Abstract
Ultraviolet blood irradiation (UBI) was extensively used in the 1940s and 1950s to treat many diseases including septicemia, pneumonia, tuberculosis, arthritis, asthma and even poliomyelitis. The early studies were carried out by several physicians in USA and published in the American Journal of Surgery. However with the development of antibiotics, UBI use declined and it has now been called “the cure that time forgot”. Later studies were mostly performed by Russian workers and in other Eastern countries and the modern view in Western countries is that UBI remains highly controversial.
This chapter discusses the potential of UBI as an alternative approach to current methods used to treat infections, as an immune-modulating therapy and as a method for normalizing blood parameters. No resistance of microorganisms to UV irradiation has been reported, and multi- antibiotic resistant strains are as susceptible as their wild-type counterparts. Low and mild doses of UV kill microorganisms by damaging the DNA, while any DNA damage in host cells can be rapidly repaired by DNA repair enzymes. However the use of UBI to treat septicemia cannot be solely due to UV-mediated killing of bacteria in the blood-stream, as only 5–7% of blood volume needs to be treated with UV to produce the optimum benefit. UBI may enhance the phagocytic capacity of various phagocytic cells (neutrophils and dendritic cells), inhibit lymphocytes, and oxidize blood lipids. The oxidative nature of UBI may have mechanisms in common with ozone therapy and other oxygen therapies. There may be some similarities to extracorporeal photopheresis (ECP) using psoralens and UVA irradiation. However there are differences between UBI and ECP in that UBI tends to stimulate the immune system, while ECP tends to be immunosuppressive. With the recent emergence of bacteria that are resistant to all known antibiotics, UBI should be more investigated as an alternative approach to infections, and as an immune-modulating therapy.
Keywords: Ultraviolet C, Knott hemo-irradiator, UBI, DNA repair, Blood cells, Antigen-presenting cells, Infections, Cytokines
25.1. Historical Introduction
Ultraviolet (UV) radiation is part of the electromagnetic spectrum with a wavelength range (100–400 nm) shorter than that of visible light (400–700 nm), but longer than x-rays (<100 nm). UV radiation is divided into four distinct spectral areas including vacuum UV (100–200 nm), UVC (200–280 nm), UVB (280–315 nm) and UVA (315–400 nm). Only part of UVB and UVA can reach on earth, because wavelengths shorter than 280 nm are filtered out by the atmosphere especially by the “ozone layer”.
In 1801 Johann Wilhelm Ritter, a Polish physicist working at the University of Jena in Germany discovered a form of light beyond the violet end of the spectrum that he called “Chemical Rays” and which later became “Ultraviolet” light [1]. In 1845, Bonnet [2] first reported that sunlight could be used to treat tuberculosis arthritis (a bacterial infection of the joints).
In the second half of the nineteenth century, the therapeutic application of sunlight known as heliotherapy gradually became popular. In 1855, Rikli from Switzerland opened a thermal station in Veldes in Slovenia for the provision of helio-therapy [3]. In 1877, Downes and Blunt discovered by chance that sunlight could kill bacteria [4]. They noted that sugar water placed on a window- sill turned cloudy in the shade but remained clear while in the sun. Upon microscopic examination of the two solutions, they realized that bacteria were growing in the shaded solution but not in the one exposed to sunlight.
In 1904, the Danish physician Niels Finsen was awarded the Nobel Prize in Physiology or Medicine for his work on UV treatment of various skin conditions. He had a success rate of 98% in thousands of cases, mostly the form of cutaneous tuberculosis known as lupus vulgaris [5]. Walter H Ude reported a series of 100 cases of erysipelas (a cutaneous infection caused by Streptococcus pyogenes) in the 1920s, with high cure rates using irradiation of the skin with UV light [6].
Emmett K Knott (Fig. 25.1) in Seattle, WA reasoned that the beneficial effects of UV irradiation to the skin obtained by Ude, might (at least partly) be explained by the irradiation of blood circulating in the superficial capillaries of the skin. With his collaborator Edblom, an irradiation chamber was constructed to allow direct exposure of the blood to UV. The irradiation chamber was circular and contained a labyrinthine set of channels that connected the inlet and outlet ports. All these channels were covered with a quartz window that formed the top of the chamber. The irradiation chamber was so designed as to provide maximum turbulence of the blood flowing through (see Fig. 25.2). This was done in order to: (a) prevent the formation of a thin film of blood on the chamber window that would absorb and filter out much of the UV light; (b) insure that all the blood passing through the chamber was equally exposed to UV [7].
Fig. 25.1.
Emmett K Knott
Fig. 25.2.
The Knott Hemo-Irradiator
Knott and co-workers then carried out a series of experiments using UV irradiation of blood extracted from dogs that had been intravenously infected with Staphylococcus aureus bacteria and hemolytic Streptococcus species, and then the treated blood was reinfused into the dogs. They found that it was unnecessary to deliver a sufficient exposure of UV light to the blood to directory kill all the bacteria in the circulation. It was also found unnecessary to expose the total blood volume in the dogs. The optimum amount of blood to be irradiated was determined to be only 5–7% of the estimated blood volume or approximately 3.5 mL per kg of body weight. Exceeding these limits led to loss of the benefits of the therapy. All the dogs that were treated with the optimized dose of UV to the blood, recovered from an overwhelming infection (while many dogs in the control group died). None of the dogs that were treated and survived, showed any long-term ill effects after 4 months of observation [7].
The first treatment on a human took place in 1928 when a patient was determined to be in a moribund state after a septic abortion complicated by hemolytic streptococcus septicemia. UBI therapy was commenced as a last resort, and the patient responded well to the treatment and made a full recovery [7]. She proceeded to give birth to two children.
Hancock and Knott [8] had similar success in another patient suffering from advanced hemolytic streptococcal septicemia. These workers noted that in the majority of cases, a marked cyanosis (blue tinge to the skin caused by a lack of oxygenated blood flow) was present at the time of initiation of UBI. It was noted that during (or immediately following) the treatment a rapid relief of the cyanosis occurred, with improvement in respiration accompanied by a noticeable flushing of the skin, with a distinct loss of pallor.
These observations led to application of UBI in patients suffering from pneumonia. In a series of 75 cases in which the diagnoses of pneumonia were confirmed by X-rays, all patients responded well to UBI showing a rapid decrease in temperature, disappearance of cyanosis (often within 3–5 min), cessation of delirium if present, a marked reduction in pulse rate and a rapid resolution of pulmonary consolidation. A shortening of the time of hospitalizations and accelerated convalescence was regularly observed.
The knowledge gained in these successful studies led to the redesign of the irradiation chamber to allow a more thoroughly uniform exposure of the circulating blood, and led to the development of the “Knott Technic of Ultraviolet Blood Irradiation.” A number of irradiation units were manufactured and placed in the hands of physicians interested in the procedure, so that more extensive clinical data could be accumulated [7]. The Knott technique involved removing approximately 3.5 mL/kg venous blood, citrating it as an anticoagulant, and passing it through the radiation chamber. The exposure time per given unit of blood was approximately 10 s, at a peak wavelength of 253.7 nm (ultraviolet C) provided by a mercury quartz burner, and the blood was immediately re-perfused [7].
George P Miley at the Hahnemann Hospital, Philadelphia, PA published a series of articles on the use of the procedure in the treatment of thrombophlebitis, staphylococcal septicemia, peritonitis, botulism, poliomyelitis, non-healing wounds, and asthma [9–22].
Henry A Barrett at the Willard Parker Hospital in New York City in 1940 reported on 110 cases including a number of different infections. Twenty-nine different conditions were described as being responsive, including the following: infectious arthritis, septic abortion, osteoarthritis, tuberculosis glands, chronic blepharitis, mastoiditis, uveitis, furunculosis, chronic paranasal sinusitis, acne vulgaris, and secondary anemia [23, 24].
EV Rebbeck at the Shadyside Hospital in Pittsburgh, PA, reported the use of UBI in Escherichia coli septicemia, post-abortion sepsis, puerperal sepsis, peritonitis, and typhoid fever [25–29] and Robert C Olney at the Providence Hospital, Lincoln, NE, treated biliary disease, pelvic cellulitis and viral hepatitis [30–32].
In this chapter, we will discuss the mechanisms and the potential of UBI as an alternative approach to infections and as a new method to modulate the immune system. Our goal is to remind people to continue to do more research and explore more clinical uses. The topics include the efficacy of UBI for infections (both bacterial and viral), to cure autoimmune disease, disease, and the similarities and differences between UBI, and intravenous ozone therapy, and extracorporeal psoralen-mediated photochemotherapy (photophoresis).
25.2. Mechanisms of Action of UBI
One of the major obstacles that UBI has consistently faced throughout the almost 90 years since the first patient was treated has been the lack of understanding of the mechanisms of action. Over the years its acceptance by the broad medical community has been hindered by this uncertainty. Confusion has been caused by the widely held idea that since UV is used for sterilization of water and surgical instruments; therefore its use against infection must also rely on UV-mediated direct destruction of pathogens. Another highly confusing aspect is the wide assortment of diseases, which have been claimed to be successfully treated by UBI. It is often thought that something that appears to be “too good to be true” usually is.
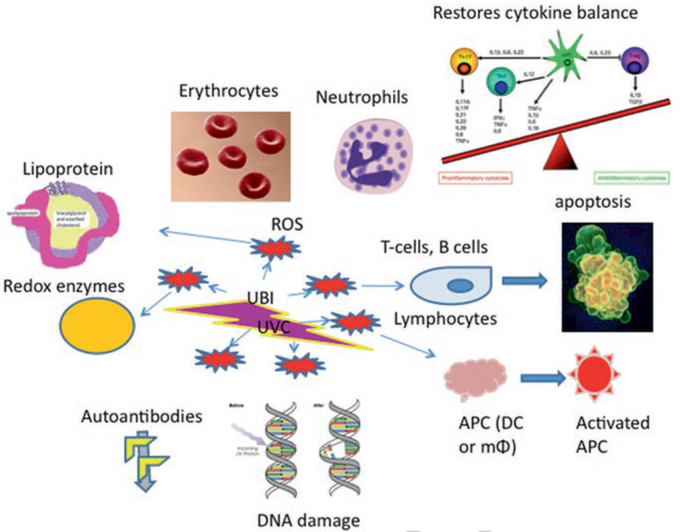
UBI affects various functions of red blood cells and various different leukocytes as has been proven in various in vitro studies. A common model is stimulator cells in mixed leukocyte cultures; another is helper cells in mitogen- stimulated cultures. UV also reversed cytokine production and blocked cytokine release. UV can also disturb cell membrane mobilization (Fig. 25.3).
Fig. 25.3.
Proposed mechanisms of UBI[AU4]
25.2.1. Effects on Red Blood Cells
Anaerobic conditions strongly inhibited the process by which long wave UV light induces the loss of K+ ions from red blood cells. Kabat proved that UV-irradiation could affect the osmotic properties of red blood cells, the submicroscopic structure and the metabolism of adenine nucleotides. Irradiation times (60, 120, 180, 240 and 300 minutes) were used; during the irradiation, ATP decreased while the amounts of ADP, AXP, adenine compounds all increased. UV also increased hypotonic Na + and K+ ion exchange and the hematocrit value increased [33].
When Rh-positive blood was irradiated with UV light there was a significant increase in immunosorption activity. Vasil’eva et al. [34] studied varying UV irradiation conditions on both red blood cells and leucocyte-thrombocyte suspensions. Immunosorption activity increased immediately after irradiation in whole blood and red blood cells; however the immunosorption capacity in leucocyte–thrombocyte suspensions was lost after 2 days.
A two-phase polymer system containing poly-dextran was used to show that the cell surface of circulating erythrocytes was reduced after UV irradiation. This contributed to the prolongation of survival of transfused erythrocytes and was suggested to explain the more effective therapeutic activity of autotransfused blood [35]. Snopov et al. suggested that some structural alterations in the erythrocytes, particularly in the glycocalyx were related to the improved effect of autotrans-fused blood after UV-irradiation [36]. Ichiki et al. showed that the cellular volume and the membrane potential of erythrocytes could be changed by UV irradiation. However an excessive dose of UV could decrease the production of H2O2 [37].
25.2.2. Effects on Neutrophils
Lower doses of UV (<0.1 J/cm2) increased the production of peroxides (H2O2) by polymorphonuclear leukocytes (which is the largest amongst all the different blood cells). The ability of UBI to increase the production of reactive oxygen species (ROS) by neutrophils could be inhibited by addition of arachidonic acid or lysophosphatidylcholine (LPC), as well as the anti-oxidant, α-tocopherol [38]. In chronic inflammatory diseases, the concentration of large IC--IgG, IgM, and small IC–IgM showed an inverse linear correlation with increased UBI dose delivered to autotransfused blood [39].
Artiukhov suggested that the generation of nitric oxide (NO) by photomodified neutrophils was due to the activation of the iNOS enzyme. De novo NO synthesis was increased by UV-irradiation, which also affected TNF-alpha production. Irradiation with lower dose (75.5 J/ m2) allowed the maintenance of the physiological homeostasis. While higher dose (755 and 2265 J/m2) delivered to neutrophils led to potential damage, by increasing the concentration of NO metabolites. When UV-irradiated cells were incubated with the transcriptional inhibitor of protein synthesis, cycloheximide the activation of iNOS and NO synthesis was prevented. High doses of UV-irradiation (755 J/m2) on neutrophils, showed a positive correlation between NO and TNF-alpha concentrations [40].
Zor’kina carried out a 30-day rabbit experiment, and suggested that the chronic stress produced with a combination of hypodynamia and UBI, affected neutrophils and eliminated coagulation. UBI contributed to improvement in the body’s abilities to resist long-term hypodynamia and ameliorated chronic stress. UBI enhanced the adaptive process through activated neutrophils, prevented disseminated intravascular coagulation, and changed the atherogenic metabolic profile [41].
25.2.3. Effects on Lymphocytes (T-Cells and B-Cells)
UBI generally decreases lymphocyte viability. UVC irradiation is the most effective among the three UV spectral regions. UVB and UVC irradiation can abolish the proliferative and stimulatory ability as well as the accessory/ antigen-presenting ability of lymphocytes in vitro. The cell-surface properties, calcium mobilization, cytokine production and release, and other sub cellular processes could all be changed by UV irradiation [42]. Areltt et al. used the “Comet “assay to detect DNA-strand breakage (single cell gel electrophoresis) as an indicator of excision repair to prove that circulating human T–lymphocytes were exquisitely hyper-sensitive to the DNA-damaging and lethal effects of UV-B radiation, raising the possibility that UV-B may make a contribution to immunosuppression via a direct effect on extracapilliary T-lymphocytes [43].
Teunissen et al. suggested that UVB radiation neither selectively affects either Th1 or Th2 nor CD4 or CD8 T-cell subsets. Compared with different dose of UVB irradiation, although the phototoxic effect was not immediately apparent, a low dose of UVB (LD50: 0.5–1 mJ/cm2) irradiation was sufficient to kill most T cells after 48–72 h [44]. There was a dose dependent reduction in all measured cytokines (IL-2, IL-4, IL-5, IFN-ɤ, TNF-a) in the same way 72 h after irradiation. This fall in production was indicated by a remarkable correlation between loss of viability and reduction of cytokine production that may be caused directly by cell death. However, CD4+ or CD8+ T cell subsets, expression of CD4 and CD8 as well as the CD4/CD8 ratio compared with the non-irradiated control, was not altered by UVB, suggesting that none of the T-cell subsets was selectively affected.
Schieven et al. observed that UV-induced tyrosine phosphorylation in B cells after surface immunoglobulin cross-linking. This observation was very similar to the production of Ca2+ signals in T cells. It means that UV irradiation of lymphocytes could induce both tyrosine phosphorylation and Ca2+ signals. Ca2+ channels in lymphocyte membranes are sensitive to UV irradiation; UV radiation causes DNA damage through the activation of cellular signal-transduction processes. UV radiation (depending on dose and wavelength) not only induces tyrosine phosphorylation in lymphocytes but also Ca2+ signals in Jurkat T cells. Furthermore, the pattern of surface immunoglobulin cross-linking was similar to the UV-induced tyrosine phosphorylation in B cells. The UBI effect on lymphocyte function may play an important role in tyrosine phosphorylation and Ca2+ signals, which can escape from normal receptor control. They showed that both CD4+ and CD8+ T cells (normal human lymphocytes) gave strong reactions during UV-irradiation [45].
In a similar study, Spielberg et al. found that UV-induced lymphocyte inhibition showed a similar course in disruption of Ca2+ homeostasis by comparing UV with gamma irradiation, which have different effects on lymphocyte membranes [46]. Furthermore, the presence of Ca2+ channels in lymphocyte membranes that are sensitive to UV irradiation was shown by indo-1 staining and cytofluorometry. Intracellular calcium [Ca2+]i kinetics was measured in UVC or UVB-exposed human peripheral blood leukocytes (PBL) and Jurkat cells were in parallel with functional assays. The UV-induced i[Ca2+] rise was predominantly due to an influx of extracellular calcium, and it was more pronounced in T-cells than in non-T cells. It was observed that [Ca2+]i increased within 2–3 h of irradiation; these increases were UV-dose dependent and reached maxima of 240% and 180% above the baseline level (130 nM) for UVB and UVC. UV induced a bigger [Ca2+]i rise in T-cells than in non-T cells, due to the influx of extracellular calcium. UV-induced calcium shifts, and UV irradiation on the plasma membrane decreased the sensitivity to respond to phytohemagglutinin (PHA) in mixed leukocyte cultures.
A series of studies confirmed that UVR irradiated lymphocytes were not able to induce allogeneic cells in the mixed lymphocyte culture (MLC) as first reported by Lindahl-kiessling. [47–49]. Clusters formed by specialized accessory cells after mitogenic or allogenic stimulation, with dendritic cells (DC) are necessary for lymphocyte activation to occur. Aprile found that UV irradiation of DC before culture completely abrogated accessory activity was capable to block both cluster formation and no lymphocyte proliferation occurred [50].
Kovacs et al. [51] found that induction of DNA repair mechanisms was dependent on the dose of UVC light between 2 and 16 J/cm2. It was evaluated in irradiated and non-irradiated lymphocytes in 51 healthy blood donors. UVC irradiation (253.7 nm) at doses of 2, 4, 8 and 16 J/m2 by measuring [3H] thymidine incorporation in the presence of 2 mM hydroxyurea added 30 min before irradiation to inhibit DNA-replication synthesis. No significant age-related difference was found in donors between 17 and 74 years.
UV-induced differentiation in human lymphocytes, and accelerated the intensity of DNA repair in these cells [52]. Exposure to UV irradiation was more effective than methyl methane sulfonate (MMS) in increasing unscheduled DNA synthesis, especially when MMS was added prior to the UV-irradiation, at 2 h or 26 h before UVC, because MMS affects DNA repair by alkylating the DNA polymerase [53]. Photo-modification of HLA-D/ DR antigens could be a trigger mechanism for activation of immunocompetent cells by UV-irradiation. Lymphocytes were isolated from non-irradiated blood, irradiated blood and a mixture of the two in different ratios (1:10,1:40,1:160) [54].
UBI before transfusion can inhabit immune recognition and prevent bone marrow graft rejection in vivo. After 9.2 Gy of total body irradiation (TBI) and 2.8 ± 2.1 × 108/Kg donor marrow cells were infused, whole blood was exposed for 30 minutes to UV light at a dose of 1.35 J/cm2 and then injected into the recipient dogs. The control group, which was transfused with sham-exposed blood, rejected the bone marrow grafts, while no rejection was found in the group, which received UV-exposed blood before the transplanted marrow. UV irradiation on blood inhibited lymphocyte activation by eliminating a critical DC-dependent signal [55].
Oluwole et al. suggested that transfusion of UV-irradiated blood into recipients prior to heart transplantation could be carried out, in order to inhibit immune response, and reduce lymphocyte- mediated rejection [56]. Three sets of different rat strains (ACI, Lewis, W/F) were used for heart transplantation in his research. In the series where ACI rats received a Lewis heart, 1 mL transfusion of donor-type blood with or without UV-irradiation was transfused at 1, 2, and 3 weeks prior to the transplantation. A mixed lymphocyte reaction showed that ACI lymphocytes were weaker responders to Lewis lymphocytes, and the same as the other two series of different type heart transplantations. UV irradiation of donor rhesus-positive blood can be used to increase the therapeutic effect of blood exchange transfusion in children with rhesus-conflict hemolytic disease [57].
25.2.4. Effects on Monocytes, Macrophages and Dendritic Cells
All these types of blood cells including monocytes, macrophages and dendritic arise from the myelocytic lineage of hematogenous stem cells, and act as phagocytes and antigen presenting cells. The phagocytic capacity of UV-B irradiated mononuclear cells derived from human peripheral blood could be enhanced by all four types of deoxyribonucleoside supplementation [58].
Stimulation of phagocytic activity (PhA) appears to be one of the earliest mechanisms in immuno-correction by UV-irradiation of blood therapy. In Samoĭlova’s research, non-irradiated blood, mixed with 1:10 irradiation blood, were tested for PhA of monocytes and granulocytes. Increase of 1.4–1.7 times of PhA compare with non-supplemented blood, because monocytes and granulocytes could be increase by adding UV-irradiated blood into healthy adults. The enhancement of PhA depends on its initial level and may occur simultaneously with structural changes of the cell surface components [59].
UV-irradiation increased the phagocytic activity of human monocytes and granulocytes, and the “integrated phagocytic index” increased in proportion to the irradiation dose, while a lower initial level would increase more than a higher initial rate after UV-irradiation [60].
Simon et al. [61] concluded that UVB could convert Langerhans cells (LC) or splenic adherent cells (SAC) from an immunogenic phenotype into a tolerogenic phenotype, as far as antigen presenting cells were concerned (LC or SAC). In his research, a single dose of irradiation (200 J/cm2) was delivered to LC and SAC. The loss of responsiveness was found when UV-LC or UV-SAC were incubated with Th1 cells that had been pre-incubated with keyhole limpet hemocyanin (KLH). Furthermore, such loss of responsiveness was not related to the release of soluble suppressor factors, but was Ag-specific, MHC-restricted, and long-lasting. The hypothesis to explain these results was that delivery of a costimulatory signal(s) had been interfered with by UVB irradiation, because unresponsiveness by UVB-LC or UVB-SAC could not be induced by non-irradiated allogeneic SAC.
25.2.5. Effects on Platelets
H2O2 production in platelets is low at very low UV dose, but it increased suddenly as the dose increased above 0.4 J/cm2. Pamphilon reported that platelet concentrates (PC) could become non-immunogenic after UVR and after being stored for 5 days in DuPont Stericell containers. Lactate levels, β-thromboglobulin and platelet factor were higher after UV, while glucose levels decreased with an irradiation dose of 3000 J/m2 at a mean wavelength of 310 nm applied in DuPont Stericell bags [62]. Ultraviolet B (UVB) irradiation of platelet concentrate (PC) accelerated downregulation of CD14 and nonspecifically increased the loss of monocytes by inhibiting the upregulation of ICAM-1 and HLA-DR [63]. However, UV irradiation of platelet concentrates produced a reduction of immunological response in a cell suspension [64–66].
25.2.6. Effects on Low Density Lipoprotein (LDL) and Lipids
Roshchupkin et al. found that UV irradiation played a core role in lipid peroxidation in the membranes of blood cells [67]. UV irradiation of blood could stimulate arachidonic acid to be metabolized by cyclooxygenase, and could induce dark lipid autoperoxidation into free radicals and direct photolysis of photooxidants. UV contributed to lipid photoperoxidation producing lipid hydroperoxides.
UV irradiated lipid emulsion greatly enhanced the production of reactive oxygen species (ROS) by monocytes, and highly atherogenic oxidized LDL could be generated in the blood circulation. UV light-oxidized lipofundin (a parenteral lipid emulsion designed for injection) was injected into rabbits, then blood samples were taken from the ear vein with EDTA (before and 6 h after after) lipofundin treatment. Although UV-oxidized lipofundin induced less chemiluminescence from monocytes compared with Fe3+−oxidized lipofundin, the effect lasted 2.3 times longer. UV–oxidized lipofundin could more effectively stimulate H2O2 production than monocyte-oxidized LDL, even with the same concentration of thiobarbituric acid reactive substances (TBARS) in the preparations. Six hours after injection of oxidized lipofundin, the lipid peroxide content was significantly increased, however the neutral lipids in LDL isolated from rabbit plasma showed no significantly difference to the monocyte-oxidized human LDL [68].
Salmon found that UVB (280–315 nm) irradiation could easily damage LDL and also the tryptophan (Trp) residues in high density lipoprotein (HDL) [69]. The TBARS assay was used to measure the photooxidation of tryptophan residues which accompanied the peroxidation of low and high density lipoprotein unsaturated fatty acids. Vitamin E and carotenoids were also rapidly destroyed by UVB. However UVA radiation could not destroy tryptophan residues and cause lipid peroxidation.
UV radiation (wavelength range 290–385 nm) easily oxidized the lipoproteins contained in the suction blister fluid of healthy volunteers, which is a good model of the interstitial fluid feeding the epidermal cells. Apolipoprotein B of LDL and apolipoprotein A-I and II of HDL were all altered in a similar way under UV irradiation. Irradiation with wavelengths in the range 290–385 nm altered the single Trp (tryptophan) residue of serum albumin which is susceptible to photo-oxidation. UVA irradiation of undiluted suction blister fluid induced A-I aggregation; however purified lipoproteins were not degraded. During UV irradiation of suction blister fluid, antigenic apolipoprotein B is fragmented and polymerized. Reactive oxygen radicals in the suction blister fluid were derived from lipid peroxidation occurring in HDL. UV-light irradiation could play an important role in triggering inflammation and degeneration by inducing lipoprotein photo-oxidation which could have systemic effects [70].
25.2.7. Redox Status
Artyukhov et al. [71] discovered that dose- dependent UV-irradiation could activate the myeloperoxidase (MPO) and the NADPH- oxidase systems in donor blood. Two doses of UV-light were used (75.5 and 151.0 J/m2) and the higher dose activated more free radicals and H2O2 than the lower dose, another two groups were divided by the type of relationship between MPO activity and UV light dose (from 75.5 to 1510 J/m2), low enzyme activity (group 1) increased under the effect of UV exposure at doses of 75.5 and 151.0 J/m2, while in group 2 this parameter (MPO activity) decreased. MPO activity showed the same results in dose dependent UV-irradiation, however, increasing the dose to 1510 J/m2 could not increase the activity of MPO. In the next experiments, lipid peroxidation (LPO) was evaluated after UV exposure of the blood. Two groups of donors were distinguished by the relationship between blood content of LPO products and UV exposure dose. UV irradiation at low doses (75.5–151.0 J/m2) decreased initially high LPO values and increased initially low LPO levels. In phagocytes, NADPH-oxidase plays one of the most important roles as a photoacceptor for UV light. NADPH oxidase causes increased superoxide (O2•—) production after UV-irradiation of blood by activation of the enzyme complex. UV irradiation also decreases intracellular pH caused by activation of the NADPH-oxidase complex.
UBI can also protect against free radical damage by elevating the activity of various antioxidants after spinal cord injury in rabbits, 186 rabbits were randomly divided into 4 groups, (control, blood transfusion, injured and UV treatment). UV irradiation (wavelength 253.7 nm, 5.68 mW/m2) was used in the treatment group at 48–72 h after surgery for spinal cord injury. Free radical signals (FR), malondialdehyde (MDA), superoxide dismutase (SOD) and glutathione peroxidase (GSH-PX) were measured. In the treatment group, superoxide dismutase and glutathione peroxidase were much increased and showed significant differences compared with the other groups, while FR and MDA decreased significantly compared to other groups. Because UV irradiation of blood decreased the MDA and FR content in spinal cord tissue; they also suggested that these two factors contributed to higher SOD activity and increased GSH-PX [72].
25.2.8. Conclusions Regarding Mechanisms
UBI has always caused much confusion, both in the general public and also in some medical professionals, because germicidal UV light (UVC) is used to sterilize water, disinfect surfaces, and as an aid to infection control in operating rooms, and food processing and packaging plants. Many people therefore assume that UBI must act by killing pathogens (bacteria, viruses or other microorganisms) circulating in the bloodstream. However there is no evidence that this is actually the case. Therefore the mechanisms of action must lie in some other action of UV on the various components of blood. Although the entire body of evidence on the mechanisms of action of UBI is very complex, as can be seen from the foregoing material, we can attempt to draw some general conclusions. Firstly UBI is clearly an example of the well-known phenomenon called “hormesis” or “biphasic dose response’. This phenomenon has been well reviewed by Edward Calabrese from U Mass Amherst [73, 74]. The basic concept states that any toxic chemical substance or drug, or any physical insult (such as ionizing radiation, hyperthermia, or oxidative stress) can be beneficial, protective or even therapeutic, provided the dose is low enough. If the dose is increased, the beneficial or protective effects disappear, and if the dose is even further increased, then the detrimental effects of the treatment become very evident. This is clearly shown by Knott’s original experiments on dogs that led to the establishment of only 5–7% of total blood volume as the optimal amount of blood to be irradiated.
UBI appears to have three broadly different classes of effects on different blood components. In the case of neutrophils, monocytes, macrophages, and dendritic cells, UBI can activate phagocytosis, increase the secretion of NO and reactive nitrogen species, and convert the DC phenotype from an immunogenic one into a tolerogenic one, thus perhaps lessening the effects of a “cytokine storm” as is often found in sepsis. In the case of lymphocytes, the effects of UBI are to inhibit (or in fact kill) various classes of lymphocytes. This is not perhaps very surprising, considering the well-established cell-death pathways and apoptotic signaling found in lymphocytes. However it is not impossible, that the killing of circulating lymphocytes could reduce systemic inflammation, which would again be beneficial in cases of sepsis. It is also clear that UBI can oxidize blood lipids and lipoproteins, and therefore increase oxidative stress. However it is also possible that a brief burst of oxidative stress, may be beneficial, whereas continued chronic levels of oxidative stress have been generally considered as detrimental. Many antioxidant defenses are up-regulated by brief exposure to oxidative stress, and this has been postulated to be one of the fundamental mechanisms responsible for may aspects of hormesis. The oxidative nature of UBI has encouraged us to draw parallels with ozone therapy and other forms of ‘oxygen therapy”.
25.3. Ozone Therapy
Since UBI is generally considered to be controversial, then ozone therapy is even more controversial. Ozone therapy consists of the introduction of ozone (O3) into the body via various methods, usually involving its mixture with various gases and liquids before injection, with potential routes including the vagina, rectum, intramuscular, subcutaneously, or intravenously Ozone can also be introduced via a process called “autohemotherapy”, in which blood is drawn from the patient, exposed to ozone and re-injected into the patient [75]
The United States Food and Drug Administration initially stated in 1976, and reiterated its position in 2006, “that when inhaled, ozone is a toxic gas which has no demonstrated safe medical application”, though their position statements primarily deal with its potential for causing inflammation and pulmonary edema in the lungs. Moreover there exist additional types of “oxygen therapy” involving hyperbaric oxygen, hydrogen peroxide, and various kinds of “oxygenated water”.
25.4. Extracorporeal Photochemotherapy (ECP)
Extracorporeal photochemotherapy (ECP) involves the addition of a photosensitizing drug 8-methoxypsoralen (8-MOP) into blood that is then treated with UVA light (320–360 nm). ECP was originally derived from the use of PUVA (psoralen and UVA) to treat psoriasis and other skin diseases. In the case of dermatology the psoralen was administered either orally (pills) or as a bath therapy. Often the whole body was exposed to light in a “PUVA box” containing UVA emitting fluorescent tube lights. ECP has been widely used as immunotherapy for cutaneous T cell lymphoma (CTCL) since it received US Food and Drug Administration (FDA) approval in 1988. As an apheresis-based immunomodulatory therapy which involves UVA irradiation of autologous peripheral blood mononuclear cells (PBMCs) exposed to the 8-MOP, there are a numbers of features of ECP that distinguish it from other immunologic therapy, which are beneficial in immune-stimulation against cancer and in the transplant setting as an immune-modulator; for induction of antigen presenting cells (APCS), to extracorporeal sequester and modify processed leukocytes, and so on. [76] It has used for treatment of other autoimmune-mediated disorders and organ allograft rejection, and is especially beneficial for cutaneous T-cell lymphoma (CTCL) and graft-versus host disease (GVHD). Both these indications require killing of lymphocytes.
25.4.1. ECP Therapy Treatment
The standard schedule of ECP treatment involves 2 successive days at 4 week intervals Tens of thousands of patients afflicted with CTCL, organ transplant rejection, GVHD, Crohn’s disease and type 1 diabetes [77–82], have received benefits from treatment with ECP since the first report of the systemic efficacy of by Edelson [83]. In his studies, he carried out treatment of skin manifestations in patients with cutaneous T-cell lymphoma (CTCL) and achieved a response rate of greater than 70% compared with other forms of treatment. Wollnia tested ECP in fourteen patients (all male) aged 38–72 years with CTCL of the mycosis fungoides type, stage IIa/IIb, and achieved a total response rate of 56% [84].
25.4.2. Mechanism of ECP
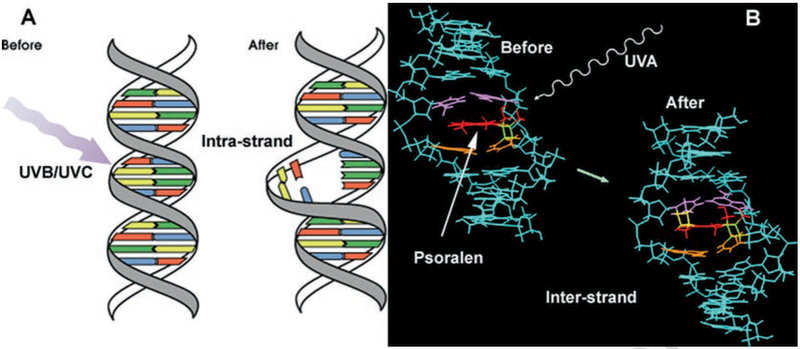
It is known that both UVC and UVB can damage DNA strands, as well as UVA activated 8-MOP. However the types of DNA lesions produced are very different for these two different kinds of UV-mediated DNA damage (Fig. 25.4). UVC and UVB both produce defined UV photo-products which are mainly the cyclobutane pyrimidine dimers (particularly TT dimers [85]) and pyrimidine-pyrimidone (6–4) photoproducts [86]. On the other hand, PUVA or ECPBM as it is known today cross-links the pyrimidine bases of DNA in complementary sister strands (inter- strand cross-links). These two different mechanisms of action are shown in Fig. 25.2. DNA damage by whatever means it is caused is likely to cause apoptosis of the extracorporally targeted lymphocytes [87]. ECP can treat erythrodermic CTCL by killing malignant CD8 T-cells but also by stimulating an immune response against thee malignant cells [88]. Two major effects of ECP have been well-confirmed: one is its immunostimulatory effects against neoplastic cells in CTCL; the other is its immunosuppressive effects against T-cell-mediated disorders such as GVHD and rejection in organ transplantation [89].
Fig. 25.4.
Comparison of DNA damage produced by (a) UVB or UVC (intra-strand cross-links), and (b) DNA damage produced by psoralens and UVA (ECP, inter-strand cross-links)
25.5. Modern Devices to Carry Out UBI
Although it is often said that UBI is “the cure that time forgot” [90, 91], it has not actually been completely forgotten. There are several companies, organizations and devices existing at the present time, which are being used or proposed (on a rather small scale) to carry out UBI, or as it often called “Photoluminescence Therapy (PT)”. Several websites provide information on UBI and PT. Perhaps one of the most comprehensive is (http://www.mnwelldir.org/docs/uv_light/uv_light3.htm) that provides a listing of practitioners located in USA that offer UBI to patients. UBI medical (http://ubimedical.com/about-us.html) also has a lot of information available. The web-site entitled “Infections cured” (http://infectionscured.com) is also worth checking out. Physicians UBI Awareness Center (http://drsubi.com) even has a video posted online comparing different kinds of UBI machines.
25.6. Conclusion
UV irradiation of blood was hailed as a miracle therapy for treating serious infections in the 1940s and 1950s. In an ironic quirk of fate, this historical time period coincided with the widespread introduction of penicillin antibiotics, which were rapidly found to be an even bigger medical miracle therapy. Moreover another major success of UBI, which was becoming increasingly used to treat polio, was also eclipsed by the introduction of the Salk polio vaccine in 1955 [91]. UBI had originally been an American discovery, but then was transitioned to being more studied in Russia and other eastern countries, which had long concentrated on physical therapies for many diseases, which were more usually treated with drugs in the West.
However in the last decade the problem of multi-antibiotic resistant bacteria has grown relentlessly. Multidrug-resistant (MDR) and pandrug resistant (PDR) bacterial strains and their related infections are emerging threats to public health throughout the world [92]. These are associated with approximately two-fold higher mortality rates and considerably prolonged hospital admissions [93]. The infections caused by antibiotic resistant strains are often exceptionally hard to treat due to the limited range of therapeutic options [94]. Recently in Feb 2015, the Review on Antimicrobial Resistance stated “Drug- resistant infections could kill an extra 10 million people across the world every year by 2050 if they are not tackled. By this date they could also cost the world around $100 trillion in lost output: more than the size of the current world economy, and roughly equivalent to the world losing the output of the UK economy every year, for 35 years” [95].
Sepsis is an uncontrolled response to infection involving massive cytokine release, widespread inflammation, which leads to blood clots and leaky vessels. Multi-organ failure can follow. Every year, severe sepsis strikes more than a million Americans. It is estimated that between 28–50% percent of these people die. Patients with sepsis are usually treated in hospital intensive care units with broad-spectrum antibiotics, oxygen and intravenous fluids to maintain normal blood oxygen levels and blood pressure. Despite decades of research, no drugs that specifically target the aggressive immune response that characterizes sepsis have been developed.
We would like to propose that UBI be reconsidered and re-investigated as a treatment for systemic infections caused by multi-drug resistant Gram-positive and Gram-negative bacteria in patients who are running out of (or who have already run out) of options. Patients at risk of death from sepsis could also be considered as candidates for UBI. Further research is required into the mechanisms of action of UBI. The present confusion about exactly what is happening during and after the treatment is playing a large role in the controversy about whether UBI could ever be a mainstream medical therapy, or must remain side-lined in the “alternative and complementary” category where it has been allowed to be forgotten for the last 50 years.
References
- 1.Frercksa J, Weberb H, Wiesenfeldt G (2009) Reception and discovery: the nature of Johann Wilhelm Ritter’s invisible rays. Stud Hist Philos Sci Part A 40:143–156 [Google Scholar]
- 2.Bonnet A (1845) Traite des Maladies des Articulations. Bailliere, Paris [Google Scholar]
- 3.Barth J, Kohler U (1992) Photodermatologie in Dresden-ein historischer Abriss Festschrift anlasslich des 75. Geburtstages von Prof. Dr. Dr. Dr. h.c. H.-E. Kleine-Natrop (1917–1985). Dresden [Google Scholar]
- 4.Downes A, Blunt TP (1877) Researches on the effect of light upon bacteria and other organisms. Proc R Soc Lond 26:488–500 [Google Scholar]
- 5.Finsen NR (1901) Phototherapy. Edward Arnold, London [Google Scholar]
- 6.Ude WH (1929) Ultraviolet radiation therapy in erysipela. Radiology 13:504 [Google Scholar]
- 7.Knott EK (1948) Development of ultraviolet blood irradiation. Am J Surg 76(2):165–171 [DOI] [PubMed] [Google Scholar]
- 8.Hancock VK, Knott EK (1934) Irradiated blood transfusion in the treatment of infections. Northwest Med 200(33) [Google Scholar]
- 9.Miley G, Christensen JA (1947) Ultraviolet blood irradiation further studies in acute infections. Am J Surg LxxIII (4):486–493 [DOI] [PubMed] [Google Scholar]
- 10.Miley G Uv irradiation non healing wounds. Am J Surg LXV(3):368–372, 1944 [Google Scholar]
- 11.Miley GP (1946) Recovery from botulism coma following ultraviolet blood irradiation. Rev Gastroenterol 13:17–19 [PubMed] [Google Scholar]
- 12.Miley GP, Seidel RE, Christensen JA (1946) Ultraviolet blood irradiation therapy of apparently intractable bronchial asthma. Arch Phys Med Rehabil 27:24–29 [PubMed] [Google Scholar]
- 13.Miley G (1943) The control of acute thrombophlebitis with ultraviolet blood irradiation therapy. Am J Surg 60:354–360 [Google Scholar]
- 14.Miley G (1944) Efficacy of ultraviolet blood irraidation therapy in the control of staphylococcemias. Am J Surg 64:313–322 [Google Scholar]
- 15.Miley G (1944) Ultraviolet blood irraidation therapy in acute poliomyelitis. Arch Phys Ther 25:651–656 [Google Scholar]
- 16.Miley G (1943) Disapperance of hemolytic staphylococcus aureus septicemia following ultraviolet blood irradiation therapy. Am J Surg 62:241–245 [Google Scholar]
- 17.Miley G (1942) The knott technic of ultraviolet blood irradiation in acute pyogenic infections. New York state Med 42:38–46 [Google Scholar]
- 18.Miley G (1944) Present status of ultraviolet blood irradiation (Knott technic). Arch Phys Ther 25:368–372 [Google Scholar]
- 19.Miley G (1942) Ultravilet blood irradiation. Arch Phys Ther 536(23) [Google Scholar]
- 20.Miley G (1942) Ultraviolet blood irradiation therapy (knott technic) in acute pyogenic infections. Am J Surg 493(57) [DOI] [PubMed] [Google Scholar]
- 21.Miley G (1943) The knott technic of ultraviolet blood irradiation as a control of infection in peritonitis. Rev Gastroenterol 1(10) [Google Scholar]
- 22.Miley GP, Seidel RE, Christensen JA (1943) Preliminary report of results observed in eighty cases of intractable bronchial asthma. Arch Phys Ther 533(24) [PubMed] [Google Scholar]
- 23.Barrett HA (1940) The irradiation of autotransfused blood by ultraviolet spectral energy. Result of therapy in 110 cases. Med clin N Am 721(24):1040 [Google Scholar]
- 24.Barrett HA (1943) Five years’ experience with hemo- irradiation according to the Knott technic. Am J Surg 61(1):42–53 [Google Scholar]
- 25.Rebbeck EW (1942) Double septicemia following prostatectomy treated by the knott technic of ultraviolet blood irradiation. Am J Surg 57(3):536–538 [Google Scholar]
- 26.Rebbeck EW (1943) Preoperative hemo-irradiations. Am J Surg 61(2):259–265 [Google Scholar]
- 27.Rebbeck EW (1941) Ultraviolet irradiation of autotransfused blood in the treatment of puerperal sepsis. Am J Surg 54(3):691–700 [Google Scholar]
- 28.Rebbeck EW (1942) Ultraviolet irradiation of autotransfused blood in the treatment of postabortional sepsis. Am J Surg 55(3):476–486 [Google Scholar]
- 29.Rebbeck EW (1943) Ultraviolet irradiation of blood in the treatment of escherichia coli septicemia. Arch Phys Ther 24:158–167 [Google Scholar]
- 30.Olney RC (1946) Ultraviolet blood irradiation in biliary disease; Knott method. Am J Surg 72:235–237 [DOI] [PubMed] [Google Scholar]
- 31.Olney RC (1947) Ultraviolet blood irradiation treatment of pelvic cellulitis; Knott method. Am J Surg 74(4):440–443 [DOI] [PubMed] [Google Scholar]
- 32.Olney RC (1955) Treatment of viral hepatitis with the Knott technic of blood irradiation. Am J Surg 90(3):402–409 [DOI] [PubMed] [Google Scholar]
- 33.Kabat IA, Sysa J, Zakrzewska I, Leyko W (1976) Effect of UV-irradiation of shifts of energy-rich phosphate compounds: ADP, ATP and AXP in human red blood cells represented by a trigonometrical polynomial. Zentralbl Bakteriol Orig B 162(3–4):393–401 [PubMed] [Google Scholar]
- 34.Vasil’eva ZF, Samoilova KA, Shtil’bans VI, Obolenskaia KD, Vitiuk NG (1991) Changes of immunosorption properties in the blood and its components at various times after UV-irradiation. Gematol Transfuziol 36(5):26–27 [PubMed] [Google Scholar]
- 35.Samoilova KA, Snopov SA, Belisheva NK, Kukui LM, Ganelina IE (1987) Functional and structural changes in the surface of human erythrocytes after irradiation by different wave lengths of UV rays. III. The immediate effect of the autotransfusion of UV-irradiated blood. Tsitologiia 29(7):810–817 [PubMed] [Google Scholar]
- 36.Snopov SA, Aritsishevskaia RA, Samoilova KA, Marchenko AV, Dutkevich IG (1989) Functional and structural changes in the surface of human erythrocytes following irradiation with ultraviolet rays of various wave lengths. V. Modification of the glycocalyx in autotransfusions of UV-irradiated blood. Tsitologiia 31(6):696–705 [PubMed] [Google Scholar]
- 37.Ichiki H, Sakurada H, Kamo N, Takahashi TA, Sekiguchi S (1994) Generation of active oxygens, cell deformation and membrane potential changes upon UV-B irradiation in human blood cells. Biol Pharm Bull 17(8):1065–1069 [DOI] [PubMed] [Google Scholar]
- 38.Savage JE, Theron AJ, Anderson R (1993) Activation of neutrophil membrane-associated oxidative metabolism by ultraviolet radiation. J Invest Dermatol 101(4):532–536 [DOI] [PubMed] [Google Scholar]
- 39.Ivanov EM, Kapshienko IN, Tril NM (1989) Effect of the UV irradiation of autologous blood on the humoral link in the immune response of patients with chronic inflammatory processes. Vopr Kurortol Fizioter Lech Fiz Kult 1:45–47 [PubMed] [Google Scholar]
- 40.Artiukhov VF, Gusinskaia VV, Mikhileva EA (2005) Level of nitric oxide and tumor necrosis factor-alpha production by human blood neutrophils under UV-irradiation. Radiats Biol Radioecol 45(5):576–580 [PubMed] [Google Scholar]
- 41.Zor’kina AV, Inchina VI, Kostin Ia V (1996) Effect of UV-irradiation of blood on the course of adaptation to conditions of hypodynamia. Patol Fiziol Eksp Ter 2:22–24 [PubMed] [Google Scholar]
- 42.Deeg HJ (1988) Ultraviolet irradiation in transplantation biology. Manipulation of immunity and immunogenicity. Transplantation 45(5):845–851 [DOI] [PubMed] [Google Scholar]
- 43.Arlett CF, Lowe JE, Harcourt SA et al. (1993) Hypersensitivity of human lymphocytes to UV-B and solar irradiation. Cancer Res 53(3):609–614 [PubMed] [Google Scholar]
- 44.Teunissen MB, Sylva-Steenland RM, Bos JD (1993) Effect of low-dose ultraviolet-B radiation on the function of human T lymphocytes in vitro. Clin Exp Immunol 94(1):208–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schieven GL, Ledbetter JA (1993) Ultraviolet radiation induces differential calcium signals in human peripheral blood lymphocyte subsets. J Immunother Emphasis Tumor Immunol 14(3):221–225 [DOI] [PubMed] [Google Scholar]
- 46.Spielberg H, June CH, Blair OC, Nystrom-Rosander C, Cereb N, Deeg HJ (1991) UV irradiation of lymphocytes triggers an increase in intracellular Ca2+ and prevents lectin-stimulated Ca2+ mobilization: evidence for UV- and nifedipine-sensitive Ca2+ channels. Exp Hematol 19(8):742–748 [PubMed] [Google Scholar]
- 47.Pamphilon DH, Corbin SA, Saunders J, Tandy NP (1989) Applications of ultraviolet light in the preparation of platelet concentrates. Transfusion 29(5):379–383 [DOI] [PubMed] [Google Scholar]
- 48.Lindahl-Kiessling K, Safwenberg J (1971) Inability of UV-irradiated lymphocytes to stimulate allogeneic cells in mixed lymphocyte culture. Int Arch Allergy Appl Immunol 41(5):670–678 [DOI] [PubMed] [Google Scholar]
- 49.Slater LM, Murray S, Liu J, Hudelson B (1980) Dissimilar effects of ultraviolet light on HLA-D and HLA-DR antigens. Tissue Antigens 15(5):431–435 [DOI] [PubMed] [Google Scholar]
- 50.Aprile J, Deeg HJ (1986) Ultraviolet irradiation of canine dendritic cells prevents mitogen-induced cluster formation and lymphocyte proliferation. Transplantation 42(6):653–660 [DOI] [PubMed] [Google Scholar]
- 51.Kovacs E, Weber W, Muller H (1984) Age-related variation in the DNA-repair synthesis after UV-C irradiation in unstimulated lymphocytes of healthy blood donors. Mutat Res 131(5–6):231–237 [DOI] [PubMed] [Google Scholar]
- 52.Genter EI, Zhestianikov VD, Mikhel’son VM, Prokof’eva VV (1984) DNA repair in the UV irradiation of human peripheral blood lymphocytes (healthy donors and xeroderma pigmentosum patients) in relation to the dedifferentiation process in phytohemagglutinin exposure. Tsitologiia 26(5):599–604 [PubMed] [Google Scholar]
- 53.Genter EI, Mikhel’son VM, Zhestianikov VD (1989) The modifying action of methylmethane sulfonate on unscheduled DNA synthesis in the UV irradiation of human peripheral blood lymphocytes. Radiobiologiia 29(4):562–564 [PubMed] [Google Scholar]
- 54.Volgareva EV, Volgarev AP, Samoilova KA (1990) The effect of UV irradiation and of UV-irradiated autologous blood on the functional state of human peripheral blood lymphocytes. Tsitologiia 32(12):1217–1224 [PubMed] [Google Scholar]
- 55.Deeg HJ, Aprile J, Graham TC, Appelbaum FR, Storb R (1986) Ultraviolet irradiation of blood prevents transfusion-induced sensitization and marrow graft rejection in dogs. Blood 67(2):537–539 [PubMed] [Google Scholar]
- 56.Oluwole SF, Iga C, Lau H, Hardy MA (1985) Prolongation of rat heart allografts by donor-specific blood transfusion treated with ultraviolet irradiation. J Heart Transplant 4(4):385–389 [PubMed] [Google Scholar]
- 57.Vasil’eva ZF, Shtil’bans VI, Samoilova KS, Obolenskaia KD (1989) The activation of the immunosorptive properties of blood during its UV irradiation at therapeutic doses. Biull Eksp Biol Med 108(12):689–691 [PubMed] [Google Scholar]
- 58.Green MH, Waugh AP, Lowe JE, Harcourt SA, Cole J, Arlett CF (1994) Effect of deoxyribonucleosides on the hypersensitivity of human peripheral blood lymphocytes to UV-B and UV-C irradiation. Mutat Res 315(1):25–32 [DOI] [PubMed] [Google Scholar]
- 59.Samoilova KA, Obolenskaia KD, Freidlin IS (1987) Changes in the leukocyte phagocytic activity of donor blood after its UV irradiation. II. Simulation of the effect of the autotransfusion of UV-irradiated blood. Tsitologiia 29(9):1048–1055 [PubMed] [Google Scholar]
- 60.Obolenskaia KD, Freidlin IS, Samoilova KA (1987) Changes in the leukocyte phagocytic activity of donor blood after its UV irradiation. I. Its relation to the irradiation dose and initial level of phagocytic activity. Tsitologiia 29(8):948–954 [PubMed] [Google Scholar]
- 61.Simon JC, Tigelaar RE, Bergstresser PR, Edelbaum D, Cruz PD Jr (1991) Ultraviolet B radiation converts Langerhans cells from immunogenic to tolerogenic antigen-presenting cells. Induction of specific clonal anergy in CD4+ T helper 1 cells. J Immunol 146(2):485–491 [PubMed] [Google Scholar]
- 62.Pamphilon DH, Potter M, Cutts M et al. (1990) Platelet concentrates irradiated with ultraviolet light retain satisfactory in vitro storage characteristics and in vivo survival. Br J Haematol 75(2):240–244 [DOI] [PubMed] [Google Scholar]
- 63.Fiebig E, Lane TA (1994) Effect of storage and ultraviolet B irradiation on CD14-bearing antigen- presenting cells (monocytes) in platelet concentrates. Transfusion 34(10):846–851 [DOI] [PubMed] [Google Scholar]
- 64.Kahn RA, Duffy BF, Rodey GG (1985) Ultraviolet irradiation of platelet concentrate abrogates lymphocyte activation without affecting platelet function in vitro. Transfusion 25(6):547–550 [DOI] [PubMed] [Google Scholar]
- 65.Andreu G, Boccaccio C, Klaren J et al. (1992) The role of UV radiation in the prevention of human leukocyte antigen alloimmunization. Transfus Med Rev 6(3):212–224 [DOI] [PubMed] [Google Scholar]
- 66.Tandy NP, Pamphilon DH (1991) Platelet transfusions irradiated with ultraviolet-B light may have a role in reducing recipient alloimmunization. Blood Coagul Fibrinolysis 2(2):383–388 [DOI] [PubMed] [Google Scholar]
- 67.Roshchupkin DI, Murina MA (1998) Free-radical and cyclooxygenase-catalyzed lipid peroxidation in membranes of blood cells under UV irradiation. Membr Cell Biol 12(2):279–286 [PubMed] [Google Scholar]
- 68.Gorog P (1991) Activation of human blood monocytes by oxidized polyunsaturated fatty acids: a possible mechanism for the generation of lipid peroxides in the circulation. Int J Exp Pathol 72(2):227–237 [PMC free article] [PubMed] [Google Scholar]
- 69.Salmon S, Maziere JC, Santus R, Morliere P, Bouchemal N (1990) UVB-induced photoperoxidation of lipids of human low and high density lipoproteins. A possible role of tryptophan residues. Photochem Photobiol 52(3):541–545 [DOI] [PubMed] [Google Scholar]
- 70.Salmon S, Haigle J, Bazin M, Santus R, Maziere JC, Dubertret L (1996) Alteration of lipoproteins of suction blister fluid by UV radiation. J Photochem Photobiol B 33(3):233–238 [DOI] [PubMed] [Google Scholar]
- 71.Artyukhov VG, Iskusnykh AY, Basharina OV, Konstantinova TS (2005) Effect of UV irradiation on functional activity of donor blood neutrophils. Bull Exp Biol Med 139(3):313–315 [DOI] [PubMed] [Google Scholar]
- 72.Dong Y, Shou T, Zhou Y, Jiang S, Hua X (2000) Ultraviolet blood irradiation and oxygenation affects free radicals and antioxidase after rabbit spinal cord injury. Chin Med J 113(11):991–995 [PubMed] [Google Scholar]
- 73.Calabrese EJ, Dhawan G, Kapoor R, Iavicoli I, Calabrese V (2015) HORMESIS: a fundamental concept with widespread biological and biomedical applications. Gerontology 62:530. [DOI] [PubMed] [Google Scholar]
- 74.Calabrese EJ (2014) Hormesis: from mainstream to therapy. J Cell Commun Signal 8(4):289–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zaky S, Kamel SE, Hassan MS et al. (2011) Preliminary results of ozone therapy as a possible treatment for patients with chronic hepatitis C. J Altern Complement Med 17(3):259–263 [DOI] [PubMed] [Google Scholar]
- 76.Edelson RL (2014) Mechanistic insights into extracorporeal photochemotherapy: efficient induction of monocyte-to-dendritic cell maturation. Transfus Apher Sci 50(3):322–329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Child FJ, Ratnavel R, Watkins P et al. (1999) Extracorporeal photopheresis (ECP) in the treatment of chronic graft-versus-host disease (GVHD). Bone Marrow Transplant 23(9):881–887 [DOI] [PubMed] [Google Scholar]
- 78.Atta M, Papanicolaou N, Tsirigotis P (2012) The role of extracorporeal photopheresis in the treatment of cutaneous T-cell lymphomas. Transfus Apher Sci 46(2):195–202 [DOI] [PubMed] [Google Scholar]
- 79.De Waure C, Capri S, Veneziano MA et al. (2015) Extracorporeal Photopheresis for second-line treatment of chronic graft-versus-host diseases: Results from a health technology assessment in Italy. Value Health 18(4):457–466 [DOI] [PubMed] [Google Scholar]
- 80.Patel J, Klapper E, Shafi H, Kobashigawa JA (2015) Extracorporeal photopheresis in heart transplant rejection. Transfus Apher Sci 52(2):167–170 [DOI] [PubMed] [Google Scholar]
- 81.Reinisch W, Knobler R, Rutgeerts PJ et al. (2013) Extracorporeal photopheresis (ECP) in patients with steroid-dependent Crohn’s disease: an open-label, multicenter, prospective trial. Inflamm Bowel Dis 19(2):293–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ludvigsson J, Samuelsson U, Ernerudh J, Johansson C, Stenhammar L, Berlin G (2001) Photopheresis at onset of type 1 diabetes: a randomised, double blind, placebo controlled trial. Arch Dis Child 85(2):149–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Edelson R, Berger C, Gasparro F et al. (1987) Treatment of cutaneous T-cell lymphoma by extracorporeal photochemotherapy. Preliminary results. N Engl J Med 316(6):297–303 [DOI] [PubMed] [Google Scholar]
- 84.Wollina U, Looks A, Meyer J et al. (2001) Treatment of stage II cutaneous T-cell lymphoma with interferon alfa-2a and extracorporeal photochemotherapy: a prospective controlled trial. J Am Acad Dermatol 44(2):253–260 [DOI] [PubMed] [Google Scholar]
- 85.Niggli HJ, Rothlisberger R (1988) Cyclobutane-type pyrimidine photodimer formation and induction of ornithine decarboxylase in human skin fibroblasts after UV irradiation. J Invest Dermatol 91(6):579–584 [DOI] [PubMed] [Google Scholar]
- 86.Vendrell-Criado V, Rodriguez-Muniz GM, Lhiaubet- Vallet V, Cuquerella MC, Miranda MA (2016) The (6–4) Dimeric Lesion as a DNA Photosensitizer. Chem Phys Chem 17(13):1979–1982 [DOI] [PubMed] [Google Scholar]
- 87.Santella RM, Dharmaraja N, Gasparro FP, Edelson RL (1985) Monoclonal antibodies to DNA modified by 8-methoxypsoralen and ultraviolet A light. Nucleic Acids Res 13(7):2533–2544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Heald P, Rook A, Perez M et al. (1992) Treatment of erythrodermic cutaneous T-cell lymphoma with extra-corporeal photochemotherapy. J Am Acad Dermatol 27(3):427–433 [DOI] [PubMed] [Google Scholar]
- 89.Hart JW, Shiue LH, Shpall EJ, Alousi AM (2013) Extracorporeal photopheresis in the treatment of graft-versus-host disease: evidence and opinion. Ther Adv Hematol 4(5):320–334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rowen RJ (1996) Ultraviolet blood irradiation therapy (Photo-Oxidation) the cure that time forgot. Int J Biosocial Med Research 14(2):115–132 [Google Scholar]
- 91.Wu X, Hu X, Hamblin MR (2016) Ultraviolet blood irradiation: is it time to remember “the cure that time forgot”? J Photochem Photobiol B 157:89–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kraus CN (2008) Low hanging fruit in infectious disease drug development. Curr Opin Microbiol 11(5):434–438 [DOI] [PubMed] [Google Scholar]
- 93.Munoz-Price LS, Poirel L, Bonomo RA et al. (2013) Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis 13(9):785–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Yoneyama H, Katsumata R (2006) Antibiotic resistance in bacteria and its future for novel antibiotic development. Biosci Biotechnol Biochem 70(5):1060–1075 [DOI] [PubMed] [Google Scholar]
- 95.O’neill J (2015) Review on antimicrobial resistance: tackling a global health crisis. Initial Steps