Abstract
We present a case report of a patient with severe valgus deformity of the right knee due to multiple hereditary exostoses (MHEs) treated with total knee arthroplasty (TKA). The surgical management of MHE affecting the knee encompasses exostoses resection, joint deformity rectification, and limb-length discrepancy alignment. On rare occasions, distraction osteogenesis and TKA have been used to correct valgus deformities of the knee. TKA in MHE patients with knee involvement has only been described in 6 cases. Several considerations, such as extensive knowledge of frequently occurring skeletal aberrations, are required to successfully correct the deformities associated with MHE via TKA. This report describes a case of severe valgus knee deformity with a rotational component in MHE managed with TKA, the surgical technique, and future recommendations.
Keywords: Exostoses, Knee, Arthroplasty, Replacement, Valgus, Total
Introduction
Multiple hereditary exostosis (MHE) is an autosomal dominant condition caused by a point mutation in the family of exostosin genes [1]. Mutations in the exostosin-1 gene are associated with more severe clinical manifestations along with an increased risk of malignant degeneration [2]. The overall prevalence of MHE is currently unknown due to many unreported asymptomatic cases. However, the approximated prevalence in Caucasian populations (the most widely studied population) spans from 0.9 to 2 individuals per 100,000 [3]. MHE is characterized by multiple pedunculated or sessile cartilage-capped bony outgrowths that may lead to joint deformities, restricted range of motion (ROM), and early-onset osteoarthritis [4]. Other associated findings are limb-length discrepancies, pectoral/pelvic asymmetry, and short stature, with limb-length discrepancies (10%-50%) and short stature (37%-44%) being the most prevalent [5], [6]. The clinical manifestations of MHE most commonly affect the long bones but may also affect the iliac crests, ribs, and scapulae [6]. The most common location of exostoses in MHE is the knee with prevalence of distal femur and proximal tibia involvement ranging from 70% to 98%. The fibula is less commonly involved with prevalence ranging from 30% to 97% [6]. Complications associated with MHE include: aneurysms/pseudoaneurysms, arterial/venous thrombosis, neurovascular compromise, and malignant degeneration [7].
It is a known fact that the knee is the most frequently affected joint, yet little is known about the surgical management of MHE with severe valgus deformities of the knee. Surgical management of MHE affecting the knee encompasses exostoses resection, joint deformity rectification, and limb-length discrepancy alignment [8]. On rare occasions, distraction osteogenesis and total knee arthroplasty (TKA) have been used to correct valgus deformities of the knee [1], [8], [9]. To our knowledge, only 6 reported cases of valgus deformity due to MHE have been managed via TKA [8], [9]. We present the first case of MHE with severe valgus deformity, in excess of 45°, corrected by TKA using metaphyseal sleeves and describe our surgical technique.
Case history
Preoperative evaluation
A 67-year-old Hispanic man, former smoker and construction worker presented to the clinic due to progressive bilateral knee pain and severe valgus angulation of the right knee. The patient stated that he began to notice aberrant growths on his right knee at age 12. However, the patient failed to seek medical advice due to lack of symptoms. Approximately 8 years before presentation, the patient began using a cane due to progressive bilateral knee pain and difficulty in walking. Family history revealed a daughter, brother, and 2 nephews who suffer from aberrant growths on the knees.
Upon physical examination, inspection of the right lower extremity revealed external rotation and severe valgus deformity of the knee, valgus angulation of the ankle, and no protruding or visible masses (Fig. 1). Palpation of the right knee elicited pain in the lateral compartment. Patellar evaluation failed to reveal hypermobility, hypomobility, or tilting. Evaluation of the peripheral vasculature resulted in findings within normal limits. Right knee ROM was 0°-120°. On valgus/varus stress test, the valgus deformity of the right knee was fixed and laxity of the medial collateral ligament (MCL) was identified. Evaluation of bilateral lower extremity motor function using the Oxford muscle grading scale was 3/5 for dorsiflexion of the right ankle. All other lower extremity movements were 5/5. Preoperative Knee Society Knee Score was 14 and Function Score was 55, for a total Knee Society Score of 69. Preoperative Western Ontario McMaster Score was 61.4.
Figure 1.
Preoperative standing clinical image.
Radiographic imaging using anteroposterior and lateral views showed 2 radiopaque sessile growths affecting the proximal medial and lateral portions of the right tibia and proximal fibula (Figs. 2 and 3). Using the anteroposterior radiograph, the valgus angulation of the right knee was determined by using the anatomical axis of the femur and tibia. Given the patient's clinical presentation, family history, and radiological findings, a clinical diagnosis of MHE was made and TKA was recommended. The patient was informed of the alternative treatment options, along with the risks and benefits associated with each alternative, and the patient consented to proceed with the TKA.
Figure 2.
Preoperative standing radiograph with anteroposterior view of the right knee exhibiting the severe valgus alignment and rotational component of the deformity.
Figure 3.
Preoperative standing radiograph with lateral view of the right knee elucidating the rotational component of the deformity.
Surgical technique
The surgery was performed by the senior author with the use of a tourniquet. Using standard instrumentation, the angle of bone resection, depth of resection, and femoral and tibial rotational alignment were carefully considered. The angle of bone resection was determined preoperatively via radiographic templating. Digital templating was not used.
We used an anterior midline incision and standard medial parapatellar arthrotomy. The medial dissection was limited to the articular level due to MCL laxity. Quadriceps snip was not required due to uncomplicated patellar eversion. Extra care was taken during medial retraction to avoid excessive strain on the MCL. This was followed by preparation of the femoral and tibial components.
The distal femoral cut was done at 5° of valgus, resulting in scant resection (2 mm) of distal lateral femur and 12-mm resection of medial femur. The proximal tibia cut was performed using 8 mm from the medial resection as reference. The extension gap obtained was asymmetric, and complete iliotibial band release was performed. The final measure of the extension gap was 17 mm. The transepicondylar axis was used to establish femoral rotation. Tibial rotational alignment was based on anatomic landmarks. Flexion-gap balancing required release of the popliteal tendon.
Trials were performed using rotating platform–constrained polyethylene insert. Symmetric opening in valgus and varus of less than 2 mm resulted. No instability in extension, mid-flexion, and flexion was encountered. Patellofemoral tracking was excellent using the “no thumb rule”. Lateral retinacular release was not performed.
Femoral and tibial canals were reamed until sufficient endosteal contact was obtained with a desired length of 75 mm. Metaphyseal sleeve preparation (DePuy Synthes, Warsaw, Indiana) with wider reamers and sequential broaching was the next step. Solid rotational fixation was obtained. A constrained hinge design prosthesis was immediately available, if it would have been necessary. Customized implants were not used.
Based on the intraoperative findings, a constrained condylar knee DePuy Synthes revision system with rotating platform prosthesis was selected for implantation. The final components were fixed by applying cement only on the articular surface of the tibial plateau as the sleeves and fluted stems allowed biologic fixation. Care was taken to prevent cement from spreading to the in-growth surface of the porous titanium sleeve. Postoperative neurovascular check reported ipsilateral ankle dorsiflexion comparable to preoperative ROM. Full extension and 90° of flexion was obtained before discharge to an inpatient rehabilitation facility with instructions for standard preoperative care, weight-bearing, and ROM as tolerated.
Postoperative evaluation
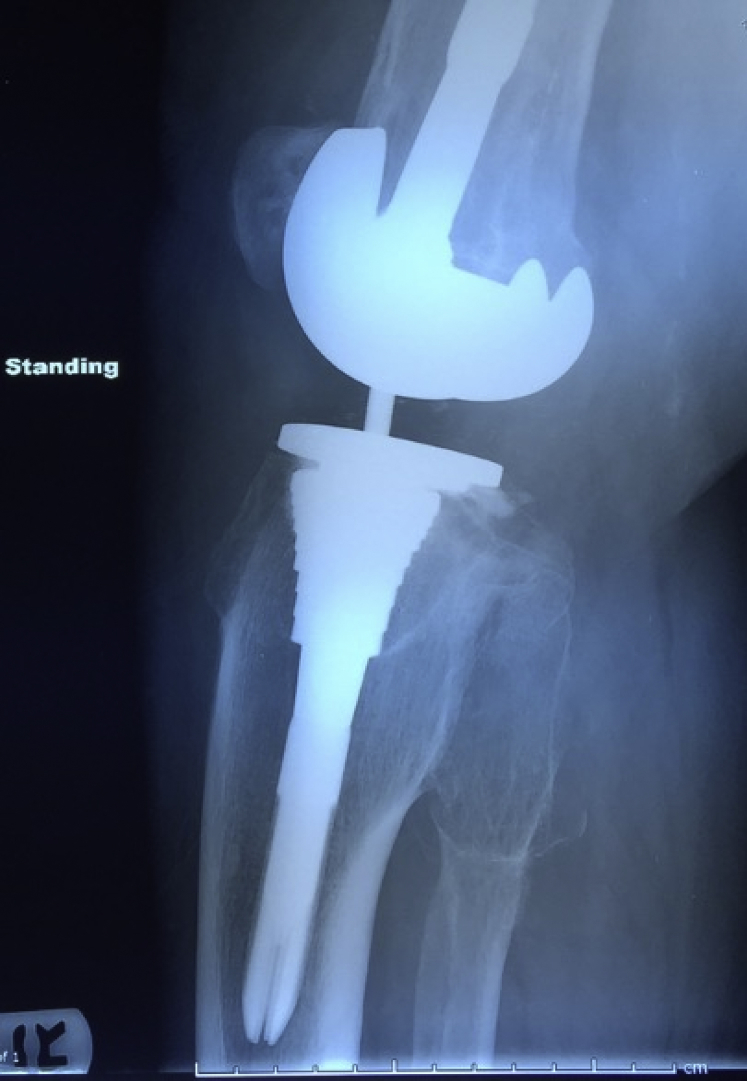
Postoperative evaluation at 6 months revealed correction of the valgus deformity (Fig. 4), right knee ROM was 10°-105°, and ipsilateral ankle dorsiflexion was equivalent to that observed during preoperative evaluation. Postoperative radiographic imaging using anteroposterior and lateral views demonstrated proper anatomical alignment and no signs of prosthesis loosening (Figs. 5 and 6). Postoperative Knee Society Knee Score was 82 and Function Score was 65, for a total Knee Society Score of 147. Postoperative Western Ontario McMaster score was 90.2. There were no other reported postoperative complications, and the patient stated that he was able to perform his normal daily activities without difficulty. The patient provided the authors with informed consent to report this case in the literature.
Figure 4.
Postoperative standing clinical image at 6 months follow-up demonstrating correction of severe valgus alignment and rotational deformity.
Figure 5.
Postoperative standing radiograph with anteroposterior view of the right knee at 6 months follow-up displaying anatomical alignment.
Figure 6.
Postoperative standing radiograph with lateral view of the right knee at 6 months follow-up demonstrating anatomical alignment.
Discussion
MHE is a condition that most commonly affects the long and flat bones, often leading to severe deformities that may complicate the surgical management of these patients. The majority of patients with MHE and knee involvement are managed with removal of the exostoses, rectification of joint deformities, and alignment of limb-length discrepancies [8]. However, only 6 cases of MHE with knee involvement managed with TKA have been reported. When considering the use of TKA in patients with MHE involving the knee, several considerations are required.
One consideration when contemplating TKA in MHE patients with knee involvement is ensuring that the surgeon has a thorough comprehension of frequently occurring skeletal aberrations associated with MHE. A detailed understanding of this concept is necessary for adequate preoperative planning and subsequent surgical management. Given that genu valgus deformity is a frequent complication in patients with MHE, it is imperative to consider this possibility during surgical planning. In our case, the genu valgus deformity with rotational accentuation and the chondral masses mandated meticulous attention to preoperative planning and extensive knowledge of the fundamental principles of managing severe skeletal deformity. Essential aspects of preoperative planning include precise templating, comprehensive assessment of bony dimensions, and availability of various implant sizes or custom implants. In patients of smaller stature, a detailed evaluation of the bony dimensions is crucial to determine if custom implants are necessary [9]. In our case, we used a constrained condylar knee rotating platform DePuy Synthes Revision system with metaphyseal sleeves, and custom implants were not required. However, a constrained hinge design prosthesis was readily available if we were to require it. Furthermore, the use of digital templating may be used as an adjuvant for preoperative planning to improve accuracy for actual implant size prediction and determining an adequate origin in selecting implant size and position [10]. Kim et al.[9] used computer navigation in managing achondroplasia with TKA in anticipation of possible complications with intramedullary instrumentation due to considerable femoral bowing and varus deformities. In our case, digital templating was not used and, to our knowledge, digital templating was not used in any of the previous cases of TKA in MHE with knee involvement. Digital templating should be considered when confronted with a similar situation in the future.
Additionally, it is vital that all painful lesions be carefully assessed for malignant degeneration. This can be completed via bone scan with subsequent pathologic evaluation or pathological evaluation alone. The removed exostoses were sent for pathological analysis and the results were negative for malignancy. We did not perform a bone scan on this patient.
Moreover, the surgeon should be prepared for encountering soft-tissue imbalances. In the previous 6 cases of MHE with knee involvement managed with TKA, 5 of 6 cases required soft-tissue release to obtain adequate ligamentous balancing [8], [9]. Our case required iliotibial band and popliteal tendon release to balance the extension and flexion gaps. If soft-tissue release is not sufficient to achieve symmetric extension and flexion gaps, there are several alternatives that the surgeon may use. A lateral epicondylar sliding osteotomy is one approach that may be used to obtain symmetric extension and flexion gaps [11]. Another option that may be used to achieve adequate symmetry of the extension and flexion gaps is to augment the constraint by using a varus-valgus constraining tibial insert [9]. In the case of global ligamentous laxity, a hinge may be used to achieve adequate stability and symmetric extension and flexion gaps [12]. We were able to achieve symmetric extension and flexion gaps with soft-tissue release and did not require the use of a lateral epicondylar sliding osteotomy or hinge. Although the patient suffered from significant ligamentous laxity, replacement of bone and cartilage loss with femoral and tibial components compensated for damage caused by long-standing genu valgus deformity eliminating the need for a constrained hinge design prosthesis.
Similarly, it is possible to encounter patellar maltracking in the valgus knee due to ligamentous contracture. If confronted with patellar maltracking, realignment of the proximal extensor mechanism may be performed through a lateral retinacular release, patellar resurfacing, reconstruction of the medial patellofemoral ligament, or tibial tuberosity transfer [13], [14]. We did not use any of these surgical techniques because of adequate central patellar tracking achieved through soft-tissue release.
In addition, the use of metaphyseal sleeves should be considered due to its associated benefits. Metaphyseal sleeves have been primarily used for hinged knee arthroplasty and revision TKA in the past, with indications including bone loss, increasing stability of prosthesis-bone construct, and providing long-term fixation of the implant to bone [15], [16]. In the setting of revision TKA, metaphyseal sleeves are often used for correction of bony defects, epiphyseal damage upon implant removal, epiphyseal fixation protection, improvement of rotational stability, and obtaining stable fixation [16], [17], [18], [19], [20]. More recently, metaphyseal sleeves have been modified to permit their use with semi-constrained revision implants [15]. To our knowledge, this was the first case of valgus deformity in a patient with MHE managed with TKA using metaphyseal sleeves. The use of metaphyseal sleeves in this patient provided several advantages, such as allowing solid metaphyseal fixation with the use of shorter stems. In this case, the application of metaphyseal sleeves allowed us to avoid femoral and tibial diaphyseal deformities. Moreover, the biologic rigid fixation obtained with osseous integration provides a base for increased durability when using higher levels of constraint. Furthermore, metaphyseal sleeves avoid the potential complications of cemented block and wedge augments and potential disease transmission of allografts [17].
Finally, due to the presence of bony defects in patients with MHE, it is likely that additional bone may need to be cut to correct these deformities. Resection of additional bone may be corrected with tibial augments [21]. In our case, resection of additional bone was not required due to the location of the exostoses not interfering with the femoral or tibial cuts.
Current controversies and future considerations
The ideal management for patients with MHE affecting the knee currently remains unclear. The orthopaedic surgeon should consider management options on a case-by-case basis. Resection of exostoses with satisfactory pathological analysis would be the best surgical option for MHE patients suffering from knee pain without joint deformity. Distraction osteogenesis or TKA would be a suitable surgical option for MHE patients suffering from limb-length discrepancies. TKA should be the choice of surgical intervention for patients with MHE suffering from knee joint deformity.
When considering TKA in MHE patients with knee deformity, only orthopaedic surgeons with extensive experience in skeletal deformities should attempt surgical intervention placing great emphasis on digitalized preoperative templating, precise measuring of bony dimensions, deformity correction, and ligamentous balancing.
Summary
The current literature on arthroplasty in patients with MHE affecting the knee is limited. Owing to the unusual anatomy often associated with MHE, the surgical approach in these situations must be cautious with great attention to detail and adequate preoperative planning. We recommend that only surgeons with prior experience in correcting skeletal deformities perform TKA in patients with MHE. Despite the extensive technical considerations required to successfully perform TKA in patients with MHE, TKA is a suitable alternative to restore adequate function and alleviate pain in this patient population. Currently, there are studies addressing correction of extra-articular deformities of MHE. However, there are no large cohort studies focusing on functional outcomes and long-term follow-up of TKA in patients with MHE. Additional studies are needed to support TKA as a consistent management alternative in patients with MHE and knee involvement. The case presented serves to further solidify TKA as an acceptable means of correcting the severe deformities observed in patients with MHE affecting the knees.
Key points.
-
•
MHE most commonly affects the knee and may lead to joint deformities, restricted ROM, and early-onset osteoarthritis.
-
•
Surgical management of MHE includes exostoses resection, joint deformity rectification, limb-length discrepancy alignment, distraction osteogenesis, and TKA.
-
•
Only orthopaedic surgeons with considerable experience in extra-articular and intra-articular deformities should attempt to correct joint deformities in MHE patients.
-
•
Although TKA has not been widely used as a surgical option for MHE patients, TKA should be considered more often in this patient subset given the current outcomes.
Footnotes
No author associated with this article has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2017.11.008.
Appendix A. Supplementary data
References
- 1.Ofiram E., Eylon S., Porat S. Correction of knee and ankle valgus in hereditary multiple exostoses using the Ilizarov apparatus. J Orthop Traumatol. 2008;9:11. doi: 10.1007/s10195-008-0098-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jennes I., Pedrini E., Zuntini M. Multiple osteochondromas: mutation update and description of the multiple osteochondromas mutation database (MOdb) Hum Mutat. 2009;30:1620. doi: 10.1002/humu.21123. [DOI] [PubMed] [Google Scholar]
- 3.Thompson R.L., Hosseinzadeh P., Muchow R.D. Syringomyelia and vertebral osteochondromas in patients with multiple hereditary exostosis. J Pediatr Orthop B. 2014;23:449. doi: 10.1097/BPB.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 4.Schmale G.A., Conrad E.U., 3rd, Raskind W.H. The natural history of hereditary multiple exostoses. J Bone Joint Surg Am. 1994;76:986. doi: 10.2106/00004623-199407000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Bovee J.V. Multiple osteochondromas. Orphanet J Rare Dis. 2008;3:3. doi: 10.1186/1750-1172-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stieber J.R., Dormans J.P. Manifestations of hereditary multiple exostoses. The J Am Acad Orthop Surg. 2005;13:110. doi: 10.5435/00124635-200503000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Delgado M.A., Martinez-Domenech G., Sarrion P. A broad spectrum of genomic changes in latinamerican patients with EXT1/EXT2-CDG. Sci Rep. 2014;4:6407. doi: 10.1038/srep06407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mesfin A., Goddard M.S., Tuakli-Wosornu Y.A. Total hip and knee arthroplasty in patients with hereditary multiple exostoses. Orthopedics. 2012;35:e1807. doi: 10.3928/01477447-20121120-29. [DOI] [PubMed] [Google Scholar]
- 9.Kim R.H., Scuderi G.R., Dennis D.A. Technical challenges of total knee arthroplasty in skeletal dysplasia. Clin Orthop Relat Res. 2011;469:69. doi: 10.1007/s11999-010-1516-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller A.G., Purtill J.J. Accuracy of digital templating in total knee arthroplasty. Am J Orthop (Belle Mead NJ) 2012;41:510. [PubMed] [Google Scholar]
- 11.Brilhault J., Lautman S., Favard L. Lateral femoral sliding osteotomy lateral release in total knee arthroplasty for a fixed valgus deformity. J Bone Joint Surg Br. 2002;84:1131. doi: 10.1302/0301-620x.84b8.12824. [DOI] [PubMed] [Google Scholar]
- 12.Yang J.H., Yoon J.R., Oh C.H. Primary total knee arthroplasty using rotating-hinge prosthesis in severely affected knees. Knee Surg Sports Traumatol Arthrosc. 2012;20:517. doi: 10.1007/s00167-011-1590-1. [DOI] [PubMed] [Google Scholar]
- 13.Gasparini G., Familiari F., Ranuccio F. Patellar malalignment treatment in total knee arthroplasty. Joints. 2013;1:10. [PMC free article] [PubMed] [Google Scholar]
- 14.Momoli A., Modena M., Giaretta S. Extensor mechanism realignment procedures in the treatment of patellofemoral instability. Joints. 2013;1:21. [PMC free article] [PubMed] [Google Scholar]
- 15.Bugler K.E., Maheshwari R., Ahmed I. Metaphyseal sleeves for revision total knee arthroplasty: good short-term outcomes. J Arthroplasty. 2015;30:1990. doi: 10.1016/j.arth.2015.05.015. [DOI] [PubMed] [Google Scholar]
- 16.Chen A.F., Pagnotto M.R., Crossett L.S. Metaphyseal sleeves in revision total knee arthroplasty. Oper Tech Orthop. 2012;22:203. [Google Scholar]
- 17.Alexander G.E., Bernasek T.L., Crank R.L. Cementless metaphyseal sleeves used for large tibial defects in revision total knee arthroplasty. J Arthroplasty. 2013;28:604. doi: 10.1016/j.arth.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 18.Barnett S.L., Mayer R.R., Gondusky J.S. Use of stepped porous titanium metaphyseal sleeves for tibial defects in revision total knee arthroplasty: short term results. J Arthroplasty. 2014;29:1219. doi: 10.1016/j.arth.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 19.Chalmers B.P., Desy N.M., Pagnano M.W. Survivorship of metaphyseal sleeves in revision total knee arthroplasty. J Arthroplasty. 2017;32:1565. doi: 10.1016/j.arth.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Haidukewych G.J., Hanssen A., Jones R.D. Metaphyseal fixation in revision total knee arthroplasty: indications and techniques. J Am Acad Orthop Surg. 2011;19:311. doi: 10.5435/00124635-201106000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Baek S.W., Kim C.W., Choi C.H. Management of tibial bony defect with metal block in primary total knee replacement arthroplasty. Knee Surg Relat Res. 2013;25:7. doi: 10.5792/ksrr.2013.25.1.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.