Abstract
Introduction
Studies testing novel tobacco products often provide participants with free product and assess consumption. Some, but not all, studies find that providing free cigarettes increases smoking. We tested changes in smoking when free cigarettes were provided to nondaily, intermittent smokers, who constitute one-third of US adult smokers.
Methods
Cigarette consumption was assessed by Time-Line Follow-Back in 235 intermittent smokers for two 2-week periods: when providing their own cigarettes and when provided own-brand cigarettes for free. Smoking topography and carbon monoxide boost were assessed for one cigarette at the end of each period.
Results
Cigarette consumption increased significantly, by 66% (from 1.98 to 3.28 cigarettes per day), when cigarettes were available for free; both the number of days the subjects smoked and the number of cigarettes on those days increased. The increases were significantly greater among African Americans, those Fagerström Tobacco Nicotine Dependence scores >0, those with incomes less than US $25,000 per year, those who engaged in greater conscious restraint of smoking, and for smokers of menthol cigarettes, or “longs.” Smoking intensity (smoke volume, by topography) and carbon monoxide boost decreased significantly when cigarettes were provided for free.
Conclusions
Providing intermittent smokers with free cigarettes substantially increased their smoking while decreasing smoking intensity. The increases in smoking varied according to multiple individual and cigarette-type differences. These phenomena may complicate interpretation of studies that compare consumption of a free test product with cigarette consumption or constituent exposure when smokers are providing their own cigarettes. They also suggest that cigarette cost and variations in low-level dependence and in smoking restraint are factors in nondaily smoking.
Implications
The study shows that providing nondaily smokers with free cigarettes increases cigarette consumption, but does differentially for different subgroups and cigarette types, while also decreasing smoking intensity. This suggests the value of using free-cigarette baseline data in studies where interventions provide free cigarettes.
Introduction
There has been a proliferation of novel tobacco/nicotine products, which creates a need to test their effects on cigarette consumption and exposure. Examples include cigarettes manipulated to have very low1,2 or very high3,4 nicotine levels, and products that do not burn tobacco but either aerosolize nicotine (ie, e-cigarettes)5 or heat it without burning.6 Studies of such alternative products provide the test products for free and assess changes in consumption compared with participants’ baseline smoking. However, the effect of providing the test products for free can complicate interpretation of the results because the intervention introduces two changes: the change in the product and making the product available for free. If providing products for free increases consumption, as seen in some, but not all studies,1,2 this is likely to complicate interpretation of the effect of the product itself. (See eg, Donny et al.,1 where all groups of participants initially increased their smoking [vs. baseline] by about 20% when given free cigarettes, whether they were very low nicotine or not, so that the conclusion that low nicotine cigarettes reduce smoking had to be inferred, from the observation that their smoking had increased less than the other groups’.)
In this study, we assess the effect of providing free cigarettes on nondaily smokers. Nondaily or intermittent smokers (ITS) constitute an increasingly important segment of the US smoker population. They now comprise about one-third of the US adult smokers7 and are of public health concern, as they do suffer adverse health consequences from smoking.8,9 Previous research has shown that nondaily smoking can be a stable long-term pattern,10,11 that ITS do inhale and take in nicotine when they smoke,12 and that ITS have nearly as much difficulty quitting as daily smokers do.13
As ITS are heterogeneous, it is also important to consider whether the effect of free cigarettes might differ across relevant subgroups. For example, making cigarettes available for free might have a greater effect on ITS who have previously been daily smokers, whom we have labeled converted ITS,11 as they might be more inclined to increase their smoking. On the other hand, converted ITS might be those whose environment restrains their smoking, implying that they would be less influenced by cost. Similar considerations would apply to ITS who show any sign of dependence,14 who may have a greater latent need to smoke, but also have demonstrated considerable control. Making cigarettes available for free might also differentially affect ITS who are consciously restraining their smoking;15 in studies of eating, restrained eaters are more likely to increase eating in response to various manipulations.16 Free cigarettes may have a greater influence on low-income smokers, for whom cost is more material. Demographic differences that moderate other smoking behaviors, for example, gender and ethnicity,17–20 also need to be considered. Finally, responses to free cigarettes might differ by type of cigarettes smoked, such as menthol cigarettes, “longs” (100 or 120 mm, compared with the dominant 79- to 88-mm lengths),21 or those with nominally lower nicotine delivery (so-called “lights”). If observed, such moderation by individual differences or cigarette types could provide insight into ITS smoking, while at the same time further complicating interpretation of intervention effects when smokers are given free product.
Cigarette consumption is a relatively crude measure of smoking behavior and smoke exposure because smokers can change how they smoke each cigarette in such a way that changes their exposure and manipulates their true exposure to smoke.22,23 In this study, smoking topography measures and increases in carbon monoxide (CO) due to smoking provided measures of smoking intensity.24,25
Methods
Subjects
Subjects were 235 ITS enrolled in an ongoing study of very low nicotine cigarettes, who were recruited via TV and print advertisements, social media campaigns, etc. To qualify, subjects had to smoke 4–27 days per month, have been smoking for ≥3 years, and nondaily for ≥1 year. Smokers who said that cost was the primary reason they smoked nondaily were excluded, as were individuals planning to quit within the next 3 months. Subjects had to be ≥18 years old and be willing to be randomized to very low nicotine cigarettes. The analysis focused on those who completed the per-protocol 2-week (10–18 days, median = 14) own-brand smoking period, as described below. Participants averaged 38.0 years old (SD = 13.8), were 52% female, 42% were college graduates, 62% were White, 27% African American, and 11% other ethnicities, with 5% identifying as Hispanic. Subjects had smoked for an average of 16.8 years (SD = 12.3), and 73% had a score of 0 on the Fagerström Tobacco Nicotine Dependence (FTND).26 Half of the participants had previously smoked daily for at least 6 months.
The cigarettes smoked by the sample comprised 58 varieties, as defined by brands, sub-brands, flavor, and lengths. About half (51%) of the participants smoked menthol cigarettes, a third smoked so-called Light (25%) or Ultra-Light (8%) brands, and 31% smoked “Longs” (100 or 120 mm).
Procedures
The study was approved by the University of Pittsburgh Institutional Review Board and participants provided written informed consent. At their first visit, participants reported their daily cigarette consumption via a Time-Line Follow-Back (TLFB),27 had their smoking topography assessed with their own cigarettes, and were provided with a supply of their own-brand cigarettes for the following week equal to twice their stated weekly consumption, to ensure that consumption was not limited by supply.
Participants returned for a second visit 1 week later and were again provided free cigarettes for a second week of ad libitum smoking. In a third visit, participants’ smoking topography was again measured with their own-brand cigarettes. Subsequently, participants were randomized to receive research cigarettes that delivered either “normal” nicotine levels or very low nicotine levels. The present analysis deals only with behavior prior to randomization.
At each visit, participants used custom software on a tablet to complete TLFB reports of recent smoking. At visit one, they reported their smoking for the preceding 28 days; data from the preceding 14 days were used in analysis, to match the subsequent 14-day free-cigarette period. At subsequent visits, participants completed a TLFB for smoking in the preceding week. The TLFB data were used to compute average daily cigarette consumption, percentage of days smoked, and cigarette consumption on the days they smoked for the 2-week period when participants provided their own cigarettes and the 2-week period when they were provided for free.
At the first visit, before they had been provided with any free cigarettes, and again at the third visit, when they had been smoking free cigarettes for 2 weeks, participants smoked one of their own-brand cigarettes in a casual environment, decorated like living room, in which they were left alone while topography was assessed by a CReSS Pocket device (Borgwaldt KC Inc, Richmond, VA), yielding measures of the number of puffs, total puff time, and total puff volume. We emphasize total puff volume as a measure of overall smoke exposure; the other measures were consistent with it. End-tidal CO measures were taken before and after smoking using a Vitalograph Breath CO monitor (Vitalograph Inc, Lenexa, KS) to compute the increase in CO due to smoking (“CO boost”). Examination of the topography data indicated that in some sessions, the topography instrument produced anomalous values with very high volumes, some as high as 5 L, and a pattern of decreasing CO boost with increasing puffs and volumes. Inspection of the relationship between volume and CO boost determined that the association reversed direction at 1.2 L, and this was confirmed by joinpoint analysis.28,29 Experimentation and instrumented testing determined that these invalid measurements occurred when the cigarette was not fully seated in the topography device, even though the device’s electronic confirmation indicated that the cigarette was adequately seated, yielding invalid measurements. Accordingly, we excluded topography sessions in which the instrument yielded readings exceeding 1.2 L, yielding a sample size of 190 for topography analyses. Sensitivity analyses including the anomalous data, using nonparametric analyses to limit their influence, showed that the conclusions were similar regardless.
At entry, details of the participant’s cigarette brand were recorded, and subjects completed assessments of demographic factors, smoking history, smoking restraint (slightly modified from the work of Blake et al.),15 and dependence. For analysis, the FTND was scored without using the item on cigarette consumption, to avoid confounding with smoking rate. The FTND distribution was highly skewed, with most subjects scoring at 0, so the score was dichotomized as zero versus any other value.
Analyses used difference scores to assess change in all parameters from session one (“paid cigarettes”) to session three (“free cigarettes”); nonparametric Wilcoxon tests were also conducted. The primary endpoint was average cigarettes per day (across all days); for the sample as a whole, we also tested changes in the smoking metrics that comprise this overall endpoint: the proportion of days smoked and the number of cigarettes smoked on smoking days. Moderator effects of individual differences were tested in regression models predicting change in average cigarettes per day. Because some possible moderators might also be related to baseline smoking or topography measures, significant moderator effects were retested while controlling for the “paid” baseline measure as a covariate. Test of the effects of cigarette type also controlled for key participant characteristics (ethnicity, income, and FTND).
Results
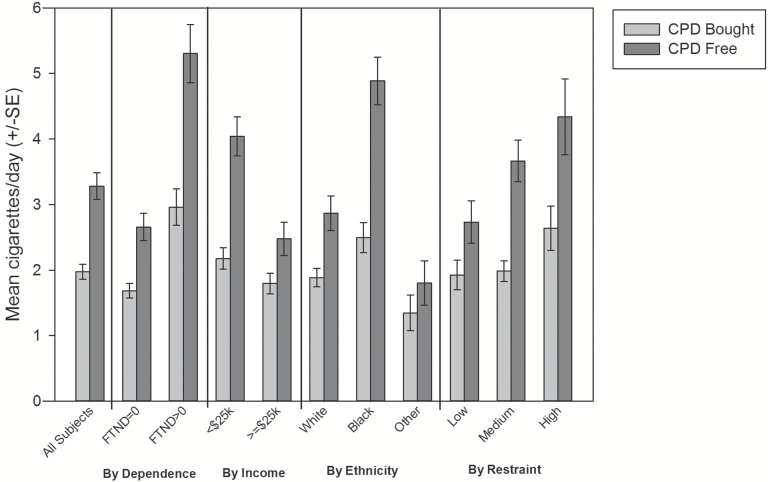
Figure 1 shows the results for cigarette consumption. Average daily cigarette consumption increased significantly, by 65% (from 2.0 to 3.3 cigarettes per day), during the free cigarette period. This reflected both a significant increase in the percentage of days smoked, which increased 29% (from 3.8 to 4.9 days per week), as well as a significant 22% increase in the number of cigarettes smoked on smoking days (from 3.5 to 4.3). Nonparametric tests confirmed all the observed effects without requiring distributional assumptions.
Figure 1.
Increases in cigarettes per day over a 2-week period, when smokers had been paying for cigarettes versus when they had been provided for free. Data are displayed for all subjects, and by significant moderators: dependence, income, ethnicity, and smoking restraint.
However, as shown in Table 1, smoking topography measures indicated that smoking intensity decreased modestly but significantly when free cigarettes were provided: The total puff volume decreased significantly (by 7%, from 626 to 581 mL), as did the number of puffs and total puff time. The CO boost due to smoking the topography cigarette also decreased significantly (by 10%, from 2.7 to 2.4 ppm). All changes were also made significant by nonparametric tests.
Table 1.
Smoking Topography Parameters and CO Boost
| Smoking parameter | Bought | Free |
|---|---|---|
| Mean (SD) | Mean (SD) | |
| Volume (mL)** | 625.64 (209.81) | 581.18 (227.55) |
| No. of puffs* | 15.78 (5.97) | 15.14 (6.11) |
| Puff time (s)** | 24.38 (10.25) | 22.64 (10.59) |
| CO boost (ppm)* | 2.72 (1.90) | 2.43 (1.83) |
Change (n = 190): *p < .05; **p < .001.
Moderation by Individual Differences and Cigarette Type
Neither gender nor a history of daily smoking had any effect on any changes from bought to free cigarettes, but other individual differences did moderate the effect. Smokers reporting annual income of less than US $25,000 increased their smoking to a greater degree, as did those with FTND scores greater than zero (Figure 1). African American smokers increased their smoking more than either White smokers or those of “other” ethnicities. More restrained smokers also increased their smoking to a greater degree. These moderator effects held even when cigarette consumption prior to study enrollment was included as a covariate, indicating that the effects are not due to differences in prior cigarette consumption. The four moderators were all correlated with each other. In a multivariate regression model to assess their independent contributions, only smoking restraint became nonsignificant (because of its relation to ethnicity: African Americans were more restrained); all the others remained significant independent predictors of greater increases when cigarettes were available for free.
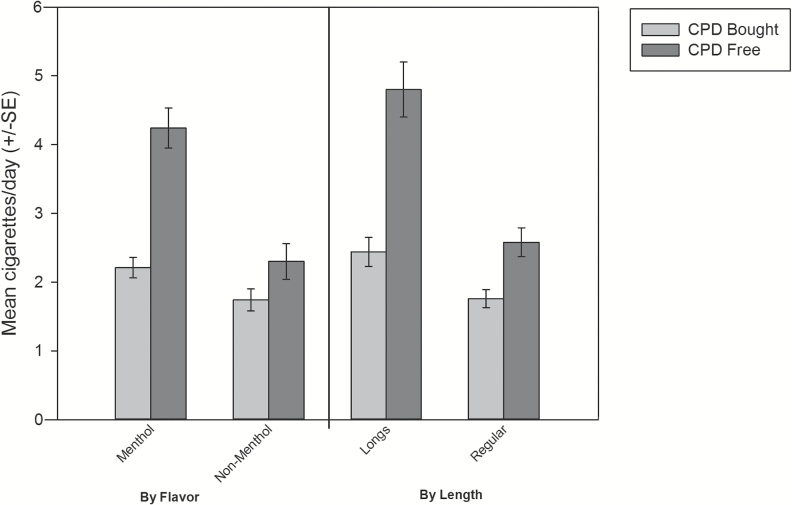
Controlling for ethnicity, income, and FTND, those who smoked menthol cigarettes and those who smoked “longs” increased their smoking significantly more (see Figure 2). The effects of menthol and longs were independent and remained significant when both were assessed in a multivariate model. The association with longs was also independent of age and gender, which are correlated with use of longs.21 Smoking “Lights” (vs. regular-strength cigarettes) did not moderate the change in smoking when cigarettes were available for free.
Figure 2.
Increases in cigarettes per day over a 2-week period, when smokers had been paying for cigarettes versus when they had been provided for free, by type of cigarette smoked. The graph represents observed mean cigarette consumption. The analyses controlled for the effects shown in Figure 1 (FTND, income, ethnicity, and smoking restraint).
None of the individual differences or cigarette types significantly moderated the decreased smoke volume or CO boost in topography sessions.
Discussion
When provided their own brand of cigarettes for free, ITS substantially increased their cigarette consumption. At the same time, however, their smoking intensity slightly decreased such that their per-cigarette smoke exposure declined. In other words, they smoked more, but less intensely. Considering these opposing trends, the data suggest that their overall smoke exposure likely rose, as cigarette consumption increased by 66%, whereas per-cigarette exposure measures declined by 10% (for CO boost), implying a 59% increase in exposure (discounting the 66% increased consumption by 10%). In any case, the fact that cigarette consumption and per-cigarette exposure changed in opposite directions complicates interpretation of smoking data when free tobacco products are introduced.
Moreover, the effects were not constant across subjects. Perhaps not surprisingly from an economic point of view, smokers with lower incomes increased their smoking to a greater extent when provided with free cigarettes. Moderation of price effects by income has been observed previously.30 ITS who showed any sign of dependence at all (FTND > 0) increased their cigarette smoking to a greater degree, even after accounting for their baseline cigarette consumption. African Americans also increased their smoking to a greater degree. Multiple indicators in other studies suggest different dynamics for smoking among African Americans: they are more likely to be ITS and, among daily smokers, tend to show lower cigarette consumption, but higher dependence at a given level of consumption.19,31–33 That the ethnic difference observed here is independent of baseline cigarette consumption and dependence suggests even more complex ethnic differences in relation to escalation of smoking when cigarettes are provided for free. Smokers who reported consciously restraining their smoking showed bigger increases when given free cigarettes; this is consistent with the observation in the eating restraint literature that restraint can actually make individuals more vulnerable to interventions that increase consumption.34 The finding confirms that smoking restraint may be a useful concept.15,35
The increase in cigarette consumption when cigarettes were available for free also differed according to the type of cigarette the participant smoked. Those who smoked longs roughly doubled their consumption. These individuals may have chosen longs as a way to get more tobacco for their money, so may have reacted more strongly to the availability of free tobacco.21 Those who smoked menthol cigarettes also reacted more strongly to being given free cigarettes. Although use of menthol cigarettes is much more common among African Americans36 (and was in this sample), the menthol effect was independent of ethnicity. If the soothing effect of menthol minimizes throat irritation,37 this could have allowed the menthol smokers to more easily increase their consumption.
The study has implications for understanding ITS behavior. It reconfirms that even at this very lowest end of the dependence spectrum, variations in dependence influence behavior (see Shiffman et al.14) in that ITS with even very modest levels of dependence are more prone to escalating their smoking when conditions favor that. The findings also suggest that conscious restraint may play a role in nondaily smoking. It was surprising that those with a history of daily smoking were not more affected by removal of price as a barrier; they may reside in environments that limit smoking or may have had to develop stronger controls over their smoking to maintain nondaily smoking after a history of daily smoking.
ITS’ cigarette consumption appeared to be affected by economics, just as daily smokers’ (DS) smoking is.30,38 One might think that providing free cigarettes might particularly disinhibit smoking for ITS, compared with DS, on the premise that ITS’ limited smoking is due to not being able to afford more cigarettes. However, we previously found11 that ITS had higher incomes than DS, reported less suppression of smoking by cost, and said that they expected smaller increases in smoking if cigarettes were available for free. Moreover, in the present study, volunteers who stated that financial constraints were their primary reason for limiting their smoking were excluded, which likely minimized price-sensitivity relative to the ITS population at large. The absolute increases in smoking were modest—just 1.3 cigarettes per day—but they were proportionately quite large—a 66% increase in consumption. And they were reflected increases in both the number of days smoked and the number of cigarettes smoked on those days.
The cost of cigarettes is known to suppress cigarette consumption on daily smokers as well, as amply illustrated by studies of cigarette taxation,39 which show that population cigarette consumption declines as taxes (or other costs) increase. If removing cost as a barrier increased cigarette consumption, why did smoking intensity decline? This might be understood from a behavior–economic perspective: when cigarettes are costly, there is an incentive to extract as much of the underlying “good” (presumably nicotine, but also possibly sensory effects of smoking)40 from each one. When they are available for free, this incentive decreases. Although reduction in smoking intensity due to price decreases has not previously been reported, the opposite—increases in smoking intensity when price rises—was previously reported in two population studies.41,42
The findings also have implications for the methodology of tobacco research studies that aim to assess change in consumption and/or exposure when smokers are switched to a test product that is provided for free. They suggest that consumption and exposure cannot be directly compared between a naturalistic observational baseline, where cigarettes must be purchased, and a test-product condition when the product is provided for free. They further suggest that, in such comparisons, observed changes in consumption cannot be assumed to imply concomitant changes in exposure, as consumption and per-use exposure may both change, in opposite directions. Moreover, the fact that the effects differ according to a variety of individual differences, and by cigarette type, further complicates matters, introducing further variance and possibly bias, depending on the composition of the sample. In effect, studies that first introduce a free product when they introduce test products, such as very-low-nicotine content cigarettes, are introducing two different interventions simultaneously—the effect of giving free products, and the effect of the particular test product, making interpretation of subsequent changes difficult. This suggests that studies that intend to provide cigarettes or other tobacco or nicotine products gratis may benefit from using a free-own-cigarette condition as the baseline measure against which test-product conditions are compared.
The generalizability of these findings may be limited, given that participants were ITS who do not smoke daily. ITS may have more “headroom” to increase their smoking when provided with free cigarettes, so the findings for DS may be different. However, the report of Donny et al.1 of increased smoking among DS suggests a similar phenomenon among DS. Previous observations12,43 suggest that topography and nicotine intake per cigarette are similar for ITS as for DS, suggesting that those results may be generalizable as well. In any case, ITS are an important smoking population in their own right, as they now constitute 25%–33% of US adult smokers.7,44,45
The own-cigarette and free-cigarette conditions were run serially, in the same order for all participants. Thus, it is possible that the effects observed are due to time, rather than to switching from own-cigarettes to free cigarettes. However, previous studies have shown that neither TLFB-measured cigarette consumption46,47 nor smoking topography measures48 change systematically over time or over repeated measurements, rendering this interpretation unlikely. Studies of reactivity in recording smoking indicate that reactivity is minimal when the subjects are not trying to quit and when the event is not recorded just before smoking,49 the situation that applies in this study.
The study could have been improved with more extensive biomarker data. Although both topography measures and CO boost after smoking a cigarette in the laboratory indicated a reduction in smoking intensity, analysis of biomarkers such as cotinine or 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol24 might have enabled more robust assessment of smoking intensity in the field.
In any case, providing ITS with free cigarettes increases how many cigarettes are smoked, but decreases how intensely they are smoked. The changes in cigarette consumption are moderated by income, ethnicity, dependence, smoking restraint, and cigarette type, further complicating the effect. Besides shedding light on ITS smoking dynamics, these findings have implications for the design of studies assessing how consumption and exposure change compared with baseline when people are provided with an alternative tobacco or nicotine product.
Funding
This work was supported by National Cancer Institute at the National Institutes of Health grant [to S. Shiffman], awarded as a supplement to grant number P30CA047904, N. Davidson, Principal Investigator.
Declaration of Interests
S. Shiffman consults to Reynolds American, Inc (RAI), on smoking cessation and tobacco harm minimization products and policies (no consulting on combustible conventional cigarettes).
Acknowledgments
The authors are grateful to Allison Brown for assistance overseeing the study, to David Colarusso, Corinne Hogge, and Ian Jutsum for their work conducting research sessions, to James Moorehead for data management and preparation, and to Alexsys Brown for editorial assistance. We are also grateful to Eric Donny and John Hughes for helpful comments on earlier drafts of the paper.
References
- 1. Donny EC, Denlinger RL, Tidey JW et al. Randomized trial of reduced-nicotine standards for cigarettes. N Engl J Med. 2015;373(14):1340–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Strasser AA, Lerman C, Sanborn PM, Pickworth WB, Feldman EA. New lower nicotine cigarettes can produce compensatory smoking and increased carbon monoxide exposure. Drug Alcohol Depend. 2007;86(2-3):294–300. [DOI] [PubMed] [Google Scholar]
- 3. Business Wire. 22nd Century’s RED SUN Brand Launches Extremely Nicotine Campaign; Companyhowcases “Extremist” RED SUN Brand Enthusiasts. http://www.businesswire.com/news/home/20151221005946/en/22nd-Century%E2%80%99s-RED-SUN-Brand-Launches-Extremely. Accessed December 21, 2015. [Google Scholar]
- 4. Mendelson JH, Sholar MB, Goletiani N, Siegel AJ, Mello NK. Effects of low- and high-nicotine cigarette smoking on mood states and the HPA axis in men. Neuropsychopharmacology. 2005;30(9):1751–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hajek P, Etter JF, Benowitz N, Eissenberg T, McRobbie H. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addiction. 2014;109(11):1801–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lüdicke F, Baker G, Magnette J, Picavet P, Weitkunat R. Reduced exposure to harmful and potentially harmful smoke constituents with the tobacco heating system 2.1. Nicotine Tob Res. 2017;19(2):168–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: National Findings, NSDUH Series H-48, HHS Publication No. (SMA) 14–4863. Rockville, MD: Substance Abuse and Mental Health Services Administration, 2014. [Google Scholar]
- 8. Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association of long-term, low-intensity smoking with all-cause and cause-specific mortality in the national institutes of health-AARP diet and health study. JAMA Intern Med. 2017;177(1):87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schane RE, Ling PM, Glantz SA. Health effects of light and intermittent smoking: a review. Circulation. 2010;121(13):1518–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Evans NJ, Gilpin E, Pierce JP et al. Occasional smoking among adults: evidence from the california tobacco survey. Tob Control. 1992;1(3):169–175. [Google Scholar]
- 11. Shiffman S, Tindle H, Li X, Scholl S, Dunbar M, Mitchell-Miland C. Characteristics and smoking patterns of intermittent smokers. Exp Clin Psychopharmacol. 2012;20(4):264–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shiffman S, Dunbar MS, Benowitz NL. A comparison of nicotine biomarkers and smoking patterns in daily and nondaily smokers. Cancer Epidemiol Biomarkers Prev. 2014;23(7):1264–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tindle HA, Shiffman S. Smoking cessation behavior among intermittent smokers versus daily smokers. Am J Public Health. 2011;101(7):e1–e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shiffman S, Ferguson SG, Dunbar MS, Scholl SM. Tobacco dependence among intermittent smokers. Nicotine Tob Res. 2012;14(11):1372–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Blake GA, Ferguson SG, Palmer MA, Shiffman S. Development and psychometric properties of the Smoking Restraint Questionnaire. Psychol Addict Behav. 2016;30(2):238–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Polivy J, Herman CP. Restrained Eating and Food Cues: Recent Findings and Conclusions. Curr Obes Rep. 2017;6(1):79–85. [DOI] [PubMed] [Google Scholar]
- 17. Allen AM, Scheuermann TS, Nollen N, Hatsukami D, Ahluwalia JS. Gender differences in smoking behavior and dependence motives among daily and nondaily smokers. Nicotine Tob Res. 2016;18(6):1408–1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Bauer T, Göhlmann S, Sinning M. Gender differences in smoking behavior. Health Econ. 2007;16(9):895–909. [DOI] [PubMed] [Google Scholar]
- 19. Schoenborn CA, Adams PF, Peregoy JA. Health behaviors of adults: United States, 2008–2010. Vital Health Stat. 2013;257(10):1–184. [PubMed] [Google Scholar]
- 20. US Department of Health and Human Services. Tobacco use among U.S. racial/ethnic minority groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, Hispanics. A report of the surgeon general. MMWR Recomm Rep. 1998;47(RR-18):v–xv, 1–16. [PubMed] [Google Scholar]
- 21. Agaku IT, Vardavas CI, Ayo-Yusuf OA, Alpert HR, Connolly GN. Gender and racial differences in smoking of long/ultra-long and king size cigarettes among U.S. adult smokers, NHANES 1999–2012. Drug Alcohol Depend. 2014;136:28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ashton H, Stepney R, Thompson JW. Self-titration by cigarette smokers. Br Med J. 1979;2(6186):357–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hasenfratz M, Baldinger B, Bättig K. Nicotine or tar titration in cigarette smoking behavior?Psychopharmacology (Berl). 1993;112(2-3):253–258. [DOI] [PubMed] [Google Scholar]
- 24. Benowitz NL, Hukkanen J, Jacob PR. Nicotine chemistry, metabolism, kinetics and biomarkers. Handb. Exp. Pharmacol. 2009;192:29–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. US Public Health Service. Office of the surgeon general, office on smoking and health. In Pinney JM, ed. Smoking and health: a report of the Surgeon General. Rockville, MD: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Office of the Assistant Secretary for Health; 1979, DHEW publication no (PHS) 79-50066, 1250 pages. [Google Scholar]
- 26. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The fagerström test for nicotine dependence: a revision of the fagerström tolerance questionnaire. Br J Addict. 1991;86(9):1119–1127. [DOI] [PubMed] [Google Scholar]
- 27. Sobell MB, Sobell LC, Maisto SA. Time-line follow-back assessment method [TLFB]. In: Lettieri DJ, Nelson JE, Sayers MA, eds. Alcoholism Treatment Assessment Research Instruments. (NIAAA Treatment Handbook Series, Vol 2). Rockville, MD: National Institute on Alcoholism and Alcohol Abuse; 1979:167–188. [Google Scholar]
- 28. Joinpoint Regression Program Version 4.5.0.0, Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute, [computer program]. May 2017. [Google Scholar]
- 29. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. [DOI] [PubMed] [Google Scholar]
- 30. Hersch J. Gender, income levels, and the demand for cigarettes. J Risk Uncertainty. 2000; 21(2–3):263–282. [Google Scholar]
- 31. Ahijevych K, Gillespie J. Nicotine dependence and smoking topography among black and white women. Res Nurs Health. 1997;20(6):505–514. [DOI] [PubMed] [Google Scholar]
- 32. Royce JM, Hymowitz N, Corbett K, Hartwell TD, Orlandi MA. Smoking cessation factors among African Americans and whites. COMMIT Research Group. Am J Public Health. 1993;83(2):220–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Trinidad DR, Pérez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine Tob Res. 2009;11(2):203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Moldovan AR, David D. Features of automaticity in eating behavior. Eat Behav. 2012;13(1):46–48. [DOI] [PubMed] [Google Scholar]
- 35. Nordgren LF, van Harreveld F, van der Pligt J. The restraint bias: how the illusion of self-restraint promotes impulsive behavior. Psychol Sci. 2009;20(12):1523–1528. [DOI] [PubMed] [Google Scholar]
- 36. Lawrence D, Rose A, Fagan P, Moolchan ET, Gibson JT, Backinger CL. National patterns and correlates of mentholated cigarette use in the United States. Addiction. 2010;105(Suppl 1):13–31. [DOI] [PubMed] [Google Scholar]
- 37. Willis DN, Liu B, Ha MA, Jordt SE, Morris JB. Menthol attenuates respiratory irritation responses to multiple cigarette smoke irritants. FASEB J. 2011;25(12):4434–4444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Farrelly MC, Bray JW. Response to increases in cigarette prices by race/ethnicity, income, and age groups—United States, 1976–1993 (Reprinted from MMWR, vol 47, pp. 605–609, 1998). Jama-J Am Med Assoc. 1998;280(23):1979–1980. [Google Scholar]
- 39. Contreary KA, Chattopadhyay SK, Hopkins DP et al. ; Community Preventive Services Task Force. Economic impact of tobacco price increases through taxation: a community guide systematic review. Am J Prev Med. 2015;49(5):800–808. [DOI] [PubMed] [Google Scholar]
- 40. Rose JE. Disrupting nicotine reinforcement: from cigarette to brain. Ann N Y Acad Sci. 2008;1141:233–256. [DOI] [PubMed] [Google Scholar]
- 41. Adda J, Cornaglia F. Taxes, cigarette consumption, and smoking intensity. Am Econ Rev. 2006;96(4):1013–1028. [PubMed] [Google Scholar]
- 42. Evans WN, Farrelly MC. The compensating behavior of smokers: taxes, tar, and nicotine. Rand J Econ. 1998;29(3):578–595. [PubMed] [Google Scholar]
- 43. Shiffman S, Dunbar MS, Kirchner TR et al. Cue reactivity in non-daily smokers: effects on craving and on smoking behavior. Psychopharmacology (Berl). 2013;226(2):321–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Centers for Disease Control and Prevention. Cigarette smoking among adults—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(45):1221–1226. [PubMed] [Google Scholar]
- 45. Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services; 2012. [Google Scholar]
- 46. Brown RA, Burgess ES, Sales SD, Whiteley JA, Evans DM, Miller IW. Reliability and validity of a smoking timeline follow-back interview. Psychol Addict Behav. 1998;12(2):101–112. [Google Scholar]
- 47. Gariti PW, Alterman AI, Ehrman RN, Pettinati HM. Reliability and validity of the aggregate method of determining number of cigarettes smoked per day. Am J Addict. 1998;7(4):283–287. [PubMed] [Google Scholar]
- 48. Lee EM, Malson JL, Waters AJ, Moolchan ET, Pickworth WB. Smoking topography: reliability and validity in dependent smokers. Nicotine Tob Res. 2003;5(5):673–679. [DOI] [PubMed] [Google Scholar]
- 49. McFall RM. Parameters of self-monitoring. In: Stuart RB, ed. Behavioral self-management: Strategies, techniques, and outcome. New York: Brunner/Mazel; 1977:196–214. [Google Scholar]