Abstract
Background/Objective:
The purpose of this paper is to examine drug use and incarceration history among rural Appalachian women.
Methods:
This study involved random selection, screening, and interviews with rural women from local jails in Appalachia.
Results:
Of the women randomly selected and screened, 97% met criteria for substance use intervention. Significant factors associated with incarceration history included age, education, custody status, and mental health. A significant interaction was observed between male sex partners and drug use on incarceration history.
Conclusions:
Study findings suggest that the drug/crime relationship among rural Appalachian women is associated with their high-risk home environment, partner relationships, and mental health. Specifically, in addition to drug use, factors such as family and child relationships, anxiety, victimization, and relationships with partners should also be considered in the trajectory of criminal careers among rural Appalachian women.
Keywords: rural, Appalachia, women, offenders
Introduction
Women are growing faster than any other demographic group in the criminal justice system with an increase of more than 600% between 1980 and 2010, a rate of 1.5 times higher than men (Porter, 2013). The number of women incarcerated in local jails more specifically has increased significantly in recent years, 48% compared to a 17% increase in male jail inmates (Minton et al., 2015). Jails differ from prisons in that they are typically short-term facilities managed by locally elected administrators (BJA, 2016) and often have fewer resources for health and behavioral health services. U.S. data from jail samples of inmates suggest that the majority (74%) of incarcerated males and females reported a history of drug use, more than two-thirds (68%) met diagnostic criteria for abuse or dependence, and more than half (55%) reported active drug use in the month before arrest (Karberg & James, 2005; Wilson, 2000). Thus, jails can provide critical venues for research on high-risk, understudied, out-of-treatment female drug users.
Importance of research on rural women
In addition to limited jail research in general, there are also significant gaps in the literature on specific vulnerable groups of women offenders, such as rural women. Rural women suffer distinct health disparities including increased rates of cervical cancer and other female reproductive health issues (Tjaden, 2015), which has been attributed to significant limitations in rural primary care and specialty care (such as OB/GYN services) (Bennett et al., 2013). Rural women are more likely to experience chronic illness, suffer from chronic depression, poor maternal health, suicide, and have significant barriers to health services compared to urban women (American Psychological Association, n.d.). These health disparities have often been attributed to low socioeconomic status, education, and employment opportunities (Tjaden, 2015), as well as the isolation and cultural issues of living in a rural community (Foxhall, 2000), all of which can impact both access to adequate health and behavioral health care.
While correlates of health disparities among rural women have been attributed to poverty and limitations in health care access in rural Appalachia, these issues are also exacerbated by substance abuse. The health of a large number of rural Appalachians has been significantly compromised by an opioid epidemic, which has been associated with rapid spread of Hepatitis C (HCV), and rising overdose rates (Estep, 2016; Suryaprasad et al., 2014; Zibbell et al., 2015). In fact, per 100,000 people, some Appalachian counties have overdose rates three times higher than the national average (KY Office of Drug Control Policy, 2015). The high rate of opioid and other substance use in Appalachia has captured the attention of law enforcement, policymakers, and researchers nationwide.
Compounding the risks associated with prescription opioid abuse in general, injection drug use has become the primary route of administration of drugs in the Appalachian region, growing exponentially in recent years (Staton-Tindall et al., 2015a; Young & Havens, 2012). Rural Appalachian substance users are more likely to inject opiates compared to urban users (Young, Havens, & Leukefeld, 2010). Injecting drugs not only poses a significant health risk when needles and equipment are shared, but women often find themselves in vulnerable situations of being injected by a partner or a dealer (Young et al., 2014), which limits their control over the use of safe or clean injection equipment. Among a sample of rural drug users, women were more likely to have engaged in sexual intercourse with their injecting partner prior to or after their first injection than men (Young, et al., 2014). These practices place rural women in a position of even greater risk for disease, as well as the potential for physical harm.
Examining the drug/crime relationship among rural women
Thus, rural women face cultural, behavioral health, and geographic challenges associated with drug use. While the association between drug use and crime has been examined among female offenders, less attention has been paid to characteristics of rural women drug users who become involved in the criminal justice system. While it is expected that drug use and crime are related among rural women, it is not clear how other factors associated with rural culture or lifestyle may influence the drug/crime relationship. For example, due to low population density, rural women may have limited mobility and anonymity (Friedman, 2003), suggesting that a high-risk home environment where family members or peers use drugs may present challenges for rural women to “escape”. Additionally, based on findings from studies on partner availability analysis in other cultural groups of women (Oser et al., 2016), it is possible that the availability of partners who are not engaged in drug use and criminal activity are limited for rural women drug-users in Appalachia. Thus, high-risk partners may increase the likelihood of rural women engaging in high-risk behaviors.
Mental health is another factor associated with drug use and/or criminal involvement among women, but has been less studied among rural women. Women offenders, for example, have been shown to be more likely to experience mental health problems than males (Gunter et al., 2012; Johnson, 2006; Macdonald, 2013; Peters, et al., 1997; Webster et al., 2007), with depression and anxiety being most common (Sacks, 2004; Staton-Tindall, Leukefeld, & Webster, 2003). While mental health rates have been noted to be considerably higher among rural women than other women in jails (Staton-Tindall et al., 2015), it is important to better understand the role of mental health in the drug/crime relationship.
The current study
Studies with rural women drug users are challenging because recruitment can be limited by the lack of formal treatment opportunities, travel distances to study sites, and generally the protective nature of social networks that characterize rural areas (Friedman, 2003). Thus, conducting rural drug abuse research in real-world settings where high-risk, non-treatment seeking individuals can be located is important, particularly during critical windows of sobriety. Therefore, this study utilizes rural jails as venues to better understand the drug/crime relationship among rural Appalachian women. To our knowledge, no other empirical study has used a random selection design to recruit rural women from real-world settings to examine drug use, crime, and related factors.
The purpose of the current study is to examine the relationship between drug use and incarceration among rural Appalachian women, as well as the potential role of contextual factors including home environment, risky partner relationships, and mental health. The following specific objectives guide the study: 1) to profile drug use using a validated screening tool (Alcohol Smoking Substance Involved Screening Test – ASSIST) among a randomly selected sample of women recruited from rural jails; 2) to describe the relationship between drug use and incarceration history among rural women meeting ASSIST criteria for the study; and 3) to examine drug use as an independent correlate of incarceration history with other factors including the home environment, partner relationships, and mental health considered.
Method
Participants
Adult women (aged 18 and older) participating in this study (NIH/NIDA, 1R01-DA033866) were randomly selected from three rural jails in Appalachia, screened, and interviewed face-to-face in a private room in the jail. Study eligibility was determined through screening and included: 1) moderate risk of substance abuse based on the NIDA-modified Alcohol, Smoking and Substance Involvement Screening Test (NM-ASSIST) score of 4+ for any drug (NIDA, 2009); 2) residing in a designated Appalachian county before incarceration; and 3) willingness to participate.
Measures
Demographics
To profile the study sample, demographic data were collected including age (a continuous measure of self-reported age at the time of the baseline), race (category of racial group identified), marital status (categorically coded as married/living with someone as married vs. other), parenting status (dichotomous measure of having any children at the time of the interview vs. not), education (a continuous measure of total number of years of formal education), and employment (percentage of women reporting any employment including full-time or part-time prior to incarceration vs. not working). Considering the sample was recruited from jails, other descriptive measures included length of the current incarceration and number of lifetime months incarcerated.
Drug use
The NIDA-modified version of the Alcohol, Smoking and Substance Involvement Screening Test (NM-ASSIST) was used to measure drug use severity among women randomly selected from rural jails for study screening (NIDA, 2009). The ASSIST was developed by the World Health Organization (WHO, 2002) for use in primary health care settings, and modified by NIDA to separate specific categories of prescription opiate and stimulant use (Pagliaro & Pagliaro, 2012). The NM-ASSIST takes 5–10 minutes to administer and has been validated as an efficient and effective screening tool for substance use in criminal justice settings (Holmwood, Marriott, & Humeniuk, 2008; Wolff & Shi, 2015). Timeframe for the NM-ASSIST focuses on the past 3 months, but was modified for this study to include the 3 months before incarceration. The NM-ASSIST is easily scored for each substance yielding a Substance Involvement (SI) score ranging from 0 to 39, with higher scores being indicative of higher degree of drug use severity (scores 4+ indicate moderate need for drug use intervention).
Incarceration history
Incarceration history was primarily examined by the self-reported number of times incarcerated (in any correctional facility including prisons, jails, and lock-ups) as an adult.
Covariates
The following covariates were included to understand their role in the relationship between drug use and incarceration history: 1) High-risk home environment as measured by three binary (yes/no) variables, including having family members with drug abuse problems, the presence of drug use in respondent’s home, and whether or not the participant has lost custody of any of her children; 2) Partner relationships including a continuous measure of number of lifetime male sex partners and a binary measure of having a main partner who injected drugs (yes/no); and 3) Mental health including endorsing symptoms (binary variable yes/no) consistent with depression, anxiety, and post-traumatic stress using the GAIN (Global Appraisal of Individual Needs, Dennis et al., 2008), as well as self-reported experience of victimization/violence (yes/no), and if applicable, a continuous measure of age when victimization first occurred.
Procedure
This study used random sampling to recruit a sample of hard-to-reach, out-of-treatment, rural drug-using women in Appalachia from three local area jails. The jail daily census varies, as does the offense type (e.g., more alcohol and drug related weekend offenses). Therefore, recruitment dates were randomized monthly at each of the three rural jails. On each targeted recruitment day, research staff worked closely with jail administrators to access the daily census sheet for the names of potential study participants living at the facility. Potential participants were included in the targeted recruitment sampling frame if they had at least 2 weeks to 3 months (as verified by jail records) to serve on their sentence. This time frame was selected in order to ensure that participants would be able to engage in all study activities prior to release.
All women who met this initial screening criterion had an equal opportunity of being selected for study screening. From this sampling frame, research staff then randomly selected (using Research Randomizer, www.randomizer.org) between 10 – 20 women for study screening each day (depending on the size of the jail facility).
Randomly selected women were invited to participate in a group screening session in a private, confidential room in the jail. While jail staff assisted in escorting women to the screening room, no jail staff or representatives from the criminal justice system were present during the screening sessions. The screening session included informed consent and a question/answer time with the research staff regarding study details. Interested participants were then asked to complete survey-based screening assessments including the NM-ASSIST, anticipated release dates from jail, their “home” county to ensure they were from an Appalachian area, and confirmation of interest to participate in the study. Screening surveys were examined on site, and women who met all study eligibility were asked to return for a face-to-face interview at the jail within 2 days of study screening.
During the study recruitment phase between December 2012 and August 2015, 900 women were randomly selected from the three target jails. Of those, 688 (76.4%) participated in the study screening sessions in the jails (101 refused to participate, and 111 were released early between random selection and screening). Among women who participated in screening, 248 (36%) did not meet study eligibility criteria due to the following reasons: not being released during the 2 week to 3 month time frame (n=203), not engaging in any risky sexual practices (n=15), not being from an Appalachian county (n=21), and not meeting study NM-ASSIST criteria for drug use (n=9). The majority (97%) of the women randomly selected from the jail and screened for the study met NM-ASSIST criteria for problematic substance use in need of intervention (score of 4+ on the ASSIST).
Of the 688 screened, 440 (64%) met all study criteria to participate in the baseline. Anticipating jail release dates proved to be challenging due to court proceedings, family arrangements for bail, and unavailable details about cases in records. Thus, despite screening for anticipated release date (both through jail records and self-report), 40 potential participants were released from jail prior to being scheduled for the baseline interview. The final study sample (N=400) participated in face-to-face interviews in a private room in each jail using Computer-Assisted Personal Interview (CAPI) software. Research staff were female interviewers from the local Appalachian area, and they were trained on jail facility policies and procedures by jail administrators prior to study implementation. Participants were paid $25 for the baseline interview, and all study screening and data collection procedures were approved by the university IRB and protected under a federal Certificate of Confidentiality.
Statistical analysis
To profile drug use among the randomly selected sample (objective 1), descriptive statistics were examined for the NM-ASSIST for 688 rural women who participated in the screening. Both mean scores and level of risk for each substance were examined. To describe the relationship between drug use and incarceration history (objective 2), bivariate associations were examined between the measure of incarceration history (the primary DV of interest) and NM-ASSIST scores using simple negative binomial regression for the N=400 who entered the study and completed a baseline interview. Bivariate associations between incarceration history, demographic measures and potential covariates (high-risk home environment, partner relationship, and mental health) were also examined using a series of negative binomial regressions. For objective 3, a multivariate regression model was used to examine drug use as a independent contributor to incarceration history while controlling for covariates. Specifically, negative binomial regression was used to estimate two specific models. Model 1 included the NM-ASSIST score and all the potential covariates which were significantly associated with the dependent variable of lifetime incarceration history at the .05 level or below in the bivariate analysis. For clarity and ease of interpretation, non-significant associations were removed from the final model. Exclusion of the non-significant variables did not appreciably change the model estimates. In addition, moderation analyses between NM-ASSIST and covariates (high-risk home environment, risky partner relationship, and mental health) were explored for their relationship with incarceration history in Model 2. Results of the multivariate regression model are reported including incident risk ratios (IRRs) and 95% confidence intervals. An alpha level of .05 was used for all statistical tests. Data analyses were conducted using Stata/SE version 13.0.
Results
NM-ASSIST screening
Substance Involvement (SI) scores were computed for seven of the nine drug categories of the NM-ASSIST for the 688 randomly selected women who participated in the study screening (See Table 1). Frequencies for inhalant (24.3%) and hallucinogen (26.7%) use were considerably lower than the other categories and not included in analysis. The highest mean NM-ASSIST SI score was calculated by examining the MAX value for any drug, and the mean score was 32.7 (sd=9.7), with a range of 4–39. Mean scores for prescription opioids in particular (26.5, sd=14.3) and categorical risk indicators (62.4% high risk) suggest that abuse of prescription opioids was the highest risk for these women. By comparison, the next highest NM-ASSIST mean SI score was for non-prescription sedatives/sleeping pills (M=19.7, sd=14.9), with less than half being in the high-risk category (41.6%).
Table 1.
Average NM-ASSIST SI scores and risk categories among randomly selected rural women in jails (N=688)
| Mean SI score | Low risk | Moderate risk | High risk | |
|---|---|---|---|---|
| Prescription opioids | 26.5 (sd=14.3) | 14.8% | 22.8% | 62.4% |
| Sedatives/Sleep Pills | 19.7 (sd=14.9) | 26.5% | 32.0% | 41.6% |
| Methamphetamine | 14.9 (sd=15.7) | 44.0% | 23.4% | 32.6% |
| Marijuana | 11.8 (sd=11.7) | 36.1% | 48.1% | 15.8% |
| Street Opioids1 | 10.0 (sd=14.7) | 62.4% | 16.3% | 21.4% |
| Cocaine | 8.9 (sd=12.2) | 55.1% | 31.1% | 13.8% |
| Prescription stimulants | 6.6 (sd=11.0) | 65.3% | 24.7% | 10.0% |
Note: Level of risk associated with different Substance Involvement Score: 0–3 Lower Risk; 4–26 Moderate Risk; 27+ High Risk.
It should be noted that “street opioids” in this analysis includes heroin.
Demographics and incarceration history
Among women meeting study eligibility criteria (N=400), baseline data indicated that participants were about 33 years old (M=32.8, SD=8.2, Range 18–61) and mostly white (99%), which is consistent with the race/ethnicity demographic in rural Appalachia (Pollard & Jacobsen, 2016). About a third of women were married (32.0%) and the majority (87.2%) reported having children. Participants completed 11.1 (SD=2.3) years of education and about a quarter (22.8%) were working 6 months before incarceration.
The average length of the current incarceration was 70.2 (sd=87.8) days with a median of 35 days and a range between 3 – 800 days. The majority of women were serving their current sentence for a drug or property related crime (55.8%) or serving time for a court related offense (such as a parole/probation violation – 30.1%). Participants were incarcerated an average of 6 times in their lifetime (sd=10.4, range 1–150, median= 4.0), and spent an average of 16.3 lifetime months incarcerated (sd=25.0, range <1–20, median=8.0).
Relationship between drug use and incarceration history
Bivariate analysis examined the association between the number of lifetime incarcerations in any correctional facility (primary DV of interest) and the highest overall NM-ASSIST SI score, as well as the other covariates --demographic characteristics, high-risk home environment, partner relationships, and mental health (See Table 3). At the bivariate level, higher NM-ASSIST scores were significantly associated with fewer lifetime incarcerations (p<.01).
Table 3.
Bivariate analysis of months of incarceration, substance use, and related correlates (N=399)*
| Number of times incarcerated IRR (S.E) |
|
|---|---|
| NM-ASSIST highest SI score | .99 (.01)** |
| Demographics | |
| Age | 1.03 (.01)*** |
| Education | .89 (.02)*** |
| Full or part-time employed | .77 (.09)* |
| Married | 1.00 (.10) |
| Average income in 6 months before jail | 1.00 (2.63) |
| High-risk environment | |
| Number of days in 6 months before incarceration other people used drugs where they were living |
1.00 (.00)*** |
| Has had blood relatives with drug use problems |
1.38 (.16)** |
| Ever lost custody of any children | 1.46 (.15)*** |
| Risky relationships | |
| Number of lifetime male sexual partners | 1.01 (.00)*** |
| Used drugs/alcohol before sex | 1.23 (.15) |
| Had a main partner who injected drugs | 1.26 (.12)* |
| Mental health | |
| Depression | 1.72 (.17)*** |
| Anxiety | 1.57 (.14)*** |
| PTSD | 1.54 (.15)*** |
| Ever experienced violence/victimization | 1.93 (.23)*** |
| Age when violence acts happened | .99 (.01) |
Note: IRR = Incident Rate Ratio
p<.05
p<.01
p<.001
Study covariates were also significantly associated with incarceration history including demographics (age, education, and employment). Specifically, older women had more lifetime incarcerations (IRR=1.03, p<.001), while more educated (IRR=.89, p<.001) and employed (IRR=.77, p<.05) women had fewer lifetime incarcerations. In addition, a high-risk home environment including having family members with drug problems (IRR=1.38, p<.01) and losing custody of children were also positively associated with lifetime incarcerations (IRR=1.46, p<.001).
Risky partner relationships were also significantly and positively associated with number of lifetime incarcerations including having more lifetime male sex partners (IRR=1.01, p<.001) and having a main partner who injects drugs (IRR=1.26, p<.05). Finally, poorer mental health, such as identifying symptoms consistent with depression (IRR=1.72, p<.001), generalized anxiety (IRR=1.57, p<.001), and PTSD (IRR=1.54, p<.001), as well as lifetime victimization experiences (IRR=1.93, p<.001) were significant, positive correlates of incarceration history.
Drug use as an independent correlate of incarceration history
A multivariate negative binomial regression model was used to examine drug use as an independent contributor to incarceration history while controlling for other covariates (see Table 4). As shown in Model 1, drug use was not significantly associated with incarceration history when other covariates were controlled. When holding covariates constant, age was positively associated with incarceration history (IRR=1.01, p<.05), and having more years of education was associated with fewer lifetime incarcerations (IRR=.95, p<.05). Women who had lost custody of any of their children had higher estimated lifetime incarceration rate, controlling for independent variables (IRR=1.30, p<.01). Mental health issues were also significant correlates among women endorsing criteria consistent with generalized anxiety (GAIN), the estimated rate of lifetime incarceration was increased by a factor of 1.30 (p<.01), holding covariates constant. Similarly, women with histories of victimization or violence had a higher estimated lifetime incarceration rate, net of covariates (IRR=1.42, p<.01). Finally, an increase in lifetime male sexual partners was associated increase in the rate of incarceration by a factor of 1.01 (p<.001), holding covariates constant.
Table 4.
Negative Binomial Regression of Incidence of Incarceration (N=399)
| Model 1 | Model 2 | |
|---|---|---|
| IRR (SE) | IRR (SE) | |
| NM-ASSIST | 1.00 (.00) | 1.01 (.01)* |
| Age | 1.01 (.01)* | 1.01 (.01) |
| Education | .95 (02)* | .95 (.02)* |
| Ever lost custody of any children (1 = Yes) | 1.30 (.13)** | 1.29 (.12) |
| GAIN Generalized Anxiety Disorder (1 = Yes) |
1.30 (.19)** | 1.22 (.12)* |
| Ever experienced violence/victimization | 1.42 (.19)*** | 1.45 (.19) |
| Number of lifetime male sexual partners | 1.01 (.00)*** | 1.02 (.00)*** |
| ASSIST x # of lifetime male sexual partners | 1.00 (.00)*** | |
| Likelihood Ratio Chi-Square | 108.87*** | 125.21*** |
| Pseudo R-Squared | .06 | .06 |
p<.05
p<.01
p<.001
As shown in Model 2, the only significant interaction effect was observed for the NM-ASSIST and male partners. Specifically, an observed increase in the number of lifetime male sexual partners had a stronger effect on the predicted instances of incarceration among women with lower and mid-range ASSIST scores, relative to those with high ASSIST scores (See Figure 1).
Figure 1.
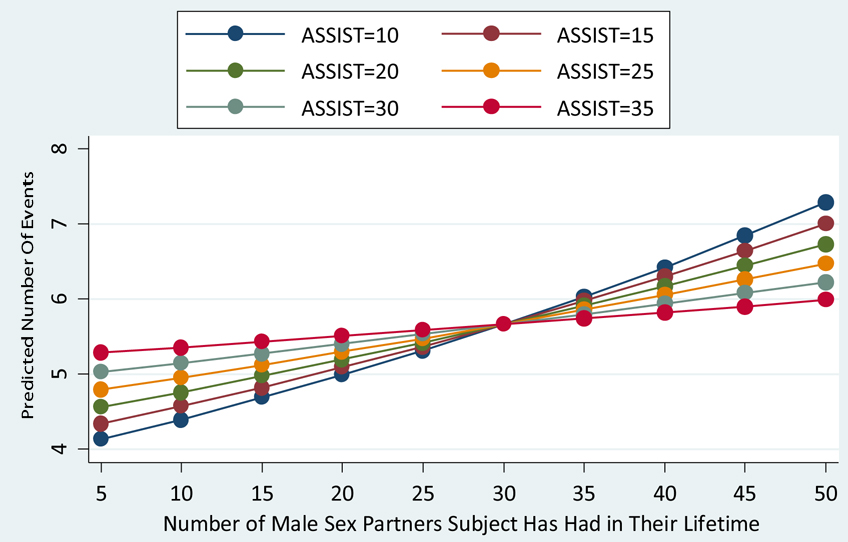
Predicted Instances of Incarceration by ASSIST and Number of Male Sex Partners
Discussion
This study utilizes rural jails to identify high-risk women drug users in rural Appalachia. The random selection design is an innovative approach to recruiting high-risk rural women drug users from real-world settings (jail) to better understand high-risk drug use practices, and increases external validity of study findings. Much of what we know about the commission of crime and characteristics associated with criminal offenders is based on research in urban areas (Weisheit, Falcone, & Wells, 2006). Conducting research in rural jails as places or venues to outreach to high-risk drug users is critical – not only because jails typically house a high volume of drug users (Karberg & James, 2005), but also because many of these individuals will never be identified as having a substance abuse problem or be engaged in treatment. The purpose of this study was to examine drug use and incarceration among rural women recruited from jail, as well as to understand factors that may contribute to the drug/crime relationship including high-risk environments, partner relationships, and mental health.
The first study objective was to profile drug use among a randomly selected group of rural women using the NM-ASSIST as a screening tool. Norms for the ASSIST have been established on more than 1000 individuals seeking primary care in seven countries, and the highest Substance Involvement (SI) scores of 7.0 for tobacco and 6.3 for alcohol, all other SI scores for illicit drug use fell below a mean of 3.0 (Humeniuk & Ali, 2006). With the prevalence of illicit drug use among criminal justice populations, it is not surprising that scores in this randomly selected sample of rural Appalachian women were considerably higher than primary care settings. However, of those randomly selected and screened for the study, 97% met NM-ASSIST criteria for moderate need of substance use intervention with a score of 4 or higher. In addition, the mean highest overall ASSIST SI score was 32.7, and about two-thirds of the sample fell in the “high risk” category for illicit use of prescription opioids. These findings are considerably higher for opiate use than previously reported in the literature, even among incarcerated individuals (Holmwood, Marriott, & Humeniuk, 2008; Wolff & Shi, 2015). This is also considerably higher than national trends for drug use among male and female jail inmates combined (Karberg & James, 2005; Wilson, 2000).
The second objective of this study was to examine the bivariate relationship between drug use and incarceration history. The range of incarceration time (between 3 −800 days) is likely attributed to the variation of arrests, which could range from first time arrests to persistent felony offenses. Rural women in this study were incarcerated an average of about 6 times, which is slightly lower than other samples of female offenders with substance abuse issues (ranging from 7.2 – 15.5), with most of the research focused in urban areas (Du et al., 2013; Grella & Greenwell, 2007; Lemieux, 2002). With consistent rates of problematic substance use, fewer arrests could be attributed to the protective nature of the rural environment where crime is generally less frequent and drug use tends to occur in tightly knit networks (Weisheit, Falcone, & Wells, 2006).
There was a significant relationship between NM-ASSIST scores and incarceration history, but findings were not in the anticipated direction. The relationship between drug use and criminality has been widely studied, with consistent findings for a positive relationship across male and female offenders (Horton, 2011; Peters et al., 1997; Staton-Tindall et al., 2007a; Staton-Tindall et al., 2007b). At the bivariate level, these findings suggested that higher NM-ASSIST scores were associated with fewer lifetime arrests. It is possible that age is an important factor, as shown in the multivariate models. It is also possible with the overall age of 33 for women in this study, that the escalation of substance abuse severity is more recent, and women may be on the forefront of their criminal careers – further strengthening the need for assessment and interventions in real-world settings like jails. However, due to the limitations of this cross-sectional dataset, future research should examine the causal linkages in terms of whether initiation of drug use leads to more criminal justice involvement, or whether involvement in the criminal lifestyle (e.g., drug trafficking) exacerbates problematic substance use.
This study also focused on other factors possibly related to drug use and incarceration among rural women. Specifically, covariates which were significant at the bivariate level were examined in a multivariate model to understand the relationship between drug use and incarceration history. It is interesting to note that when these covariates were added to the model, the negative relationship between NM-ASSIST scores and incarceration history was no longer significant. This finding highlights the importance of the complexity of the relationship between drug use and criminal involvement among rural women when other contextual factors are considered. Among rural women in this study, incarceration history was highly influenced by a number of demographic, relationship, and mental health factors.
Living in a high-risk home environment where family and friends use drugs, having relatives with drug use problems, and losing custody of children were significantly and positively associated with incarceration history for rural women at the bivariate level. This is consistent with other studies which suggest that stressful relationships are highly influential in women’s drug use and crime (Davey-Rothwell & Latkin, 2007; Falkin & Strauss, 2003; Pottieger & Tressell, 2000). However, considering the tight-knit kinship and social networks in rural areas (Beggs, Haines, & Hurlbert, 1996; Draus & Carlson, 2009; Keyes et al., 2014; Weisheit, Falcone, & Wells, 2006), having high-risk relationships where drug use is a part of the culture among family and peers may be even greater risk factors for rural women.
It should also be noted that in the multivariate model, losing custody of children remained a significant correlate of incarceration in the multivariate model. This is consistent with the literature which has suggested there is a relationship between caregiver arrests and negative child outcomes (Staton-Tindall, Sprang, & Clark, 2012). It is highly plausible that the drug use lifestyle may be characterized by behaviors indicative of parental risk, particularly neglect, that could increase the likelihood of child welfare system involvement. This is likely a significant factor in the increasing rate of grandparents raising their grandchildren due to the drug-use epidemic in Appalachia (Smith & Kounang, 2013). It is also recognized that this relationship may be bidirectional and should be further examined in future research.
Among these rural women, mental health was another significant factor related to incarceration history. Specifically, at the bivariate level, symptoms consistent with depression, generalized anxiety disorder, PTSD, and lifetime experiences of victimization/violence were each associated with increased incarcerations. However, in the multivariate model, only anxiety and victimization remained significant. The prevalence of mental health issues in general among incarcerated women has been well-documented (e.g., Gunter et al., 2012; Peters et al., 1997), as well as the prevalence of co-occurring mental health and substance abuse issues (Sacks, 2004; Staton-Tindall, Leukefeld, & Webster, 2003). Histories of victimization and violence among incarcerated women are also well-documented (e.g., Johnson et al., 2015; Radatz & Wright, 2015; Saxena, Messina, & Grella, 2014), and victimization has been noted as a factor distinguishing first time and repeat women offenders (Herbst, et al., 2016). Thus, these findings are fairly consistent with the broader literature for female offenders.
However, the relationship between anxiety, victimization, and incarceration histories among rural women has not been examined as extensively. For example, it is possible that among rural women, extreme poverty, limited access to resources, and limited behavioral health care resources (Oser et al., 2011; Oser et al., 2012) lead to anxiety that perpetuates involvement in a criminal lifestyle. It is also possible that living in a rural community may be associated with increased barriers to seeking treatment for victimization (Logan et al., 2004; Staton, et al., 2001; Weisheit, Falcone, & Wells, 2006), which could also lead to increased anxiety. The role of mental health in criminal activities should be a focus of future research, particularly as it relates to assessment and treatment opportunities in criminal justice settings.
Significant covariates were examined through a series of moderation analyses to further understand the relationship between drug use and incarceration history. The only significant interaction was between drug use (NM-ASSIST score) and having more lifetime male sexual partners on incarceration history. Specifically, the number of male sexual partners moderated the relationship between NM-ASSIST scores and lifetime incarcerations. An increased number of male sexual partners is perhaps a marker for high-risk sexual activity, which is consistent with other studies with incarcerated women (e.g., Fogel et al., 2014; Staton-Tindall et al., 2015). However, considering the importance of relationships, traditional gender roles, and close knit social networks in the Appalachian culture, it is feasible that more male sex partners may be a contributing factor in the relationship between drug use and crime among rural women. In addition, living in disadvantaged areas, particularly if the number of healthy and desirable partners is limited, has been associated with high-risk sexual practices (Ramaswamy & Kelly, 2015; Oser et al., 2016). While the significance of the interaction in this study may suggest that sexual activity with more partners contributes to drug use and crime among rural women, the complexity of drug use and high-risk sexual practices should be assessed in criminal justice venues more broadly for both rural and urban women. This assessment is critical not only for the potential increased risk for recidivism, but also for the health consequences associated with sexually transmitted diseases, HIV, or HCV.
This study has limitations. Women were randomly selected and recruited for the study from three purposefully selected rural Appalachian area jails. While this is an innovation, it limits generalizability to other substance-using women involved in the criminal justice system in urban areas. Also, findings may not be generalizable to other rural women since the target recruitment sites were in central Appalachia. While self-report is common in social and behavioral research and has been shown to be valid for substance use (Del Boca & Noll, 2000; Rutherford, et al., 2000), it is possible that self-report of sensitive information like drug use and criminal activities may lead to concerns related to social desirability response bias. Also, with regard to the approach, face-to-face interviews were conducted in a private room in each of the three jails with no correctional officers or others present, and a Certificate of Confidentiality was obtained to increase protections. However, it is possible that women were concerned about confidentiality in the jail environment. Finally, the study used data collected at the baseline interview, and the cross-sectional nature of the data could limit the understanding of the temporal nature of some of the findings, including the relationship between drug use and crime.
Despite limitations, this study makes an important contribution to understanding the drug/crime relationship among rural Appalachian women. Study findings suggest that while drug use is related to incarceration history, the drug/crime association is perhaps better explained for rural Appalachian women in a broader context that considers their high-risk home environment, partner relationships, and mental health. Specifically, in addition to drug use, factors such as family and child relationships, anxiety, victimization, and relationships with partners should also be considered in the trajectory of criminal careers among rural Appalachian women drug users. Considering the dearth of research on this high-risk population, the extreme health disparities, and limited services in rural Appalachia, these findings underscore the importance of outreach and intervention in real-world settings, including jails.
Table 2.
Demographics and incarceration history (N=399)*
| Percent/Mean (SD) | Range | |
|---|---|---|
| Number of times incarcerated | 5.9 (10.4), median=4 | 1–150 |
| Number of lifetime months incarcerated | 16.3 (25.00), median=8 | 1–20 |
| Length of current incarceration | 70.2 (87.8), median=35 | 3–800 |
| NM-ASSIST highest SI score | 32.7 (9.7), median=38 | 4–39 |
| Demographics | ||
| Age | 32.8 (8.2) | 18–61 |
| Highest grade of education completed | 11.1 (2.3) | 0–19 |
| Working full or part time in past 6 months |
22.8% | |
| Married | 32.0% | |
| Has children | 87.2% | |
| Average income in 6 months before jail | $8,467.2 ($18,558.9) | 0–$210,000 |
| High-risk environment | ||
| Number of days in 6 months before incarceration other people used drugs where they were living |
91.3 (86.7) | 0–180 |
| Has had blood relatives with drug use problems |
77.4% | |
| Ever lost custody of any children | 48.0% | |
| Risky relationships | ||
| Number of lifetime male sexual partners | 33.1 | 2–500 |
| Used drugs/alcohol before sex | 79.5% | |
| Had a main partner who injected drugs | 60.22% | |
| Mental health | ||
| Depression | 68.7% | |
| Anxiety | 45.4% | |
| PTSD | 67.6% | |
| Ever experienced violence/victimization | 80.2% | |
| Age when violence acts happened | 15.14 (7.8) | 1–50 |
Note: One case was dropped due to missing information on the DV
Acknowledgment
Research reported in this manuscript was supported by the National Institute On Drug Abuse of the National Institutes of Health under Awards R01DA033866 and K02DA035116. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We would also like to recognize the cooperation and partnership with the [state] Department of Corrections and the local jails participating in this study.
Footnotes
Declaration of Interest
The authors report no conflicts of interest.
Contributor Information
Michele Staton, University of Kentucky, College of Medicine, Department of Behavioral Science, 141 Medical Behavioral Science Bldg., Lexington, KY 40536
Gabriele Ciciurkaite, Department of Sociology, Social Work and Anthropology Utah State University, 0730 Old Main Hill, Logan, UT 84322-0730.
Carrie Oser, University of Kentucky, Department of Sociology, 1531 Patterson Office Tower, Lexington, KY 40508
Martha Tillson, University of Kentucky, Department of Behavioral Science, Center on Drug and Alcohol Research, 845 Angliana Ave, Lexington, KY 40502.
Carl Leukefeld, University of Kentucky, Department of Behavioral Science, Center on Drug and Alcohol Research, 111 Medical Science Building, Lexington, KY 40536
J. Matthew Webster, University of Kentucky, Department of Behavioral Science, Center on Drug and Alcohol Research 111 Medical Science Building, Lexington, KY 40536
Jennifer R. Havens, University of Kentucky, Department of Behavioral Science, Center on Drug and Alcohol Research 845 Angliana Ave, Lexington, KY 40502
References
- [APA] American Psychological Association (n.d.) The behavioral health care needs of rural women Retrieved August 14, 2011 from www.apa.org/pubs/info/reports/rural-women.pdf.
- Bennett KJ, Lopes JE, & Spencer K (2013). Rural women’s health. National Rural Health Association Policy Brief, January 2013 Retrieved July 30, 2016 from www.ruralhealthweb.org/index.cfm.
- [BJS] Bureau of Justice Statistics (2016). Local jail inmates and jail facilities. Office of Justice Programs Retrieved July 31, 2016 from http://www.bjs.gov/index.cfm?ty=tp&tid=12#data_collections.
- Beggs JJ, Haines VA, & Hurlbert JS (1996). Revisiting the rural-urban contrast: Personal networks in nonmetropolitan and metropolitan settings. Rural Sociology, 61(2), 306–325. [Google Scholar]
- Conrad KJ, Conrad KM, Dennis ML, Riley BB, & Funk R (2011). Validation of the Substance Problem Scale (SPS) to the Rasch Measurement Model, GAIN Methods Report 1.2 Chicago, IL: Chestnut Health Systems; Retrieved from http://www.gaincc.org/_data/files/Psychometrics_and_Publications/Working_Papers/Conrad_et_al_2011_SPS_Report.pdf [Google Scholar]
- Davey-Rothwell MA, & Latkin CA (2007) Gender differences in social network influence among injection drug users: Perceived norms and needle sharing. Journal of Urban Health, 84(5): 691–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Boca FK, & Noll JA (2000). Truth or consequences: The validity of self-report data in health services research on addictions. Addiction, 95, 347–360. [DOI] [PubMed] [Google Scholar]
- Dennis ML, White MK, Titus JC, & Unsicker JI (2008). Global Appraisal of Individual Needs: Administration Guide for the GAIN and Related Measures Chestnut Health Systems; Bloomington, IL [Google Scholar]
- Draus P & Carlson RG (2009). Down on main street: Drugs and the small-town vortex. Health & Place, 15, 247–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du J, Huang D, Zhao M, & Hser YI (2013). Drug-abusing offenders with co-morbid mental disorders: Gender differences in problem severity, treatment participation, and recidivism. Biomedical and Environmental Science, 26(1), 32–39. [DOI] [PubMed] [Google Scholar]
- Epperson MW, Khan MR, Miller DP, Perron BE, El-Bassel N, & Gilbert L (2010). Assessing criminal justice involvement as an indicator of human immunodeficiency virus risk among women in methadone treatment. Journal of Substance Abuse Treatment, 38, 375–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estep B (2016). Drug overdose deaths climb to record level in Kentucky Retrieved July 3, 2016 from kentucky.com/news/state/article83770067.html.
- Falkin GP, & Strauss SM (2003). Social supporters and drug use enablers: A dilemma for women in recovery. Addictive Behaviors, 28, 141–155. [DOI] [PubMed] [Google Scholar]
- Fogel CI, Gelaude DJ, Carry M, Herbst JH, Parker S, Scheyette A, & Neevel A (2014). Context of risk for HIV and sexually transmitted infections among incarcerated women in the south: Individual, interpersonal, and societal factors. Women’s Health, 54(8): 694–711. [DOI] [PubMed] [Google Scholar]
- Foxall K (2000). Rural life holds particular stressors for women. APA Monitor, 31(11), 30. [Google Scholar]
- Friedman P (2003). Meeting the challenge of social service delivery in rural areas. Welfare Information Network, 7(2). Retrieved July 1, 2016 from http://www.wkkf.org/news-and-media/article/2004/02/meeting-the-challenge-of-social-service-delivery-in-rural-areas. [Google Scholar]
- Grella CE & Greenwell L (2007). Treatment needs and completion of community-based aftercare among substance-abusing women offenders. Women’s Health Issues, 17, 244–255. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Back SE, Lawson K, & Brady KT (2010). Substance abuse in women. The Psychiatric Clinics of North America, 33(2), 339:355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunter TD, Chibnall JT, Antoniak SK, McCormick B, & Black DW (2012). Relative contributions of gender and traumatic life experience to the prediction of mental disorders in a sample of incarcerated offenders. Behavioral Science Law, 30, 615–630. doi: 10.1002/bsl.2037. [DOI] [PubMed] [Google Scholar]
- Herbst JH, Branscomb-Burgess O, Gelaude DJ, Seth P, Parker S, & Fogel CI (2016). Risk profiles of women experiencing initial and repeat incarcerations: Implications for prevention programs. AIDS Education & Prevention: 29(4): 299–311. doi: 10.1521/aeap.2016.28.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmwood C, Marriott M, & Humeniuk R (2008). Substance use patterns in newly admitted male and female South Australian prisoners using the WHO-ASSIST (Alcohol, Smoking and Substance Involvement Screening Test). International Journal of Prisoner Health, 4(4): 198–207. [DOI] [PubMed] [Google Scholar]
- Horton A (2011). Heroin users: The need for improved treatment for incarcerated women. Social Work Public Health, 26, 176–188. 10.1080/19371910903182773. [DOI] [PubMed] [Google Scholar]
- Humeniuk R & Ali R (2006). Validation of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and Pilot Brief Intervention: A Technical Report of Phase II Findings of the WHO ASSIST Project WHO Press: Geneva, Switzerland: Retrieved June 30, 2016 from http://www.who.int/substance_abuse/activities/assist/en/index.html. [Google Scholar]
- Johnson H (2006). Drug use by incarcerated women offenders. Drug and Alcohol Review, 25, 433–437. [DOI] [PubMed] [Google Scholar]
- Johnson JE, Peabody ME, Wechsberg WM, Rosen RK, Fernandes K, & Zlotnick C (2015). Feasibility of an HIV/STI risk-reduction program for incarcerated women who have experienced interpersonal violence. Journal of Interpersonal Violence, 30(18): 3244–3266. doi: 10.1177/0886260514555013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karberg & James (2005). Substance Dependence, Abuse, and Treatment of Jail Inmates, 2002 Bureau of Justice Statistics, US Department of Justice; Publication # 209588. [Google Scholar]
- Keyes KM, Cerdá M, Brady JE, Havens JR, & Galea S (2014). Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health, 104(2), e52–e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KY Office of Drug Control Policy (2015). 2015 Overdose fatality report. KY Office of Drug Control Policy Retrieved June 8, 2017 from http://odcp.ky.gov/Pages/Overdose-Fatality-Report.aspx.
- Lemieux CM (2002). Social support among offenders with substance abuse problems: Overlooked and underused? Journal of Addictions & Offender Counseling, 23, 41–57. [Google Scholar]
- Logan TK, Stevenson E, Evans L, & Leukefeld C (2004). Rural and urban women’s perceptions of barriers to health, mental health, and criminal justice services: implications for victim services. Violence & Victims, 19(1):37–62. [DOI] [PubMed] [Google Scholar]
- Macdonald M (2013). Women prisoners, mental health, violence and abuse. International Journal of Law Psychiatry, 36, 293–303. 10.1016/j.ijlp.2013.04.014. [DOI] [PubMed] [Google Scholar]
- McNeely J, Strauss SM, Rotrosen J, Ramautar A, & Gourevitch MN (2016). Validation of an audio computer-assisted self-interview (ACASI) version of the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) in primary care patients. Addiction, 111(2): 233–244. doi: 10.1111/add.13165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minton TD, Ginder S, Brumbaugh SM, Smiley-McDonald H, Rohloff H (2015). Census of jails: Population changes, 1999–2013 US Department of Justice: Bureau of Justice Statistics; Retrieved July 23, 2016 from http://www.bjs.gov/content/pub/pdf/cjpc9913.pdf. [Google Scholar]
- Mullings JL, Pollock J, & Crouch BM (2002). Drugs and criminality. Women & Criminal Justice, 13 (4): 69–96. 10.1300/J012v13n04_05 [DOI] [Google Scholar]
- Mumola CJ & Karberg JC(2007). Drug Use and Dependence, State and Federal Prisoners, 2004 Washington, DC: US Dept. of Justice, January, 2007. [Google Scholar]
- [NIDA] National Institute on Drug Abuse. (2009) NIDA Modified-ASSIST Retrieved October 20, 2010 from http://www.drugabuse.gov/nidamed/screening/.
- Oser C, Harp K, O’Connell D, Martin S, & Leukefeld C (2012). Correlates of participation in self-help groups as well as voluntary and mandated substance abuse treatment among rural and urban probationers. Journal of Substance Abuse Treatment, 42(1), 95–101. PMC3218255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oser C, Leukefeld C, Staton Tindall M, Garrity T, Carlson R, Falck R, Wang J, & Booth B (2011). Rural drug users: Factors associated with substance abuse treatment utilization. International Journal of Offender Therapy and Comparative Criminology, 55(4), 567–586. PMC2923294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oser C, Pullen E, Stevens-Watkins D, Perry B, Staton-Tindall M, Havens J, & Leukefeld C (2016). African American women and sexually transmitted infections: The perception of the contextual influence of unbalanced sex ratios and individual risk behaviors. In press, Journal of Drug Issues [DOI] [PMC free article] [PubMed]
- Pagliaro LA & Pagliaro AM (2012). Handbook of child and adolescent drug and substance abuse: Pharmacological, developmental, and clinical considerations John Wiley & Sons, Inc: Hoboken, NJ. [Google Scholar]
- Peters RH, Strozier AL, Murrin MR, & Kearns WD (1997). Treatment of substance-abusing jail inmates. Examination of gender differences. Journal of Substance Abuse Treatment, 14, 339–349. [DOI] [PubMed] [Google Scholar]
- Porter ND (2013). The state of sentencing 2012: Developments in policy and practice Retrieved June 30, 2016 from http://www.sentencingproject.org/wp-content/uploads/2016/01/State-of-Sentencing-2012.pdf.
- Pottieger AE, & Tressell PA (2000). Social relationships of crime-involved women cocaine users. Journal of Psychoactive Drugs, 32(4): 445–460. 10.1080/02791072.2000.10400246. [DOI] [PubMed] [Google Scholar]
- Radatz DL, & Wright EM (2015). Does polyvictimization affect incarcerated and non-incarcerated adult women differently? An exploration into internalizing problems. Journal of Interpersonal Violence, pii: 0886260515588921. [DOI] [PubMed] [Google Scholar]
- Ramaswamy M, & Kelly PJ (2015). Sexual health risk and the movement of women between disadvantaged communities and local jails. Behavioral Medicine, 41(3): 115–122. doi: 10.1080/08964289.2015.1024602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutherford MJ, Cacciola JS, Alterman AI, McKay JR, & Cook TG (2000).Contrasts between admitters and deniers of drug use. Journal of Substance Abuse Treatment, 18, 343–348. [DOI] [PubMed] [Google Scholar]
- Sacks JY (2004). Women with co-occurring substance use and mental disorders (COD) in the criminal justice system: A research review. Behavioral Sciences & the Law, 22, 449–466. [DOI] [PubMed] [Google Scholar]
- Saxena P, Messina N, & Grella CE (2014). Who benefits from gender responsive treatment? Accounting for abuse history on longitudinal outcomes for women in prison. Criminal Justice & Behavior, 41(4): 417–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith S, & Kounang N (2013). Prescription drugs ‘orphan’ children in eastern Kentucky Retrieved June 30, 2016 from http://www.cnn.com/2012/12/14/health/kentucky-overdoses/.
- Staton M, Leukefeld C, & Logan TK. (2001). Health service utilization and victimization among incarcerated female substance users. Substance Use & Misuse 36(6–7):701–16. [DOI] [PubMed] [Google Scholar]
- Staton M, Leukefeld C, & Webster JM (2003). Substance use, health, and mental health: Problems and service utilization among incarcerated women. International Journal of Offender Therapy and Comparative Criminology, 47(2), 224–239. [DOI] [PubMed] [Google Scholar]
- Staton Tindall M, Duvall JL, Leukefeld C, & Oser CB (2007). Health, mental health, substance use, and service utilization among rural and urban incarcerated women. Women’s Health Issues, 17(4), 183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staton-Tindall M, Royse D, & Leukefeld C (2007). Substance use, criminality, and social support: An exploratory analysis with incarcerated women. American Journal of Drug & Alcohol Abuse, 33(2), 237–243. [DOI] [PubMed] [Google Scholar]
- Staton-Tindall M, Duvall J, McNees E, Walker R & Leukefeld C (2011). Outcomes following prison and jail-based treatment among women residing in metro and non-metro communities following release. Journal of Drug Issues, 41(2), 197–216. [Google Scholar]
- Staton-Tindall M, Webster JM, Oser CB, Havens JR, & Leukefeld CG (2015). Drug use, hepatitis C, and service availability: Perspectives of incarcerated rural women. Social Work in Public Health, 30(4): 385–396. 10.1080/19371918.2015.1021024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staton-Tindall M, Sprang G, & Clark J (2012). Caregiver drug use and arrest as correlates of child trauma exposure. Journal of Evidence-Based Social Work 9:3,265–282. 10.1080/15433714.2010.494982. [DOI] [PubMed] [Google Scholar]
- Suryaprasad AG, White JZ, Xu F, Eichler B, Hamilton J, Patel A,… Holmberg SD (2014). Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006–2012. Clinical Infectious Diseases, 59(10), 1411–1419. [DOI] [PubMed] [Google Scholar]
- Tjaden K (2015). Health disparities between rural and urban women in Minnesota. Minnesota Medicine, 98(10): 40–43. [PubMed] [Google Scholar]
- Webster JM, Rosen PJ, Smiley McDonald H, Staton-Tindall M, Garrity TF, & Leukefeld CG (2007). Mental health as a mediator of gender differences in employment barriers among drug abusers. The American Journal of Drug and Alcohol Abuse, 33(2), 259–265. [DOI] [PubMed] [Google Scholar]
- Weisheit RA, Falcone DN, & Wells LE (2006). Crime and policing in rural and small-town America Waveland Press, Inc: Long Grove, IL. [Google Scholar]
- [WHO] World Health Organization (2002). WHO ASSIST Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction, 97 (9): 1183–1194. [DOI] [PubMed] [Google Scholar]
- Wilson DJ (2000). Drug use, testing, and treatment in jails US Department of Justice, Bureau of Justice Statistics Special Report. NCJ 17999; Retrieved August 2, 2016 from http://www.bjs.gov/content/pub/pdf/duttj.pdf. [Google Scholar]
- Wolff N, & Shi J (2015). Screening for substance use disorder among incarcerated men with the Alcohol, Smoking, Substance Involvement Screening Test (ASSIST): A comparative analysis of computer-administered and interviewer-administered modalities. Journal of Substance Abuse Treatment, 53: 22–32. doi: 10.1016/j.jsat.2015.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AM & Havens JR (2012). Transition from first illicit drug use to first injection drug use among rural Appalachian drug users: A cross sectional comparison and retrospective survival analysis. Addiction, 107(3):587–96. doi: 10.1111/j.1360-0443.2011.03635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AM, Havens JR, & Leukefeld CG (2010). Route of administration for illicit prescription opioids: A comparison of rural and urban drug users. Harm Reduction Journal, 15:7–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AM, Larian N, & Havens JR (2014). Gender differences in circumstances surrounding first injection experience of rural injection drug users in the United States. Drug & Alcohol Dependence, 134, 401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zibbell JE, Iqbal K, Patel RC, Suryaprasad A, Sanders KJ, Moore-Moravian L, Serrecchia J, Blankenship S, Ward JW, & Holtzman D (2015). Increases in hepatitis C virus infection related to injection drug use among persons aged ≤30 years – Kentucky, Tennessee, Virginia, and West Virginia, 2006–2012. Centers for Disease Control and Prevention: Morbidity and Mortality Weekly Report, 64(17), 453–454. [PMC free article] [PubMed] [Google Scholar]


