Abstract
Background
Iron metabolism disorders have been associated with an increased risk of cardiovascular events. However, the prognostic impact on patients (pts) with acute coronary syndrome (ACS) has yet to be clarified.
Objective
To determine the prognostic value of serum iron and ferritin levels in pts with ACS in the short and long-term.
Methods
Consecutive pts admitted to a coronary care unit with a diagnosis of ACS, for a period of 2 years, were evaluated. The population was divided into tertiles of serum iron and ferritin distribution. The primary adverse events were the occurrence of in-hospital death or heart failure (HF) and death or HF at 1 year of follow-up.
Results
We studied 280 pts (73% males; mean age 68 ± 13 years). The mean levels of serum iron and ferritin were 59 ± 34 mcg/dL and 205 ± 185 ng/mL, respectively. Patients included in the 1st tertile of serum iron (≤ 40 mcg/dL) had a higher rate of adverse events, in-hospital and after 1 year. Lower and higher levels of ferritin (1st and 3rd tertiles, ≤ 110; >219 ng/ml, respectively) were associated with a higher incidence of HF during hospitalization and death at 1 year. A ferritin value >316 ng /mL was an independent risk factor for death at 1 year (adjusted OR: 14; 95%CI: 2.6 to 75.9).
Conclusion
In this population, iron metabolism alterations were associated with a higher rate of adverse events and higher ferritin levels constituted an independent mortality predictor in the long-term.
Keywords: Acute Coronary Syndrome, Iron Metabolism Disorders, Prognostic
Introduction
Iron is an important micronutrient in cell metabolism, necessary for body homeostasis.1 Iron deficiency affects more than one-third of the world’s population and is often a chronic disease complication (inflammatory bowel disease, chronic kidney disease, Parkinson's disease, rheumatoid arthritis) and plays a role in the sympathetic nervous system activation, as well as in ventricular hypertrophy and dilation.1
According to the EMPIRE study, 1 in 3 Portuguese individuals have iron deficiency.2 Iron deficiency is an important comorbidity factor in chronic heart failure (HF), as well as in HF decompensation periods, regardless of the presence of anemia.1,3
The CONFIRM-HF study demonstrated a favorable effect on the functional capacity and quality of life of HF patients, as well as the reduction in the number of hospitalizations for decompensated HF in patients submitted to intravenous iron therapy.1,3,4
Meanwhile, the debate between the role of ferritin and iron in the atherosclerosis metabolism persists, and the function of iron metabolism in coronary disease is unclear. Although small, there are studies that consider iron a proatherogenic agent for its role in free radical formation, with consequent oxidative stress at the vascular level.5,6
Studies in animals have confirmed that chronic iron administration accelerates thrombus formation.6 On the other hand, low iron levels may be associated with ischemia and major cardiovascular events (MACE) in patients with acute coronary syndrome (ACS).5
In a recent study, Steen et al. failed to establish any association between iron and the risk of myocardial infarction, as well as recurrent ischemic events.7 Ferritin is considered by some studies as a cytoprotective agent, yet multivariate analyses have shown that low ferritin levels are predictors of 30-day MACE in patients with ACS.5,8
Despite the several studies, the controversy over the role of iron in ACS persists, and the true correlation between iron and atherosclerotic disease is yet to be determined.
In the present study, we aim to determine the short- and long-term prognostic value of serum iron and ferritin levels in patients admitted for ACS.
Methods
Sample
The sample was retrospectively evaluated and consisted of consecutive patients admitted to a Coronary Unit with an ACS diagnosis between June 2011 and June 2013. Patients whose iron profile was not determined during hospitalization were excluded.
Variables
The population was characterized according to their baseline characteristics (age and gender); clinical characteristics (personal history, type of ACS, Killip Class, LV ejection fraction) and laboratory test results (serum levels of creatinine, BNP, hemoglobin), and was grouped according to the tertiles of distribution of serum iron (1st tertile ≤ 40; 2nd tercile > 40 and ≤ 67; 3rd tertile >67 mcg/dL) and ferritin (1st tertile ≤ 110; 2nd tertile < 110 and ≤ 219; 3rd tertile >219 ng/mL).
The cut-off values of serum iron and serum ferritin were, respectively, 60-180 mcg/dL and 10-120 ng / mL, according to the hospital laboratory.
End-point
The short- and long-term prognoses were assessed based on primary adverse events: in-hospital death and 1-year death; in-hospital heart failure (Killip Class ≥ 2 and BNP ≥ 400 pg/mL) and 1-year follow-up (ejection fraction < 50% and NYHA Class ≥ 2). Other secondary endpoints were reinfarction and ischemic cerebrovascular accident at 1 year of follow-up.
Statistical analysis
The program IBM SPSS Statistics, version 20 for Windows 8, was used to perform the statistical analysis. Continuous variables were shown as mean ± standard deviation and compared according to iron and ferritin tertiles by ANOVA. Categorical variables were shown as absolute values and/or percentages and compared using the chi-square test. The associations were considered statistically significant in the presence of a p-value < 0.05. Continuous variables were associated with primary adverse events (Death and HF) through receiver operating characteristic (ROC) curves. The predictive value of iron and ferritin levels over the risk of in-hospital and 1-year adverse events was determined by the odds ratio, with a 95% confidence interval (95%CI).
Results
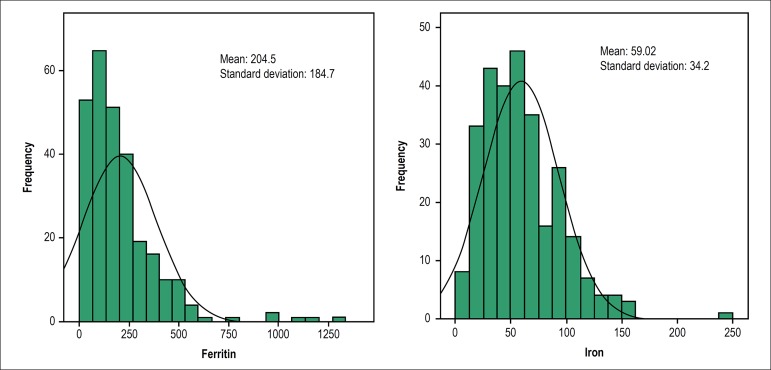
The baseline, clinical and laboratory characteristics of the total population and according to serum iron and ferritin tertiles are shown in Tables 1 and 2. A total of 280 patients were studied (73% males) with a mean age of 68 ± 13 years. The distribution of serum iron and ferritin levels is shown in figure 1.
Table 1.
Basal and clinical characteristics, according to iron and ferritin tertiles
| Basal characteristics | Population n = 280 | 1st iron tertile (≤ 40 mcg/dL) | 2nd iron tertile (> 40 or ≤ 67 mcg/dL) | 3rd iron tertile (> 67 mcg/dL) | p value | 1st ferritin tertile (≤ 110 ng/mL) | 2nd ferritin tertile (>110 or ≤ 219 ng/mL) | 3rd ferritin tertile (> 219 ng/mL) | p value |
|---|---|---|---|---|---|---|---|---|---|
| Age, years | 68 ± 13 | 69 ± 15 | 69 ± 12 | 67 ± 13 | < 0.001 | 73 ± 12 | 66 ± 14 | 67 ± 13 | 0.001 |
| Male gender | 204 (73) | 63 (23) | 73 (26) | 68 (24) | 0.12 | 53 (19) | 68 (24) | 78 (28) | 0.12 |
| Personal history | |||||||||
| SAH | 186 (66.4) | 56 (20) | 70 (25) | 60 (21) | 0.12 | 69 (25) | 58 (21) | 57 (20) | 0.12 |
| Diabetes mellitus | 90 (32) | 36 (13) | 30 (11) | 24 (9) | 0.21 | 32 (11.4) | 32 (11.4) | 26 (9.3) | 0.69 |
| Dyslipidemia | 140 (50) | 37 (13) | 59 (21) | 44 (16) | 0.87 | 46 (16) | 49 (18) | 43 (15) | 0.34 |
| History of AMI | 44 (16) | 10 (3.6) | 18 (6.4) | 16 (6) | 0.21 | 18 (6.4) | 15 (5.3) | 11 (4) | 0.42 |
| History of HF | 9 (3.2) | 2 (0.7) | 5 (1.8) | 2 (0.7) | 0.34 | 2 (0.7) | 3 (1.1) | 4 (1.4) | 0.68 |
| Renal failure | 21 (8) | 8 (3) | 7 (2.5) | 6 (2) | 0.8 | 9 (3.2) | 6 (2) | 6 (2) | 0.6 |
| PAD | 11 (4) | 3 (1) | 3 (1) | 5 (1.8) | 0.7 | 8 (3) | 3 (1) | 0 | 0.7 |
| ACS type | |||||||||
| Unstable angina | 12 (4.3) | 3 (1) | 2 (0.7) | 7 (2.5) | 0.21 | 7 (2.5) | 3 (1) | 2 (0.7) | 0.85 |
| STEMI | 125 (45) | 50 (18) | 43 (15.3) | 32 (11) | 35 (13) | 41 (15) | 45 (16) | ||
| NSTEMI | 122 (44) | 36 (13) | 41 (15) | 45 (16) | 41 (15) | 40 (14) | 40 (14) | ||
| Undetermined AMI | 21 (8) | 6 (2.1) | 6 (2.1) | 9 (3.2) | 9 (3.2) | 10 (4) | 2 (0.7) |
Results expressed as n (%) or mean ± median. SAH: systemic arterial hypertension; AMI: acute myocardial infarction; HF: heart failure; PAD: peripheral arterial disease; ACS: acute coronary syndrome; STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction.
Table 2.
Clinical and laboratory characteristics, according to iron and ferritin tertiles
| Clinical presentation | Population n = 280 | 1st iron tertile (≤ 40 mcg/dL) | 2nd iron tertile (> 40 or ≤ 67 mcg/dL) | 3rd iron tertile (> 67 mcg/dL) | p value | 1st ferritin tertile (≤ 110 ng/mL) | 2nd ferritin tertile (>110 or ≤ 219 ng/mL) | 3rd ferritin tertile (> 219 ng/mL) | p value |
|---|---|---|---|---|---|---|---|---|---|
| Killip Class I | 244 (87) | 74 (27) | 83 (30) | 87 (31) | 0.12 | 73 (26) | 88 (31.4) | 78 (28) | 0.23 |
| Killip Class II | 18 (6.4) | 11 (4) | 4 (1.4) | 3 (1) | 14 (5) | 2 (0.7) | 2 (0.7) | ||
| Killip Class III | 11 (3.9) | 4 (1.4) | 4 (1.4) | 3 (1) | 3 (1) | 2 (0.7) | 6 (2.1) | ||
| Killip Class IV | 7 (2.5) | 6 (2.1) | 4 (1.4) | 0 | 2 (0.7) | 2 (0.7) | 3 (1) | ||
| Ejection fraction classification | |||||||||
| LVEF > 50% | 157 (69) | 42 (15) | 58 (21) | 57 (20) | 0.08 | 43 (15) | 59 (21) | 54 (19) | 0.7 |
| LVEF 41-50% | 23 (10) | 16 (6) | 3 (1) | 4 (1.4) | 7 (2.5) | 9 (3) | 7 (2.5) | ||
| LVEF 30-40% | 38 (17) | 16 (6) | 14 (5) | 8 (3) | 16 (6) | 8 (3) | 11 (4) | ||
| LVEF < 30% | 11 (5) | 4 (1.4) | 4 (1.4) | 3 (1) | 6 (2.1) | 2 (0.7) | 3 (1) | ||
| Laboratory assessment | |||||||||
| Creatinine, mg/dL | 1.08 ± 0.9 | 1.2 ± 1.2 | 1.05 ± 0.6 | 0.9± 1.8 | 0.9 | 1.1 ± 0.7 | 1 ± 0.6 | 1.1 ± 1.2 | 0.8 |
| BNP, pg/mL | 331.6 ± 499 | 567 ± 712 | 266 ± 371 | 180 ± 212 | < 0.001 | 488 ± 684 | 204 ± 270 | 346 ± 427 | 0.001 |
| Hemoglobin, g/dL | 13.1 ± 2 | 11.8 ± 2.2 | 13.4 ± 2 | 14 ± 16 | < 0.001 | 12 ± 2.2 | 14 ± 1.7 | 14 ± 2 | <0.001 |
Results expressed as n (%) or mean ± median. LVEF: left ventricular ejection fraction; BNP: brain natriuretic peptide.
Figure 1.
Distribution of serum levels of iron and ferritin in the population.
The main diagnosis at admission was ST-segment elevation myocardial infarction (STEMI) in 45% (n = 125) and non-ST-segment elevation myocardial infarction (NSTEMI) in 44% (n = 122) of the patients.
Approximately 87% of the patients (n = 244) were admitted with Killip I Class, and only 2.5% (n = 7) were admitted in cardiogenic shock. In 11 (5%) patients, the transthoracic echocardiography showed severe left ventricular systolic dysfunction.
Regarding the short-term prognosis: 1.1% (n = 3) of the patients died during hospitalization and 28% (n = 79) showed evidence of heart failure. Regarding the long-term impact, approximately 7% (n = 19) of the patients died in the first year of follow-up and 12% (n = 33) developed HF criteria during the clinical follow-up (Tables 3 and 4).
Table 3.
Short-term and long-term events, according to iron levels
| Event | 1st iron tertile (≤ 40 mcg/dL) | 2nd iron tertile (> 40 or ≤ 67 mcg/dL) | 3rd iron tertile (> 67 mcg/dL) | p value |
|---|---|---|---|---|
| In-hospital death | 3 | 0 | 0 | 0.04 |
| Death at 1 year | 12 | 4 | 3 | 0.02 |
| In-hospital HF | 46 | 19 | 14 | < 0.001 |
| HF at 1 year | 17 | 9 | 7 | 0.08 |
| Reinfarction at 1 year | 3 | 3 | 2 | 0.9 |
| CVA at 1 year | 0 | 1 | 1 | 0.8 |
HF: heart failure; CVA: cerebrovascular accident.
Table 4.
Short-term and long-term events, according to ferritin levels
| Event | 1st ferritin tertile (≤ 110 ng/mL) | 2nd ferritin tertile (> 110 or ≤ 219 ng/mL) | 3rd ferritin tertile (> 219 ng/mL) | p value |
|---|---|---|---|---|
| In-hospital death | 1 | 1 | 1 | 0.8 |
| Death at 1 year | 9 | 2 | 8 | 0.04 |
| In-hospital HF | 38 | 16 | 25 | 0.001 |
| HF at 1 year | 13 | 9 | 11 | 0.1 |
| Reinfarction at 1 year | 4 | 3 | 1 | 0.1 |
| CVA at 1 year | 1 | 1 | 0 | 0.5 |
HF: heart failure; CVA: cerebrovascular accident.
The multivariate regression analysis showed that a ferritin value > 316 ng/mL is an independent risk predictor for 1-year death (adjusted OR:14; 95%CI: 2.6-75.9, p = 0.0023). (Table 5)
Table 5.
Establishment of independent variables associated with cardiovascular events in the short and long-term.
| Variable | Odds ratio | 95%CI | p value |
|---|---|---|---|
| Death at 1 year | |||
| Iron ≤ 36 mcg/dL | 2.6 | 0.7-9 | 0.13 |
| Ferritin > 316 ng/mL | 14 | 2.5-75 | 0.0027 |
| Hemoglobin ≤ 11.7 g/dL | 17 | 3-102 | 0.0016 |
| Age > 70 year | 21 | 2-237 | 0.01 |
| In-hospital death | |||
| Iron ≤ 14 mcg/dL | 3.9 | 1-9 | 0.99 |
| Ferritin > 104 ng/ml | 1.17 | 2-70 | 0.99 |
| Heart failure at 1 year | |||
| Iron ≤ 40 mcg/dL | 0.9 | 0.2-3.9 | 0.9 |
| Ferritin ≤ 157 ng/mL | 0.36 | 0.06-2.1 | 0.2 |
| In-hospital heart failure | |||
| Iron ≤ 30 mcg/dL | 1.8 | 0.6-5.3 | 0.3 |
| Ferritin ≤ 116 ng/mL | 0.5 | 0.15-1.8 | 0.3 |
Values determined from the Receiver Operating Characteristic curves. 95% CI: 95% confidence interval.
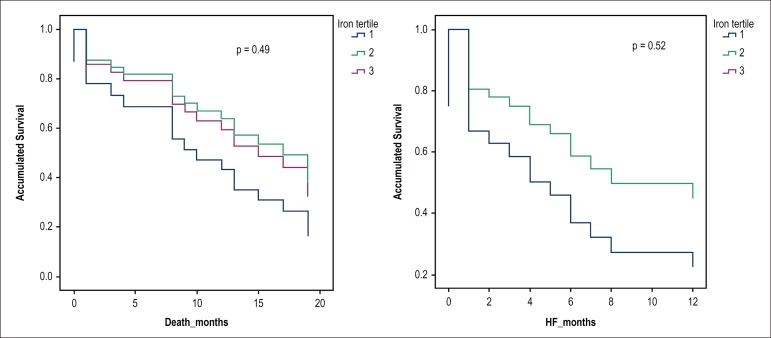
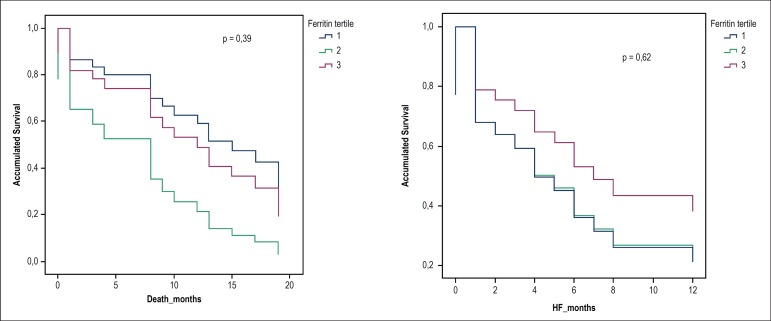
The survival curves for Death and HF according to iron and ferritin tertiles showed no statistical difference. (Figures 2 and 3)
Figure 2.
Survival curves according to iron tertiles.
Figure 3.
Survival curves according to ferritin tertiles.
Discussion
Iron deficiency is a common and clinically relevant heart failure comorbidity, being associated with a worse prognosis. Some studies (CONFIRM-HF) have shown the benefit of iron correction in terms of quality of life and exercise tolerance in patients with HF and decreased systolic function.1,3
According to current European recommendations for HF treatment, intravenous iron is indicated with Class IIa in symptomatic patients with decreased systolic function and iron deficiency (serum ferritin levels <100ng / mL or ferritin level between 100-299 ng / mL and transferrin saturation <20%).3 On the other hand, the role of iron and ferritin is uncertain in the context of atherosclerotic disease and ACS.5-8
In this population, the type of ACS, as well as its clinical presentation regarding Killip class and LV systolic function impairment were not statistically influenced by iron or ferritin levels.
Age had a statistical impact on serum iron and ferritin levels, which may be explained by an iron-poor diet, impaired intestinal absorption that increases with age, and the presence of more comorbidities that interfere with iron metabolism.
Lower levels of iron and ferritin were statistically associated with lower Hb levels, as expected, with a mean value of 12 g/dL.
Mean BNP values >450 pg/mL were statistically associated with the 1st tertiles of iron and ferritin, which is consistent with several studies in the HF scenario, in which iron and ferritin deficiencies were found as a frequent comorbidity of HF.1,3
Alberto Dominguez-Rodriguez demonstrated that low iron levels may be associated with major cardiovascular events (MACE) in patients with ACS.5 In this population of ACS patients, alterations in iron metabolism were associated with a higher occurrence of adverse events.
Iron levels ≤ 40 mcg/dL had a negative impact regarding mortality and in-hospital HF, with statistical significance; however, serum iron levels were not an independent risk factor for the occurrence of cardiovascular events.
Is ferritin a cytoprotective or atherogenic agent or, on the other hand, is its deficiency a predictor of major cardiovascular events in patients with ACS? The literature results are not in agreement regarding the role of ferritin in atherosclerosis.3 Patients with ACS and major cardiovascular events (MACE) showed low levels of ferritin versus patients with ACS without adverse events.5
In our population, regarding ferritin levels, the 1st and 3rd tertiles were associated with the occurrence of more adverse events, with statistical significance in terms of in-hospital HF and 1-year death. A serum ferritin level of 316 ng/mL was considered an independent risk predictor for 1-year death (adjusted OR:14; 95%CI: 2.6-75.9, p = 0.0023), which differs from the conclusions of some studies, as previously mentioned. The serum ferritin level was not an independent risk predictor for heart failure.
Limitations
The present study is subject to the limitations associated with all retrospective, non-randomized analyses carried out in a single center.
Conclusion
In this population of patients with ACS, iron metabolism alterations were associated with a higher occurrence of adverse events. Elevated ferritin levels were an independent predictor of long-term mortality. Serum iron levels did not constitute an independent risk factor for the occurrence of cardiovascular events.
Additional studies are required to clarify whether serum iron or ferritin levels constitute a vascular injury/prognostic marker in ACS patients and establish the “actual” role of iron and ferritin in this type of cardiovascular disease.
Footnotes
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors.
Author contributions
Conception and design of the research: Duarte T, Gonçalves S; Acquisition of data: Duarte T, Sá C, Rodrigues R, Marinheiro R, Fonseca M; Analysis and interpretation of the data, statistical analysis and writing of the manuscript: Duarte T; Critical revision of the manuscript for intellectual content: Gonçalves S, Seixo F, Caria R.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
- 1.Jankowska EA, von Haehling S, Anker SD, Macdougall IC, Ponikowski P. Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J. 2013;34(11):816–829. doi: 10.1093/eurheartj/ehs224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fonseca C, Marques F, Robalo Nunes A, Belo A, Brilhante D, Cortez J. Prevalence of anaemia and iron deficiency in Portugal: the EMPIRE study. Intern Med J. 2016;46(4):470–478. doi: 10.1111/imj.13020. [DOI] [PubMed] [Google Scholar]
- 3.Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. ESC Scientific Document Group 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure; The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37(27):2129–2200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 4.Ponikowski P, van Veldhuisen DJ, Comin-Colet J, Ertl G, Komajda M, Mareev V, et al. CONFIRM-HF Investigators Beneficial effects of long-term intravenous iron therapy with ferric carboxymaltose in patients with symptomatic heart failure and iron deficiency. Eur Heart J. 2015;36(11):657–668. doi: 10.1093/eurheartj/ehu385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dominguez-Rodriguez A, Abreu-Gonzalez P. Quantification of serum ferritin in the acute coronary syndrome: a puzzle still to be resolved? Int J Cardiol. 2012;154(2):215–215. doi: 10.1016/j.ijcard.2011.10.050. [DOI] [PubMed] [Google Scholar]
- 6.Yalta K, Sivri N, Yalta T, Yetkin E. Serum ferritin: a potential determinant of myocardial ischemic burden in the setting of ischemic conditions? Int J Cardiol. 2011;153(2):225–226. doi: 10.1016/j.ijcard.2011.09.057. [DOI] [PubMed] [Google Scholar]
- 7.Basuli D, Stevens RG, Torti FM, Torti SV. Epidemiological associations between iron and cardiovascular disease and diabetes. Front Pharmacol. 2014 May 20;5:11–11. doi: 10.3389/fphar.2014.00117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dominguez-Rodriguez A, Carrillo-Perez Tome M, Hernandez-Garcia C, Arroyo-Ucar E, Juarez-Prera R, Blanco-Palacios G, et al. Serum ferritin and acute coronary syndrome: a strong prognostic factor? Int J Cardiol. 2011;152(1):129–130. doi: 10.1016/j.ijcard.2011.07.052. [DOI] [PubMed] [Google Scholar]