Abstract
Significance:
Full-field prisms that fill the entire spectacle eye wire have been considered as field expansion devices for homonymous hemianopia (HH) and acquired monocular vision (AMV). While full-field prism is used for addressing binocular dysfunction following brain injury and prism adaptation training as treatment for spatial hemineglect, we show that the full-field prism for field expansion does not effectively expand the visual field in either HH or AMV.
Purpose:
Full-field prisms may shift a portion of the blind side to the residual seeing side. However, foveal fixation on an object of interest through a full-field prism requires head and/or eye rotation away from the blind side, thus negating the shift of the field towards the blind side.
Methods:
We fit meniscus and flat full-field 7Δ and 12Δ yoked prisms and conducted Goldmann perimetry in HH and AMV. We compared the perimetry results to ray tracing calculations.
Results:
The rated prism power was in effect at the primary position of gaze for all prisms, and the meniscus prisms maintained almost constant power at all eccentricities. To fixate on the perimetry target, the subjects needed to turn their head and/or eyes away from the blind side, which negated the field shift into the blind side. In HH, there was no difference in the perimetry results on the blind side with any of the prisms. In AMV, the lower nasal field of view was slightly shifted into the blind side with the flat prisms, but not with the meniscus prisms.
Conclusions:
Full-field prisms are not an effective field expansion device due to the inevitable fixation shift. There is potential for a small shift with the flat full-field prism in AMV, but such lenses cannot incorporate refractive correction. Further, in considering the apical scotoma, the shift provides a mere field substitution at best.
Keywords: Prism, field expansion, yoked prism, full-field, monocular vision, hemianopia, head rotation, eye rotation, fixation
Full-field Prisms and Configurations
Full-field prisms1, 2 (full prisms or full-diameter prisms3), which fill the entire spectacle eye wire have been used in a number of ophthalmic applications including addressing binocular dysfunction, controlling for midline shift3 or other postural stability symptoms following brain injury,4 and temporarily in prism adaptation training as a treatment for spatial hemineglect.5
Full-field prisms have also been considered as field expansion devices for many decades6 and are still actively prescribed for peripheral field loss conditions such as homonymous hemianopia1–3, 7, 8 and acquired monocular vision.9, 10 Full-field prisms have been regarded as an attractive field expansion solution because “these glasses have the appearance of ordinary eyeglasses, fit in any standard eyeglass frame, are light-weight and low-cost, and do not require any special user intelligence, awareness or training”.9 Conceptually, full-field prisms with the base toward the blind side shift the entire field-of-view laterally from the non-seeing towards the seeing field. In this paper, we only address the use of the full-field prisms for field expansion, though some of the considerations discussed here may be relevant also for other applications.
In homonymous hemianopia, bilateral full-field yoked prisms1–3 are intended to extend the seeing area outward from the central edge of the field loss. On the other hand, in acquired monocular vision9, 10 the aim is to extend the field of view to compensate for the missing temporal crescent. While monocular full-field prisms are sometimes used in acquired monocular vision, bilateral full-field yoked prisms provide better balance in terms of weight and cosmetics.9, 10 The efficacy of full-field prisms for field expansion has not been perimetrically measured or reported.
The power of ophthalmic full-field prisms used for field expansion has usually been limited to less than 15Δ (prism diopter).1, 6, 9 Since a higher power full-field prism require a heavier prism segment with a thicker base edge, the prism power of ophthalmic prisms is mechanically limited. In addition, the prism power of full-field prisms for field expansion is limited by the reduced image quality caused by spatial distortion, chromatic dispersion, and scattering of light (especially in Fresnel full-field prisms), all of which affect visual acuity and contrast sensitivity.11, 12 Since Fresnel full-field prisms have worse image quality,11, 12 the use of Fresnel full-field prisms has not been recommended for field expansion, to the best of our knowledge.9 Only non-Fresnel ophthalmic prisms with limited prism power have been reported as full-field prisms for field expansion purpose.
Meniscus (Fig. 1A) or flat ophthalmic prisms (Figs. 1B&C) with limited prism power have been used for field expansion of homonymous hemianopia and acquired monocular vision. The meniscus full-field prisms, which have a convex front surface and a concave back surface with an apex angle between them, are more popular as they enable a refractive correction to be incorporated. The meniscus prisms are more cosmetically appealing as they look like normal ophthalmic lenses. The prisms also require a frame with small horizontal extent to limit thickness of the base end. The thickness of the base end of full-field ophthalmic prisms also requires careful consideration of the position of the lens bevel when it is mounted into the frame.
Figure 1.
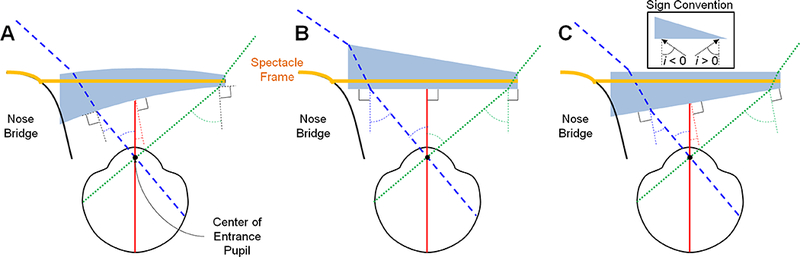
Schematic illustration (right eye with base-in prisms) of full-field prism configurations. (A) Meniscus full-field prisms mounted with the bevel positioned at the front surface for the best cosmetics. (B) Flat full-field prisms with the bevel positioned at the back surface for mounting to the frame (outward prism serration). (C) Flat prisms mounted with bevel positioned at the front surface (eyeward prism serration). Due to the difference in back surface shape (curved, flat or slanted), the angle of incidence, i (from the normal to the back surface, see the inset), varies with prism configuration and direction. The smaller angles of incidence at the base end (blue dashed lines) in (A) and (C) result in lower effective prism powers than in (B).
The meniscus full-field prisms are mounted with the bevel positioned at the front surface of the lens (Fig. 1A). The flat prisms may be mounted with the bevel positioned at the back surface (Fig. 1B) or the front surface (Fig. 1C). Previously, we defined two configurations of Fresnel prisms as outward prism serration or eyeward prism serration.13 These terms can be extended in this paper to the full-field prisms with the bevel positioned towards the back surface (outward prism serration, Fig. 1B) or front surface (eyeward prism serration, Fig. 1C), where the ophthalmic prism is regarded as a single serration.
While cosmetics dictate mounting the full-field prisms with the frame’s bevel positioned at the front surface of the lens as in the meniscus (Fig. 1A) and flat eyeward prism serration ophthalmic prisms (Fig. 1C), thus hiding most of the lens edge, mechanical considerations require some compromises.14 If the bevel is positioned at the back of the lens such as the flat outward prism serration ophthalmic prism (Fig. 1B), the thick prism base will protrude in front of the lens, making for very poor cosmetics. However, the eyeward prism serration will severely limit the use of full-field prisms in the base-in configuration, as the base edge of the prism will push into the nose and may touch the eyelashes.
In addition to the mechanical differences, the angle of incidence (defined from the normal to the back surface of the prism) differs among the configurations (Fig. 1) and affects the effective prism power.13 The effective prism power at the primary position of gaze or at the base end may affect field expansion for homonymous hemianopia or acquired monocular vision. We showed that in a high power prism (e.g, 40Δ or 57Δ), even a small change in angle of incidence towards the base rapidly increases the prism power and image compression, while light transmittance drops.13 At the limit of the angle of incidence, total internal reflection blocks the utility of the prism as a field shifting device and limits the effectiveness of eye scanning.13 Within the limited range of angles of incidence available in peripheral (Peli) prisms, the low power of full-field prisms (up to ~15Δ) may be approximated as constant power with no total internal reflection.13 However, because the full-field prisms cover a wider field a wider range of angles of incidence should be considered, even with the low power of full-field prisms.
Fixation Shift through Full-field Prisms
Patients with homonymous hemianopia and acquired monocular vision fixate foveally on objects of interest (i.e., fixation target in Fig. 2A). When patients wear the full-field prisms, the full-field prisms shift the field-of-view from the blind side to seeing side by an angle approximately equal to the prism power (Fig. 2B). Based on this effect, full-field prisms have been thought to be useful field expansion devices.
Figure 2.
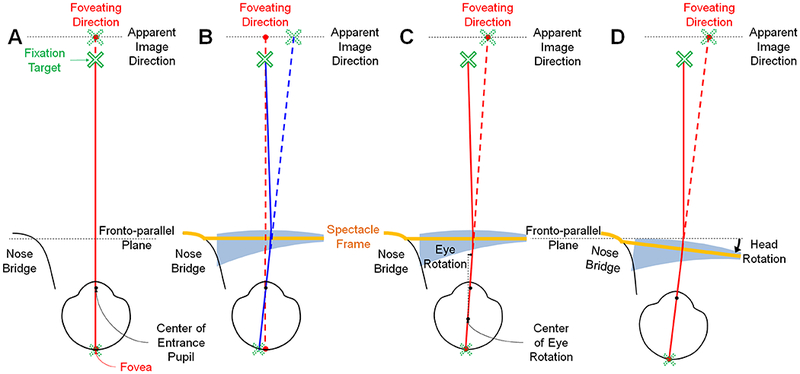
Fixation shift through full-field prisms. For simplicity, we illustrate right eye only with a base-in full-field prism. Note that we assume the flat spectacle frame (orange solid line) is orthogonal to the head direction, and the fronto-parallel plane is orthogonal to the line of sight to the fixation target (green cross mark) with no prism. The solid lines indicate the actual ray path from the fixation target to the retina (through the full-field prism in B-D), and the dashed lines show the apparent path. (A) When a patient with left homonymous hemianopia or right acquired monocular vision (right seeing eye) fixates on a far fixation target with the eye at the primary position of gaze, the fovea aims at the fixation target. (B) The image of the fixation target through the full-field prism is shifted toward the apex of the full-field prism (see dashed blue line and apparent cross image shifted from the fixation direction). The fixation target is now imaged off the fovea. The patient may rotate (C) the eyes and/or (D) the head and eyes together away from the blind side to foveate on the fixation target through the full-field prism, which may negate the field-of-view shift towards the base (red solid line).
This interpretation may need to be reconsidered because the prism in front of the eye shifts the fixation target, and thus it is imaged off the fovea (blue lines in Fig. 2B). Apfelbaum et al.15 commented that the effectiveness of field expansion with such full-field prisms may be limited by the head and/or eye rotations to refixate on the fixation target but did not provide a detailed explanation or an empirical measure of the effect.
Since the full-field prism shifts the image of the object of interest towards the apex (see apparent image direction in Fig. 2B), the patient looking through the full-field prisms may have to rotate the eyes (Fig. 2C) or turn the head while the eyes remain at primary position of gaze away from the blind side (Fig. 2D) so that foveal fixation returns to the object of interest (fixation target). If the magnitude of the head and/or eye rotation away from the blind side is approximately the same as the rated prism power at the primary position of gaze, this may approximately negate the field-of-view shift towards the blind side.
Apical Scotoma in Full-field Prisms
Apical scotoma, the angular gap between the light rays bent by a prism at the apex (or apex end within seeing field) and the first visible ray just outside the prism apex, has been mentioned in the prismatic field expansion literature.3, 16 The size of apical scotoma is the same as the effective prism power at the apex [Jung et al., IOVS 2014:E-Abstract 9264]. More recently its functional significance in mounting partial prism segments or sectors for field expansion has been elaborated.13,15,17
The apical scotoma in full-field prisms has not been considered or has been considered unimportant since the size is small and the apex is located at the edge of the lens on the far periphery of the seeing side and abuts frame scotoma.18, 19 If the full-field prism brings some of the field-of-view from the blind side into seeing visual field, but loses a similar amount of the field-of-view on the seeing side (i.e., due to apical scotoma), the total extent of field-of-view with the prisms remains about the same as that of the visual field. This is considered field substitution, not field expansion, even though the patient can see farther into the blind side and may benefit from the trade-off. Although the size of apical scotoma in the full-field prisms is usually small, if it is larger than the size of any field-of-view shift through a full-field prism due to the variation of effective prism power with high angle of incidence,13 as a result there is a net loss in field of view extent.
We analyzed the optical differences among the configurations of full-field prisms using ray tracing and present illustrations of simulated field diagrams guided by the ray tracing results. We examined the effectiveness of full-field prisms as field expansion devices, taking into consideration the fixation shift, apical scotoma, and effective prism power within different configurations. Perimetric measurements of subjects with homonymous hemianopia or acquired monocular vision are used to verify and confirm our analyses.
METHODS
All procedures were approved by the Massachusetts Eye and Ear Human Studies Committee in accordance with the Declaration of Helsinki, and all subjects provided informed consent.
Full-field Prism Glasses
We ordered three different configurations of full-field ophthalmic prism glasses (Chadwick Optical, Souderton, PA) (Fig. 3) for perimetric measurements with left homonymous hemianopia and right acquired monocular vision (right-seeing eye) subjects. The full-field prisms were mounted in a frame with narrow eye wire dimensions 40–23 and an interpupillary distance of 65 mm. A narrow eye wire is desired with a full-field prism to minimize the thickness of the base edge.
Figure 3.

Pictures of full-field prism configurations (12Δ yoked prisms). (A) Meniscus full-field prisms mounted with the bevel positioned at the front surface. (B) Flat full-field prisms with bevel positioned at the back surface to mount to the frame (outward prism serration). (C) Flat prisms mounted with bevel positioned at the front surface (eyeward prism serration). Note that the prisms were mounted in a special frame with very narrow eyewire to reduce the thickness of the prism base.
For the meniscus prisms, we use +4.00 diopter base curve lenses. We tested 7Δ, the maximum prism power previously suggested for acquired monocular vision,9, 10 and 12Δ, the maximum practical prism power in meniscus prisms with the bevel positioned at the front surface for the best cosmetic appearance.
Ray Tracing Simulation
To calculate the variation in effective prism power of different full-field prism configurations, we simulated 7Δ and 12Δ PMMA flat and meniscus full-field prisms using an optical ray tracing program (Zemax, Bellevue, WA). The full-field prism glasses were modeled with same dimensions and interpupillary distance as the spectacles we ordered (Fig. 3).
We set the center of the entrance pupil of the eye (3 mm behind cornea)20 as the reference point for rays entering the eye. Since the back vertex distance varies between the three configurations due to different back surfaces, we set the distance between the spectacle frame and the cornea (9 mm as we measured with the frames in Fig. 3) as the reference for all configurations. For simplicity, we assume a spectacle frame without face-form tilt.21
For convenience, we trace rays through the full-field prisms as if the rays were emerging from the eye rather than from the object of regard.13, 22 According to the principle of optical reversibility, the actual rays entering the eye through the full-field prism from objects of regard follow the same path.
Using the ray tracing results, we calculated field diagrams for a patient with complete left homonymous hemianopia and a patient with right acquired monocular vision. We assume that the visual field extends to about 55° nasally and 90° temporally. We hypothesized that subjects would turn their head to the right to fixate on the perimeter fixation target through the base-left full-field prisms.
Perimetric Measurement with Subjects
Kinetic Goldmann perimetry with a V4e target was conducted for a subject with left (incomplete) homonymous hemianopia (male, age 51, onset at age 27 due to the partial lobectomy for therapeutic control of seizures) and a subject with right acquired monocular vision (female, age 23, normal vision with left eye patched) wearing 7Δ and 12Δ full-field yoked prism glasses.
As the subjects might use head and/or eye rotation to refixate on the fixation target through a full-field prism, we removed the headband on the perimeter and allowed the subjects to freely turn their head and/or eyes to a comfortable position to maintain fixation on the fixation target of the perimeter. Since the thick base edge of flat eyeward prism serration full-field prisms (Fig. 3C) would push the nose and touch the eyelashes of the subjects, we only tested a meniscus and flat outward prism serration full-field prisms in perimetric measurements.
RESULTS
Calculated Perimetric Effects of Full-field Prisms
We traced rays from −60° (base side) to +50° (apex side) visual eccentricities in the modeled full-field prisms on the right eye of a frame as shown in Figs. 4A–C and calculated effective prism power (Figs. 4D&E). Note that we define the angle of incidence directed towards the base as negative (inset in Fig. 2A).13, 17, 22 In all full-field prisms, visual eccentricity toward the apex is limited to about 55° by the spectacle frames we used. The full-field prism glasses were designed to mount very close to the eye and thus cover a wide field-of-view despite the narrow eye wire. However, rays entering near the base end of the full-field prism are shifted to the base surface of the prism (red dotted surface in Figs. 4A–C) and do not provide the desired shifted view. We call this effect base surface obscuration which could cause spurious reflections that show incorrect directional information13 or reduce the image quality (e.g., blurry, hazy, or dimmer) depending on the base surface finish.
Figure 4.
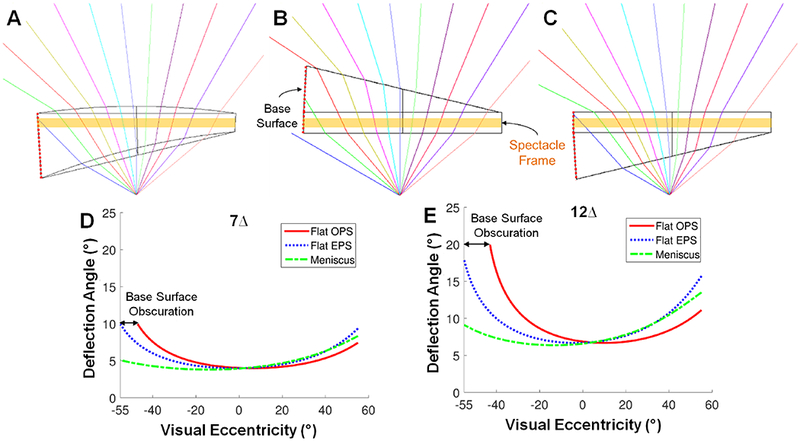
Simulated optical ray tracing in full-field prisms and calculated effective prism power variation. (A) Meniscus, (B) flat outward (OPS), and (C) eyeward prism serrations (EPS) full-field prisms (12Δ). Colored ray tracings indicate visual eccentricities from −60° (left, base side) to 50° (right, apex side) at 10° intervals. The angle of incidence and range of visual eccentricities covered by the full-field prisms vary between the configurations due to the different back surfaces. Graphs show the effective prism power variation of (D) 7Δ and (E) 12Δ in each configuration as a function of visual eccentricity. The effective prism power in flat outward prism serration full-field prisms is higher than other configurations. However, the base surface obscuration hitting the base surface of the prism (red dotted surface) further limits the effective range of visual eccentricities in the flat outward prism serration.
The meniscus and the flat eyeward prism serration full-field prisms (Figs. 4A&C) were within the normal nasal field eccentricity (≈55°)23. However, in the flat outward prism serration full-field prisms, the base surface obscuration interferes at nasal visual eccentricities larger than 47° in the 7Δ and 43° in the 12Δ full field prisms (Figs. 4D&E). This further limits the utility of the flat outward prism serration full-field prisms. Note, however, that a wider frame may be used for this configuration to reduce this effect, though such an approach will result in a thicker base edge. Such frames are frequently used in classroom demonstrations of prism adaptation effects.
Figs. 4D&E show the effective prism power (deflection angle) variation in flat and meniscus full-field prisms within the visual eccentricities covered by the frame. The angle of incidence in a flat outward prism serration full-field prism is the same as the visual eccentricity (Fig. 1B) because the back surface is parallel to the flat spectacle frame (the fronto-parallel plane). The angle of incidence in a meniscus full-field prism (Fig. 1A) or flat eyeward prism serration full-field prism (Fig. 1C) is affected by the curved or slanted back surface.
At the primary position of gaze, the angle of incidence (red lines in Fig. 1) is 0° in the flat outward prism serration full-field prism (Fig. 1B) and is higher in the flat eyeward prism serration and meniscus full-field prisms (Figs. 1A&C). However, with the low power of full-field prisms, there is minimal variation in prism power with the angle of incidence,13 and thus the effective prism powers of all configurations at the primary position of gaze (0° eccentricity at Figs. 4D&E) are approximately equal to the rated prism power. Since the visual eccentricities in effect in homonymous hemianopia are only to the center of the lens at the primary position of gaze, there is no difference among configurations.
At higher angles of incidence such as at the apex and base ends, the effective prism power varies between the configurations (Figs. 4D&E). Important for acquired monocular vision treatment, the angle of incidence at the nasal base end (blue dashed arrows in Fig. 1) in the flat outward prism serration full-field prisms is larger than in the flat eyeward prism serration and meniscus full-field prisms. The effective prism power at the apex (size of apical scotoma) in all configurations is higher than the rated prism power. The The angle of incidence at the apex end in the flat outward prism serration full-field prisms (green dotted lines in Fig. 1) is smaller than in the other two configurations, which results in a smaller apical scotoma. Therefore, the flat outward prism serration full-field prisms have the highest effective prism power at the base (field-of-view shift) and lowest effective prism power at the apex (size of apical scotoma) as shown in Figs. 4D&E. The base surface obscuration of this configuration further blocks about 10° of the nasal field, which reduces all advantages of the flat outward prism serration full-field prism, and it may not result in net field expansion in acquired monocular vision. The meniscus and flat eyeward prism serration full-field prisms have a lower effective prism power at the base and higher effective prism power at the apex, which may result in net field loss.
Effects of Full-field Prisms in Homonymous Hemianopia
We calculated field diagrams based on the effective prism power variation in different configurations (Figs. 4D&E) with the assumption of fixation shifts. We then compared the calculated results with perimetric measurements to verify the effect. Fig. 5 shows the calculated and measured binocular field diagrams of a patient with left homonymous hemianopia wearing a meniscus and flat outward prism serration full-field prisms (7Δ and 12Δ). The difference among prism power and configurations for field expansion is not larger than the measurement errors and variability. The eyeward prism serration was excluded from the perimetric measurement for touching eyelash of the subjects. The calculated field diagram for the flat eyeward prism serration is in the Appendix.
Figure 5.
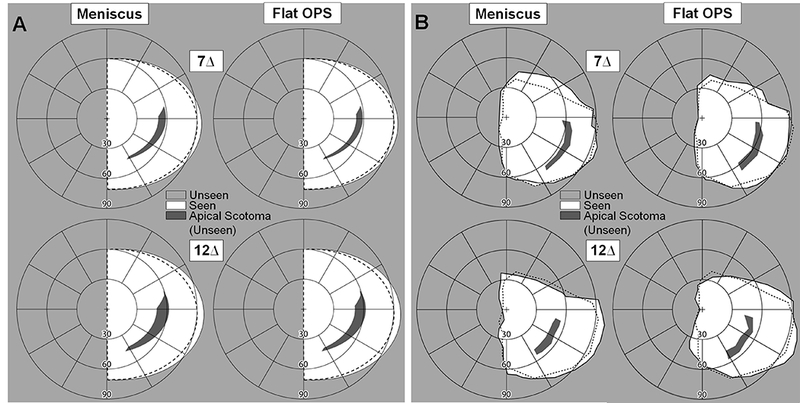
(A) Calculated and (B) measured binocular field diagrams of a patient with left homonymous hemianopia with two configurations of bilateral yoked full-field prisms. Left and right columns show the effects of full-field prisms in the meniscus and flat outward prism serration (OPS), respectively. Results for 7Δ and 12Δ are in the top and bottom row, respectively. The dashed line shows the binocular visual field without prisms. Due to the fixation shift, there is no field-of-view shift into the blind side (left). The compensatory head rotation toward the seeing (right) side for the fixation shift is expected to result in far right temporal field expansion on the seeing side, which is verified by the measurements. The calculated apical scotomas shown are from the right prism, and the upper parts of these may be compensated for by the nasal field of the left eye as seen in the measurements. The apical scotomas in the mid-periphery are wider than the magnitude of the temporal field shift. Note that the patient had incomplete hemianopia, which was consistent with his prior perimetry records.
No useful field expansion was calculated (Fig. 5A) with the assumption that the subject would require eye and/or head rotation to the right to fixate on the perimeter fixation target through full-field prisms as the rated prism power, which was verified by the perimetric measurements (Fig. 5B). The head rotation resulted in a wider temporal field-of-view on the right (outside of the full-field prisms). The 12Δ full-field prisms resulted in a slightly larger temporal field shift than the 7Δ prism due to larger head and/or eye rotation required by the higher prism power. However, there was no expansion of the field-of-view to the left blindside at all. The fixation shift was also verified by the location of the blind spot measured monocularly (not shown here, but see Fig. 6 for the same effect).
Figure 6.
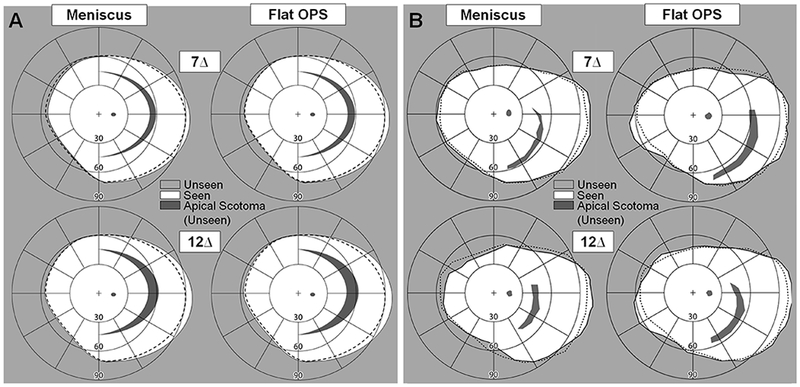
(A) Calculated and (B) measured field diagrams of a patient with right acquired monocular vision with different configurations of full-field prisms. Left and right columns show the effects of full-field prisms in the meniscus and the flat outward prism serration (OPS), respectively. Results for 7Δ and 12Δ are in the top and bottom row, respectively. The dashed line shows the visual field without prisms. Due to the head and eye rotation required for the fixation shift, the prisms show slightly farther temporal field-of-view (non-interesting side). With the flat outward prism serration full-field prisms (right columns), the eye rotation resulted in a slight field-of-view shift into the blind nasal side as the visual field was no longer blocked by the nose tip and wing at primary position of gaze. Taking into consideration the apical scotoma, this resulted in field substitution at best.
Considering the apical scotoma, the full-field prisms are not field expansion devices, but result in field substitution or a net field loss, with the field-of-view shift outside of the full-field prism into the temporal seeing side. As shown in Figs. 4D&E, the effective prism power at the (right) apex end, which defines the size of the right apical scotoma,13 varies with the configuration. The size of the apical scotoma in all configurations is larger than the magnitude of the temporal field-of-view shift (increase) (Fig. 5). Therefore, there is no useful field expansion from full-field prisms for homonymous hemianopia, unless some of the apical scotoma can be eliminated by the left eye. Additionally, the field expansion is on the far temporal periphery of the seeing side, which is not a particularly beneficial effect, while the apical scotoma is in the mid periphery where there is the highest risk of collision with other pedestrians.24
Note that the apical scotoma (of the right eye) could only be recorded in the lower quadrant (Fig. 5B), where the nasal seeing hemifield of the left eye was blocked by the tip and wing of the nose. Above the midline, the nasal field of the left eye eliminated part of apical scotoma as it does with peripheral prisms mounted unilaterally.15 Note that the vertical position of the apical scotoma is not well controlled since the vertical head posture is not controlled well in the perimeter due to the removal of the headband for head rotation.
When the observer rotates the eye instead of the head to fixate on the fixation target through the full-field prism, the apical scotoma will be more central. In this case, the amount of far temporal periphery shift will be smaller than with head rotation because the temporal orbit will block the view.23 Therefore, the full-field prism with eye rotation alone for fixation shift results in net field loss.
Effects of Full-field Prisms for Acquired Monocular Vision
Fig. 6 shows calculated and measured field diagrams of the right acquired monocular vision with full-field prisms. In the calculated field diagrams (Fig. 6A), we hypothesized that head rotation due to the fixation shift would reduce the field-of-view shift into the nasal side and result in a wider temporal field-of-view recorded outside of the full-field prisms. We ignored details of interactions with nose bridge, tip, and wing as well as eye movements,23 as these have minimal impact.
The perimetric measurement results (Fig. 6B) were similar to the calculated results and verified the eye and/or head rotation away from the blind side. The location of the physiological blind spot confirmed the subject’s fixation on the perimeter fixation target with and without the full-field prisms. There were slight field-of-view shifts into the temporal right side (measured out of the full-field prisms), which is hardly a useful expansion for acquired monocular vision.
The size of the apical scotomas in acquired monocular vision is larger than those in homonymous hemianopia (Fig. 5) since there is no fellow eye to compensate for the upper part of the apical scotoma. There were some errors in measurement of the location and size of the apical scotomas. Specifically, the back surface in the meniscus full-field prisms caused the subject to wear the glasses a little farther forward than the flat full-field prisms, which resulted in a slight shift of the apical scotoma towards the center. Here too, the vertical position of the apical scotoma is affected by a head tilt down in the perimeter, which shifted the prism and the apical scotoma down.
In the meniscus configuration (left columns in Fig. 6), the back surface toward the nose covered more of the nasal visual field, but this did not contribute to the field-of-view shift into the blind side. This is because the effective prism power at the base end is almost the same as the prism power at the primary position of gaze (Figs. 4D&E) which is negated by the head and/or eye rotations. As a result, there is no useful field expansion in full-field prisms for acquired monocular vision.
Although the flat outward prism serration full-field prisms (right columns in Fig. 6) have a higher effective prism power at the base end (nasal) than other configurations, the usable visual eccentricity is narrower due to the base surface obscuration (47° in 7Δ and 43° in 12Δ for this configuration compared with 55° toward the base in other configurations). The eye rotation resulted in a field-of-view shift into the blind side in the lower nasal field (right column in Fig. 6B). However, this small effect is from the eye rotation combined with a head turn away from the blind side due to the fixation shift. This happened only with the flat outward prism serration full-field prisms (right column in Fig. 6B) since there were slight gaps between the full-field prisms and the nose bridge. Overall, the full-field prisms for acquired monocular vision were not found to be a useful field expansion device, and they are a field substitution device with the apical scotomas at best.
In the case of temporal eye rotation (rather than head rotation), a slight portion of the nasal visual field blocked by the nose at the primary position of gaze (about 5 – 8°)23 becomes available, but the far temporal periphery is smaller than with head rotation, because it is blocked by the temporal orbital structure. In addition, the apical scotoma is more central, where collision risk is highest. Therefore, there is no meaningful improvement compared with the case of head rotation only.
DISCUSSION
We computed and perimetrically verified that no useful field expansion is provided with the use of full-field prisms for homonymous hemianopia or acquired monocular vision. The fixation shift through the full-field prism causes the head and/or eye to rotate away from the blind side, which negates the field-of-view shift into the blind side. Since the magnitude of the head and/or eye rotation is about the same as the rated prism power, there is no field-of-view shift into the blind hemifield in homonymous hemianopia through the full-field prisms. The full-field prisms in homonymous hemianopia could be considered to reduce the field with the additional effect of the apical scotoma, though it is a small effect.
In acquired monocular vision, there is a theoretical possibility for some field-of-view shift into the blind side in the flat outward prism serration full-field prisms due to the eye rotation and the position of the nose. An additional 5 – 8° of the nasal visual field,23 which is blocked by the nose at the primary position of gaze, becomes effective with the head and eye rotation in response to the fixation shift and may be slightly helpful. However, mechanical factors of the frames and prisms may negate the small effect. The thickness of the base edge of the full-field prisms, base surface obscuration, and the spectacle frame itself18, 19 limits this additional nasal field, rendering it mostly useless for field-of-view expansion into the blind side. It may only be useful in the flat outward prism serration full-field prisms, which cannot provide spectacle correction and have a large protrusion. The same effect may be achieved by turning the head toward the blind side while keeping the seeing eye looking straight.25–27
Since the base surface obscuration limits the effective prism power at the base of the flat full-field prisms for acquired monocular vision, we could consider a wider eyewire frame to shift the base surface to a larger nasal eccentricity. Nonetheless, total internal reflection limits the prism power and thus ~55° angle of incidence toward the base only allows up to 7Δ.13, 28 If there is no base surface obscuration in wider 12Δ flat full-field prisms (starts at 43°), the total internal reflection would still limit utility of visual eccentricities higher than 45° nasal eccentricity. Therefore, a wider field-of-view shift into the blind side is not expected with higher powered full-field prisms than the results we showed with 12Δ.
Except for the flat outward prism serration full-field prisms, the effective prism power at the apex (the size of the apical scotoma) is always higher than the rated prism power. In addition, the scotoma caused by the spectacle frame itself18, 19 may be wider than the apical scotoma with the suitable low power full-field prisms. Therefore, most full-field prisms are likely to result in a net field loss or substitution at best.
The location of the apical scotoma with full-field prisms for field expansion of homonymous hemianopia and acquired monocular vision is at an eccentricity of about 45° - 60°. Peli et al.24 have shown that the collision risk with other pedestrians is highest at ~45°. Therefore, the use of full-field prisms may even increase the risk of collision with pedestrians on the seeing side without providing any benefit on the blind side.
With the limitations, we described and verified, the full-field prisms are hardly an effective field expansion device for homonymous hemianopia or acquired monocular vision field loss. We found that none of the full-field prisms configurations provide useful field expansion. In fact, some configurations block the field-of-view where it would cause the greatest increase of risk in mobility. While only briefly discussed, all of the full-field prisms result in some acuity and contrast sensitivity loss both centrally and peripherally due to the effect of color dispersion.11,12
With these results, we recommend that the use of full-field prisms for field expansion be avoided. For field expansion of homonymous hemianopia, partial prisms such as sector,29 Gottlieb,30 and the Peli peripheral31 prisms should be considered. A major difference between partial prism field expansion devices and the full-field prisms is the interaction with foveal vision. Whereas the full-field prisms always affect foveal vision and require a shift of fixation, the partial prisms do not affect foveal vision at the primary position of gaze and do not change fixation when fitting properly. However, apical scotoma and diplopia13,15 should be considered when fitting sector prisms. Multiplexing prism17,28 can provide true field expansion of acquired monocular vision though there are monocular confusion and reduced contrast as side effects.
ACKNOWLEDGMENTS
Supported in part by NIH grants R01EY023385 and P30EY003790. We thank Merve Tuccar, Sailaja Manda, and Rachel Castle for help with subject tests and preparation of figures.
REFERENCES
- 1.Cohen JM. An Overview of Enhancement Techniques for Peripheral Field Loss. J Am Optom Assoc 1993;64:60–70. [PubMed] [Google Scholar]
- 2.Cohen JM, Waiss B. Visual field remediation In: Cole RG, Rosenthal BP, eds. Remediation and Management of Low Vision. St. Louis: Mosby; 1996:1–25. [Google Scholar]
- 3.Cotter SA. Uses of prism in low vision In: Weiss NJ, Brown WL, eds. Clinical Uses of Prism; a Spectrum of Applications. St. Louis: Mosby-Year Book, Inc.; 1995:279–300. [Google Scholar]
- 4.Padula WV, Wu L, Vicci V, et al. Evaluating and treating visual dysfunction In: Zasler ND, Katz DI, Zafonte RD, eds. Brain Injury Medicine: Principles and Practice. New York: Demos; 2007:511–28. [Google Scholar]
- 5.Rossetti Y, Rode G, Pisella L, et al. Prism Adaptation to a Rightward Optical Deviation Rehabilitates Left Hemispatial Neglect. Nature 1998;395:166–9. [DOI] [PubMed] [Google Scholar]
- 6.Braunschweig P Hemianopsia Aided by Prisms In: Jackson E, Finnoff WC, eds. Ophthalmic Year Book. Chicago: Ophthalmic Publishing Company; 1922:395. [Google Scholar]
- 7.Toffel K, Rumer D, Jun W. Hemianopsia and Falls Prevention. Insight: Res Pract Visual Impair Blin 2012;5:41–6. Available at: https://noravisionrehab.com/storage/app/media/Current-site-back-up/REFERENCES_articles_for_professional_page_NORA.doc2.pdf. Accessed June 25, 2018. [Google Scholar]
- 8.Bansal S, Han E, Ciuffreda KJ. Use of Yoked Prisms in Patients with Acquired Brain Injury: A Retrospective Analysis. Brain Inj 2014;28:1441–6. [DOI] [PubMed] [Google Scholar]
- 9.The National Institute for Rehabilitation Engineering. Vision Aids for People Having Homonymous Hemianopsia. Available at: http://www.schepens.harvard.edu/images/stories/nire/one_eye.pdf. Accessed: January 30, 2018.
- 10.The National Institute for Rehabilitation Engineering. Cros-vision glasses for people sighted in one eye. Available at: http://www.schepens.harvard.edu/images/stories/nire/nire_cros_vision_glasses.pdf. Accessed: January 30, 2018.
- 11.Katz M Contrast Sensitivity Through Hybrid Diffractive, Fresnel, and Refractive Prisms. Optometry 2004;75:509–16. [DOI] [PubMed] [Google Scholar]
- 12.Katz M Visual Acuity Through Fresnel, Refractive, and Hybrid Diffractive/Refractive Prisms. Optometry 2004;75:503–8. [DOI] [PubMed] [Google Scholar]
- 13.Jung JH, Peli E. Impact of High Power and Angle of Incidence on Prism Corrections for Visual Field Loss. Opt Eng 2014;53:P133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brooks CW. Essentials of Opthalmic Lens Finishing. St. Louis, MO: Butterworth-Heinemann; 2003. [Google Scholar]
- 15.Apfelbaum HL, Ross NC, Bowers AB, et al. Considering Apical Scotomas, Confusion, and Diplopia When Prescribing Prisms for Homonymous Hemianopia. Transl Vis Sci Technol 2013;2:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dickinson C Low Vision: Principles and Practice. Oxford: Butterworth; 1998. [Google Scholar]
- 17.Peli E, Jung JH. Multiplexing Prisms for Field Expansion. Optom Vis Sci 2017;94:817–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dille JR, Marano JA. The Effects of Spectacle Frames on Field of Vision. Aviat Space Environ Med 1984;55:957–9. [PubMed] [Google Scholar]
- 19.Steel SE, Mackie SW, Walsh G. Visual Field Defects due to Spectacle Frames: Their Prediction and Relationship to UK Driving Standards. Ophthalmic Physiol Opt 1996;16:95–100. [PubMed] [Google Scholar]
- 20.Gross H, Blechinger F, Achtner B. Human eye In: Gross H, ed. Handbook of Optical Systems, Volume 4: Survey of Optical Instruments. Weinheim, Germany: Wiley-VCH Verlag GmBH & Co. KGaA; 2008:1–45. [Google Scholar]
- 21.Fry GA. Face-form Frames. J Am Optom Assoc 1978;49:31–8. [PubMed] [Google Scholar]
- 22.Peli E, Bowers AR, Keeney K, et al. High-Power Prismatic Devices for Oblique Peripheral Prisms. Optom Vis Sci 2016;93:521–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Good GW, Fogt N, Daum KM, et al. Dynamic Visual Fields of One-Eyed Observers. Optometry 2005;76:285–92. [DOI] [PubMed] [Google Scholar]
- 24.Peli E, Apfelbaum H, Berson EL, et al. The Risk of Pedestrian Collisions with Peripheral Visual Field Loss. J Vis 2016;16:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coday MP, Warner MA, Jahrling KV, et al. Acquired Monocular Vision: Functional Consequences from the Patient’s Perspective. Ophthal Plast Reconstr Surg 2002;18:56–63. [DOI] [PubMed] [Google Scholar]
- 26.Goltz HC, Steinbach MJ, Gallie BL. Head Turn in 1-eyed and Normally Sighted Individuals during Monocular Viewing. Arch Ophthalmol 1997;115:748–50. [DOI] [PubMed] [Google Scholar]
- 27.Marotta JJ, Perrot TS, Nicolle D, et al. Adapting to Monocular Vision: Grasping with One Eye. Exp Brain Res 1995;104:107–14. [DOI] [PubMed] [Google Scholar]
- 28.Jung JH, Peli E. Field Expansion for Acquired Monocular Vision Using a Multiplexing Prism. Optom Vis Sci 2018;95:XXX–X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee AG, Perez AM. Improving Awareness of Peripheral Visual Field using Sectorial Prism. J Am Optom Assoc 1999;70:624–8. [PubMed] [Google Scholar]
- 30.Gottlieb DD. Method of Using a Prism in Lens for the Treatment of Visual Field Loss. United States Patent 4,779,972. October 25, 1988. [Google Scholar]
- 31.Peli E Field Expansion for Homonymous Hemianopia by Optically-Induced Peripheral Exotropia. Optom Vis Sci 2000;77:453–64. [DOI] [PubMed] [Google Scholar]


