Abstract
Aims/Introduction
Variants on chromosome 1p13 have been associated with coronary artery disease and acute myocardial infarction risk in different ethnic groups. The present study aimed to investigate the association between 1p13 polymorphisms and the development of peripheral artery disease (PAD) in a Chinese population with type 2 diabetes mellitus.
Materials and Methods
1p13 polymorphisms, rs599839, rs646776 and rs12740374, were assessed in a cohort of 882 type 2 diabetes mellitus patients including 440 type 2 diabetes mellitus patients with PAD (DM + PAD group) and 442 patients without PAD (DM group). Genotyping was carried out using TaqMan assay.
Results
Compared with the DM group, the frequencies of the minor G allele of both rs599839 and rs646776 and the minor T allele of rs12740374 decreased (P = 0.013, P = 0.019 and P = 0.005, respectively), and the frequencies of rs599839 AG + GG, rs646776 AG + GG and rs12740374 CT+TT genotypes were statistically significantly decreased as well (P = 0.017, P = 0.011 and P = 0.007, respectively) in the dominant model in the DM + PAD group than in the DM group. Multivariate unconditional logistic regression analyses adjusted for age, glycated hemoglobin, triglyceride, low‐density lipoprotein cholesterol, smoking, hypertension, diabetes duration, coronary heart disease and cerebral infarction showed that the genotypic distribution of rs599839 AG + GG, rs646776 AG + GG and rs12740374 CT + TT remained statistically different between the DM and DM + PAD group (P = 0.014, P = 0.003 and P = 0.004, respectively). The frequencies of haplotype GGT were statistically significantly different between groups (P = 0.08).
Conclusions
The present study strongly supports that genotypes of rs599839, rs646776 and rs12740374 on 1p13 are protective factors for diabetic PAD in a Chinese population. Haplotype GGT generated by rs599839, rs646776 and rs12740374 might also decrease the risk of the disease.
Keywords: 1p13, Diabetic peripheral arterial disease, Single‐nucleotide polymorphism
Introduction
Peripheral arterial disease (PAD), characterized by reduced blood flow to the lower extremities, is a manifestation of systemic atherosclerosis. It commonly affects people with type 2 diabetes mellitus, which influences the development and progress of PAD. Each 1% increase in hemoglobin A1c, an indicator for the average level of blood glucose over the past 2 or 3 months, is associated with a 28% increased risk of PAD (95% confidence interval [CI]: 12–46)1. Compared with general population‐based prevalence, a higher prevalence of PAD over the age of 50 years was observed in diabetes patients2. The prevalence of PAD in diabetes patients ranged from 6.3% to 36.1% in different countries and races3, 4, 5, 6. In addition, there are several other traditional risk factors for PAD, such as smoking, hypertension and dyslipidemia.
Genetic factors also play an important role in the development of PAD. Genome‐wide association studies (GWAS) have discovered multiple loci associated with the risk of disease7, 8, 9, 10, 11, 12. It has been found that chromosome 1p31 locus is specific to peripheral arterial occlusive disease, which is diagnosed angiographically and/or surgically13. Rs1333049 on chromosome 9p21 was not only associated with coronary artery disease (CAD) susceptibility14, 15, 16, but also associated with PAD17, 18, which indicated that CAD and PAD might have a common genetic basis.
It was found that 1p13 single‐nucleotide polymorphisms (SNPs), rs599839, rs646776 and rs12740374, were associated with the incidence of CAD in Asia, Europe and America19, 20, 21, 22, 23, 24. Rs599839 and rs646776 SNPs and myocardial infarction (MI) risk are also significantly correlated21, 25, 26, and they also showed nominal significance with vascular calcification27, 28. However, the association between 1p13 polymorphisms and PAD has not yet been fully investigated. In the present study, we investigated the association of rs599839, rs646776 and rs12740374 with diabetic PAD.
Methods
This study was approved by the Institutional Ethics Review Board of Tangshan Gongren Hospital, and all patients provided written informed consent. The design of the study conforms to the provisions of the Declaration of Helsinki II.
Participants
A total of 442 patients with type 2 diabetes mellitus (DM group) and 440 PAD patients with type 2 diabetes mellitus (DM + PAD group) were recruited from Tangshan Gongren Hospital (Tangshan, China) from March 2012 to June 2015. All of them were from the Chinese Han population and unrelated. Diagnosis of type 2 diabetes mellitus was carried out in accordance with the criteria established by the World Health Organization (1999) diagnostic standard. Inclusion criteria o included type 2 diabetes mellitus patients aged ≥45 years and patients in the DM + PAD group who had an ankle brachial index ≤0.9 or a history of PAD therapy (stent, atherectomy and other surgical treatment). Exclusion criteria included patients with type 1 diabetes mellitus; patients who refused to provide informed consent; patients with ankle brachial index ≥1.4 were excluded to eliminate the effects of incompressible and calcified arteries29; serious heart failure, liver and kidney dysfunction; venous embolism; infection; malignant tumor and diseases of the immune system; and patients for whom genotyping of 12 samples failed.
Coronary artery disease was defined as a history of coronary artery revascularization or percutaneous coronary angiography (70% stenosis in a major coronary artery) or myocardial infarction according to the World Health Organization criteria30. Cerebral infarction was defined as a history of cerebral infarction or was diagnosed according to brain computed tomography or magnetic resonance imaging.
Peripheral blood deoxyribonucleic acid extraction and genotyping
For peripheral blood deoxyribonucleic acid (DNA) extraction and genotyping, 3 mL of peripheral blood was collected into sterile tubes containing ethylenediaminetetraacetic acid from all the study populations. Genomic DNA was extracted from peripheral blood leukocyte using a QIAamp DNA mini kit (QIAGEN GmbH, Hilden, Germany) according to the manufacturer's guidelines. Spectrophotometric DNA quantification was carried out using a TU‐1800 UV spectrophotometer (Bio‐Rad, Hercules, California, USA).Three SNPs (rs599839/rs646776/rs12740374) were selected from the Hapmap Chinese Han in Beijing, China, data (http://hapmap.ncbi.nlm.nih.gov/) using Haploview Software 4.2 (Broad Institute of MIT and Harvard, Cambridge, Massachusetts, USA). The distance between rs599839 and rs646776, rs646776 and rs12740374, and rs599839 and rs12740374 was 3,637, 941 and 4,577 bp, respectively. The minor allele frequency of the three SNPs among Chinese Han in Beijing, China, was as follows: rs599839 M G = 0.033, rs646776 M G = 0.012, rs12740374 M T = 0.011. According to previously published literature, polymorphisms of these loci might also be associated with the susceptibility to CAD or MI.
The SNPs of rs599839, rs646776 and rs12740374 were detected by TaqMan technology. The TaqMan probes to the selected loci were found on the Applied Biosystems website, where each number of the probes was send to synthesize probes and to synthesize primers of the loci. The target DNA sequences were amplified by polymerase chain reaction in the 7900 HT Real‐Time PCR System using TaqMan® SNP Genotyping Assays (Applied Biosystems, Foster City, California, USA). The DNA sequence was amplified using 1 ng of genomic DNA, 0.12 μL of Assay Mix (×40), 2.5 μL of Master Mix (×2) and 20 pmol of each primer in a total reaction volume of 5 μL with the following procedure: initial DNA denaturation at 95°C for 10 min followed by 40 cycles of 15 s of denaturation at 95°C, 60 s of annealing and extension at 60°C to complete the reaction. Quality control was carried out with 5% of samples, to ensure reproducibility.
Statistical analysis
Statistical analysis was carried out by SPSS 16.0 software (SPSS Inc., Chicago, Illinois, USA). The Hardy–Weinberg equilibrium was assessed in the DM group and DM + PAD group, by the χ2‐test. Continuous data were expressed as mean ± standard deviation or median (interquartile range), and between‐group differences were analyzed using independent‐samples t‐test or the Mann–Whitney U‐test. Measurement data and the frequencies of genotypes and alleles in each group were compared by the χ2‐test.
Linkage disequilibrium calculation and haplotype construction were carried out using the SheSIS software (Bio‐X Center, Shanghai Jiao Tong University, Shanghai, China). The linkage disequilibrium coefficient D’ and the value of r 2 were calculated. The values of D’ and r 2 ranged from 0 (linkage equilibrium) to 1 (complete linkage disequilibrium). The haplotype analysis was carried out to compare frequencies of haplotypes generated by rs599839, rs646776 and rs12740374 between the two groups. The association between genetic polymorphisms and PAD was assessed by multivariate unconditional logistic regression analyses in dominant genetic model of inheritance. Odds ratios (ORs) and 95% CIs were determined. A P‐value <0.05 was considered to show statistical significance.
Results
Demographic and clinical characteristics of each group
We studied 440 type 2 diabetes patients with PAD, and 442 sex‐matched type 2 diabetes patients without PAD. The demographic and clinical characteristics of the study population are described in Table 1. There was no significant difference between the groups in terms of sex and triglyceride. Whereas age, total cholesterol, high‐density lipoprotein cholesterol, low‐density lipoprotein cholesterol (LDL‐C), body mass index, smoking, glycated hemoglobin, diabetes duration and CAD, cerebral infarction, hypertension, and lipid‐lowering therapy were significantly different in the DM + PAD group compared with the DM group.
Table 1.
Demographic and clinical characteristics of the study population
| Variable | DM + PAD (n = 440) | DM (n = 442) | P |
|---|---|---|---|
| Male | 223 (50.7) | 246 (55.7) | 0.139 |
| Age (years) | 66.70 ± 7.57 | 60.43 ± 7.95 | <0.001*** |
| HbA1c (%) | 9.4 (3.3) | 8.9 (3.2) | 0.024* |
| TC (mmol/L) | 5.13 ± 0.88 | 4.93 ± 0.97 | 0.002** |
| TG (mmol/L) | 2.55 (1.67) | 2.43 (1.67) | 0.119 |
| HDL‐C (mmol/L) | 1.34 ± 0.25 | 1.40 ± 0.28 | <0.001*** |
| LDL‐C (mmol/L) | 3.29 ± 0.98 | 3.11 ± 0.98 | 0.005** |
| BMI (kg/m2) | 25.55 ± 3.09 | 25.06 ± 3.17 | 0.020* |
| Smoking | 200 (45.5) | 159 (36) | 0.004** |
| Hypertension | 249 (56.6) | 214 (48.4) | 0.015* |
| Lipid‐lowering therapy | 151 (34.3) | 122 (27.6) | 0.031* |
| Duration of diabetes (year) | 13.38 ± 5.82 | 10.60 ± 5.43 | <0.001*** |
| Coronary heart disease | 168 (38.2) | 87 (19.7) | <0.001*** |
| Cerebral infarction | 131 (29.8) | 64 (14.5) | <0.001*** |
Data are mean ± standard deviation, medians (interquartile range) or percentages. *P < 0.05, **P < 0.01 and ***P < 0.001. BMI, body mass index; DM, patients with type 2 diabetes mellitus; DM + PAD, peripheral artery disease patients with type 2 diabetes mellitus; HbA1c, glycated hemoglobin; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; TC, total cholesterol; TG, triglyceride.
Association study of Rs599839, Rs646776 and Rs12740374 polymorphisms with diabetic PAD
Rs599839, rs646776 and rs12740374 were in the Hardy–Weinberg genetic equilibrium in both groups. It was found that frequencies of the minor G allele of both rs599839 and rs646776, and the minor T allele of rs12740374 were significantly decreased in the DM + PAD group compared with the DM group. Genotype frequencies of three loci decreased significantly in the dominant model in the DM + PAD group compared with the DM group. Genotype frequencies were not statistically different in the recessive model (Table 2).
Table 2.
Rs599839, rs646776 and rs12740374 genotype and allele distribution in the peripheral artery disease patients with type 2 diabetes mellitus and patients with type 2 diabetes mellitus group
| Genotypes | DM + PAD (n = 440) | DM (n = 442) | P |
|---|---|---|---|
| rs599839 | |||
| Allele | |||
| G | 37 (4.2) | 61 (6.9) | 0.013* |
| Dominant model | |||
| AA | 404 (91.8) | 384 (86.9) | 0.017* |
| AG + GG | 36 (8.2) | 58 (13.1) | |
| Recessive model | |||
| AA + AG | 439 (99.8) | 439 (99.3) | 0.624† |
| GG | 1 (0.2) | 3 (0.7) | |
| rs646776 | |||
| Allele | |||
| G | 27 (3.1) | 47 (5.3) | 0.019* |
| Dominant model | |||
| AA | 414 (94.1) | 395 (89.4) | 0.011* |
| AG + GG | 26 (5.9) | 47 (10.6) | |
| Recessive model | |||
| AA + AG | 439 (99.8) | 442 (100.0) | 0.499† |
| GG | 1 (0.2) | 0 (0.0) | |
| rs12740374 | |||
| Allele | |||
| T | 25 (2.8) | 49 (5.5) | 0.005** |
| Dominant model | |||
| GG | 415 (94.3) | 395 (89.4) | 0.007** |
| GT + TT | 25 (5.7) | 47 (10.6) | |
| Recessive model | |||
| GG + GT | 440 (100.0) | 440 (99.5) | 0.499† |
| TT | 0 (0.0) | 2 (0.5) | |
Data are expressed as n (%). *P < 0.05, **P < 0.01. †Calculated by Fisher's exact test. DM, patients with type 2 diabetes mellitus; DM + PAD, peripheral artery disease patients with type 2 diabetes mellitus.
Univariate unconditional logistic regression analyses showed that rs599839 AG + GG, rs646776 AG + GG and rs12740374 CT + TT genotypes were correlated with PAD in diabetes patients (P = 0.018, P = 0.012 and P = 0.008, respectively). To evaluate the independent genetic effect of each SNP on the susceptibility to diabetic PAD, multivariate unconditional logistic regression analyses were carried out (Table 3). Adjusted for age, glycated hemoglobin, triglyceride, LDL‐C, smoking, hypertension and duration of diabetes, the genotypic distribution of rs599839 AG + GG, rs646776 AG + GG and rs12740374 CT + TT remained statistically different between the groups (P = 0.014, P = 0.003 and P = 0.004, respectively).
Table 3.
Logistic regression analysis for the association of rs599839, rs646776 and rs12740374 polymorphisms with peripheral artery disease in diabetes
| Univariate regression | Multiple regression | |||
|---|---|---|---|---|
| Crude OR (95% CI) | Crude P | Adj OR (95% CI) | Adj P | |
| rs599839 (dominant model) | 0.590 (0.380–0.915) | 0.018* | 0.497 (0.285–0.866) | 0.014* |
| rs646776 (dominant model) | 0.528 (0.321–0.869) | 0.012* | 0.381 (0.200–0.728) | 0.003** |
| rs12740374 (dominant model) | 0.506 (0.306–0.838) | 0.008** | 0.385 (0.200–0.739) | 0.004** |
Multiple regression was adjusted by: sex, age, glycated hemoglobin, total cholesterol, triglyceride, high‐density lipoprotein cholesterol, low‐density lipoprotein cholesterol, smoking, hypertension, lipid‐lowering therapy, body mass index, duration of diabetes, coronary heart disease and cerebral infarction. *P < 0.05, **P < 0.01. Adj, adjusted.
Linkage disequilibrium of the three loci was observed in each group and both. Linkage disequilibrium coefficients D’ and r 2 of rs12740374 and rs599839, rs12740374 and rs646776, and rs599839 and rs646776 were 0.933, 0.977 and 0.930, and 0.689, 0.914 and 0.655, respectively in the DM group. In the DM + PAD group, Linkage disequilibrium coefficients D’ and r 2 of rs12740374 and rs599839, rs12740374 and rs646776, and rs599839 and rs646776 were 0.915, 0.959 and 0.922, and 0.558, 0.849 and 0.613, respectively. We showed the haplotype of the three loci in Table 4. Frequencies of haplotype AAG generated from rs599839, rs646776 and rs12740374 between the DM group and DM + PAD group were statistically significantly different (P = 0.011), the odds ratio was 1.683 (95% CI: 1.118–2.535). Frequencies of haplotype GGT were statistically significantly different between the DM group and DM + PAD group (P = 0.008), the odds ratio was 0.502 (95% CI: 0.297–0.846).
Table 4.
Haplotype analysis of rs599839, rs646776 and rs12740374 in the patients with type 2 diabetes mellitus group and peripheral artery disease patients with type 2 diabetes mellitus group
| Haplotype | DM + PAD (freq) | DM (freq) | χ2 | P | OR | 95% CI |
|---|---|---|---|---|---|---|
| AAG | 840.97 (0.956) | 819.95 (0.928) | 6.333 | 0.011* | 1.683 | 1.118–2.535 |
| GAG | 11.03 (0.013) | 14.05 (0.016) | 0.355 | 0.551 | 0.786 | 0.335–1.739 |
| GGG | 3.00 (0.003) | 1.01 (0.001) | 1.005 | 0.316 | 3.005 | 0.313–28.822 |
| GAT | 1.00 (0.001) | 3.00 (0.003) | 0.797 | 0.372 | 0.333 | 0.049–2.263 |
| AGT | 2.03 (0.002) | 3.05 (0.003) | 0.203 | 0.652 | 0.666 | 0.112–3.947 |
| GGT | 21.97 (0.025) | 42.94 (0.049) | 6.934 | 0.008** | 0.502 | 0.297–0.846 |
Haplotypes were constructed for: rs12740374, rs646776 and rs599839. *P < 0.05, **P < 0.01. CI, confidence interval; DM, patients with type 2 diabetes mellitus; DM + PAD, peripheral artery disease patients with type 2 diabetes mellitus; freq, frequency; OR, odds ratio.
Discussion
The current study showed an association between rs599839, rs646776 and rs12740374 genotypes and PAD in diabetes patients. Genotypic frequencies of rs599839, rs646776 and rs12740374 increased in the dominant model in diabetes patients with PAD, which showed that rs599839 AG + GG, rs646776 AG + GG and rs12740374 GT + TT were associated with a decreased risk of PAD in diabetes patients. Haplotype GGT of rs599839, rs646776 and rs12740374 was also an independent protective factor for PAD in diabetes patients.
Rs599839, rs646776 and rs12740374 are located on chromosome 1p13 (Figure 1), in which SNPs are associated with cardiovascular diseases, as well as macrovascular disease. It has been found that the minor G allele of rs599839 and the minor G allele of rs646776 were independent protective factors for CAD and MI20, 21, 26. Ellis et al.31 showed that an individual with cardiovascular disease or not carrying one or more rs599839 G allele had a lower prevalence of dyslipidemia or lower levels of LDL‐C and total cholesterol and/or less history of MI compared with AA participants. Furthermore, AG/GG carriers with coronary disease and post‐MI had better cardiac function, and fewer AG/GG carriers with coronary heart disease were readmitted for a non‐ST‐segment elevation MI31. One copy of the rs599839 G allele was associated with a decrease of serum LDL‐C by 0.14 mmol/L and a 9% decrease in CAD risk22. The rs599839 has been reported to be associated with a reduced risk of coronary heart disease in the Chinese population, and its association with decreased LDL levels was also observed32. Rs646776 also showed a significant protective association with CAD (OR 0.422, 95% CI: 0.181–0.981)20. Rs599839, rs646776 and rs12740374 are near the genes SORT1, PSRC1 and CELSR2, which can interfere with lipid metabolism (Table 1). Rs12740374 T increased the expression of SORT1 messenger ribonucleic acid and the level of SORT1 protein, which reduced the levels of very LDL‐C and LDL‐C in the blood, and then reduced the risk of CAD13. Similar to the present study, these studies suggest that the minor G allele of rs599839 and rs646776, and the minor T allele of rs12740374 are protective factors for atherosclerosis and cardiovascular disease risk.
Figure 1.
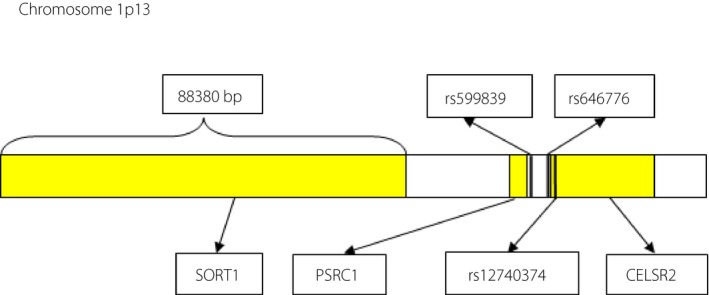
Location of rs599839, rs646776 and rs12740374 on chromosome 1p13.
Concordantly, some meta‐analyses found that the A allele of rs599839 and T allele of rs646776 were associated with increased cardiovascular disease risk as well as total cholesterol and LDL‐C, apolipoprotein B, and decreased high‐density lipoprotein cholesterol33, 34. The similar association was also observed in a Korean population24. However, the GWAS of PAD in East Asians had not found that 1p13 locus was significantly associated with PAD7. This is different from the present findings, which showed that rs599839 and rs646776 were protective factors in diabetic PAD patients. Considering the discordant reports from different ethnic groups, it is possible that the three SNPs are markers, but not causative variants, and the discrepancy in studies could also be related with different study population, ethnic differences, different genotypic frequency, gene–environment and gene–gene interactions. Sample bias and/or other confounding factors might also to be responsible for such differences.
In addition, it was found that rs599839, rs646776 and coronary artery calcification were correlated27, 28. The occurrence of coronary artery calcification could increase the risk of cardiovascular disease, and it is also an important predictor of all‐cause mortality and cardiovascular mortality.
There are fewer studies on the correlation between variant 1p13 and cerebrovascular disease. Rs646776 has been found to be associated with carotid artery disease35, which is one of the important risk factors for stroke.
Haplotypes play key roles in the study of human disease and genetics36. The haplotype GC generated by rs599839 and rs646776 was shown to be a protective factor of CAD20. In the present study, diabetes patients with haplotype GGT had a decreased PAD risk, whereas those with haplotype AAG had an increased risk. However, the association between haplotype AAG and risk of PAD was not supported by allelic analysis of rs599839 A, rs646776 A and rs12740374 G in the recessive model, which suggests that the susceptibility loci might exist in haplotype AAG or nearby.
In conclusion, the present study showed that genotypes of rs599839, rs646776 and rs12740374 on 1p13 are protective factors for PAD in a Chinese population with type 2 diabetic mellitus. Haplotype GGT generated by rs599839, rs646776 and rs12740374 might also decrease the risk of the disease. The mechanism of the association should be further confirmed. There were still some limitations to the present study, such as the ankle brachial index only being able to reflect local lesions, and it can be falsely high with poorly compressive vessels often seen in diabetes patients, so the diagnosis might need to be improved in future research.
Disclosure
The authors declare no conflict of interest.
Acknowledgments
This research did not receive any specific grant from any funding agency in the public, commercial or not‐for‐profit sector. The authors thank all of the people who participated in the studies, and particularly thank Yu‐Kai Li for the collection of patients and Dr Yun‐tao Zhou for helpful advice and genetic analyses.
J Diabetes Investig 2018; 9: 1189–1195
References
- 1. Adler AI, Stevens RJ, Neil A, et al UKPDS 59: hyperglycemia and other potentially modifiable risk factors for peripheral vascular disease in type 2 diabetes. Diabetes Care 2002; 25: 894–899. [DOI] [PubMed] [Google Scholar]
- 2. Knowles JW, Assimes TL, Li J, et al Genetic susceptibility to peripheral arterial disease: a dark corner in vascular biology. Arterioscler Thromb Vasc Biol 2007; 27: 2068–2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Premalatha G, Shanthirani S, Deepa R, et al Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: the Chennai Urban Population Study. Diabetes Care 2000; 23: 1295–1300. [DOI] [PubMed] [Google Scholar]
- 4. Hirsch AT, Criqui MH, Treat‐Jacobson D, et al Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA 2001; 286: 1317–1324. [DOI] [PubMed] [Google Scholar]
- 5. Rhee SY, Guan H, Liu ZM, et al Multi‐country study on the prevalence and clinical features of peripheral arterial disease in Asian type 2 diabetes patients at high risk of atherosclerosis. Diabetes Res Clin Pract 2007; 76: 82–92. [DOI] [PubMed] [Google Scholar]
- 6. Cacoub P, Cambou JP, Kownator S, et al Prevalence of peripheral arterial disease in high‐risk patients using ankle‐brachial index in general practice: a cross‐sectional study. Int J Clin Pract 2009; 63: 63–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Matsukura M, Ozaki K, Takahashi A, et al Genome‐wide association study of peripheral arterial disease in a Japanese Population. PLoS One 2015; 10: e0139262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thorgeirsson TE, Geller F, Sulem P, et al A variant associated with nicotine dependence, lung cancer and peripheral arterial disease. Nature 2008; 452: 638–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gretarsdottir S, Baas AF, Thorleifsson G, et al Genome‐wide association study identifies a sequence variant within the DAB2IP gene conferring susceptibility to abdominal aortic aneurysm. Nat Genet 2010; 42: 692–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Koriyama H, Nakagami H, Katsuya T, et al Identification of evidence suggestive of an association with peripheral arterial disease at the OSBPL10 locus by genome‐wide investigation in the Japanese population. J Atheroscler Thromb 2010; 17: 1054–1062. [DOI] [PubMed] [Google Scholar]
- 11. Murabito JM, White CC, Kavousi M, et al Association between chromosome 9p21 variants and the ankle‐brachial index identified by a meta‐analysis of 21 genome‐wide association studies. Circ Cardiovasc Genet 2012; 5: 100–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Helgadottir A, Thorleifsson G, Magnusson KP, et al The same sequence variant on 9p21 associates with myocardial infarction, abdominal aortic aneurysm and intracranial aneurysm. Nat Genet 2008; 40: 217–224. [DOI] [PubMed] [Google Scholar]
- 13. Gudmundsson G, Matthiasson SE, Arason H, et al Localization of a gene for peripheral arterial occlusive disease to chromosome 1p31. Am J Hum Genet 2002; 70: 586–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lian J, Ba Y, Dai D, et al A replication study and a meta‐analysis of the association between the CDKN2A rs1333049 polymorphism and coronary heart disease. J Atheroscler Thromb 2014; 21: 1109–1120. [DOI] [PubMed] [Google Scholar]
- 15. Abid K, Mili D, Kenani A. Polymorphism on chromosome 9p21.3 is associated with severity and early‐onset CAD in type 2 diabetic Tunisian population. Dis Markers 2015; 2015: 792679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Çakmak HA, Bayoğlu B, Durmaz E, et al Evaluation of association between common genetic variants on chromosome 9p21 and coronary artery disease in Turkish population. Anatol J Cardiol 2015; 15: 196–20317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cluett C, McDermott MM, Guralnik J, et al The 9p21 myocardial infarction risk allele increases risk of peripheral artery disease in older people. Circ Cardiovasc Genet 2009; 2: 347–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tian LB, Fang H, Gao L, et al 9p21 polymorphisms increase the risk of peripheral artery disease in the Han Chinese population. J Int Med Res 2013; 41: 106–114. [DOI] [PubMed] [Google Scholar]
- 19. Musunuru K, Strong A, Frank‐Kamenetsky M, et al From noncoding variant to phenotype via SORT1 at the 1p13 cholesterol locus. Nature 2010; 466: 714–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Arvind P, Nair J, Jambunathan S, et al CELSR2‐PSRC1‐SORT1 gene expression and association with coronary artery disease and plasma lipid levels in an Asian Indian cohort. J Cardiol 2014; 64: 339–346. [DOI] [PubMed] [Google Scholar]
- 21. Kleber ME, Renner W, Grammer TB, et al Association of the single nucleotide polymorphism rs599839 in the vicinity of the sortilin 1 gene with LDL and triglyceride metabolism, coronary heart disease and myocardial infarction. The Ludwigshafen Risk and Cardiovascular Health Study. Atherosclerosis 2010; 209: 492–497. [DOI] [PubMed] [Google Scholar]
- 22. Linsel‐Nitschke P, Heeren J, Aherrahrou Z, et al Genetic variation at chromosome 1p13.3 affects sortilin mRNA expression, cellular LDL uptake and serum LDL levels which translates to the risk of coronary artery disease. Atherosclerosis 2010; 208: 183–189. [DOI] [PubMed] [Google Scholar]
- 23. Angelakopoulou A, Shah T, Sofat R, et al Comparative analysis of genome‐wide association studies signals for lipids, diabetes, and coronary heart disease: cardiovascular Biomarker Genetics Collaboration. Eur Heart J 2012; 33: 393–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee JY, Lee BS, Shin DJ, et al A genome‐wide association study of a coronary artery disease risk variant. J Hum Genet 2013; 58: 120–126. [DOI] [PubMed] [Google Scholar]
- 25. Qi Lu, Ma J, Qi Q, et al Genetic risk score and risk of myocardial infarction in Hispanics. Circulation 2011; 123: 374–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Matsuoka R, Abe S, Tokoro F, et al Association of six genetic variants with myocardial infarction. Int J Mol Med 2015; 35: 1451–1459. [DOI] [PubMed] [Google Scholar]
- 27. O'Donnell CJ, Kavousi M, Smith AV, et al Genome‐wide Association Study for Coronary Artery Calcification with Follow‐up in Myocardial Infarction. Circulation 2011; 124: 2855–2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Adams JN, Raffield LM, Freedman BI, et al Analysis of common and coding variants with cardiovascular disease in the diabetes heart study. Cardiovasc Diabetol 2014; 13: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Resnick HE, Lindsay RS, McDermott MM, et al Relationship of high and low ankle brachial index to all‐cause and cardiovascular disease mortality: the Strong Heart Study. Circulation 2004; 109: 733–739. [DOI] [PubMed] [Google Scholar]
- 30. Tunstall‐Pedoe H, Kuulasmaa K, Amouyel P, et al Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case‐fatality rates in 38 populations from 21 countries in four continents. Circulation 1994; 90: 583–612. [DOI] [PubMed] [Google Scholar]
- 31. Ellis KL, Frampton CM, Pilbrow AP, et al Genomic risk variants at 1p13.3, 1q41, and 3q22.3 are associated with subsequent cardiovascular outcomes in healthy controls and in established coronary artery disease. Circ Cardiovasc Genet 2011; 4: 636–646. [DOI] [PubMed] [Google Scholar]
- 32. Zhou L, Ding H, Zhang X, et al Genetic variants at newly identified lipid loci are associated with coronary heart disease in a Chinese Han population. PLoS One 2011; 6: e27481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Coronary Artery Disease Consortium , Samani NJ, Deloukas P, et al Large scale association analysis of novel genetic loci for coronary artery disease. Arterioscler Thromb Vasc Biol 2009; 29: 774–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. He QC, Hu YY, Zhang QP, et al A meta‐analysis of three identified single nucleotide polymorphisms at 1p13.3 and 1q41 and their associations with lipid levels and coronary artery disease. Kaohsiung J Med Sci 2017; 33: 1–10. [DOI] [PubMed] [Google Scholar]
- 35. Ronald J, Rajagopalan R, Ranchalis JE, et al Analysis of recently identified dyslipidemia alleles reveals two loci that contribute to risk for carotid artery disease. Lipids Health Dis 2009; 8: 52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Schaid DJ. Evaluating associations of haplotypes with traits. Genet Epidemiol 2004; 27: 348–364. [DOI] [PubMed] [Google Scholar]


