Abstract
Objective
Our objective was to identify the factors that impact mental health service use among American Indian (AI) older adults living in South Dakota compared to their White counterparts.
Design and Methods
Using a cross-sectional design with 735 participants (n = 502 Whites, n = 233 AIs), we used ordinal regressions to analyze the extent to which predisposing, need, and enabling/hindering factors predicted the level of mental health service utilization.
Results
White older adults used more mental health services as compared with AI older adults. For both groups, more adverse childhood experiences along with prior negative experience with mental health service use were significantly related to an increased level of mental health service use. Compared to their White counterparts, AI older adults who reported a higher level of depressive symptoms, better self-perceived physical health, and a more positive attitude toward mental health services tended to use more mental health services.
Conclusions
To reduce mental health disparities among AI older adults, community, local government, and academic partners should pay attention to how to encourage the use of mental health services to meet the unique needs of AI older adults.
Keywords: American Indians, Older adults, South Dakota, Mental health service use
Racial/ethnic disparities in mental health service use have increasingly captured national attention. Despite the profoundly debilitating effects of mental disorders in all populations, racial/ethnic minorities are less likely than Whites to access mental health services and to receive needed care [54]. Existing data indicate that American Indian and Alaska Native (AI/AN) populations disproportionately suffer from a range of mental health problems and are at greater risk for mental illnesses than other racial/ethnic groups [8, 30, 54], yet less is understood about the determinants AI/AN of mental health problems than other minority populations [30]. Moreover, when minority populations receive treatment, the care they receive is more likely to be of poor quality [54]. To reduce the notable gaps in access to mental health care, we examined factors associated with mental health service use in AI and White older adults. The current study is guided by the Gelberg et al. [28] behavioral health model that conceptualizes associations among predisposing, enabling and need factors, which may facilitate or deter service use, particularly for vulnerable populations.
AI/ANs, the Indigenous peoples of North and South America with cultural identification rooted in their tribal affiliations or community attachments, are among the U.S. nation’s fastest growing populations, constituting about 1.7% of the total US population (over 5.2 million) and increasing by 39% from the previous Census [67]. AI/ANs are composed of extremely heterogeneous groups of more than 567 federally recognized tribes (each with sovereign political status), each with its own language, cultural traditions and customs, and historical context [40, 67]. In comparison with other minority groups, AI/ANs have the highest rate of serious psychological distress (nearly 1.5 times the rate of the general population), which may result in elevated risks for disability, and concomitantly, more health service use [3]. A primary mental health challenge reported by AI/ANs includes depression, one of the leading causes of suicide and mortality [2, 8, 30, 52]. In fact, the AI/AN suicide rate is 1.7 times higher than that of the general U.S. population, and, among older adults, the life expectancy is 4.4 years less than the US “all races” population (73.7 years and 78.1 years, respectively) [40].
Older adults are particularly vulnerable to psychological distress and unmet mental health needs [6, 27]. In particular, research consistently suggests that AI/AN older adults suffer more psychological distress than their White counterparts due to their experiences with the historical oppression and trauma related to colonization and subjugation and the associated numerous broken treaties, discrimination, poverty, and violence [10, 13, 65]. This historical oppression is exacerbated by the more limited psychological, social, and financial resources to cope with this stress than their White counterparts [10]. Distinct from their White counterparts, AIs often use culturally-traditional treatment approaches (traditional healers, [8, 30]). This greater historical oppression, stress, and limited resources contributes to higher rates of depression reported among this population. Indeed, according to Kramer [45], over 30% of AI/AN older adults visiting an urban Indian Health Services (IHS) outpatient medical facility reported significant depressive symptoms. This statistic is substantially higher than most published estimates of the prevalence of depression among older Whites with chronic illnesses (9–31%) ([49], cited in [27]). In another clinic-based examination, the National Institute of Mental Health [54] (2001) indicated that nearly 20% of AI/AN elders who received primary care reported significant psychiatric symptoms, with rates increasing as a function of age. Strikingly, the number of AI/AN elders with depression is expected to nearly quadruple to 81,702 cased by 2050 (in comparison with 20,950 cases reported in 2010 [27]).
However, despite the severity of mental health challenges, very low rates of mental health service use tend to be reported for older adult AI/AN populations, acknowledging some variation in help-seeking rates across gender, tribe, and region [50, 58]. In addition, when seeking professional help, many AI/AN older adults may experience discomfort and cultural incongruence with the available providers and treatment methods, making treatment attrition salient [35, 64].
A number of factors have been identified to explain the under-utilization of mental health service among AI/AN elders. Mounting evidence has suggested that Indigenous people’s concepts and expressions of mental illness are different from those of the dominant culture [32]. AI/AN cultures emphasize the balance of mind, body, and spirit, with a focus on a holistic approach to healing, making little distinction between mental and physical health [3, 32, 38]. Such beliefs and attitudes may, in turn, lead AI/AN older adults to turn to traditional health practices or spiritual healers rather than formal mental health care providers [8, 70, 73]. Preliminary evidence has suggested that approximately 34 to 49% of AI/ANs with diagnosed behavioral disorders sought help from traditional healers and that 16 to 32% of AI/ANs using biomedical services for emotional problems had also used a traditional healer [8]. Similarly, in a more recent study on beliefs about mental health treatment among adult anxious primary care patients, Hunt et al. [39] found that, in comparison to other racial/ethnic groups (African-Americans, Hispanics, Asian-Americans, and Whites), AI/AN adult primary care patients were least likely to be convinced about the benefits of psychotherapy, believing that one in three persons with mental illness would recover without treatment. Mental health service use among AI/AN older adults is further complicated by the stigma attached to mental illness, mental health beliefs, and preferred treatment modalities.
Despite the rapid growth of the nation’s elderly populations and persistent disparities in AI/AN mental health service use, little is known about the racial/ethnic, cultural, and attitudinal factors affecting the gaps in mental health service utilization, particularly among AI/AN older adults in a rural area [27, 61]. Race/ethnicity and culture inextricably shape beliefs, attitudes, and expression of symptoms, and hence have a significant impact on the types of mental health services accessed [50]. Thus, factors that may facilitate or deter people from utilizing mental health care may vary across racial/ethnic groups. Although there is a considerable literature on determinants of mental health care use among African Americans (i.e., a higher level of education, being female, having cooccurring mental and substance disorders, experiencing a mental health episode in the past 12 months, and large social networks [53, 66], scarce attention has been paid to mental health service use and the needs of AI/ANs [30].
Given the urgent need to reduce racial/ethnic disparities in mental health services, we examined factors associated with mental health service use in AI and White older adults, exploring similarities and differences in determinants between the two groups. To the best of our knowledge, this is one of the few efforts to date to compare factors affecting the utilization of mental health service in a rural sample of AI and White older adults. Our contribution to the understanding of facilitators of or barriers to mental health service utilization will aid researchers and clinicians alike in developing culturally relevant interventions and helping to ensure adequate access to mental health care to meet the needs of this often-invisible population.
Conceptual Framework
Based on Andersen’s [5] behavioral model for health care utilization, Gelberg et al. [28] proposed a revised and expanded behavioral model for vulnerable populations, which explicates elatively comprehensive guidelines for conceptualizing the relationships between the multiple explanatory factors associated with service utilization. Gelberg et al.’s model has been extensively applied to studies of diverse racial/ethnic populations, including AI/ANs (e.g., [14, 60]. This model categorizes the determinants of health service utilization into the following three components: (a) predisposing; (b) need for service; and (c) enabling factors. The next sections provide an overview of such factors as relevant to our research [28].
Predisposing Factors
Although they are not directly responsible for service use, predisposing factors (e.g., age, gender) represent demographics, which may affect one’s proclivity toward using mental health services. Age and gender are two of the most widely used variables that may predispose an individual to use or to not use services. Researchers generally have found lower rates of mental health service use among older adults and males as compared to their younger and female counterparts ([7, 41]; Roh et al. 2017; [71]). Nonetheless, the directions of these associations vary substantially depending on study populations, sample characteristics, and the research methods used. For example, in a study of health service use in Canada and the US, the younger women cohort aged 18 to 44 were found to be more likely to contact a doctor than those participants in the older women cohort, and women aged 45 to 64 had lower odds of being hospitalized than younger women or women older than 64 [9]. In the same study, men aged 45 to 64 had higher odds of being hospitalized than men younger than 45 or men older than 64.
The revised and expanded behavioral model for vulnerable populations [28] includes not only existing demographics and conditions which may influence health/illness and health service use, but also social structure, sexual orientation and childhood characteristics. In particular, they suggest that childhood characteristics (e.g., abuse and neglect history) are predisposing factors, which influence enabling (e.g., personal resources) and need factors (e.g., perceived health), along with health behavior and services use.
For the purpose of this study, we explored adverse childhood experience (ACE) as variables of particular relevance to AI mental health, particularly given the elevated rates of trauma experienced by AIs across the life course [21]. Indeed, available data indicate elevated rates of child maltreatment [48], domestic violence [21], alcohol abuse and other forms of addiction [36, 47], and incarceration [22] in many AI communities. Childhood maltreatment and adverse experiences are key public mental health issues, particularly due to their devastating impacts which often persist into adulthood [4, 20]. ACE includes child abuse (i.e., psychological/emotional, physical, or sexual) and neglect, dysfunctional household dynamics (e.g., witnessing domestic violence, substance abuse in the home), and criminal behaviors in the household. ACE has been found to be associated with negative mental health outcomes, including depression and PTSD [23], an elevated risk of suicide [19, 23], and violence [74]. Consequently, many AI children may experience the psychological and social impacts of exposure to high rates of violence, substance use, and/or mental health challenges across the life course. It is conceivable that such traumatic experiences in childhood are likely to increase AIs’ risk for negative mental health outcomes as (older) adults, consequently increasing their need for mental health services. However, research on ACE and mental health service use among AI older adults is virtually nonexistent.
Need Factors
Factors related to need for service reflect both the perceived and actual need for health care services. Such factors may include an individual’s’ perceived or actual physical health as well as behavioral health factors, such as depressive symptoms. Numerous researchers have documented a significant association between depressive symptoms (i.e., need) and an increased likelihood of mental health service use [26, 31, 41, 56, 57]. Perceived health is also indicative of a need for services and is often influenced by an individual’s past treatment experience and knowledge of health services. While specific diagnoses of health status (e.g., diabetes, hypertension, chronic diseases) tend to lead to much higher service use, perceived physical health is another factor which can result in a higher service utilization [1, 7, 12, 16]. However, research on the relationship between perceived physical health and use of mental health service among older AIs is lacking.
Enabling/Hindering Factors
Enabling/hindering factors in the revised and expanded model include a variety of elements that facilitate or hinder mental health service use, including personal/family resources (e.g., income as financial resources, perceived barriers to care) and community resources (e.g., health service resources). For the purpose of this study, we were particularly interested in several variables that addressed the unique sociocultural characteristics pertinent to AI communities, such as stigma, prior negative experience with mental health services, knowledge of depression, and attitudes toward mental health services. Stigma attached to mental illness and seeking psychological help often prevents AI older adults from accessing the mental health service they need [32, 59, 68]. Attitudes toward mental health services and beliefs about mental illness are also an integral element in models of service utilization.
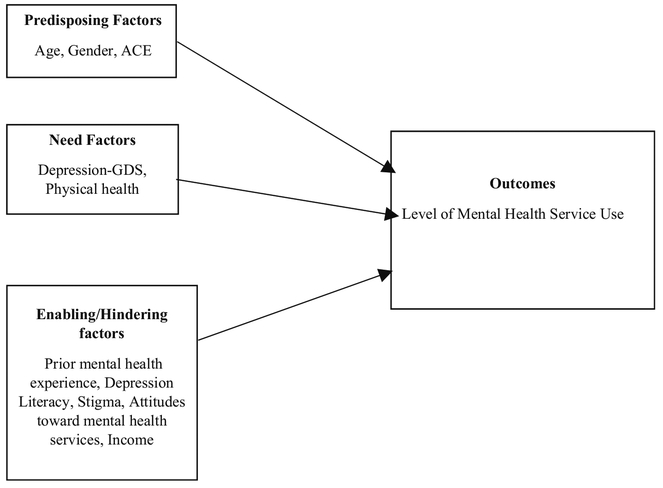
An individual’s knowledge (or absence of knowledge) about depression and mental health serves is an important factor in shaping their decisions about service utilization [15]. Research suggests that a lack of knowledge tends to result in negative attitudes about mental illness and a reduction in help-seeking behaviors [63]. Likewise, a prior negative experience with mental health services is likely to influence subsequent treatment behaviors and to result in a decrease in willingness to seek professional help [34, 37]. Finally, we included income as an enabling factor for service utilization. Figure 1 displays our conceptual model, depicting key factors relating to the predisposing (i.e., age, gender, and ACE), need (i.e., depressive symptoms, physical health), and enabling (i.e., income, prior mental health experiences, depression literacy, stigma, and attitudes toward mental health services) constructs.
Fig. 1.
Conceptual framework of factors associated with the level of mental health service use
The aforementioned predisposing, need, and enabling factors are likely to affect mental health service use among AI older adults. Building upon previous research, our purposes were (1) to explore racial/ethnic differences in mental health service utilization; (2) to examine the predisposing, need, and enabling factors that predict mental health service use by different racial/ethnic groups; and (3) to examine the predisposing, need, and enabling factors that predict mental health service use excluding non- physician health care use and non-physician health care use. A more complete understanding of the factors that influence mental health service use in AI older adults may guide intervention efforts aimed at facilitating access to mental health care and reducing racial/ethnic disparities in service utilization.
Method
Data Source
We used a cross-sectional design with self-administered surveys with a convenience sample of 755 rural and urban adults (ages 50+ years) in South Dakota. After obtaining approval from the Institutional Review Board at the University of South Dakota, data collection took place between January 2013 and May 2013. Participants were recruited from a variety of venues, including local churches, restaurants, social service centers, senior housing facilities, senior centers, food pantries and three pow wows (specifically, Sundance, which is an annual event). Inclusion criteria for participants included being age 50 years or older and being free of cognitive impairments. For the purpose of this analysis, due to the small sample sizes of certain racial groups, we excluded African Americans (n = 6), Hispanics (n = 5), Asian Americans (n = 2), and others (n = 1) and missing cases in race (n = 6), leaving 735 (502 Whites, 233 AIs). All participants provided informed written consent before the interview. Although the survey questionnaires were designed to be self-administered, college students trained as interviewers were available to assist anyone who needed help; five participants needed such assistance. The survey took about 30 min to complete, and respondents were paid $10 cash for their participation.
Measures
Dependent Variables
Mental Health Service Use
The five survey questions asked participants about any mental health service use: BDuring the past 12 months, have you visited a physician (e.g., family physician, gynecologist, urologist, cardiologist)”; “…have you visited a non-physician health care provider (e.g., herbalist, Native traditional healer, minister)”; “..received a mental health professional service (e.g., a social worker, psychologist, psychiatrist, psychiatric nurse practitioner)”; “…gone to the emergency room; and had inpatient hospitalization for mental health problems.” Responses were coded dichotomously: “yes” (1) vs. “no” (0). We summed responses for the total scores of the level of mental health service use (which ranged from 0 to 5), and the total scores of the level of mental health service use excluding non-physician health care use, with higher scores being indicative of a higher level of mental health service use (α = .612, α = .63, respectively). Also the individual item of these five questions (B…have you visited a non-physician health care provider (e.g., herbalist, Native traditional healer, minister) was used for an additional analysis.
Predisposing Factors
Demographic Variables
Age (in years) and gender (1 = female, 0 = male) were included.
Adverse Childhood Experiences
ACE was defined as any exposure to traumatic situations, chronic stressors, or specific traumatic events before the age of 18. Childhood adversity was measured using the ACE Questionnaire, which assesses 10 types of childhood adversity in three domains of childhood abuse: emotional, sexual, and physical abuse, physical neglect, and abuse associated with living in a dysfunctional household [23, 24]. Responses were coded as yes (1) or no (0). We summed responses for the total ACE score (which ranged from 0 to 10), with higher scores indicative of more adverse childhood experiences (α = .752).
Need Factors
Depressive Symptoms
We used the Geriatric Depression Scale-Short Form (GDS-SF) to assess the level of depression in the participants [75]. This 15-item measure captures a wide range of depressive symptoms (e.g., “Do you feel happy?”, “Do you feel your life is empty?”, “Are you in good spirits mostly?”) with a yes/no response format. Total scores (summed across questions) ranged from 0 to 15, with higher scores indicative of higher levels of depressive symptoms (α = .791).
Perceived Physical Health
Perceived physical health was assessed using the single question “how would you rate your overall general health at the present time?” Participants were asked to rate their health on a 4-point scale ranging from (1) “poor” to (4) “excellent.”
Enabling/Hindering Factors
Prior Mental Health Service Experience
We used a three-item questionnaire to assess participants’ experience about their level of access to health care (e.g., experienced treatment delay, delay in receiving mental health care, and perceived discrimination in receiving healthcare). Participants’ responses (“yes” = 1, “no” = 0) were then summed to create the total score (α = .70).
Depression Literacy
We used the Depression in Late Life Quiz [55] to assess individuals’ knowledge of depression. This scale consists of 12 items that ask about depression literacy. Items include: “It is normal for older people to feel depressed a good part of the time”, “There is a higher suicide rate among the elderly than among younger adults”, and “Health professionals often have difficulty diagnosing depression in the older person.” Although the original response format is “True”, “False”, and “I do not know”, we used a simple true/false response because a majority of the AI elders endorsed the “I do not know” response for many of the items during pilot testing. At .60, the internal consistency was relatively low, but this reflects the broad content area as well as variations in the difficulty of the items. We used the total number of correct answers in the analysis, with scores potentially ranging from 0 to 12.
Perceived Stigma
We measured stigma toward receiving psychological help with the Social Stigma for Receiving Psychological Help scale (SSRPH; [44]). The SSRPH was devised to evaluate individuals’ perceptions of how stigmatizing it is to receive professional psychological help. It consists of five items rated on a 4-point scale from (1) “strongly disagree” to (4) “strongly agree.” Scores from 12 to 20 indicate greater perception of social stigma associated with receiving professional psychological help; scores from 4 to 11 indicate less social stigma. A sample item is “people tend to like less those who are receiving professional psychological help” (α = .82).
Attitudes toward Mental Health Services
We adopted a 10-item version of the Attitudes Toward Seeking Professional Psychological Help Scale (ATSPPHS-SF; [25]) to assess individuals’ propensity to use mental health services. The scale includes five positive statements (e.g., “If I believed I was having a mental breakdown, my first inclination would be to get professional attention”, A person with an emotional problem is not likely to solve it alone; he or she is likely to solve it with professional help”) and five negative statements (e.g., “The idea of talking about problems with a psychologist strikes me as a poor way to get rid of emotional conflicts”,” A person should work out his or her own problems; getting psychological counseling would be a last resort”). Individuals were asked to rate each statement using a four-point scale ranging from 0 (“disagree”) to 3 (“agree”). We reverse-coded the responses to the negative statements (α = .752).
Income was included (1 = under $20,000 to 6 = $100,000 and over), and it was collapsed into three categories (less than $20,000; $20,000–$39,999; and $40,000 or more) due to small numbers in categories over $60,000.
Data Analysis
Pearson correlation coefficients assessed multicollinearity between study variables, and we used a cutpoint of r > .70 to indicate that multicollinearity was present. We did not find evidence of multicollinearity; the highest correlation (r = .456, p < .001) was between age and race. We used two-tailed independent t-tests and chi-square tests to assess whether AI and White older adults reported different results with respect to sociodemographic and other study variables. We used ordinal regressions with simultaneous entry of variables to investigate factors associated with the level of mental health service use (Table 3). Lastly, we used ordinal regressions to examine factors associated with the level of mental health services excluding the non-physician health care and binary logistic regression with the non-physician health care use among American Indians (Table 4).
Table 3.
Factors associated with the Level of Mental Health Service Use
| Factors | Level of Mental Health Service use (total) | Level of Mental Health Service use (Whites) | Level of Mental Health Service use (AIs) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | p | B | SE | β | p | B | SE | β | p | |
| Predisposing factors | ||||||||||||
| Age | −.207 | .059 | −.155 | .000 | −.010 | .003 | −.193 | .000 | −.015 | .006 | −.143 | .021 |
| Gender (female) | −.100 | .057 | −.074 | .078 | −.111 | .065 | −.094 | .088 | −.028 | .099 | −.017 | .781 |
| ACE | .060 | .015 | .183 | .000 | .054 | .020 | .149 | .007 | .045 | .021 | .140 | .036 |
| Need factors | ||||||||||||
| GDS | .039 | .012 | .151 | .001 | .021 | .015 | .088 | .156 | .077 | .020 | .264 | .000 |
| Perceived physical health | .406 | .176 | .095 | .022 | −.006 | .048 | −.008 | .893 | .239 | .073 | .212 | .001 |
| Enabling/hindering factors | ||||||||||||
| Prior negative experience with mental health service use | .455 | .064 | .302 | .000 | .219 | .101 | .116 | .031 | .588 | .084 | .439 | .000 |
| Knowledge of depression | .008 | .012 | .025 | .548 | .010 | .014 | .039 | .480 | .025 | .023 | .071 | .270 |
| Stigma | −.013 | .010 | −.061 | .166 | −.008 | .011 | −.042 | .472 | −.008 | .017 | −.031 | .646 |
| Attitudes toward mental health services | .011 | .005 | .103 | .017 | .006 | .005 | .069 | .220 | .030 | .009 | .202 | .001 |
| Income | −.183 | .057 | −.130 | .002 | −.174 | .068 | −.142 | .011 | −.208 | .101 | −.124 | .041 |
| R2 | .266 | .133 | .478 | |||||||||
| F(11, 477) = 15.322 p < .001 | F(10, 329) = 5.046 p <.001 | F(10, 150) = 13.751 p <.001 | ||||||||||
Notes. ACE indicates the Adverse Childhood Experiences Scale; GDS indicates the Geriatric Depression Scale-
Table 4.
Factors associated with level of mental health service use excluding the non- physician health care use and non-physician health care use among American Indian older adults
| Factors | Level of mental health service use excluding non- physician health care use | Non-physician health care use | ||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | β | p | Exp (B) | 95% C.I. | p | ||
| Predisposing factors | ||||||||
| Age | −.153 | .101 | −.095 | .132 | .573 | .231 | 1.424 | .231 |
| Gender | −.054 | .091 | −.037 | .554 | .455 | .187 | 1.107 | .083 |
| ACE | .045 | .020 | .156 | .024 | 1.278 | 1.070 | 1.526 | .007 |
| Need factors | ||||||||
| GDS | .059 | .018 | .232 | .002 | 1.074 | .922 | 1.253 | .359 |
| Perceived physical health | .503 | .241 | .134 | .038 | 1.691 | 1.180 | 1.891. | .646 |
| Enabling/hindering factors | ||||||||
| Prior negative experience with mental health service use | .524 | .076 | .449 | .000 | .971 | .459 | 2.054 | .940 |
| Knowledge of depression | .022 | .020 | .073 | .272 | 1.019 | .842 | 1.233 | .846 |
| Stigma | −.021 | .016 | −.089 | 184 | .960 | .830 | 1.11 | .585 |
| Attitudes toward mental health services | .021 | .008 | .164 | .010 | .974 | .906 | 1.048 | .485 |
| Income | −.116 | .093 | −.079 | .214 | .790 | .327 | 1.908 | .600 |
| R2 | .462 | |||||||
| F(10,156) = 12.535 p < .001 | X2 = 18.309, df = 10, p < .05 | |||||||
Notes. ACE indicates Adverse Childhood Experiences; GDS indicates Geriatric Depression Scale-
Results
Racial Differences in Predisposing, Need, and Enabling Factors
The descriptive analysis results appear in Table 1. The mean age of the AI and White participants was 60.69 (±8.41) and 72.06 (±11.08) years, respectively. Over half of each group was female and more than half of the study population had a high school education or less, with 68% of the White older adults (in comparison to approximately 51% of the AI older adults) falling into this category. Over one-third of the total sample earned less than $ 20,000 per year, with almost one-half of the AI population being low-income in comparison with approximately 33% of Whites. More than four-fifths of the total sample indicated they had insurance, with a significantly lower proportion (63%) of AIs having insurance versus 93% of White older adults. Finally, over one-third of the total sample were employed, with almost half (49%) of AI older adults employed, in comparison with 33% of White older adults. Almost half (46%) of the total sample were married, over half (51%) of Whites were married versus 36% of AI older adults. Thus, among demographic variables significant variation occurred between AI and White older adults.
Table 1.
Profile of Sample
| Characteristic | Race | |||
|---|---|---|---|---|
| Total Sample (N = 735) Mean (SD) or % | Whites (n = 502) Mean (SD) or % | American Indians (n = 233) Mean (SD) or % | p | |
| Age (years) | 68.41(11.59) | 72.06(11.08) | 60.69(8.41) | <.001 |
| Female gender | 64.4 | 69.1 | 54.3 | <.001 |
| High school or less Income | 62.8 | 68.2 | 50.7 | ns < 0.0–01 |
| Less than $20,000 | 37.9 | 33.4 | 46.7 | |
| $20,000–39,999 | 28.7 | 31.9 | 23.3 | |
| $40,000 or more | 33.4 | 35.5 | 30 | |
| Health insurance | 82.4 | 93.4 | 62.8 | <0.0–01 |
| Employed | 38.2 | 32.9 | 49.1 | <0.0–01 |
| Marital status | ns | |||
| Married | 46.1 | 50.7 | 36.4 | |
| Widowed | 24.2 | 30.1 | 12.1 | |
| Divorced | 16.5 | 13 | 22.5 | |
| Single (never married) | 9.5 | 5.8 | 17.7 | |
| Others | 3.8 | .4 | 11.2 | |
| ACE | 1.47(2.0) | .95(1.50) | 2.58(2.46) | <.001 |
Note. ACE indicates the Adverse Childhood Experience Scale
Statistically speaking, there were no significant differences between the AI and White participants with respect to education and marital status. However, compared with White older adults, AI older adults were younger on average (t (723) = −13.761, p < .001). White older adults tended to be more affluent (χ2 (5, N = 694) =17.23, p = .004), were more likely to have health insurance (χ2 (1, N = 731) = 108.762, p < .001), and were less likely to be employed (χ2 (1, N = 723) = 17.328, p < .001). Compared to White older adults, however, AI older adults had significantly more ACEs (t (698) =10.736, p < .000), which approached nearly three times the number of ACEs that White older adults had.
As shown in Table 2, there were no significant differences in depressive symptoms, perceived stigma for receiving psychological help, perceived mental health, attitude toward seeking mental health service, and non-physician health care use between the two older adult groups. However, AIs reported a lower self-perceived physical health (t (728) = −3.10, p = .002), more negative previous experience related to mental health service use (t (733) =25.601, p < .000) and a lower level of knowledge of depression (t (629) = −2.30, p = .022). Finally, AIs reported a higher level of mental health service use (t (733) =2.321, p = .021) and a higher level of mental health service use excluding non-physician health care use (t (733) =2.392, p = .017).
Table 2.
The Comparison of Key Factors between American Indian and White Older Adults
| Factors | Race | |||
|---|---|---|---|---|
| Total sample (N = 735) Mean (SD) | Whites (n = 502) Mean (SD) | American Indians (n = 233) Mean (SD) | p value | |
| Need Factors | ||||
| GDS | 64.4 | 2.00 (2.36) | 2.29 (2.76) | ns |
| Perceived physical health | 2.95 (.69) | 3.00 (.67) | 2.83 (.72) | .002 |
| Enable/Hindering Factors | ||||
| Prior negative experience of mental health service use | .11 (.43) | .05 (.28) | .25 (.67) | <0.001 |
| Knowledge of depression | 4.95 (2.32) | 5.07 (2.22) | 4.62 (2.45) | .022 |
| Stigma | 10.52 (3.05) | 10.51 (3.01) | 10.52 (3.17) | ns |
| Attitudes toward mental health services | 18.77 (5.94) | 18.63 (7.64) | 18.83 (6.10) | ns |
| Outcome variables | ||||
| Level of mental health service use (Total) | .25 (.67) | .21 (.59) | .34 (.83) | .021 |
| Level of mental health services use excluding non-physical health care use | 20 (.57) | .17 (.49) | .28 (.73) | .017 |
| Non-physician health care use (yes, n (%)) | 38 (5%) | 23 (4.6%) | 14 (6%) | ns |
Notes: Income is presented in Table 1; GDS indicates the Geriatric Depression Scale
Regression Analyses
As seen in Table 3, with the exception of gender, two predisposing factors (younger age and a higher level of ACE) were significantly associated with a high level of mental health service use for both groups. Regarding need factors, for White participants, none of the main variables were significant, whereas for enabling factors, more prior negative experience with mental health services, more positive attitudes toward help-seeking, and lower income were significantly associated with a higher level of mental health service use. As for AI participants, all need factors were significantly associated with the level of mental health service use. Moreover, among AIs, higher levels of depressive symptoms and better perceived physical health were significantly associated with a higher level of mental health service use. Regarding enabling/hindering factors among AIs, negative experience with mental health services along with more positive help-seeking attitudes toward mental health services and lower income were significantly associated with a high level of mental health service use.
Lastly, among AI older adults, as shown in Table 4, a higher level of ACE was significantly associated with a high level of mental health service (excluding non-physician health service use) and non-physician health care use. Two need factors (feeling more depressed, better perceived physical health) and two enabling/hindering factors (more prior negative experience with mental health services, more positive attitudes toward help-seeking) predicted a high level of mental health service excluding non-physician health service use.
Discussion
Before examining key factors across samples, some demographic differences between the White and AI sample are noteworthy. First, significant differences were reported in age, namely the average age of AIs was more than 10 years less than that of Whites (61 vs. 72). Likewise, the AI sample had a significantly lower income, with almost 47% of the populations earning less than $20,000 a year, versus only 33% of the White sample falling into this category. Moreover, the AI sample was much less likely to be insured, but more likely to be employed, which may be related to the significantly lower age of the AI sample. Given that more AIs were employed, the lower income among this population is even more striking. With poverty being a risk factor for mental distress, addressing these persistent and pervasive socioeconomic disparities, which may drive mental health disparities, are important to address [30].
Regarding the comparison of key factors between Whites and AIs, there were no significant differences between the groups regarding reported depressive symptoms, mental health stigma, and attitudes toward mental health services. Consistent with prior research [50, 58], there were significant differences among other factors, with AI older adults reporting significantly higher levels of ACE, more negative prior experience of mental health service use, lower levels of perceived physical health, and less knowledge related to depression. Counterintuitively, a higher level of mental health service use was reported among these AI older adults compared to their White counterparts. Although there was no statistically significant difference between the two groups in non-physician health care use, AI older adults reported more non-physician health care use compared to their White older adults. However, AI older adults and White older adults showed a similar positive attitude toward mental health service use. This may be related to the specific context of the study sample, and more exploratory analysis and potential follow-up qualitative research may illuminate reasons for the positive perceptions of mental health service use. Given research demonstrating a lower rate of mental health service utilization as age increases [18, 72], on average, younger AI adults may have more positive attitudes toward mental service use which may lead to a higher level of actual mental health service use.
For both AIs and Whites, the higher levels of mental health service use are partially explained by a predisposing factor (i.e., young age and more ACEs) and enabling/hindering factors (i.e., more prior negative mental health experiences, and lower income). To the best of our knowledge, there is no study examining the association between ACE and mental health service use among AI older adults. AI participants experienced an almost threefold higher rate of ACE experiences than their White counterparts. Given the findings from studies with other populations [11, 23], traumatic experiences in early life often lead to mental health problems, which then results in a higher level of mental service use regardless of racial/ethnic minority status. Indeed, disproportionately high rates of trauma experienced by AIs likely drive observed health disparities [21], including depression.
AIs were more likely to report negative experiences with mental health services. Compared to AI older adults, White older adults reported fewer negative past experiences with mental health services, which is likely due to real deficits in the quality of mental health care and funding available to adequately serve AIs [30]. One possible explanation is that White older adults have more exposure to mental healthcare, such as having opportunities to attend public awareness campaigns and mental health education, as well as opportunities to be screened and receive and treatment for depression and other mental illnesses. Yet, AI older adults may have more constrained access to quality mental health providers and resources [30].
Previous researchers have investigated the roles of enabling or hindering factors, including knowledge about health and health services, health beliefs and attitudes, and access to health services among ethnic minorities [62]. However, few have examined how previous negative experiences are associated with the level of health service use, in particular, among AIs. Importantly, those who reported greater levels of negative experience in our study population were likely to be younger, more educated, and more depressed. This is particularly concerning given that those with the highest need (i.e., those with more depressive symptoms) are experiencing the most unsatisfactory mental health experiences. Despite their negative experiences, interestingly, AI participants reported more knowledge about resources and more active help-seeking behaviors.
Unlike Whites, a higher level of mental service use was also partially explained by a greater level of depression, better physical health and a more negative attitude toward mental health services among AI adults. It is worth mentioning that, among the array of predictor variables, perceived physical health was the most influential in explaining mental health service use among AI older adults, highlighting the importance of understanding the intersections between physical and mental health. This finding is inconsistent with several previous studies of the general population [42, 43, 76]. It may be the case that AI adults who are not burdened by physical illness may be more willing and able to seek help for emotional and psychological problems because they are not preoccupied with physical illness. Unlike previous studies, the finding showed that when AI older adults experienced significantly higher rates of negative experiences with mental health services, they were more likely to use the mental health service. This may relate to the greater severity or need for mental health services (e.g., higher levels of depressive symptoms) superseding the effect that negative experiences may play in deterring service use. As AI older adults utilize more mental health services due to more serious mental health disturbances, they are exposed to a greater of negative experiences, including culturally insensitive service—a logical consequence of lower quality and under-resourced health facilities [30]. Because AIs may prefer a combination of both culturally-traditional and conventional mental health treatment approaches [30], developing mental health services that incorporate culturally relevant components is critical to promoting healthier lives among AIs.
Given the significant differences across the AI and White results of this study, more information about the specific AI mental health service context is needed to tailor services to be culturally sensitive and relevant to this population. This may be conducted through follow-up research, which may include qualitative studies with AI older adults focusing on their experiences and perceptions of mental health services, their preferences for conventional versus AI specific services, and identified barriers to treatment.
AI mental health services have conventionally been approached from a non-AI perspective and have been found to be less effective and even harmful to AIs [13, 30, 69]. Culturally relevant intervention development—interventions that incorporate AI worldviews, practices, and values—may increase the efficacy of treatment while minimizing spontaneous adaptations (which may compromise fidelity and intervention effectiveness) made by practitioners [51]. Other benefits of culturally relevant interventions include increasing engagement and retention, leading to sustainable and long-lasting improvements in behavioral health [46, 51]. A meta-analysis of 76 studies of culturally adapted interventions demonstrated a weighted average effect size of .45, indicating a moderately strong benefit to such adaptations in comparison with nonadapted interventions [33]. Despite a strong need, there is a glaring lack of intervention research focused on AI populations, with no known research focusing on AI older adults [29].
Likewise, interventions targeted to a specific cultural group have been found to be four times more effective than interventions provided to groups from a variety of cultural backgrounds [33]. In fact, following a non-targeted multicultural substance abuse prevention intervention conducted by Dixon et al. [17], AI drug use was found to actually increase after the intervention. Given the significant differences in mental health outcomes for people of differing ethnic and tribal backgrounds, research indicates the strong need for culturally specific programs. For example, since AIs tend to highly value traditional and spiritual healing practices, the traditional healer could partner with formal mental health care providers to provide culturally relevant care, depending on the preferences of AI individuals and families. Given the lack of evidence-based mental health programs developed for and with AI populations, research developing such programs is needed as well [29].
Limitations
Several limitations of the present study should be recognized. First, the study sample may have selection bias because it was not based on random sampling. For example, the level of depression and mental health service use among those who are homebound or institutionalized might be lower than for those who are actively involved in senior centers, pow wows, and other social service centers. Studies with more representative samples of AI older adults generally and also across different tribes and rural/urban contexts will provide a fuller picture of physical and behavioral health effects. Our results are suggestive only and will need further investigation with a representative sample. Second, we used a cross-sectional survey design, which requires careful interpretations in causality. Further development using a longitudinal study design may validate our findings. Third, we used a limited set of study variables, including some socio-economic factors and depression, to report their direct effects on mental health service use. We believe that future work involving various factors, such as culture and physical status, which may influence mental health service use, should be performed. Although we did not report in the results, the current study found that with the total sample, gender was a moderating factor of the knowledge of depression, attitude toward mental health, and income for the level of mental health service use. However, both for White and AI older adults, we found no significant moderating effect of gender. Future studies should examine the moderating and mediating effects of socio-economic factors on mental health service use. We believe that future work involving various factors, such as culture and physical status, which may influence mental health service use, should be performed. Likewise, although we examined propensity to use formal helping systems, we did not assess measures of AI/ANs use of traditional helping systems.
Future studies that include help-seeking of traditional helping systems are recommended. Fourth, culture and ACE are inseparably interwoven together; the reporting accuracy of ACE may vary by individuals’ background (e.g., age, gender, race) or culture. Objective testing for ACEs would add strength to the assessment of the connection between childhood victimization and mental health among older adults. The reliability of the instruments we used, therefore, should be further examined with AI older adults. Also, the validity of the depression literacy and perceived stigma scales have not yet been evaluated with AI populations. Furthermore, the instrument assessing attitudes toward mental health services has not yet been validated with AI older adults; this research is needed, since attitudes toward mental health service may be perceived in distinctly different ways for AIs, who embrace a more collective social structure.
More research is needed to develop culturally-sensitive, empirically-validated instruments to measure mental health service use among AI older populations. The study findings are limited to older AIs and Whites in the Northern Plains. Thus, we cannot generalize the study findings to other older adult groups. Despite differences in culture, religion, language, and history among AI/AN tries, the current study does not take any differences in tribes into consideration. Future study should pay attention to the role of tribal identification as it relates to mental health service use; yet close attention to protecting the anonymity of tribal affiliation is necessary to prevent unintended negative outcomes of sensitive research results. Due to the limited measures in the current study, we only included individual level measures, and did not conduct multilevel analysis to understand the effects of neighborhood characteristics (e.g., availability of health care centers, ethnic composition of neighborhood) on mental health service use. Despite the significant difference in health insurance between AI and White older adults, the coverage for AI older adults may be understated because information regarding potential sources of healthcare/coverage from the Indian Health Service was not available in this study.
Conclusion
Despite the limitations of our study, the present study is among the few gerontological health research to examine factors that predict mental health service use among AI older adults living in a rural area. Thus, our findings contribute to the body of health disparity research in AIs by revealing different need and enabling factors that might impact the level of mental health service use of AIs compared to their White counterparts. As indicated by past research [30], social disadvantage tends to disproportionately affect AI groups and our work was no exception, with poverty, higher levels of childhood trauma, and more negative experiences with mental health affecting AIs and concomitant mental health service utilization. Our results indicate culturally specific outcomes regarding mental health service utilization and that culturally-specific and targeted interventions that are holistic and relevant to AIs are highly needed. AIs are less likely to seek help when services reflect a lack of cultural sensitivity and competence among service providers [33]. Because of a lack of AI-specific interventions, more sustainable, efficient, and equitable services, and culturally relevant evidence-based programs should be developed in partnership with AI communities [13].
Compliance with Ethical Standards
Conflict of Interest Author Dr. Moon declares that he/she has no conflict of interest. Author Dr. Lee declares that he/she has no conflict of interest. Author Dr. Roh declares that he/she has no conflict of interest. Author Dr. Burnette declares that he/she has no conflict of interest.
Ethical Approval This article does not contain any studies with human participants performed by any of the authors.
References
- 1.Afilalo J, Marinovich A, Afilalo M, Colacone A, Léger R, Unger B, et al. Nonurgent emergency department patient characteristics and barriers to primary care. Acad Emerg Med. 2004;11(12):1302–10. 10.1197/j.aem.2004.08.032. [DOI] [PubMed] [Google Scholar]
- 2.American Association of Suicidology. Some facts about suicide and depression. 2010; Retrieved from http://www.suicidology.org/c/document_library/get_file?folderId=232&name=DLFE-246.pdf.
- 3.American Psychiatric Association (2010) Mental health disparities: American Indians and Alaska Natives Retrieved from http://www.integration.samhsa.gov/workforce/mental_health_disparities_american_indian_and_alaskan_natives.pdf.
- 4.Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield CH, Perry BD, … and Giles WH (2006). The enduring effects of abuse and related adverse experiences in childhood. Eur Arch Psychiatry Clin Neurosci, 256(3), 174–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andersen R Behavioral model of families’ use of health services Research Series No. 25 Chicago: Center for Health Administration Studies, University of Chicago; 1968. [Google Scholar]
- 6.Anderson NB, Bulatao RA, Cohen B. Critical perspectives on racial and ethnic differences in health in late life. Washingon D.C: National Academies Press; 2004. [PubMed] [Google Scholar]
- 7.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s behavioral model of health services use: a systematic review of studies from 1998–2011. GMS Psycho-Social-Medicine. 2012;9:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help-seeking in 2 American Indian reservation populations. Arch Gen Psychiatry. 2005;62(1):99–108. [DOI] [PubMed] [Google Scholar]
- 9.Blackwell DL, Martinez ME, Gentleman JF, Sanmartin C, Berthelot JM. Socioeconomic status and utilization of health care services in Canada and the United States: findings from a binational health survey. Med Care. 2009;47(11):1136–46. [DOI] [PubMed] [Google Scholar]
- 10.Braun KL, LaCounte C. The historic and ongoing issue of health disparities among native elders. Generations. 2014;38(4):60–9. [Google Scholar]
- 11.Browne A, Finkelhor D. Impact of child sexual abuse: a review of the research. Psychol Bull. 1986;99(1):66. [PubMed] [Google Scholar]
- 12.Broyles RW, McAuley WJ, Baird-Holmes D. The medically vulnerable: their health risks, health status, and use of physician care. J Health Care Poor Underserved. 1999;10(2):186–200. 10.1353/hpu.2010.0498. [DOI] [PubMed] [Google Scholar]
- 13.Burnette CE, Figley CR. Risk and protective factors related to the wellness of american indian and alaska native youth: a systematic review. Int Public Health J. 2016;8(2):58–75. [Google Scholar]
- 14.Choi S Longitudinal changes in access to health care by immigrant status among older adults: the importance of health insurance as a mediator. The Gerontologist. 2011;51(2):156–69. [DOI] [PubMed] [Google Scholar]
- 15.Conner KO, Lee B, Mayers V, Robinson D. Attitudes and beliefs about mental health among African American older adults suffering from depression. J Aging Stud. 2010;24(4):266–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dhingra SS, Zack M, Strine T, Pearson WS, Balluz L. Determining prevalence and correlates of psychiatric treatment with Andersen’s behavioral model of health services use. Psychiatr Serv. 2010;61(5): 524–8. 10.1176/appi.ps.61.5.524. [DOI] [PubMed] [Google Scholar]
- 17.Dixon AL, Yabiku ST, Okamoto SK, Tann SS, Marsiglia FF, Kulis S, et al. The efficacy of a multicultural prevention intervention among urban american indian youth in the southwest US. J Prim Prev. 2007;28(6):547–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dobalian A, Rivers PA. Racial and ethnic disparities in the use of mental health services. J Behav Health Serv Res. 2008;35(2):128–41. [DOI] [PubMed] [Google Scholar]
- 19.Dube SR, Anda RF, Felitti VJ, Edwards VJ, Williamson DF. Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: implications for health and social services. Violence Vict. 2002;17(1):3–17. [DOI] [PubMed] [Google Scholar]
- 20.Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. Jama. 2001;286(24), 3089–3096. [DOI] [PubMed] [Google Scholar]
- 21.Evans-Campbell T, Lindhorst T, Huang B, Walters KL. Interpersonal violence in the lives of urban American Indian and Alaska native women: implications for health, mental health, and help-seeking. Am J Public Health. 2006;96(8):1416–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Feldstein SW, Venner KL, May PA. American Indian/Alaska native alcohol- related incarceration and treatment. Am Indian Alsk Native Ment Health Res. 2010;13(3):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Felitti VJ. The relationship of adverse childhood experiences to adult health: turning gold into lead. Zeitschrift Fur Psychosomatische Medizin Und Psychotherapie. 2002;48(4):359–69. [DOI] [PubMed] [Google Scholar]
- 24.Felitti M, Vincent J, Anda M, Robert F, Nordenberg M, Williamson M,… Edwards B (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am J Prev Med, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- 25.Fischer EH, Farina A. Attitudes toward seeking professional psychological help: a shortened form and considerations for research. J Coll Stud Dev. 1995;36:368–73. [Google Scholar]
- 26.Fleury MJ, Grenier G, Bamvita JM, Caron J. Determinants and patterns of service utilization and recourse to professionals for mental health reasons. BMC Health Serv Res. 2014;14(1):161 10.1186/1472-6963-14-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garrett MD, Baldridge D, Benson W, Crowder J, Aldrich N. Mental health disorders among an invisible minority: depression and dementia among American Indian and Alaska native elders. The Gerontologist. 2015; 10.1093/geront/gnu181. [DOI] [PubMed] [Google Scholar]
- 28.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273. [PMC free article] [PubMed] [Google Scholar]
- 29.Gone JP, Alcántara C. Identifying effective mental health interventions for American Indians and Alaska natives: a review of the literature. Cult Divers Ethn Minor Psychol. 2007;13(4):356. [DOI] [PubMed] [Google Scholar]
- 30.Gone JP, Trimble JE. American Indian and Alaska native mental health: diverse perspectives on enduring disparities. Annu Rev Clin Psychol 2012;8:131–60. [DOI] [PubMed] [Google Scholar]
- 31.Goodwin RD, Hoven CW, Lyons JS, Stein MB. Mental health service utilization: the role of personality factors. Soc Psychiatry Psychiatr Epidemiol. 2002;37:561–6. [DOI] [PubMed] [Google Scholar]
- 32.Grandbois D Stigma of mental illness among American Indian and Alaska native nations: historic and contemporary perspectives. Issues Ment Health Nurs. 2005;26:1001–24. [DOI] [PubMed] [Google Scholar]
- 33.Griner D, Smith TB. Culturally adapted mental health intervention: a meta- analytic review. Psychother Theory Res Pract Train. 2006;43(4):531–48. [DOI] [PubMed] [Google Scholar]
- 34.Gulliver A, Griffiths KM, Christensen H. Internet-based interventions to promote mental health help-seeking in elite athletes: an exploratory randomized controlled trial. J Med Internet Res. 2012;14(3):e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hartmann WE, Gone JP. Incorporating traditional healing into an urban American Indian health organization: a case study of community member perspectives. J Couns Psychol. 2012;59:542–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hawkins EH, Cummins LH, Marlatt GA. Preventing substance abuse in American Indian and Alaska native youth: promising strategies for healthier communities. Psychol Bull 2004;130(2):304. [DOI] [PubMed] [Google Scholar]
- 37.Henderson C, Evans-Lacko S, Thornicroft G. Mental illness stigma, help-seeking, and public health programs. Am J Public Health. 2013;103(5):777–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hill DL. Sense of belonging as connectedness, American Indian world-view, and mental health. Arch Psychiatr Nurs. 2006;20(5):210–6. [DOI] [PubMed] [Google Scholar]
- 39.Hunt J, Sullivan G, Chavira DA, Stein MB, Craske MG, Golinelli D, et al. Race and beliefs about mental health treatment among anxious primary care patients. J Nerv Ment Dis. 2013;201(3):188–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Indian Health Service (2016) Indian health service fact sheets: Indian health disparities Retrieved from https://www.ihs.gov/newsroom/includes/themes/newihstheme/display_objects/documents/factsheets/Disparities.pdf.
- 41.Jang Y, Kim G, Hansen L, Chiriboga DA. Attitudes of older Korean Americans toward mental health services. J Am Geriatr Soc. 2007;55:616–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kessler RC, Frank RG, Edlund M, Katz SJ, Lin E, Leaf P. Differences in the use of psychiatric outpatient services between the United States and Ontario. N Engl J Med. 1997;336:551–7. [DOI] [PubMed] [Google Scholar]
- 43.Kessler RC, Berglund PA, Bruce ML, Koch R, Laska EM, Leaf PJ, et al. The prevalence and correlates of untreated serious mental illness. Health Serv Res. 2001;36:987–1007. [PMC free article] [PubMed] [Google Scholar]
- 44.Komiya N, Good GE, Sherrod NB. Emotional openness as a predictor of college students’ attitudes toward seeking psychological help. J Couns Psychol. 2000;47(1):138–43. [Google Scholar]
- 45.Kramer BJ. Urban American Indian aging. J Cross Cult Gerontol. 1991;6:205–17. [DOI] [PubMed] [Google Scholar]
- 46.Kumpfer KL, Alvarado R, Smith P, Bellamy N. Cultural sensitivity and adaptation in family-based prevention interventions. Prev Sci. 2002;3(3):241–6. [DOI] [PubMed] [Google Scholar]
- 47.Landen M, Roeber J, Naimi T, Nielsen L, Sewell M. Alcohol-attributable mortality among American Indians and Alaska natives in the United States, 1999–2009. Am J Public Health. 2014;104(S3):S343–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lujan C, DeBruyn LM, May PA, Bird ME. Profile of abused and neglected American Indian children in the southwest. Child Abuse Negl. 1989;13(4):449–61. [DOI] [PubMed] [Google Scholar]
- 49.Manson SM. Long-term care of older American Indians: challenges in the development of institutional services In: Barresi C, Stull DE, editors. Ethnicity and long-term care. New York: Springer; 1992. p. 130–43. [Google Scholar]
- 50.Manson SM. Mental health services for American Indians and Alaska natives: need, use, and barriers to effective care. Can J Psychiatr. 2000;45:617–26. [DOI] [PubMed] [Google Scholar]
- 51.Marsiglia FF, Booth JM. Cultural adaptation of interventions in real practice settings. Res Soc Work Pract. 2015;25(4):423–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.National Alliance on Mental Illness (NAMI). American Indian and Alaska Native women and depression fact sheet. Arlington: National Alliance on Mental Illness; 2009. Retrieved August 10, 2012 from http://www.nami.org/Template.cfm?Section=Women_and_Depression&Template=/ContentManagement/ContentDisplay.cfm&ContentID=88885 [Google Scholar]
- 53.Neighbors HW, Caldwell C, Williams DR, Nesse R, Taylor RJ, Bullard KM, et al. Race, ethnicity, and the use of services for mental disorders: results from the National Survey of American life. Arch Gen Psychiatry. 2007;64(4):485–94. [DOI] [PubMed] [Google Scholar]
- 54.Office of the Surgeon General (US); Center for Mental Health Services (US). Mental health: Culture, race, and ethnicity: A supplement to mental health: A report of the surgeon general Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2001. [PubMed] [Google Scholar]
- 55.Pratt W, Benthin, Schmall. Alcohol problems and depression in later life: development of two knowledge quizzes. Gerontologist. 1992;32:175–83. [DOI] [PubMed] [Google Scholar]
- 56.Rayburn NR, Wenzel SL, Elliott MN, Hambarsoomians K, Marshall GN, Tucker JS. Trauma, depression, coping, and mental health service seeking among impoverished women. J Consult Clin Psychol. 2005;73:667–77. [DOI] [PubMed] [Google Scholar]
- 57.Rhodes A, Jaakkimainen L, Bondy S, Fung K . Depression and mental health visits to physicians: a prospective records-based study. Soc Sci Med. 2006;62:828–34. [DOI] [PubMed] [Google Scholar]
- 58.Robin RW, Chester B, Rasmussen JK, Jaranson JM, Goldman D. Factors influencing utilization of mental health and substance abuse services by American Indian men and women. Psychiatr Serv. 1997;48:826–32. [DOI] [PubMed] [Google Scholar]
- 59.Roh S, Brown-Rice KA, Lee KH, Lee YS, Yee-Melichar D, Talbot EP. Attitudes toward mental health services among American Indians by two age groups. Community mental health journal. 2015;51(8):970–977. [DOI] [PubMed] [Google Scholar]
- 60.Roh S, Burnette CE, Lee KH, Lee YS, Martin JI,Lawler MJ. Predicting Help-Seeking Attitudes Toward Mental Health Services Among American Indian Older Adults: Is Andersen’s Behavioral Model a Good Fit?. Journal of Applied Gerontology. 2017;36(1):94–115. [DOI] [PubMed] [Google Scholar]
- 61.Roman SP, Jervis LL, Manson SM. Psychology of older American Indians and Alaska natives: strengths and challenges to maintaining mental health In: Chang EC, Downey CA, editors. Handbook of race and development in mental health. New York: Springer; 2012. p. 127–46. 10.1007/978-1-4614-0424-8_8. [DOI] [Google Scholar]
- 62.Scheppers E, van Dongen E, Dekker J, Geertzen J, Dekker J. Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract. 2006;23(3):325–48. [DOI] [PubMed] [Google Scholar]
- 63.Segal DL, Coolidge FL, Mincic MS, O’Riley A. Beliefs about mental illness and willingness to seek help: a cross-sectional study. Aging Ment Health. 2005;9:363–7. [DOI] [PubMed] [Google Scholar]
- 64.Shavers VL, Fagan P, Jones D, Klein WM, Boyington J, Moten C, et al. The state of research on racial/ethnic discrimination in the receipt of health care. Am J Public Health. 2012;102(5):953–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sotero M A conceptual model of historical trauma: implications for public health practice and research. J Health Disparities Res Pract. 2006;1(1):93–108. [Google Scholar]
- 66.Toler Woodward A, Taylor RJ, Chatters LM. Use of professional and informal support by black men with mental disorders. Res Soc Work Pract. 2011;21(3):328–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.U.S. Census Bureau (2012) American Indian and Alaska Native heritage month: Nov 2012. Retrieved from http://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb12-ff22.html.
- 68.U.S. Department of Health and Human Services. American Indian/Alaska native behavioral health briefing book. Rockville: U.S. Department of Health and Human Services, Indian Health Service, Division of Behavioral Health, Office of Clinical and Preventive Services; 2011. [Google Scholar]
- 69.Urban Indian Health Institute. Supporting sobriety among American Indians and Alaska natives: a literature review. Seattle: Urban Indian Health Institute; 2014. [Google Scholar]
- 70.Walls ML, Johnson KD, Whitbeck LB, Hoyt DR. Mental health and substance abuse services preferences among American Indian people of the northern Midwest. Community Ment Health J. 2006;42(6):521–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang PS, Berglund P, Olfson M, Pincus HA, Wells KB, Kessler RC. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:603–13. [DOI] [PubMed] [Google Scholar]
- 72.Wei W, Sambamoorthi U, Olfson M, Walkup JT, Crystal S. Use of psychotherapy for depression in older adults. Am J Psychiatr. 2005;162(4):711–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.West A, Williams E, Suzukovich E, Strangeman K, Novins D. A mental health needs assessment of urban American Indian youth and families. Am J Community Psychol. 2012;49(3):441–53. [DOI] [PubMed] [Google Scholar]
- 74.Whitfield CL, Anda RF, Dube SR, Felitti VJ. Violent childhood experiences and the risk of intimate partner violence in adults assessment in a large health maintenance organization. J Interpers Violence. 2003;18(2):166–85. [Google Scholar]
- 75.Yesavage JA, Sheikh JI. Geriatric depression scale (GDS) recent evidence and development of a shorter violence. Clin Gerontol. 1986;5(1–2):165–73. [Google Scholar]
- 76.Zuvekas SH, Fleishman JA. Self-rated mental health and racial/ethnic disparities in mental health service use. Med Care. 2008;46:915–23. [DOI] [PubMed] [Google Scholar]