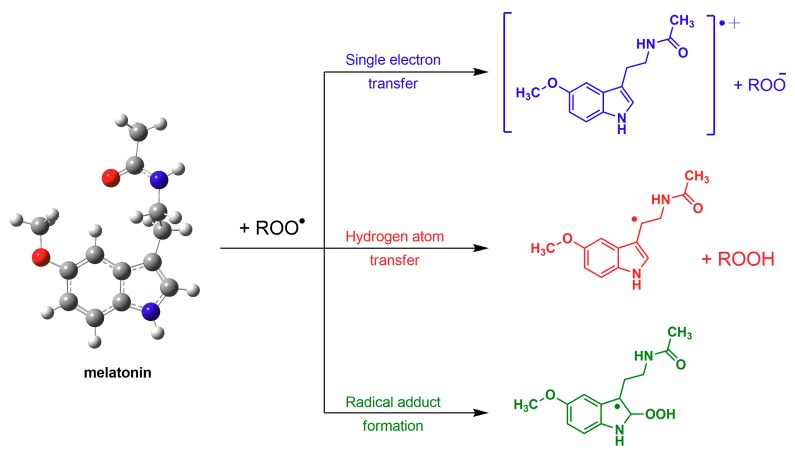
Some of the mechanisms by which melatonin detoxifies the peroxyl radical include (a) single electron transfer; (b) hydrogen atom transfer; or (c) possibly radical adduct formation [101,102,103] (Figure 2). When melatonin interacts with other radicals the adducts formed may be different than the one shown in the figure. Despite overwhelming evidence, there may be some who deny that melatonin is a radical scavenger or that it can curb oxidative stress [104,105] or they claim that it is only a weak scavenger [104,106].
Figure 2.
The means by which melatonin detoxifies a lipid peroxyl radical (LOO•) are shown in this figure and include electron transfer, hydrogen ion transfer and radical adduct formation. These are examples of actions of melatonin that are receptor independent. If the free radical was a •OH radical rather than a LOO• radical, because of the very high reactivity of the former, the number of reaction products would be much greater.
Those who assert that melatonin is unlikely an essential physiological antioxidant in vivo argue that, because pharmacological quantities must be given to combat severe oxidative damage, e.g., during ischemia/reperfusion events, it is normally inconsequential as an inhibitor of oxidative stress. Oxidative damage would never occur if physiological concentrations of all antioxidants combined, i.e., vitamin C, glutathione, uric acid, melatonin, etc., were adequate to overcome the massive onslaught of free radicals that occur under such conditions. Thus, “pharmacological” amounts of free radicals are produced during these catastrophic events, which requires pharmacological concentrations of any antioxidant, not only melatonin, to effectively combat the molecular damage.
Other aspects of melatonin that contribute to its image as a highly-effective antioxidant include (a) metabolites that are formed when melatonin incapacitates a radical species also function in free radical detoxification [66,107,108,109,110,111,112,113] in what is called the antioxidant cascade; (b) melatonin chelates metal ions that are involved in the Haber-Weiss and Fenton reactions thereby preventing the formation of the devastatingly reactive •OH [114,115]; (c) melatonin stimulates antioxidant enzymes which removes potential damaging species from the intercellular environment [116,117,118,119,120,121,122,123] while; (d) inhibiting pro-oxidant enzymes (e.g., myeloperoxidase, lipoxygenase, etc.) [124]; (e) melatonin also synergizes with classic radical scavengers making them more effective in reducing oxidative damage [125,126]; (f) melatonin stimulates a cytosolic detoxifying enzyme quinone reductase [127]; and (g) melatonin increases the efficiency of the transfer of electrons between the mitochondrial respiratory complexes thereby reducing electron leakage and free radical formation [128,129]. Considering the multiple means by which melatonin annihilates reactive oxygen species, it would seem to be relentless in preventing molecular damage and maintaining a functional subcellular infrastructure.
3. Intrinsic Sources of Melatonin
Melatonin, although initially thought to be synthesized only in the pineal gland [130,131,132], was soon found to be produced in the vertebrate retinas as well [133,134]. Of these two sites, only the mammalian pineal gland is known to release significant amounts, presumably by simple diffusion out of the cells, of melatonin that would function systematically, with two routes of discharge being utilized, i.e., directly into the third ventricle of the central nervous system [124,135,136,137] and into the blood capillaries that are abundant in this tissue [138,139]. Although there may be some “incidental” leakage of small amounts of melatonin into the blood from other tissues (e.g., gut) there is no compelling evidence for a persistent or cyclic release of melatonin from these organs [140] as has been shown for the pineal gland [141,142]. If melatonin escapes the pinealocyte by simple diffusion into the blood, why melatonin produced in other cells does not do so as well is unexplained. Thus, following surgical removal of the pineal gland, circulating levels of melatonin persist at values that are barely measurable [141,142]. Exogenously administered melatonin, e.g., orally, subcutaneously, or intraperitoneally, does cause transient large increases in blood melatonin concentrations [143,144].
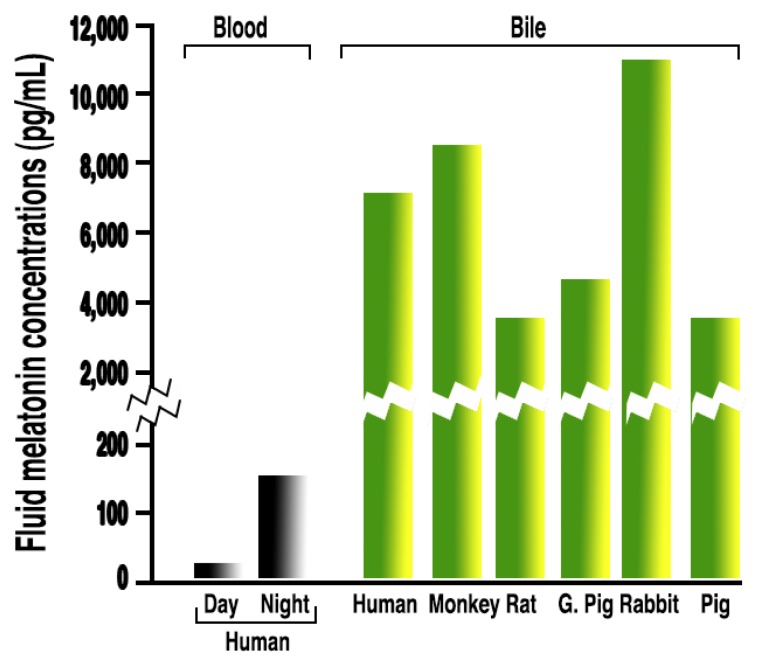
3.1. Melatonin in Bodily Fluids
Despite these general observations, based on the high melatonin concentrations in some bodily fluids, the possibility that other cells may produce and release melatonin into fluids other than the blood has been speculated, e.g., very high levels of melatonin in the bile (Figure 3) may be from hepatocytes [145] and concentrations of melatonin in ovarian follicular fluid that exceed those in the blood may be from granulosa cells [146,147] and perhaps from oocytes themselves [148].
Figure 3.
Radioimmunoassayable melatonin levels in the bile of six mammalian species. These values are clearly much higher than in the blood, both during the day or at night (two bars on far left). Levels of melatonin in the fluids other than the blood that exceed the concentration of this indole in the blood is not unusual. Melatonin values in several other bodily fluids and within subcellular organelles also exceed those in the blood.
In the pineal gland, melatonin is produced and released in a photoperiodic-dependent circadian manner [149,150] with the cerebrospinal fluid (CSF) and blood levels modulating, respectively, organismal-wide circadian rhythms via actions on the master biological clock, the suprachiasmatic nucleus (SCN) [151,152,153], and on peripheral oscillators that exist in presumably all cells [154,155,156,157]. How important the quantity of melatonin released from the pineal gland is relative to the total amount of oxidative stress an animal experiences, e.g., as a result of the persistent mitochondrial metabolism of oxygen and production of adenosine triphosphate (ATP), is not well defined [158,159,160]. Moreover, whether the elevated oxidative stress that occurs after surgical removal of the pineal gland is exclusively related to the loss of the nocturnal rise in melatonin or whether it is a consequence of circadian dysregulation remains undetermined. Any treatment that causes a perturbation of the melatonin rhythm is likewise associated with some change in circadian rhythmicity, and vice versa [161]. Thus, identifying which of those is the cause of a specific abnormality cannot always be deciphered.
If the amount of melatonin that is released from the pineal gland is, in fact, relevant as a direct intracellular free radical scavenger in peripheral tissues, by necessity it would have to enter cells and gain access to mitochondria, the major site of reactive oxygen species (ROS) generation. Physiological levels of circulating melatonin have a short half-life in the blood (30–40 min) indicating it is rapidly taken up by peripheral tissues, either for metabolic breakdown (e.g., by hepatocytes) or by all tissues so it can carry out its intracellular functions (e.g., as a radical quencher).
Under extremely stressful conditions, e.g., forced swimming for rats, even high nocturnal levels of melatonin in the blood almost instantaneously disappear [162,163]; this very rapid disappearance seemingly exceeds the ability of the liver to catabolize such large amounts of melatonin in very short time. Rather, the swift drop in circulating blood melatonin concentrations under conditions of intensive stress more likely relates to its rapid uptake by cells throughout the body where it is needed to neutralize, directly or indirectly, the massive numbers of free radicals that are being produced, especially at the mitochondrial level [164,165].
3.2. Mitochondrial Melatonin
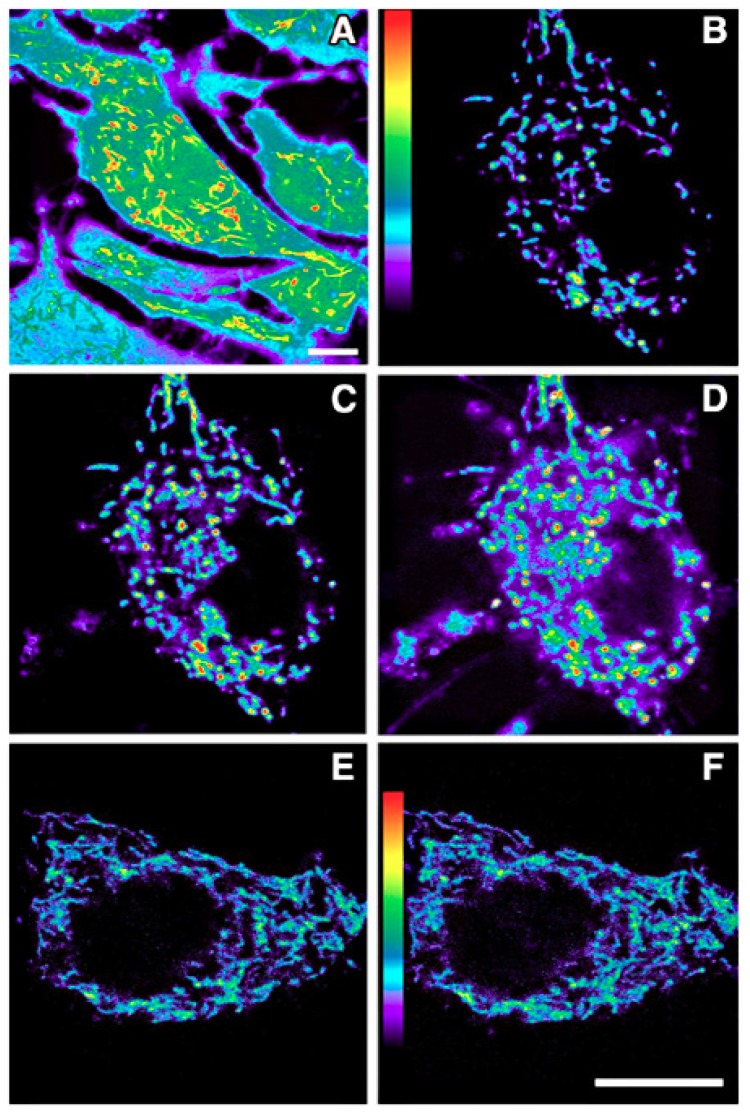
That melatonin can enter cells and their mitochondria is undisputed. Using fluorescence imaging techniques, Jou and her colleagues [166,167,168] have repeatedly shown that high free radical generation by mitochondria is quickly quenched when the cells are incubated in a solution containing melatonin (Figure 4). These findings are consistent with melatonin from the incubation medium quickly penetrating the membranes of both the cell and of the mitochondria where it neutralizes, either by direct scavenging or via indirect means, the free radicals formed in the intermembrane space and in the matrix. Besides functioning as a radical scavenger in mitochondria, melatonin has other actions that probably necessitate its presence in these organelles. Thus, at this level, melatonin enhances mitochondrial antioxidant enzymes, promotes respiration and ATP production, negates the intrinsic apoptosis pathway, and mediates its effects on sirtuins [1,169,170]. These actions would generally require more time to appear since they would involve induction mechanisms.
Figure 4.
Fluorescent imaging of the intense generation of reactive oxygen species in a cultured astrocyte at 5 min (C) and 10 min (D) after its exposure to an oxidizing agent (H2O2). The cell shown in panels (E) (5 min) and (F) (10 min) was also exposed to the H2O2, but additionally, melatonin was present in the culture medium. Clearly, melatonin was taken into the cell and into mitochondria where it reduced reactive oxygen species generation or quickly scavenged them when they were produced. Dihydrorhodamine 123 was used to visualize free radical generation. (A) is an enhanced pseudocolor image which shows the higher levels of reactive oxygen species in mitochondria relative to other organelles. (B) is the astrocyte (also shown in the panels (C,D)) before its exposure to H2O2. Figure provided by Mei-Jie Jou. Scale bar = 1 µm.
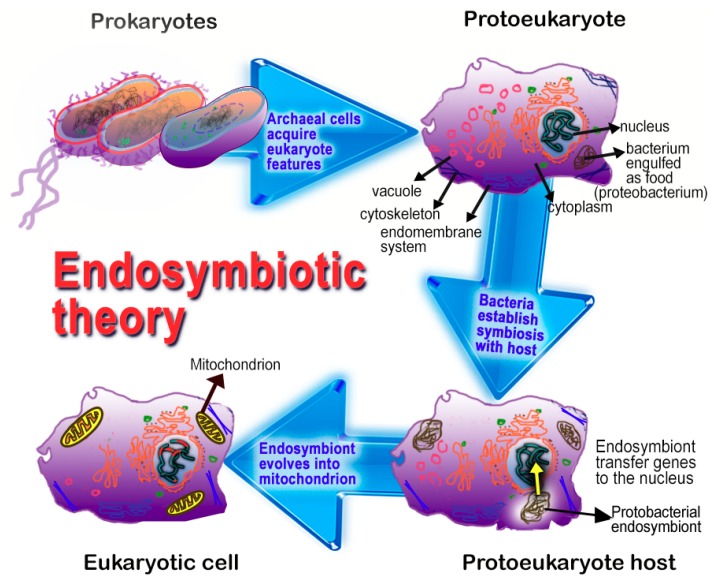
To explain the ever-widening array of cells that synthesized melatonin, we recently proposed that multicellular organisms actually synthesize melatonin in their mitochondria [171]. This hypothesis is based on considerations related to the proposed origin of mitochondria in eukaryotes. According to the Endosymbiotic Theory, mitochondria in eukaryotes are derived from bacteria which were initially engulfed for their nutrient value; eventually, the phagocytosed bacteria developed a symbiotic relationship with their host cells and evolved into mitochondria (Figure 5) [172,173]. During evolution, the newly-developed mitochondria kept the important functions that their precursors possessed. Thus, they retained their ability to carry on oxidative phosphorylation and ATP production and their capacity to synthesize melatonin [28,171]. While bacteria have long been known to produce ATP as an energy source, only recently have bacteria been shown to contain melatonin, presumably a result of synthesis in these organisms [174,175,176]. Thus, any cell (animal or plant) that contains mitochondria may also have the capability to produce melatonin [28,171] since mitochondria derived from melatonin-producing bacteria [174,175]. The production of melatonin by mitochondria is now supported by reports that have been published after mitochondria being a source of melatonin was suggested (see below).
Figure 5.
A summary of the major theory, the Endosymbiotic Theory, that explains the evolution of mitochondria as they exist in current-day eukaryotic cells. Accordingly, prokaryotic “cells” evolved features of eukaryotes over millions of years. An example of one major development, as it relates to the current review, is the phagocytosis of proteobacteria by prokaryotes; the bacteria were initially engulfed as nutrients by their digestion in intracellular granules. Eventually, the engulfed bacteria established a mutually beneficial association (a symbiotic relationship) with the host cell; the new endosymbiont sent much of its genetic material to the nucleus of the host while the symbiont gradually evolved into a mitochondrion. Since the proteobacteria already had the capability to produce energy (ATP) and melatonin, these functions were retained by the mitochondria and proved beneficial to the host cells. As a result, it is our contention that every mitochondria-containing cell produces melatonin in their mitochondria. The Endosymbiotic Theory for the origin of mitochondria was suggested more than 100 years ago and has been refined, and widely accepted, in the last three decades. Using current molecular technologies, it has been possible to document many metabolic similarities between bacteria and mitochondria. The Endosymbiotic Theory is used as an explanation as to why mitochondria produce melatonin, a function inherited from their precursors, i.e., bacteria.
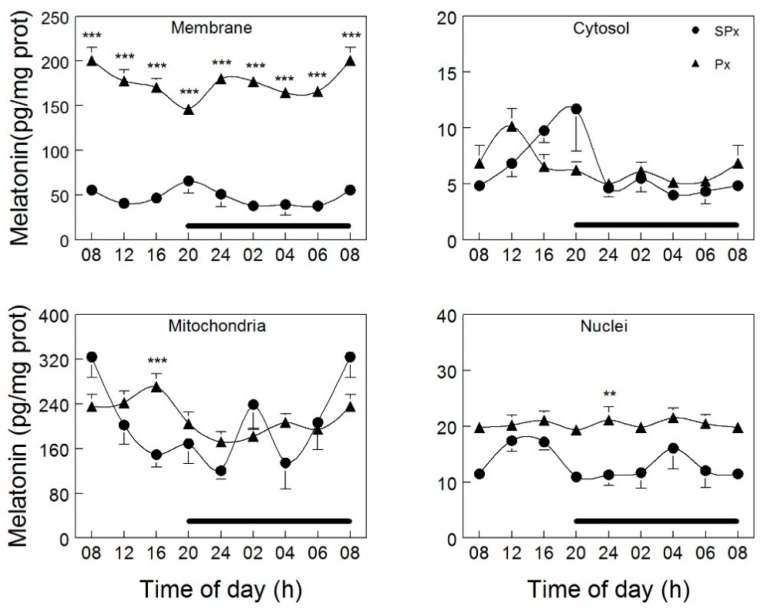
In 2012, Venegas and coworkers [177] collected the brain and liver from rats at 4-h intervals over a 24-h light:dark cycle. For the purposes of determining whether melatonin was differentially distributed in neurons and hepatocytes and, if so, whether the concentrations varied between the light and dark periods, they isolated cellular membranes, cytosol, mitochondria, and nuclei. The results unequivocally show that, at least for brain cells and hepatocytes, melatonin levels are not in equilibrium at the subcellular level. Of the four fractions in which melatonin was measured, brain mitochondria had much higher melatonin concentrations than the other sites; thus, the levels of melatonin were about 25 times greater in mitochondria than in cytosol (Figure 6). When hepatocyte-derived mitochondria were examined, these values were not at the same high level as those seen in brain mitochondria.
Figure 6.
Concentrations and fluctuations of melatonin in organelles obtained from cells of the cerebral cortex of rats that were either intact (SPx) or pinealectomized (Px). Only in cellular membranes did Px markedly change melatonin levels; in this organelle, melatonin values rose substantially as a consequence of pineal removal (p < 0.001). In the mitochondria and nucleus, at one time point each, melatonin levels were elevated (** p < 0.05 and *** p < 0.001 respectively). Tissues were collected at 4 h intervals over a 24-h light:dark cycle. The period of darkness is identified by the horizontal black bar. What is most apparent is that levels of melatonin in brain mitochondria greatly exceed its values in other subcellular locations. Figure provided by Dario Acuna-Castroviejo.
The intracellular melatonin levels were clearly not derived from the blood since when these measurements were made in cells that were obtained from pinealectomized animals, a procedure which reduces circulating melatonin levels to essentially zero, the concentrations of melatonin actually increased in the membranes (10-fold) and cytosol (2-fold), but was essentially without influence on these levels in either the brain nuclei or mitochondria [177]. In both the intact and pinealectomized animals, organellar levels of melatonin did not vary over a 24-h period. The exceptionally high levels of melatonin in brain mitochondria speaks to the likelihood that this organelle is uncommonly efficient in sequestering/retaining melatonin or it produces it. The remarkably high concentrations of melatonin in brain mitochondria is fortuitous considering that this organelle produces many free radicals during respiration. This is supported by the fact that the central nervous system has a very high metabolic rate and uses a much larger portion of the inhaled oxygen than would be predicted based on its size.
The observations of Venegas et al. [177] do not preclude the possibility that mitochondria may both avidly take up melatonin from extracellular locations, e.g., blood, as well as synthesize it. As shown above, the reports of Jou et al. [167,168] document that when cultured cells are incubated with melatonin, it may rapidly gain access to mitochondria where it visually lowers free radical products. Similarly, also as mentioned above, melatonin given to animals via any route reduces reactive oxygen species damage to cells implying that the indole gets to the source of the bulk of the free radicals, i.e., the mitochondria.
It has generally been assumed that, as noted above, due to the high lipophilicity of melatonin, it readily enters cells via simple diffusion. While this remains a possible route for its entrance into cells, recent studies have examined active transport means by which it passes through membranes. The first serious attempt to determine how high intracellular levels of melatonin are achieved, Hevia et al. [178] examined the uptake of melatonin in a variety of normal and cancer cells. For this purpose, cells were incubated in a solution containing pharmacological concentrations (1 mM) of melatonin. Independent of the cell type, incubation for 24 h always increased intracellular levels of the indole. The findings were not consistent with the passive uptake of the indole; rather the data suggested a protein-mediated uptake process which was impacted by the ambient glucose concentration. The protein involved was subsequently identified as the GLUT1 transporter. Accelerated melatonin uptake is further exaggerated in a high glucose environment in erythrocytes [179].
Huo and colleagues [180] recently defined another means by which melatonin may enter both cells and mitochondria; in this case, however, only human cancer cells were examined. The results are consistent with the involvement of the PEPT1/2 oligopeptide transporters in the transfer of melatonin through both the cell and mitochondrial membranes. Docking analysis studies as well as kinetic measurements support a role for the oligopeptide transporters aiding the uptake and retention of melatonin within cells and especially within mitochondria. For a detailed discussion of the active transport mechanisms for melatonin, the reader is directed to a recent report by Mayo et al. [1].
In view of the seemingly special association of melatonin with mitochondria [27,171] along with the protective advantages against free radicals that this would provide, interest in the potential local synthesis of melatonin by mitochondria has become a subject of active investigation. Considering that melatonin-producing bacteria [174,175] are widely accepted to be the progenitors of eukaryotic mitochondria (see Endosymbiotic Theory mentioned above and in Figure 5), it seems likely that this important function would have been retained by eukaryotic cells as we have proposed [171].
3.3. Mitochondrial Synthesis of Melatonin
In addition to the rapid uptake of melatonin by mitochondria, as noted above, we have recently drawn attention to the unique relationship of melatonin with mitochondria [27] and we proposed that this organelle likely produces its own melatonin [171]. Despite this, some toxic radicals escape being neutralized and damage adjacent macromolecules. The idea that mitochondria synthesize melatonin is based primarily on the predicted origin of mitochondria from bacteria, there is one very early study that also alluded to this possibility. In 1975, Kerenyi et al. [181] while examining the subcellular distribution of the rate-limiting enzyme in melatonin synthesis, arylalkylamine N-acetyltransferase (AANAT), claimed that in pinealocytes the reaction product for this enzyme is exclusively limited to the mitochondria. While the images of the mitochondria in this ultrastructural study are rather fragmented, nevertheless, the author’s interpretation of the findings cannot be disputed; the reaction product is in mitochondria. The results of the Kerenyi et al. [181] study were, however, rarely acknowledged in the subsequent years since individuals working on the synthesis of melatonin were likely convinced that this process was relegated to the cytosol and, also, the cytochemical method used to identify AANAT activity was less than optimal. The findings reported in the Kerenyi et al. [181] report were, however, used to support the argument of Tan et al. [171] that mitochondria are the primary site of the conversion of serotonin to melatonin.
He et al. [148] recently examined mouse oocytes as a likely location of melatonin synthesis. In an electron micrographic study, immunocytochemical AANAT was restricted to the mitochondria. More importantly, when they incubated isolated oocyte mitochondria with serotonin, a necessary precursor of melatonin production, melatonin levels were markedly increased in the mitochondria as well as in the medium in which they were incubated; in the absence of serotonin no melatonin was formed. These findings have implications beyond the identification of melatonin in oocyte mitochondria. In all offspring of fertilized ova, the mitochondria are exclusively of maternal origin. Thus, it seems likely that since oocyte mitochondria produce melatonin, all cells in the offspring would also do so.
A more complete study to establish where in cells melatonin formation occurs was published by Suofu and colleagues [182]. They used non-synaptosomal brain mitochondria for this purpose. The two terminal enzymes in melatonin production, AANAT and HIOMT, along with the AANAT chaperone, 14-3-3ζ, were in mitochondria. Like Venegas et al. [177], when melatonin synthesis was measured over a 24-h light:dark cycle, no rhythm in any of the parameters was apparent. Digesting the outer mitochondrial membrane with a combination of proteins K and digitonin did not lead to a loss of enzyme activities prompting the authors to conclude that melatonin synthesis likely occurs in the matrix. Finally, when brain mitochondria were incubated with deuterated (D4) serotonin, they yielded D4-N-acetylserotonin and D4 melatonin. The findings of Suofu et al. [182] are the most complete data indicating that mitochondria are a location of melatonin synthesis.
While the findings of Venegas et al. [177] and Suofu and coworkers [182] are noteworthy, in both reports the organ of greatest concern was the brain. In this organ, melatonin concentrations in mitochondria were very high [177] and the proteins of the melatonin-forming enzymes, AANAT and HIOMT/ASMT, were also present [182]. Thus, the presumed production of melatonin in neural tissue, of which the pineal is a part, may be unique to this organ and awaits identification in other tissues. However, based on the findings of He et al. [148] on the production of melatonin by oocyte mitochondria along with the organism-wide distribution of mitochondria from the oocyte, we feel that the mitochondria of all cells manufacture melatonin, possibly in tissue specific amounts as needed, i.e., melatonin may be inducible.
Melatonin solicits a large variety of auxiliary means to reduce mitochondrial damage potentially inflicted on hapless macromolecules as a consequence of the persistent low-level free radical generation or, in the case of toxin exposure, hypoxia, etc., to the torrents of ROS that are produced. Some of the allied processes utilized by melatonin to reduce these catastrophic effects, e.g., indiscriminate molecular destruction which ultimately leads to cellular apoptosis, include improving the efficacy of the mitochondria respiratory complexes [129,183,184], enriching ATP production [185,186], reducing free radical generation by limiting electron leakage, commonly referred to as radical avoidance [128], upregulating antioxidative enzymes [187,188], stimulating glutathione synthesis [189,190], direct radical detoxification [103,191] and probably yet to be defined means. The outcome of these combined actions is the preservation of cellular and organ physiology, as well as the prevention of organismal death, by mitigating cellular loss due to apoptosis [167,192,193,194,195].
4. The Melatonin/SIRT3 Interactions
Many post-translational modifications are mediated by sirtuins [6,7]. SIRT3 is a member of a family of seven sirtuins (1–7) that are collectively referred to as the cellular acylome [21]. Sirtuins mediate post-translational modifications of lysine residues; these actions are reversible and involve proteins in a wide variety of molecular pathways. As such, the sirtuins have a major impact on the physiology of cells [21,196,197,198,199,200]. Like melatonin, SIRT3 has actions related to reducing oxidative stress. For example, both melatonin and SIRT3 influence the generation of partially reduced oxygen species at the level of the mitochondrial respiratory complexes and both detoxify these reactants by promoting antioxidant enzyme activities [122,123]. Forkhead box 03 (FOXO3a) is a direct target of SIRT3 which is also involved in processes related to defense against oxidative damage [201,202], not unlike the actions of melatonin. Considering the common functional features of melatonin, FOXO3a and SIRT3 in mitochondria, their physiological association would seem to be a logical assumption.
4.1. Reproductive Organ Protection
Considering that human females are planning pregnancies later in their reproductive life span, there is increasing interest in identifying molecules that maintain ovarian, oocyte and uterine physiology in a more youthful state to ensure a successful pregnancy and healthy offspring. The human female reproductive axis typically declines quickly in women after the age of 35. Since, as in other organs, free radical damage contributes to diminished reproductive processes including the onset of menopause [203,204], the antioxidant melatonin has been tested for its potential in deferring the slowed follicular maturation and reduced oocyte quality observed in the aging female. The results of these studies verify that melatonin has significant benefits in maintaining the function of the ovary and adnexa which normally deteriorates with age or after exposure to toxins, etc. [205,206,207,208,209].
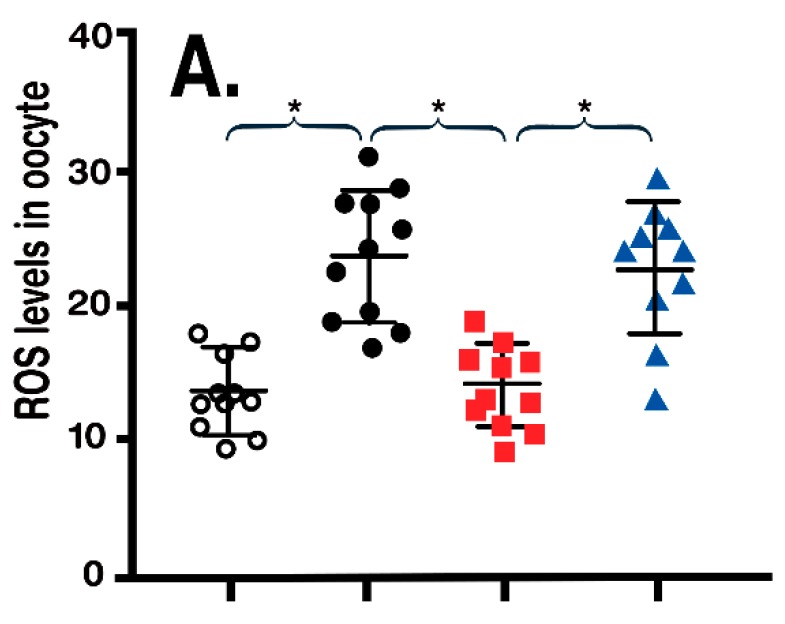
Obesity in rodents, as in humans, due to feeding/consuming a high fat diet (HFD) causes the acetylation of SIRT3, which reduces its activity and causes the catastrophic cellular damage due to unrestrained ROS generation. This damage occurs in many tissues including the oocyte, which, because of its diminished quality, jeopardizes successful fertilization and pregnancy. Because of the worldwide increase in obesity, female fertility has shown a marked decline. Since mitochondrial SIRT3 is suppressed in obese rodents, which leads to reduced SOD2 and unrestrained ROS formation, Han et al. [210] fed melatonin to obese rats. As anticipated, melatonin greatly improved oocyte quality and fertilizability; this was accompanied by an activation (deacetylation) of SIRT3, which induced SOD2 ultimately reducing oxidative stress in the oocytes. To further confirm the mechanism by which melatonin improved oocyte quality in obese mice, we used morpholino to knockdown SIRT3, a procedure that eliminated the protective actions of melatonin at the oocyte level (Figure 7).
Figure 7.
Reactive oxygen species (ROS) levels in oocytes of normal control (NO) and obese (OB) mice (A) and mean spindle/chromosomal defects (B) of the oocytes (values are means ± SEM). Obesity was associated with an increase in ROS and elevated molecular damage in oocytes. Melatonin (MEL) treatment reduced both parameters. When SIRT3 was silenced (with siRNA) the actions of melatonin were negated. This suggests that the antioxidant action of melatonin in oocytes depends on stimulation (deacetylation) of SIRT3 which enhances the activity of the antioxidant enzyme, superoxide dismutase. Figure drawn from the data of Han et al. [210]. * p > 0.001.
When melatonin was orally administered chronically to aging female mice and rats, clearly their reproductive function and performance were improved relative to those in age-matched controls not treated with melatonin. In mice, the improvement was obvious in the maintained follicle pool, litter size after mating and telomere length as well as oocyte number and quality [211]. Similarly, in female rats, melatonin delayed ovarian aging as estimated by many of the same parameters [212] measured in mice. Both Song et al. [211] and Tamura and coworkers [212] predicted that SIRT3 upregulation would be related to the melatonin maintenance of ovarian physiology in the aged rodents. In mice, melatonin treatment was accompanied by enhanced ovarian granulosa cell SIRT3 activity along with the translocation of FOXO3a to the nucleus where it bound to the promoters of SOD2 and catalase (CAT) [211]. Both SOD2 and CAT are mitochondrial antioxidant enzymes. The mitochondria of the granulosa cells also less easily generated ROS due to the H2O2 treatment when melatonin was present. In addition to the upregulation of sirtuins, melatonin may defer ovarian aging due to its direct radical scavenging activities, stimulation of telomerase, reducing autophagy, etc.
The data showing that melatonin reduces free radical generation/damage in mitochondria along with the findings of several groups which indicate that this organelle rapidly takes up and synthesizes melatonin is of great interest; however, the specific mechanisms by which the indole limits oxidative damage to this organelle remains to be determined. As already noted, melatonin has a plethora of means to curtail molecular damage resulting from exposure to free radicals. Which accounts for the reduced oxidative stress along with the subcellular mechanisms involved requires definition.
4.2. Cardiovascular Protection
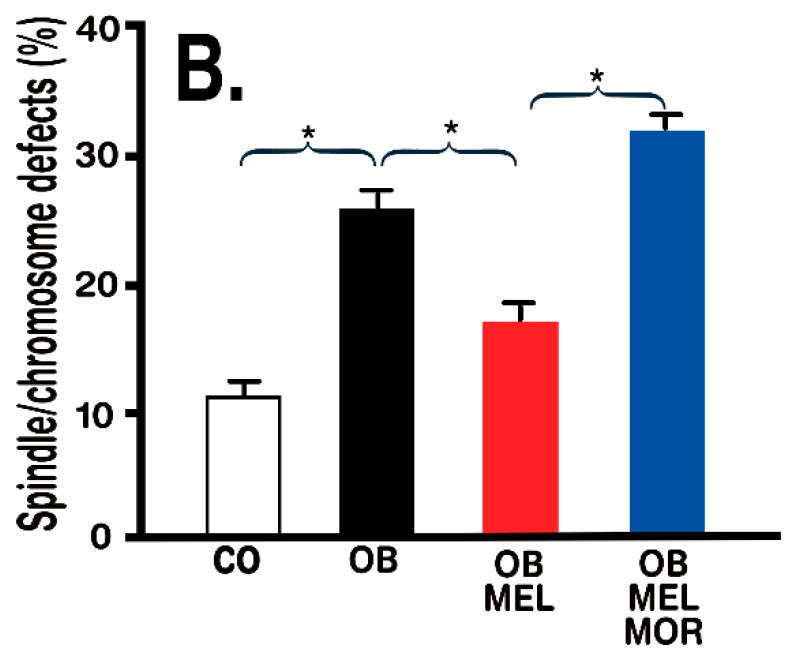
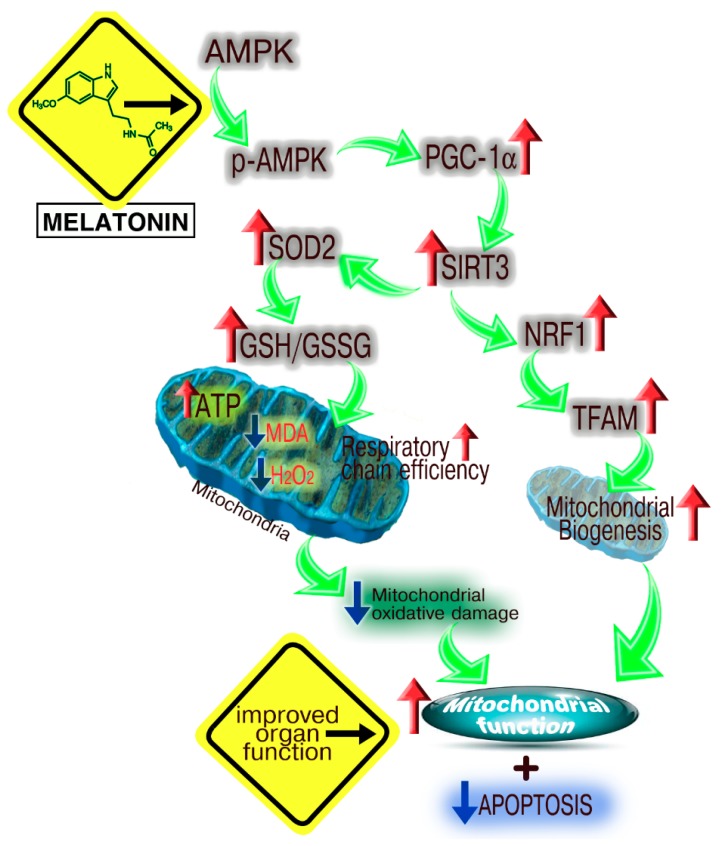
There are numerous published reports showing that melatonin reduces ischemia/reperfusion (I/R) injury in multiple organs [213,214,215] (see also some data in Table 1). One I/R model involving the heart was used to examine the possible involvement of mitochondrial SIRT3 upregulation in melatonin’s protective actions in myocardial tissue subjected to anoxia/reoxygenation. Yu and colleagues [216] tested this in type 1 diabetic rats (induced by streptozotocin) after left anterior descending coronary artery ligation for 30 min. This study was specifically directed to examining the action of melatonin at the mitochondrial level. This comprehensive investigation validated that melatonin in I/R-damaged myocardium improved cardiac physiology by augmenting ATP production and improving respiratory chain function (Complexes II, III, and IV), stimulating SOD2 activity, limiting apoptosis of cardiomyocytes and reducing H2O2 generation and lipid peroxidation. Mechanistically, Yu et al. [216] found that melatonin’s beneficial effects stemmed from its stimulation of the adenosine monophosphate–activated kinase (AMPK)-PGC-1α-SIRT3 signaling and the activation of mitochondrial superoxide dismutase (SOD) and elevated NRF (nuclear factor (erythroid-derived 2)-like 2) and TFAM (mitochondrial transcription factor A) expression (Figure 8).
Figure 8.
A summary of the proposed mechanisms by which melatonin preserves myocardial cell function after ischemia/reperfusion injury in type 1 diabetic rats. The involvement of AMPK→pAMPK was shown using compound C, a specific blocker of AMPK-signaling. The role of SIRT3 was documented with the use of SIRT3 siRNA. Melatonin protects against myocardial damage due to ischemia/reperfusion as indicated. Figure drawn from the findings of Yu et al. [216]. Red arrows indicate stimulation; blue arrows indicate inhibition; green arrows indicate flow of information.
Two subsequent reports also confirmed the involvement of melatonin and SIRT3 in protecting the heart from ROS injury [217,218]. Based on the findings of Zhai et al. [217], the role played by SIRT3 was shown by the observation that a selective inhibitor of SIRT3 [3-(1H-1,2,3-triazol-4-yl) pyridine, 3-TYP) negated the effects of melatonin as a cardioprotective agent. Due to the depression of SIRT3, SOD2 is not upregulated and oxidative stress remains at a high level which severely compromises melatonin’s ability to protect the myocardium from free radical destruction.
Zhang et al. [218] used a different model to judge how effective melatonin is in protecting the myocardium from free radical damage. The model was the diabetic cardiomyopathic mouse. Heart function was monitored echocardiographically; these measurements showed that melatonin mitigated left ventricular cardiac remodeling and preserved cardiac function in diabetic animals. The authors suspected melatonin’s advantage resulted from its actions at the mitochondrial level. To prove this, Zhang et al. [218] examined the involvement of SIRT3; this confirmed that melatonin inhibited Mst phosphorylation which led to SIRT3 stimulation and elevated antioxidant protection. Melatonin’s efficacy disappeared in Mst knockout mice. They concluded that, as others have, that the upregulation of SIRT3 is essential to the ability of melatonin to protect mitochondria from oxidation stress.
Endothelial cell dysfunction in coronary arteries and elsewhere is a feature that is essential for the development of atherosclerotic lesions [219]. While the basic process involves inflammation of the endothelial lining, the associated oxidative stress including oxidation of low-density lipoprotein are important mediators of endothelial cell malfunctions eventually culminating in plaque formation and other subsequent negative effects [220]. Previously, melatonin was shown to maintain the optimal fluidity of cell membranes [221,222] and to protect them from damage normally inflicted by free radicals.
Against this background of information, Lee et al. [223] examined the efficacy of melatonin to forestall endothelial cell damage in an ischemic limb, after lipopolysaccharide treatment and in an in vitro model using human umbilical vein endothelial cells (HUVECs). As anticipated, melatonin protected against endothelial cell destruction in the in vivo model and reduced oxidative stress levels, inflammatory reactions, cell death and mitochondrial dysfunction in HUVECs. Of special interest to the current report, when mitochondrial SIRT3 was silenced (with siRNA), melatonin’s in vitro effects were absent indicating that, as in other reports, melatonin’s antioxidant actions in mitochondria rely, to a large degree, on SIRT3 deacetylation. The authors point out that the reversal of the actions of melatonin by silencing SIRT3 are as others have observed in earlier reports. They do not provide, however, any additional information as to the signaling mechanisms by which melatonin modulates SIRT3/oxidative stress/mitochondrial malfunction.
4.3. Hepatic Protection
Fluorosis is a condition that occurs as a consequence of the long-term ingestion of fluoride. It is a progressive degenerative condition which is, in part, a result of exaggerated ROS production in hepatocyte mitochondria [224]. Melatonin has been successfully used to combat liver damage related to chronic ingestion of fluoride by experimental animals [225]. The mechanisms of protection afforded by melatonin involve limiting oxidative stress. Song et al. [226] showed that incubating human liver cells (L02) with sodium fluoride (NaF) increased intracellular superoxide production leading to the accumulation of oxidative stress and apoptotic cell death; these changes were attenuated when melatonin was added to the incubation medium. At the molecular level, melatonin stimulated SIRT3 deacetylation leading to the rapid dismutation of the superoxide; this was accompanied by SIRT3-triggered DNA binding of FOXO3a. The inhibitory pathway analysis showed that melatonin enhanced PGe-1α expression due to the activation of PI3K/AKT signaling. With the use of membrane melatonin receptor blocker, these workers proved the effects of melatonin were mediated by the MT1 receptor; this was confirmed when the L02 cells were transfected with MT1 siRNA. Presumably, the MT1 receptor involved was in the plasma membrane although it may have been in the outer mitochondrial membrane [182].
Chen and coworkers [227] examined the association of melatonin and SIRT3 on oxidative damage induced in cultured L02 hepatocytes and in mice after ligation of the bile duct. L02 is a spontaneously immortalized cell line. For the cell culture study, the active biliary toxin was glycochenodeoxycholic acid (GCDCA). Co-treatment of hepatocytes with melatonin and GCDCA highly significantly reduced mitochondrial ROS generation that was apparent in cells only treated with GCDCA. The protective actions of melatonin were associated with an upregulation of SIRT3 and the elevated deacetylation of SOD2. The actions of melatonin were blocked in hepatocytes transfected with AMP-activated, alpha-1 catalytic subunit (AMPK) siRNA. In the in vivo studies where the bile duct was ligated to produce cholestasis, the findings were similar. Melatonin’s beneficial actions in these studies were most likely related to its ability to modulate the AMPK-SIRT3-SOD2 pathway. The in vivo results are consistent with the ability of melatonin to reduce gross liver pathophysiology resulting from cholestasis due to obstruction of the bile duct [228,229].
5. Concluding Remarks
In recent years, investigations related to melatonin’s actions in cells have become progressively more focused to the mitochondria without, however, precluding functions in other subcellular compartments. Since melatonin is a powerful inhibitor of oxidative stress, its actions at the level of the mitochondria may not only be fortuitous, but necessary considering its highly protective actions. Mitochondria, more than any other organelle, spawns ROS/free radicals even under so-called “resting” conditions, but especially under taxing circumstances. It is essential that potentially-damaging ROS be quelled at their source to ensure the molecular damage they mete out can be averted.
More than a decade ago, it was immunocytochemically shown that melatonin quenched the fluorescent-signal associated with ROS generation in the mitochondria [167]. Roughly a decade later, melatonin was shown to be in exceptionally high concentrations in mitochondria, more so than in any other cellular compartment [177]. Among several interesting features of the Venegas et al. [177] report was that the mitochondria, in which the very high levels of melatonin were measured, were obtained from brain tissue, rather than being of pineal gland origin. After consideration of the preceding data, we speculated that melatonin is likely produced in the mitochondria of all cells, animals, and plants [171]. This hypothesis relies heavily on what is referred to as the Endosymbiotic Theory (Figure 5) for the origin of mitochondria in eukaryote cells. Since bacteria contain melatonin, presumably a result of its synthesis in these prokaryotes [174], and mitochondria derived from bacteria that were initially phagocytized as food by early eukaryotes, we surmised that the melatonin-synthesizing machinery of bacteria was retained by the evolved mitochondria. This idea stimulated investigations that have led to compelling evidence that mitochondria of every cell fabricates melatonin for its own use [145,182]; this explains the very wide distribution of melatonin in multicellular organisms [230,231]. That mitochondria produce melatonin has only been shown in a small number of cells, i.e., brain and oocyte. Whether this is a universal feature of mitochondria awaits investigation.
The original studies by Jou et al. [167,168] also suggested that, in addition to manufacturing melatonin, it is rapidly taken up by cells from the extracellular environment. This entry was thought to be related to simple diffusion of melatonin, which is highly lipophilic, through the plasma and mitochondrial membranes. While this possibility is still viable, melatonin has been shown to enter cells via the GLUT1 transporter [178] and by means of the PEPT1/2 oligopeptide transporters [180]. The latter proteins also exist in mitochondrial membranes where they presumably aid in the rapid uptake of melatonin against a gradient. It is anticipated that data related to the uptake and synthesis of melatonin by mitochondria will grow rapidly in the next five years.
Like melatonin, sirtuins are both ubiquitously distributed and likely acquired by eukaryotes after the engulfment of α-proteobacteria [232]. As with melatonin, the sirtuins are therefore very ancient. The fact that both melatonin and sirtuins co-existed in cells for eons, it could be expected that they would have “learned” to collaborate. The data summarized above clearly shows that SIRT3 is required for melatonin to neutralize oxidative stress at the mitochondrial level, at least in the conditions under which it was investigated. These findings, although not numerous, were comprehensively reviewed within the last year [1,28]. The fact that melatonin promotes the deacetylation of mitochondrial SIRT3 and FOXO3a, which results in the stimulation of the antioxidant enzyme, SOD2, leaves unexplained the importance of the direct free radical scavenging component of melatonin in protecting this organelle and the cell as a whole from free radical damage; this issue requires resolution.
SIRT3 has multiple functions in mitochondria. It impacts the respiratory chain complexes and elevates ATP production, influences enzymes of the citric acid cycle, holds sway over amino acid metabolism and controls fatty acid oxidation. Additionally, SIRT3 affects mitochondrial dynamics [233,234,235,236,237]. Melatonin shares many of these same actions [231,238,239,240,241,242,243]. Whether melatonin’s effects on mitophagy, mitochondrial bioenergetics, fusion or fission are a consequence of its epigenetic actions may be a fruitful area of investigation.
Considering the multiple overlapping functions and their very long-standing cohabitation in mitochondria, it seems likely that SIRT3 and melatonin have interactions beyond regulating SOD2 activity. It is our prediction that they cooperate in the regulation of a variety of mitochondrial functions. We also expect these interactions will be clarified in the near future.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Mayo J.C., Sainz R.M., Gonzalez-Menendez P., Cepas V., Tan D.X., Reiter R.J. Melatonin and sirtuins: A “not-so unexpected” relationship. J. Pineal Res. 2017;62:e12391. doi: 10.1111/jpi.12391. [DOI] [PubMed] [Google Scholar]
- 2.Otto G.M., Brar G.A. Seq-ing answers: Uncovering the unexpected in global gene regulation. Curr. Genet. 2018 doi: 10.1007/s00294-018-0839-3. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaubai A., Pile L.A. Same agent, different messages: Insight into transcriptional regulation by SIN3 isoforms. Epigenet. Chromatin. 2018;11:17. doi: 10.1186/s13072-018-0188-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Godini R., Lafta H.Y., Fallahi H. Epigenetics modifications in the embryonic and induced pluripotent stem cells. Gene Expr. Patterns. 2018;29:1–9. doi: 10.1016/j.gep.2018.04.001. [DOI] [PubMed] [Google Scholar]
- 5.Korkmaz A., Rosales-Corral S., Tan D.X., Reiter R.J. Gene regulation by melatonin linked to epigenetic phenomena. Gene. 2012;503:1–11. doi: 10.1016/j.gene.2012.04.040. [DOI] [PubMed] [Google Scholar]
- 6.Feinberg A.P. The key role of epigenetics in human disease prevention and mitigation. N. Engl. J. Med. 2018;378:1323–1334. doi: 10.1056/NEJMra1402513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nadal S., Raj R., Mohammed S., Davis B.G. Synthetic post-translational modification of histones. Curr. Opin. Chem. Biol. 2018;45:35–47. doi: 10.1016/j.cbpa.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 8.Klar A.J., Fogel S., MacLeod K. MAR1-a regulator of the HMa and HMalpha loci in Saccharomyces cerevisiae. Genetics. 1979;93:37–50. doi: 10.1093/genetics/93.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klar A.J., Kakar S.N., Ivy J.M., Hicks J.B., Livi G.P., Miglio L.M. SUM1, an apparent positive regulator of the cryptic mating-type in Saccharomyces cerevisiae. Genetics. 1985;111:745–758. doi: 10.1093/genetics/111.4.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rine J., Herskowitz I. Four genes responsible for a position effect on expression from HML and HMR in Saccharomyces cerevisiae. Genetics. 1987;116:9–22. doi: 10.1093/genetics/116.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rusche L.N., Kirchmaier A.L., Rine J. Ordered nucleation and spreading of silenced chromatin in Saccharomyces cerevisiae. Mol. Biol. Cell. 2002;13:2007–2022. doi: 10.1091/mbc.e02-03-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morris B.J. Seven sirtuins for seven deadly diseases of aging. Free Radic. Biol. Med. 2013;56:133–171. doi: 10.1016/j.freeradbiomed.2012.10.525. [DOI] [PubMed] [Google Scholar]
- 13.Ajami M., Pazoki-Toroudi H., Amani H., Nabavi S.F., Braidy N., Vacca R.A., Atanasov A.G., Mocan A., Nabavi S.M. Therapeutic role of sirtuins in neurodegeneration disease and their modulation by polyphenols. Neurosci. Biobehav. Rev. 2017;73:39–47. doi: 10.1016/j.neubiorev.2016.11.022. [DOI] [PubMed] [Google Scholar]
- 14.Dang W. The controversial world of sirtuins. Drug Discov. Today Technol. 2014;12:e9–e17. doi: 10.1016/j.ddtec.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Watroba M., Dudek I., Skoda M., Stangret A., Rzodkiewicz P., Szurkiewicz D. Sirtuins, epigenetics and longevity. Ageing Res. Rev. 2017;40:11–19. doi: 10.1016/j.arr.2017.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Jung-Hynes B., Reiter R.J., Ahmad N. Sirtuins, melatonin, and circadian rhythms: Building a bridge between aging and cancer. J. Pineal Res. 2010;48:9–19. doi: 10.1111/j.1600-079X.2009.00729.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ong A.L.C., Ramasamy T.S. Role of Sirtuin1-p53 regulatory axis in aging, cancer and cellular reprogramming. Ageing Res. Rev. 2018;43:64–80. doi: 10.1016/j.arr.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Jung-Hynes B., Ahmad N. SIRT1 controls circadian clock circuitry and promotes cell survival: A connection with age-related neoplasms. FASEB J. 2009;23:2803–2809. doi: 10.1096/fj.09-129148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masri S. Sirtuin-dependent clock control: New advances in metabolism, aging and cancer. Curr. Opin. Clin. Nutr. Metab. Care. 2015;18:521–527. doi: 10.1097/MCO.0000000000000219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao Y., Wang R.H. Associations among metabolism, circadian rhythms and age-associated diseases. Aging Dis. 2017;8:314–333. doi: 10.14336/AD.2016.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Carrico C., Meyer J.G., He W., Gibson B.W., Verdin E. The mitochondrial acylome emerges: Proteomics, regulation of sirtuins and metabolic and disease implications. Cell Metab. 2018;27:497–512. doi: 10.1016/j.cmet.2018.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gertz M., Steegborn C. Function and regulation of the mitochondrial sirtuin isoform Sirt5 in mammalia. Biochim. Biophys. Acta. 2010;1804:1658–1665. doi: 10.1016/j.bbapap.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 23.Lin S., Xing H., Zang T., Ruan X., Wo L., He M. Sirtuins in mitochondrial stress: Indispensable helpers behind the scenes. Ageing Res. Rev. 2018;44:22–32. doi: 10.1016/j.arr.2018.03.006. [DOI] [PubMed] [Google Scholar]
- 24.Lombard D.B., Alt F.W., Cheng H.L., Bunkenborg J., Streeper R.S., Mostoslovsky R., Kim J., Yancopoulos G., Valenzuela D., Murphy A., et al. Mammalian Sir2 homolog SIRT3 regulates global mitochondrial lysine acetylation. Mol. Cell. Biol. 2007;27:8807–8814. doi: 10.1128/MCB.01636-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Noqueiras R., Habegger K.M., Chaudhary M., Finan B., Banks A.S., Dietrich M.O., Horvath T.L., Sinclair D.A., Pfluger P.T., Tschop M.H. Sirtuin 1 and sirtuin 3: Physiological modulators of metabolism. Physiol. Rev. 2012;92:1479–1514. doi: 10.1152/physrev.00022.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ong S.G., Hausenloy D.J. Hypoxia-inducible factor as a therapeutic target for cardioprotection. Pharmacol. Ther. 2012;136:69–81. doi: 10.1016/j.pharmthera.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 27.Reiter R.J., Tan D.X., Galano A. Melatonin: Exceeding expectations. Physiology. 2014;29:325–333. doi: 10.1152/physiol.00011.2014. [DOI] [PubMed] [Google Scholar]
- 28.Reiter R.J., Rosales-Corral S., Tan D.X., Jou M.J., Galano A., Xu B. Melatonin as a mitochondria-targeted antioxidant: One of evolution’s best ideas. Cell. Mol. Life Sci. 2017;74:3863–3881. doi: 10.1007/s00018-017-2609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reiter R.J., Tan D.X., Rosales-Corral S., Galano A., Zhou X.J., Xu B. Mitochondria: Central organelles for melatonin’s antioxidant and anti-aging actions. Molecules. 2018;23:509. doi: 10.3390/molecules23020509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tan D.X., Manchester L.C., Qin L., Reiter R.J. Melatonin: A mitochondrial-targeting molecule involving mitochondrial proteins and energetics. Int. J. Mol. Sci. 2016;17:2124. doi: 10.3390/ijms17122124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haigis M.C., Mostoslavky R., Haigis K.M., Fahie K., Christodoulou D.C., Murphy A.J., Valenzuela D.M., Yancopoulos G.D., Karow M., Blander G., et al. SIRT4 inhibits glutamate dehydrogenase and opposes the effects of caloric restriction in pancreatic beta cells. Cell. 2006;126:941–954. doi: 10.1016/j.cell.2006.06.057. [DOI] [PubMed] [Google Scholar]
- 32.Huang J.Y., Hirschey M.D., Shimazu T., Ho L., Verdin E. Mitochondrial sirtuins. Biochim. Biophys. Acta. 2010;1804:1645–1651. doi: 10.1016/j.bbapap.2009.12.021. [DOI] [PubMed] [Google Scholar]
- 33.Hallows W.C., Yu W., Smith B.C., Devries M.K., Ellinger J.J., Someya S., Shortreed M.R., Prolla T., Markley J.L., Smith L.M., et al. Sirt3 promotes the urea cycle and fatty acid oxidation during dietary restriction. Mol. Cell. 2011;41:139–149. doi: 10.1016/j.molcel.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tan D.X., Chen L.D., Poeggeler B., Manchester L.C., Reiter R.J. Melatonin: A potent hydroxyl radical scavenger. Endocr. J. 1993;1:57–60. [Google Scholar]
- 35.Tan D.X., Poeggeler B., Reiter R.J., Chen L.D., Chen S., Manchester L.C., Barlow-Walden L.R. The pineal hormone melatonin inhibits DNA-adduct formation induced by the chemical carcinogen safrole in vivo. Neurosci. Lett. 1993;157:131–134. doi: 10.1016/0304-3835(93)90076-L. [DOI] [PubMed] [Google Scholar]
- 36.Trush M.A., Kensler T.W. An overview of the relationship between oxidative stress and chemical carcinogenesis. Free Radic. Biol. Med. 1991;10:201–209. doi: 10.1016/0891-5849(91)90077-G. [DOI] [PubMed] [Google Scholar]
- 37.Harman D. The free radical theory of aging. Antioxid. Redox Signal. 2003;5:557–561. doi: 10.1089/152308603770310202. [DOI] [PubMed] [Google Scholar]
- 38.Finkelstein E., Rosen G.M., Rauckmann E.J. Spin trapping of superoxide and hydroxyl radical: Practical aspects. J. Am. Chem. Soc. 1980;102:4994–4999. doi: 10.1021/ja00535a029. [DOI] [PubMed] [Google Scholar]
- 39.Floyd R.A. Role of oxygen free radicals in carcinogenesis and brain ischemia. FASEB J. 1990;4:2587–2597. doi: 10.1096/fasebj.4.9.2189775. [DOI] [PubMed] [Google Scholar]
- 40.Dubocovich M.L. Pharmacology and function of melatonin receptors. FASEB J. 1988;2:2765–2773. doi: 10.1096/fasebj.2.12.2842214. [DOI] [PubMed] [Google Scholar]
- 41.Stankov B., Reiter R.J. Melatonin receptors: Current status, facts, and hypotheses. Life Sci. 1990;46:971–982. doi: 10.1016/0024-3205(90)90020-R. [DOI] [PubMed] [Google Scholar]
- 42.Poeggeler B., Saarela S., Reiter R.J., Tan D.X., Chen L.D., Manchester L.C., Barlow-Walden L.R. Melatonin—A highly potent endogenous radical scavenger and electron donor: New aspects of the oxidation chemistry of this indole assessed in vitro. Ann. N. Y. Acad. Sci. 1994;738:419–420. doi: 10.1111/j.1749-6632.1994.tb21831.x. [DOI] [PubMed] [Google Scholar]
- 43.Abe R., Reiter R.J., Orhii P.B., Hara M., Poeggeler B. Inhibitory effect of melatonin on cataract formation in newborn rats: Evidence for an antioxidative role for melatonin. J. Pineal Res. 1994;17:94–100. doi: 10.1111/j.1600-079X.1994.tb00119.x. [DOI] [PubMed] [Google Scholar]
- 44.Vijayalaxmi, Reiter R.J., Meltz M.L. Melatonin protects human blood lymphocytes from radiation-induced chromosome damage. Mutat. Res. 1995;346:23–31. doi: 10.1016/0165-7992(95)90065-9. [DOI] [PubMed] [Google Scholar]
- 45.Melchiorri D., Reiter R.J., Attia A.M., Hara M., Burgos A., Nistico G. Potent protective effect of melatonin on in vivo paraquat-induced oxidative damage in rats. Life Sci. 1995;56:83–89. doi: 10.1016/0024-3205(94)00417-Q. [DOI] [PubMed] [Google Scholar]
- 46.Sewerynek E., Abe M., Reiter R.J., Barlow-Walden L.R., Chen L.D., McCabe T.J., Roman L.J., Diaz-Lopez B. Melatonin administration prevents lipopolysaccharide-induced oxidative damage in phenobarbital-treated rats. J. Cell. Biochem. 1995;58:436–444. doi: 10.1002/jcb.240580406. [DOI] [PubMed] [Google Scholar]
- 47.Sewerynek E., Melchiorri D., Chen L.D., Reiter R.J. Melatonin reduces both basal and bacterial lipopolysaccharide-induced lipid peroxidation in vitro. Free Radic. Biol. Med. 1995;19:903–909. doi: 10.1016/0891-5849(95)00101-3. [DOI] [PubMed] [Google Scholar]
- 48.Melchiorri D., Reiter R.J., Sewerynek E., Chen L.D., Nistico G. Melatonin reduces kainate-induced lipid peroxidation in homogenates of different brain regions. FASEB J. 1995;9:1205–1210. doi: 10.1096/fasebj.9.12.7672513. [DOI] [PubMed] [Google Scholar]
- 49.Sewerynek E., Reiter R.J., Melchiorri D., Ortiz G.G., Lewinski A. Oxidative damage in the liver induced by ischemia-reperfusion: Protection by melatonin. Hepato-Gastroenterology. 1996;43:898–905. [PubMed] [Google Scholar]
- 50.Pieri C., Marra M., Moroni F., Recchioni R., Marcheselli F. Melatonin: A peroxyl radical scavenger more effective than vitamin E. Life Sci. 1994;55:271–276. doi: 10.1016/0024-3205(94)00666-0. [DOI] [PubMed] [Google Scholar]
- 51.Pieri C., Moroni F., Marra M., Marcheselli F., Recchioni R. Melatonin is an efficient antioxidant. Arch. Gerontol. Geriatr. 1995;20:159–165. doi: 10.1016/0167-4943(94)00593-V. [DOI] [PubMed] [Google Scholar]
- 52.Scaiano J.C. Exploratory laser flash photolysis study of the free radical reactions and magnetic field effects in melatonin chemistry. J. Pineal Res. 1995;19:189–195. doi: 10.1111/j.1600-079X.1995.tb00188.x. [DOI] [PubMed] [Google Scholar]
- 53.Matuszak Z., Reszka K.J., Chignell C.F. Reaction of melatonin and related indoles with hydroxyl radicals: EPR and spin trapping investigation. Free Radic. Biol. Med. 1997;23:367–372. doi: 10.1016/S0891-5849(96)00614-4. [DOI] [PubMed] [Google Scholar]
- 54.Stasica P., Ulanski P., Rosiak J.M. Melatonin as a hydroxyl radical scavenger. J. Pineal Res. 1998;25:65–66. doi: 10.1111/j.1600-079X.1998.tb00387.x. [DOI] [PubMed] [Google Scholar]
- 55.Stasica P., Paneth P., Rosiak J.M. Hydroxyl radical reaction with melatonin molecule: A computational study. J. Pineal Res. 2000;29:125–127. doi: 10.1034/j.1600-079X.2000.290209.x. [DOI] [PubMed] [Google Scholar]
- 56.Stasica P., Ulanski P., Roriak J.M. Reactions of melatonin with radicals in deoxygenated aqueous solutions. J. Radioanal. Nucl. Chem. 1998;232:107–113. doi: 10.1007/BF02383723. [DOI] [Google Scholar]
- 57.Livrea M.A., Tesoriere L., D’Arpa D., Morreale M. Reaction of melatonin with lipoperoxyl radicals in phospholipid bilayers. Free Radic. Biol. Med. 1997;23:706–711. doi: 10.1016/S0891-5849(97)00018-X. [DOI] [PubMed] [Google Scholar]
- 58.Zang L.Y., Cosma G., Gardner H., Vallyathan V. Scavenging of reactive oxygen species by melatonin. Biochim. Biophys. Acta. 1998;1425:469–477. doi: 10.1016/S0304-4165(98)00099-3. [DOI] [PubMed] [Google Scholar]
- 59.Turjanski A.G., Rosenstein R.E., Estrin D.A. Reactions of melatonin and related indoles with free radicals: A computational study. J. Med. Chem. 1998;41:3684–3689. doi: 10.1021/jm980117m. [DOI] [PubMed] [Google Scholar]
- 60.Brömme H.J., Mörke W., Peschke E., Ebelt H., Peschke D. Scavenging effect of melatonin on hydroxyl radicals generated by alloxan. J. Pineal Res. 2000;29:201–209. doi: 10.1034/j.1600-0633.2002.290402.x. [DOI] [PubMed] [Google Scholar]
- 61.Zavodnik I.B., Domanski A.V., Lapshina E.A., Bryszewska M., Reiter R.J. Melatonin directly scavenges free radicals generated in red blood cells and a cell-free system: Chemiluminescence measurements and theoretical calculations. Life Sci. 2006;79:391–400. doi: 10.1016/j.lfs.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 62.Brömme H.J., Ebelt H., Peschke D., Peschke E. Alloxan acts as a prooxiant only under reducing conditions: Influence of melatonin. Cell. Mol. Life Sci. 1999;55:487–493. doi: 10.1007/s000180050305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mahal H.S., Sharma H.S., Mukherjie T. Antioxidant properties of melatonin: A pulse radiolysis study. Free Radic. Biol. Med. 1999;26:557–565. doi: 10.1016/S0891-5849(98)00226-3. [DOI] [PubMed] [Google Scholar]
- 64.Valko M., Leibfritz D., Moncol J., Cronin M.T.D., Mazur M., Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int. J. Biochem. Cell Biol. 2007;39:44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 65.Galano A. On the direct scavenging activity of melatonin towards hydroxyl and a series of peroxyl radicals. Phys. Chem. Chem. Phys. 2011;13:7178–7188. doi: 10.1039/c0cp02801k. [DOI] [PubMed] [Google Scholar]
- 66.Galano A., Tan D.X., Reiter R.J. Melatonin and related compounds: Chemical insights into their protective effects against oxidative stress. Curr. Org. Chem. 2017;21:2077–2095. doi: 10.2174/1385272820666161024124058. [DOI] [Google Scholar]
- 67.Galano A., Tan D.X., Reiter R.J. Melatonin as a natural ally against oxidative stress: A physicochemical examination. J. Pineal Res. 2011;51:1–16. doi: 10.1111/j.1600-079X.2011.00916.x. [DOI] [PubMed] [Google Scholar]
- 68.Pshenichnyuk S.A., Modelli A., Jones D., Lazneva E.F., Komolov A.S. Low-energy electron interaction with melatonin and related compounds. J. Phys. Chem. B. 2017;121:3965–3974. doi: 10.1021/acs.jpcb.7b01408. [DOI] [PubMed] [Google Scholar]
- 69.Daniels W.M.O., Reiter R.J., Melchiorri D., Seweryneck E., Pablos M.I., Ortiz G.G. Melatonin counteracts lipid peroxidation induced by carbon tetrachloride but does not restore glucose-6 phosphatase activity. J. Pineal Res. 1995;19:1–6. doi: 10.1111/j.1600-079X.1995.tb00164.x. [DOI] [PubMed] [Google Scholar]
- 70.Pablos M.I., Reiter R.J., Chuang J.I., Ortiz G.G., Guerrero J.M., Sewerynek E., Agapito M.T., Melchiorri D., Lawrence R., Deneke S.M. Acutely administered melatonin reduces oxidative damage in lung and brain induced by hyperbaric oxygen. J. Appl. Physiol. 1997;83:354–358. doi: 10.1152/jappl.1997.83.2.354. [DOI] [PubMed] [Google Scholar]
- 71.Kim S.J., Reiter R.J., Rouvier-Garay M.V., El-Sokkary G.H., Tan D.X. 2-Nitropropane-induced lipid peroxidation and DNA damage: Antitoxic effects of melatonin. Toxicology. 1998;19:117–123. doi: 10.1016/s0300-483x(98)00111-5. [DOI] [PubMed] [Google Scholar]
- 72.Qi W., Tan D.X., Reiter R.J., Kim S.J., Manchester L.C., Cabrera J., Sainz R.M., Mayo J.C. Melatonin reduces lipid peroxidation and tissue edema in cerulein-induced acute pancreatitis in rats. Dig. Dis. Sci. 1999;44:2257–2262. doi: 10.1023/A:1026656720868. [DOI] [PubMed] [Google Scholar]
- 73.Cabrera J., Reiter R.J., Tan D.X., Qi W., Sainz R.M., Mayo J.C., Garcia J.J., Kim S.J., El-Sokkary G. Melatonin reduces oxidative neurotoxicity due to quinolinic acid: In vitro and in vivo findings. Neuropharmacology. 2000;39:507–514. doi: 10.1016/S0028-3908(99)00128-8. [DOI] [PubMed] [Google Scholar]
- 74.Karbownik M., Tan D.X., Reiter R.J. Melatonin reduces the oxidation of nuclear DNA and membrane lipids induced by the carcinogen delta-aminolevulinic acid. Int. J. Cancer. 2000;88:7–11. doi: 10.1002/1097-0215(20001001)88:1<7::AID-IJC2>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 75.Fulia F., Gitto E., Cuzzocrea S., Reiter R.J., Dugo L., Gitto P., Barberi S., Cordaro S., Barberi I. Increased levels of malondialdehyde and nitrite/nitrate in blood of asphyxiated newborns: Reduction by melatonin. J. Pineal Res. 2001;31:343–349. doi: 10.1034/j.1600-079X.2001.310409.x. [DOI] [PubMed] [Google Scholar]
- 76.Meki A.R., Hussein A.A. Melatonin reduces oxidative stress induced by ochratoxin A in rat liver and kidney. Comp. Biochem. Physiol. C Toxicol. Pharmacol. 2001;130:305–313. doi: 10.1016/S1532-0456(01)00248-4. [DOI] [PubMed] [Google Scholar]
- 77.Fischer T.W., Scholz G., Knoll B., Hipler U.C., Elsner P. Melatonin suppresses reactive oxygen species induced by UV irradiation in leukocytes. J. Pineal Res. 2004;37:107–112. doi: 10.1111/j.1600-079X.2004.00142.x. [DOI] [PubMed] [Google Scholar]
- 78.Gitto E., Reiter R.J., Amodio A., Romeo C., Cuzzocrea E., Sabatino G., Buonocore G., Cordaro V., Trimarchi G., Barberi I. Early indicators of chronic lung disease in preterm infants with respiratory distress syndrome and their inhibition by melatonin. J. Pineal Res. 2004;30:250–255. doi: 10.1111/j.1600-079X.2004.00124.x. [DOI] [PubMed] [Google Scholar]
- 79.Thomas B., Mohanakumar K.P. Melatonin protects against oxidative stress caused by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine in the mouse nigrostriatum. J. Pineal Res. 2004;36:25–32. doi: 10.1046/j.1600-079X.2003.00096.x. [DOI] [PubMed] [Google Scholar]
- 80.Vairetti M., Ferrigno A., Bertone R., Rizzo V., Richelmi P., Berte F., Reiter R.J., Freitas I. Exogenous melatonin enhances bile flow and ATP levels after cold storage and reperfusion in rat liver: Implications for liver transplantation. J. Pineal Res. 2005;38:223–230. doi: 10.1111/j.1600-079X.2004.00193.x. [DOI] [PubMed] [Google Scholar]
- 81.Zhang L., Wei W., Xu J., Min F., Wang X., Cao S., Tan D.X., Qi W., Reiter R.J. Inhibitory effect of melatonin on diquat-induced lipid peroxidation in vivo assessed by the measurement of F2-isoprostanes. J. Pineal Res. 2008;40:326–331. doi: 10.1111/j.1600-079X.2005.00311.x. [DOI] [PubMed] [Google Scholar]
- 82.Ozacmak V.H., Barut F., Ozacmak H.S. Melatonin provides neuroprotection by reducing oxidative stress and HSP70 expression during chronic cerebral hypoperfusion in ovariectomized rats. J. Pineal Res. 2009;47:156–163. doi: 10.1111/j.1600-079X.2009.00695.x. [DOI] [PubMed] [Google Scholar]
- 83.Konturek P.C., Konturek S.J., Celinski K., Slomka M., Cichoz-Lach H., Bielanski W., Reiter R.J. Role of melatonin on mucosal gastroprotection against aspirin-induced gastric lesions in humans. J. Pineal Res. 2010;48:318–323. doi: 10.1111/j.1600-079X.2010.00755.x. [DOI] [PubMed] [Google Scholar]
- 84.Laothong U., Pinlaor P., Hiraku Y., Boonsiri P., Prakobwong S., Khoontawad J., Pinlaor S. Protective effects of melatonin against Opisthorchis viverrini-induced oxidative and nitrosative damage and liver injury in hamsters. J. Pineal Res. 2010;49:271–282. doi: 10.1111/j.1600-079X.2010.00792.x. [DOI] [PubMed] [Google Scholar]
- 85.Nopparat C., Porter J.E., Ebadi M., Govitrapong P. The mechanisms for the neuroprotective effect of melatonin against methamphetamine-induced autophagy. J. Pineal Res. 2010;49:382–389. doi: 10.1111/j.1600-079X.2010.00805.x. [DOI] [PubMed] [Google Scholar]
- 86.Govender J., Loos B., Marais E., Engelbrecht A.M. Mitochondrial catastrophe during doxorubicin-induced cardiotoxicity: A review of the protective role of melatonin. J. Pineal Res. 2014;57:367–380. doi: 10.1111/jpi.12176. [DOI] [PubMed] [Google Scholar]
- 87.Abdel Moneim A.E., Ortiz F., Leonardo-Mendonca R.C., Vergano-Villodres R., Guerrero-Martinez D.A., Lopez L.C., Acuna-Castroviejo D., Escames G. Protective effects of melatonin against oxidative damage induced by Egyptian cobra (Naja haje) venom in rats. Acta Trop. 2015;143:58–65. doi: 10.1016/j.actatropica.2014.12.007. [DOI] [PubMed] [Google Scholar]
- 88.Borges-Lda S., Dermargos A., da Silva Junior E.P., Weimann E., Lambertucci R.H., Hatanaks E. Melatonin decreases muscular oxidative stress and inflammation induced by strenuous exercise and stimulates growth factor synthesis. J. Pineal Res. 2015;58:166–172. doi: 10.1111/jpi.12202. [DOI] [PubMed] [Google Scholar]
- 89.Ortiz F., Acuna-Castroviejo D., Doerrier C., Dayoub J.C., Lopez L.C., Venegas C., Garcia J.A., Lopez A., Volt H., Luna-Sanchez M., et al. Melatonin blunts the mitochondrial/NLRP3 connection and protects against radiation-induced mucositis. J. Pineal Res. 2015;58:34–49. doi: 10.1111/jpi.12191. [DOI] [PubMed] [Google Scholar]
- 90.Dwaich K.H., Al-Amran F.G., Al-Sheibani B.I., Al-Aubaidy H.A. Melatonin effects on myocardial ischemia-reperfusion injury: Impact on the outcome in patients undergoing coronary artery bypass grafting surgery. Int. J. Cardiol. 2016;221:977–986. doi: 10.1016/j.ijcard.2016.07.108. [DOI] [PubMed] [Google Scholar]
- 91.Xu S., Pi H., Zhang L., Zhang N., Li Y., Zhang H., Tang J., Li H., Feng M., Deng P., et al. Melatonin prevents abnormal mitochondrial dynamics resulting from the neurotoxicity of cadmium by blocking calcium-dependent translocation of Drp1 to the mitochondria. J. Pineal Res. 2016;60:291–302. doi: 10.1111/jpi.12310. [DOI] [PubMed] [Google Scholar]
- 92.Asghari M.H., Abdollahi M., de Oliveira M.R., Nabavi S.M. A review of the protective role of melatonin during phosphine-induced cardiotoxicity: Focus on mitochondrial dysfunction, oxidative stress and apoptosis. J. Pharm. Pharmacol. 2017;69:236–243. doi: 10.1111/jphp.12682. [DOI] [PubMed] [Google Scholar]
- 93.D’Angelo G., Marseglia L., Reiter R.J., Buonocore G., Gitto E. Melatonin and neonatal sepsis: A promising antioxidant adjuvant agent. Am. J. Perinatol. 2017;34:1382–1388. doi: 10.1055/s-0037-1604244. [DOI] [PubMed] [Google Scholar]
- 94.Dominguez-Rodriguez A., Abreu-Gonzalez P., de la Torre-Hernandez J.M., Consuegra-Sanchez L., Piccolo R., Gonzalez-Gonzalez J., Garcia-Camarero T., Del Mar Garcia-Sainz M., Aldea-Perona A., Reiter R.J., et al. Usefulness of early treatment with melatonin to reduce infarct size in patients with ST-segment elevation myocardial infarction receiving percutaneous coronary intervention (from the melatonin adjunct in the acute myocardial infarction treated with angioplasty trial) Am. J. Cardiol. 2017;120:522–526. doi: 10.1016/j.amjcard.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 95.Feng D., Wang B., Wang L., Abraham N., Tao K., Huang L., Shi W., Dong Y., Qu Y. Pre-ischemia melatonin treatment alleviated acute neuronal injury after ischemic stroke by inhibiting endoplasmic reticulum stress-dependent autophagy via PERK and IRE1 signaling. J. Pineal Res. 2017;62:e12395. doi: 10.1111/jpi.12395. [DOI] [PubMed] [Google Scholar]
- 96.Yun S.P., Han Y.S., Lee J.H., Kim S.M., Lee S.H. Melatonin rescues mesenchymal stem cells from senescence induced by the uremic toxin p-cresol via inhibiting mTOR-dependent autophagy. Biomol. Ther. (Seoul) 2018;26:389–398. doi: 10.4062/biomolther.2017.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhang Y., Wei Z., Liu W., Wang J., He X., Huang H., Zhang J., Yang Z. Melatonin protects against arsenic trioxide-induced liver injury by the upregulation of Nrf2 expression through the activation of Pl3K/AKT pathway. Oncotarget. 2017;8:3773–3780. doi: 10.18632/oncotarget.13931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Espino J., Rodriguez A.B., Pariente J.A. Melatonin and oxidative stress in the diabetic state: Clinical implications and potential therapeutic applications. Curr. Med. Chem. 2018 doi: 10.2174/0929867325666180410094149. in press. [DOI] [PubMed] [Google Scholar]
- 99.Lv Y., Zhang P., Guo J., Zhu Z., Li X., Xu D., Zeng W. Melatonin protects mouse spermatogonial stem cells against hexavalent chromium-induced apoptosis and epigenetic histone modifications. Toxicol. Appl. Pharmacol. 2018;340:30–38. doi: 10.1016/j.taap.2017.12.017. [DOI] [PubMed] [Google Scholar]
- 100.Wang M.L., Wei C.H., Wang W.D., Wang J.S., Zhang J., Wang J.J. Melatonin attenuates lung ischemia-reperfusion injury via inhibition of oxidative stress and inflammation. Interact. Cardiovasc. Thorac. Surg. 2018;26:761–767. doi: 10.1093/icvts/ivx440. [DOI] [PubMed] [Google Scholar]
- 101.Poeggeler B., Reiter R.J., Hardeland R., Tan D.X., Barlow-Walden L.R. Melatonin and structurally-related, endogenous indoles act as potent electron donors and radical scavengers in vitro. Redox Rep. 1996;2:179–181. doi: 10.1080/13510002.1996.11747046. [DOI] [PubMed] [Google Scholar]
- 102.Alvarez-Diduk R., Galano A., Tan D.X., Reiter R.J. The key role of the sequential proton loss electron transfer mechanism on the free radical scavenging activity of some melatonin-related compounds. Theor. Chem. Acc. 2016;139:1–5. doi: 10.1007/s00214-015-1785-5. [DOI] [Google Scholar]
- 103.Galano A., Tan D.X., Reiter R.J. Melatonin: A versatile protector against oxidative DNA damage. Molecule. 2018;23:530. doi: 10.3390/molecules23030530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Abuja P.M., Leibmann P., Hayn M., Schauenstein K., Esterbauer H. Antioxidant role of melatonin in lipid peroxidation of human LDL. FEBS Lett. 1997;413:289–293. doi: 10.1016/S0014-5793(97)00918-6. [DOI] [PubMed] [Google Scholar]
- 105.Antunes F., Barclay L.R., Ingold K.U., King M., Norris J.Q., Scaiano J.C., Xi F. On the antioxidant activity of melatonin. Free Radic. Biol. Med. 1999;26:117–128. doi: 10.1016/S0891-5849(98)00168-3. [DOI] [PubMed] [Google Scholar]
- 106.Marshall K.C., Reiter R.J., Poeggeler B., Aruoma O.I., Halliwell B. Evaluation of the antioxidant activity of melatonin in vitro. Free Radic. Biol. Med. 1996;21:307–315. doi: 10.1016/0891-5849(96)00046-9. [DOI] [PubMed] [Google Scholar]
- 107.Tan D.X., Manchester L.C., Terron M.P., Flores L.J., Reiter R.J. One molecule, many derivatives: A never-ending interaction of melatonin with reactive oxygen and nitrogen species? J. Pineal Res. 2007;42:28–42. doi: 10.1111/j.1600-079X.2006.00407.x. [DOI] [PubMed] [Google Scholar]
- 108.Hardeland R., Tan D.X., Reiter R.J. Kynuramines, metabolites of melatonin and other indoles: The resurrection of an almost forgotten class of biogenic amines. J. Pineal Res. 2009;47:109–126. doi: 10.1111/j.1600-079X.2009.00701.x. [DOI] [PubMed] [Google Scholar]
- 109.Hardeland R., Reiter R.J., Poeggeler B., Tan D.X. The significance of the metabolism of the neurohormone melatonin: Antioxidative protection and formation of bioactive substances. Neurosci. Biobehav. Rev. 1993;17:347–357. doi: 10.1016/S0149-7634(05)80016-8. [DOI] [PubMed] [Google Scholar]
- 110.Tsia P.L., Hu M.K. Free radical scavenging and antioxidative activity of melatonin derivatives. J. Pharm. Pharmacol. 2003;55:1655–1660. doi: 10.1211/0022357022250. [DOI] [PubMed] [Google Scholar]
- 111.Tan D.X., Manchester L.C., Burkhardt S., Sainz R.M., Mayo J.C., Kohen R., Shohami E., Huo Y.S., Hardeland R., Reiter R.J. N1-acetyl-N2-formyl-5-methoxykynuramine, a biogenic amine and melatonin metabolite, functions as a potent antioxidant. FASEB J. 2001;15:2294–2296. doi: 10.1096/fj.01-0309fje. [DOI] [PubMed] [Google Scholar]
- 112.Tan D.X., Manchester L.C., Reiter R.J., Plummer R.F., Limson J., Weintraub S.T., Qi W. Melatonin directly scavenges hydrogen peroxide: A potentially new metabolic pathway of melatonin biotransformation. Free Radic. Biol. Med. 2000;29:1177–1185. doi: 10.1016/S0891-5849(00)00435-4. [DOI] [PubMed] [Google Scholar]
- 113.Galano A., Tan D.X., Reiter R.J. On the free radical scavenging activities of melatonin’s metabolites, AFMK and AMK. J. Pineal Res. 2013;54:245–257. doi: 10.1111/jpi.12010. [DOI] [PubMed] [Google Scholar]
- 114.Limson J., Nyokong T., Daya S. The interaction of melatonin and its precursors with aluminum, cadmium, copper, iron, lead, and zinc: An absorptive voltammetric study. J. Pineal Res. 1998;24:15–21. doi: 10.1111/j.1600-079X.1998.tb00361.x. [DOI] [PubMed] [Google Scholar]
- 115.Galano A., Medina M.D., Tan D.X., Reiter R.J. Melatonin and its metabolites as copper chelating agents and their role in inhibiting oxidative stress: A physicochemical study. J. Pineal Res. 2015;58:107–116. doi: 10.1111/jpi.12196. [DOI] [PubMed] [Google Scholar]
- 116.Barlow-Walden L.R., Reiter R.J., Abe M., Pablos M.I., Menendez-Pelaez A., Chen L.D., Poeggeler B. Melatonin stimulates brain glutathione peroxidase activity. Neurochem. Int. 1995;26:497–502. doi: 10.1016/0197-0186(94)00154-M. [DOI] [PubMed] [Google Scholar]
- 117.Pablos M.I., Agapito M.T., Gutierrez R., Recio J.M., Reiter R.J., Barlow-Walden L.R., Acuna-Castroviejo D., Menendez-Pelaez A. Melatonin stimulates the activity of the detoxifying enzyme glutathione peroxidase in several tissues of chicks. J. Pineal Res. 1995;19:111–115. doi: 10.1111/j.1600-079X.1995.tb00178.x. [DOI] [PubMed] [Google Scholar]
- 118.Pablos M.I., Reiter R.J., Ortiz G.G., Guerrero J.M., Agapito M.T., Chuang J.J., Sewerynek E. Rhythms of glutathione peroxidase and glutathione reductase in brain of chick and their inhibition by light. Neurochem. Int. 1998;32:69–75. doi: 10.1016/S0197-0186(97)00043-0. [DOI] [PubMed] [Google Scholar]
- 119.Antolin I., Rodriquez C., Sainz R.M., Mayo J.C., Uria H., Kotler M.L., Rodriquez-Colunga M.J., Tolivia D., Menendez-Pelaez A. Neurohormone melatonin prevents cell damage: Effect on gene expression for antioxidant enzymes. FASEB J. 1996;10:882–890. doi: 10.1096/fasebj.10.8.8666165. [DOI] [PubMed] [Google Scholar]
- 120.Kotler M.L., Rodriguez C., Sainz R.M., Antolin I., Menendez-Pelaez A. Melatonin increases gene expression for antioxidant enzymes in rat brain cortex. J. Pineal Res. 1998;24:83–89. doi: 10.1111/j.1600-079X.1998.tb00371.x. [DOI] [PubMed] [Google Scholar]
- 121.Pablos M.I., Guerrero J.M., Ortiz G.G., Agapito M.T., Reiter R.J. Both melatonin and a putative nuclear melatonin receptor agonist CGP 52608 stimulate glutathione peroxidase and glutathione reductase activities in mouse brain in vivo. Neuroendocrinol. Lett. 1997;18:49–58. [Google Scholar]
- 122.Reiter R.J., Tan D.X., Osuna C., Gitto E. Actions of melatonin in the reduction of oxidative stress: A review. J. Biomed. Sci. 2000;7:444–458. doi: 10.1007/BF02253360. [DOI] [PubMed] [Google Scholar]
- 123.Rodriquez C., Mayo J.C., Sainz R.M., Antolin I., Herrera F., Martin V., Reiter R.J. Regulation of antioxidant enzymes: A significant role for melatonin. J. Pineal Res. 2004;36:1–9. doi: 10.1046/j.1600-079X.2003.00092.x. [DOI] [PubMed] [Google Scholar]
- 124.Reiter R.J., Tan D.X., Rosales-Corral S., Manchester L.C. The universal nature, unequal distribution and antioxidant functions of melatonin and its derivatives. Mini Rev. Med. Chem. 2013;13:373–384. doi: 10.2174/1389557511313030006. [DOI] [PubMed] [Google Scholar]
- 125.Gitto E., Tan D.X., Reiter R.J., Karbownik M., Manchester L.C., Cuzzocrea S., Fulia F., Barberi I. Individual and synergistic antioxidative actions of melatonin: Studies with vitamin E, vitamin C, glutathione and desferrioxamine (desferoxamine) in rat liver homogenates. J. Pharm. Pharmacol. 2001;53:1393–1401. doi: 10.1211/0022357011777747. [DOI] [PubMed] [Google Scholar]
- 126.Milczarek R., Hallmann A., Sokolowska E., Kaletha K., Klimek J. Melatonin enhances antioxidant action of α-tocopherol and ascorbate against NADPH- and iron-dependent lipid peroxidation in human placental mitochondria. J. Pineal Res. 2010;49:149–155. doi: 10.1111/j.1600-079X.2010.00779.x. [DOI] [PubMed] [Google Scholar]
- 127.Boutin J.A. Quinone reductase 2 as a promising target of melatonin therapeutic actions. Expert Opin. Ther. Targets. 2016;20:303–317. doi: 10.1517/14728222.2016.1091882. [DOI] [PubMed] [Google Scholar]
- 128.Hardeland R. Antioxidant protection by melatonin: Multiplicity of mechanisms from radical detoxification to radical avoidance. Endocrine. 2005;27:119–130. doi: 10.1385/ENDO:27:2:119. [DOI] [PubMed] [Google Scholar]
- 129.Hardeland R. Melatonin and the electron transport chain. Cell. Mol. Life Sci. 2017;74:3883–3896. doi: 10.1007/s00018-017-2615-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lerner A.B., Case J.D., Takahashi Y., Lee T.H., Mori W. Isolation of melatonin, the pineal gland factor that lightens melanocytes. J. Am. Chem. Soc. 1958;80:2587. doi: 10.1021/ja01543a060. [DOI] [Google Scholar]
- 131.Axelrod J., Wurtman R.J., Snyder S.H. Control of hydroxyindole O-methyltransferase activity in the rat pineal gland by environmental lighting. J. Biol. Chem. 1965;240:949–954. [PubMed] [Google Scholar]
- 132.Champney T.H., Holtorf A.P., Steger R.W., Reiter R.J. Concurrent determination of enzymatic activities and substrate concentrations in the melatonin synthetic pathway within the same rat pineal gland. J. Neurosci. Res. 1984;11:59–66. doi: 10.1002/jnr.490110107. [DOI] [PubMed] [Google Scholar]
- 133.Cardinali D.P., Rosner J.M. Ocular distribution of hydroxyindole O-methyltransferase (HIOMT) in the duck (Anas platyrhynchos) Gen. Comp. Endocrinol. 1972;18:407–409. doi: 10.1016/0016-6480(72)90231-6. [DOI] [PubMed] [Google Scholar]
- 134.Cardinali D.P., Wurtman R.J. Hydroxyindole-O-methyltransferases in rat pineal, retina and Harderian gland. Endocrinology. 1972;91:247–252. doi: 10.1210/endo-91-1-247. [DOI] [PubMed] [Google Scholar]
- 135.Tricoire H., Moller M., Chermineau P., Malpaux B. Origin of cerebrospinal fluid melatonin and possible function in the integration of photoperiod. Reprod. Suppl. 2003;61:311–321. [PubMed] [Google Scholar]
- 136.Reiter R.J., Tan D.X., Kim S.J., Cruz M.H. Delivery of pineal melatonin to the brain and SCN: Role of canaliculi, cerebrospinal fluid, tanycytes and Virchow-Robin perivascular spaces. Brain Struct. Funct. 2014;219:1873–1887. doi: 10.1007/s00429-014-0719-7. [DOI] [PubMed] [Google Scholar]
- 137.Legros C., Chesneau D., Boutin J.A., Barc L., Malpaux B. Melatonin from cerebrospinal fluid but not from blood reaches sheep cerebral tissues under physiological conditions. J. Neuroendocrinol. 2014;26:151–163. doi: 10.1111/jne.12134. [DOI] [PubMed] [Google Scholar]
- 138.Goldman H., Wurtman R.J. Flow of blood to the pineal body of the rat. Nature. 1964;203:87–88. doi: 10.1038/203087a0. [DOI] [PubMed] [Google Scholar]
- 139.Matsushima S., Reiter R.J. Ultrastructural observations at pineal gland capillaries in four rodent species. Am. J. Anat. 1975;143:265–281. doi: 10.1002/aja.1001430302. [DOI] [PubMed] [Google Scholar]
- 140.Bubenik G.A. Localization, physiological significance and possible clinical implications of gastrointestinal melatonin. Biol. Signals Recept. 2001;10:350–366. doi: 10.1159/000046903. [DOI] [PubMed] [Google Scholar]
- 141.Lynch H.J., Ozaki Y., Shakal D., Wurtman R.J. Melatonin excretion of man and rats: Effect of time of day, sleep, Pinealectomy and food consumption. Int. J. Biometeorol. 1975;19:267–279. doi: 10.1007/BF01451037. [DOI] [PubMed] [Google Scholar]
- 142.Tetsno M., Perlow M.J., Mishkin M., Markey S.P. Light exposure reduces and pinealectomy virtually stops urinary excretion of 6-hydroxymelatonin by rhesus monkeys. Endocrinology. 1982;110:997–1003. doi: 10.1210/endo-110-3-997. [DOI] [PubMed] [Google Scholar]
- 143.Waldhauser F., Waldhauser M., Lieberman H.R., Deng M.H., Lynch H.J., Wurtman R.J. Bioavailability of oral melatonin in humans. Neuroendocrinology. 1984;39:307–314. doi: 10.1159/000123997. [DOI] [PubMed] [Google Scholar]
- 144.English J., Bojkowski L.J., Poulton A.L., Symons A.M., Arendt J. Metabolism pharmacokinetics of melatonin in the ewe. J. Pineal Res. 1987;4:351–358. doi: 10.1111/j.1600-079X.1987.tb00874.x. [DOI] [PubMed] [Google Scholar]
- 145.Tan D.X., Manchester L.C., Reiter R.J., Qi W., Hanes M.A., Farley N.J. High physiological levels of melatonin in the bile of mammals. Life Sci. 1999;65:2523–2529. doi: 10.1016/S0024-3205(99)00519-6. [DOI] [PubMed] [Google Scholar]
- 146.Tamura J., Nakamura Y., Korkmaz A., Manchester L.C., Tan D.X., Sugino N., Reiter R.J. Melatonin and the ovary: Physiological and pathophysiological implications. Fertil. Steril. 2009;92:328–343. doi: 10.1016/j.fertnstert.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 147.Coelho L.A., Peres R., Amaral F.G., Reiter R.J., Cipolla-Neto J. Daily differential expression of melatonin-related genes and clock genes in rat cumulus-oocyte complex: Changes after pinealectomy. J. Pineal Res. 2015;58:490–499. doi: 10.1111/jpi.12234. [DOI] [PubMed] [Google Scholar]
- 148.He C., Wang J., Zhang Z., Yang M., Li Y., Tian X., Ma T., Tao J., Zhu K., Song Y., et al. Mitochondria synthesize melatonin to ameliorate its function and improve mice oocyte’s quality under in vitro conditions. Int. J. Mol. Sci. 2016;17:939. doi: 10.3390/ijms17060939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Vaughan G.M., Pelham R.W., Pang S.F., Loughlin L.L., Wilson K.M., Sandock L., Vaughn M.K., Koslow S.H., Reiter R.J. Nocturnal elevation of plasma melatonin and urinary 5-hydroxyindoleacetic acid in young men: Attempts at modification by brief changes in environmental lighting and sleep and by autonomic drugs. J. Clin. Endocrinol. Metab. 1976;42:752–764. doi: 10.1210/jcem-42-4-752. [DOI] [PubMed] [Google Scholar]
- 150.Stehle J.H., Saade A., Rawashdeh O., Ackermann K., Jilg A., Sebesteny T., Maronde E. A survey of molecular details in the human pineal gland in the light of phylogeny, structure function and chronobiological diseases. J. Pineal Res. 2011;51:17–43. doi: 10.1111/j.1600-079X.2011.00856.x. [DOI] [PubMed] [Google Scholar]
- 151.Houdek P., Novakova M., Polidarova L., Sladek M., Sumova A. Melatonin is a redundant entraining signal in the rat circadian system. Horm. Behav. 2016;83:1–5. doi: 10.1016/j.yhbeh.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 152.Pevet P. Melatonin receptors as therapeutic targets in the suprachiasmatic nucleus. Expert Opin. Ther. Targets. 2016;20:1209–1218. doi: 10.1080/14728222.2016.1179284. [DOI] [PubMed] [Google Scholar]
- 153.Pfeffer M., Korf H.W., Wicht H. Synchronizing effects of melatonin on diurnal and circadian rhythms. Gen. Comp. Endocrinol. 2018;258:215–221. doi: 10.1016/j.ygcen.2017.05.013. [DOI] [PubMed] [Google Scholar]
- 154.Reiter R.J., Tamura H., Tau D.X., Xu X.Y. Melatonin and the circadian system: Contributions to successful female reproduction. Fertil. Steril. 2014;102:321–328. doi: 10.1016/j.fertnstert.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 155.Zerman M., Herichova I. Melatonin and clock genes expression in the cardiovascular system. Front. Biosci. 2013;5:743–753. doi: 10.2741/S404. [DOI] [PubMed] [Google Scholar]
- 156.Reiter R.J., Tan D.X., Korkmaz A., Rosales-Corral S.A. Melatonin and stable circadian rhythms optimize maternal, placental and fetal physiology. Hum. Reprod. Update. 2014;20:293–307. doi: 10.1093/humupd/dmt054. [DOI] [PubMed] [Google Scholar]
- 157.Hardeland R. Melatonin and circadian oscillators in aging—A dynamic approach to the multiply connected players. Interdiscip. Top. Gerontol. 2015;40:128–140. doi: 10.1159/000364975. [DOI] [PubMed] [Google Scholar]
- 158.Faraut B., Bayon V., Leger D. Neuroendocrine, immune and oxidative stress in shift workers. Sleep Med. Dev. 2013;17:430–444. doi: 10.1016/j.smrv.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 159.Ndiaye M.A., Nihal M., Wood G.S., Ahmad N. Skin, reactive oxygen species, and circadian clocks. Antioxid. Redox Signal. 2014;20:2982–2996. doi: 10.1089/ars.2013.5645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Reiter R.J., Mayo J.C., Tan D.X., Sainz R.M., Alatorre-Jimenez M., Qin L. Melatonin as an antioxidant: Under promises but over delivers. J. Pineal Res. 2016;61:253–278. doi: 10.1111/jpi.12360. [DOI] [PubMed] [Google Scholar]
- 161.Reiter R.J., Rosales-Corral S.A., Tan D.X., Alatorre-Jimenez M., Lopez C. Circadian dysregulation and melatonin rhythm suppression in the context of aging. In: Jazwinski S.M., Belancio V.P., Hill S.M., editors. Circadian Rhythms and Their Impact on Aging. Springer; Chambersburg, PA, USA: 2017. pp. 1–25. [Google Scholar]
- 162.Troini M.E., Reiter R.J., Tannenbaum M.G., Puig-Domingo M., Guerrero M.M., Menendez-Pelaez A. Neither the pituitary gland nor the sympathetic nervous system is responsible for eliciting the large drop in elevated rat pineal melatonin levels due to swimming. J. Neural Transm. 1988;74:149–160. doi: 10.1007/BF01244781. [DOI] [PubMed] [Google Scholar]
- 163.Wu W., Chen Y.C., Reiter R.J. Day-night differences in the response of the pineal gland to swimming stress. Proc. Soc. Exp. Biol. Med. 1988;187:315–319. doi: 10.3181/00379727-187-42670. [DOI] [PubMed] [Google Scholar]
- 164.Adamo A.M., Llesuy S.F., Pasquini J.M., Boveris A. Brain chemiluminescence and oxidative stress in hyperthyroid rats. Biochem. J. 1989;263:273–277. doi: 10.1042/bj2630273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sjodin B., Hellsten Westing Y., Apple F.S. Biochemical mechanisms for oxygen free radical formation during exercise. Sport Med. 1990;10:236–254. doi: 10.2165/00007256-199010040-00003. [DOI] [PubMed] [Google Scholar]
- 166.Jou M.J., Peng T.I., Hsu L.F., Jou S.B., Reiter R.J., Yang C.M., Chiao C.C., Lin Y.F., Chen C.C. Visualization of melatonin’s multiple mitochondrial levels of protection against mitochondrial Ca(2+)-mediated permeability transition and beyond in rat brain astrocytes. J. Pineal Res. 2010;48:20–38. doi: 10.1111/j.1600-079X.2009.00721.x. [DOI] [PubMed] [Google Scholar]
- 167.Jou M.J., Peng T.I., Reiter R.J., Jou S.B., Wu H.Y., Wen S.T. Visualization of the antioxidant effects of melatonin at the mitochondrial level during oxidative stress-induced apoptosis of rat brain astrocytes. J. Pineal Res. 2004;37:55–70. doi: 10.1111/j.1600-079X.2004.00140.x. [DOI] [PubMed] [Google Scholar]
- 168.Jou M.J., Peng T.I., Yu P.Z., Jou S.B., Reiter R.J., Chen J.Y., Wu H.Y., Chen C.C., Hsu L.F. Melatonin protects against common deletion of mitochondrial DNA-augmented mitochondrial oxidative stress and apoptosis. J. Pineal Res. 2007;43:389–403. doi: 10.1111/j.1600-079X.2007.00490.x. [DOI] [PubMed] [Google Scholar]
- 169.Acuna-Castroviejo D., Martin M., Macias M., Escames G., Leon J., Khaldy H., Reiter R.J. Melatonin, mitochondria, and cellular bioenergetics. J. Pineal Res. 2001;30:65–74. doi: 10.1034/j.1600-079X.2001.300201.x. [DOI] [PubMed] [Google Scholar]
- 170.Acuna-Castroviejo D., Escames G., Rodriguez M.I., Lopez L.C. Melatonin role in the mitochondrial function. Front. Biosci. 2007;12:947–963. doi: 10.2741/2116. [DOI] [PubMed] [Google Scholar]
- 171.Tan D.X., Manchester L.C., Liu X., Rosales-Corral S.A., Acuna-Castroviejo D., Reiter R.J. Mitochondria and chloroplasts as the original sites of melatonin synthesis: A hypothesis related to melatonin’s primary function and evolution in eukaryotes. J. Pineal Res. 2013;54:127–138. doi: 10.1111/jpi.12026. [DOI] [PubMed] [Google Scholar]
- 172.Margulis L. Symbiotic theory of the origin of eukaryotic organelles: Criteria for proof. Symp. Soc. Exp. Biol. 1975;29:21–38. [PubMed] [Google Scholar]
- 173.Archibald J.M. Endosymbiosis and eukaryotic cell evolution. Curr. Biol. 2015;25:R911–R921. doi: 10.1016/j.cub.2015.07.055. [DOI] [PubMed] [Google Scholar]
- 174.Manchester L.C., Poeggeler B., Alvares F.L., Ogden G.B., Reiter R.J. Melatonin immunoreactivity in the photosynthetic prokaryote Rhodospirillum rubrum: Implications for an ancient antioxidant system. Cell. Mol. Biol. Res. 1995;41:391–395. [PubMed] [Google Scholar]
- 175.Tilden A.R., Becker M.A., Amma L.L., Arciniega J., McGaw A.K. Melatonin production in an aerobic photosynthetic bacterium: An evolutionarily early association with darkness. J. Pineal Res. 1997;22:102–106. doi: 10.1111/j.1600-079X.1997.tb00310.x. [DOI] [PubMed] [Google Scholar]
- 176.Konopelski P., Ufnal M. Indoles—Gut bacteria metabolites of tryptophan with pharmacotherapeutic potential. Curr. Drug Metab. 2018 doi: 10.2174/1389200219666180427164731. in press. [DOI] [PubMed] [Google Scholar]
- 177.Venegas C., Garcia J.A., Escames G., Ortiz F., Lopez A., Doerrier C., Garcia-Corzo L., Lopez L.C., Reiter R.J., Acuna-Castroviejo D. Extrapineal melatonin: Analysis of its subcellular distribution and daily fluctuations. J. Pineal Res. 2012;52:217–227. doi: 10.1111/j.1600-079X.2011.00931.x. [DOI] [PubMed] [Google Scholar]
- 178.Hevia D., Gonzalez-Menendez P., Quiros-Gonzalez I., Miar A., Rodriguez-Garcia A., Tan D.X., Reiter R.J., Mayo J.C., Sainz R.M. Melatonin uptake through glucose transporters: A new target for melatonin inhibition of cancer. J. Pineal Res. 2015;58:234–250. doi: 10.1111/jpi.12210. [DOI] [PubMed] [Google Scholar]
- 179.Deng D., Sun P., Yan C., Ke M., Jiang X., Xiong L., Ren W., Hirata K., Yamamoto M., Fan S., et al. Molecular basis of ligand recognition and transport by glucose transporters. Nature. 2015;526:391–396. doi: 10.1038/nature14655. [DOI] [PubMed] [Google Scholar]
- 180.Huo X., Wang C., Yu Z., Peng Y., Wang S., Feng S., Zhang S., Tian X., Sun C., Liu K., et al. Human transporters, PEPT1/2, facilitate melatonin transportation into mitochondria of cancer cells: An implication of the therapeutic potential. J. Pineal Res. 2017;62:e12390. doi: 10.1111/jpi.12390. [DOI] [PubMed] [Google Scholar]
- 181.Kerenyi N.A., Balogh I., Somogyi E., Satonyi P. Cytochemical investigation of acetyl-serotonin-transferase activity in the pineal gland. Cell. Mol. Biol. Incl. Cyto-Enzymol. 1979;25:259–262. [PubMed] [Google Scholar]
- 182.Suofu Y., Li W., Jean-Alphonse F.G., Jia J., Khattar N.K., Li J., Baranov S.V., Leronni D., Mihalik A.C., He Y., et al. Dual role of mitochondria in producing melatonin and driving GPCR signaling to block cytochrome C release. Proc. Nat. Acad. Sci. USA. 2017;115:E1944. doi: 10.1073/pnas.1800449115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Martin M., Macias M., Escames G., Reiter R.J., Agapito M.T., Ortiz G.G., Acuna-Castroviejo D. Melatonin-induced increased activity of the respiratory chain complexes I and IV can prevent mitochondrial damage induced by ruthenium red in vivo. J. Pineal Res. 2000;28:242–248. doi: 10.1034/j.1600-079X.2000.280407.x. [DOI] [PubMed] [Google Scholar]
- 184.Jimenez-Aranda A., Fernandez-Vazquez G., Mohammad A-Serrano M., Reiter R.J., Agil A. Melatonin improves mitochondrial function in inguinal white adipose tissue of Zucker diabetic fatty rats. J. Pineal Res. 2014;57:103–109. doi: 10.1111/jpi.12147. [DOI] [PubMed] [Google Scholar]
- 185.Acuna-Castroviejo D., Lopez L.C., Escames G., Lopez A., Garcia J.A., Reiter R.J. Melatonin-mitochondria interplay in health and disease. Curr. Top. Med. Chem. 2011;11:221–240. doi: 10.2174/156802611794863517. [DOI] [PubMed] [Google Scholar]
- 186.Liu L.F., Qin Q., Qian Z.H., Shi M., Deng Q.C., Zhu W.P., Zhang H., Tao X.M., Liu Y. Protective effects of melatonin on ischemia-reperfusion induced myocardial damage and hemodynamic recovery in rats. Eur. Rev. Med. Pharmacol. Sci. 2014;18:3681–3686. [PubMed] [Google Scholar]
- 187.Miller E., Morel A., Saso L., Saluk J. Melatonin redox activity. Its potential clinical applications in neurodegenerative disorders. Curr. Top. Med. Chem. 2015;15:163–169. doi: 10.2174/1568026615666141209160556. [DOI] [PubMed] [Google Scholar]
- 188.Skobowiat C., Brozyna A.A., Janyetovic Z., Jeayeng S., Oak A.S.W., Kim T.K., Panich U., Reiter R.J., Slominski A.T. Melatonin and its derivatives counteract the ultraviolet B radiation-induced damage in human and porcine skin ex vivo. J. Pineal Res. 2018:e312501. doi: 10.1111/jpi.12501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Winiarska K., Fraczyk T., Maliniska D., Drozak J., Bryla J. Melatonin attenuates diabetes-induced oxidative stress in rabbits. J. Pineal Res. 2006;40:168–176. doi: 10.1111/j.1600-079X.2005.00295.x. [DOI] [PubMed] [Google Scholar]
- 190.Urata Y., Honma S., Goto S., Todoroki S., Iida T., Cho S., Honma K., Kondo T. Melatonin induces gamma-glutamylcysteine synthetase mediated by activator protein-1 in human vascular endothelial cells. Free Radic. Biol. Med. 1999;27:838–847. doi: 10.1016/S0891-5849(99)00131-8. [DOI] [PubMed] [Google Scholar]
- 191.Esteban-Zubero E., Garcia-Gil F.A., Lopez-Pingarron L., Alatorre-Jimenez M.A., Inigo-Gil P., Tan D.X., Garcia J.J., Reiter R.J. Potential benefits of melatonin in organ transplantation: A review. J. Endocrinol. 2016;229:129–146. doi: 10.1530/JOE-16-0117. [DOI] [PubMed] [Google Scholar]
- 192.Radogna F., Cristofanon S., Patemoster L., D’Alessio M., DeNicola M., Cerella C., Dicato M., Diederich M., Ghibelli L. Melatonin antagonizes the intrinsic pathway of apoptosis via mitochondrial targeting of Bcl-2. J. Pineal Res. 2008;44:316–325. doi: 10.1111/j.1600-079X.2007.00532.x. [DOI] [PubMed] [Google Scholar]
- 193.Paredes S.D., Forman K.A., Garcia C., Vara E., Escames G., Tresguerres J.A. Protective actions of melatonin and growth hormone on the aged cardiovascular system. Horm. Mol. Biol. Clin. Investig. 2014;18:79–88. doi: 10.1515/hmbci-2014-0016. [DOI] [PubMed] [Google Scholar]
- 194.Fernandez A., Ordonez R., Reiter R.J., Gonzalez-Gallego J., Mauriz J.L. Melatonin and endoplasmic reticulum stress: Relation to autophagy and apoptosis. J. Pineal Res. 2015;59:292–307. doi: 10.1111/jpi.12264. [DOI] [PubMed] [Google Scholar]
- 195.Ma Z., Xin Z., Di W., Yan X., Li X., Reiter R.J., Yang Y. Melatonin and mitochondrial function during ischemia/reperfusion injury. Cell. Mol. Life Sci. 2017;74:3989–3998. doi: 10.1007/s00018-017-2618-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Tatone C., Di Emidio G., Barbonetti A., Carta G., Luciano A.M., Falone S., Amicarelli F. Sirtuins in gamete biology and reproductive physiology: Emerging roles and therapeutic potential in female and male infertility. Hum. Reprod. Update. 2018;24:267–289. doi: 10.1093/humupd/dmy003. [DOI] [PubMed] [Google Scholar]
- 197.Watroba M., Szukiewicz D. The role of sirtuins in aging and age-related diseases. Adv. Med. Sci. 2016;61:52–62. doi: 10.1016/j.advms.2015.09.003. [DOI] [PubMed] [Google Scholar]
- 198.Kumar S., Lombard D.B. Functions of the sirtuin deacylase SIRT5 in normal physiology and pathophysiology. Crit. Rev. Biochem. Mol. Biol. 2018;53:311–334. doi: 10.1080/10409238.2018.1458071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Lim J.H., Lee Y.M., Chun Y.S., Chen J., Kim J.E., Park J.W. Sirtuin 1 modulates cellular responses to hypoxia by deacetylating hypoxia-inducible factor 1α. Mol. Cell. 2010;38:864–878. doi: 10.1016/j.molcel.2010.05.023. [DOI] [PubMed] [Google Scholar]
- 200.Liu G., Bin P., Wang T., Ren W., Zhong J., Liang J., Hu C.A., Zeng Z., Yin Y. DNA methylation and the potential role of methyl-containing nutrients in cardiovascular diseases. Oxid. Med. Cell. Longev. 2017;2017:1670815. doi: 10.1155/2017/1670815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Sundaresan N.R., Gupta M., Kim G., Rajamohan S.B., Isbatan A., Gupta M.P. Sirt3 blocks the cardiac hypertrophic response by augmenting Foxo3a-dependent antioxidant defense mechanisms in mice. J. Clin. Investig. 2009;119:2758–2771. doi: 10.1172/JCI39162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Tseng A.H., Shieh S.S., Wang D.L. SIRT3 deacetylates FOXO3 to protect mitochondria against oxidative damage. Free Radic. Biol. Med. 2013;63:222–234. doi: 10.1016/j.freeradbiomed.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 203.Taleb-Belkadi O., Chaib H., Zemour L., Fatah A., Chafi B., Mekki K. Lipid prolife, inflammation, and oxidative status in peri- and postmenopausal women. Gynecol. Endocrinol. 2016;32:982–985. doi: 10.1080/09513590.2016.1214257. [DOI] [PubMed] [Google Scholar]
- 204.Pertynska-Marczewska M., Diamanti-Kandarakis E. Aging ovary and the role for advanced glycation end products. Menopause. 2017;24:345–351. doi: 10.1097/GME.0000000000000755. [DOI] [PubMed] [Google Scholar]
- 205.Tamura H., Takasaki A., Miwa I., Taniguchi K., Maekawa R., Asada H., Taketani T., Matsuoka A., Yamagata Y., Shimamura K., et al. Oxidative stress impairs oocyte quality and melatonin protects oocytes from free radical damage and improves fertilization rate. J. Pineal Res. 2008;44:280–287. doi: 10.1111/j.1600-079X.2007.00524.x. [DOI] [PubMed] [Google Scholar]
- 206.Budani M.C., Carletti E., Tiboni G.M. Cigarette smoke is associated with altered expression of antioxidant enzymes in granulosa cells from women undergoing in vitro fertilization. Zygote. 2017;25:296–303. doi: 10.1017/S0967199417000132. [DOI] [PubMed] [Google Scholar]
- 207.Mishra B., Ripperdan R., Ortiz L., Luderer U. Very low doses of heavy oxygen ion radiation induce premature ovarian failure. Reproduction. 2017;154:123–133. doi: 10.1530/REP-17-0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Wang T., Gao Y.Y., Chen L., Nei Z.W., Cheng W., Liu X., Schatten H., Zhang X., Miao Y.L. Melatonin prevents postovulatory oocyte aging and promotes subsequent embryonic development in the pig. Aging. 2017;9:1552–1564. doi: 10.18632/aging.101252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Pang Y., Zhao S., Sun Y., Jiang X., Hao H., Du W., Zhu H. Protective effects of melatonin on the in vitro developmental competence of bovine oocytes. Anim. Sci. J. 2018;89:648–660. doi: 10.1111/asj.12970. [DOI] [PubMed] [Google Scholar]
- 210.Han L., Wang H., Li L., Li X., Ge J., Reiter R.J., Wang Q. Melatonin protects against maternal obesity-associated oxidative stress and meiotic defects in oocytes via the SIRT3-SOD2-dependent pathway. J. Pineal Res. 2017;63:12431. doi: 10.1111/jpi.12431. [DOI] [PubMed] [Google Scholar]
- 211.Song C., Peng W., Yin S., Zhao J., Fu B., Zhang J., Mao T., Wu H., Zhang Y. Melatonin improves age-induced fertility decline and attenuates ovarian mitochondrial oxidative stress in mice. Sci. Rep. 2016;6:35165. doi: 10.1038/srep35165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Tamura H., Kawamoto M., Sato S., Tamura I., Maekawa R., Taketani T., Aasada H.S., Takaki E., Nakai A., Reiter R.J., et al. Long term melatonin treatment delays ovarian aging. J. Pineal Res. 2017;62:e12381. doi: 10.1111/jpi.12381. [DOI] [PubMed] [Google Scholar]
- 213.Li Y., Yang Y., Feng Y., Yan J., Fan C., Jiang S., Qu Y. A review of melatonin in hepatic ischemia/reperfusion injury and clinical liver disease. Ann. Med. 2014;46:503–511. doi: 10.3109/07853890.2014.934275. [DOI] [PubMed] [Google Scholar]
- 214.Halladin N.L. Oxidative and inflammatory biomarkers of ischemia and reperfusion injuries. Dan. Med. J. 2015;62:B5054. [PubMed] [Google Scholar]
- 215.Paterniti I., Cordaro M., Esposito E., Cuzzocrea S. The antioxidant property of melatonin against brain ischemia. Exp. Rev. Neurother. 2016;16:841–848. doi: 10.1080/14737175.2016.1182020. [DOI] [PubMed] [Google Scholar]
- 216.Yu L., Gong B., Duan W., Fan C., Zhang J., Li Z., Xue X., Xu Y., Meng D., Li B., et al. Melatonin ameliorates myocardial ischemia/reperfusion injury in type 1 diabetic rats by preserving mitochondrial function: Role of AMPK-PGC-1α-SIRT3 signaling. Sci. Rep. 2017;7:41337. doi: 10.1038/srep41337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Zhai M., Li B., Duan W., Jing L., Zhang B., Zhang M., Yu L., Liu Z., Yu B., Ren K., et al. Melatonin ameliorates myocardial ischemia reperfusion injury through SIRT3-dependent regulation of oxidative stress and apoptosis. J. Pineal Res. 2017;63:e12419. doi: 10.1111/jpi.12419. [DOI] [PubMed] [Google Scholar]
- 218.Zhang M., Lin J., Wang S., Cheng Z., Hu J., Wang T., Man W., Yin T., Guo W., Gao E., et al. Melatonin protects against diabetic cardiomyopathy through Mst1/Sirt 3 signaling. J. Pineal Res. 2017;63:e12418. doi: 10.1111/jpi.12418. [DOI] [PubMed] [Google Scholar]
- 219.Ross R. Arthrosclerosis—An inflammatory disease. N. Engl. J. Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 220.Yip H.K., Sun C.K., Chang L.T., Wu C.J. Strong correlation between serum levels of inflammatory mediators and their distribution in infarct-related coronary artery. Circ. J. 2006;70:838–845. doi: 10.1253/circj.70.838. [DOI] [PubMed] [Google Scholar]
- 221.Reiter R.J., Tan D.X., Kim S.J., Manchester L.C., Qi W., Garcia J.J., Cabrera J.C., El-Sokkary G., Rouvier-Garay V. Augmentation of indices of oxidative damage in life-long melatonin-deficient rats. Mech. Ageing Rev. 1999;110:157–173. doi: 10.1016/S0047-6374(99)00058-5. [DOI] [PubMed] [Google Scholar]
- 222.Garcia J.J., Lopez-Pingarron, Almeida-Souza P., Tres A., Escudero P., Garcia-Gil F.A., Tan D.X., Reiter R.J., Ramirez J.M., Bernal-Perez M. Protective effects of melatonin in reducing oxidative stress and in preserving the fluidity of biological membranes: A review. J. Pineal Res. 2014;56:225–237. doi: 10.1111/jpi.12128. [DOI] [PubMed] [Google Scholar]
- 223.Lee F.Y., Sun C.K., Sung P.H., Chen K.H., Chua S., Sheu J.J., Chung S.Y., Chai H.T., Chen Y.L., Huang T.H., et al. Daily melatonin protects the endothelial lineage and functions integrity against the aging process, oxidative stress, and toxic environment and restores blood flow in critical limb ischemia area in mice. J. Pineal Res. 2018;64:e12489. doi: 10.1111/jpi.12489. [DOI] [PubMed] [Google Scholar]
- 224.Pereira H.A., Leite Ade S., Charone S., Lobo J.G., Cestari T.M., Peres-Buzalaf C., Buzalaf M.A. Proteomic analysis of liver in rats chronically exposed to fluoride. PLoS ONE. 2013;8:e75343. doi: 10.1371/annotation/54b8fb45-bb22-469e-96b3-77e99ba62b77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Bharti V.K., Srivastava R.S., Kumar S., Bag S., Majumdar A.C., Singh G., Pandi-Perumal S.R., Brown G.M. Effects of melatonin and epiphyseal proteins on fluoride-induced adverse changes in antioxidant status of heart, liver, and kidney of rat. Adv. Pharmacol. Sci. 2014;2014:532969. doi: 10.1155/2014/532969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Song C., Zhao J., Fu B., Li D., Mao T., Peng W., Wu H., Zhang Y. Melatonin-mediated upregulation of Sirt3 attenuates sodium fluoride-induced hepatotoxicity by activating the MT1-PI3K/AKT-PGC-1α signaling pathway. Free Radic. Biol. Med. 2017;112:616–630. doi: 10.1016/j.freeradbiomed.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 227.Chen Y., Qing W., Sun M., Lv L., Guo D., Jiang Y. Melatonin protects hepatocytes against bile-acid-induced mitochondrial oxidative stress via the AMPK-SIRT3-SOD2 pathway. Free Radic. Res. 2015;49:1275–1284. doi: 10.3109/10715762.2015.1067806. [DOI] [PubMed] [Google Scholar]
- 228.Ohta Y., Kongo M., Kishikawa T. Melatonin exerts a therapeutic effect on cholestatic liver injury in rats with bile duct ligation. J. Pineal Res. 2003;34:119–126. doi: 10.1034/j.1600-079X.2003.00018.x. [DOI] [PubMed] [Google Scholar]
- 229.Ohta Y., Kongo-Nishimura M., Imai Y., Matsura T., Kitagawa A., Yamada K. Alpha-tocopherol protects against alpha-naphthylisothiocyanate-induced hepatotoxicity in rats less effectively than melatonin. Chem. Biol. Interact. 2006;161:115–124. doi: 10.1016/j.cbi.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 230.Acuna-Castroviejo D., Escames G., Leon J., Carazo A., Khaldy H. Mitochondrial regulation by melatonin and its metabolites. Adv. Exp. Med. Biol. 2003;527:549–557. doi: 10.1007/978-1-4615-0135-0_63. [DOI] [PubMed] [Google Scholar]
- 231.Acuna-Castroviejo D., Rahim I., Acuna-Fernandez C., Fernandez-Ortiz M., Solera-Marin J., Sayed R.K.A., Diaz-Casado M.E., Rusanova I., Lopez L.C., Escames G. Melatonin, clock genes and mitochondria in sepsis. Cell. Mol. Life Sci. 2017;74:3965–3987. doi: 10.1007/s00018-017-2610-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Bordo D. Structure and evolution of human sirtuins. Curr. Drug Targets. 2013;14:662–665. doi: 10.2174/1389450111314060007. [DOI] [PubMed] [Google Scholar]
- 233.Choi B.S., Park J.E., Jang C.Y. Sirt3 controls chromosome alignment by regulating spindle dynamics during mitosis. Biochem. Biophys. Res. Commun. 2014;444:662–669. doi: 10.1016/j.bbrc.2014.01.124. [DOI] [PubMed] [Google Scholar]
- 234.Lombard D.B., Zwaans B.M. SIRT3: As simple as it seems. Gerontology. 2014;60:56–64. doi: 10.1159/000354382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.McDonnel E., Peterson B.S., Bomze H.M., Hirschey M.D. SIRT3 regulates progression and development of diseases of aging. Trends Endocrinol. Metab. 2015;26:486–492. doi: 10.1016/j.tem.2015.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Benigni A., Perico L., Macconi D. Mitochondrial dynamics are linked to longevity and protect from end-organ injury: The emerging role of sirtuin 3. Antioxid. Redox Signal. 2016;25:185–199. doi: 10.1089/ars.2016.6682. [DOI] [PubMed] [Google Scholar]
- 237.Tang X., Chen X.F., Chen H.Z., Lui D.P. Mitochondrial sirtuins in cardiometabolic diseases. Clin. Sci. 2017;131:2063–2078. doi: 10.1042/CS20160685. [DOI] [PubMed] [Google Scholar]
- 238.Kincaid B., Bossy-Wetzel E. Forever young: SIRT3 a shield against mitochondrial meltdown, aging, and neurodegeneration. Front. Aging. Neurosci. 2013;5:48. doi: 10.3389/fnagi.2013.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Bause A.S., Haigis M.C. SIRT3 regulation of mitochondrial oxidative stress. Exp. Gerontol. 2013;48:634–639. doi: 10.1016/j.exger.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 240.Proietti S., Cucina A., Minini M., Bizzarri M. Melatonin, mitochondria and the cancer cell. Cell. Mol. Life Sci. 2017;74:4015–4025. doi: 10.1007/s00018-017-2612-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Ding M., Ning J., Feng N., Li Z., Liu Z., Wang Y., Wang Y., Li X., Huo C., Jia X., et al. Dynamin-related protein 1-mediated mitochondrial fission contributes to the post-traumatic cardiac dysfunction in rats and the protective effect of melatonin. J. Pineal Res. 2018;64:12447. doi: 10.1111/jpi.12447. [DOI] [PubMed] [Google Scholar]
- 242.Reiter R.J., Rosales-Corral S., Zhou X., Tan D.X. Role of SIRT3/SOD2 signaling in mediating the antioxidant actions of melatonin in mitochondria. Curr. Trends Endocrinol. 2017;9:45–49. [Google Scholar]
- 243.Paradies G., Paradies V., Ruggiero F.M., Petrosillo G. Mitochondrial bioenergetics decay in aging: Beneficial effect of melatonin. Cell. Mol. Life Sci. 2017;74:3897–3911. doi: 10.1007/s00018-017-2619-5. [DOI] [PMC free article] [PubMed] [Google Scholar]