Abstract
Objective
The aim of this study was to evaluate the effect of Botulinum toxin type A by injecting in the submandibular and parotid glands on the frequency and severity of sialorrhea.
Methods
Pediatric patients who were referred to our department with sialorrhea were evaluated using their parents’ frequency and severity scores of sialorrhea with visual analog scales before and after 3 months of botulinum toxin type A injections. Bilateral submandibular and parotid glands were injected with Botulinum toxin type A.
Results
Twenty-seven pediatric patients who were referred to our department with a complaint of sialorrhea were included in this study. Seventeen patients were female and 10 were male. Severe sialorrhea with cerebral palsy was present in all the patients. There were no complications after the procedure.
Conclusion
Botulinum toxin A injected in the major salivary glands in pediatric patients with neurological disorders is a safe and effective method.
Keywords: Sialorrhea, botulinum toxin, parotid gland, submandibular gland, cerebral palsy
Introduction
Sialorrhea is characterized by excessive drooling or salivation. Whilst normal in the early years, the condition should be regarded as pathological after the age of four (1, 2). Pathologic drooling can occur as an isolated condition associated with hypersalivation, but also as the side effects of amyotrophic lateral sclerosis, cerebral palsy, Parkinson’s disease, or of their respective medication. Its most common cause in childhood is cerebral palsy, with a rate of 10 to 38% of the cases (3). In adults, Parkinson’s disease is the most common (70 to 80%) cause of sialorrhea (4, 5). It is also seen in about 30 to 80% of adult schizophrenia patients as a result of clozapine treatment (6). While the underlying diseases alone are significant conditions, concomitant presence of sialorrhea can give rise to both social issues and local issues such as aspiration, skin problems or infection (7).
Treatment of sialorrhea is not easy. Therefore, as well as conservative treatment methods, highly invasive methods are also used. Conservative treatment often begins by regulating dietary habits. Oral-motor exercises, intraoral devices or palatal training devices can be used. While medical treatment modalities include medication and botulinum toxin, invasive methods like surgery or radiotherapy are also among the available options (8, 9).
This study was designed to evaluate the effectiveness of botulinum toxin type A injections in the pediatric patients referred to our clinic because of sialorrhea.
Methods
Incidence of sialorrhea in each pediatric patient was followed with the help of their families and assessed before and in the third month after their botulinum toxin type A injection (Botox®, Allergan, USA). The study was launched in May 2016 after approval was obtained from the Ethics Committee of Çukurova University, Faculty of Medicine. Consent was obtained from the families of all patients.
Botulinum toxin type A injection (Botox®, Allergan, USA) was administered to both pairs of the parotid glands and the submandibular glands in each patient. The procedure was performed in the operating room under sterile conditions and injections were administered under sedation in all patients. In each patient, botulinum toxin type A injection was first administered to the two parotid glands, then to the two submandibular glands. Botulinum toxin type A, delivered by cold chain, was diluted with 1cc sterile physiological saline to obtain 100IU botulinum toxin. The syringe was changed after this process and the solution was administered via insulin syringes. After the respective regions of the parotid glands and the submandibular glands were cleansed with antiseptic solution, botulinum toxin injections were administered via an insulin syringe to the parotid gland (10 units each) and the submandibular gland pairs (20 units each) at a maximum of 2mg/kg in total. No additional therapies were given after the procedure and all patients were discharged on the same day. Families of patients were asked to fill out visual analog scales before the procedure and in the third month after the procedure and rate the severity and frequency of their patient’s condition on a scale of 0 to 10. The effectiveness of the method was assessed by comparing these results.
Results
Twenty-seven pediatric patients who were referred to and treated for sialorrhea at the Otolaryngology Department, Faculty of Medicine of the Çukurova University were included in the study. Of the 27 patients 17 were female and 10 were male with a mean age of 11.5 (Min: 6, Max: 16 years). All patients had cerebral palsy accompanied by severe sialorrhea. According to the visual analog scale filled out by the families, all patients had profuse sialorrhea to the extent of soiling their clothes and hands. Visual analog scale analysis of patients before the injections showed a mean drooling value of 7.9 (Min: 5, Max: 10) and a mean frequency value of 7.7 (Min: 5, Max: 10). Analysis of the visual analog scales filled out by the families three months after the injection showed a mean drooling value of 4.4 (Min: 3, Max: 9) and a mean frequency value of 4.6 (Min: 3, Max: 9) (Figure 1). The analysis showed significant reduction both in the severity and the frequency of sialorrhea in a majority of the patients after botulinum toxin type A injection. No complications were experienced in any of the patients after the procedure.
Figure 1.
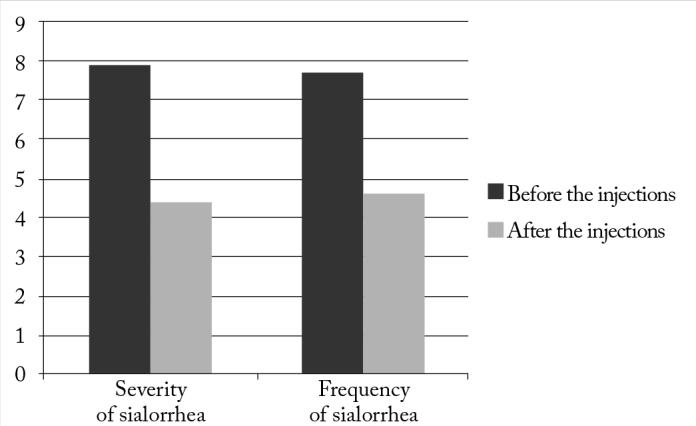
Severity and frequency of sialorrhea shown on the visual analog scale before and after the injections
Discussion
Efficacy of botulinum toxin, a potent neurotoxin that inhibits acetylcholine release, in sialorrhea was first reported in patients with Parkinson’s disease (10). There are many studies that report about the effectiveness of botulinum toxin injections into the parotid and the submandibular glands in the management of sialorrhea. Facial paralysis, however, is the major risk associated with this procedure. While local anesthesia is recommended in some studies, there are others that recommend, as we did in our study, to perform the procedure under general anesthesia or sedation (11, 12).
Many studies indicate that administering botulinum toxin injections in the right doses and at the right intervals are vital for the efficacy of the treatment, and discuss the impact of patient-related factors and the surgeon’s experience on the outcome (13–15). Research has shown that the dosage of injection to the salivary glands, and injecting botulinum toxin to the submandibular glands in addition to the parotid glands will increase the effectiveness of the treatment (14, 16). In our cases, the aim was to manage sialorrhea in a single dose, without increasing the dosage and by injecting botulinum toxin into both pairs of the parotid and submandibular glands. Many studies indicate that a need for booster injections arose in the long-term follow-up of patients (7, 11, 12).
Facial paralysis or another kind of complication associated with injection to the parotid glands was not encountered in any of our patients. One study reported effective results and a success rate of up to 89% in the management of sialorrhea with weight-based dosing strategy (17). There are also studies reporting of unsuccessful response in 30 to 50% of the cases when botulinum toxin was administered only to the submandibular glands (16, 18). Booster injections may be needed in some patients since the effect of the toxin is temporary. In our study we aimed to present the early results after a single dose of botulinum toxin.
There are studies that report ultrasound-guided administration of the injections to the submandibular glands could increase the success of the method by up to 80% (19). Another study describing ultrasound-guided administration of botulinum toxin injections in 111 patients reported that the method is safe and effective and could provide reduction in the rates of adverse events. The study reported a 68% success rate with this technique in the management of sialorrhea (20). Lack of ultrasound usage in the procedure and the short follow-up periods are major shortcomings of our study.
Conclusion
Botulinum toxin type A was found to be an effective, safe and less invasive method for the management of sialorrhea in pediatric patients.
Footnotes
This study was presented at the 38th National Otolaryngology head and neck surgery congress, October 26–30, 2016, Antalya, Turkey.
Ethics Committee Approval: Ethics committee approval was received for this study from the Ethics Committee of Çukurova University School of Medicine (04/Mayıs/2016 No: 4/2016).
Informed Consent: Written informed consent was obtained from the parents of patients who participated in this study.
Peer-review: Externally peer-reviewed.
Conflict of Interest: The authors have no conflicts of interest to declare.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Garnock-Jones KP. Glycopyrrolate oral solution: for chronic, severe drooling in pediatric patients with neurologic conditions. Paediatr Drugs. 2012;14:263–9. doi: 10.2165/11208120-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 2.Hamdy S, Aziz Q, Rothwell JC, Hobson A, Barlow J, Thompson DG. Cranial nerve modulation of human cortical swallowing motor pathways. Am J Physiol. 1997;272:802–8. doi: 10.1152/ajpgi.1997.272.4.G802. [DOI] [PubMed] [Google Scholar]
- 3.Johnson H, Scott A. Saliva Management. In: Cichero, JAY, Murdoch, BE, editors. Dysphagia: Foundation, Theory and Practice. John Wiley & Sons Ltd; West Sussex, UK: 2006. pp. 126–9. [Google Scholar]
- 4.Volonté MA, Porta M, Comi G. Clinical assessment of dysphagia in early phases of Parkinson’s disease. Neurol Sci. 2002;23:121–2. doi: 10.1007/s100720200099. [DOI] [PubMed] [Google Scholar]
- 5.Glickman S, Deaney CN. Treatment of relative sialorrhoea with botulinum toxin type A: description and rationale for an injection procedure with case report. Eur J Neurol. 2001;8:567–71. doi: 10.1046/j.1468-1331.2001.00328.x. [DOI] [PubMed] [Google Scholar]
- 6.Hung CC, Fu PK, Wang HY, Chan CH, Lan TH. Treatment effects of traditional Chinese medicines Suoquan Pill and Wuling Powder on clozapine-induced hypersalivation in patients with schizophrenia: study protocol of a randomized, placebo-controlled trial. Zhong Xi Yi Jie He Xue Bao. 2011;9:495–502. doi: 10.3736/jcim20110506. [DOI] [PubMed] [Google Scholar]
- 7.Scully C, Limeres J, Gleeson M, Tomás I, Diz P. Drooling. J Oral Pathol Med. 2009;38:321–7. doi: 10.1111/j.1600-0714.2008.00727.x. [DOI] [PubMed] [Google Scholar]
- 8.Holsinger FC, Bui DT. Anatomy, function and evaluation of the salivary glands. In: Myers EN, Ferris RL, editors. Salivary Gland Disorders. Berlin, Heidelberg: Springer; 2007. pp. 1–16. [Google Scholar]
- 9.Lin YC, Shieh JY, Cheng ML, Yang PY. Botulinum toxin type a for control of drooling in Asian patients with cerebral palsy. Neurology. 2008;70:316–8. doi: 10.1212/01.wnl.0000300421.38081.7d. [DOI] [PubMed] [Google Scholar]
- 10.Fairhurst CB, Cockerill H. Management of drooling in children. Arch Dis Child Educ Pract Ed. 2011;96:25–30. doi: 10.1136/adc.2007.129478. [DOI] [PubMed] [Google Scholar]
- 11.Pal PK, Calne DB, Calne S, Tsui JK. Botulinum toxin A as treatment for drooling saliva in PD. Neurology. 2000;54:244–7. doi: 10.1212/WNL.54.1.244. [DOI] [PubMed] [Google Scholar]
- 12.Wilken B, Aslami B, Backes H. Successful treatment of drooling in children with neurological disorders with botulinum toxin A or B. Neuropediatrics. 2008;39:200–4. doi: 10.1055/s-0028-1112115. [DOI] [PubMed] [Google Scholar]
- 13.Meece RW, Fishlock KF, Bayley EW, Keller MS. Ultrasound-guided Botox injections of salivary glands in children with drooling. J Radiol Nurs. 2010;29:20–4. doi: 10.1016/j.jradnu.2009.12.002. [DOI] [Google Scholar]
- 14.Hassin-Baer S, Scheuer E, Buchman AS, Jacobson I, Ben-Zeev B. Botulinum toxin injections for children with excessive drooling. J Child Neurol. 2005;20:120–3. doi: 10.1177/08830738050200020701. [DOI] [PubMed] [Google Scholar]
- 15.Marina MB, Sani A, Hamzaini AH, Hamidon BB. Ultrasound-guided botulinum toxin A injection: an alternative treatment for dribbling. J Laryngol Otol. 2008;122:609–14. doi: 10.1017/S0022215107008730. [DOI] [PubMed] [Google Scholar]
- 16.Jongerius PH, van den Hoogen FJ, van Limbeek J, Gabreels FJ, van Hulst K, Rotteveel JJ. The effect of botulinum toxin in the treatment of drooling: a controlled clinical trial. Pediatrics. 2004;114:620–7. doi: 10.1542/peds.2003-1104-L. [DOI] [PubMed] [Google Scholar]
- 17.Tiigimäe-Saar J, Leibur E, Kolk A, Talvik I, Tamme T. Use of botulinum neurotoxin A in uncontrolled salivation in children with cerebral palsy: a pilot study. Int J Oral Maxillofac Surg. 2012;41:1540–5. doi: 10.1016/j.ijom.2012.09.015. [DOI] [PubMed] [Google Scholar]
- 18.Jongerius PH, van Hulst K, van den Hoogen FJ, Rotteveel JJ. The treatment of posterior drooling by botulinum toxin in a child with cerebral palsy. J Pediatr Gastroenterol Nutr. 2005;41:351–3. doi: 10.1097/01.mpg.0000175565.61072.1a. [DOI] [PubMed] [Google Scholar]
- 19.Çiftçi T, Akıncı D, Yurttutan N, Akhan O. US-guided botulinum toxin injection for excessive drooling in children. Diagn Interv Radiol. 2013;19:56–60. doi: 10.4261/1305-3825.DIR.5940-12.1. [DOI] [PubMed] [Google Scholar]
- 20.Lungren MP, Halula S, Coyne S, Sidell D, Racadio JM, Patel MN. Ultrasound-guided Botulinum Toxin Type A salivary gland injection in children for refractory sialorrhea: 10-year experience at a large tertiary children’s hospital. Pediatr Neurol. 2016;54:70–5. doi: 10.1016/j.pediatrneurol.2015.09.014. [DOI] [PubMed] [Google Scholar]


