Abstract
Psychotic spectrum disorders are serious illnesses with symptoms that significantly impact functioning and quality of life. An accumulating body of literature has demonstrated that specialized treatments that are offered early after symptom onset are disproportionately more effective in managing symptoms and improving outcomes than when these same treatments are provided later in the course of illness. Specialized, multicomponent treatment packages are of particular importance, which are comprised of services offered as soon as possible after the onset of psychosis with the goal of addressing multiple care needs within a single care setting. As specialized programs continue to develop worldwide, it is crucial to consider how to increase access to such specialized services. In the current review, we utilize an ecological model of understanding barriers to care, with emphasis on understanding how individuals with first-episode psychosis interact with and are influenced by a variety of systemic factors that impact help-seeking behaviors and engagement with treatment. Future work in this area will be important in understanding how to most effectively design and implement specialized care for individuals early in the course of a psychotic disorder.
Keywords: first-episode psychosis, early intervention, social ecology, emerging adulthood
Psychosis and treatment: an overview
Psychotic spectrum disorders, which include schizophrenia spectrum disorders and mood disorders with psychotic features, are pervasive and serious illnesses. Under usual systems of care, the course of these illnesses is characterized by repeated symptomatic relapses,1 numerous comorbidities (eg, anxiety, depressive episodes, substance use),2 and an average life span that is reduced by up to 25 years.3 Relative to their prevalence, the economic burden of these illnesses is disproportionately high. For example, despite affecting only 0.3%–1.6% of the US population,4 the estimated cost of one commonly diagnosed psychotic spectrum disorder (ie, schizophrenia) in the USA during 2013 was $155.7 billion.5
Research strongly suggests that the first few years following the onset of psychotic symptoms represents a critical period for intervention.3 More specifically, this is when 1) the majority of the decline in health and functioning unfolds6 and 2) individuals with psychosis experience the greatest therapeutic response to existing pharmacological and psychosocial treatments.7,8 These findings have, in part, sparked the rapid international expansion of specialty multicomponent treatment programs for individuals with first-episode psychosis (FEP). This treatment approach – referred to within the USA as “Coordinated Specialty Care” and recognized internationally as specialized care for FEP – has been shown to produce improvements in symptomatology and functional outcomes among individuals with FEP9 that may exceed those experienced under usual care.10,11
Unfortunately, many individuals with FEP experience a prolonged delay between the first onset of frank psychotic symptoms and receipt of adequate mental health care12 – a period of time referred to as the duration of untreated psychosis (DUP). Given strong evidence indicating that longer DUP is associated with negative clinical outcomes and worse response to treatment among individuals with FEP,10,13,14 DUP has been identified as an important modifiable risk factor for improving the course of psychotic disorders.15,16 With some notable exceptions,17,18 attempts to reduce DUP and to increase access to specialized care programs for individuals with FEP have been largely unsuccessful.19 Given the complexity of factors contributing to DUP and the variation of these factors across different healthcare environments, there is likely no singular approach to reducing DUP that can be effectively implemented across settings.20,21 Consequently, there is a need for the development of accurate heuristics to guide the identification of the unique factors that influence access to specialized services among individuals with FEP within specific communities.12,22
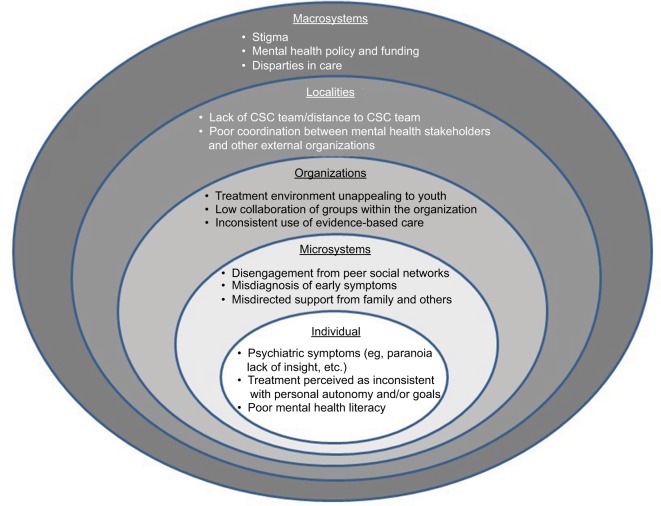
In this manuscript, we will review the working model of factors influencing access to specialized services for FEP developed at a specialized care clinic (the Ohio State University-Early Psychosis Intervention Center [OSU-EPICENTER]), as guided by existing theoretical models of social ecology and human development. This working model considers efforts to improve access to specialized care as “multilevel interventions.”23 Growing data suggest that health interventions that simultaneously target factors at multiple levels of the ecological context in which the health concern exists (eg, individual level, organizational level, population level) are more effective than interventions that target only a single level.24 Drawing on the ecological levels of analysis model25 as a guiding framework – which, in turn, is guided by Bronfenbrenner’s seminal ecological theory of human development26 – our working model focuses on five nested interdependent levels of factors hypothesized to influence access to care: 1) individuals; 2) microsystems; 3) organizations; 4) localities; and 5) macrosystems – see Figure 1. Below, we highlight examples of factors at each level of analysis that may influence access to specialized care for FEP. However, given local variation in factors influencing access to care across different settings, we advocate for the development of community-based models in which community stakeholders shape the identification of the specific multilevel factors influencing access to care in their community as well as the proposed solutions to these problems.23 Consequently, when applied to a specific community, this working model should serve only a heuristic to guide discussion and identification of the specific factors influencing access to care within that locale.
Figure 1.
An ecological model for understanding access to care for first-episode psychosis.
Abbreviation: CSC, Coordinated Specialty Care.
Multilevel factors influencing access to specialized care
Individuals
Individual factors influencing human behavior range from biological factors (eg, genetics, neuroanatomy) to psychological factors (eg, self-efficacy, cognition) to social factors (eg, perceived social support). Numerous individual factors influence access to specialized care among individuals with FEP, including the severity of psychiatric symptoms and mental health literacy.
Various psychiatric factors have the potential to delay access to care for individuals with FEP. Paranoid thinking and persecutory delusions can interfere with an individual’s willingness to seek help. Moreover, psychiatric comorbidities commonly experienced by individuals with FEP (eg, anxiety, depression) may also interfere with help-seeking via increased attention to potential sources of threat (eg, social rejection, stigma concerns), higher levels of shame around illness, and the use of less effective emotion regulation strategies such as avoidance and suppression.27–29 Lack of insight into illness or minimization of symptoms may further hinder help-seeking behavior.30,31
Deficits in mental health literacy and negative perceptions of mental health care are additional individual-level barriers to care. Mental health literacy – the ability to recognize mental health problems, to understand causes and risks, and to seek appropriate consultation or treatment32 – can contribute to a failure to seek professional help via a generalized lack of awareness around mental health and illness. Evidence suggests that young people are reluctant to seek care for mental health problems,33 possibly due in part to the onset of symptoms occurring during a period marked by still-developing knowledge and experience.32 Young people are also more likely to erroneously believe that they should be able to deal with their mental health symptoms on their own.33 When young people do experience distress in response to psychological symptoms, they are prone to use labels such as “stress” or “life problem” that are intended to normalize, yet are less likely to facilitate help-seeking behavior.32 Self-stigma around mental illness may underlie this pattern of behavior,22 as the prospect of acknowledging mental illness in oneself can lead to significant reductions in self-esteem.34 Finally, negative perceptions with regard to mental health treatment may further hinder help-seeking. Studies indicate that as many as one third of individuals with FEP report a lack of interest in receiving treatment,30 and they may also feel overwhelmed by the process of initiating care, or that there are “too many steps” that need to be navigated.22 Individuals with FEP may also be hesitant to seek care if they perceive its focus as only the management of psychiatric symptoms or otherwise inconsistent with their personal goals (eg, a young adult with psychosis may be interested in getting a job, but less so in addressing hallucinations or delusions).
Addressing barriers to care at the individual level involves the consideration of developmentally informed and personalized interventions that are maximally attractive to young people with FEP. As psychotic disorders generally manifest in the late teenage or early adult years,35 considering the unique needs of this developmental stage is crucial in optimizing our approaches to engaging youth in care. Arnett36 has described this developmental period as “emerging adulthood,” a stage of life marked by identity exploration in the domains of work and relationships with the goal of becoming self-sufficient. Thus, one possible approach to address individual-level barriers is the provision of care that embraces these developmental needs by focusing on the areas of skill development relevant to obtaining these milestones (eg, supported employment and education and strategies for forming and maintaining relationships) in addition to psychoeducation to address mental health literacy and skills for coping with psychiatric symptoms. This approach is consistent with information obtained via studies of qualitative interviews with youth with psychosis, which suggests that programs should emphasize all aspects of the program as not to dissuade those reluctant to have only “psychiatric” treatment (ie, psychosocial elements should be discussed along with pharmacological and physician aspects).22 In addition, utilizing a flexible, person-oriented approach to facilitating motivation for treatment is paramount in fostering engagement with care. Given that a variety of presenting psychiatric symptoms may interfere with building trust and willingness to proceed with treatment (lack of insight, motivational deficits, and/or paranoid thinking styles), striving to immediately establish a healthy alliance as soon as individuals seek care and forming collaborative client-centered goals are imperative.
Microsystems
Microsystems are the immediate environments in which individuals engage in direct, personal interactions over time.25 Microsystems are diverse and unique to each individual, but generally include interactions with one’s immediate family, peers, and other settings of daily living activities. Among individuals with FEP, examples of microsystem factors that may hinder access to care include disengagement from peer networks, misguided support from family and others, and misdiagnosis of early symptoms.
Psychotic disorders are marked by impairments in social functioning that are present even before the full onset of positive symptoms37 and contribute to a deterioration of relationships early in the illness.38 Disengagement from peer networks may impede access to care via reduced likelihood of others who know the individual well noticing and communicating about concerning changes in behavior and also in increasing the risk for the individual with FEP to encounter social stressors that exacerbate psychiatric symptoms or increase reticence to ask others for help (ie, bullying, rejection, and hostility from peers).39,40
In addition, the early signs and symptoms of FEP may be missed or even misinterpreted by others in the immediate environment of the individual. Many of the early signs of psychosis – changes in social behavior, school misconduct, and inconsistent interest in previously enjoyed activities – may be difficult for family members to disentangle from more normative shifts and changes associated with teenage and young adult behavior.41 Further, the stigma of mental illness may lead some families to be reluctant to recommend mental health treatment to their relative with psychosis – at times in an effort to avoid diagnoses that may confer negative responses from others.42 It is important to note that such occurrences are not limited solely to familial caregivers – similar patterns of vulnerability to misdiagnosis and lack of appropriate support are also observed among professional providers. For example, research in population-based samples suggests that frontline healthcare providers also evidence a delayed recognition of the early signs of the illness or may make misguided attempts to manage the psychotic symptoms without additional referral.43
Addressing microsystem barriers to the receipt of specialized care for individuals with FEP involves, in many cases, providing education and support to activate and engage the potential of important relationships in the individual’s life to facilitate connection with appropriate care. As the relationships at this level are characterized by frequent interactions over periods of time (ie, families, peers, and providers of general health care), their potential to support and direct individuals with FEP to appropriate care is paramount. A potential strategy for addressing barriers at this level may be offering support services to families themselves. These services are conducive to creating supportive relationships of family members to the individual with FEP and also provide an important venue for concerned family members to receive information from care providers and other families facing similar struggles. Further, research shows that when individuals with FEP do not themselves engage with appropriate treatment, relatives often play a crucial role in connecting them to care.30,44 Thus, providing this type of support may improve rates of accessing specialized care for FEP. Possible specialized forms of family education and support include multifamily group psychoeducation45 – a clinically beneficial and cost-effective format46 that involves multiple families offering and receiving support to one another. Providing opportunities for engagement with peers may also increase willingness to engage with specialized care, and youth with FEP note desires for peer contact as part of their treatment (ie, opportunities to interact with other young adults receiving similar care).22 To foster peer engagement, specialized treatment programs may offer group interventions or provide peer-mentoring opportunities. Individuals with FEP also request interventions aimed at increasing social resilience and providing skills for establishing and maintaining healthy relationships.47 Finally, efforts to provide education and resources to frontline healthcare providers have potential to reduce delayed recognition or misdiagnosis of early signs of psychosis (see “Localities” section).
Organizations
The organizations level refers to the associations or consortiums that encompass the collection of microsystems with which the individual interacts (eg, clinics, human service organizations, schools)25 – including organizations that provide treatment for FEP. Possible examples of barriers to care at this level include factors related to the organization and provision of care, including treatment environments that are unappealing to youth, inconsistent availability of evidence-based practices, and low levels of collaboration within microsystems of the organization.
The environment of FEP programs can impact the willingness of young adults to establish and maintain care. In particular, certain settings of care may operate with designs that are unappealing to youth with FEP. For example, young adults receiving care for FEP have noted that characteristics common to many mental health settings (long waits in austere waiting rooms full of strangers and meeting with different providers who have limited communication and thus needing to recount personal details many times at different appointments before receiving care)22 negatively impact desire to receive care. Some youth find these typical settings stigmatizing or incongruent with their developmental and cultural needs,48 which may further influence the avoidance of seeking specialized care for FEP. Taken together, these findings highlight the need to consider ways to create treatment environments that are “youth-friendly” and thus conducive to accessing and engaging with services.
In addition, the availability of evidence-based treatments within organizations providing care for FEP is variable. Although numerous trials of evidence-based, multicomponent care for FEP have demonstrated significant benefit from this type of treatment,11,50 there is a notable interprogram variability in the specific types of interventions that are actually offered51 – meaning that not all services providing care for FEP are utilizing treatment approaches that are most supported by research. Programs also differ in their assessment of fidelity to treatment, and thus, the degree to which evidence-based practices are implemented and followed is difficult to ascertain. Further, many specialized care programs do not routinely monitor the outcomes of individuals participating in their services. In fact, among the numerous specialized treatment programs within the USA, only five organizations/networks have published data demonstrating the benefits of their clinical programs.10,12,49,51,52 Completing specialized training in evidence-based interventions for FEP and building routine outcomes assessment into services may present several challenges to programs providing care for FEP (eg, accessing training in evidence-based practices for FEP, turnover among trained staff, limited experience with implementing outcomes assessment). However, collaborations with academic partners with expertise in specialized care for FEP may provide crucial support in the process of effectuating this type of system (see “Localities” section).
Although the evidence suggests that specialized care for FEP has a clear clinical benefit, functional outcomes for many individuals receiving care from these programs remain suboptimal.16 One avenue for optimizing access to care at the organizational level is to increase the initiation of care by creating a “youth-friendly” environment. Recently, additional attention has been given to the creation of mental health services that are sensitive to the developmental and cultural needs of young people in order to improve service utilization.53 This approach – which is apparent in the design of broad, specialized youth mental health program outside of the USA (ie, headspace in Australia and Jigsaw in Ireland)54 – is focused on responsive, hope-oriented delivery of care in a stigma-free, youth-engaging location that is easily accessible via public transportation. More recently, in the USA, the Institute for Mental Health Research (IMHR)-EPICENTER55 in Phoenix, AZ, USA, utilized youth-friendly considerations in selecting the location and designing the clinical spaces to promote engagement with care. This process involved selecting a centrally located building that is easily accessible via public transportation and within walking distance to other sites of interest to young adults (eg, coffee shops, libraries, educational organizations). The interior of the selected building was also designed to create an inviting, nonstigmatizing youth environment that would be conducive to prolonged periods of “hanging out” with other youth receiving care (ie, televisions, computers with Internet access, video game consoles, ample spread-out seating). The outside, street-facing wall of the IMHR-EPICENTER clinic features a recovery-oriented mural that depicts youth in valued social roles and was painted by a local psychosocial rehabilitation group of individuals with lived experience of mental illness.56
Finally, the way that each treatment program creates intraorganizational relationships will impact access to care for individuals with FEP. The microsystems within each organization are likely to vary (eg, a hospital-based first-episode program will likely have a psychiatric inpatient unit, while most community mental health centers will not), but even smaller organizations will likely have multiple focuses or “care teams” within the same setting. However, routine communication between clinical teams is not necessarily standard, nor are routes for collaboration always easily accessible. Although some young adults with psychosis do access care directly via specialized first-episode programs, many others will make treatment contact via other institutional inroads (ie, inpatient units or primary care)12 – and without frequent communication and collaboration, these young adults may not reach the specialized care they need. Thus, creating ongoing collaboration between clinical services and teams within organizations providing treatment to youth with FEP is another potential avenue for optimizing access to specialized care. Successful approaches will vary based on the individual characteristics of each organization, with common goals of streamlining referral of eligible individuals to specialized FEP treatment as well as providing appropriate integrated consultation and care for the needs of individuals with FEP across specialties (eg, a young adult with FEP receiving specialized care may benefit from meeting with a primary care physician outside of the team to address physical health comorbidities). Organizations with inpatient units represent a particularly relevant opportunity for collaboration, as many youth with FEP have their first treatment contact in this setting.57 Although studies have suggested that individuals with psychosis can benefit from evidence-based psychosocial interventions in the inpatient setting,58 almost all specialized interventions are available only on an outpatient basis. Although it may not be prudent to implement an entire specialized FEP treatment program in the inpatient setting, integrating elements of care can reduce the delay of specialized care in a way that may facilitate greater likelihood to connect with specialized care following discharge.
Localities
The localities level describes a system of organizations and their constituent microsystems, typically within an identifiable geographic locality.25 In terms of optimizing access to high-quality care for individuals with FEP, examples of potential barriers include lack of a proximal specialized care teams providing evidence-based care and poor coordination between mental health stakeholders and other relevant organizations in the community.
Improved availability of specialized care for FEP is a well-recognized need in the treatment community. Further, research has shown that for each additional mile of distance between an individual’s home and specialized care clinic, that individual’s respective DUP increases by 1 month59 – thus highlighting the importance that services are available in proximity to each individual’s community. Thus, one of the greatest accomplishments of the Recovery After an Initial Schizophrenia Episode Early Treatment Programs (RAISE ETP) trial10 may have been the demonstration that evidence-based practices for FEP can successfully be disseminated within the USA community mental health system.50 However, the mental health literature is replete with examples of dissemination projects in which the benefits of evidence-based practices drop precipitously, and may disappear entirely, when transferred from laboratory settings to community settings60,61 – a phenomenon known as the “implementation cliff.”62
To address this concern, many developing community specialized care programs have partnered with one of the five specialized FEP networks/programs with demonstrated clinical efficacy for technical assistance and support. Such community–academic partnerships have been shown to be effective in supporting the dissemination and sustainability of evidence-based practices in community settings.63,64 Yet, literature on effective models of technical assistance is scant.65 Consequently, below we provide a brief overview of the technical assistance model used by one specialized care program – EPICENTER52 – in assisting community agencies to launch new FEP programs. Although this model is only one example and is a developing model, it may serve as a useful foundation for agencies interested in delivering or receiving technical assistance with regard to specialized care for FEP within their respective settings.
The technical assistance model implemented by EPICENTER is guided by self-determination theory,66 which postulates that human motivation and well-being are enhanced via satisfaction of three basic psychological needs: autonomy (ie, choice and volitional control with regard to one’s actions), competence (ie, perceived effectiveness in one’s activities), and relatedness (ie, feeling connected to others in one’s community). Within organization settings, satisfaction of these basic needs has been shown to improve employee job satisfaction and performance, to increase acceptance of organizational change, and to facilitate greater motivation to implement new work practices67 – factors that may be critical in implementing a new evidence-based practice, such as specialized care for FEP, in a community mental health center.68,69 Table 1 summarizes the components of the technical assistance model and the basic psychological need(s) of the developing treatment teams they target.
Table 1.
EPICENTER technical assistance model
| Activity | Goal | Basic psychological need addressed for the CSC team |
|---|---|---|
| 1. Creation of shared vision | • Develop plan for CSC team that is consistent with goals/vision of the CMHC and leverages their existing strengths | • Autonomy |
| • Establish relationship between CMHC and EPICENTER defined by collaboration and cooperation | • Relatedness | |
| 2. In-person training | • Train CMHC staff in CSC interventions and assessments as well as recruitment and engagement strategies | • Autonomy, competence |
| 3. Ongoing consultation | • Provide ongoing assistance and support to CSC team | • Competence |
| • Continue to foster relationship between CMHC and EPICENTER defined by collaboration and cooperation | • Relatedness | |
| 4. Connection with professional learning community | • Connection with other CSC teams to support program sustainability and establish networks for support and further innovation | • Relatedness |
| 5. Program evaluation | • Assess and verify CSC team’s ability to produce improvements in consumer outcomes | • Competence |
| • Monitor and identify implementation of program component that may contribute to consumer outcomes | ||
| 6. Train the trainer | • Facilitate sustainability of CSC team by training CMHC staff member to train new staff and complete future program evaluations for CSC team | • Autonomy, competence |
Abbreviations: CMHC, Community Mental Health Center; CSC, Coordinated Specialty Care; EPICENTER, Early Psychosis Intervention Center.
In sum, EPICENTER technical assistance efforts involve the provision of specialized training in evidence-based practices for FEP and ongoing consultation for treatment implementation that is mindful of the shared vision for each organization. In addition, EPICENTER assists organizations in forging connections within their broader communities. This approach, guided by procedures implemented at the Specialized Treatment Early in Psychosis,12 involves targeted outreach to stakeholder groups that are impacted by and/or provides services to youth with FEP and their family members. Figure 2 shows these stakeholder groups with which FEP teams may endeavor to engage and collaborate. This outreach is crucial in improving awareness of the specialized care program to other organizations in the community and also providing specific instruction on referring youth with FEP and their families to services. Importantly, outreach to these stakeholders does not occur only once, but instead becomes an ongoing, regular pipeline for communication and referrals.
Figure 2.
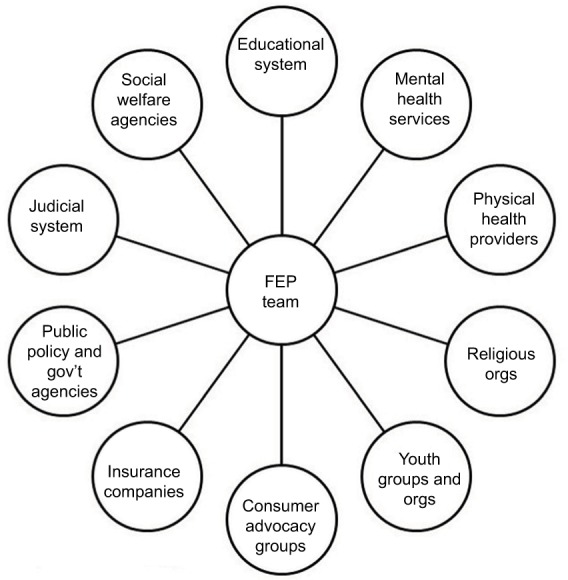
Community stakeholders.
Note: Data from Srihari et al.12
Abbreviation: FEP, first-episode psychosis.
Ongoing collaborations with external organizations likely to interface with youth with FEP are also relevant in connecting individuals with FEP to care as early as possible. As studies have shown, the first point of contact for individuals with onset of psychosis is often a family physician or hospital emergency provider,30 efforts have been made to provide education to healthcare providers to facilitate appropriate referrals to specialized services. Although some research has shown that targeted educational campaigns have potential to reduce delays in the receipt of care,17 other studies have found that similar educational interventions do not result in a significant reduction in delay of referral to specialized care – even when an external specialized first-episode care program is readily available.70 Of note, one study found that if the first treatment contact point for an individual with FEP is in the community mental health setting, the delay in the receipt of specialized intervention services was even longer than for those who presented initially to emergency or crisis services.21 Taken together, these findings highlight the importance of not only expanding the availability of specialized treatment programs but also ensuring that these programs are integrated effectively into their larger communities and interface directly with other community organizations to tap into existing pathways of care.
Macrosystems
The final encompassing level of the ecological model is the macrosystems level, which is characterized by cultural forces, attitudes around change, and other factors that contribute to disparities in care.25 As the outermost level, macrosystems create the context within which other levels operate and are influenced by society-level factors. Examples of factors that have potential to interfere with access to care for FEP at this level include stigma, mental health policy and funding, and disparities in approaches to care.
Stigma surrounding psychotic disorders – meaning the stereotypes and prejudices that result from misinformation and/or misunderstanding about mental illness34 – is of major concern in understanding barriers to treatment. Stigma surrounding schizophrenia and psychotic disorders often includes beliefs that people with these disorders are dangerous and unpredictable,71 despite evidence suggesting any relationship is small and influenced by coexisting factors (ie, substance abuse).72 Although stigma about mental illness is thought to be highly prevalent among the general public, stigmatizing views regarding mental illness are also present among mental health professionals.34,73 Psychosis is further stigmatized via representation in the media and popular culture, with people with psychotic illnesses often portrayed as violent and dangerous in modern horror films,74 horror video games,75 and even media intended for children (eg, cartoons).76 Reviews of US newspapers from 2000 to 2010 found that it is not uncommon to use psychotic disorder diagnoses metaphorically in-print – eg, saying that “the weather will be schizophrenic” when it is thought to be unpredictable or dangerous.77 As modern youth culture is marked by heavy media consumption in various formats,78 these messages are particularly likely to influence perceptions about mental illness among youth with mental health concerns – including those with FEP. These messages have significant potential to be disempowering to youth with FEP – misconceptions about mental illness may lead individuals to believe that mental health concerns are their fault or that they are dangerous or otherwise unwanted in society. Thus, the prevalence of stigma may significantly reduce the likelihood that youth with FEP seek treatment by perpetuating beliefs that they are undesirable, solely responsible for the struggles and symptoms they are facing, or at risk of being given a diagnosis that would render them unable to integrate meaningfully into society. Research demonstrating that stigma interferes with help-seeking behavior among youth is consistent with this reasoning;79 some individuals with psychosis note a desire to avoid a label of an illness which society perceives as negative as a barrier to connecting with services.34 Surveys of individuals with psychosis further reveal that the majority of respondents indicate efforts to conceal their disorders due to significant worry that others may respond unfavorably.80 At minimum, educational campaigns aimed at stigma reduction are warranted. The literature suggests that there is sufficient evidence for the development and rollout of educational programs aimed at reducing stigmatizing beliefs held by individuals.81 The work done by López et al82 to create La CLAve – a culturally minded psychoeducational program to improve mental health literacy among Spanish-speaking individuals in the western USA – is of particular relevance, which has demonstrated a beneficial impact on knowledge regarding symptoms, illness attributions, and willingness to seek help among community members.
The climate around mental health policy and funding also influences accessibility to care. Adequate financing is essential to implementing and maintaining services for individuals with FEP, and evidence suggests that dedicated funds for these services are the best predictor of success.83 Following successful demonstration that specialized care for FEP is effective and can be disseminated into the community, legislation was passed by the US Federal Government providing states with a 5% increase in the Mental Health Block Grants provided by the Substance Abuse and Mental Health Services Administration in 2014 and 2015 to support the dissemination of specialized programs. This funding increased to a 10% in 2016 and has sparked an unprecedented dissemination of specialized care for FEP.84 Despite expansion of funding for specialized care for FEP, many states continue to struggle with financial barriers to program implementation – including insufficient funds to cover operation costs and lack of reimbursement for some components of care.50
Additional strategies include the utilization of funding mechanisms local to each program (eg, opportunities with local or regional mental health boards) and engaging tactics for covering services of uninsured individuals.85 The need for continued innovation and creativity in financing specialized care for FEP is further highlighted by the uncertainty around healthcare accessibility and affordability. For example, federal legislation in the USA that has expanded accessibility and affordability of specialized FEP care (eg, the Affordable Care Act and Medicaid expansion) has an uncertain future and may be disbanded or unfunded. At this time, however, it is certain that continued public support and funding of specialized FEP care will be crucial to its continued expansion and community proliferation.
Last, understanding treatment disparities for FEP is necessary in improving care. The way that physical health is addressed – or not addressed – is of particular relevance among people with psychotic disorders. Adults with psychotic disorders have a shortened life expectancy and are at an increased risk for a variety of physical health problems (eg, cardiovascular disease,86 cancer,87 and diabetes).88 There are limited data for individuals with FEP, but 10-year follow-up data from Norway and Denmark have demonstrated 11-fold increases in all-cause mortality.89 Data from the RAISE ETP study10 showed that first-episode individuals have higher rates of dyslipidemia and prehypertension when compared with age-matched controls.86 Despite elevated rates of health problems and behavioral risk factors, there are significant disparities in how primary care is delivered to individuals with FEP. For example, a recent meta-analysis demonstrated that individuals with schizophrenia were 31% less likely to be prescribed medications for chronic medical conditions compared with individuals without serious mental illnesses.90 This is in line with findings that individuals with serious mental illness were 30% less likely to receive hospital care for cardiovascular disease or diabetes complications or receive blood glucose and lipid tests.91 A more recent study has found that individuals with schizophrenia and coronary heart disease were approximately half as likely to be prescribed recommended medications compared with those without serious mental illness.92 Given the disparities in behavioral risk factors and degree of primary care received, interventions need to be implemented for each individual and within the health system more broadly.93 This approach could include focusing on increasing levels of physical activity and to achieving and maintaining a healthy weight. Although these interventions are not yet widespread, some have been developed for use with people with psychosis.94 Health care–level interventions are also limited, with many aiming at increasing access to care or to health-screening services. We encourage continued development of these initiatives, with a possible future direction of use of algorithms to address prescription disparities. Medication algorithms, created from evidence-based guidelines, have been used to select initial antipsychotic medications for people with FEP.95 However, these types of medication algorithms have not been used to initiate pharmacologic care for comorbid chronic medical conditions.
Conclusion
Given increased research and funding attention given to the treatment of psychotic disorders in their early stages, we have made significant gains in our ability to assist individuals living with these illnesses to recover and live full, meaningful lives. The development and dissemination of specialized care for FEP has been a crucial element of this progress; however, many opportunities for improving access to high-quality care remain. Looking forward, continuing to examine barriers within multiple levels of the ecological model is promising in identifying factors that may be amenable to modification. Navigating this process will require an additional effort to situate these programs effectively and advantageously in their respective communities and cultural contexts. Specifically, the inclusion of other community stakeholders and local knowledge in the development of specialized care programs for FEP has the potential to provide meaningful ideas and input on the specific aspects of content, process, and outcomes for designing a specialized FEP clinical team for a specific locale.23 Finally, although we have made efforts to address factors that influence access to care across multiple levels, the current model is not considered definitive or exhaustive. Additional needs remain, including improving our understanding of how best to engage difficult-to-reach populations (eg, homeless individuals) and to address cultural needs across different locales and settings. Thus, the current model should only be considered as a heuristic for programs seeking to optimize access to care within their respective settings as well as a guide for future research examining additional factors influencing access to care among individuals with FEP.
Footnotes
Disclosure
Moe and Breitborde have received salary support from the IMHR to support the launch of IMHR’s new clinical service for individuals with FEP. They both have received salary support from the Ohio Department of Mental Health and Addiction Services to support the launch of new clinical services for individuals with FEP in Fairfield County, OH, USA; Franklin County, OH, USA; and Athens County, OH, USA.
References
- 1.Mason P, Harrison G, Glazebrook C, Medley I, Croudace T. The course of schizophrenia over 13 years. A report from the International Study on Schizophrenia (ISoS) coordinated by the World Health Organization. Br J Psychiatry. 1996;169(5):580–586. doi: 10.1192/bjp.169.5.580. [DOI] [PubMed] [Google Scholar]
- 2.Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35(2):383–402. doi: 10.1093/schbul/sbn135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birchwood M, Todd P, Jackson C. Early intervention in psychosis. The critical period hypothesis. Br J Psychiatry Suppl. 1998;172(33):53–59. [PubMed] [Google Scholar]
- 4.Kessler RC, Birnbaum H, Demler O, et al. The prevalence and correlates of nonaffective psychosis in the National Comorbidity Sample Replication (NCS-R) Biol Psychiatry. 2005;58(8):668–676. doi: 10.1016/j.biopsych.2005.04.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cloutier M, Aigbogun MS, Guerin A, et al. The economic burden of schizophrenia in the United States in 2013. J Clin Psychiatry. 2016;77(6):764–771. doi: 10.4088/JCP.15m10278. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman JA, Perkins D, Belger A, et al. The early stages of schizophrenia: speculations on pathogenesis, pathophysiology, and therapeutic approaches. Biol Psychiatry. 2001;50(11):884–897. doi: 10.1016/s0006-3223(01)01303-8. [DOI] [PubMed] [Google Scholar]
- 7.Goldstein MJ. Psycho-education and family treatment related to the phase of a psychotic disorder. Int Clin Psychopharmacol. 1996;11(Suppl 2):77–83. doi: 10.1097/00004850-199605002-00013. [DOI] [PubMed] [Google Scholar]
- 8.Robinson DG, Woerner MG, Alvir JM, et al. Predictors of treatment response from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 1999;156(4):544–549. doi: 10.1176/ajp.156.4.544. [DOI] [PubMed] [Google Scholar]
- 9.Azrin ST, Goldstein AB, Heinssen RK. Expansion of coordinated specialty care for first-episode psychosis in the US. Focal Point: Youth, Young Adults, and Mental Health. 2016;30:9–11. [Google Scholar]
- 10.Kane JM, Robinson DG, Schooler NR, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. Am J Psychiatry. 2016;173(4):362–372. doi: 10.1176/appi.ajp.2015.15050632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srihari VH, Tek C, Kucukgoncu S, et al. First-episode services for psychotic disorders in the U.S. public sector: a pragmatic randomized controlled trial. Psychiatr Serv. 2015;66(7):705–712. doi: 10.1176/appi.ps.201400236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Srihari VH, Tek C, Pollard J, et al. Reducing the duration of untreated psychosis and its impact in the US: the STEP-ED study. BMC Psychiatry. 2014;14(1):335. doi: 10.1186/s12888-014-0335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162(10):1785–1804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- 14.Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005;62(9):975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 15.McGlashan TH. Duration of untreated psychosis in first-episode schizophrenia: marker or determinant of course? Biol Psychiatry. 1999;46(7):899–907. doi: 10.1016/s0006-3223(99)00084-0. [DOI] [PubMed] [Google Scholar]
- 16.Breitborde NJ, Moe AM, Ered A, Ellman LM, Bell EK. Optimizing psychosocial interventions in first-episode psychosis: current perspectives and future perspective. Psychol Res Behav Manag. 2017;10:119–128. doi: 10.2147/PRBM.S111593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Melle I, Larsen TK, Haahr U, et al. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Arch Gen Psychiatry. 2004;61(2):143–150. doi: 10.1001/archpsyc.61.2.143. [DOI] [PubMed] [Google Scholar]
- 18.Chong SA, Mythily S, Verma S. Reducing the duration of untreated psychosis and changing help-seeking behaviour in Singapore. Soc Psychiatry Psychiatr Epidemiol. 2005;40(8):619–621. doi: 10.1007/s00127-005-0948-4. [DOI] [PubMed] [Google Scholar]
- 19.Lloyd-Evans B, Crosby M, Stockton S, et al. Initiatives to shorten duration of untreated psychosis: systematic review. Br J Psychiatry. 2011;198(4):256–263. doi: 10.1192/bjp.bp.109.075622. [DOI] [PubMed] [Google Scholar]
- 20.Jansen JE, Wøldike PM, Haahr UH, Simonsen E. Service user perspectives on the experience of illness and pathway to care in first-episode psychosis: a qualitative study within the TOP project. Psychiatr Q. 2015;86(1):83–94. doi: 10.1007/s11126-014-9332-4. [DOI] [PubMed] [Google Scholar]
- 21.Birchwood M, Connor C, Lester H, et al. Reducing duration of untreated psychosis: care pathways to early intervention in psychosis services. Br J Psychiatry. 2013;203(1):58–64. doi: 10.1192/bjp.bp.112.125500. [DOI] [PubMed] [Google Scholar]
- 22.Anderson KK, Fuhrer R, Malla AK. “There are too many steps before you get to where you need to be”: help-seeking by patients with first-episode psychosis. J Ment Health. 2013;22(4):384–395. doi: 10.3109/09638237.2012.705922. [DOI] [PubMed] [Google Scholar]
- 23.Trickett EJ. Multilevel community-based culturally situated interventions and community impact: an ecological perspective. Am J Community Psychol. 2009;43(3–4):257–266. doi: 10.1007/s10464-009-9227-y. [DOI] [PubMed] [Google Scholar]
- 24.Saegert SC, Klitzman S, Freudenberg N, Cooperman-Mroczek J, Nassar S. Healthy housing: a structured review of published evaluations of US interventions to improve health by modifying housing in the United States, 1990–2001. Am J Public Health. 2003;93(9):1471–1477. doi: 10.2105/ajph.93.9.1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dalton JH, Elias MJ, Wandersman A. Community Psychology: Linking Individuals and Communities. Belmont: Thomson Wadsworth; 2001. [Google Scholar]
- 26.Bronfenbrenner U. The Ecology of Human Development. Cambridge: Harvard University; 1979. [Google Scholar]
- 27.Birchwood M, Trower P, Brunet K, Gilbert P, Iqbal Z, Jackson C. Social anxiety and the shame of psychosis: a study in first episode psychosis. Behav Res Ther. 2007;45(5):1025–1037. doi: 10.1016/j.brat.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 28.Kimhy D, Vakhrusheva J, Jobson-Ahmed L, Tarrier N, Malaspina D, Gross JJ. Emotion awareness and regulation in individuals with schizophrenia: implications for social functioning. Psychiatry Res. 2012;200(2–3):193–201. doi: 10.1016/j.psychres.2012.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skeate A, Jackson C, Birchwood M, Jones C. Duration of untreated psychosis and pathways to care in first-episode psychosis. Br J Psychiatry Suppl. 2002;43:s73–s77. doi: 10.1192/bjp.181.43.s73. [DOI] [PubMed] [Google Scholar]
- 30.Norman RM, Malla AK, Verdi MB, Hassall LD, Fazekas C. Understanding delay in treatment for first-episode psychosis. Psychol Med. 2004;34(2):255–266. doi: 10.1017/s0033291703001119. [DOI] [PubMed] [Google Scholar]
- 31.Reed SI. First-episode psychosis: a literature review. Int J Ment Health Nurs. 2008;17(2):85–91. doi: 10.1111/j.1447-0349.2008.00515.x. [DOI] [PubMed] [Google Scholar]
- 32.Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. 2012;67(3):231–243. doi: 10.1037/a0025957. [DOI] [PubMed] [Google Scholar]
- 33.Rickwood DJ, Deane FP, Wilson CJ. When and how do young people seek professional help for mental health problems? Med J Aust. 2007;187(7 Suppl):S35–S39. doi: 10.5694/j.1326-5377.2007.tb01334.x. [DOI] [PubMed] [Google Scholar]
- 34.Corrigan PW, Watson AC. Understanding the impact of stigma on people with mental illness. World Psychiatry. 2002;1(1):16–20. [PMC free article] [PubMed] [Google Scholar]
- 35.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20(4):359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arnett JJ. Emerging adulthood: a theory of development from the late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 37.Addington J, Penn D, Woods SW, Addington D, Perkins DO. Social functioning in individuals at clinical high risk for psychosis. Schizophr Res. 2008;99(1):119–124. doi: 10.1016/j.schres.2007.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Horan WP, Subotnik KL, Snyder KS, Nuechterlein KH. Do recent-onset schizophrenia patients experience a “social network crisis”? Psychiatry. 2006;69(2):115–129. doi: 10.1521/psyc.2006.69.2.115. [DOI] [PubMed] [Google Scholar]
- 39.Trotta A, Di Forti M, Mondelli V, et al. Prevalence of bullying victimisation amongst first-episode psychosis patients and unaffected controls. Schizophr Res. 2013;150(1):169–175. doi: 10.1016/j.schres.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Campbell ML, Morrison AP. The relationship between bullying, psychotic-like experiences and appraisals in 14–16-year olds. Behav Res Ther. 2007;45(7):1579–1591. doi: 10.1016/j.brat.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 41.Spear LP. Neurobehavioral changes in adolescence. Curr Dir Psychol Sci. 2000;9(4):111–114. [Google Scholar]
- 42.Franz L, Carter T, Leiner AS, Bergner E, Thompson NJ, Compton MT. Stigma and treatment delay in first-episode psychosis: a grounded theory study. Early Interv Psychiatry. 2010;4(1):47–56. doi: 10.1111/j.1751-7893.2009.00155.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Anderson KK, Fuhrer R, Wynant W, Abrahamowicz M, Buckeridge DL, Malla A. Patterns of health services use prior to a first diagnosis of psychosis: the importance of primary care. Soc Psychiatry Psychiatr Epidemiol. 2013;48(9):1389–1398. doi: 10.1007/s00127-013-0665-3. [DOI] [PubMed] [Google Scholar]
- 44.Lincoln C, Harrigan S, McGorry PD. Understanding the topography of the early psychosis pathways: an opportunity to reduce delays in treatment. Br J Psychiatry Suppl. 1998;172(33):21–25. [PubMed] [Google Scholar]
- 45.McFarlane WR. Multifamily Groups in the Treatment of Severe Psychiatric Disorders. New York: Guilford Press; 2004. [Google Scholar]
- 46.Breitborde NJ, Woods SW, Srihari VH. Multifamily psychoeducation for first-episode psychosis: a cost-effectiveness analysis. Psychiatr Serv. 2009;60(11):1477–1483. doi: 10.1176/ps.2009.60.11.1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mackrell L, Lavender T. Peer relationships in adolescents experiencing a first episode of psychosis. J Ment Health. 2004;13(5):467–479. [Google Scholar]
- 48.McGorry P, Bates T, Birchwood M. Designing youth mental health services for the 21st century: examples from Australia, Ireland and the UK. Br J Psychiatry Suppl. 2013;54:s30–s35. doi: 10.1192/bjp.bp.112.119214. [DOI] [PubMed] [Google Scholar]
- 49.Dixon LB, Goldman HH, Bennett ME, et al. Implementing coordinated specialty care for early psychosis: the RAISE Connection Program. Psychiatr Serv. 2015;66(7):691–698. doi: 10.1176/appi.ps.201400281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Breitborde NJK, Moe AM. Early intervention in psychosis in the United States: from science to policy reform. Policy Insights Behav Brain Sci. 2017;4(1):79–87. [Google Scholar]
- 51.Uzenoff SR, Penn DL, Graham KA, Saade S, Smith BB, Perkins DO. Evaluation of a multi-element treatment center for early psychosis in the United States. Soc Psychiatry Psychiatr Epidemiol. 2012;47(10):1607–1615. doi: 10.1007/s00127-011-0467-4. [DOI] [PubMed] [Google Scholar]
- 52.Breitborde NJ, Bell EK, Dawley D, et al. The Early Psychosis Intervention Center (EPICENTER): development and six-month outcomes of an American first-episode psychosis clinical service. BMC Psychiatry. 2015;15:266. doi: 10.1186/s12888-015-0650-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McGorry PD. The specialist youth mental health model: strengthening the weakest link in the public mental health system. Med J Aust. 2007;187(7 Suppl):S53–S56. doi: 10.5694/j.1326-5377.2007.tb01338.x. [DOI] [PubMed] [Google Scholar]
- 54.Malla A, Iyer S, McGorry P, et al. From early intervention in psychosis to youth mental health reform: a review of the evolution and transformation of mental health services for young people. Soc Psychiatry Psychiatr Epidemiol. 2016;51(3):319–326. doi: 10.1007/s00127-015-1165-4. [DOI] [PubMed] [Google Scholar]
- 55.Breitborde NJK, Labreque L, Moe AM, Gary T, Meyer M. Community-academic partnership: establishing the Institute for Mental Health Research Early Psychosis Intervention Center. Psychiat Serv. 2018;69(5):505–507. doi: 10.1176/appi.ps.201700516. [DOI] [PubMed] [Google Scholar]
- 56.Breitborde NJK, Labrecque L, Moe A, Gary T, Meyer M. Community-academic partnership: establishing the Institute for Mental Health Research Early Psychosis Intervention Center (IMHR-EPICENTER) 2018;69(5):505–507. doi: 10.1176/appi.ps.201700516. [DOI] [PubMed] [Google Scholar]
- 57.Anderson KK, Fuhrer R, Malla AK. The pathways to mental health care of first-episode psychosis patients: a systematic review. Psychol Med. 2010;40(10):1585–1597. doi: 10.1017/S0033291710000371. [DOI] [PubMed] [Google Scholar]
- 58.Haddock G, Tarrier N, Morrison AP, Hopkins R, Drake R, Lewis S. A pilot study evaluating the effectiveness of individual inpatient cognitive-behavioural therapy in early psychosis. Soc Psychiatry Psychiatr Epidemiol. 1999;34(5):254–258. doi: 10.1007/s001270050141. [DOI] [PubMed] [Google Scholar]
- 59.Breitborde NJK, Woods SW, Pollard J, et al. Age and social support moderate the relationship between geographical location and access to early intervention programs for first-episode psychosis. Early Interv Psychiatry. 2008;2:A73. [Google Scholar]
- 60.Bickman L. Continuum of care. More is not always better. Am Psychol. 1996;51(7):689–701. doi: 10.1037//0003-066x.51.7.689. [DOI] [PubMed] [Google Scholar]
- 61.Weisz JR, Han SS, Valeri SM. More of what? Issues raised by the Fort Bragg study. Am Psychol. 1997;52(5):541–545. doi: 10.1037//0003-066x.52.5.541. [DOI] [PubMed] [Google Scholar]
- 62.Weisz JR, Ng MY, Bearman SK. Odd couple? Reenvisioning the relation between science and practice in the dissemination-implementation era. Clin Psychol Sci. 2014;2(1):58–74. [Google Scholar]
- 63.Marty D, Rapp C, McHugo G, Whitley R. Factors influencing consumer outcome monitoring in implementation of evidence-based practices: results from the National EBP Implementation Project. Adm Policy Ment Health. 2008;35(3):204–211. doi: 10.1007/s10488-007-0157-4. [DOI] [PubMed] [Google Scholar]
- 64.Lindamer LA, Lebowitz BD, Hough RL, et al. Public-academic partnerships: Improving care for older persons with schizophrenia through an academic-community partnership. Psychiatr Serv. 2008;59(3):236–239. doi: 10.1176/appi.ps.59.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Salyers MP, McKasson M, Bond GR, McGrew JH, Rollins AL, Boyle C. The role of technical assistance centers in implementing evidence-based practices: lessons learned. Am J Psychiatr Rehab. 2007;10(2):85–101. [Google Scholar]
- 66.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 67.Gagné M, Deci EL. Self-determination theory and work motivation. J Organ Behav. 2005;26(4):331–362. [Google Scholar]
- 68.Aarons GA. Mental health provider attitudes toward adoption of evidence-based practice: the Evidence-Based Practice Attitude Scale (EBPAS) Ment Health Serv Res. 2004;6(2):61–74. doi: 10.1023/b:mhsr.0000024351.12294.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aarons GA, Wells RS, Zagursky K, Fettes DL, Palinkas LA. Implementing evidence-based practice in community mental health agencies: a multiple stakeholder analysis. Am J Pub Health. 2009;99(11):2087–2095. doi: 10.2105/AJPH.2009.161711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Malla A, Jordan G, Joober R, et al. A controlled evaluation of a targeted early case detection intervention for reducing delay in treatment of first episode psychosis. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1711–1718. doi: 10.1007/s00127-014-0893-1. [DOI] [PubMed] [Google Scholar]
- 71.Levey S, Howells K, Levey S. Dangerousness, unpredictability and the fear of people with schizophrenia. J Forens Psychiatry. 1995;6(1):19–39. [Google Scholar]
- 72.Walsh E, Buchanan A, Fahy T. Violence and schizophrenia: examining the evidence. Br J Psychiatry. 2002;180(6):490–495. doi: 10.1192/bjp.180.6.490. [DOI] [PubMed] [Google Scholar]
- 73.Nordt C, Rössler W, Lauber C. Attitudes of mental health professionals toward people with schizophrenia and major depression. Schizophr Bull. 2006;32(4):709–714. doi: 10.1093/schbul/sbj065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Goodwin J. The horror of stigma: psychosis and mental health care environments in twenty-first-century horror film (Part II) Perspect Psychiatr Care. 2014;50(4):224–234. doi: 10.1111/ppc.12044. [DOI] [PubMed] [Google Scholar]
- 75.Dickens EG. An evaluation of mental health stigma perpetuated by Horror Video gaming. Young Res. 2017;1(1):108–117. [Google Scholar]
- 76.Wahl O. Depictions of mental illnesses in children’s media. J Ment Health. 2003;12(3):249–258. [Google Scholar]
- 77.Vahabzadeh A, Wittenauer J, Carr E. Stigma, schizophrenia and the media: exploring changes in the reporting of schizophrenia in major U.S. newspapers. J Psychiatr Pract. 2011;17(6):439–446. doi: 10.1097/01.pra.0000407969.65098.35. [DOI] [PubMed] [Google Scholar]
- 78.Livingstone S. Young People and New Media: Childhood and the Changing Media Environment. London: Sage; 2002. [Google Scholar]
- 79.Gronholm PC, Thornicroft G, Laurens KR, Evans-Lacko S. Mental health-related stigma and pathways to care for people at risk of psychotic disorders or experiencing first-episode psychosis: a systematic review. Psychol Med. 2017;47(11):1867–1879. doi: 10.1017/S0033291717000344. [DOI] [PubMed] [Google Scholar]
- 80.Wahl OF. Mental health consumers: experience of stigma. Schizophr Bull. 1999;25(3):467–478. doi: 10.1093/oxfordjournals.schbul.a033394. [DOI] [PubMed] [Google Scholar]
- 81.Griffiths KM, Carron-Arthur B, Parsons A, Reid R. Effectiveness of programs for reducing the stigma associated with mental disorders. A meta-analysis of randomized controlled trials. World Psychiatry. 2014;13(2):161–175. doi: 10.1002/wps.20129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.López SR, Lara Mdel DC, Kopelowicz A, Solano S, Foncerrada H, Aguilera A. La CLAve to increase psychosis literacy of Spanish-speaking community residents and family caregivers. J Consult Clin Psychol. 2009;77(4):763–774. doi: 10.1037/a0016031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Catts SV, O’Toole BI, Carr VJ, et al. Appraising evidence for intervention effectiveness in early psychosis: conceptual framework and review of evaluation approaches. Austr N Z J Psychiatry. 2010;44(3):195–219. doi: 10.3109/00048670903487167. [DOI] [PubMed] [Google Scholar]
- 84.Heinssen R, McGorry P, Nordentoft M. RAISE 2.0: establishing a national Early Psychosis Intervention Network in the US. Early Interv Psychiatry. 2016;10(Suppl 1):4. [Google Scholar]
- 85.Goldman HH, Karakus M, Frey W, Beronio K. Economic grand rounds: financing FEP services in the United States. Psychiatr Serv. 2013;64(6):506–508. doi: 10.1176/appi.ps.201300106. [DOI] [PubMed] [Google Scholar]
- 86.Correll CU, Robinson DG, Schooler NR, et al. Cardiometabolic risk in patients with first-episode schizophrenia spectrum disorders: baseline results from the RAISE-ETP study. JAMA Psychiatry. 2014;71(12):1350–1363. doi: 10.1001/jamapsychiatry.2014.1314. [DOI] [PubMed] [Google Scholar]
- 87.Olfson M, Gerhard T, Huang C, Crystal S, Stroup TS. Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry. 2015;72(12):1172–1181. doi: 10.1001/jamapsychiatry.2015.1737. [DOI] [PubMed] [Google Scholar]
- 88.Vancampfort D, Correll CU, Wampers M, et al. Metabolic syndrome and metabolic abnormalities in patients with major depressive disorder: a meta-analysis of prevalences and moderating variables. Psychol Med. 2014;44(10):2017–2028. doi: 10.1017/S0033291713002778. [DOI] [PubMed] [Google Scholar]
- 89.Melle I, Olav Johannesen J, Haahr UH, et al. Causes and predictors of premature death in first-episode schizophrenia spectrum disorders. World Psychiatry. 2017;16(2):217–218. doi: 10.1002/wps.20431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mitchell AJ, Lord O, Malone D. Differences in the prescribing of medication for physical disorders in individuals with v. without mental illness: meta-analysis. Br J Psychiatry. 2012;201(6):435–443. doi: 10.1192/bjp.bp.111.094532. [DOI] [PubMed] [Google Scholar]
- 91.Scott D, Platania-Phung C, Happell B. Quality of care for cardiovascular disease and diabetes amongst individuals with serious mental illness and those using antipsychotic medications. J Healthc Qual. 2012;34(5):15–21. doi: 10.1111/j.1945-1474.2011.00155.x. [DOI] [PubMed] [Google Scholar]
- 92.Woodhead C, Ashworth M, Broadbent M, et al. Cardiovascular disease treatment among patients with severe mental illness: a data linkage study between primary and secondary care. Br J Gen Pract. 2016;66(647):e374–e381. doi: 10.3399/bjgp16X685189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Liu NH, Daumit GL, Dua T, et al. Excess mortality in persons with severe mental disorders: a multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry. 2017;16(1):30–40. doi: 10.1002/wps.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Naslund JA, Whiteman KL, McHugo GJ, Aschbrenner KA, Marsch LA, Bartels SJ. Lifestyle interventions for weight loss among overweight and obese adults with serious mental illness: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2017;47:83–102. doi: 10.1016/j.genhosppsych.2017.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Yeisen RA, Joa I, Johannessen JO, Opjordsmoen S. Use of medication algorithms in first episode psychosis: a naturalistic observational study. Early Interv Psychiatry. 2016;10(6):503–510. doi: 10.1111/eip.12203. [DOI] [PubMed] [Google Scholar]