Abstract
The aim of this study was to investigate the effect of montelukast on the expression of CD4+CD25+ regulatory T cells in children with acute bronchial asthma. Fifty-six child patients with acute bronchial asthma treated in the Department of Pneumology at the Shangluo Central Hospital were selected and randomly divided into the control group (n=28) and treatment group (n=28). The control group was treated with the conventional therapy of bronchial asthma, while the treatment group received montelukast on the basis of the control group for 7 days. The clinical symptoms, lung function and proportion of CD4+CD25+ regulatory T cells in peripheral T lymphocyte subsets in patients in the two groups were observed. Moreover, the levels of inflammatory factors and immunoglobulin E (IgE) in peripheral blood in both groups were detected. The effective treatment rate in the treatment group was significantly higher than that in the control group (P<0.05), and the forced expiratory volume in 1 sec/forced vital capacity (FEV1/FVC), peak expiratory flow (PEF) and 25% peak expiratory flow (PEF25) in the treatment group were significantly higher than those in the control group (P<0.05). The proportions of CD4+CD25+ regulatory T cells in the two groups after drug therapy were significantly increased. The proportion and content per unit volume of peripheral CD4+CD25+ regulatory T cells in the treatment group were obviously higher than those in the control group (P<0.01). After treatment, the levels of interleukin-4 (IL-4), IL-5 and IL-6 in peripheral blood in the two groups were significantly decreased. However, the levels of transferrin-γ (TFN-γ) and IL-10 were significantly increased (P<0.01). The IgE level in the treatment group was also significantly higher than that in the control group (P<0.01). In conclusion, montelukast can regulate the T helper 1 (Th1)/Th2 balance, increase the expression of CD4+CD25+ regulatory T cells, and improve the airway inflammation caused by acute bronchial asthma and the clinical symptoms and lung function of patients with acute bronchial asthma.
Keywords: montelukast, bronchial asthma, CD4+CD25+ regulatory T cells, inflammatory factors
Introduction
Bronchial asthma is a kind of chronic airway disease that affects patients worldwide. According to the report of the World Health Organization (WHO), the number of patients with bronchial asthma is up to 30 million in China, showing an increasing trend year by year. Bronchial asthma is mainly manifested as acute bronchial asthma that often occurs in children (1–3). The main symptoms of bronchial asthma are airway smooth muscle spasm and airway inflammatory infiltration, and its incidence is jointly affected by genetic factors and environmental factors, but its specific pathogenesis remains unclear. Studies have reported that it is closely related to the airway inflammation, allergic reaction, neurohumor and other factors (4,5). Glucocorticoid therapy is the most common therapeutic regimen for acute bronchial asthma, which has strong anti-inflammatory and immunosuppressive effects. However, the long-term application of glucocorticoid leads to obvious adverse reactions and withdrawal effect (6). In recent years, a large number of clinical reports in China and foreign countries have suggested that montelukast can be used to replace glucocorticoid in the treatment of acute bronchial asthma (7,8). Montelukast is a kind of antagonist of cysteinyl leukotriene (Cys-LT) receptor that can regulate the leukotriene pathway, which is clinically used in the acute and long-term treatment of asthma and widely applied in the treatment of asthma children currently (9). Moreover, montelukast can block the pro-inflammatory effect mediated by Cys-LT1 by binding to the Cys-LT1 receptor on target cells (10). CD4+CD25+ regulatory T cells are cells derived from thymus used to regulate the immune balance and mediate immune tolerance. It is reported that CD4+CD25+ T cells can inhibit the production of T helper 2 (Th2) cytokines and aggregation of airway eosinophils (EOS) (11). Therefore, investigations on the role of CD4+CD25+ regulatory T cells in bronchial asthma and its molecular mechanism can be a feasible research direction for the targeted therapy of bronchial asthma.
In this study, the therapeutical effect of montelukast on children with acute bronchial asthma and the regulating effect on CD4+CD25+ regulatory T cells were investigated, and its mechanism was further studied, so as to provide a theoretical basis for the application of montelukast in the treatment of acute bronchial asthma.
Materials and methods
Subjects of study
In this study, a total of 56 child patients with acute asthma aged 7–13 years treated in Pneumology Department of Shangluo Central Hospital from March 2015 to March 2016 were selected, and all patients met the diagnostic criteria in the Guidelines for Prevention and Treatment of Bronchial Asthma: i) recurrent wheezing, shortness of breath, chest tightness and cough; ii) expiratory-phase wheezing rale can be heard in asthmatic attack; iii) the above symptoms can be relieved after treatment or spontaneously. The above patients were randomly divided into the control group (n=28) and treatment group (n=28). The control group, including 17 males and 11 females with an average age of 10.25±3.82 years, was treated with conventional therapy (anti-infection combined with aminophylline therapy), while the treatment group, including 18 males and 10 females with an average age of 9.85±3.68 years, took montelukast sodium tablets (Sichuan Otsuka Pharmaceutical Co., Ltd., Sichuan, China; NMPN H20064370) orally once per day (5 mg/time) before sleep. Patients in the two groups were treated for one week. None of the patients suffered from other autoimmune diseases, lung infection and other wasting diseases, and they did not take glucocorticoid and leukotriene receptor antagonist within one month. There were no statistically significant differences in age, sex, condition and course of disease between the two groups.
Parents or their guardians signed the written informed consent. The experimental scheme was approved by the Ethics Committee of Shangluo Central Hospital (Shangluo, China) and the above patients had the complete clinical and pathological data and the complete therapeutic regimen.
Determination of lung function
The lung function of all the patients was detected by the physician in the Pneumology Department of our hospital using the lung function apparatus (Jaeger Master Diffusion; Jaeger, Hoechberg, Germany). The lung function parameters were recorded in detail: the ratio of forced expiratory volume in 1 sec to forced vital capacity (FEV1/FVC), peak expiratory flow (PEF) and 25% PEF (PEF25). The above lung function parameters were statistically analyzed by experienced physicians who were not involved in the previous experiment.
Evaluation of therapeutic effects
The treatment effects on acute bronchial asthma in the above patients were evaluated: remarkably effective (3 points): dyspnea and other symptoms were improved and wheezing rale in lung disappeared within 3 days of treatment; effective (2 points): dyspnea and other symptoms were improved and wheezing rale in lung disappeared within 7 days of treatment; ineffective (1 point): serious cough and wheezing still occurred and wheezing rale in lung still existed after 1 week of treatment.
Separation and detection of peripheral CD4+CD25+ regulatory T cells
Fasting peripheral blood (5 ml) was drawn from all the patients, added and mixed with the anticoagulant, and the mixture was labeled using CD4 and CD25 multicolor fluorescent antibodies. IgG1-fluorescein isothiocyanate (FITC) and IgG1-PE were used as negative controls. The mixture was incubated in the dark at room temperature for 10 min and detected using a FACSCalibur flow cytometer (BD Biosciences, San Jose, CA, USA). The positive rate (%) of CD4+CD25+ regulatory T cells in peripheral blood was calculated, and the absolute number of CD4+CD25+ regulatory T cells in 1 µl peripheral blood was also calculated, followed by signal acquisition and results analysis using Cellquest Pro software.
Inflammatory factor detection
The serum was separated from the peripheral blood of patients, and the concentrations of interleukin-4 (IL-4), IL-5, IL-6, transferrin-γ (TFN-γ), IL-10 and immunoglobulin E (IgE) were detected using the corresponding enzyme-linked immunosorbent assay (ELISA) kits. The standard sample was added onto an ELISA plate to prepare the standard curve. The serum sample in each group was diluted 10-fold using the sample diluent was added into each well, and the plate was sealed with sealing membrane for reaction at room temperature for 60 min. The solution was discarded, and the corresponding biotin-labeled antibody was added for reaction at 37°C for 60 min. The plate was then washed with cleaning solution 3 times (1 min/time). Avidin-peroxidase complex (100 µl) was added for reaction at 37°C for 30 min. The liquid waste was discarded, and the plate was washed again with cleaning solution and added with 100 µl stop buffer to terminate the reaction. The optical density (OD) value of each well was measured using a microplate reader and the standard curve was drawn using the software. Finally, the serum IL-4, IL-5, IL-6, TFN-γ, IL-10 and IgE levels in each group were calculated through the standard curve.
Statistical analysis
Graphpad Prism 6.0 was used for the statistical analysis of data, and data were presented as mean ± SD. The t-test was used for analysis. P<0.05 was considered to indicate a statistically significant difference.
Results
Changes in lung function
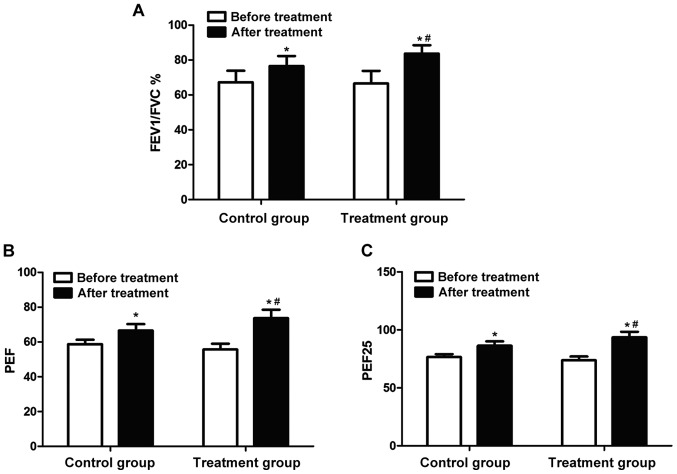
The lung function of patients in each group was detected using the lung function monitor. The results (Fig. 1) showed that there were no statistically significant differences in FEV1/FVC, PEF and PEF25 between the two groups before treatment (P>0.05). FEV1/FVC, PEF and PEF25 in both groups were significantly increased after treatment for 7 days (P<0.05); FEV1/FVC, PEF and PEF25 in the treatment group were obviously higher than those in the control group (P<0.05).
Figure 1.
Detection of lung function of patients in each group using the lung function monitor; (A) FEV1/FVC; (B) PEF; (C) PEF25. FEV1/FVC, PEF and PEF25 in patients in both groups after treatment with different therapeutic regimens for 1 week are significantly higher than those before treatment (*P<0.05). After treatment, FEV1/FVC, PEF and PEF25 in the treatment group are significantly higher than those in the control group (#P<0.05).
Evaluation of therapeutic effects after treatment
The therapeutic effects on acute bronchial asthma in patients in both groups after treatment for one week were evaluated. The effective treatment rate (Table I) and therapeutic effect score (Fig. 2) showed that the effective treatment rate in treatment group was significantly higher than that in the control group (P<0.05). The therapeutic effect score in the treatment group was also significantly higher to that in the control group (P<0.05).
Table I.
Effective treatment rate of acute bronchial asthma.
| Groups | Remarkably effective (n) | Effective (n) | Ineffective (n) | Total effective rate (%) |
|---|---|---|---|---|
| Control group | 22 | 4 | 2 | 92.85 |
| Treatment group | 15 | 4 | 9 | 67.85 |
| P-value | <0.05 | >0.05 | <0.05 | <0.05 |
| t-test | 0.832 | 0.126 | 0.765 | 0.693 |
Figure 2.
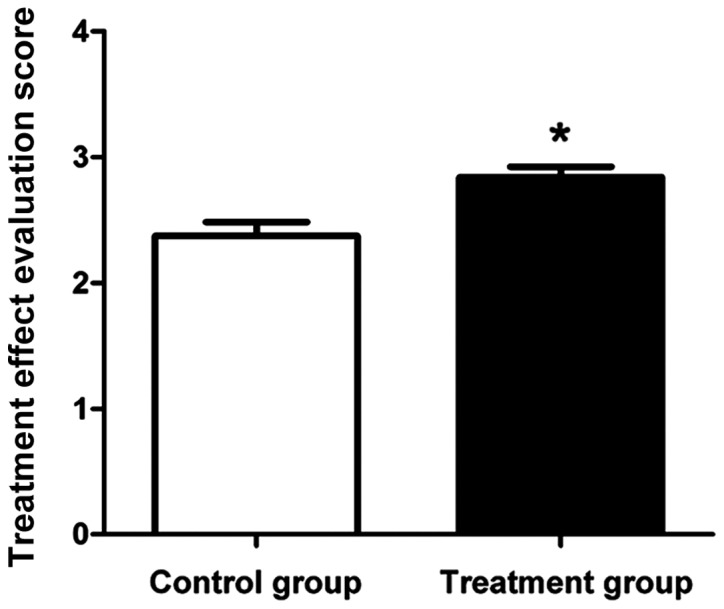
Therapeutic effect score of acute bronchial asthma. The score of patients in the treatment group is significantly higher than that of patients in the control group after treatment for 1 week; *P<0.05.
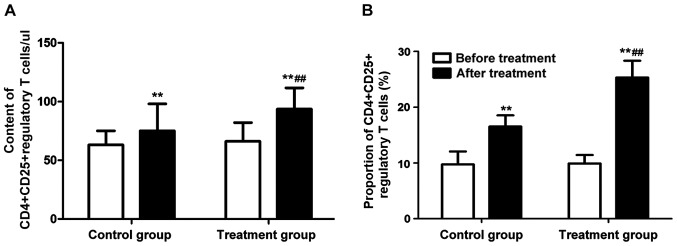
Changes in CD4+CD25+ regulatory T cells
CD4+CD25+ regulatory T cells in peripheral blood of patients in each group were detected before and after treatment. The results revealed that the content of CD4+CD25+ regulatory T cells in peripheral blood and its proportion in T lymphocytes in patients with acute bronchial asthma after treatment were obviously increased (P<0.01) (Fig. 3). In addition, the content of CD4+CD25+ regulatory T cells in peripheral blood and its proportion in T lymphocytes in patients in the treatment group were significantly higher than those in the control group, and the differences were statistically significant (P<0.01).
Figure 3.
Changes in CD4+CD25+ regulatory T cells in peripheral blood of patients with acute bronchial asthma in each group. (A) Content of CD4+CD25+ regulatory T cells in 1 µl peripheral blood. (B) Proportion of CD4+CD25+ regulatory T cells in T lymphocytes. Compared with that before treatment, **P<0.01. Compared with the control group, ##P<0.01.
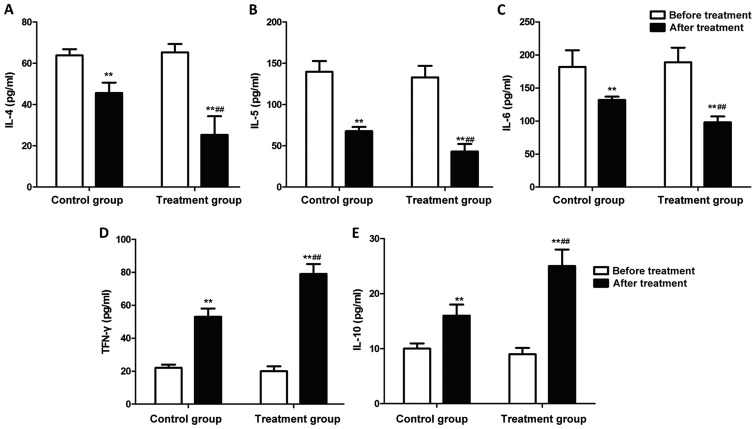
Changes in inflammatory factors
The changes in inflammatory factors in peripheral blood of patients in each group were detected using the ELISA kit. Fig. 4 shows that after drug therapy for 7 days, the levels of IL-4, IL-5 and IL-6 in patients in both groups were significantly decreased, but the levels of TFN-γ and IL-10 were significantly increased (P<0.01). Furthermore, the levels of IL-4, IL-5 and IL-6 in peripheral blood in the treatment group were lower than those in the control group, but the levels of TFN-γ and IL-10 were higher than those in the control group (P<0.01).
Figure 4.
Detection of levels of inflammatory factors in peripheral blood in each group using the ELISA kit. The levels of (A) IL-4, (B) IL-5 and (C) IL-6 in patients in both groups are significantly decreased after treatment, but the levels of (D) TFN-γ and (E) IL-10 are significantly increased. The levels of IL-4, IL-5 and IL-6 in peripheral blood in the treatment group are lower than those in the control group, but the levels of TFN-γ and IL-10 are higher than those in the control group. Compared with that before treatment, **P<0.01. Compared with the control group, ##P<0.01.
Change in serum IgE level
The change in serum IgE in peripheral blood of patients in each group was detected using the ELISA kit. The results (Fig. 5) showed that the serum IgE levels were significantly increased in both groups after drug therapy for 7 days (P<0.01). The serum IgE level in peripheral blood of patients in the treatment group was higher than that in the control group (P<0.01).
Figure 5.
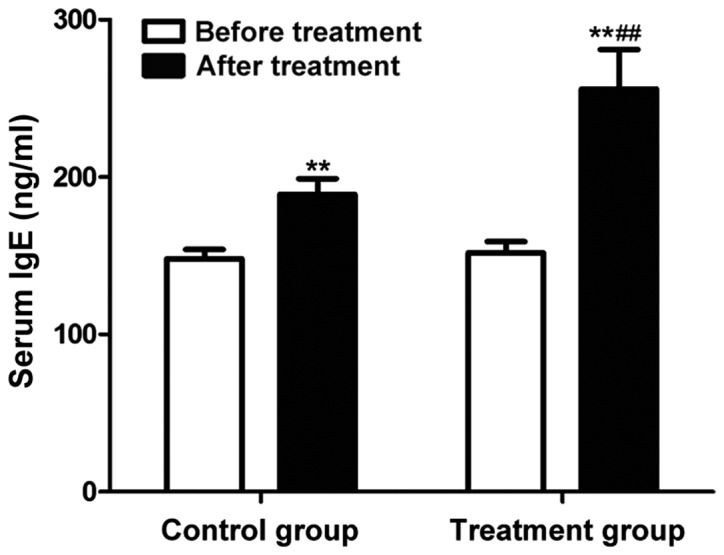
Change in serum IgE level. The serum IgE levels are significantly increased in both groups after treatment. The serum IgE level in peripheral blood of patients in the treatment group is higher than that in the control group. Compared with that before treatment, **P<0.01. Compared with the control group, ##P<0.01.
Discussion
Acute bronchial asthma is a kind of global disease affecting the life and health, as well as a multi-cell and multi-media chronic airway inflammation. Bronchial asthma is characterized by chronic airway inflammation and airway remodeling, involving a variety of cytokines (12). Cys-LT is the metabolite of leukotrienes, and previous findings have shown that a high concentration of Cys-LT is present in asthma patients, which is thought to be one of the causes and important mediators of asthma (13). Montelukast is a non-steroidal anti-inflammatory drug, which, as a selective inhibitor of Cys-LT, can relieve the airway spasm by reducing the Cys-LT concentration in patients, thus playing a role in the treatment of acute bronchial asthma (14). Moreover, montelukast can inhibit the accumulation and proliferation of inflammatory cells in the airway, reducing the glandular secretion of mucus in the body, and affecting the activation and differentiation of lymphocytes, thus reducing the permeability of blood vessels and playing an important role in the treatment of pulmonary fibrosis and trachea remode ling (15). Regulatory T cells are the cell population that can inhibit the functions of other cells and mediate other immune-active cells, which can be divided into CD4+CD25+ regulatory T cells, Th3 and Tr1, according to different cell compositions. These cells play important roles in bronchial asthma and other allergic diseases (16).
By studying the therapeutic effect of montelukast on children with acute bronchitis, the therapeutic effect of montelukast is examined from the perspective of improving clinical symptoms and lung function. Montelukast has a significant function in the treatment of acute bronchial asthma, which can effectively treat the bronchial asthma, increase the effective treatment rate, and significantly enhance the lung function of patients with bronchial asthma. Han et al (17) studied and found that montelukast can effectively reduce the level of airway eosinophils (EOS) in mice induced by inhaled ovalbumin, decrease the formation of mucous plug and inhibit the proliferation of airway smooth muscle. Additionally, the increased Th1-induced Th1/Th2 imbalance is an important mechanism of asthmatic attack. Th2 cytokines mainly include IL-4 and IL-5, and TFN-γ and IL-12 are typical Th1 cytokines. IL-4 and IL-5 are increased and TFN-γ is decreased in patients with bronchial asthma (18). The results of this study were consistent with the aboveme ones. It was found that the montelukast treatment for one week could significantly reduce the levels of IL-4, IL-5 and IL-6, but increase the levels of TFN-γ and IL-10, and regulate the Th1/Th2 balance, thus treating bronchial asthma. Moreover, montelukast increased the level of CD4+CD25+ regulatory T cells in patients with bronchial asthma by affecting the Th1/Th2 balance. The functions of EOS and epithelial cells can increase the synthesis of Cys-LT. IL-5 is an EOS differentiation factor, as well as an important stimulus for EOS release (19). IL-4 can upregulate the Cys-LT synthetase activity; TFN-γ can inhibit the IL-4-induced high expression of IgE and the occurrence of allergic reaction (20). There were still some shortcomings in this study; for example, the specific molecular mechanism was not deeply studied.
In conclusion, montelukast can regulate the Th1/Th2 balance, increase the expression of CD4+CD25+ regulatory T cells, inhibit the lung inflammation, and improve the lung function, which has an important therapeutic effect on acute bronchial asthma.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
XQ was involved in the conception and design of the study. YC performed the experiments. XQ and CY analysed the data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
The experimental scheme was approved by the Ethics Committee of Shangluo Central Hospital (Shangluo, China). Parents or their guardians signed the written informed consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Canonica GW, Senna G, Mitchell PD, O'Byrne PM, Passalacqua G, Varricchi G. Therapeutic interventions in severe asthma. World Allergy Organ J. 2016;9:40. doi: 10.1186/s40413-016-0130-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung LP, Baltic S, Ferreira M, Temple S, Waterer G, Thompson PJ. Beta2 adrenergic receptor (ADRβ2) haplotype pair (2/4) is associated with severe asthma. PLoS One. 2014;9:e93695. doi: 10.1371/journal.pone.0093695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grieger JA, Wood LG, Clifton VL. Improving asthma during pregnancy with dietary antioxidants: The current evidence. Nutrients. 2013;5:3212–3234. doi: 10.3390/nu5083212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jung JW, Choi JC, Shin JW, Kim JY, Park IW, Choi BW. Clinical characteristics according to sensitized allergens in adult korean patients with bronchial asthma. Allergy Asthma Immunol Res. 2010;2:102–107. doi: 10.4168/aair.2010.2.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akpinarli A, Tuncer A, Saraçlar Y, Sekerel BE, Kalayci O. Effect of formoterol on clinical parameters and lung functions in patients with bronchial asthma: A randomised controlled trial. Arch Dis Child. 1999;81:45–48. doi: 10.1136/adc.81.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scott M, Raza A, Karmaus W, Mitchell F, Grundy J, Kurukulaaratchy RJ, Arshad SH, Roberts G. Influence of atopy and asthma on exhaled nitric oxide in an unselected birth cohort study. Thorax. 2010;65:258–262. doi: 10.1136/thx.2009.125443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scaparrotta A, Di Pillo S, Attanasi M, Rapino D, Cingolani A, Consilvio NP, Verini M, Chiarelli F. Montelukast versus inhaled corticosteroids in the management of pediatric mild persistent asthma. Multidiscip Respir Med. 2012;7:13. doi: 10.1186/2049-6958-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jindal A, Suriyan S, Sagadevan S, Narasimhan M, Shanmuganathan A, Vallabhaneni V, Rajalingam R. Comparison of oral montelukast and intranasal fluticasone in patients with asthma and allergic rhinitis. J Clin Diagn Res. 2016;10:OC06–OC10. doi: 10.7860/JCDR/2016/20741.8268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciebiada MG, Barylski M, Ciebiada M. Wheal and flare reactions in skin prick tests of patients treated with montelukast alone or in combination with antihistamines. Inflamm Res. 2014;63:191–195. doi: 10.1007/s00011-013-0688-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bao W, Liu P, Qiu Z, Yu L, Hang J, Gao X, Zhou X. Efficacy of add-on montelukast in nonasthmatic eosinophilic bronchitis: The additive effect on airway inflammation, cough and life quality. Chin Med J (Engl) 2015;128:39–45. doi: 10.4103/0366-6999.147805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee J-H, Yu H-H, Wang L-C, Yang Y-H, Lin Y-T, Chiang B-L. The levels of CD4+CD25+ regulatory T cells in paediatric patients with allergic rhinitis and bronchial asthma. Clin Exp Immunol. 2007;148:53–63. doi: 10.1111/j.1365-2249.2007.03329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watanabe T, Fajt ML, Trudeau JB, Voraphani N, Hu H, Zhou X, Holguin F, Wenzel SE. Brain-derived neurotrophic factor expression in asthma. Association with severity and type 2 inflammatory processes. Am J Respir Cell Mol Biol. 2015;53:844–852. doi: 10.1165/rcmb.2015-0015OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.FitzGerald JM, Foucart S, Coyle S, Sampalis J, Haine D, Psaradellis E, McIvor RA. Montelukast as add-on therapy to inhaled corticosteroids in the management of asthma (the SAS trial) Can Respir J. 2009;16(Suppl A):5A–14A. doi: 10.1155/2009/593753. (In French) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reiss TF, Hill JB, Harman E, Zhang J, Tanaka WK, Bronsky E, Guerreiro D, Hendeles L. Increased urinary excretion of LTE4 after exercise and attenuation of exercise-induced bronchospasm by montelukast, a cysteinyl leukotriene receptor antagonist. Thorax. 1997;52:1030–1035. doi: 10.1136/thx.52.12.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Keith PK, Koch C, Djandji M, Bouchard J, Psaradellis E, Sampalis JS, Schellenberg RR, McIvor RA. Montelukast as add-on therapy with inhaled corticosteroids or inhaled corticosteroids and long-acting beta-2-agonists in the management of patients diagnosed with asthma and concurrent allergic rhinitis (the RADAR trial) Can Respir J. 2009;16(Suppl A):17A–31A. doi: 10.1155/2009/409285. (In French) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bernstein JM, Lehman H, Lis M, Sands A, Wilding GE, Shultz L, Bankert R, Bobek L. Humanized mouse model used to monitor MUC gene expression in nasal polyps and to preclinically evaluate the efficacy of montelukast in reducing mucus production. Ann Otol Rhinol Laryngol. 2012;121:307–316. doi: 10.1177/000348941212100505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Han J, Jia Y, Takeda K, Shiraishi Y, Okamoto M, Dakhama A, Gelfand EW. Montelukast during primary infection prevents airway hyperresponsiveness and inflammation after reinfection with respiratory syncytial virus. Am J Respir Crit Care Med. 2010;182:455–463. doi: 10.1164/rccm.200912-1811OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kianmehr M, Haghmorad D, Nosratabadi R, Rezaei A, Alavinezhad A, Boskabady MH. The effect of Zataria multiflora on Th1/Th2 and Th17/T regulatory in a mouse model of allergic asthma. Front Pharmacol. 2017;8:458. doi: 10.3389/fphar.2017.00458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rolfes MC, Juhn YJ, Wi C-I, Sheen YH. Asthma and the risk of rheumatoid arthritis: An insight into the heterogeneity and phenotypes of asthma. Tuberc Respir Dis (Seoul) 2017;80:113–135. doi: 10.4046/trd.2017.80.2.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cui A-H, Zhao J, Liu S-X, Hao Y-S. Associations of IL-4, IL-6, and IL-12 levels in peripheral blood with lung function, cellular immune function, and quality of life in children with moderate-to-severe asthma. Medicine (Baltimore) 2017;96:e6265. doi: 10.1097/MD.0000000000006265. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.