Abstract
Aim:
To examine the stroke risks associated with aircraft, road traffic, and railway noise exposure in a large case–control study.
Materials and Methods:
All people aged ≥40 years living around the Frankfurt airport that were insured by one of three large statutory health insurance funds between 2005 and 2010 were included in the study (n = 1,026,670). Address-specific exposure to aircraft, road, and railway traffic noise was estimated for 2005. We used insurance claim data to identify 25,495 newly diagnosed cases of stroke between 2006 and 2010 and compared them with 827,601 control participants. Logistic regression analysis was used to calculate the odds ratios adjusted for age, sex, local proportion of people receiving unemployment benefits, and if available individual indicators of socioeconomic status (education, occupation).
Results:
For 24-h continuous aircraft noise exposure, neither increased risk estimates nor a positive linear exposure–risk relation was found. However, stroke risk was statistically significantly increased by 7% [95% confidence intervals (95%CI): 2–13%] for people who were exposed to <40 dB of 24-h continuous aircraft noise, but ≥6 events of maximum nightly sound pressure levels ≥50 dB. For road and railway traffic noise, there was a positive linear exposure–risk relation: Per 10 dB the stroke risk increased by 1.7% (95%CI: 0.3–3.2%) for road traffic noise and by 1.8% (95%CI: 0.1–3.3%) for railway traffic noise. The maximum risk increase of 7% (95%CI: 0–14%) for road traffic noise and 18% (95%CI: 2–38%) for railway traffic noise was found in the exposure category ≥65 to <70 dB.
Conclusion:
This large case–control study indicates that traffic noise exposure may lead to an increase in stroke risk. It furthermore suggests that maximum aircraft noise levels at night increase the stroke risk even when continuous noise exposure is low, and thus highlights the relevance of maximum noise levels for research and policies on noise protection.
Keywords: Case–control study, stroke, traffic noise
Introduction
Noncommunicable diseases constitute one of today’s leading public health challenges, with 70% of all deaths worldwide being currently attributable to these diseases.[1] Cardiovascular diseases account for nearly half of that mortality, comprising 17.5 million deaths per annum worldwide[2] and more than 4 million deaths in Europe alone.[3] According to World Health Organisation (WHO) mortality data for Europe, stroke accounts for 9% of these deaths in men and 14% in women.[3] Additionally, cerebrovascular diseases constitute an enormous public health burden because they often result in disability and long-term care dependency.
Noise disturbance is also a widespread problem. A recent survey revealed that almost every second person in Germany feels impacted and disturbed by environmental noise, and one of the main sources of this noise disturbance is traffic noise.[4] The WHO estimates that in Western Europe alone at least one million disability-adjusted life years are lost annually due to traffic noise induced diseases.[5] Noise exposure is presumed to activate the autonomous nervous system, resulting in a release of stress hormones (e.g., adrenaline, noradrenaline, cortisol), which can cause acute and chronic changes in the body.[6] Nocturnal sleep disturbance (e.g., night-time waking reactions) is another potential mechanism for the harmful effects of noise on health. Sleep disturbance can have detrimental effects on physiological resting and regeneration processes and lead to an increase in stress level and tiredness on the following day.[7,8] The pathophysiological processes negatively influenced by stress are supposed to contribute to the development of cardiovascular morbidity, ultimately manifesting as endpoints such as arterial hypertension, myocardial infarction, and stroke.[9,10,11]
Traffic is a major source of environmental noise, especially in urbanized settings. The connection between traffic noise and cardiovascular health outcomes is complex, because different sources of noise in the environment (e.g., road traffic, railway, aircraft noise) have to be taken into account. Additionally, a multitude of confounding factors might distort the potential association between noise exposure and cardiovascular risk, and effects may be different for different types of cardiovascular disease.
A possible connection between aircraft noise exposure and stroke has been examined by numerous studies, with heterogeneous results. A study focusing on London-Heathrow airport compared the stroke risk of people exposed to over 63 dB of daytime aircraft noise to people exposed to <51 dB (L Aeq, 07:00–23:00 h).[12] They found increased hospitalization rates for stroke [risk ratio (RR) = 1.24; 95% confidence intervals (95%CI): 1.08–1.43]. The HYENA study which was conducted in six European countries found no increased stroke risk (self-reporting of a physician’s diagnosis of stroke) after adjusting for confounders [odds ratios (ORs) = 1.08; 95%CI: 0.82–1.41 per 10 dB in L Aeq, 07:00–23:00 h].[13] In the Swiss National Cohort, no associations between aircraft traffic noise measured in Ldn and stroke were found.[14] In line with that, a recent ecological study from France also could not show any significant risk increase of stroke mortality.[15]
Several meta-analyses have investigated the nonauditory effects of road traffic noise and particularly effects on hypertension and ischemic heart disease.[16,17] A recent meta-analysis of 14 studies on the effects of road traffic noise on coronary heart disease[18] found that the relative risk significantly increased; however, the validity of these results is limited by the fact that the analysis was not based on a systematic review. Regarding stroke, a cohort study from Denmark[19] suggested an association of residential road traffic noise and a higher risk for stroke among older people. In contrast, two studies from the Netherlands did not find significant associations between road traffic noise and cerebrovascular risk.[20,21]
To our knowledge, there are no pre-existing studies investigating the association between railway noise and stroke risk. However, the results of a recent study examining railway noise exposure suggest an increased overall mortality risk.[22]
A recent meta-analysis examining the combined effects of all sources of traffic noise exposure (no studies were identified for railway noise) found a nonsignificant increase in stroke risk of 1.4% (95%CI: 0.964–1.066) per 10 dB.[23] A study based in metropolitan Vancouver (Canada) found an increase in stroke mortality risk for community noise, including all three types of traffic noise. However, this was nonsignificant after adjusting for confounders (RR = 1.03; 95%CI: 0.91–1.16),[24] and railway noise exposure was very rare in the study populations.
As the study design, methodological quality, and results of the current body of evidence are heterogeneous, additional large-scale studies of rigorous methodology are important to improve epidemiological knowledge on the stroke-traffic-noise link. The present study therefore aims at assessing the relation between aircraft, road, and railway traffic noise exposure and stroke risk in a large case–control study.
Materials and Methods
Study population
All people aged 40 years or older in 2010, living around Frankfurt airport (refer to Figure 1 for an illustration of the study region) that were insured by one of three large statutory health insurance funds between 2005 and 2010 were included in the study (n = 1,026,670).
Figure 1.
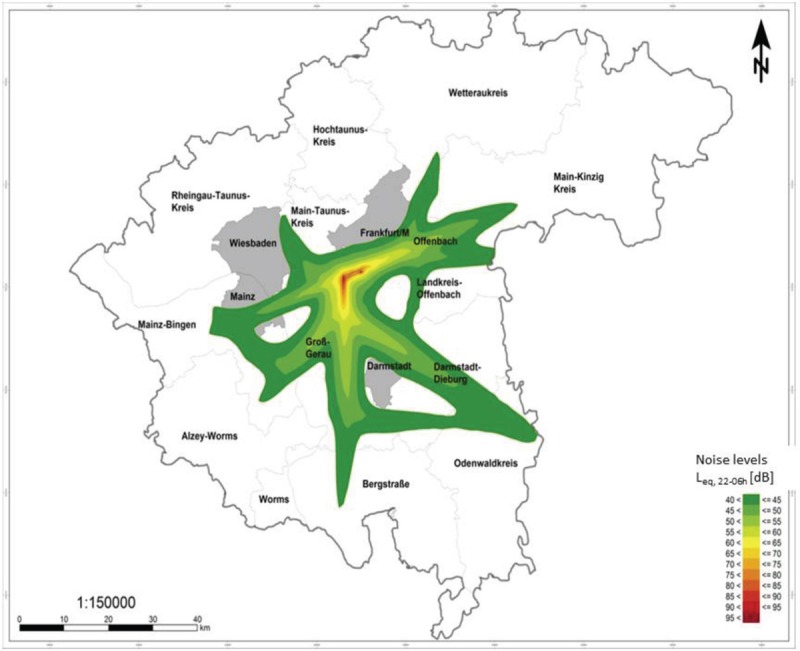
Map of the study area (gray line) and contours of continuous sound levels for night time aircraft noise exposure in 2005. Areas with night time (22:00–06:00 h) sound levels below 40 dB are shaded white
Noise exposure assessment
Address-specific noise exposure was estimated separately for aircraft, railway, and road traffic noise. For aircraft noise, average and maximum sound levels at the center of the building were calculated according to the guidelines for the calculations of noise abatement zones[25] using historical radar data from the German flight safety operator. The estimates were verified by comparison with the values of local monitoring stations. For road and railway traffic noise, the estimates of traffic exposure at source were obtained by road counts and information by the Federal Railway Authority and the German Railway environmental department. Sound reduction between source and emission site was then calculated according to the methods of calculation for EU noise mapping[26,27] to estimate address-specific noise exposure based on digital landscape modeling. The landscape modeling included information on the position of walls and noise barriers, footprints of buildings, and the landscape. Refer to Möhler et al.[28] for more information on the acoustic models, exposure calculations, uncertainties, and plausibility checks.
Definition of cases and controls
Hospital and ambulatory diagnoses (ICD 10 codes) and prescription data according to the Anatomical Therapeutic Chemical/Defined Daily Dose Classification were provided by the participating health insurance funds. Individuals with a primary hospital discharge or secondary diagnosis of stroke (ICD-10: I61.-: intracerebral hemorrhage, I63.-: cerebral infarction and I64.-: stroke, not specified as hemorrhage or infarction) between 2006 and 2010 but not in 2005 were included as newly diagnosed cases (n = 25,495). Ambulant diagnoses were not included since nearly all individuals with stroke get hospitalized.[29,30,31] Individuals without a stroke diagnosis in the study period and a minimum duration of insurance of 12 months were included as control participants (n = 827,601).
Data linkage
The health insurance funds provided pseudonymized health claims and prescription data to the Data Analysis Office in Dresden. Individual address data were linked to traffic noise data by the Data Linkage Office located in Bremen for two of the health insurance funds, while the third fund linked the data itself. Traffic noise and address data could be successfully linked for 95.5% of individuals (n = 907,736). The outcome and exposure data were then combined and analyzed at the Data Analysis Office in Dresden.
Potential confounders and statistics
Continuous sound pressure levels below 40 dB were used as a reference category, sound levels above 40 dB were grouped in 5 dB exposure categories. For aircraft noise, an additional exposure category was considered with continuous sound levels below 40 dB, but more than six single incidents of noise exposure above 50 dB between 22:00 and 06:00 h at night (NAT6). For each of these exposure categories, logistic regression analysis was performed to derive ORs and 95%CIs for each type of traffic noise separately. To examine the exposure–risk relationship, we applied a linear or third-degree polynomial regression model to the 24-h continuous sound levels starting at 35 dB. The linear model was considered acceptable if the difference between the Akaike Information Criteria for the models was 5 points or less. Age, sex, and the local proportion of people receiving unemployment benefits as an indicator of SES were included as confounders. Individual’s socioeconomic status (education and job title) were included if available. However, due to retirement, unemployment, or co-insurance with a family member, this was only the case for 10% of cases and 30% of control participants. Sensitivity analyses were conducted analyzing ischemic and hemorrhagic stroke separately, only including individuals with available SES information, and excluding NAT6 from continuous exposure–risk association calculations for aircraft noise exposure.
Results
Characteristics of cases and control participants are reported in Table 1. Patients with a diagnosis of stroke were on average older than control participants [median 76 (IQR = 15) versus 60 (interquartile range, IQR = 24) years]. Case numbers and ORs for the different sources of traffic noise are shown in Table 2. The linear model adequately represented the exposure–risk relation between all types of traffic noise and stroke risk.
Table 1.
Characteristics of cases with stroke and control participants
| Cases | Control participants | |||
|---|---|---|---|---|
|
|
|
|||
| n | % | n | % | |
| Total | 25,495 | 100% | 827,601 | 100% |
| Sex | ||||
| Males | 11,456 | 44.9% | 362,088 | 43.8% |
| Females | 14,039 | 55.1% | 465,513 | 56.2% |
| Age (years)+ | ||||
| 35 to <45 | 268 | 1.1% | 131,366 | 15.9% |
| 45 to <50 | 555 | 2.2% | 98,895 | 11.9% |
| 50 to <55 | 783 | 3.1% | 88,943 | 10.7% |
| 55 to <60 | 1200 | 4.7% | 88,196 | 10.7% |
| 60 to <65 | 1605 | 6.3% | 79,117 | 9.6% |
| 65 to <70 | 2748 | 10.8% | 93,183 | 11.3% |
| 70 to <75 | 3967 | 15.6% | 88,042 | 10.6% |
| 75 to <80 | 4376 | 17.2% | 62,221 | 7.5% |
| 80 to <85 | 4742 | 18.6% | 49,313 | 6.0% |
| ≥85 | 5251 | 20.6% | 48,325 | 5.8% |
| Statutory health insurance funds | ||||
| Health insurance 1 | 16,517 | 64.8% | 521,410 | 63.0% |
| Health insurance 2 | 1894 | 7.4% | 61,211 | 7.4% |
| Health insurance 3 | 7084 | 27.8% | 244,980 | 29.6% |
| Education | ||||
| Primary/secondary education, no vocational education | 629 | 2.5% | 66,137 | 8.0% |
| Primary/secondary education with vocational education | 1216 | 4.8% | 141,209 | 17.1% |
| Graduated from high school, no vocational education | 121 | 0.5% | 4405 | 0.5% |
| Graduated from high school and vocational education | 283 | 1.1% | 14,172 | 1.7% |
| College degree | 240 | 0.9% | 10,615 | 1.3% |
| University degree | 93 | 0.4% | 11,750 | 1.4% |
| Education unknown | 22,913 | 89.9% | 579,313 | 70.0% |
| Occupation according to Blossfeld | ||||
| AGR − agricultural occupations | 18 | 0.1% | 3048 | 0.4% |
| EMB − unskilled manual occupations | 286 | 1.1% | 35,796 | 4.3% |
| QMB − skilled manual occupations | 287 | 1.1% | 33,778 | 4.1% |
| TEC − technicians | 37 | 0.1% | 5327 | 0.6% |
| ING − engineers | 17 | 0.1% | 2286 | 0.3% |
| EDI − simple services | 591 | 2.3% | 62,710 | 7.6% |
| QDI − qualified services | 81 | 0.3% | 11,927 | 1.4% |
| SEMI − semiprofessionals | 125 | 0.5% | 20,138 | 2.4% |
| PROF − professionals | 13 | 0.1% | 2262 | 0.3% |
| EVB − simple commercial and administrative occupations | 184 | 0.7% | 25,013 | 3.0% |
| QVB − qualified commercial and administrative occupations | 428 | 1.7% | 59,444 | 7.2% |
| MAN − managers | 59 | 0.2% | 5710 | 0.7% |
| SONS − other | 79 | 0.3% | 7677 | 0.9% |
| Unknown | 23,290 | 91.4% | 552,485 | 66.8% |
| Local proportion of persons receiving unemployment benefits (SGBII; quintiles*) | ||||
| ≤6.7% | 8748 | 34.3% | 275,317 | 33.3% |
| >6.7 to ≤7.5% | 4387 | 17.2% | 134,146 | 16.2% |
| >7.5 to ≤8.7% | 2938 | 11.5% | 91,797 | 11.1% |
| >8.7 to ≤12.7% | 6680 | 26.2% | 245,344 | 29.6% |
| >12.7% | 2742 | 10.8% | 80,997 | 9.8% |
The percentages were rounded to one decimal and therefore do not always add up to exactly 100%. *Calculation of quintiles: frequent duplication of SGB II-values led to an uneven distribution. +Age at time of diagnosis for the case group, and average time of diagnosis (2008) for the control group.
Table 2.
Traffic noise (L pAeq,24h, L pAeq,night) and stroke for different types of traffic noise
| Exposure | Aircraft noise | Road traffic noise | Railway noise | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||||
| Cases | Control participants | OR | 95%CI | Cases | Control participants | OR | 95%CI | Cases | Control participants | OR | 95%CI | |||
| 24 h sound levels | ||||||||||||||
| <40 dB, Max. <50 dB | 10,595 | 325,613 | 1.00 | – | 2918 | 87,246 | 1.00 | – | 14,044 | 442,991 | 1.00 | – | ||
| <40 dB, Max. ≥50 dB | 1732 | 52,373 | 1.07 | 1.02–1.13 | – | – | – | – | – | – | – | – | ||
| ≥40 to <45 dB | 7304 | 247,877 | 0.98 | 0.95–1.01 | 5675 | 175,718 | 1.00 | 0.96–1.05 | 2970 | 103,496 | 0.97 | 0.93–1.01 | ||
| ≥45 to <50 dB | 3973 | 133,244 | 1.02 | 0.98–1.06 | 6046 | 198,841 | 0.98 | 0.93–1.02 | 4017 | 131,243 | 1.03 | 0.99–1.07 | ||
| ≥50 to <55 dB | 1470 | 52,507 | 0.97 | 0.92–1.03 | 4231 | 147,350 | 0.98 | 0.93–1.03 | 2598 | 91,225 | 0.97 | 0.93–1.01 | ||
| ≥55 to <60 dB | 413 | 15,792 | 0.86 | 0.77–0.95 | 2873 | 90,631 | 1.05 | 1.00–1.11 | 1124 | 35,680 | 1.06 | 1.00–1.13 | ||
| ≥60 to <65 dB | 8 | 195 | 1.62 | 0.79–3.34 | 1987 | 68,230 | 1.01 | 0.95–1.07 | 465 | 13,622 | 1.13 | 1.02–1.24 | ||
| ≥65 to <70 dB | – | – | – | – | 1400 | 46,374 | 1.07 | 1.00–1.14 | 187 | 5899 | 1.18 | 1.02–1.38 | ||
| ≥70 dB | – | – | – | – | 365 | 13,211 | 1.02 | 0.91–1.14 | 90 | 3445 | 0.98 | 0.79–1.21 | ||
| Continuous (per 10 dB) | 0.976 | 0.953–1.000 | 1.017 | 1.003–1.032 | 1.018 | 1.001–1.034 | ||||||||
| P = 0.048 | P = 0.020 | P = 0.033 | ||||||||||||
| Night time period 22:00–06:00 h | ||||||||||||||
| <40 dB, Max. <50 dB | 12,006 | 376,860 | 1.00 | – | 10,792 | 333,823 | 1.00 | – | 13,960 | 439,690 | 1.00 | – | ||
| <40 dB, Max. ≥50 dB | 6707 | 220,495 | 1.01 | 0.98–1.04 | ||||||||||
| ≥40 to <45 dB | 4209 | 139,373 | 1.02 | 0.98–1.05 | 4911 | 168,536 | 0.96 | 0.93–0.99 | 2980 | 102,197 | 0.97 | 0.93–1.01 | ||
| ≥45 to <50 dB | 1804 | 65,201 | 1.00 | 0.95–1.06 | 3936 | 130,800 | 1.01 | 0.97–1.05 | 3744 | 126,798 | 1.02 | 0.98–1.06 | ||
| ≥50 to <55 dB | 741 | 24,541 | 0.99 | 0.91–1.07 | 2931 | 94,774 | 1.05 | 1.00–1.09 | 2781 | 93,386 | 0.99 | 0.95–1.03 | ||
| ≥55 to <60 dB | 28 | 1131 | 1.00 | 0.68–1.46 | 1990 | 66,678 | 1.05 | 1.00–1.11 | 1218 | 40,559 | 1.01 | 0.95–1.08 | ||
| ≥60 dB | 0 | 0 | 935 | 32,990 | 1.02 | 0.95–1.10 | 812 | 24,971 | 1.12 | 1.04–1.20 | ||||
OR = odds ratio; adjusted for age, sex, education, job title (when available), and local proportion of persons receiving unemployment benefits. 95%CI = 95% confidence intervals.
Aircraft noise and stroke
In the linear model, there was a small negative exposure–risk association between continuous aircraft traffic noise exposure and stroke risk, with a risk decrease between 4.7 and 0% per 10 dB (P = 0.05). In the categorical analysis of continuous aircraft noise exposure, the effect sizes were all around 1.00 (refer Table 2 for ORs and 95%CIs). The effect size for the exposure category ≥55 to <60 dB was significantly smaller than 1.00 with an OR of 0.86 (95%CI: 0.77–0.95). However, the numbers of cases and control participants in the higher exposure categories were small. Thus, the fairly large effect size (OR = 1.62; 95%CI: 0.79–3.34) in the highest exposure category of ≥60 dB did not reach statistical significance. For continuous night time exposure (22:00–06:00 h), the risk estimates were around 1.00 for all exposure categories [Table 2]. However, there were no cases or control participants that were exposed to night time aircraft traffic noise above 60 dB, and the number of cases in the second highest exposure category ≥55 to <60 dB was low. There was a statistically significant risk increase for people exposed to continuous sound levels below 40 dB, but more than six nightly single incidents of noise exposure above 50 dB (NAT6, OR = 1.07; 95%CI: 1.02–1.13).
Road traffic noise and stroke
In the linear model, the stroke risk was estimated to increase by 1.7% (95%CI: 0.3–3.2%) per 10 dB of road traffic noise increase. In the categorical analysis, the effect size estimates were around OR = 1.00 for exposure categories below 55 dB [Table 2]. For higher exposure categories, stroke risk estimates were elevated (however, not all of them statistically significant). In the exposure category ≥55 to <60 dB the stroke risk was elevated to OR = 1.05 (95%CI: 1.00–1.11), for ≥60 to <65 dB it was OR = 1.01 (95%CI: 0.95–1.07). For ≥65 to <70 dB of continuous noise exposure, the highest risk estimate was found with OR = 1.07 (95%CI: 1.00–1.14) and for ≥70 dB the stroke risk was OR = 1.02 (95%CI: 0.91–1.14). For the night time period, there was a statistically significant risk increase for the exposure category ≥50 to <55 dB (OR = 1.05, 95%CI: 1.00–1.09) and for the category ≥55 to <60 dB (OR = 1.05, 95%CI: 1.00–1.11). For the exposure category above 60 dB, there was no statistically significant risk increase (OR = 1.02; 95%CI: 0.95–1.10).
Railway traffic noise and stroke
An elevated stroke risk was seen for railway traffic noise, with a risk increase of 1.8% (95%CI: 0.1–3.4%) per 10 dB. Similar to road traffic noise, risk estimates were around 1.00 for noise exposure up to 55 dB. For higher noise exposure categories, there was a statistically significant increase in stroke risk, reaching OR = 1.18 (95%CI: 1.02–1.38) for the exposure category ≥65 to <70 dB. For the highest exposure category above 70 dB, the risk estimate was not significantly different from 1.00; however, case numbers were low. For night time railway traffic noise exposure, there was a statistically significant increase in stroke risk for the highest exposure category of ≥60 dB with an OR of 1.12 (95%CI: 1.04–1.20).
Sensitivity analysis: ischemic and hemorrhagic stroke
As shown in Table 3, there were 22,122 cases with ischemic stroke and 3236 with hemorrhagic stroke. For aircraft noise exposure, both types of stroke showed a statistically significant increase in stroke risk for the NAT6 metric. The effect was stronger for hemorrhagic stroke with an OR of 1.16 (95%CI: 1.02–1.33) than for ischemic stroke with an OR of 1.06 (95%CI: 1.00–1.12). For both types of stroke, there was a tendency toward higher risk in the highest exposure category (>60 dB); however, case numbers were small and the observed effects were not statistically significant.
Table 3.
Traffic noise (L pAeq,24h, L pAeq,night) for different types of stroke
| Exposure | Aircraft noise | Road traffic noise | Railway noise | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||||||||
| Cases | Control participants | OR | 95%CI | Cases | Control participants | OR | 95%CI | Cases | Control participants | OR | 95%CI | ||||
| Restricted to cases with ischemic stroke (n = 22,122) | |||||||||||||||
| 24 h sound levels | |||||||||||||||
| <40 dB, Max. <50 dB | 9141 | 325,613 | 1.00 | – | 2484 | 87,246 | 1.00 | – | 12,217 | 442,991 | 1.00 | – | |||
| <40 dB, Max. ≥50 dB | 1465 | 52,373 | 1.06 | 1.00–1.12 | – | – | – | – | |||||||
| ≥40 to <45 dB | 6392 | 247,876 | 0.99 | 0.96–1.03 | 4903 | 175,718 | 1.02 | 0.97–1.07 | 2581 | 103,496 | 0.97 | 0.93–1.01 | |||
| ≥45 to <50 dB | 3489 | 133,244 | 1.04 | 0.99–1.09 | 5269 | 198,841 | 1.00 | 0.95–1.00 | 3463 | 131,243 | 1.02 | 0.98–1.06 | |||
| ≥50 to <55 dB | 1273 | 52,507 | 1.06 | 0.92–1.04 | 3698 | 147,350 | 1.01 | 0.95–1.06 | 2240 | 91,225 | 0.96 | 0.92–1.01 | |||
| ≥55 to <60 dB | 356 | 15,792 | 0.85 | 0.76–0.95 | 2510 | 90,631 | 1.08 | 1.02–1.14 | 967 | 35,680 | 1.05 | 0.98–1.12 | |||
| ≥60 to <65 dB | 6 | 195 | 1.41 | 0.62–3.22 | 1718 | 68,230 | 1.03 | 0.96–1.09 | 404 | 13,622 | 1.12 | 1.01–1.24 | |||
| ≥65 to <70 dB | – | – | – | – | 1221 | 46,374 | 1.10 | 1.02–1.18 | 163 | 5899 | 1.18 | 1.01–1.39 | |||
| ≥70 dB | – | – | – | – | 319 | 13,210 | 1.04 | 0.92–1.17 | 87 | 3445 | 1.08 | 0.87–1.35 | |||
| Continuous (per 10 dB) | – | – | 0.982 | 0.957–1.008 | 1.023 | 1.008–1.039 | 1.015 | 0.998–1.033 | |||||||
| P = 0.175 | P = 0.020 | P = 0.087 | |||||||||||||
| Restricted to cases with hemorrhagic stroke (n = 3236) | |||||||||||||||
| 24 h sound levels | |||||||||||||||
| <40 dB, Max. <50 dB | 1389 | 325,613 | 1.00 | – | 408 | 87,246 | 1.00 | – | 1746 | 442,991 | 1.00 | ||||
| <40 dB, Max. ≥50 dB | 256 | 52,373 | 1.16 | 1.02–1.33 | – | – | – | – | – | – | |||||
| ≥40 to <45 dB | 874 | 247,876 | 0.90 | 0.82–0.99 | 740 | 175,718 | 0.94 | 0.83–1.06 | 369 | 103,496 | 0.99 | 0.88–1.11 | |||
| ≥45 to <50 dB | 470 | 133,244 | 0.94 | 0.84–1.05 | 760 | 198,841 | 0.89 | 0.79–1.00 | 541 | 131,243 | 1.15 | 1.04–1.26 | |||
| ≥50 to <55 dB | 192 | 52,507 | 0.99 | 0.85–1.16 | 509 | 147,350 | 0.85 | 0.75–0.97 | 342 | 91,225 | 1.04 | 0.92–1.17 | |||
| ≥55 to <60 dB | 53 | 15,792 | 0.91 | 0.69–1.21 | 349 | 90,631 | 0.93 | 0.80–1.07 | 153 | 35,680 | 1.16 | 0.98–1.37 | |||
| ≥60 to <65 dB | 2 | 195 | 3.22 | 0.79–13.10 | 259 | 68,230 | 0.95 | 0.81–1.11 | 59 | 13,622 | 1.15 | 0.89–1.50 | |||
| ≥65 to <70 dB | – | – | – | – | 169 | 46,374 | 0.94 | 0.78–1.12 | 23 | 5899 | 1.20 | 0.79–1.82 | |||
| ≥70 dB | – | – | – | – | 42 | 13,210 | 0.85 | 0.62–1.17 | 3 | 3445 | 0.26 | 0.08–0.82 | |||
| Continuous (per 10 dB) | 0.945 | 0.884–1.011 | 0.979 | 0.940–1.019 | 1.041 | 0.997–1.087 | |||||||||
| P = 0.100 | P = 0.296 | P = 0.069 | |||||||||||||
OR: odds ratio; adjusted for age, sex, education, job title (when available), and local proportion of persons receiving unemployment benefits. 95%CI = 95% confidence intervals
For road traffic noise, the risk of ischemic stroke was estimated to increase by 2.3% (95%CI: 0.8–3.9%) per 10 dB increase in road traffic noise, and the risk estimates in the higher exposure categories were comparable to but slightly higher than the risk estimates in the main analysis. There was no statistically significant association between road traffic noise and risk of hemorrhagic stroke.
For railway noise, the continuous model approached statistical significance in both types of stroke with a 1.5% (95%CI: −0.2 to 3.3%) per 10 dB increase in ischemic stroke risk, and a 4.1% (95%CI: −0.3 to 8.7%) per 10 dB increase in hemorrhagic stroke. The estimators in the categorical analyses for railway noise were comparable across stroke types.
Sensitivity analysis: available SES information
To consider potential confounding due to missing socioeconomic status (SES) information, a subanalysis was performed including only individuals whose individual SES information was available from health insurance data (no table). The risk estimates were comparable to those from the full sample.
Sensitivity analysis: excluding NAT6 from continuous exposure–risk association
We conducted a sensitivity analysis excluding the NAT6 group of individuals with low continuous noise levels, but repeated single incidents of elevated nightly noise exposure, to examine how the elevated stroke risk in this low-continuous-exposure group drove the exposure–risk association. Excluding the NAT6 group attenuated the negative exposure–response effect for stroke risk, the OR was 0.98 (95%CI: 0.96–1.01; P = 0.20).
Discussion
This large case–control study used health insurance data to examine the relationship between aircraft, road, and railway traffic noise exposure and the diagnosis of stroke. For aircraft noise, there was an elevated stroke risk for individuals exposed to <40 dB of continuous aircraft noise, but at least six events of maximum nightly sound pressure levels above 50 dB. No increased stroke risk was found for the different categories of 24 h continuous aircraft noise pressure levels; however, the case numbers in the high exposure categories were low. There was a small negative exposure–risk association that became nonsignificant when people with low continuous noise exposure, but repeated nightly maximum events above 50 dB were excluded. For road traffic and railway traffic noise, a positive linear exposure–risk relation was found. In the continuous exposure categories, there were elevated risks for most of the noise exposure categories above 55 dB; however, effect sizes were fairly small.
Strengths and limitations
In this large case–control study, stroke risk estimates were provided separately for aircraft, road, and railway traffic noise. Address-specific individual traffic noise exposure was estimated using digital landscape models and state-of-the-art calculations. For aircraft noise, maximum nightly sound pressure levels were considered in addition to continuous sound pressure levels. The possibility of selection bias was reduced through the use of secondary health-claim data, including all insurees of the three participating health insurance funds. The health insurance funds cover about 23% of the total resident population living in the study area.
There may have been residual confounding since individual information on SES was only known for currently employed people: that is only 10% of cases and 30% of control participants. The percentage of cases with known SES was lower due to the higher mean age and thus a higher proportion of people in retirement. For each individual, information on the local proportion of people receiving unemployment benefits as an indicator of SES was included in the analysis. Furthermore, a subanalysis including only individuals with available SES information was conducted to assess confounding by SES in more depth, suggesting no relevant confounding influence of SES.
We did not have the data to control for air pollution as a potential confounder. A review by Stansfeld[32] found only small associations between air pollutants (such as PM10, PM2.5, NOx, NO, NO2) and aircraft as well as railway traffic noise, while the associations were stronger for road traffic noise. However, Sørensen et al. found that the effect of road traffic noise on stroke risk was not confounded by air pollution in 2011.[19] Another study examining potential combined effects of air pollution and road traffic noise on stroke showed that only road traffic noise but not air pollution had an effect on ischemic stroke, whereas air pollution increased fatal stroke risks in mutually adjusted models.[33] The reported effects of traffic noise independent of air pollutants give us some confidence in our results, despite not being able to adjust for air pollutants. Railway transportation is usually associated with little air pollution in the study area, because most trains run on electricity. For aircraft noise, the only exposure group that had a statistically significant risk increase was the group experiencing low continuous noise but at least six noise events above 50 dB per night (NAT6). It appears unlikely that this specific type of exposure should be confounded by air pollutants.
Comparison of risk estimates for aircraft, road, and railway traffic noise
For continuous noise pressure levels, road traffic noise and railway traffic noise show a comparable increase in stroke risk with higher noise exposure (1.7% per 10 dB for road traffic noise, 1.8% per 10 dB for railway traffic noise), while there was no statistically significant effect of continuous aircraft noise exposure on stroke risk. This may be because considerably elevated stroke risks for railway and traffic noise exposure were found at sound pressure levels above 55 dB, but only 2.6% of participants were exposed to continuous aircraft noise above 55 dB. It is thus possible that the risk increase is comparable across the sources of traffic noise, but this study lacked the power to detect a risk increase for aircraft noise.
For road and railway traffic noise, we found a linear positive exposure–risk relationship starting at 35 dB. Consequently, in accordance with other studies on the cardiovascular effects of traffic noise (e.g., Vienneau et al.[23], we were not able to identify a threshold value below which there are no cardiovascular risk elevations.
Ischemic and hemorrhagic stroke
Overall, we saw heterogeneous results for the sensitivity analysis examining the different types of traffic noise and risk of stroke, which have to be interpreted cautiously, because particularly for hemorrhagic stroke, numbers were fairly small.
In the literature, there are indications for different etiologies of the two different types of stroke. Differences between ischemic and hemorrhagic stroke have been noted for several risk factors,[34] such as obesity,[35] diet,[36] and occupational stress.[37,38] For stress, sleep, and hypertension as potential mechanisms linking traffic noise and stroke, former studies also point toward different risk patterns for ischemic and hemorrhagic stroke. Occupational stress seems to be a risk factor for ischemic but not (or at least not to the same extent) for hemorrhagic stroke,[37,38] while for stress overall the evidence for differences between the two types of stroke is unclear.[34,39] Hypertension increases the risk of both types of stroke, but especially hemorrhagic stroke.[39] The risk estimates found in the current study for ischemic stroke are similar to risk estimates derived for myocardial infarction[40] which may be explained by shared pathophysiological mechanisms.
People’s (health) reaction to noise may not only be influenced by amplitude but by other factors such as regularity and fluctuation strength.[41,42] While street traffic noise is a rather continuous and monotonous source of noise, railway, and aircraft traffic noise are characterized by noise events (i.e., a train or plane passing by). In our study, the risk for hemorrhagic stroke was particularly high for the group that experienced low continuous aircraft noise but several nightly noise events. Moreover, for railway noise − which is also characterized by single, potentially disturbing noise events − risk estimates for hemorrhagic stroke also tended to be higher than risk estimates for ischemic stroke. In contrast, we found road traffic noise to be associated with ischemic stroke, but not with hemorrhagic stroke. This may indicate that the risk for hemorrhagic stroke might be particularly increased by single disturbing nightly noise events, whereas the risk for ischemic stroke might be better reflected by continuous noise pressure levels. However, to date a convincing pathophysiological mechanism explaining this potential difference between the risks of ischemic and hemorrhagic stroke is lacking. One potential explanation could be that nightly disturbance may lead to acute blood pressure elevation which might have a stronger effect on hemorrhagic stroke risk than ischemic stroke risk. This would be in line with the finding that hypertension is a stronger predictor of hemorrhagic than of ischemic stroke,[39] and with the finding that traffic noise exposure is associated with a higher risk of hypertension-related diseases.[43]
Implications and future studies
An important novel result of our study is that nightly maximum aircraft noise levels are associated with an increased stroke risk, implying a strong effect of nightly disturbance that takes place from single maximum noise events, even if the continuous noise pressure levels are relatively low. It supports the hypothesis of disturbed sleep as one pathophysiological mechanism through which traffic noise increases stroke risk. The finding is similar to the risk increase for nightly maximum aircraft noise found for other cardiovascular diseases in previous studies, such as hypertensive heart disease and heart failure (OR = 1.06; 95%CI: 1.03–1.09),[44] and myocardial infarction (OR = 1.05 risk increase; 95%CI: 1.02–1.11).[40] These results could have important implications for the discussion about laws on banning night flights and exceptions to these bans, indicating that nightly maximum noise may be important when estimating health risks for populations living around airports. Furthermore, there are important implications for future research. Only examining continuous noise exposure (and thus adding the group exposed to low continuous noise but high maximum noise to the reference category) may lead to an underestimation of actual risks.
New approaches to classifying noise beyond continuous noise exposure, such as the intermittency ratio (expressing "the proportion of the acoustical energy contribution in the total energetic dose that is created by individual noise events above a certain threshold")[45] are currently being developed or have recently been published. Future research should examine different noise measures to determine those that are particularly relevant for predicting disease risks, and whether different types of noise (e.g., maximum versus continuous) increase the risk for different types of diseases. While in this study we only had data available on single incidents of noise exposure for aircraft traffic noise, future studies should investigate whether there are similar effects for railway traffic noise, and possibly also for road traffic noise.
Conclusion
Overall, this study suggests that traffic noise exposure may increase stroke risk. It furthermore indicates that maximum aircraft noise levels at night increase the stroke risk even when continuous noise exposure is low. This highlights the relevance of maximum noise levels for future research and policies regarding aircraft noise protection measures.
Financial support and sponsorship
This work was supported by the Gemeinnützige Umwelthaus GmbH, Kelsterbach. The funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the article; and in the decision to submit the article for publication.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organisation. Noncommunicable Diseases Progress Monitor. Geneva: World Health Organization; 2017. [Google Scholar]
- 2.Mendis S. Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: The World Health Organization; 2014. [DOI] [PubMed] [Google Scholar]
- 3.Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur Heart J. 2016;37:3232–45. doi: 10.1093/eurheartj/ehw334. [DOI] [PubMed] [Google Scholar]
- 4.Niemann H, Hoebel J, Hammersen F, Laußmann D. Noise Annoyance − Results of the GEDA Study 2012. Berlin: Robert Koch Institute; 2014. [Google Scholar]
- 5.WHO. Burden of Disease from Environmental Noise: Quantification of Healthy Life Years Lost in Europe. Bonn: WHO, European Centre for Environment and Health; 2010. [Last accessed on 2015 Oct 12]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0008/136466/e94888.pdf . [Google Scholar]
- 6.Münzel T, Gori T, Babisch W, Basner M. Cardiovascular effects of environmental noise exposure. Eur Heart J. 2014;35:829–36. doi: 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elmenhorst EM, Elmenhorst D, Wenzel J, Quehl J, Mueller U, Maass H, et al. Effects of nocturnal aircraft noise on cognitive performance in the following morning: Dose-response relationships in laboratory and field. Int Arch Occup Environ Health. 2010;83:743–51. doi: 10.1007/s00420-010-0515-5. [DOI] [PubMed] [Google Scholar]
- 8.Halonen JI, Vahtera J, Stansfeld S, Yli-Tuomi T, Salo P, Pentti J, et al. Associations between nighttime traffic noise and sleep: The Finnish public sector study. Environ Health Perspect. 2012;120:1391. doi: 10.1289/ehp.1205026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Babisch W. Stress hormones in the research on cardiovascular effects of noise. Noise Health. 2003;5:1–11. [PubMed] [Google Scholar]
- 10.Basner M, Babisch W, Davis A, Brink M, Clark C, Janssen S, et al. Auditory and non-auditory effects of noise on health. Lancet. 2014;383:1325–32. doi: 10.1016/S0140-6736(13)61613-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Badran M, Yassin BA, Fox N, Laher I, Ayas N. Epidemiology of sleep disturbances and cardiovascular consequences. Can J Cardiol. 2015;31:873–9. doi: 10.1016/j.cjca.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Hansell AL, Blangiardo M, Fortunato L, Floud S, de Hoogh K, Fecht D, et al. Aircraft noise and cardiovascular disease near Heathrow airport in London: small area study. BMJ. 2013;347:f5432. doi: 10.1136/bmj.f5432. [DOI] [PubMed] [Google Scholar]
- 13.Floud S, Blangiardo M, Clark C, de Hoogh K, Babisch W, Houthuijs D, et al. Exposure to aircraft and road traffic noise and associations with heart disease and stroke in six European countries: A cross-sectional study. Environ Health. 2013;12:89. doi: 10.1186/1476-069X-12-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huss A, Spoerri A, Egger M, Röösli M, Group SNCS. Aircraft noise, air pollution, and mortality from myocardial infarction. Epidemiology. 2010;21:829–36. doi: 10.1097/EDE.0b013e3181f4e634. [DOI] [PubMed] [Google Scholar]
- 15.Evrard AS, Bouaoun L, Champelovier P, Lambert J, Laumon B. Does exposure to aircraft noise increase the mortality from cardiovascular disease in the population living in the vicinity of airports? Results of an ecological study in France. Noise Health. 2015;17:328–36. doi: 10.4103/1463-1741.165058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Kempen EE, Kruize H, Boshuizen HC, Ameling CB, Staatsen BA, de Hollander AE. The association between noise exposure and blood pressure and ischemic heart disease: A meta-analysis. Environ Health Perspect. 2002;110:307–17. doi: 10.1289/ehp.02110307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ndrepepa A, Twardella D. Relationship between noise annoyance from road traffic noise and cardiovascular diseases: A meta-analysis. Noise Health. 2011;13:251–9. doi: 10.4103/1463-1741.80163. [DOI] [PubMed] [Google Scholar]
- 18.Babisch W. Updated exposure-response relationship between road traffic noise and coronary heart diseases: A meta-analysis. Noise Health. 2014;16:1–9. doi: 10.4103/1463-1741.127847. [DOI] [PubMed] [Google Scholar]
- 19.Sørensen M, Hvidberg M, Andersen ZJ, Nordsborg RB, Lillelund KG, Jakobsen J, et al. Road traffic noise and stroke: A prospective cohort study. Eur Heart J. 2011;32:737–44. doi: 10.1093/eurheartj/ehq466. [DOI] [PubMed] [Google Scholar]
- 20.de Kluizenaar Y, van Lenthe FJ, Visschedijk AJ, Zandveld PY, Miedema HM, Mackenbach JP. Road traffic noise, air pollution components and cardiovascular events. Noise Health. 2013;15:388. doi: 10.4103/1463-1741.121230. [DOI] [PubMed] [Google Scholar]
- 21.Beelen R, Hoek G, Houthuijs D, van den Brandt PA, Goldbohm RA, Fischer P, et al. The joint association of air pollution and noise from road traffic with cardiovascular mortality in a cohort study. Occup Environ Med. 2009;66:243–50. doi: 10.1136/oem.2008.042358. [DOI] [PubMed] [Google Scholar]
- 22.Greiser E, Greiser C. Environmental noise and health effects in Bremen city. Report for the German Federal Environment Agency. 2014 [Google Scholar]
- 23.Vienneau D, Perez L, Schindler C, Lieb C, Sommer H, Probst-Hensch N, et al. Years of life lost and morbidity cases attributable to transportation noise and air pollution: A comparative health risk assessment for Switzerland in 2010. Int J Hyg Environ Health. 2015;218:514–21. doi: 10.1016/j.ijheh.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 24.Gan WQ, Davies HW, Koehoorn M, Brauer M. Association of long-term exposure to community noise and traffic-related air pollution with coronary heart disease mortality. Am J Epidemiol. 2012;175:898–906. doi: 10.1093/aje/kwr424. [DOI] [PubMed] [Google Scholar]
- 25.Bundesregierung. German federal government. First decree about data collection and the calculation process for the determination of noise protection zones starting from December 27, 2008. Bundesanzeiger. 2008;2008(195a):192. [Google Scholar]
- 26.Bundesregierung. German Federal Government. Decree for the implementation of the national emission protection act (decree about noise mapping) Bundesanzeiger. 2006;2006(154a):156. [Google Scholar]
- 27.European Union. Directive 2002/49/EC of the European Parliament and of the Council of 25 June 2002 relating to the assessment and management of environmental noise − Declaration by the Commission in the Conciliation Committee on the Directive relating to the assessment and management of environmental noise. 2002. [32002L0049. [Last accessed on 2015 Nov 27]]. Available from: http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX .
- 28.Möhler U, Liepert M, Mühlbacher M, Beronius A, Nunberger M, Braunstein G, et al. Dokumentation zur Berechnung der akustischen Daten in NORAH. In: NORAH (Noise-related annoyance, cognition and health). Verkehrslärmwirkungen im Flughafenumfeld. Endbericht, Band 2. Gemeinnützige Umwelthaus GmbH; 2015. [Google Scholar]
- 29.Hoffmann B, Robra B-P, Swart E. Social inequality and road traffic noise in the residential environment: an evaluation of the national health survey. Gesundheitswesen. 2003;65:393–401. doi: 10.1055/s-2003-40308. [DOI] [PubMed] [Google Scholar]
- 30.Schubert I, Ihle P, Köster I. Internal validation of diagnoses in public health insurance routine data: conceptual design with examples and case definitions. Gesundheitswesen. 2010;72:316–22. doi: 10.1055/s-0030-1249688. [DOI] [PubMed] [Google Scholar]
- 31.Schmitt J, Ford D. Psoriasis is independently associated with psychiatric morbidity and adverse cardiovascular risk factors, but not with cardiovascular events in a population-based sample. J Eur Acad Dermatol Venereol. 2010;24:885–92. doi: 10.1111/j.1468-3083.2009.03537.x. [DOI] [PubMed] [Google Scholar]
- 32.Stansfeld SA. Noise effects on health in the context of air pollution exposure. Int J Environ Res Public Health. 2015;12:12735–60. doi: 10.3390/ijerph121012735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sørensen M, Lühdorf P, Ketzel M, Andersen ZJ, Tjønneland A, Overvad K, et al. Combined effects of road traffic noise and ambient air pollution in relation to risk for stroke? Environ Res. 2014;133:49–55. doi: 10.1016/j.envres.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 34.Blomstrand A, Blomstrand C, Ariai N, Bengtsson C, Björkelund C. Stroke incidence and association with risk factors in women: A 32-year follow-up of the Prospective Population Study of Women in Gothenburg. BMJ Open. 2014;4:e005173. doi: 10.1136/bmjopen-2014-005173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kroll ME, Green J, Beral V, Sudlow CL, Brown A, Kirichek O, et al. Adiposity and ischemic and hemorrhagic stroke: Prospective study in women and meta-analysis. Neurology. 2016;87:1473–81. doi: 10.1212/WNL.0000000000003171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laursen AS, Dahm CC, Johnsen SP, Tjonneland A, Overvad K, Jakobsen MU. Substitutions of dairy product intake and risk of stroke: A Danish cohort study. Eur J Epidemiol. 2018;33:201–12. doi: 10.1007/s10654-017-0271-x. [DOI] [PubMed] [Google Scholar]
- 37.Kivimäki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep. 2015;17:74. doi: 10.1007/s11886-015-0630-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fransson EI, Nyberg ST, Heikkilä K, Alfredsson L, Bjorner JB, Borritz M, et al. Job strain and the risk of stroke: An individual-participant data meta-analysis. Stroke. 2015;46:557–9. doi: 10.1161/STROKEAHA.114.008019. [DOI] [PubMed] [Google Scholar]
- 39.O’Donnell MJ, Xavier D, Liu L, Zhang H, Chin SL, Rao-Melacini P, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet. 2010;376:112–23. doi: 10.1016/S0140-6736(10)60834-3. [DOI] [PubMed] [Google Scholar]
- 40.Seidler A, Wagner M, Schubert M, Dröge P, Jörn Pons-Kühnemann J, Swart E, et al. Myocardial infarction risk due to aircraft, road, and rail traffic noise: Results of a case–control study based on secondary data. Dtsch Ärztebl Int. 2016;113:407–14. doi: 10.3238/arztebl.2016.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fastl H. The psychoacoustics of sound-quality evaluation. Acta Acust United Acust. 1997;83:754–64. [Google Scholar]
- 42.Marquis-Favre C, Premat E, Aubrée D. Noise and its effects − A review on qualitative aspects of sound. Part II: Noise and annoyance. Acta Acust United Acust. 2005;91:626–42. [Google Scholar]
- 43.Zeeb H, Hegewald J, Schubert M, Wagner M, Dröge P, Swart E, et al. Traffic noise and hypertension − Results from a large case-control study. Environ Res. 2017;157:110–7. doi: 10.1016/j.envres.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 44.Seidler A, Wagner M, Schubert M, Dröge P, Römer K, Pons-Kühnemann J, et al. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease − A case–control study based on secondary data. Int J Hyg Environ Health. 2016;219:749–58. doi: 10.1016/j.ijheh.2016.09.012. [DOI] [PubMed] [Google Scholar]
- 45.Wunderli JM, Pieren R, Habermacher M, Vienneau D, Cajochen C, Probst-Hensch N, et al. Intermittency ratio: A metric reflecting short-term temporal variations of transportation noise exposure. J Expo Sci Environ Epidemiol. 2016;26:575–85. doi: 10.1038/jes.2015.56. [DOI] [PMC free article] [PubMed] [Google Scholar]


