Abstract
Clinical diagnostic values of B-mode ultrasound and computed tomography (CT) for tuberculous pleuritis were investigated. A total of 685 patients clinically diagnosed with tuberculous pleuritis in Yantaishan Hospital from January 2012 to August 2016 were selected as study subjects. The patients were examined by B-mode ultrasound and CT. The accuracy of B-mode ultrasound and CT in the diagnosis of tuberculous pleuritis was evaluated and the benefit-cost ratios of the two auxiliary diagnostic methods were compared. According to the imaging diagnostic results of 685 tuberculous pleuritis patients, B-mode ultrasound examinations identified 415 cases with tuberculous pleuritis and the accuracy rate was 60.15%. CT examinations identified 501 cases with the tuberculous pleuritis and the accuracy rate was 70.07%. The combined use of these two methods identified 546 cases with the tuberculous pleuritis and the accuracy rate was significantly increased to 85.99%. B-mode ultrasound imaging findings showed that the lesions of tuberculous pleuritis were localized on the right pleural cavities and the majority of images presented the free type; multiple anechoic areas were seen in the effusion. CT findings indicated obvious free effusion in the pleural cavities, local thickening of the pleural cavities, encapsulated pleural effusion and extensive pleural adhesion, thickening and calcification. Both B-mode ultrasound and CT examinations can be used to accurately diagnose tuberculous pleuritis and the combined diagnosis can significantly improve the accuracy.
Keywords: B-mode ultrasound, computed tomography, tuberculous pleuritis, imaging manifestations, diagnosis
Introduction
Tuberculous pleuritis is the pleuritis induced by the entering of tuberculous bacilli and their metabolites and autolysates into the pleural cavities of hypersensitive organisms and is a common disease in clinical practice (1,2). The tuberculous pleuritis is an acute disease and mainly exhibits two major symptoms (3), namely, the local symptom induced by pleural effusion accumulation and the systemic toxic symptom caused by tuberculosis. Tuberculous pleuritis belongs to the infectious diseases and its infection source is tuberculous bacillus (4). Globally, there are ~2.1 billion individuals infected with the tuberculous bacillus every year, and most patients were reported in India and Russia (5). Pulmonary tuberculosis induced by the tuberculous bacillus is the most common type, and patients with tuberculous pleuritis account for ~3.0% of all pulmonary tuberculosis patients (4). Treatment of the tuberculous pleuritis is not difficult but the treatment period is long and the recurrence rate is high. Therefore, early diagnosis and treatment are still critical (6).
Currently, the most common diagnostic method of this disease is B-mode ultrasound imaging or computed tomography (CT) examination, but the application of single examination are challenged by some shortcomings, such as the low accuracy rate and high rate of misdiagnosis (7). In this study, a total of 685 cases with tuberculous pleuritis who were admitted to Yantaishan Hospital (Yantai, China) from January 2012 to August 2016 were selected as the study subjects. Indicators of the tuberculous pleuritis diagnoses by B-mode ultrasound, CT and the combined application were analyzed, respectively, to provide reference and guidance for the clinical diagnoses of the tuberculous pleuritis.
Patients and methods
Clinical data
A total of 685 patients who were treated in Yantaishan Hospital from January 2012 to August 2016 and pathologically diagnosed with tuberculous pleuritis, were selected to serve as study subjects. Those patients included 399 male cases and 286 female cases with a mean age of 48.6±12.3 years. Clinical data of patients including sex, age and hospitalization time were collected. The study was approved by the Ethics Committee of Yantaishan Hospital (Yantai, China) and informed consents were signed by the patients or the guardians.
Methods
All patients underwent CT examination 1–2 weeks after B-mode ultrasound in Yantaishan Hospital. B-mode ultrasound diagnosis: Philips EPIQ5 B-mode ultrasound examination instrument (Philips Healthcare, Amsterdam, The Netherlands) was used. Patients were fixed in sitting position with both hands raised and the body slightly bending forward and the examination of the longitudinal section was started from the area between the 7th and 8th rib of the posterior axillary lines. The effusion area was reached when no echoes were detected. Examination was then conducted on the diagonal plane along the intercostal spaces and the range and thickness of the effusion were recorded. Pleural thickness of patients was observed and the range of the liquid anechoic area was measured to confirm the existence of suspicious echoes. Puncture fluid was collected under the guidance of B-mode ultrasound if suspicious echoes existed to conduct further examination. CT diagnosis: LightSpeed spiral CT examination instrument with 64 rows and 128 layers (GE Healthcare, Chicago, IL, USA) was used. Patients were fixed in supine position and the routine 4-mm thick-layer interval-free scanning was conducted in the area from the scanned pulmonary apexes to the bilateral costal diaphragmatic angles with breath-holding. If obvious shaded area could not be recognized, foregoing scanning could be replaced by 2-mm thin-layer interval-free scanning or high-resolution computed tomography (HRCT) scanning. B-mode ultrasound and CT imaging results were evaluated with reference to the diagnostic standard for the tuberculous pleuritis established by Porcel (4). With pathological diagnosis with reference, the diagnostic values of B-mode ultrasound, CT diagnosis and combined diagnosis were compared. Diagnostic sensitivity = true-positive number of patients/(number of true-positive patients + false-negative patients) ×100%; diagnostic specificity = true-negative number of patients/(number of false-positive + true-negative patients) ×100%; diagnostic coincidence = (number of true-positive + true-negative patients)/total number of patients ×100%; positive predictive value = true-positive number of patients/(number of true-positive patients + false-positive patients) ×100%.
Inclusion and exclusion criteria
Inclusion criteria: patients with clinical symptoms of the tuberculous pleuritis; patients diagnosed with B-mode ultrasound and CT; patients pathologically diagnosed with tuberculous pleuritis; patients with positive results of purified protein derivative (PPD). Exclusion criteria: patients accompanied with other pulmonary diseases; patients with a history of cardiopulmonary diseases; patients that suffered from pulmonary dysfunction; patients transferred to other hospitals during treatment. All the patients signed an informed consent.
Interpretation of results
All imaging results were reviewed by the 3 senior imaging physicians of the hospital using a double-blind method. B-mode ultrasonography usually showed free-style images, and patients with multiple echo-free areas within the effusion were diagnosed with tuberculous pleurisy. In CT examination, patients with free pleural effusion, pleural constriction thickening, pleural effusion, pleural extensive thickening, adhesion, calcification, mild to moderate contrast medium injection and CT value >25 HU were diagnosed with tuberculous pleurisy. In the combination, patients with positive diagnosis of both examinations were diagnosed with tuberculous pleurisy.
Statistical analysis
Experimental results were analyzed by Statistical Product and Service Solutions (SPSS) 22.0 statistical software [AsiaAnalytics (formerly SPSS China), Shanghai, China]. Enumeration data are expressed as rate. Intergroup comparisons were made by χ2 test. P<0.05 was considered to indicate a statistically significant difference.
Results
Clinical data
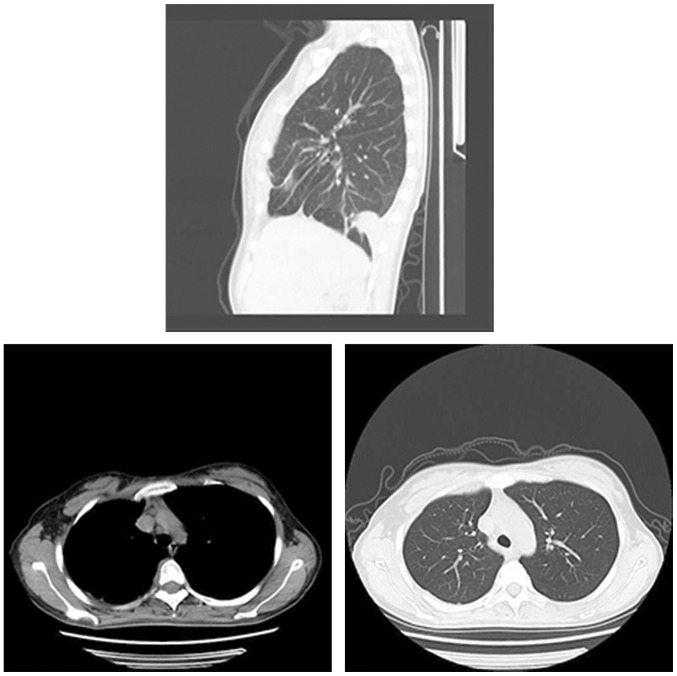
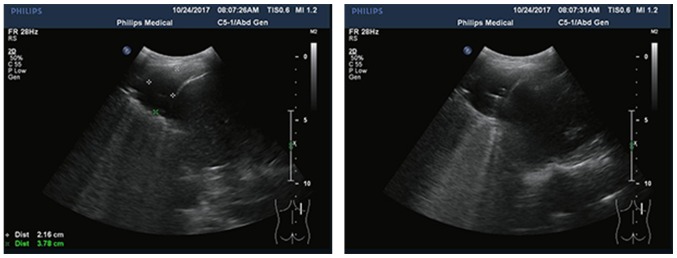
Clinical data of patients including sex, age and hospitalization time are shown in Table I. Pleural effusion was mainly localized in the right parts and the amount of yellow pleural effusion was significantly more than bloody effusion (Table I). The typical CT and ultrasound images are shown in Figs. 1 and 2.
Table I.
Clinical data of patients (n, %).
| Variables | Values |
|---|---|
| Sex | |
| Male | 399 (58.2) |
| Female | 286 (41.8) |
| Age (years) | |
| <30 | 428 (62.5) |
| ≥30 | 257 (37.5) |
| Hospitalization time (h) | |
| <10 | 345 (50.4) |
| ≥10 | 340 (49.6) |
| Clinical symptoms | |
| Fever | 272 (39.7) |
| Chest pain | 178 (26.0) |
| Chest distress | 156 (22.8) |
| Dyspnea | 79 (11.5) |
| Residential location | |
| Urban | 386 (56.4) |
| Rural | 299 (43.6) |
| Distribution of pleural effusion | |
| Left | 171 (25.0) |
| Right | 418 (61.0) |
| Bilateral | 96 (14.0) |
| Exercise habit | |
| Yes | 441 (64.4) |
| No | 244 (35.6) |
| Smoking history | |
| Yes | 496 (72.4) |
| No | 189 (27.6) |
| Color of pleural effusion | |
| Yellow | 562 (82.1) |
| Bloody | 123 (17.9) |
Figures 1.
CT images of patients with tuberculous pleurisy. Thorax is symmetrical and mediastinum is in the middle. Lung texture is natural. The right lung is scattered in a strip-like high-density shadow. The right side of the pleura shows nodular thickening. Trachea and bronchi are unobstructed, with no thickening of the wall of the tube. There were no enlarged lymph nodes and abnormal lumps in the mediastinum. The size and shape of the heart were normal, and no abnormal changes were seen in the vasculature. Right lung shows a patchy shadow, possibly indicating right pneumonic lesion and right pleural effusion. Right pleural nodules were thickened, indicating tuberculous pleurisy or pleural lesions. CT, computed tomography.
Figure 2.
Tuberculous pleurisy B-scan images. Multi-section scanning at the back: sheet liquid dark area was detected at the right chest cavity, upper and lower diameter was ~3.8 cm, and the depth was ~2.2 cm. No visible fluid dark areas were seen in the left thoracic cavity and a small amount of effusion was seen in the right thoracic cavity.
Diagnostic results
Among 685 patients, there were 574 cases of tuberculous pleurisy and 111 cases of other types of pleurisy, including 34 cases of fibrin pleurisy, 57 cases of connective tissue disease, 18 cases of serofibrin pleurisy and 2 cases of tumor pleurisy. Further observation showed that the patients with tuberculous pleurisy had been in contact with the same type of patients, suggesting that more attention should be paid to the isolation of infectious diseases. A total of 451 cases of tuberculous pleurisy were diagnosed by B-mode ultrasound, 501 cases were diagnosed by CT and 546 cases were diagnosed by B-mode ultrasound combined with CT (Tables II–IV).
Table II.
Tuberculous pleurisy diagnosed by B-mode ultrasound.
| Item | Bacterial culture (+) | Bacterial culture (−) | Total |
|---|---|---|---|
| B-mode ultrasound (+) | 376 | 75 | 451 |
| B-mode ultrasound (−) | 198 | 36 | 234 |
| Total | 574 | 111 |
Table IV.
Tuberculous pleurisy diagnosed by B-mode ultrasound combined with CT.
| Item | Bacterial culture (+) | Bacterial culture (−) | Total |
|---|---|---|---|
| Combination diagnosis (+) | 512 | 34 | 546 |
| Combination diagnosis (−) | 62 | 77 | 139 |
| Total | 574 | 111 |
CT, computed tomography.
Differences between B-mode ultrasound and CT examination
Compared with the findings of CT examination, B-mode ultrasound examination was less effective concerning the thickening of the parietal pleura and the combined pericardial effusion. There were no obvious differences concerning the pleural effusion and calcification between the results of the two methods (P>0.05) (Table V).
Table V.
Imaging diagnostic results of B-mode ultrasound and CT examinations (n, %).
| Item | B-mode ultrasound | CT | χ2 | P-value |
|---|---|---|---|---|
| Pleural effusion | 534 (77.96) | 492 (71.82) | 6.847 | 0.071 |
| Pleural calcification | 507 (74.01) | 497 (72.55) | 0.373 | 0.068 |
| Parietal pleura thickening | 19 (2.77) | 149 (21.75) | 114.723 | 0.021 |
| Pericardial effusion | 41 (5.99) | 86 (12.55) | 17.571 | 0.036 |
CT, computed tomography.
Sensitivity and specificity of B-mode ultrasound, CT and the combined diagnosis
The sensitivity and specificity of the three diagnostic methods for the tuberculous pleuritis were as follows: the sensitivity of B-mode ultrasound was 85.51%, the specificity 72.34%, the diagnostic accordance rate 60.15% and the positive predictive value 83.37%; the sensitivity of CT was 79.69%, the specificity 83.44%, the diagnostic accordance rate 70.07% and the positive predictive value 86.83%; the sensitivity of B-mode ultrasound + CT was 93.81%, the specificity 95.75%, the diagnostic accordance rate 85.99% and the positive predictive value 93.77%. The sensitivity, specificity, diagnostic accordance rate and positive predictive value of the combined diagnosis were increased compared with those of single examination (P<0.05) (Table VI).
Table VI.
Sensitivity and specificity of the three kinds of diagnostic methods (%).
| Item | Sensitivity | Specificity | Diagnostic accordance rate | Positive predictive value |
|---|---|---|---|---|
| B-mode ultrasound | 85.51 | 72.34 | 60.15 | 83.37 |
| CT | 79.69 | 83.44 | 70.07 | 86.83 |
| B-mode ultrasound + CT | 93.81 | 95.75 | 85.99 | 93.77 |
| χ2 | 91.031 | 23.964 | 115.673 | 27.530 |
| P-value | 0.0429 | 0.0457 | 0.0305 | 0.0427 |
CT, computed tomography.
Discussion
Tuberculous pleuritis is the most common cause of pleural effusion (8). After tuberculous bacilli infects pleura, cell-mediated immune response is induced by the stimulation of the inflammation, leading to a series of symptoms such as edema and congestion, proliferation of lymphocytes and the exudation of fibrous proteins on the pleural surfaces. Under those conditions, capillary permeability is greatly increased, and a large amount of proteins, blood cells and water is accumulated in pleural cavities and form the pleural effusion (9,10). Accumulation of the pleural effusion causes the decline in absorption ability of visceral pleura and non-absorbable proteins and celluloses form fibrous moss in pleura. As a result, the thickening, wrapping and adhesion of the pleura occurs. In severe cases, the respiratory function is directly affected, leading to asphyxia (11,12).
According to patients' clinical data, most patients with tuberculous pleuritis were younger than 30 years old, the pleural effusion of patients mainly aggregated in the right side and was mostly yellow effusion. Clinical symptoms mainly included fever, the incidence among urban residents was higher than that among rural residents, and higher incidence was observed in smoking individuals. Possible explanations for these observations are: young and adult patients are more vulnerable to this disease due to the stronger response to the infection of tuberculosis bacilli compared with patients in other age groups (13); urban residents were exposed to harmful gases (factory emission, vehicle exhaust and passive smoking) and transmission of the tuberculous pleuritis is easier; for the smoking patients, nicotine, tar, carbon monoxide and other harmful gases may destroy the original immune system and the filtration system of the lungs, thus it is easier for the tuberculous bacillus to infect the cardio-pulmonary functions (14,15). The bacteriological culture examination cannot make the diagnosis to the pleurisy caused by the non-bacterial pathogen, therefore, the tuberculous pleurisy is generally excluded and needs to go through many examinations to confirm the pathological type. Accuracy rates of B-mode ultrasound, CT examination and the combined diagnosis were compared with the pathological diagnosis. Results showed that there were basically no differences in the accuracy between B-mode ultrasound and CT diagnoses. CT examination is more helpful in the identification of the thickening of parietal pleura and combined pericardial effusion. However, the accuracy, specificity and sensitivity of the combined diagnosis were higher than those of single examination. B-mode ultrasound diagnosis is the simplest examination method with high economic effectiveness and CT examination has not been popularized in the majority of primary hospitals. Therefore, most patients with tuberculous pleuritis are diagnosed by B-mode ultrasound. B-mode ultrasound is highly sensitive to pleural effusion and can accurately localize the effusion. B-mode ultrasound can be used to accurately estimate effusion location and volume. In addition, B-mode ultrasound can also be used to guide the extraction of the puncture fluid from the pleural cavities and the identification of the thickening of pleura (16). Nevertheless, with B-mode ultrasound it is hard to detect substantive void, the place communicating with the pleural cavity, lymph node enlargement and other lesion conditions in the lungs of the tuberculous pleuritis patients, thus the specificity is not high. Therefore, the accuracy of B-mode ultrasound in the diagnosis of tuberculous pleuritis is slightly lower than that of CT. This is consistent with the findings reported by Brunetti et al (17). CT examination has the higher density and spatial resolution and can more accurately show the thickening of the parietal pleura and pericardial effusion in patients with tuberculous pleuritis compared with B-mode ultrasound. Moreover, it can be used to examine the lymphatic vessels and old tuberculous focus (18). The combined examination by B-mode ultrasound and CT can compensate the shortcomings of the two single examinations and improve the specificity, sensitivity and accuracy.
In this study, clinical data of 685 cases of tuberculous pleuritis were retrospectively analyzed with the expectation of providing new insights for the diagnosis of this disease using B-mode ultrasound and CT. However, there are still shortcomings. The comparison of the results of B-mode ultrasound and CT among different age groups and between smokers and non-smokers were not studied. So, more studies are still needed.
In conclusion, both B-mode ultrasound and CT can accurately diagnose tuberculous pleuritis, but the combined diagnosis by the two methods can compensate the shortcomings of each technique. Therefore, the combined diagnosis should be popularized in clinical practice.
Table III.
Tuberculous pleurisy diagnosed by CT.
| Item | Bacterial culture (+) | Bacterial culture (−) | Total |
|---|---|---|---|
| CT (+) | 435 | 66 | 501 |
| CT (−) | 139 | 45 | 184 |
| Total | 574 | 111 |
CT, computed tomography.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
SZ, JZ and YP conceived and designed the study. SZ, XS and MZ were responsible for the collection and analysis of the patient data. JZ and HL interpreted the data and drafted the manuscript. YP revised the manuscript critically for important intellectual content. All authors read and approved the final study.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Yantaishan Hospital (Yantai, China). Signed informed consents were obtained from the patients or the guardians.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Chakrabarti B, Davies PD. Pleural tuberculosis. Monaldi Arch Chest Dis. 2006;65:26–33. doi: 10.4081/monaldi.2006.582. [DOI] [PubMed] [Google Scholar]
- 2.Lee JY. Diagnosis and treatment of extrapulmonary tuberculosis. Tuberc Respir Dis (Seoul) 2015;78:47–55. doi: 10.4046/trd.2015.78.2.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vorster MJ, Allwood BW, Diacon AH, Koegelenberg CF. Tuberculous pleural effusions: Advances and controversies. J Thorac Dis. 2015;7:981–991. doi: 10.3978/j.issn.2072-1439.2015.02.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Porcel JM. Advances in the diagnosis of tuberculous pleuritis. Ann Transl Med. 2016;4:282. doi: 10.21037/atm.2016.07.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sia JK, Georgieva M, Rengarajan J. Innate immune defenses in human tuberculosis: An overview of the interactions between mycobacterium tuberculosis and innate immune cells. J Immunol Res. 2015;2015:747543. doi: 10.1155/2015/747543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen KY, Feng PH, Chang CC, Chen TT, Chuang HC, Lee CN, Su CL, Lin LY, Lee KY. Novel biomarker analysis of pleural effusion enhances differentiation of tuberculous from malignant pleural effusion. Int J Gen Med. 2016;9:183–189. doi: 10.2147/IJGM.S100237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dietrich CF, Mathis G, Cui XW, Ignee A, Hocke M, Hirche TO. Ultrasound of the pleurae and lungs. Ultrasound Med Biol. 2015;41:351–365. doi: 10.1016/j.ultrasmedbio.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Cao GQ, Li L, Wang YB, Shi ZZ, Fan DY, Chen HY. Treatment of free-flowing tuberculous pleurisy with intrapleural urokinase. Int J Tuberc Lung Dis. 2015;19:1395–1400. doi: 10.5588/ijtld.15.0128. [DOI] [PubMed] [Google Scholar]
- 9.Porcel JM, Gasol A, Bielsa S, Civit C, Light RW, Salud A. Clinical features and survival of lung cancer patients with pleural effusions. Respirology. 2015;20:654–659. doi: 10.1111/resp.12496. [DOI] [PubMed] [Google Scholar]
- 10.Yousefifard M, Baikpour M, Ghelichkhani P, Asady H, Shahsavari Nia K, Moghadas Jafari A, Hosseini M, Safari S. Screening performance characteristic of ultrasonography and radiography in detection of pleural effusion; a meta-analysis. Emerg (Tehran) 2016;4:1–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen AH, Miller EJ, Wichman CS, Berim IG, Agrawal DK. Diagnostic value of tumor antigens in malignant pleural effusion: A meta-analysis. Transl Res. 2015;166:432–439. doi: 10.1016/j.trsl.2015.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Antonangelo L, Sales RK, Corá AP, Acencio MM, Teixeira LR, Vargas FS. Pleural fluid tumour markers in malignant pleural effusion with inconclusive cytologic results. Curr Oncol. 2015;22:e336–e341. doi: 10.3747/co.22.2563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kahwati LC, Feltner C, Halpern M, Woodell CL, Boland E, Amick HR, Weber RP, Jonas DE. Primary care screening and treatment for latent tuberculosis infection in adults: Evidence report and systematic review for the US preventive services task force. JAMA. 2016;316:970–983. doi: 10.1001/jama.2016.10357. [DOI] [PubMed] [Google Scholar]
- 14.Bae KM, Lim SC, Kim HH, Lee WJ, Yun NR, Kim CM, Kim DM. The relevance of biopsy in tuberculosis patients without human immunodeficiency virus infection. Am J Trop Med Hyg. 2015;92:636–640. doi: 10.4269/ajtmh.14-0656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manglani RP, Khaja M, Hennessey K, Kennedy O. Pleural mycobacterium avium complex infection in an immunocompetent female with no risk factors. Case Rep Pulmonol. 2015;2015:760614. doi: 10.1155/2015/760614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koegelenberg CF, Irusen EM, von Groote-Bidlingmaier F, Bruwer JW, Batubara EM, Diacon AH. The utility of ultrasound-guided thoracentesis and pleural biopsy in undiagnosed pleural exudates. Thorax. 2015;70:995–997. doi: 10.1136/thoraxjnl-2014-206567. [DOI] [PubMed] [Google Scholar]
- 17.Brunetti E, Heller T, Richter J, Kaminstein D, Youkee D, Giordani MT, Goblirsch S, Tamarozzi F. Application of ultrasonography in the diagnosis of infectious diseases in resource-limited settings. Curr Infect Dis Rep. 2016;18:6. doi: 10.1007/s11908-015-0512-7. [DOI] [PubMed] [Google Scholar]
- 18.Metintas M, Yildirim H, Kaya T, Ak G, Dundar E, Ozkan R, Metintas S. CT scan-guided Abrams' needle pleural biopsy versus ultrasound-assisted cutting needle pleural biopsy for diagnosis in patients with pleural effusion: A randomized, controlled trial. Respiration. 2016;91:156–163. doi: 10.1159/000443483. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.