Abstract
The present study was conducted to screen serum exosomal microRNAs (miRNAs) for the early diagnosis of Kawasaki disease (KD) and to investigate their underlying mechanisms by analyzing microarray data under accession numbers GSE60965 [exosomal miRNA, including three pooled serum samples from 5 healthy children, 5 patients with KD and 5 patients with KD following intravenous immunoglobulin (IVIG) therapy] and GSE73577 (mRNA, including peripheral blood mononuclear cell samples from 19 patients with KD prior to and following IVIG treatment) from the Gene Expression Omnibus database. Differentially expressed miRNAs (DE-miRNAs) and genes (DEGs) were identified using the Linear Models for Microarray data method, and the mRNA targets of DE-miRNAs were predicted using the miRWalk 2.0 database. The functions of the target genes were analyzed using the Database for Annotation, Visualization and Integrated Discovery (DAVID). As a result, 65 DE-miRNAs were identified with different expression patterns between the healthy children and patients with KD and between patients with KD and patients with KD following IVIG therapy. The target genes of 15 common DE-miRNAs were predicted. Following overlapping the target genes of DE-miRNAs with 355 DEGs, 28 common genes were identified and further screened to construct a network containing 30 miRNA-mRNA regulatory associations. Of these associations, only miR-328-spectrin α, erythrocytic 1, miR-575-cyclic AMP-responsive element-binding protein 5/b-1,4-galactosyltransferase 5/WD repeat and FYVE domain-containing 3/cystatin-A/C-X-C motif chemokine receptor 1/protein phosphatase 1 regulatory subunit 3B, miR-134-acyl-CoA synthetase long chain family member 1/C-type lectin domain family 1 member A and miR-671-5p-tripartite motif containing 25/leucine rich repeat kinase 2/kinesin family member 1B/leucine rich repeat neuronal 1 were involved in the negative regulation of gene expression. Functional analysis indicated that the identified target genes may be associated with inflammation. Accordingly, serum exosomal miR-328, miR-575, miR-134 and miR-671-5p may act as potential biomarkers for the diagnosis of KD and the prediction of outcomes of the IVIG therapy by influencing the expression of inflammatory genes.
Keywords: Kawasaki disease, vasculitis, biomarker, exosome, microRNA, inflammatory, intravenous immunoglobulin
Introduction
Kawasaki disease (KD) is a common, acute, systemic vasculitis that occurs in children <5 years old in Asian populations, with estimated incidence rates of 264.8, 134.4, 66.24 and 71.9 per 100,000 children in Japanese (1), Korean (2), Taiwanese (3) and Chinese (4) populations, respectively. KD predominantly affects small- to medium-sized vessels, including coronary arteries (5). If diagnosis is delayed and KD is left untreated, coronary artery lesions may develop in 25% of patients, which, in turn, increases the formation risk of coronary artery aneurysms (CAAs) and, subsequently, can induce coronary artery thrombosis, myocardial infarction or even sudden death (6,7). Intravenous immunoglobulin (IVIG) infusion is an effective, first-line therapy for KD (8). However, ~30% of cases have been reported to be unresponsive to IVIG, and additional therapy is required (9). If patients who are unresponsive to IVIG therapy are not identified in a timely manner, CAAs may still develop (10). Therefore, the early diagnosis of KD and the prediction of the therapeutic outcomes of IVIG are important issues.
At present, the diagnosis and evaluation of therapeutic effects primarily depend on clinical symptoms (including fever for ≥ five days, conjunctivitis, erythema of the lips and oral mucosa, extremity swelling, rash and cervical lymphadenopathy) (11), and ultrasonic imaging results (including QT interval dispersion) (12). However, these presentations overlap with other febrile illnesses in childhood (including epistaxis, scarlet fever, bovillae or juvenile idiopathic arthritis) and, therefore, are not specific (13). In addition, accumulating evidence indicates that the development of KD may be associated with the abnormal activation of the immune system and inflammation (14,15). Several inflammatory cytokines in the serum [including tumor necrosis factor α (TNF-α), interleukin (IL)-6, IL-17, IL-22 and IL-23] have been suggested to be biomarkers for the diagnosis of KD and IVIG therapy (16–18). However, certain studies reported that inflammatory markers are also non-specific and usually decreased in patients who are unresponsive to initial therapy (19,20). Therefore, novel biomarkers for the diagnosis of KD and for the prediction of therapeutic effects are required.
MicroRNAs (miRNAs) are endogenous, small, non-coding RNAs (~19–22 nucleotides in length) that serve roles in the regulation of diverse physiological and pathological processes through the complementary binding of target genes in the 3′untranslated region, for cleavage or translational repression (21). Furthermore, miRNAs can be present in the serum due to resistance against ribonuclease digestion and serum miRNAs are stable with consistent levels among individuals of the same species (21). Therefore, serum miRNAs that regulate the expression of inflammatory genes may serve as potential biomarkers for the diagnosis of KD and the prediction of therapeutic outcomes. This hypothesis has been supported by recent studies. Using miRNA microarray assays, Yun et al (22) demonstrated that miR-200c and miR-371-5p were significantly upregulated in children with KD, compared with controls. Further, Zhang et al (23) observed that serum miR-200c and miR-371-5p levels were significantly increased in patients with KD who were unresponsive to IVIG therapy compared with patients with KD who exhibited a good response to IVIG therapy. The combination of serum miR-200c and miR-371-5p exhibited high predictive values for the diagnosis of patients with KD [area under the curve (AUC)=0.95] and for those with an excellent IVIG response (AUC=0.97) (23). Furthermore, Yun et al (22) predicted that miR-200c and miR-371 may be involved in KD by targeting the regulation of a series of inflammatory response genes. In addition to their intracellular presence, miRNAs can also be enveloped into nanoparticles, termed exosomes, which maintain the integrity of miRNAs and transfer the miRNAs to recipient cells, influencing their phenotypes (24). Therefore, serum exosomal miRNAs may represent important biomarkers for various diseases (24). To date, exosomal miRNAs have been demonstrated to be useful in the early diagnosis of several cancers (25,26). The studies on KD and the IVIG therapy remain rare, except for the study by Jia et al (27), which identified four exosomal miRNA biomarkers, including miR-1246, miR-4436b-5p, miR-197-3p and miR-671-5p. The roles and mechanisms through which these miRNAs may act were not investigated.
Several studies reported that the addition of serum induces the production of pro-inflammatory cytokines (IL-1Ra, IFNα, IL-6, TNF-α and C-C motif chemokine 20) by peripheral blood mononuclear cells (PBMCs) (28–31), indicating that serum-secreted factors (including exosomes) may be of importance in maintaining this function. This hypothesis was indirectly demonstrated by the following studies. Harshyne et al (32) demonstrated that exosome-enriched fractions from sera of patients with glioblastoma are capable of inducing scavenger receptor cysteine-rich type 1 protein M130 expression in normal monocytes. Zhou et al (33) demonstrated that serum exosomes primed macrophage polarization towards the M2 phenotype. Accordingly, the present study hypothesized that serum exosomal miRNAs may be involved in KD by influencing the genes expressed by PBMCs.
The aim of the present study was to further analyze the exosomal miRNA microarray data established by Jia et al (27) and to predict their functions by overlapping their predicted target genes with differentially expressed genes (DEGs) in PBMCs (34). Compared with the study by Jia et al (27), the cut-off value [log fold change (FC) ≥6 vs. FC >200] for screening differentially expressed miRNAs (DE-miRNAs) was broadened to identify an increased number of exosomal miRNAs.
Materials and methods
Microarray data
The miRNA microarray data were collected from the Gene Expression Omnibus (GEO) database (www.ncbi.nlm.nih.gov/geo), under the accession number GSE60965, which included the exosomal miRNA profiles of three pooled serum samples collected from 5 healthy children [the normal (N) group], 5 patients with Kawasaki disease (the KD group) and 5 patients with KD following IVIG therapy (the IVIG group) (27). The microarray platform was GPL16730 Agilent-039659 hs_miR_18_addvirus 038169.
The mRNA microarray dataset was also available from the GEO database, under the accession number GSE73577, in which PBMCs samples of 19 patients with KD were investigated prior to and following IVIG treatment (34). This dataset was dependent on a two-channel microarray platform (GPL4133, Agilent-014850 Whole Human Genome Microarray 4×44K G4112F), and two repeats were performed for each patient.
Data normalization and the identification of DE-miRNAs and DEGs
The raw data from the two datasets and the annotated symbols were downloaded from the corresponding platforms. All expression values were logarithmically transformed (base 2) and quantile normalized using the Bioconductor preprocessCore package (version 1.28.0; www.bioconductor.org/packages/release/bioc/html/preprocessCore.html) (35).
Since one pooled sample per group was used for the analysis of exosomal miRNA profiles, the DE-miRNAs between the N and KD groups and between the KD and IVIG groups were only screened by calculating the logFC value. |logFC|≥6 was set as the threshold value. Further, a Venn diagram was built using the Bioinformatics and Evolutionary Genomics online tool (bioinformatics.psb.ugent.be/webtools/Venn) to determine the overlap between DE-miRNAs that were upregulated or downregulated in the KD group compared with the N group and DE-miRNAs that were downregulated or upregulated in the IVIG group compared with the KD group, so that the DE-miRNA alterations that were observed in the KD group and were reversed by IVIG could be identified.
The DEGs of patients with KD prior to and following IVIG treatment were identified using the Linear Models for Microarray data (LIMMA) package (v.2.16.4; bioconductor.org/packages/release/bioc/html/limma.html) (36) in the Bioconductor R software environment (v.3.4.1; http://www.R-project.org/). The P-values of the DEGs were calculated using Student's t-test. P<0.05 and |logFC|>0.5 were considered the cut-off criteria.
A heat map of DE-miRNAs and DEGs was plotted using the pheatmap R package (v.1.0.8; cran.r-project.org/web/packages/pheatmap/index.html), based on a bidirectional hierarchical clustering analysis with Euclidean distance (37).
Target gene predictions for DE-miRNAs
mRNA targets of DE-miRNAs were predicted using the miRWalk database (v.2.0; zmf.umm.uni-heidelberg.de/apps/zmf/mirwalk2), which includes 12 prediction algorithms (DIANA-microTv4.0, DIANA-microT-CDS, miRanda-rel2010, mirBridge, miRDB4.0, miRmap, miRNAMap, PicTar2, PITA, RNA22v2, RNAhybrid2.1 and Targetscan6.2). Only the miRNA-target gene interactions predicted by ≥ four algorithms were collected to construct a regulatory network and visualized using Cytoscape software (v.2.8; www.cytoscape.org) (38).
In addition, the target genes of DE-miRNAs and DEGs were analyzed using a Venn diagram (bioinformatics.psb.ugent.be/webtools/Venn) to identify the overlapping genes. The shared DE-miRNA-target interactions were also visualized using Cytoscape software (v.2.8; www.cytoscape.org) (38).
Functional enrichment analysis
To analyze the potential functions of identified target genes, Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analyses were performed using the Database for Annotation, Visualization and Integrated Discovery (DAVID) 6.8 online tool (david.abcc.ncifcrf.gov) (39). P<0.05 was considered to indicate a statistically significant difference.
Results
Identification of exosomal DE-miRNAs
According to the threshold of |logFC|≥6, 86 exosomal DE-miRNAs were identified between the N and KD groups, including 49 that were upregulated and 37 that were downregulated, while 77 DE-miRNAs were identified between the KD and IVIG groups, including 30 that were upregulated and 47 that were downregulated.
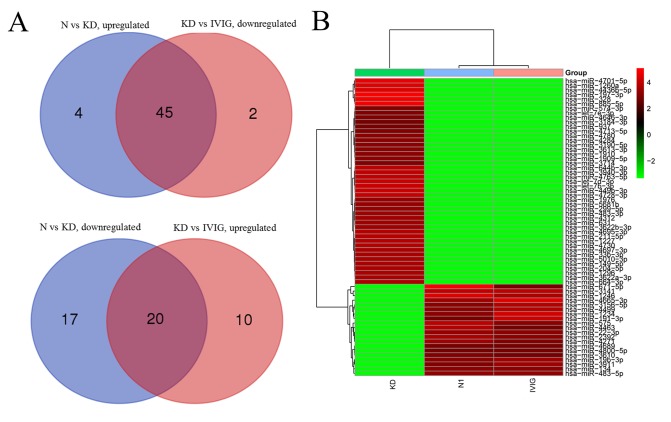
Following overlapping the DE-miRNAs that were upregulated in the KD group compared with the N group with the DE-miRNAs that were downregulated in the IVIG group compared with the KD group, 45 common DE-miRNAs were obtained. A total of 20 common DE-miRNAs were identified when the DE-miRNAs that were downregulated in the KD group compared with the N group were overlapped with the DE-miRNAs that were upregulated in the IVIG group compared with the KD group (Fig. 1A; Table I). These results suggested that these 65 shared DE-miRNAs may be biomarkers for the development of KD and could be reversed by IVIG. Therefore, they may also be used as biomarkers for evaluating the effectiveness of IVIG. These DE-miRNAs could clearly distinguish between the three groups, and the N and IVIG groups were clustered identically (Fig. 1B).
Figure 1.
Differentially expressed serum exosomal miRNAs identified between healthy children and patients with KD, or between patients with KD and patients with KD following IVIG therapy. (A) Venn diagrams to analyze the common miRNAs between the two comparisons. (B) Heatmap indicating the differentially expressed miRNAs to distinguish between the three groups. KD, patients with Kawasaki disease; IVIG, intravenous immunoglobulin; miR, microRNA; N, negative control healthy children.
Table I.
DE-miRNAs in serum exosomes from healthy children, patients with KD and patients with KD following IVIG therapy.
| miRNA | N vs. KD (logFC) | KD vs. IVIG (logFC) |
|---|---|---|
| hsa-miR-4695-3p | 7.14 | −6.98 |
| hsa-miR-328 | 8.23 | −8.07 |
| hsa-miR-631 | 6.78 | −6.62 |
| hsa-miR-3190-5p | 6.45 | −6.29 |
| hsa-miR-574-3p | 6.30 | −6.15 |
| hsa-miR-1260a | 7.85 | −7.69 |
| hsa-miR-3622a-3p | 6.92 | −6.76 |
| hsa-miR-197-3p | 8.40 | −8.24 |
| hsa-miR-664-3p | 6.92 | −6.76 |
| hsa-miR-3622b-3p | 6.75 | −6.60 |
| hsa-miR-3613-3p | 6.46 | −6.30 |
| hsa-miR-33b-3p | 7.05 | −6.89 |
| hsa-miR-149-5p | 6.95 | −6.80 |
| hsa-let-7d-3p | 7.41 | −7.25 |
| hsa-miR-4780 | 6.50 | −6.34 |
| hsa-miR-204-5p | 6.95 | −6.79 |
| hsa-miR-3940-3p | 7.28 | −7.12 |
| hsa-miR-1227 | 7.09 | −6.94 |
| hsa-miR-937 | 6.20 | −6.04 |
| hsa-miR-4763-5p | 7.30 | −7.15 |
| hsa-miR-4713-5p | 6.22 | −6.06 |
| hsa-let-7b-3p | 7.47 | −7.31 |
| hsa-miR-211-5p | 7.15 | −6.99 |
| hsa-miR-4730 | 7.12 | −6.96 |
| hsa-miR-885-5p | 8.16 | −8.00 |
| hsa-miR-3184-3p | 6.17 | −6.01 |
| hsa-let-7e-3p | 6.25 | −6.10 |
| hsa-miR-644b-3p | 7.33 | −7.18 |
| hsa-miR-1909-5p | 6.39 | −6.23 |
| hsa-miR-483-3p | 6.85 | −6.69 |
| hsa-miR-4436b-5p | 7.77 | −7.61 |
| hsa-miR-5681b | 6.72 | −6.56 |
| hsa-miR-4646-3p | 6.27 | −6.11 |
| hsa-miR-1910 | 6.40 | −6.24 |
| hsa-miR-299-5p | 6.69 | −6.54 |
| hsa-miR-4312 | 6.83 | −6.68 |
| hsa-miR-449b-3p | 7.45 | −7.29 |
| hsa-miR-4701-5p | 7.97 | −7.82 |
| hsa-miR-1296 | 6.91 | −6.75 |
| hsa-miR-4728-3p | 7.45 | −7.29 |
| hsa-miR-4284 | 6.55 | −6.39 |
| hsa-miR-1976 | 6.65 | −6.49 |
| hsa-miR-4697-3p | 7.00 | −6.85 |
| hsa-miR-3714 | 6.38 | −6.22 |
| hsa-miR-5010-3p | 7.03 | −6.88 |
| hsa-miR-3141 | −7.30 | 7.33 |
| hsa-miR-134 | −6.45 | 6.40 |
| hsa-miR-4800-5p | −6.19 | 6.10 |
| hsa-miR-19b-3p | −6.50 | 6.79 |
| hsa-miR-4665-3p | −6.72 | 7.79 |
| hsa-miR-483-5p | −6.70 | 6.71 |
| hsa-miR-4463 | −7.07 | 6.13 |
| hsa-miR-1234 | −6.38 | 7.60 |
| hsa-miR-2392 | −6.91 | 6.38 |
| hsa-miR-22-3p | −6.71 | 6.44 |
| hsa-miR-4689 | −6.13 | 6.19 |
| hsa-miR-575 | −7.37 | 6.50 |
| hsa-miR-3911 | −6.30 | 6.75 |
| hsa-miR-191-3p | −6.06 | 7.44 |
| hsa-miR-1246 | −7.85 | 7.04 |
| hsa-miR-4271 | −6.83 | 6.26 |
| hsa-miR-671-5p | −8.16 | 6.14 |
| hsa-miR-3610 | −6.25 | 6.16 |
| hsa-miR-3156-5p | −6.40 | 7.17 |
| hsa-miR-4499 | −6.39 | 7.07 |
These miRNAs were the shared differentially expressed miRNAs of the comparisons between N and KD, and between KD and IVIG. DE-miRNAs, differentially expressed miRNAs; N, normal; KD, Kawasaki disease; IVIG, intravenous immunoglobulin; FC, fold change; miRNA or miR, microRNA.
Target genes for DE-miRNAs
To understand how these 65 exosomal miRNAs may influence the pathogenesis of KD, their target genes were predicted using the miRWalk 2.0 database. As a result, only 1,192 potential targets for the 15 DE-miRNAs were identified and no targets were predicted for the remaining 50 DE-miRNAs.
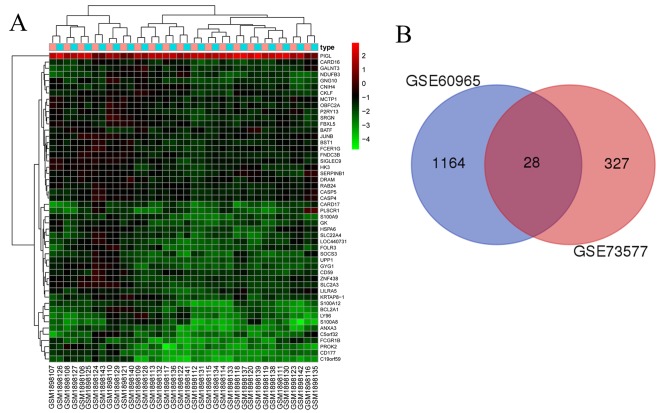
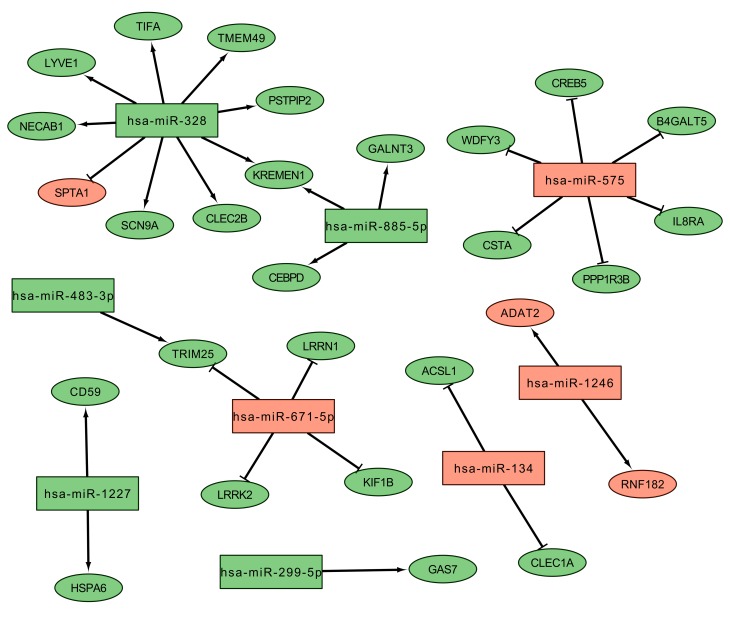
To indirectly demonstrate that the potential target genes of the identified DE-miRNAs were indeed differentially expressed in KD, and, since the present study hypothesized that exosomal DE-miRNAs in serum may serve roles in KD by regulating immune cells, the mRNA expression profiles from PBMCs of patients with KD prior to and following IVIG treatment were also investigated. As a result, 355 DEGs were screened, including 35 that were upregulated and 320 that were downregulated (Fig. 2A). Following overlapping these DEGs with the predicted target genes of the DE-miRNAs, 28 common DEGs were obtained (Fig. 2B; Table II), which constituted a network containing 30 miRNA-mRNA regulatory associations. Of these, only miR-328-spectrin α, erythrocytic 1 (SPTA1), miR-575-cyclic AMP-responsive element-binding protein 5 (CREB5)/β-1,4-galactosyltransferase 5 (B4GALT5)/WD repeat and FYVE domain-containing 3/cystatin-A/C-X-C motif chemokine receptor 1 (IL8RA)/protein phosphatase 1 regulatory subunit 3B (PPP1R3B), miR-134-acyl-CoA synthetase long chain family member 1 (ACSL1)/C-type lectin domain family 1 member A and miR-671-5p-tripartite motif containing 25/leucine rich repeat kinase 2 (LRRK2)/kinesin family member 1B/leucine rich repeat neuronal 1 were involved the negative regulation of expression (Fig. 3).
Figure 2.
DEGs in peripheral blood mononuclear cells between patients with KD prior to and following IVIG therapy. (A) Heatmap indicating the differentially expressed genes to distinguish between the KD and IVIG groups. (B) Venn diagram to analyze the overlapping genes between the differentially expressed genes and the target genes of differentially expressed microRNAs. DEGs, differentially expressed genes; KD, Kawasaki disease; IVIG, intravenous immunoglobulin.
Table II.
DEGs in peripheral blood mononuclear cells from patients with KD prior to and following intravenous immunoglobulin therapy.
| Gene | Log fold change | P-value |
|---|---|---|
| PIGL | 1.73 | 1.13×10−18 |
| CXCR3 | 1.16 | 5.66×10−18 |
| MYL5 | 1.04 | 5.64×10−17 |
| ADAT2 | 1.14 | 2.06×10−16 |
| RBM3 | 1.91 | 7.68×10−16 |
| HKDC1 | 1.03 | 1.99×10−15 |
| TARBP1 | 1.17 | 3.04×10−15 |
| LOC791120 | 1.15 | 4.04×10−15 |
| IGH | 1.19 | 2.94×10−14 |
| TK1 | 1.04 | 5.89×10−14 |
| SPTA1 | 1.09 | 3.88×10−6 |
| RNF182 | 1.42 | 6.73×10−7 |
| ANXA3 | −2.60 | 4.80×10−24 |
| UPP1 | −1.75 | 2.85×10−23 |
| RAB24 | −1.10 | 3.35×10−23 |
| CD177 | −2.52 | 3.60×10−23 |
| CARD17 | −1.99 | 1.40×10−22 |
| S100A9 | −1.87 | 1.43×10−22 |
| FCGR1B | −2.46 | 2.45×10−22 |
| C19orf59 | −2.70 | 4.38×10−22 |
| S100A12 | −2.25 | 7.53×10−22 |
| LILRA5 | −1.55 | 1.31×10−21 |
| HSPA6 | −1.50 | 4.27×10−20 |
| CD59 | −1.42 | 4.92×10−20 |
| GALNT3 | −1.38 | 9.15×10−19 |
| TMEM49 | −1.04 | 4.52×10−18 |
| PPP1R3B | −1.43 | 7.36×10−18 |
| TIFA | −1.91 | 5.18×10−17 |
| TRIM25 | −1.19 | 5.94×10−17 |
| WDFY3 | −1.33 | 2.45×10−16 |
| KIF1B | −1.37 | 2.77×10−16 |
| CREB5 | −1.24 | 1.44×10−15 |
| PSTPIP2 | −1.48 | 2.53×10−15 |
| B4GALT5 | −1.24 | 3.15×10−15 |
| GAS7 | −1.29 | 4.45×10−15 |
| ACSL1 | −1.68 | 9.49×10−15 |
| KREMEN1 | −1.53 | 1.86×10−14 |
| IL8RA | −1.07 | 1.41×10−13 |
| CLEC2B | −1.49 | 1.71×10−13 |
| LRRK2 | −1.00 | 1.99×10−13 |
| CSTA | −1.30 | 6.85×10−12 |
| SCN9A | −1.04 | 1.36×10−11 |
| CEBPD | −1.26 | 8.96×10−11 |
| CLEC1A | −1.24 | 1.17×10−7 |
| NECAB1 | −1.05 | 6.29×10−7 |
| LRRN1 | −1.28 | 9.69×10−7 |
| LYVE1 | −1.31 | 1.02×10−5 |
These genes included top 10 differentially expressed genes and 28 differentially expressed genes that overlapped with target genes of differentially expressed microRNAs. DEGs, differentially expressed genes; KD, Kawasaki disease.
Figure 3.
The regulatory associations between DE-miRNAs and DEGs. miR, microRNA; DE-miRNAs, differentially expressed miRNAs; DEGs, differentially expressed genes; red, upregulated; green, downregulated; arrowhead, similar expression trend between miRNAs and target genes; vertical line, opposite expression trend between miRNAs and target genes.
Functional enrichment analysis
The target genes of exosomal DE-miRNAs were subjected to analysis by DAVID for a functional enrichment analysis. The results indicated that 79 significant GO-biological process (BP) terms were enriched, including GO:0045893, positive regulation of transcription, DNA-templated (including CREB5); GO:0043406, positive regulation of MAP kinase activity (including LRRK2); and GO:0005975, carbohydrate metabolic process (including B4GALT5; Table III). A total of seven significant KEGG pathways were also enriched with target genes of exosomal DE-miRNAs, including hsa04390: Hippo signaling pathway (including WNT4, WNT8B); hsa05161: Hepatitis B (including CREB5); hsa04931: Insulin resistance (including CREB5 and PPP1R3B); and hsa04151: PI3K-Akt signaling pathway (including CREB5; Table IV).
Table III.
GO enrichment analysis for target genes of DE-miRNAs in exosomes of serum from healthy children, patients with KD and patients with KD patients following IVIG therapy.
| A, Target genes of DE-miRNAs | ||
|---|---|---|
| Term | P-value | Genes |
| GO:0045893, positive regulation of transcription, DNA-templated | 1.39×10−5 | PPARD, GDF2, MITF, ZXDC, TGFB3, NFKB1, CTCF, GLI3, LGR4, ZIC3, WNT4, RRN3, ZNF281, TBL1XR1, EGR2, FOXJ2, SOX11, MED14, RB1, ESR2, MED13, SIX4, HIPK2, MAPK3, ZNF711, TFAP2B, ERBB4, HOXA11, SOX2, EHF, CDH1, NFYA, TFAM, NR1D2, NPAT, CREBL2, KLF6, IL5, TRIP4, TBX3, SMAD4, IGF1, MSTN, CREB5, ATMIN, FZD4, RLF, YWHAH, SFRP1, SP1, SETD7, NEUROD1, TP53INP2, F2R |
| GO:0045944, positive regulation of transcription from RNA polymerase II promoter | 1.05×10−3 | CCNT2, HLF, GDF2, RNASEL, E2F8, STAT5B, MITF, EDN1, ARID4B,TGFB3, CTCF, NFKB1, GLI3, ZIC3, ZBTB38, CRX, PGR, PCGF5, ZNF304, SERPINE1, OGT, FGF1, TBL1XR1, SATB2, EXOSC9, EGR2, FOXJ2, SOX11, MTA2, RXRA, MED14, RB1, SIX4, MED13, CD40, GRHL2, GTF2H1, ACVR2A, VEGFA, MAPK3, HIPK2, TFAP2B, TFAP2C, CRTC3, FGFR2, SOX2, ONECUT2, TAF9B, EHF, EGLN1, CDC73, NR2C2, ATF1, TFAM, CHD7, NIPBL, DDX3X, PKD2, MYF6, IKZF4, IKZF1, CEBPD, SMAD4, IGF1, EN2, CSRP3, TET1, PARK7, DDX58, RLF, ATRX, SP1, TRPS1, NEUROD1, IRF2, NHLH2, PBX3, PBX2, FOXI1 |
| GO:0043200, response to amino acid | 1.36×10−3 | ICAM1, SLC1A2, GLRB, MTHFR, CDKN1B, GLRA3, EDN1, CDO1 |
| GO:0043406, positive regulation of MAP kinase activity | 1.49×10−3 | RASGRP1, EDN1, VEGFA, PDE5A, ADRA2A, KITLG, PDGFC, KIT, CD40, FGF1, LRRK2 |
| GO:0043268, positive regulation of potassium ion transport | 1.57×10−3 | DRD1, KIF5B, ADRA2A, STK39, DLG1 |
| GO:0051091, positive regulation of sequence-specific DNA binding transcription factor activity | 2.15×10−3 | IL5, EDN1, TRIM27, TRIM14, TRIM25, ESR2, KIT, FZD4, TRIM21, PARK7, DDX58, TRIM32, HIPK2, NEUROD1, NHLH2 |
| GO:0019228, neuronal action potential | 3.97×10−3 | DRD1, SCN1A, SCN3A, GRIK2, ANK3, KCNA1, SCN9A |
| GO:0014066, regulation of phosphatidylinositol 3-kinase signaling | 4.01×10−3 | FGFR2, C3ORF58, EREG, ERBB4, ERBB3, RASGRP1, MAPK3, KITLG, KIT, FGF1, PIP4K2A, PIP4K2C |
| GO:0050890, cognition | 5.41×10−3 | MAGT1, CHD7, NIPBL, PTCHD1, NF1, CHRNA4, CHRNB2, CHMP2B |
| GO:0007265, Ras protein signal transduction | 5.42×10−3 | ZNF304, PLD1, PLCE1, RASGRP1, NF1, ADRA2A, IGF1, RB1, SHC3, KSR1, PARK7 |
| GO:0014070, response to organic cyclic compound | 5.50×10−3 | ICAM1, CD83, ACSL1, SFRP1, TRPA1, ABCC4, ABCD3, COMT, ATF1 |
| GO:0047496, vesicle transport along microtubule | 6.24×10−3 | DYNC1I1, NDEL1, KIF5B, HTT, RASGRP1 |
| GO:0010842, retina layer formation | 6.48×10−3 | PROM1, HIPK2, FJX1, TFAP2B, CALB1, DSCAM |
| GO:0061024, membrane organization | 7.89×10−3 | YWHAH, RAB14, YWHAB, TBC1D4, PMP2, RAB10, YWHAE |
| GO:0008585, female gonad development | 8.14×10−3 | WNT4, COL9A3, SFRP1, ZFP42, TIPARP |
| GO:0060021, palate development | 9.66×10−3 | WFIKKN2, ACVR2B, SATB2, CHD7, TBX3, TIPARP, TGFB3, SMAD4, COL2A1, C5ORF42, GLI3 |
| GO:0090073, positive regulation of protein homodimerization activity | 1.14×10−2 | CRBN, TIRAP, PARK7, TRAF4 |
| GO:0048565, digestive tract development | 1.22×10−2 | FGFR2, TRPS1, TGFB3, PDGFC, RB1, KIT, LGR4 |
| GO:0007059, chromosome segregation | 1.32×10−2 | CIAO1, NDEL1, DDX3X, PPP1R7, SLC25A5, USP9X, NEK9, CTCF, SRPK1, MIS12 |
| GO:0042552, myelination | 1.34×10−2 | EGR2, TSPAN2, MAL2, ATRN, CMTM8, XK, QKI, ACSBG1 |
| GO:0001764, neuron migration | 1.44×10−2 | SATB2, TUBB2B, USP9X, CELSR1, PCM1, YWHAE, SEMA6A, NDEL1, NAV1, CCR4, NEUROD4, DCX, MYH10 |
| GO:0043154, negative regulation of cysteine-type endopeptidase activity involved in apoptotic process | 1.45×10−2 | ARL6IP1, LAMP3, DDX3X, TNFAIP8, VEGFA, TFAP2B, USP47, RAG1, BIRC5, YWHAE |
| GO:0035136, forelimb morphogenesis | 1.56×10−2 | NIPBL, TBX3, RNF165, TFAP2B |
| GO:0007156, homophilic cell adhesion via plasma membrane adhesion molecules | 1.59×10−2 | PCDHA6, ME2, PCDHA2, CLSTN2, CADM2, PCDH9, CDH1, PTPRT, CELSR1, CDH2, IGSF9B, PCDHAC2, PCDHAC1, CDH9, PCDHA10, ROBO2, DSCAM |
| GO:0043372, positive regulation of CD4-positive, alpha-beta T cell differentiation | 1.74×10−2 | CD83, TNFSF4, SASH3 |
| GO:0010951, negative regulation of endopeptidase activity | 1.80×10−2 | WFIKKN2, C5, CD109, PAPLN, FURIN, A2ML1, WFDC8, SERPINE2, SERPINE1, TFPI, PEBP1, ITIH5, CSTA, CRIM1 |
| GO:0005975, carbohydrate metabolic process | 1.83×10−2 | GALNT3, GANAB, FUT9, GNPDA2, ST8SIA1, GPD1L, MAN2A2, PGM2, PGM3, GANC, ALDH1B1, SLC2A2, AKR1B1, ST8SIA5, FUT4, SPAM1, B4GALT5, PYGB |
| GO:0040007, growth | 1.83×10−2 | OPA3, BMP3, GDF2, VEGFA, BMP8B, FOXP2 |
| GO:0006513, protein monoubiquitination | 1.83×10−2 | TSG101, DTL, KLHL12, RAD18, TRIM25, TRIM21 |
| GO:0001894, tissue homeostasis | 1.93×10−2 | AKR1B1, TRIM32, COL2A1, RB1, TP53INP2 |
| GO:0048745, smooth muscle tissue development | 2.06×10−2 | NF1, TIPARP, DLG1, FOXP2 |
| GO:0046622, positive regulation of organ growth | 2.06×10−2 | ARX, IL7, RAG2, SASH3 |
| GO:0061045, negative regulation of wound healing | 2.06×10−2 | WNT4, HMGCR, SERPINE1, CD109 |
| GO:0007519, skeletal muscle tissue development | 2.28×10−2 | MYF6, CCNT2, CFL2, NF1, SIX4, FLNB, CSRP3, FOXP2 |
| GO:0048839, inner ear development | 2.56×10−2 | CDKN1B, CXCL14, CEBPD, DUOX2, SOX2, TGFB3, NEUROD1 |
| GO:0031954, positive regulation of protein autophosphorylation | 2.73×10−2 | RAP2B, VEGFA, PDGFC, RAD50, CALM2 |
| GO:0097150, neuronal stem cell population maintenance | 2.73×10−2 | SOX2, CDH2, PCM1, HOOK3, MMP24 |
| GO:0033157, regulation of intracellular protein transport | 2.80×10−2 | NDEL1, SH3TC2, LCP1 |
| GO:0021631, optic nerve morphogenesis | 2.80×10−2 | CHRNB2, GLI3, EPHB1 |
| GO:0048511, rhythmic process | 3.03×10−2 | HLF, SP1, NR1D2, SFPQ, PASD1, PRKAA2, NFYA, FBXL3 |
| GO:0070911, global genome nucleotide-excision repair | 3.13×10−2 | SUMO3, UBE2N, DDB2, ERCC4, USP45, GTF2H1 |
| GO:0098609, cell-cell adhesion | 3.13×10−2 | ZC3HAV1, KIF5B, CKAP5, RPL15, YWHAB, TRIM25, ARFIP1, FLNB, YWHAE, PARK7, MMP24, CHMP2B, EIF4G2, GAPVD1, DDX3X, FNBP1L, SERBP1, TMOD3, PCMT1, DNAJB1, MAPRE1, RAB10, UBAP2, AHNAK |
| GO:0039702, viral budding via host ESCRT complex | 3.20×10−2 | CHMP1A, TSG101, CHMP6, VPS37C, CHMP2B |
| GO:0060078, regulation of postsynaptic membrane potential | 3.20×10−2 | SCN1A, SCN3A, PKD2, SCN9A, SCN4B |
| GO:0006366, transcription from RNA polymerase II promoter | 3.28×10−2 | CCNT2, NCBP2, HLF, POLR2E, STAT5B, TAF9B, MITF, SOX2, ONECUT2, NFKB1, EHF, CTCF, NFYA, GLI3, ATF1, ZIC3, CRX, TFAM, MAX, DDX21, VEZF1, MYF6, ZNF831, EGR2, FOXJ2, CEBPD, SOX11, SNAPC3, SMAD4, CREB5, SIX4, GRHL2, GTF2H1, TRPS1, TFAP2B, IRF2, NEUROD1, TFAP2C, PBX3, FOXI1 |
| GO:0006044, N-acetylglucosamine metabolic process | 3.29×10−2 | CHST7, GNPDA2, GNPNAT1, MGEA5 |
| GO:0060134, prepulse inhibition | 3.29×10−2 | DRD1, SLC6A3, NRXN1, CTNNA2 |
| GO:0032897, negative regulation of viral transcription | 3.29×10−2 | TRIM32, TRIM14, TRIM27, TRIM21 |
| GO:0007399, nervous system development | 3.30×10−2 | PCDHA6, GLRB, FUT9, MOBP, PCDHA2, ERBB4, CAMK2G, ARID1B, IGSF9B, GAS7, NR2C2, PCDHAC2, PCDHAC1, SEMA6A, ATXN3, NDEL1, TPP1, VEGFA, MSI1, PCDHA10, DCX, CRIM1, DLG1, WNT8B, DSCAM |
| GO:0045892, negative regulation of transcription, DNA-templated | 3.46×10−2 | PPARD, GCLC, TSG101, CTCF, GLI3, LGR4, ZBTB38, WNT4, ZNF227, NIPBL, NR1D2, GATAD2A, ZNF425, PASD1, CRY1, BAHD1, MYF6, ZNF281, IKZF4, TNFSF4, TBX3, IKZF1, CEBPD, YWHAB, SMAD4, BIRC5, RB1, SIX4, FOXP2, CHMP1A, CDKN1B, SFRP1, TRIM33, EREG, SFPQ, RBAK, USP47, TFAP2B, XCL1 |
| GO:0015758, glucose transport | 3.52×10−2 | PPARD, SLC2A10, SLC2A2, EDN1, SLC2A1, HK2 |
| GO:0051402, neuron apoptotic process | 3.52×10−2 | MAX, USP53, GRIK2, ERBB3, RB1, NLRP1 |
| GO:0006914, autophagy | 3.58×10−2 | TSG101, CHMP6, VPS41, VPS37C, PARK7, VTI1A, CHMP2B, TBC1D25, ATG5, FNBP1L, RB1CC1, ATG4A, LRRK2, VPS39 |
| GO:0050680, negative regulation of epithelial cell proliferation | 3.60×10−2 | FGFR2, PPARD, EREG, SFRP1, SOX2, CDC73, RB1, DLG1 |
| GO:0006479, protein methylation | 3.70×10−2 | PCMTD2, BHMT, PCMT1, ETF1, N6AMT1 |
| GO:0045662, negative regulation of myoblast differentiation | 3.70×10−2 | PPARD, TBX3, CXCL14, MSTN, CSRP3 |
| GO:0046854, phosphatidylinositol phosphorylation | 3.75×10−2 | FGFR2, EREG, ERBB4, ERBB3, PI4K2A, KITLG, PI4K2B, KIT, FGF1, PIP4K2A, PIP4K2C |
| GO:0045787, positive regulation of cell cycle | 3.94×10−2 | FGFR2, ANKRD17, CDKN1B, TBX3, TRIM32, TRIM21 |
| GO:0007585, respiratory gaseous exchange | 3.94×10−2 | HNMT, TMPRSS11D, EDN1, CHRNA4, PBX3, TRAF4 |
| GO:0006813, potassium ion transport | 3.96×10−2 | KCNS3, KCNMA1, KCNS1, CDKN1B, SLC12A2, ATP4B, SLC24A3, KCNA1, KCNA6, KCNJ12 |
| GO:0051260, protein homooligomerization | 4.03×10−2 | CCDC88C, GLRA3, KCNA1, PRND, KCNA6, KCNA7, KCNS3, ANXA6, STOM, KCNS1, CLDN1, KCTD16, ZBTB1, SLC1A1, EHD3, SPAST, KCTD12 |
| GO:0034454, microtubule anchoring at centrosome | 4.05×10−2 | KIF3A, PCM1, HOOK3 |
| GO:0035020, regulation of Rac protein signal transduction | 4.05×10−2 | SSX2IP, OGT, CRK |
| GO:0010606, positive regulation of cytoplasmic mRNA processing body assembly | 4.05×10−2 | CNOT6L, CNOT2, CNOT6 |
| GO:0010960, magnesium ion homeostasis | 4.05×10−2 | ANK3, KCNA1, TFAP2B |
| GO:0071910, determination of liver left/right asymmetry | 4.05×10−2 | PKD2, CCDC39, ZIC3 |
| GO:0045165, cell fate commitment | 4.22×10−2 | FGFR2, WNT4, ERBB4, TRPS1, ONECUT2, NEUROD4, WNT8B |
| GO:0071456, cellular response to hypoxia | 4.24 ×10−2 | ICAM1, PPARD, PTGIS, TBL2, STC2, CPEB2, SFRP1, EDN1, VEGFA, BNIP3L, HIPK2 |
| GO:0032456, endocytic recycling | 4.25×10−2 | STX6, VPS52, RAB14, ARL4C, EHD3 |
| GO:0030307, positive regulation of cell growth | 4.52×10−2 | EIF4G2, EXTL3, EXOSC9, DDX3X, SFRP1, TRIM32, TAF9B, USP47, H3F3B, N6AMT1 |
| GO:0042384, cilium assembly | 4.54×10−2 | KIF3A, DZIP1, ONECUT2, PCM1, C5ORF42, ACTR2, TTC30A, FNBP1L, C10ORF90, ABCC4, SSX2IP, EXOC5, EHD3 |
| GO:0009636, response to toxic substance | 4.81×10−2 | GLYAT, MAPK3, SLC30A4, SLC6A14, SCN9A, CDH1, GUCY2C, HTR1D, NQO1, PON3 |
| GO:2000679, positive regulation of transcription regulatory region DNA binding | 4.82×10−2 | NEUROD1, IGF1, RB1, PARK7 |
| GO:0022408, negative regulation of cell-cell adhesion | 4.82×10−2 | NF2, TNR, EPB41L5, CDH1 |
| GO:0007076, mitotic chromosome condensation | 4.82×10−2 | CHMP1A, NCAPH, NCAPG, CDCA5 |
| GO:0006351, transcription, DNA-templated | 4.96×10−2 | IL16, ZNF451, ZXDC, CNOT2, ZNF250, MED22, CNOT6, ZNF254, PGR, ZNF304, EPC2, MIER3, ZNF445, CRY1, SAMD4B, ZNF449, IKBKAP, SATB2, RXRA, ARID1B, TRIM33, MAPK3, TGIF2, VGLL3, CRTC3, ERBB4, HOXA11, NR2C2, ARX, ZNF227, DDX3X, CNOT6L, ZNF697, ZNF425, ZNF124, CREBL2, IKZF4, KLF6, TRIP4, IKZF1, RFX5, SMAD4, ZNF521, ZNF320, ZNF585A, ZNF627, CSRP3, TET1, FOXP2, ZNF419, ZNF417, PNRC1, JAZF1, ZNF318, PHF6, CCNT2, PPARD, ZNF518B, ZNF81, ARID4B, ZFP42, E2F8, ZNF10, ZBTB38, PCGF5, HIF1AN, BRD9, ZNF281, NFKBIZ, TBL1XR1, ZNF33A, EGR2, ZNF354A, ZNF354C, ZFY, ZFX, SF1, RB1, ESR2, ZBTB26, PURB, GTF2H1, CHMP1A, BRWD1, HIPK2, ZNF711, ZNF480, LIN54, ZNF740, POLR2E, LIN9, SCML2, ZNF660, CHD7, ZSCAN22, NR1D2, RB1CC1, NPAT, GATAD2A, PRKAA2, ZNF470, BAHD1, ZNF267, TBX3, PPHLN1, CEBPD, NLK, ZNF770, ZFP1, ZNF667, TRIM27, BIRC5, ATMIN, ZNF665, RLF, ATRX, ATXN3, SFPQ, RBAK, ZBTB5, NHLH2, ZNF461, SETD7, NEUROD4, PBX2, ZNF766, TP53INP2 |
| GO:0048661, positive regulation of smooth muscle cell proliferation | 4.96×10−2 | FGFR2, EREG, HMGCR, EDN1, AKR1B1, IGF1, ABCC4, CALCRL |
| GO:0045669, positive regulation of osteoblast differentiation | 4.96×10−2 | ACVR2A, WNT4, ACVR2B, GDF2, CEBPD, SOX11, IGF1, GLI3 |
| GO:0000122, negative regulation of transcription from RNA polymerase II promoter | 4.99×10−2 | PPARD, IMPACT, E2F8, EDN1, MITF, CNOT2, NFKB1, CTCF, HSBP1, ZNF254, GLI3, CRY1, DLG1, ZNF281, TBL1XR1, SATB2, SOX11, MTA2, RXRA, HNRNPA2B1, RB1, ESR2, PURB, ACVR2B, TRIM33, VEGFA, HIPK2, TFAP2B, TGIF2, TFAP2C, FGFR2, USP9X, TAF9B, SOX2, CDC73, ARX, NIPBL, GATAD2A, IKZF1, TBX3, RFX5, PTPN2, SMAD4, TRIM27, FOXP2, DLX1, DKK1, SFPQ, TRPS1, JAZF1, IRF2, ZBTB1 |
| B, DEGs regulated by DE-miRNAs | ||
| Term | P-value | Genes |
| GO:0060828, regulation of canonical Wnt signaling pathway | 2.82×10−2 | KREMEN1, LRRK2 |
DE-miRNAs, differentially expressed miRNAs; miRNA, microRNA; GO, Gene Ontology; KD, Kawasaki disease; IVIG, intravenous immunoglobulin; DEGs, differentially expressed genes.
Table IV.
KEGG pathway enrichment analysis for target genes of differentially expressed miRNAs in exosomes of serum from healthy children, patients with KD and patients with KD following IVIG therapy.
| A, Target genes of differentially expressed miRNAs | ||
|---|---|---|
| Term | P-value | Genes |
| hsa04390: Hippo signaling pathway | 6.54×10−4 | NF2, SOX2, YWHAB, TGFB3, SMAD4, TEAD1, CDH1, BIRC5, YWHAE, FZD4, CTNNA2, WNT4, YWHAH, RASSF6, CCND3, SERPINE1, AXIN2, FGF1, BMP8B, WNT8B, DLG1 |
| hsa05200: Pathways in cancer | 2.19×10−3 | FGFR2, ADCY1, PPARD, STAT5B, MITF, TGFB3, KITLG, NFKB1, EGLN1, CDH1, KIT, GLI3, CUL2, MAX, WNT4, RASGRP1, SLC2A1, GNG2, AXIN2, FGF1, TRAF4, WNT8B, COL4A4, PTGER3, RXRA, SMAD4, IGF1, BIRC5, RB1, FZD4, CTNNA2, CCDC6, LAMA4, CDKN1B, MAPK3, VEGFA, LAMC2, CRK, F2R |
| hsa05161: Hepatitis B | 2.70×10−2 | EGR2, STAT5B, YWHAB, TGFB3, TIRAP, SMAD4, BIRC5, CREB5, NFKB1, RB1, DDX58, CDKN1B, DDX3X, MAPK3, TICAM2, DDB2 |
| hsa04931: Insulin resistance | 2.79×10−2 | PRKAB2, CREB5, NFKB1, PRKCQ, PPP1R3B, SLC2A2, SLC2A1, MGEA5, TBC1D4, GYS2, OGT, PRKAA2, PYGB |
| hsa04066: HIF-1 signaling pathway | 3.23×10−2 | CUL2, CDKN1B, CAMK2G, MAPK3, EDN1, VEGFA, SLC2A1, SERPINE1, HK2, IGF1, NFKB1, EGLN1 |
| hsa04151: PI3K-Akt signaling pathway | 4.10×10−2 | FGFR2, PPP2R5A, KITLG, NFKB1, COL2A1, KIT, COL6A6, TNR, GYS2, PDGFC, GNG2, PRKAA2, FGF1, THBS2, COL4A4, SGK2, IL7, RXRA, YWHAB, IGF1, CREB5, YWHAE, LAMA4, CDKN1B, YWHAH, CCND3, VEGFA, MAPK3, LAMC2, F2R |
| hsa00500: Starch and sucrose metabolism | 4.51×10−2 | PGM2, GANC, HK2, GYS2, PYGB, PGM2L1 |
| B, Differentially expressed genes regulated by differentially expressed miRNAs | ||
| Term | P-value | Genes |
| hsa00512: Mucin type O-Glycan biosynthesis | 2.82×10−2 | KREMEN1, LRRK2 |
KEGG, Kyoto Encyclopedia of Genes and Genomes; GO, Gene Ontology; KD, Kawasaki disease; IVIG, intravenous immunoglobulin. 1, for all target genes of differentially expressed miRNAs; 2, for differentially expressed genes regulated by differentially expressed miRNAs.
The target genes of DE-miRNAs that overlapped with DEGs were also subjected to analysis by DAVID for functional prediction. Only one significant GO-BP term (GO:0060828, regulation of canonical Wnt signaling pathway, including LRRK2; Table III) and KEGG pathway (hsa00512: Mucin type O-Glycan biosynthesis, including B4GALT5; Table IV) were enriched.
Discussion
The present study demonstrated that exosomal miR-328, miR-575, miR-134 and miR-671-5p in serum may be used as biomarkers for the diagnosis of KD and for the prediction of therapeutic outcomes of the IVIG therapy. miR-328 was upregulated, and miR-575, miR-134 and miR-671-5p were downregulated in patients with KD. These trends were reversed following IVIG treatment, leading to downregulation of miR-328, and upregulation of miR-575, miR-134 and miR-671-5p. The present study identified novel exosomal miRNAs (miR-575 and miR-134), in addition to those reported in the study by Jia et al (27) (miR-328 and miR-671-5p).
There have been a few studies that have investigated the miRNAs in KD prior to and following IVIG therapy (22,40,41). However, the roles of miR-328, miR-575, miR-134 and miR-671-5p remain unclear. Previous studies have suggested that some of these miRNAs are predictors for coronary artery diseases (42,43). He et al (42) demonstrated that elevated plasma miR-328 levels could distinguish between patients with acute myocardial infarction (AMI) and the control group, with an AUC of 0.887. Wang et al (43) also reported good diagnostic performance of miR-328 in plasma (AUC=0.810) and in whole blood (AUC=0.872) for patients with AMI. These results suggested that the miRNAs selected in the present study may identify the presence of cardiovascular lesions in KD. Although previous evidence indicated that miR-134 may serve a diagnostic role in AMI, this result was not consistent with the results of the present study (miR-134 was previously upregulated in AMI, but was downregulated in the present study) (42,44). This difference may be attributed to the difference in the miRNA spectrum between the plasma and serum (45), or between the whole serum and the exosomal fraction. Therefore, further clinical studies are needed to confirm the diagnostic value of the exosomal miRNAs identified in the present study.
The present study also predicted that the selected miRNAs may be involved in KD by regulating the inflammatory target genes expressed in PBMCs. CXCR1 was one of the targets and previous studies have reported that IL-8 and its receptors, CXCR1 and C-X-C chemokine receptor type 2, were upregulated in patients with KD (46) and in coronary artery diseases (47). By binding to CXCR1, IL-8 may promote the production of other inflammatory mediators through the activation of the p38-mitogen-activated protein kinase/extracellular signal-regulated kinase-nuclear factor (NF)-κB pathways (48), which may subsequently induce apoptosis in vascular endothelial cells, a potential mechanism for KD (49). In addition, transcription factor CREB was also reported to enhance inflammation by inducing IL-17A production and promoting coronary artery diseases, including atherosclerosis (50). B4GALT family genes encode enzymes for the biosynthesis of different glycoconjugates and saccharide structures and are involved in protein glycosylation (51). Lactosylceramide synthesized by B4GALT6 in astrocytes activated central nervous system (CNS)-infiltrating monocytes, in a non-cell-autonomous manner, by regulating granulocyte-macrophage colony-stimulating factor, resulting in chronic CNS inflammation (52). PPP1R3B is a gene encoding the hepatic glycogen-targeting subunit of protein phosphatase-1 (PP1), which targets PP1 to glycogen synthase, increasing the activity of this enzyme in the skeletal muscles and liver (53). It has been previously demonstrated that increased glycogen accumulation is associated with obesity-linked inflammation in humans (54). LRRK2 deficiency was reported to attenuate the lipopolysaccharide-induced expression of inducible nitric oxide synthase, TNF-α, IL-1β and IL-6 through inhibition of the p38 mitogen-activated protein kinase, and NF-κB pathways, and to alter neuroinflammation (55). ACSL1 enzyme catalyzes the thioesterification of fatty acids and is a marker of inflammatory activation. It has been reported that the inflammatory phenotype of diabetic mice is associated with the increased expression of ACSL1 (56). Myeloid-selective deletion of ACSL1 protects monocytes and macrophages from the inflammatory effects of diabetes and prevents accelerated atherosclerosis (56). Heterozygous loss of spectrin in mice lead to increased expression levels of IL-1α and IL-1β through the activation of signal transducer and activator of transcription 3 (57). Accordingly, the present study hypothesized that miR-328 may exhibit pro-inflammatory effects through the downregulation of SPTA1, and miR-575, miR-134 and miR-671-5p may exhibit anti-inflammatory effects, leading to the upregulation of CREB5, IL8RA, PPP1R3B, ACSL1 and LRRK2 in KD.
There are certain limitations that should be acknowledged when interpreting the results of the present study. Firstly, the sample size for screening exosomal miRNAs for KD was not large, and an increased number of samples should be analyzed in future studies. Secondly, although several exosomal miRNAs have been suggested as potential biomarkers for the diagnosis of KD and the prediction of therapeutic outcomes for IVIG therapy, further confirmation in clinical samples is necessary. Thirdly, negative associations between miRNAs and their target genes were revealed in the present study, however, in vitro and in vivo experiments are necessary to validate these results. Fourthly, the exosomal mechanisms of these four miRNAs remain to be elucidated.
In conclusion, the present study preliminarily revealed that exosomal miR-328, miR-575, miR-134 and miR-671-5p may serve as biomarkers for the diagnosis of KD and the prediction of therapeutic outcomes for IVIG therapy by influencing the expression levels of inflammatory genes.
Acknowledgments
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the NCBI database repository (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE60965; http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE73577).
Authors' contributions
XFZ and DJS participated in the design of this study. XFZ and GDX performed the bioinformatics analyses. XFZ, GDX and DJS contributed to the acquisition and interpretation of data. XFZ and DJS were involved in drafting and revising the manuscript. All authors read and approved the final manuscript.
Ethical approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Makino N, Nakamura Y, Yashiro M, Ae R, Tsuboi S, Aoyaa Y, Kojo T, Uehara R, Kotani K, Yanagawa H. Descriptive epidemiology of Kawasaki disease in Japan, 2011–2012: From the results of the 22nd nationwide survey. J Epidemiol. 2015;25:239–245. doi: 10.2188/jea.JE20140089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim GB, Han JW, Park YW, Song MS, Hong YM, Cha SH, Kim DS, Park S. Epidemiologic features of Kawasaki disease in South Korea: Data from nationwide survey, 2009–2011. Pediatr Infect Dis J. 2014;33:24–27. doi: 10.1097/INF.0000000000000010. [DOI] [PubMed] [Google Scholar]
- 3.Lue HC, Chen LR, Lin MT, Chang LY, Wang JK, Lee CY, Wu MH. Epidemiological features of Kawasaki disease in Taiwan, 1976–2007: Results of five nationwide questionnaire hospital surveys. Pediatr Neonatol. 2014;55:92–96. doi: 10.1016/j.pedneo.2013.07.010. [DOI] [PubMed] [Google Scholar]
- 4.Chen JJ, Ma XJ, Liu F, Yan WL, Huang MR, Huang M, Huang GY. Shanghai Kawasaki Disease Research Group: Epidemiologic features of Kawasaki disease in shanghai from 2008 through 2012. Pediatr Infect Dis J. 2016;35:7–12. doi: 10.1097/INF.0000000000000914. [DOI] [PubMed] [Google Scholar]
- 5.Hartopo AB, Setianto BY. Coronary artery sequel of Kawasaki disease in adulthood, a concern for internists and cardiologists. Acta Med Indones. 2013;45:69–75. [PubMed] [Google Scholar]
- 6.Nakamura Y, Aso E, Yashiro M, Tsuboi S, Kojo T, Aoyama Y, Kotani K, Uehara R, Yanagawa H. Mortality among Japanese with a history of Kawasaki disease: Results at the end of 2009. J Epidemiol. 2013;23:429–434. doi: 10.2188/jea.JE20130048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fukazawa R, Kobayashi T, Mikami M, Saji T, Hamaoka K, Kato H, Suzuki H, Tsuda E, Ayusawa M, Miura M, et al. Nationwide survey of patients with giant coronary aneurysm secondary to Kawasaki disease 1999–2010 in Japan. Circ J. 2017;82:239–246. doi: 10.1253/circj.CJ-17-0433. [DOI] [PubMed] [Google Scholar]
- 8.Shulman ST. Intravenous immunoglobulin for the treatment of Kawasaki disease. Pediatr Ann. 2017;46:e25–e28. doi: 10.3928/19382359-20161212-01. [DOI] [PubMed] [Google Scholar]
- 9.Yoshida M, Oana S, Masuda H, Ishiguro A, Kato H, Ito S, Kobayashi T, Abe J. Recurrence of fever after initial intravenous immunoglobulin treatment in children with Kawasaki disease. Clin Pediatr (Phila) 2018;57:189–192. doi: 10.1177/0009922817694459. [DOI] [PubMed] [Google Scholar]
- 10.Rigante D, Valentini P, Rizzo D, Leo A, De Rosa G, Onesimo R, De Nisco A, Angelone DF, Compagnone A, Delogu AB. Responsiveness to intravenous immunoglobulins and occurrence of coronary artery abnormalities in a single-center cohort of Italian patients with Kawasaki syndrome. Rheumatol Int. 2010;30:841–846. doi: 10.1007/s00296-009-1337-1. [DOI] [PubMed] [Google Scholar]
- 11.Pinna GS, Kafetzis DA, Tselkas OI, Skevaki CL. Kawasaki disease: An overview. Curr Opin Infect Dis. 2008;21:263–270. doi: 10.1097/QCO.0b013e3282fbf9cd. [DOI] [PubMed] [Google Scholar]
- 12.Motoki N, Akazawa Y, Yamazaki S, Hachiya A, Motoki H, Matsuzaki S, Koike K. Prognostic significance of QT interval dispersion in the response to intravenous immunoglobulin therapy in Kawasaki disease. Circ J. 2017;81:537–542. doi: 10.1253/circj.CJ-16-0864. [DOI] [PubMed] [Google Scholar]
- 13.Komatsu H, Tateno A. Failure to distinguish systemic-onset juvenile idiopathic arthritis from incomplete Kawasaki disease in an infant. J Paediatr Child Health. 2007;43:707–709. doi: 10.1111/j.1440-1754.2007.01189.x. [DOI] [PubMed] [Google Scholar]
- 14.Capittini C, Emmi G, Mannarino S, Bossi G, Dellepiane RM, Salice P, Pietrogrande MC, Pasi A, De Silvestri A, Tinelli C, Martinetti M. An immune-molecular hypothesis supporting infectious aetiopathogenesis of Kawasaki disease in children. Eur J Immunol. 2018;48:543–545. doi: 10.1002/eji.201747226. [DOI] [PubMed] [Google Scholar]
- 15.Hara T, Nakashima Y, Sakai Y, Nishio H, Motomura Y, Yamasaki S. Kawasaki disease: A matter of innate immunity. Clin Exp Immunol. 2016;186:134–143. doi: 10.1111/cei.12832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sato S, Kawashima H, Kashiwagi Y, Hoshika A. Inflammatory cytokines as predictors of resistance to intravenous immunoglobulin therapy in Kawasaki disease patients. Int J Rheum Dis. 2013;16:168–172. doi: 10.1111/1756-185X.12082. [DOI] [PubMed] [Google Scholar]
- 17.Korematsu S, Uchiyama S, Miyahara H, Nagakura T, Okazaki N, Kawano T, Kojo M, Izumi T. The characterization of cerebrospinal fluid and serum cytokines in patients with Kawasaki disease. Pediatr Infect Dis J. 2007;26:750–753. doi: 10.1097/INF.0b013e3180f61708. [DOI] [PubMed] [Google Scholar]
- 18.Rasouli M, Heidari B, Kalani M. Downregulation of Th17 cells and the related cytokines with treatment in Kawasaki disease. Immunol Lett. 2014;162:269–275. doi: 10.1016/j.imlet.2014.09.017. [DOI] [PubMed] [Google Scholar]
- 19.Engelberg R, Martin M, Wrotniak BH, Hicar MD. Observational study of Interleukin-21 (IL-21) does not distinguish Kawasaki disease from other causes of fever in children. Pediatr Rheumatol Online J. 2017;15:32. doi: 10.1186/s12969-017-0163-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu P, Jiang GM, Wu Y, Huang BY, Liu SY, Zhang DD, Xu Y, Wu YF, Xia X, Wei W, Hu B. TNF-α is superior to conventional inflammatory mediators in forecasting IVIG nonresponse and coronary arteritis in Chinese children with Kawasaki disease. Clin Chim Acta. 2017;471:76–80. doi: 10.1016/j.cca.2017.05.019. [DOI] [PubMed] [Google Scholar]
- 21.Chen X, Ba Y, Ma L, Cai X, Yin Y, Wang K, Guo J, Zhang Y, Chen J, Guo X, et al. Characterization of microRNAs in serum: A novel class of biomarkers for diagnosis of cancer and other diseases. Cell Res. 2008;18:997–1006. doi: 10.1038/cr.2008.282. [DOI] [PubMed] [Google Scholar]
- 22.Yun KW, Lee JY, Yun SW, Lim IS, Choi ES. Elevated serum level of microRNA (miRNA) −200c and miRNA-371-5p in children with Kawasaki disease. Pediatr Cardiol. 2014;35:745–752. doi: 10.1007/s00246-013-0846-6. [DOI] [PubMed] [Google Scholar]
- 23.Zhang W, Wang Y, Zeng Y, Hu L, Zou G. Serum miR-200c and miR-371-5p as the useful diagnostic biomarkers and therapeutic targets in Kawasaki disease. Biomed Res Int. 2017;2017:8257862. doi: 10.1155/2017/8257862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang S, Wang JQ, Lv XW. Exosomal miRNAs as biomarkers in the diagnosis of liver disease. Biomark Med. 2017;11:491–501. doi: 10.2217/bmm-2017-0011. [DOI] [PubMed] [Google Scholar]
- 25.Matsumura T, Sugimachi K, Iinuma H, Takahashi Y, Kurashige J, Sawada G, Ueda M, Uchi R, Ueo H, Takano Y, et al. Exosomal microRNA in serum is a novel biomarker of recurrence in human colorectal cancer. Br J Cancer. 2015;113:275–281. doi: 10.1038/bjc.2015.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tanaka Y, Kamohara H, Kinoshita K, Kurashige J, Ishimoto T, Iwatsuki M, Watanabe M, Baba H. Clinical impact of serum exosomal microRNA-21 as a clinical biomarker in human esophageal squamous cell carcinoma. Cancer. 2013;119:1159–1167. doi: 10.1002/cncr.27895. [DOI] [PubMed] [Google Scholar]
- 27.Jia HL, Liu CW, Zhang L, Xu WJ, Gao XJ, Bai J, Xu YF, Xu MG, Zhang G. Sets of serum exosomal microRNAs as candidate diagnostic biomarkers for Kawasaki disease. Sci Rep. 2017;7:44706. doi: 10.1038/srep44706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Higuchi T, Fukuda N, Yamamoto C, Yamazaki T, Oikawa O, Ohnishi Y, Okada K, Soma M, Matsumoto K. The influence of uremic serum on interleukin-1beta and interleukin-1 receptor antagonist production by peripheral blood mononuclear cells. Ther Apher Dial. 2006;10:65–71. doi: 10.1111/j.1744-9987.2006.00346.x. [DOI] [PubMed] [Google Scholar]
- 29.Clinchy B, Gunneras M, Hakansson A, Hakansson L. Production of IL-1Ra by human mononuclear blood cells in vitro: Influence of serum factors. Cytokine. 2006;34:320–330. doi: 10.1016/j.cyto.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 30.Alidjinou EK, Sané F, Engelmann I, Hober D. Serum-dependent enhancement of coxsackievirus B4-induced production of IFNα, IL-6 and TNFα by peripheral blood mononuclear cells. J Mol Biol. 2013;425:5020–5031. doi: 10.1016/j.jmb.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 31.Sandri S, Hatanaka E, Franco AG, Pedrosa AM, Monteiro HP, Campa A. Serum amyloid A induces CCL20 secretion in mononuclear cells through MAPK (p38 and ERK1/2) signaling pathways. Immunol Lett. 2008;121:22–26. doi: 10.1016/j.imlet.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 32.Harshyne LA, Nasca BJ, Kenyon LC, Andrews DW, Hooper DC. Serum exosomes and cytokines promote a T-helper cell type 2 environment in the peripheral blood of glioblastoma patients. Neuro Oncol. 2016;18:206–215. doi: 10.1093/neuonc/nov107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou X, Jiao Z, Ji J, Li S, Huang X, Lu X, Zhao H, Peng J, Chen X, Ji Q, Ji Y. Characterization of mouse serum exosomal small RNA content: The origins and their roles in modulating inflammatory response. Oncotarget. 2017;8:42712–42727. doi: 10.18632/oncotarget.17448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Okuzaki D, Ota K, Takatsuki SI, Akiyoshi Y, Naoi K, Yabuta N, Saji T, Nojima H. FCN1 (M-ficolin), which directly associates with immunoglobulin G1, is a molecular target of intravenous immunoglobulin therapy for Kawasaki disease. Sci Rep. 2017;7:11334. doi: 10.1038/s41598-017-11108-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bolstad BM. Bolstad B preprocessCore: A collection of pre-processing functions. R Package. 2013 version 1.28. 0. [Google Scholar]
- 36.Smyth GK. Bioinformatics and computational biology solutions using R and Bioconductor. Springer; 2005. Limma: Linear models for microarray data; pp. 397–420. [DOI] [Google Scholar]
- 37.Kolde R. (2015) Pheatmap: Pretty Heatmaps. R package. 2015 version 1.0. 8. [Google Scholar]
- 38.Kohl M, Wiese S, Warscheid B. Cytoscape: software for visualization and analysis of biological networks. Methods Mol Biol. 2011;696:291–303. doi: 10.1007/978-1-60761-987-1_18. [DOI] [PubMed] [Google Scholar]
- 39.Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 40.Rong X, Jia L, Hong L, Pan L, Xue X, Zhang C, Lu J, Jin Z, Qiu H, Wu R, Chu M. Serum miR-92a-3p as a new potential biomarker for diagnosis of Kawasaki disease with coronary artery lesions. J Cardiovasc Transl Res. 2017;10:1–8. doi: 10.1007/s12265-016-9717-x. [DOI] [PubMed] [Google Scholar]
- 41.Shimizu C, Kim J, Stepanowsky P, Trinh C, Lau HD, Akers JC, Chen C, Kanegaye JT, Tremoulet A, Ohno-Machado L, Burns JC. Differential Expression of miR-145 in Children with Kawasaki disease. PLoS One. 2013;8:e58159. doi: 10.1371/journal.pone.0058159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.He F, Lv P, Zhao X, Wang X, Ma X, Meng W, Meng X, Dong S. Predictive value of circulating miR-328 and miR-134 for acute myocardial infarction. Mol Cell Biochem. 2014;394:137–144. doi: 10.1007/s11010-014-2089-0. [DOI] [PubMed] [Google Scholar]
- 43.Wang R, Li N, Zhang Y, Ran Y, Pu J. Circulating microRNAs are promising novel biomarkers of acute myocardial infarction. Intern Med. 2011;50:1789–1795. doi: 10.2169/internalmedicine.50.5129. [DOI] [PubMed] [Google Scholar]
- 44.Wang KJ, Zhao X, Liu YZ, Zeng QT, Mao XB, Li SN, Zhang M, Jiang C, Zhou Y, Qian C, et al. Circulating MiR-19b-3p, MiR-134-5p and MiR-186-5p are promising novel biomarkers for early diagnosis of acute myocardial infarction. Cell Physiol Biochem. 2016;38:1015–1029. doi: 10.1159/000443053. [DOI] [PubMed] [Google Scholar]
- 45.Wang K, Yuan Y, Cho JH, Mcclarty S, Baxter D, Galas DJ. Comparing the MicroRNA spectrum between serum and plasma. PLoS One. 2012;7:e41561. doi: 10.1371/journal.pone.0041561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jiang J, Cai Y, Li Z, Huang L, Chen J, Tian L, Wu Z, Li X, Chen Z, Chen C, Yang Z. Screening of differentially expressed genes associated with Kawasaki disease by microarray analysis. Exp Ther Med. 2017;14:3159–3164. doi: 10.3892/etm.2017.4907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Leonard DA, Merhige ME, Williams BA, Greene RS. Elevated expression of the interleukin-8 receptors CXCR1 and CXCR2 in peripheral blood cells in obstructive coronary artery disease. Coron Artery Dis. 2011;22:491–496. doi: 10.1097/MCA.0b013e32834b67e2. [DOI] [PubMed] [Google Scholar]
- 48.Chan LP, Liu C, Chiang FY, Wang LF, Lee KW, Chen WT, Kuo PL, Liang CH. IL-8 promotes inflammatory mediators and stimulates activation of p38 MAPK/ERK-NF-κB pathway and reduction of JNK in HNSCC. Oncotarget. 2017;8:56375–56388. doi: 10.18632/oncotarget.16914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Li Z, Jiang J, Tian L, Li X, Chen J, Li S, Li C, Yang Z. A plasma mir-125a-5p as a novel biomarker for Kawasaki disease and induces apoptosis in HUVECs. PLoS One. 2017;12:e0175407. doi: 10.1371/journal.pone.0175407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kotla S, Singh NK, Heckle MR, Tigyi GJ, Rao GN. The transcription factor CREB enhances interleukin-17A production and inflammation in a mouse model of atherosclerosis. Sci Signal. 2013;6:ra83. doi: 10.1126/scisignal.2004214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhou H, Ma H, Wei W, Ji D, Song X, Sun J, Zhang J, Jia L. B4GALT family mediates the multidrug resistance of human leukemia cells by regulating the hedgehog pathway and the expression of p-glycoprotein and multidrug resistance-associated protein 1. Cell Death Dis. 2013;4:e654. doi: 10.1038/cddis.2013.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mayo L, Trauger SA, Blain M, Nadeau M, Patel B, Alvarez JI, Mascanfroni ID, Yeste A, Kivisäkk P, Kallas K, et al. Regulation of astrocyte activation by glycolipids drives chronic CNS inflammation. Nat Med. 2014;20:1147–1156. doi: 10.1038/nm.3681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mehta MB, Shewale SV, Sequeira RN, Millar JS, Hand NJ, Rader DJ. Hepatic protein phosphatase 1 regulatory subunit 3B (Ppp1r3b) promotes hepatic glycogen synthesis and thereby regulates fasting energy homeostasis. J Biol Chem. 2017;292:10444–10454. doi: 10.1074/jbc.M116.766329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ceperuelo-Mallafré V, Ejarque M, Serena C, Duran X, Montori-Grau M, Rodríguez MA, Yanes O, Núñez-Roa C, Roche K, Puthanveetil P, et al. Adipose tissue glycogen accumulation is associated with obesity-linked inflammation in humans. Mol Metab. 2015;5:5–18. doi: 10.1016/j.molmet.2015.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kim B, Yang MS, Choi D, Kim JH, Kim HS, Seol W, Choi S, Jou I, Kim EY, Joe EH. Impaired inflammatory responses in murine Lrrk2-knockdown brain microglia. PLoS One. 2012;7:e34693. doi: 10.1371/journal.pone.0034693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kanter JE, Kramer F, Barnhart S, Averill MM, Vivekanandan-Giri A, Vickery T, Li LO, Becker L, Yuan W, Chait A, et al. Diabetes promotes an inflammatory macrophage phenotype and atherosclerosis through acyl-CoA synthetase 1. Proc Natl Acad Sci USA. 2012;109:E715–E724. doi: 10.1073/pnas.1111600109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lin L, Wang H, Gao B, Zhi X, He AR. Abstract 5184: Mechanistic analysis of liver inflammation and cancer formation in mice with heterozygous lose of β-spectrin (β2SP) Cancer Res. 2013;73:5184–5184. doi: 10.1158/1538-7445.AM2013-5184. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are available in the NCBI database repository (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE60965; http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE73577).