Abstract
Introduction
The most cases of excessive femoral anteversion may be asymptomatic, because the he hip joint is a ball joint. However, when the hip, knee, or ankle joint is in a pathological state, excessive femoral anteversion may not be compensated for and induce symptoms.
Case report
A 16-year-old female with achondroplasia. Medullary compression by the odontoid process caused right hemiplegia at 10 months after birth and equinus foot concomitantly developed. At 14 years old, right knee pain developed during walking. For treatment, firstly, tenodesis of medial collateral ligament of the knee joint (MCL) was performed. Oblique osteotomy was applied to the proximal MCL attachment site over the distal tibial tuberosity, followed by simple limb lengthening, which improved knee instability. To prevent recurrence of knee instability, varus and derotationosteotomy of the femur and Vulpius procedure (triceps surae muscle lengthening) were additionally performed, and gait stabilized after surgery.
Discussion
Regarding the pathogenesis, her gait was originally in-toeing because of excessive femoral anteversion, but the lower leg did not internally rotate during walking because of equinus foot, and the foot grounded in an externally rotated position, loading burdens on the MCL. This condition may have gradually caused instability of the knee over the years.
Conclusion
We surgically treated the patient with knee joint valgus instability caused by excessive femoral anteversion and equinus foot and achieved a favorable outcome.
Keywords: Laxity of medial collateral ligament, Limb lengthening, Excessive femoral anteversion, Equinus foot, Derotation osteotomy of femur, case report
Highlights
-
•
The most cases of excessive femoral anteversion may be asymptomatic, because the he hip joint is a ball joint.
-
•
The hip, knee, or ankle joint is in a pathological state, excessive femoral anteversion may not be compensated for and induce symptoms.
-
•
Oblique osteotomy was applied to the proximal MCL attachment site over the distal tibial tuberosity, followed by simple limb lengthening, which improved knee instability.
-
•
We surgically treated the patient with knee joint valgus instability caused by excessive femoral anteversion and equinus foot and achieved a favorable outcome.
1. Introduction
This work has been reported in line with the SCARE criteria [1].
The conditions indicated for rotation osteotomy to treat excessive femoral anteversion set by Staheli are: 8 years old or older, severe esthetic dysfunction, anteversion exceeding 50°, and 85° or more internal rotation with 10° or less external rotation [2]. Since fewer patients are actually surgically treated, most cases of excessive femoral anteversion may be asymptomatic.
Paley developed various osteotomy procedures for treatment of instability of the collateral ligament of the knee joint and one of these is osteotomy of the proximal MCL attachment site over the distal tibial tuberosity followed by simple limb lengthening for treatment of MCL instability and specified cases with leg length discrepancy and bilateral cases as favorable indications [3]. Since our patient originally had a short stature and varus knee on the opposite side, we simultaneously performed deformity correction and limb lengthening of the opposite side.
We report a patient with excessive femoral anteversion which caused MCL instability.
2. Case report
A 16-year-old female with achondroplasia. Medullary compression by the odontoid process caused right hemiplegia at 10 months after birth and equinus foot concomitantly developed. At 14 years old, right knee pain developed during walking and she visited our department.
3. Physical examination
The height was 118.2 cm (−7.5SD), and the body weight was 32.3 kg (−2.4SD).
The right lower limb muscle strength was low on the muscle manual test as follows: iliopsoas, 4; quadariceps, 4; major gluteus, 4; middle gluteus, 2; tibialis anterior, 2; extensor and flexor hallucis longus, 0; and gastrocnemius, 2. No muscle weakness was noted in the left lower limb.
The ranges of motion of the right/left hip joints were: flexion, 120°/120°; extension, −40°/-20°; abduction, 30°/30°; internal rotation, 80°/30° (Fig. 1a); and external rotation, 10°/25°. In the sitting position, the right and left hip joints were internally and externally rotated, respectively (Fig. 1b). No problem was noted in the range of motion of the knee joint, but marked right knee instability was observed in the presence of valgus stress (Fig. 1c). Dorsiflexion knee extensions of the right and left ankle joints were −20° and 10°, respectively, and dorsiflexion knee flexions were −10° and 20°, respectively, showing right equinus foot.
Fig. 1.
a: Internal rotations of the right and left hip joints were 80 and 30°, respectively. b: In the sitting position, the right and left hip joints were internally and externally rotated, respectively. c: Marked instability of the right knee was noted in the presence of valgus stress.
Regarding gait, the entire lower limb was rotated externally to acquire better clearance of the equinus foot in the swing phase (Fig. 2a). To complement weak hip joint flexor muscle strength, sartorius muscle strength was utilized, which may have caused external rotation of the entire lower limb. On one-leg standing in the stance phase of walking, the foot and crus were fixed in an externally rotated position on the ground, but the proximal region above the knee joint showed knee-in gait (Fig. 2b). The patient complained of knee joint pain during walking.
Fig. 2.
a: The entire lower limb was externally rotated to improve clearance disturbed by the presence of equinus foot in the swing phase. b: On one-leg standing in the stance phase, the foot and crus were fixed in an externally rotated position on the ground, but the proximal region above the knee joint showed knee-in gait.
4. Images
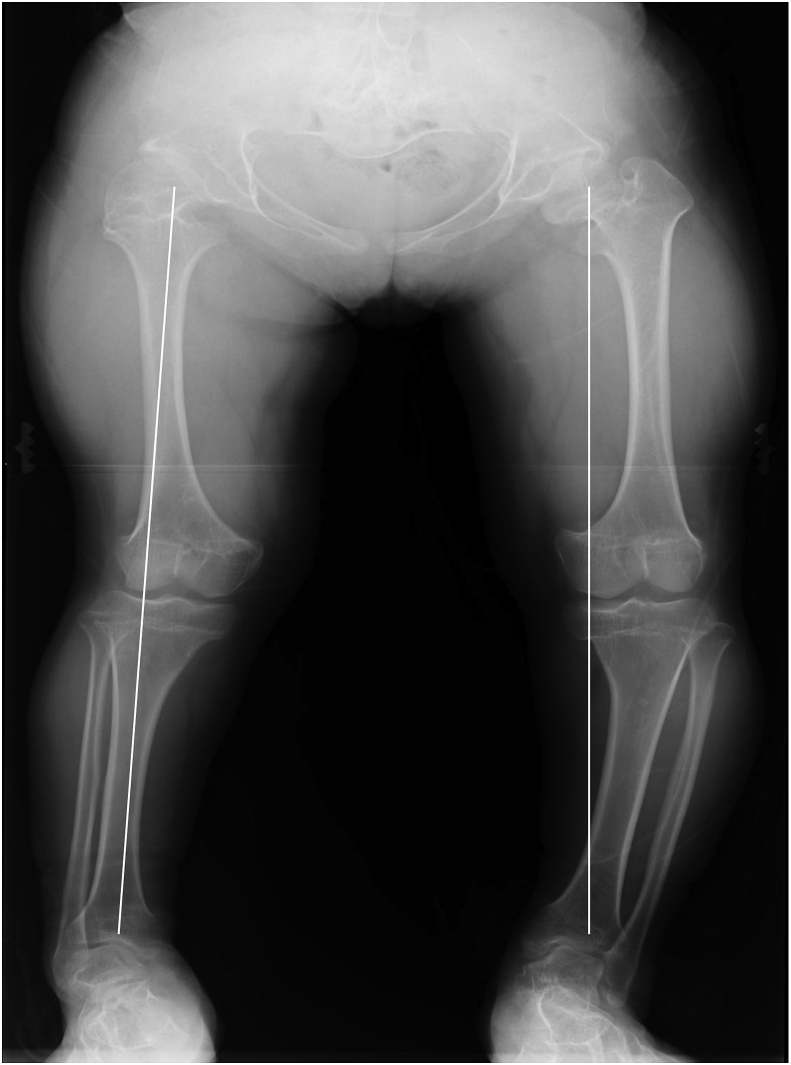
On frontal radiography in the long standing position, the mechanical axis deviations (MAD) were 19 mm toward the lateral side and 27 mm toward the medial side on the right and left legs, respectively. The mechanical lateral distal femoral angles (mLDFA) were 83 and 95°on the right and left legs, respectively, the medial proximal tibial angles (MPTA) were 89 and 80°, respectively, and the lateral distal tibial angles (LDTA) were 96 and 100°, respectively (Fig. 3).
Fig. 3.
Frontal radiology in the long standing position.
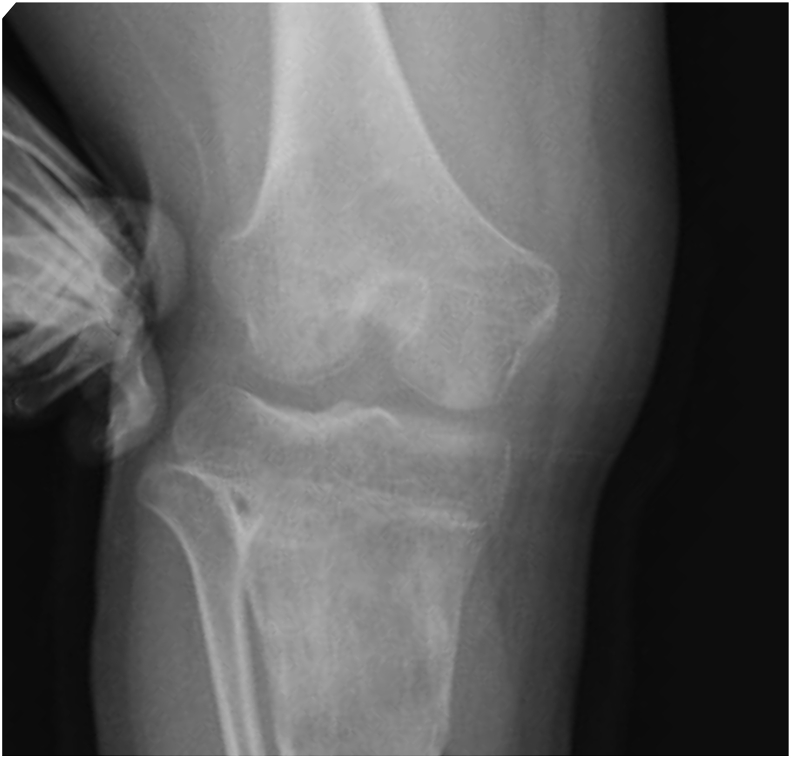
The right knee was valgus and the left knee was varus. On valgus stress radiography, marked instability of the right knee joint was observed (Fig. 4). On coronal MRI, MCL was loosened at the femoral attachment site (Fig. 5). Right and left femoral anteversion were 71 and -3°, respectively, on CT (Fig. 6).
Fig. 4.
Marked right knee joint instability was noted on valgus stress radiography.
Fig. 5.
On coronal MRI, loosening of MCL was observed at the femoral attachment site.
Fig. 6.
Right and left femoral anteversion were 71 and -3°, respectively, on CT.
5. Surgical technique
Osteotomy was applied to the proximal MCL attachment site over the distal tibial tuberosity, and 1 mm/day lengthening was initiated after one week. When lengthening reached 30 mm, the mechanical axis came to pass through the center of the knee joint in the standing position. The leg was further lengthened by 5 mm and lengthening was completed, being overcorrected (Fig. 7). Correction of the varus knee and lengthening were performed on the opposite side at the same time. The duration of external fixator attachment was 152 days, and the external fixation index was 43.4 day/cm.
Fig. 7.
Osteotomy was applied to the proximal MCL attachment site to the distal patellar tendon attachment site, followed by 35 mm lengthening.
Excessive right femoral anteversion and equinus foot remained, for which varus and derotation osteotomy of the femur and Vulpius procedure were additionally performed one year and 9 months after the first surgery.
6. Patient outcome
At 2 years and 4months after the first surgery, MAD of the right and left legs were 14 mm toward the medial side and 7 mm toward the lateral side, respectively, mLDFA of the right and left legs were 88 and 94°, respectively, MPTA were 85 and 92°, respectively, and LDTA were 116 and 104°, respectively (Fig. 8). Knee instability was resolved on valgus stress radiography (Fig. 9). Knee-in gait on one-leg standing in the stance phase of walking disappeared (Fig. 10). Loose MCL on coronal MRI was resolved on the final follow-up (Fig. 11).
Fig. 8.
Frontal radiology in the long standing position on the final follow-up.
Fig. 9.
Knee instability was resolved on valgus stress radiography.
Fig. 10.
Knee-in gait on one-leg standing in the stance phase of walking was resolved.
Fig. 11.
Loosening of MCL was resolved on coronal MRI.
7. Discussion
Gait of the present patient may have been originally in-toeing due to excessive femoral anteversion. Staheli stated the indication of rotation osteotomy for excessive femoral anteversion [2], but most cases of excessive femoral anteversion may be asymptomatic because fewer cases are actually surgically treated, and this may be due to the capability of compensating abnormal femoral rotation of the hip joint, which is a ball joint.
However, when excessive femoral anteversion and excessive tibial outward rotation concomitantly develop, such as those in miserable malalignment syndrome [4], compensation by the hip joint alone may be not possible and abnormal femoral rotation may occur. Gait of this patient was originally in-toeing, but the lower limb did not internally rotate during walking due to the equinus foot, and the foot landed on the ground in an externally rotated position, resulting in internal rotation of the femur alone. This condition may have loaded burden on MCL and gradually caused knee instability over the years.
Paley published a method to treat knee joint instability caused by loosening of MCL, in which osteotomy is applied to the proximal MCL attachment site over the distal patellar tendon attachment site followed by simple limb lengthening and specified cases with limb length discrepancy and bilateral cases as good indications [3]. Regarding the length of lengthening, 10–15 mm was considered necessary [5] but its basis was not described. In the present patient, 30-mm simple limb lengthening was applied firstly because knee joint instability was severe. The tibial morphology was not changed, but valgus knee improved as MCL became tense. The mechanical axis came to pass through the center of the knee joint. There was no basis for the 30 mm lengthening. Additional 5 mm lengthening was applied in consideration of re-loosening of MCL. The mechanical axis came to pass through on the medial side of the center of the knee joint. Further investigation of the appropriate amount of lengthening is necessary.
Since tenodesis of MCL alone did not improve excessive femoral anteversion and equinus foot, re-loosening of MCL was predicted, for which varus and derotation osteotomy of the femur for femoral excessive anteversion and Vulpius procedure fort equinus foot were performed one year and 9 months after the first surgery. Equinus foot recurred, but as of 6 years and 6 months after the first surgery, the knee symptoms have not recurred. Surgical improvement of paralysis-induced equinus foot is difficult, but it is possible for an abnormal bone morphology, excessive femoral anteversion. We consider that the present patient required additional varus and derotation osteotomy of the femur.
8. Conclusion
The patient with knee joint instability caused by excessive femoral anteversion and equinus foot was treated with knee joint osteotomy and stabilization of the knee joint by simple limb lengthening, and varus and derotation osteotomy of the femur was additionally performed, and a favorable outcome was achieved.
Provenance and peer review
Not commissioned, externally peer reviewed.
Ethical approval
Institutional review board approval was not required because all data were collected from clinical records.
Sources of funding
Author declare there is no funding resources for this paper.
Author contribution
SM wrote this paper. All authors read this paper.
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Trial registry number
Research Registry 4349.
Guarantor
Shohei Matsubayashi, the corresponding author of this paper
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.amsu.2018.08.018.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE Statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Staheli L.T. Torsion—treatment indications. Clin Orthop Res. 1989;247:61–66. [PubMed] [Google Scholar]
- 3.Paley D., Bhatnagar J., Herzenberg J.E., Bhave A. New procedures for Tightening knee collateral ligaments in conjunction with knee realignment osteotomy. Orthop. Clin. N. Am. 1994;25:533–555. [PubMed] [Google Scholar]
- 4.Bruce W.D., Stevens P.M. Surgical correction of miserable malalignment syndrome. J. Pediatr. Orthop. 2004;24:392–396. doi: 10.1097/00004694-200407000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Paley D. Malalignment due to ligamentous laxity of the knee. In: Herzenberg J.E., Paley D., editors. Principles of Deformity Correction. Springer; New York: 2002. pp. 451–464. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.