Abstract
Introduction
E-cigarettes (Electronic Nicotine Delivery Systems, or ENDS) are an increasingly popular tobacco product among youth. Some evidence suggests that e-cigarettes may be effective for harm reduction and smoking cessation, although these claims remain controversial. Little is known about how nicotine dependence may contribute to e-cigarettes’ effectiveness in reducing or quitting conventional smoking.
Methods
A cohort of young adults were surveyed over 4 years (approximately ages 19–23). Varying-coefficient models (VCMs) were used to examine the relationship between e-cigarette use and conventional smoking frequency, and how this relationship varies across users with different nicotine dependence levels.
Results
Lifetime, but not recent, e-cigarette use was associated with less frequent concurrent smoking of conventional cigarettes among those with high levels of nicotine dependence. However, nondependent e-cigarette users smoked conventional cigarettes slightly more frequently than those who had never used e-cigarettes. Nearly half of ever e-cigarette users reported using them to quit smoking at the last measurement wave. For those who used e-cigarettes in a cessation attempt, the frequency of e-cigarette use was not associated with reductions in future conventional smoking frequency.
Conclusions
These findings offer possible support that e-cigarettes may act as a smoking reduction method among highly nicotine-dependent young adult cigarette smokers. However, the opposite was found in non-dependent smokers, suggesting that e-cigarette use should be discouraged among novice tobacco users. Additionally, although a substantial proportion of young adults used e-cigarettes to help them quit smoking, these self-initiated quit attempts with e-cigarettes were not associated with future smoking reduction or cessation.
Implications
This study offers potential support for e-cigarettes as a smoking reduction tool among highly nicotine-dependent young adult conventional smokers, although the extent and nature of this remains unclear. The use of e-cigarettes as a quit aid was not associated with reductions in conventional smoking, consistent with most other quit aids in this sample except for nicotine replacement therapy, which was only effective for the most dependent smokers. Notably, these findings highlight the necessity of accounting for smokers’ nicotine dependence levels when examining tobacco use patterns.
Introduction
The use of Electronic Nicotine Delivery Systems (ENDS) or electronic cigarettes (“e-cigarettes”) has drastically increased over the recent years,1,2 and this trend has outpaced research on the implications of e-cigarette use for overall use of any tobacco product, nicotine addiction, and health outcomes. As a result, there is currently little consensus on e-cigarettes in terms of their overall risk and safety to tobacco users. On one hand, serious concerns are being raised about e-cigarettes attracting new tobacco users, especially adolescents.3–6 In particular, some argue that e-cigarettes act as a “gateway” to tobacco use for youth by spurring the development of addiction, which in turn increases adolescents’ chances of becoming lifetime users of e-cigarettes and/or conventional cigarettes.3–8
On the other hand, others point to the improvements that e-cigarettes may offer over conventional cigarettes in at least two ways. First, e-cigarettes may be a mechanism for harm reduction due to the lack of combustible components that pose such serious health risks in conventional cigarettes. That is, smokers who use e-cigarettes as a way to replace some of their conventional cigarette smoking are likely reducing their net exposure to tars and toxins, thus reducing their health risks,9–12 although e-cigarettes still contain some amount of toxins and carcinogens.13 A second possibility is that e-cigarettes might be effective at helping conventional smokers quit. In fact, a common reason for the use of e-cigarettes is to help users reduce or quit conventional cigarettes,14–17 and e-cigarettes are often marketed as such.18–21 The evidence for these claims is mixed; however, some limited evidence suggesting that e-cigarettes can help cigarette smokers quit either in randomized studies22 or in real-world settings,23,24 but others showing no effect on cessation.25,26
One important aspect of e-cigarettes that remains understudied is the potential role of nicotine dependence in smokers’ use of e-cigarettes’ to reduce or quit conventional smoking. Despite the implicit assumption that nicotine dependence contributes to the use of, and transitions between, e-cigarettes and conventional smoking, very little research has rigorously examined the role of nicotine dependence, a construct that can be independent of smoking behavior,27 especially among youth.28,29 In particular, both the smoking reduction hypothesis and the cessation aid hypothesis assume that the users have some level of underlying nicotine dependence, since they would be using e-cigarettes as nicotine replacement devices under these explanations. This raises the question of whether nicotine dependence moderates the effects of e-cigarette use on conventional smoking. For example, are e-cigarettes effective for reducing or quitting conventional smoking only among highly nicotine-dependent smokers? Conversely, are they harmful for novice and nondependent conventional smokers by triggering the development of nicotine dependence?
The current study tests the potential of e-cigarettes for smoking reduction and as a cessation aid among a cohort of young adult smokers. Varying coefficient models (VCMs) were used to examine the relationship between e-cigarette use and conventional smoking behavior, and how this relationship varies in strength across tobacco users along the full range of nicotine dependence. To test the smoking reduction hypothesis, we examined the concurrent relationships between e-cigarette use and conventional cigarette use and evaluated whether e-cigarette use was associated with reduced conventional smoking behavior among highly nicotine-dependent smokers. To test the cessation aid hypothesis, we examined whether e-cigarette use predicted future conventional smoking behavior among youth who reported using e-cigarettes to help them quit smoking.
Methods
Sample
Data were drawn from the Social and Emotional Contexts of Adolescent Smoking Patterns (SECASP) Study, a longitudinal cohort study of adolescent smokers in the greater Chicago area. Briefly, 9th and 10th graders from 16 high schools were given a brief screener survey, and those qualifying as novice smokers (smoked <100 cigarettes/lifetime) and light smokers (smoked >100 cigarettes/lifetime and smoked within the past 30 days, but smoked ≤5 cigarettes/day), as well as random samples of nonsmokers, were invited to participate (N = 3654). Of these, 1263 provided their own or their parent’s consent and completed the baseline survey. Full details of sample selection have been described previously.29
Several follow-up surveys were conducted over 8 years after the baseline survey. The current study draws data from the 5-, 6-, 7-, and 8-year follow-up waves, because these contain data on e-cigarette use. Participants were 23.6 years old on average at the 8-year follow-up. Retention at 8 years was 79.7% (n = 1007), and those who remained in the study were more likely to be female (86.9% vs. 70.4%, p < .001) and reported less frequent smoking at baseline (3.6 vs. 4.8 days smoked out of the past 30, p = .03). For the current study, nonsmokers of conventional cigarettes throughout the full-time range under consideration (5- through 8-year follow-up waves) were excluded (n = 421). The final analytic sample size was n = 586, and its demographic and tobacco use characteristics are shown in Table 1.
Table 1.
Demographic and smoking characteristics for analytic sample (n = 586)
| Characteristic | Summarya |
|---|---|
| Sex | |
| Female | 340 (58.0%) |
| Male | 243 (42.0%) |
| Race/ethnicity | |
| White | 445 (75.9%) |
| Nonwhite | 141 (24.1%) |
| Age at 8-year follow-up | 24.3 (0.8) |
| Past-month smoking frequency b | |
| 5-year follow-up | 14.5 (12.5) |
| 6-year follow-up | 14.4 (12.9) |
| 7-year follow-up | 13.8 (13.1) |
| 8-year follow-up | 11.2 (13.1) |
| Lifetime e-cigarette use | |
| 5-year follow-up | 217 (37.0%) |
| 6-year follow-up | 273 (47.2%) |
| 7-year follow-up | 350 (60.0%) |
| 8-year follow-up | 353 (60.0%) |
| Past-month e-cigarette frequency b (ever users) | |
| 5-year follow-up | 0.7 (2.0) |
| 6-year follow-up | 1.0 (3.2) |
| 7-year follow-up | 1.9 (4.5) |
| 8-year follow-up | 1.5 (4.6) |
| Nicotine Dependence Syndrome Scale Score | |
| 5-year follow-up | 2.0 (0.9) |
| 6-year follow-up | 2.1 (0.9) |
| 7-year follow-up | 2.1 (0.9) |
| 8-year follow-up | 2.1 (0.9) |
| Used e-cigarettes to quit (ever users) | |
| 5-year follow-up | 62 (28.6%) |
| 6-year follow-up | 101 (37.0%) |
| 7-year follow-up | 148 (42.4%) |
| 8-year follow-up | 166 (50.8%) |
aCategorical variables are summarized as n (valid percentage) and continuous variables are summarized as mean (standard deviation).
bFrequency is in units of number of days of the past 30.
Measures
Cigarette smoking was measured at each wave as smoking frequency in the past 30 days (“On how many days did you smoke or try cigarettes?”). Original response categories were 0, 1, 2–3, 4–5, 6–7, 8–10, 11–20, 21–29, and all 30 days, and this was used as a numeric variable based on the midpoint of each category. A measure of frequency rather than quantity (e.g., cigarettes per day) was selected as the outcome, due to prior research showing that frequency is a consistent, strong predictor of nicotine dependence among this sample.28–30
Lifetime e-cigarette use was measured at each wave as either “Have you ever tried e-cigarettes” (5- through 7-year waves) with a binary response or “How many e-cigarettes have you used in your entire life?” (8-year wave) with 8 possible response options ranging from “never used a cartridge/e-cig” to “500 or more cartridges/e-cigs.” The responses from the 8-year wave were dichotomized into never versus any e-cigarette use in order to harmonize the variable with previous waves.
Recent e-cigarette use was measured at each wave as the number of days the participant reported using e-cigarettes in the past 30 days. Original response categories were “0,” “1–2,” “3–5,” “6–9,” “10–19,” “20–29,” and “all 30 days.” These responses were coded numerically as the midpoint of each category for these analyses.
Nicotine dependence was measured using a version of the Nicotine Dependence Syndrome Scale (NDSS)31 which was adopted for use in adolescent smokers32,33 into a 10-item scale that mainly reflect “drive” and “tolerance” dimensions of nicotine dependence. Each item was assessed on a 1–4 scale, and the 10 items were averaged into a combined NDSS score.
Quit attempts were self-reported as a binary (yes/no) variable at each wave. Only data from the 5-year follow-up was analyzed. Separate items assessed quit attempts using: e-cigarettes (n = 74); a smoking cessation group (n = 7); a help or quit line (n = 1); an internet help site (n = 19); Zyban (n = 7); Chantix (n = 7); an herbal strategy (n = 23); and nicotine replacement products (n = 49). Due to small sample size, quit attempts using a smoking cessation group, help or quit line, and Internet help site were combined into a single category; and Zyban and Chantix were combined into a single category.
Past-week smoking quantity was measured at each wave using the question “during the last 7 days, how many cigarettes did you smoke?”
Demographic characteristics included age, sex, and race/ethnicity (dichotomized as white vs. non-white).
Analyses
VCMs were used to examine how the relationship between cigarette smoking and e-cigarette use is modified across the severity of nicotine dependence. VCMs were run using a publicly available SAS macro,34 version 3.1.0, developed for analyzing time-varying effects of intensive longitudinal data. VCMs are regression-based models that examine moderation continuously across a variable (most often a time variable) without imposing strong parametric assumptions about the shape of the nature of the change (e.g., specifying that the coefficient varies in a linear or quadratic manner across the range of the moderating variable).35 Instead, the curve is estimated empirically using spline methods, by fitting a lower order polynomial curve within each interval based on the user-specified number of knots.35 This TVEM macro produces coefficient estimates along the range of the moderating variable, along with corresponding 95% confidence bands. Here, VCMs were run to examine moderation along the range of nicotine dependence (rather than time), which we refer to as “nicotine dependence varying effects.” Nicotine dependence varying effects were interpreted with respect to whether the 95% confidence band is different from 0 (conservatively indicating a statistically significant coefficient), and whether the confidence bands overlap (nonoverlapping bands conservatively indicate a significant change in the coefficient), across different values of nicotine dependence. Separate models were used to test the two hypotheses as described below. All VCM’s were run with P-spline estimation and 10 knots.
Smoking Reduction Hypothesis
We examined whether e-cigarette use is associated with cigarette smoking and whether this association differs across tobacco users with varying levels of nicotine dependence. We used VCM’s to examine the nicotine-dependence-varying relationship between (1) lifetime and (2) recent e-cigarette use and past-month smoking frequency. A nicotine dependence varying intercept was also included to account for differences in mean smoking frequency across the range of nicotine dependence. All time points were pooled in this analysis both to increase sample size and because we did not anticipate large differences in the effect from year to year. Multilevel modeling was used to account for repeated observations. Control variables included age, sex, white race/ethnicity, and past week smoking quantity. Under the smoking reduction hypothesis, e-cigarette use would be negatively associated with conventional cigarette smoking (i.e., a significant and negative coefficient), reflecting that smokers are replacing conventional cigarettes with e-cigarettes as a source of nicotine, especially among those who are highly nicotine dependent (i.e., a larger negative effect at high values of nicotine dependence).
Cessation Aid Hypothesis
We next examined the potential viability of e-cigarettes as a smoking cessation aid within our sample. In order to preserve the temporality of this relationship, we analyzed smoking frequency at the next sequential wave as the outcome. This resulted in three possible pairs of time points: e-cigarette use at 5 years with smoking at 6 years, e-cigarette use at 6 years with smoking at 7 years, and e-cigarette use at 7 years with smoking at 8 years; e-cigarette use at 8 years was not examined due to the lack of data on future smoking. Using VCMs, we examined the relationship between recent e-cigarette frequency and future smoking frequency and how this likelihood differs across tobacco users with varying levels of nicotine dependence, while controlling for concurrent smoking frequency, concurrent smoking quantity, age, sex, and white race/ethnicity. Separate models were run for observations in which participants reported having used e-cigarettes to quit and those in which they did not. Under the cessation aid hypothesis, (1) we would expect the odds of using e-cigarettes as a cessation aid to increase among more nicotine-dependent conventional smokers, and (2) among those who use e-cigarettes as a cessation aid, lifetime e-cigarette use should be associated with reductions in future smoking frequency, consistent with a nicotine replacement approach. For comparison purposes, similar follow-up models were run examining other quit methods.
Results
Smoking Reduction Hypothesis
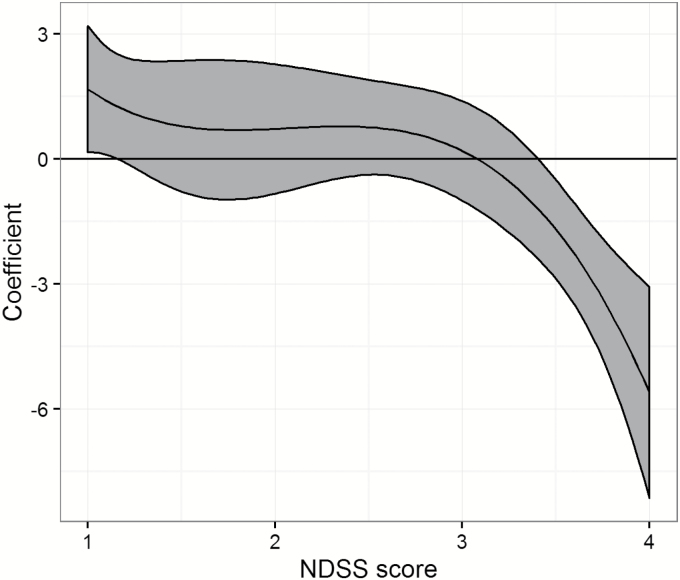
A VCM revealed that among participants who smoked at least once during the included time range, the relationship between lifetime e-cigarette use and smoking frequency substantially varied across those with different levels of nicotine dependence, after adjusting for age, sex, white race/ethnicity, past-week smoking quantity, and a time-varying intercept that allows different smoking frequencies as a function of nicotine dependence (Figure 1). Among participants with very low dependence (NDSS < 1.2), those who ever smoked e-cigarettes smoked slightly more frequently (by at most a coefficient (B) of 1.8 days out of the past month, 95% confidence interval [CI]: 0.2 to 3.2]), whereas among cigarette smokers with severe nicotine dependence (NDSS > 3.4), those who also ever used e-cigarettes smoked conventional cigarettes less frequently (by at most B = 5.6 fewer days, CI: [−8.2 to −3.1]). For those with moderate nicotine dependence (NDSS between 1.2 and 3.4), lifetime e-cigarette use had no significant effect on smoking frequency as shown by the confidence interval (CI) including zero (average B = 0.5 days, average CI: [−0.8 to 1.9).
Figure 1.
Effect of lifetime e-cigarette use on concurrent smoking frequency, moderated by nicotine dependence level. The horizontal line indicates no effect (coefficient = 0).
In contrast, recent (past-month) e-cigarette use was not associated with differences in past-month smoking frequency at any level of nicotine dependence (data not shown).
Cessation Aid Hypothesis
By wave 8, nearly half of cigarette smokers who ever used e-cigarettes reported using them to quit smoking at some point. First, a VCM was run to examine the nicotine dependence varying odds of using e-cigarettes to quit smoking. After controlling for age, sex, white race/ethnicity, and past-week smoking frequency, the odds of using e-cigarettes to quit smoking were nonsignificant across the full range of NDSS (results not shown). This indicates that a participant’s nicotine dependence did not moderate the odds of using e-cigarettes to quit smoking.
Next, the nicotine dependence varying effects of e-cigarette use on future smoking frequency were examined after accounting for prior smoking behavior and demographic factors (Figure 2). Among those who reported using e-cigarettes to quit smoking, the frequency of recent e-cigarette use was not associated with future cigarette smoking frequency, as indicated by the confidence band overlapping 0 throughout the range of nicotine dependence (average B = 0.1 days out of the past month, CI: −0.2 to 0.4]). On the other hand, among those who did not use e-cigarettes to quit smoking, recent e-cigarette use was associated with more frequent smoking for those at very low (NDSS < 1.2, by at most B = 1.1 days out of the past month, CI: 0.2 to 2.0) and high (NDSS between 3.1 and 3.8, by on average B = 0.9 days, CI: 0.2 to 1.6) levels of nicotine dependence.
Figure 2.
Effect of recent e-cigarette frequency on future conventional smoking frequency, moderated by nicotine dependence level and stratified by those who had used e-cigarettes to quit versus those who did not. Horizontal line indicates no effect (coefficient = 0).
To compare the use of e-cigarettes as a quit aid with other methods of quitting, follow-up VCMs were run examining the nicotine dependence varying effects of (1) seeking support from a cessation group, Internet, or phone resource; (2) using a prescription (Zyban or Chantix), (3) using an herbal strategy; and (4) using nicotine replacement products (all reported at the 5-year follow-up wave) on future smoking frequency (data not shown). Of these methods, only nicotine replacement products were significantly associated with later reductions in smoking frequency (by up to 11 fewer days smoked out of the past month) and only among those with the highest levels of nicotine dependence (NDSS > 3.7). Among less-dependent cigarette smokers, nicotine replacement therapy was not significantly associated (either positively or negatively) with later smoking frequency.
Discussion
This study examines the longitudinal association between e-cigarette use and conventional cigarette smoking behavior among a cohort of young adults. Importantly, we examined the moderation of these relationships by nicotine dependence severity, a factor essential to understanding the interrelationships of tobacco products, using VCM’s. In general, the relationship between lifetime e-cigarette use and conventional smoking is substantially impacted by nicotine dependence level. In particular, highly nicotine-dependent smokers tend to smoke conventional cigarettes less frequently if they ever used e-cigarettes, while the opposite was observed in nondependent smokers. However, nicotine dependence did not appear to moderate the use of use e-cigarettes for the purpose of conventional smoking reduction or cessation.
The finding that highly dependent cigarette smokers tend to smoke less frequently if they ever used e-cigarettes may indicate diversification of tobacco products. That is, highly dependent smokers may be replacing some of their conventional cigarette smoking with e-cigarettes.36 If true, e-cigarettes may be an effective method of harm reduction, since many of the harmful effects of cigarettes are due to combustible elements.9,12 On the other hand, those with very low nicotine dependence smoked slightly more frequently if they ever used e-cigarettes, which may warrant warning youth against initiating e-cigarette use.11,37 In considering whether e-cigarettes pose a net harm or benefit, the magnitudes of effect (larger for the reduction in smoking frequency) and the population distribution along the nicotine dependence range (larger for less-dependent smokers) must be weighed against each other. Alternatively, however, the fact that no concurrent relationship was observed raises another possibility that dual users of e-cigarettes and conventional cigarettes are a different subpopulation than exclusive cigarette smokers who may differ in their smoking frequencies due to other reasons.
Although the safety and long-term outcomes of e-cigarettes are still uncertain, previous work argues that e-cigarettes may be valuable as a harm reduction approach.9–11,13 The current findings support this to some extent, under the assumption that these smokers are replacing conventional smoking with e-cigarettes to some extent.36,37 However, the extent and temporality of any such replacement is unclear since recent e-cigarette use was not associated with reductions in concurrent smoking. This warrants further research with larger sample sizes of dual users. If these findings are validated in future research, e-cigarettes are likely to have the biggest positive impact on highly dependent smokers, both because they show the biggest reduction in conventional smoking and because they are the smokers most likely to persist smoking in the long term.
Additionally, our findings fail to support e-cigarettes as a tool for quitting conventional smoking. Specifically, more nicotine-dependent cigarette smokers are not more likely to use e-cigarettes to quit smoking, and those who did use e-cigarettes to quit did not show decreases in future cigarette smoking that were explained by e-cigarette use.
The lack of support for the cessation aid hypothesis may indicate that e-cigarettes are truly not effective for quitting conventional cigarette smoking; however, e-cigarettes were comparable to other quit methods in this respect, with the exception of nicotine replacement among severely nicotine-dependent cigarette smokers. Overall, e-cigarettes were not more effective than nicotine replacement in reducing subsequent smoking frequency. This finding is consistent with previous research showing that e-cigarette use is not significantly associated with later cigarette abstinence.25,26 Alternatively, these findings may indicate a lack of statistical power to detect an underlying effect. Limitations of the existing data set, namely, that we could not fully separate e-cigarette use during a cessation attempt from recreational e-cigarette use may have weakened the effect and made it more difficult to detect in our data.
The cessation potential of e-cigarettes is still a matter of active debate, and more well-controlled trials are needed to help shed light on this question. As described above, some research has failed to find e-cigarettes effective as a quit aid. On the other hand, other randomized studies concluded that e-cigarettes can be somewhat effective as a cessation aid, 22 and other studies of real-world quit attempts showed that e-cigarettes were more effective than traditional nicotine replacement therapy in maintaining abstinence.23,24 These studies suffered from notable limitations, however: Of the real-world studies, one was cross-sectional23 and the other presented only 3 individual cases.24 Further research is needed to examine whether e-cigarettes can be a cessation aid, especially in relation to the underlying nicotine dependence level.
This study extends existing research in critical ways, primarily in relation to how nicotine dependence may alter the relationship between e-cigarette use and conventional smoking. This is a notable gap, considering that many hypotheses about the implications of e-cigarettes assume the development or presence of nicotine dependence, either implicitly or explicitly. For example, e-cigarettes would only be effective in reducing or eliminating conventional smoking behavior if nicotine dependence prompts the smoker to seek out nicotine in other ways. Thus, examining nicotine dependence is an essential part of understanding the relationship between e-cigarettes and conventional cigarettes, and our findings show that the tobacco use patterns of highly nicotine-dependent users differ greatly from those with very low levels of nicotine dependence.
The current study has several limitations which should be taken into account. First, these data are observational in nature. This limits our ability to draw causal conclusions in general, and additionally may limit the analysis on the cessation potential of e-cigarettes, relative to experimental studies. However, studying self-initiated cessation attempts in participants’ natural environments is also valuable because it is likely to be more realistic. Second, these analyses are limited by the available variables, especially regarding e-cigarette use. In particular, lifetime and recent e-cigarette use did not separate use during quit attempts from recreational use; thus, those who used e-cigarettes to quit smoking may have also used e-cigarettes recreationally outside the quit attempt. This may have weakened the effects in the analysis of their potential for cessation. Third, the varying effects of nicotine dependence were examined across subjects, not within subjects, meaning these trends may reflect different types of tobacco users rather than direct effects of increasing individuals’ levels of nicotine dependence. Fourth, dependence on e-cigarettes is currently not well-studied, and thus the current study is unable to distinguish nicotine dependence due to e-cigarettes vs. conventional cigarettes. Finally, the current sample was in late adolescence or early adulthood during the rapid rise in e-cigarettes. Thus, these findings may not generalize to youth today who are entering adolescence in an environment where e-cigarettes are already prominent. Ongoing research is needed to continually assess the relationship between e-cigarettes, conventional cigarettes, and nicotine dependence as trends change.
This study has several strengths. First, the current sample is one of the only existing longitudinal cohort studies that assesses e-cigarette use, which allows a timely and important examination of their potential for harm reduction and cessation. Second, this study is among the first to examine the essential role of nicotine dependence when considering the effect of e-cigarette use on conventional smoking. Third, the use of VCM’s are an innovative and rigorous way to examine how the effect of e-cigarettes on conventional smoking may vary across tobacco users along the range of nicotine dependence.
The current study advances existing research on the correlates and outcomes of e-cigarette use, by supporting the use of e-cigarettes for some smokers but not for smoking cessation. Notably, the current findings show a complex, nonlinear relationship with nicotine dependence that may warrant different usage guidelines for different types of users. In particular, e-cigarette use may prove effective at reducing harm among highly nicotine-dependent cigarette smokers, but it may be appropriate to caution novice and nondependent smokers against using e-cigarettes see.10,11 E-cigarette use did not appear to be effective as a tool for reduction or cessation of conventional smoking. However, this effect was comparable to other quit methods except for nicotine replacement therapy, which did show a benefit among highly nicotine-dependent smokers. Future research using experimental and longitudinal designs is needed to evaluate these findings among other populations, especially as e-cigarette trends continue to change.
Funding
This research was funded by Project Grant P01 CA098262 from the National Cancer Institute and L40 DA042431 from the National Institute on Drug Abuse. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH, NCI, or NIDA.
Declaration of Interests
None declared.
References
- 1. Johnson LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE.. Monitoring the Future National Survey Results on Drug Use, 1975–2015: Overview, Key Findings on Adolescent Drug Use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- 2. Notes from the field: Electronic cigarette use among middle and high school students - United States, 2011-2012 MMWR 2013; 62(35):729–730. [PMC free article] [PubMed] [Google Scholar]
- 3. Schneider S, Diehl K. Vaping as a catalyst for smoking? an initial model on the initiation of electronic cigarette use and the transition to tobacco smoking among adolescents. Nicotine Tob Res. 2016;18(5):647–653. [DOI] [PubMed] [Google Scholar]
- 4. Pepper JK, Reiter PL, McRee AL, Cameron LD, Gilkey MB, Brewer NT. Adolescent males’ awareness of and willingness to try electronic cigarettes. J Adolesc Health. 2013;52(2):144–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rennie LJ, Bazillier-Bruneau C, Rouëssé J. Harm reduction or harm introduction? prevalence and correlates of e-cigarette use among french adolescents. J Adolesc Health. 2016;58(4):440–445. [DOI] [PubMed] [Google Scholar]
- 6. U.S. Department of Health and Human Services. E-cigarette use among youth and young adults: A report of the Surgeon General.Atlanta, GA: U.S. Department of Health and Human Services; 2016. [Google Scholar]
- 7. Choi K, Fabian L, Mottey N, Corbett A, Forster J. Young adults’ favorable perceptions of snus, dissolvable tobacco products, and electronic cigarettes: findings from a focus group study. Am J Public Health. 2012;102(11):2088–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bell K, Keane H. All gates lead to smoking: The ‘gateway theory’, e-cigarettes and the remaking of nicotine. Soc Sci Med. 2014;119:45–52. doi: 10.1016/j.socscimed.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 9. Le Houezec J, McNeill A, Britton J. Tobacco, nicotine and harm reduction. Drug Alcohol Rev. 2011;30(2):119–123. [DOI] [PubMed] [Google Scholar]
- 10. Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109(11):1801–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Franck C, Filion KB, Kimmelman J, Grad R, Eisenberg MJ. Ethical considerations of e-cigarette use for tobacco harm reduction. Respir Res. 2016;17(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wagener TL, Floyd EL, Stepanov I et al. . Have combustible cigarettes met their match? The nicotine delivery profiles and harmful constituent exposures of second-generation and third-generation electronic cigarette users. Tob Control. 2017;26(e1):e23–e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Goniewicz ML, Knysak J, Gawron M et al. . Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Camenga DR, Kong G, Cavallo DA, Krishnan-Sarin S. Current and former smokers’ use of electronic cigarettes for quitting smoking: an exploratory study of adolescents and young adults. Nicotine Tob Res. 2017;19(12):1531–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Czoli CD, Hammond D, White CM. Electronic cigarettes in Canada: prevalence of use and perceptions among youth and young adults. Can J Public Health. 2014;105(2):e97–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rass O, Pacek LR, Johnson PS, Johnson MW. Characterizing use patterns and perceptions of relative harm in dual users of electronic and tobacco cigarettes. Exp Clin Psychopharmacol. 2015;23(6):494–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tomashefski A. The perceived effects of electronic cigarettes on health by adult users: A state of the science systematic literature review. J Am Assoc Nurse Pract. 2016;28(9):510–515. [DOI] [PubMed] [Google Scholar]
- 18. Huang J, Kornfield R, Emery SL. 100 million views of electronic cigarette youtube videos and counting: quantification, content evaluation, and engagement levels of videos. J Med Internet Res. 2016;18(3):e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huang J, Kornfield R, Szczypka G, Emery SL. A cross-sectional examination of marketing of electronic cigarettes on Twitter. Tob Control. 2014;23(Suppl 3):iii26–iii30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Richardson A, Ganz O, Vallone D. Tobacco on the web: surveillance and characterisation of online tobacco and e-cigarette advertising. Tob Control. 2015;24(4):341–347. doi: 10.1136/tobaccocontrol-2013–051246. [DOI] [PubMed] [Google Scholar]
- 21. van der Tempel J, Noormohamed A, Schwartz R, Norman C, Malas M, Zawertailo L. Vape, quit, tweet? Electronic cigarettes and smoking cessation on Twitter. Int J Public Health. 2016;61(2):249–256. [DOI] [PubMed] [Google Scholar]
- 22. Bullen C, Howe C, Laugesen M et al. . Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. [DOI] [PubMed] [Google Scholar]
- 23. Brown J, Beard E, Kotz D, Michie S, West R. Real-world effectiveness of e-cigarettes when used to aid smoking cessation: a cross-sectional population study. Addiction. 2014;109(9):1531–1540. doi: 10.1111/add.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Caponnetto P, Polosa R, Russo C, Leotta C, Campagna D. Successful smoking cessation with electronic cigarettes in smokers with a documented history of recurring relapses: a case series. J Med Case Rep. 2011;5:585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brose LS, Hitchman SC, Brown J, West R, McNeill A. Is the use of electronic cigarettes while smoking associated with smoking cessation attempts, cessation and reduced cigarette consumption? A survey with a 1-year follow-up. Addiction. 2015;110(7):1160–1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gmel G, Baggio S, Mohler-Kuo M, Daeppen JB, Studer J. E-cigarette use in young Swiss men: is vaping an effective way of reducing or quitting smoking?Swiss Med Wkly. 2016;146:w14271. doi: 10.4414/smw.2016.14271. [DOI] [PubMed] [Google Scholar]
- 27. Kandel DB, Chen K. Extent of smoking and nicotine dependence in the United States: 1991-1993. Nicotine Tob Res. 2000;2(3):263–274. [DOI] [PubMed] [Google Scholar]
- 28. Dierker L, Hedeker D, Rose J, Selya A, Mermelstein R. Early emerging nicotine dependence symptoms in adolescence predict daily smoking in young adulthood. Drug Alcohol Depend. 2015;151:267–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dierker L, Mermelstein R. Early emerging nicotine-dependence symptoms: a signal of propensity for chronic smoking behavior in adolescents. J Pediatr. 2010;156(5):818–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Selya AS, Dierker LC, Rose JS, Hedeker D, Mermelstein RJ. Risk factors for adolescent smoking: Parental smoking and the mediating role of nicotine dependence. Drug Alcohol Depend. 2012; 124(3):311–318. doi: 10.1016/j.drugalcdep.2012.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Shiffman S, Waters A, Hickcox M. The nicotine dependence syndrome scale: a multidimensional measure of nicotine dependence. Nicotine Tob Res. 2004;6(2):327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- 32. Clark DB, Wood DS, Martin CS, Cornelius JR, Lynch KG, Shiffman S. Multidimensional assessment of nicotine dependence in adolescents. Drug Alcohol Depend. 2005;77(3):235–242. [DOI] [PubMed] [Google Scholar]
- 33. Sterling KL, Mermelstein R, Turner L, Diviak K, Flay B, Shiffman S. Examining the psychometric properties and predictive validity of a youth-specific version of the nicotine dependence syndrome scale (ndss) among teens with varying levels of smoking. Addict Behav. 2009;34(6-7):616–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. TVEM SAS Macro Suite (Version 3.1.0) [Software] [computer program]. University Park: The Methodology Center, Penn State; 2015. [Google Scholar]
- 35. Tan X, Shiyko MP, Li R, Li Y, Dierker L. A time-varying effect model for intensive longitudinal data. Psychol Methods. 2012;17(1):61–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Jorenby DE, Smith SS, Fiore MC, Baker TB. Nicotine levels, withdrawal symptoms, and smoking reduction success in real world use: A comparison of cigarette smokers and dual users of both cigarettes and E-cigarettes. Drug Alcohol Depend. 2017;170:93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Leduc C, Quoix E. Is there a role for e-cigarettes in smoking cessation?Ther Adv Respir Dis. 2016;10(2):130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]