Abstract
Background
Medicaid payer status has been shown to affect resource utilization across multiple medical specialties. There is no large database assessment of Medicaid and resource utilization in primary total knee arthroplasty (TKA), which this study sets out to achieve.
Methods
The Nationwide Readmissions Database was used to identify patients who underwent TKA in 2013 and corresponding “Medicaid” or “non-Medicaid” payer statuses. Demographics, 15 individual comorbidities, readmission rates, length of stay, and direct cost were evaluated. A propensity score–based matching model was then used to control for baseline confounding variables between payer groups. A chi-square test for paired proportions was used to compare readmission rates between the 2 groups. Length of stay and direct cost comparisons were evaluated using the Wilcoxon signed-rank test.
Results
A total of 8372 Medicaid and 268,261 non-Medicaid TKA patients were identified from the 2013 Nationwide Readmissions Database. A propensity score was estimated for each patient based on the baseline demographics, and 8372 non-Medicaid patients were propensity score matched to the 8372 Medicaid patients. Medicaid payer status yielded a statistically significant increase in overall readmission rates of 18.4% vs 14.0% (P < .0001, relative risk = 1.31, 95% confidence interval [1.23-1.41]) with non-Medicaid status and 90-day readmission rates of 10.0% vs 7.4%, respectively (P < .001, relative risk = 1.35, 95% confidence interval [1.22-1.48]). The mean length of stay was longer in the Medicaid group compared with the non-Medicaid group at 4.0 days vs 3.3 days (P < .0001) as well as the mean total cost of $64,487 vs $61,021 (P < .0001).
Conclusions
This study demonstrates that Medicaid payer status is independently associated with increased resource utilization, including readmission rates, length of stay, and total cost after TKA.
Keywords: Primary total knee arthroplasty, Medicaid, Insurance status, Resource utilization, Readmission
Introduction
Over the last 6 decades, the Medicaid program has grown from a health-care coverage program for welfare recipients into a large public health insurance program for low-income and disabled Americans [1]. Medicaid now provides coverage for over 72 million patients and is the single largest health insurance plan in the United States [2]. The Affordable Care Act (ACA) further expanded the Medicaid program by creating a national Medicaid minimum eligibility level of 133% of the federal poverty level beginning in 2014, which has been estimated to increase the number of covered individuals younger than 65 years of age by approximately 12 million [3], [4]. Total knee arthroplasty (TKA) is among the largest and fastest growing health-care expenditures, accounting for nearly $3 billion in Medicare reimbursement in 2013 alone [5], [6]. Recent health-care reform has tasked hospitals, surgeons, and policymakers to reduce cost while maintaining quality in TKA. Medicare programs such as the Medicare Bundled Payment for Care Improvement Initiative and the Comprehensive Care for Joint Replacement Model aim to align incentives to contain costs through bundling payments for an episode of care from the time of surgery through 90 days after discharge [7], [8], [9]. While the early results of these alternative payment models (APMs) seem promising [10], concern remains regarding patient selection and access to care [11].
Medicaid insurance status and lower socioeconomic status have repeatedly been shown to affect risk-adjusted outcomes and resource utilization across multiple medical specialties [12], [13], [14]. Varying explanations for this finding have described this disparity including complex interaction between socioeconomic status, access to care, patient factors, and clinical outcome measures. Data have been limited to small retrospective studies that suggest Medicaid patients who undergo total joint arthroplasty are more likely to have a longer length of stay, disposition to a rehabilitation facility, and increased readmission within 90 days [15], [16]. Despite evidence that patients with Medicaid status require more resources at increased cost, payers have yet to provide adjustment in reimbursement based on Medicaid payer status. With the increasing prevalence of APMs, there may be a disincentive to perform TKAs on patients with Medicaid status.
The primary purpose of this study was to examine the 90-day readmission rates associated with Medicaid versus non-Medicaid payer status after TKA and a secondary purpose to assess overall readmission, length of stay, and total cost between the 2 cohorts. A large, national administrative database was used to achieve a comprehensive analysis and allow Medicaid patients to be matched one-to-one with control patients who differed only in payer status. This study uniquely examines Medicaid payer status as an independent risk factor for morbidity and increased resource utilization at a national level and is the largest patient sample to date. The primary hypothesis is that Medicaid payer status results increased 90-day readmission rates specific to knee replacement, increased all-cause 90-day comorbidity, longer length of stay with increased resource utilization and total cost compared with a matched cohort of control patients with other payer profiles.
Material and methods
The Nationwide Readmissions Database (NRD) was used to identify patients who underwent primary TKA (International Classification of Diseases-9 code 8154) in 2013 as well as corresponding “Medicaid” or “non-Medicaid” payer statuses. The NRD is part of the federal-, state-, and industry-sponsored Healthcare Cost and Utilization Project and created to allow for analyses of national readmission rates across the United States, accounting for 49.1% of all U.S. hospitalizations. Demographics (age, gender, severity of illness, discharge to skilled facility), 15 individual risk factors/comorbidities (smoking, AIDS, alcohol abuse, deficiency anemia, rheumatoid arthritis, chronic blood loss anemia, congestive heart failure, chronic pulmonary disease, coagulopathy, depression, diabetes, peripheral vascular disorders, drug abuse, weight loss, infection), readmission rates, length of stay, and direct cost were evaluated. A propensity score–based matching model was then used to control for baseline confounding variables between payer groups [17], [18]. Propensity scores were estimated using binary logistic regression with type of insurance as the dependent variable or outcome variable (ie, the exposure groups). The independent variables for the propensity score model included covariates potentially associated with type of insurance and outcomes. Using the resulting logistic regression equation, the propensity score was calculated as the probability of each patient being in the Medicaid group.
Using only the propensity score, Medicaid cases were matched one-to-one to other insurance types using a greedy matching strategy [19]. In this approach, a Medicaid subject is randomly selected, and the control patient (other insurance type) with the closest propensity score that lies within a fixed distance (the propensity score caliper) of the Medicaid subject's propensity score is selected for matching. For these analyses, patients were matched on the logit of the propensity score using a caliper of 0.2 standard deviations of the logit of the propensity score [20]. Standardized differences were used to assess the balance of confounders between the 2 exposure groups.
Standardized differences were defined as the difference in means between the 2 exposure groups divided by a measure of the standard deviation of the variable and were computed for both continuous (ie, age) and binary covariates. Standardized differences are preferred to significance testing (to assess the balance of confounders between the 2 exposure groups) because they are in units of the pooled standard deviation, so they allow for comparisons on the same scale and not influenced by the sample size. The magnitude of the difference in the paired proportions is small even though several of the P values from the McNemar's test was statistically significant (mainly because of the large sample sizes). A standardized difference less than 0.1 suggests negligible difference in the mean or prevalence of a covariate between the 2 insurance groups in the propensity score–matched sample. Additional details on assessing the balance produced by the propensity model are shown in Figure 1, Figure 2, Figure 3. The final step involved estimating the effect of exposure on outcomes, which was readmission (overall readmission and 90-day readmission data were obtained) after TKA. Multivariable regression is not necessary because matching on the propensity scores addressed confounding. The relative risk (RR) and its 95% confidence interval for readmission were calculated based on the two-by-two table for matched pairs, where the outcome is readmission and the predictor is type of insurance. A RR estimate above 1.0 suggests Medicaid patients were at higher risk of readmission after TKA than patients with other types of insurance. Total hospital costs were calculated using the cost-to-charge ratio provided by the Healthcare Cost and Utilization Project files. Length of stay and total cost comparisons were evaluated using the Wilcoxon signed-rank test.
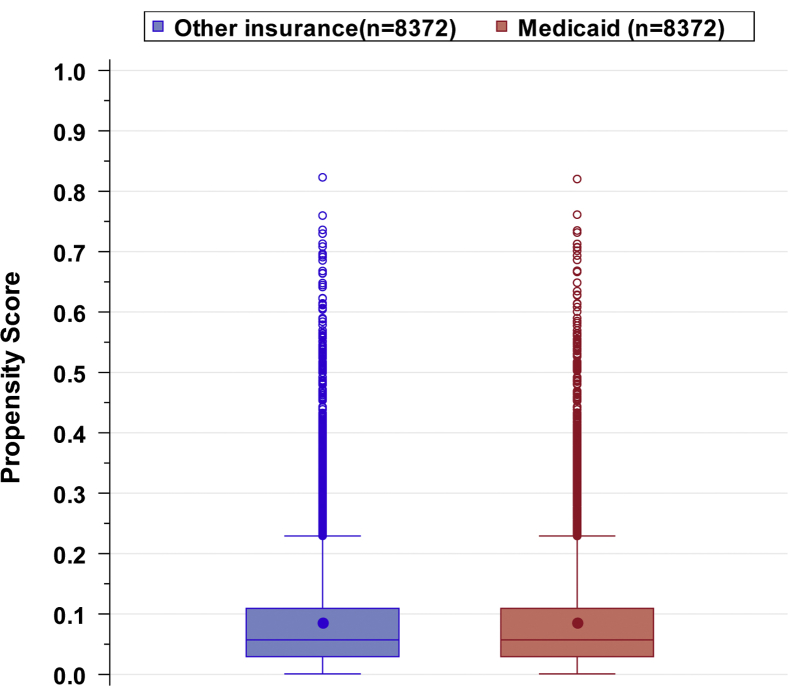
Figure 1.
Evaluation of common support using distributions of propensity scores by type of insurance. The degree to which the propensity score has been appropriately specified was ascertained through evaluation of common support. Common support is defined by overlapping distributions of propensity scores between insurance groups. Overlap in the propensity score distributions indicates the potential for a patient in the Medicaid group to be in the “other” insurance group and that patients with each level of covariates may have either exposure status (ie, supporting the assumptions of exchangeability and positivity). A lack of common support or a complete separation of propensity scores without any overlap between the 2 exposure groups (ie, Medicaid patients and patients with “other” types of insurance) indicates severe differences between the 2 exposure groups and the possibility that confounding cannot be reduced using propensity methods. This boxplot demonstrates overlapping ranges of the boxplots of propensity scores between Medicaid patients and patients with “other” types of insurance, which indicates that the propensity model exhibits common support. Circles within each boxplot denote the mean score. The middle line within the box represents the median, the top line represents the 75th percentile, and the bottom line represents the 25th percentile. The upper fence is defined as the third quartile (represented by the upper edge of the box) plus 1.5 times the interquartile range. The lower fence is defined as the first quartile (represented by the lower edge of the box) minus 1.5 times the interquartile range. Observations outside the fences are identified with an open circle.
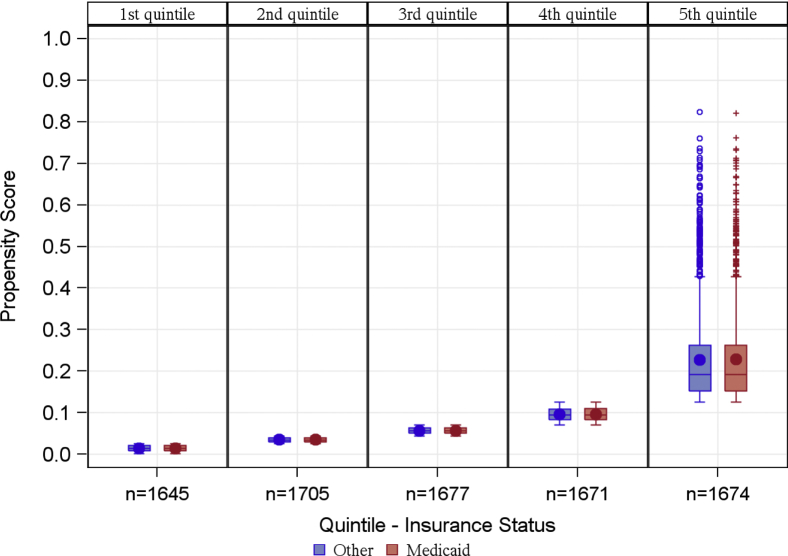
Figure 2.
Distribution of propensity scores by quintiles and type of insurance. Boxplot demonstrates distribution of propensity scores among Medicaid patients and patients with other types of insurance by quintiles of propensity scores. Circles within each boxplot denote the mean score. The middle line within the box represents the median, the top line represents the 75th percentile, and the bottom line represents the 25th percentile. The upper fence is defined as the third quartile (represented by the upper edge of the box) plus 1.5 times the interquartile range. The lower fence is defined as the first quartile (represented by the lower edge of the box) minus 1.5 times the interquartile range. Observations outside the fences are identified with an open circle.
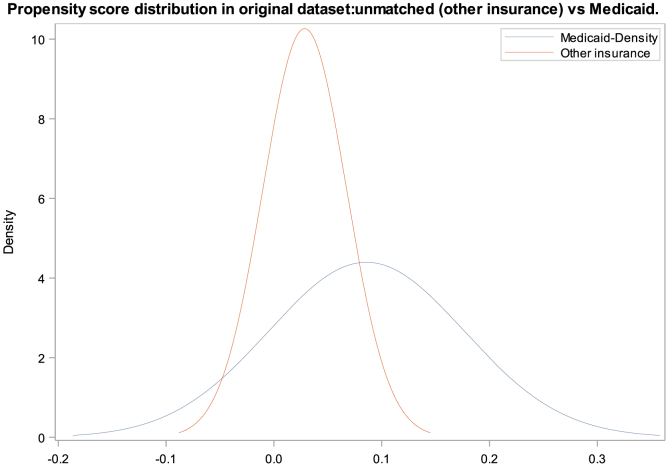
Figure 3.
Propensity score distribution of Medicaid vs non-Medicaid insurance in original unmatched datasets and matched datasets.
Results
A total of 8372 Medicaid and 268,261 non-Medicaid TKA patients were identified from the 2013 NRD. A propensity score was estimated for each patient based on the available baseline characteristics, and 8372 non-Medicaid patients were propensity score matched to the 8372 Medicaid patients. A summary of patient baseline characteristics and risk factors/comorbidities is provided in Table 1. All standardized differences were less than 0.1, suggesting negligible differences in the mean or prevalence of all patient characteristics and comorbidities between the Medicaid and non-Medicaid groups. Medicaid payer status yielded a statistically significant increase in overall readmission rates of 18.4% vs 14.0% non-Medicaid (P < .0001, RR = 1.31, 95% confidence interval [1.23-1.41]) and yielded a statistically significant increase in 90-day readmission rates of 10.0% vs 7.4%, respectively (P < .001, RR = 1.35, 95% confidence interval [1.22-1.48]). A RR estimate above 1.0 suggests Medicaid patients were at higher risk of readmission after TKA than patients with other types of insurance, which suggest that the risk of readmission at any time period is 31% higher for TKA patients with Medicaid insurance compared to patients with other types of insurance. The risk of readmission within 90 days is 35% higher for TKA patients with Medicaid insurance compared to TKA patients with other types of insurance. Tables 2 and 3 summarize the overall and 90-day readmission outcomes in propensity score–matched Medicaid vs non-Medicaid patients. The mean length of stay was longer in Medicaid group compared with non-Medicaid group at 4.0 days vs 3.3 days (P < .0001) and mean direct cost of $64,487 vs $61,021 (P < .0001). Tables 4 and 5, respectively, summarizes these findings.
Table 1.
Characteristics of the TKA (ICD-9 code 8154) patients from the 2013 NRD.
| Risk factors | Before propensity matching |
After propensity matching |
||||||
|---|---|---|---|---|---|---|---|---|
| Medicaid, N = 8372 | Other insurance, n = 268,261 | P Value | Standardized difference | Medicaid, n = 8372 | Other insurance, n = 8372 | P valuea | Standardized differenceb | |
| Age, years (mean ± SD) | 56.7 ± 9.4 | 66.7 ± 9.7 | <.0001 | 1.055 | 56.7 ± 9.4 | 56.5 ± 9.6 | <.001 | 0.014 |
| Female sex | 6072 (72.5%) | 165,227 (61.6%) | <.0001 | 0.234 | 6071 (72.5%) | 6129 (73.2%) | .004 | 0.016 |
| Severity of illness (major/extreme loss vs other) | 549 (6.6%) | 13,685 (5.1%) | <.0001 | 0.062 | 547 (6.5%) | 477 (5.7%) | <.001 | 0.035 |
| Discharged to skilled facility | 2118 (25.3%) | 75,028 (28.0%) | <.0001 | 0.061 | 2118 (25.3%) | 2142 (25.6%) | .261 | 0.007 |
| Smoking | 2711 (32.4%) | 59,997 (22.4%) | <.0001 | 0.226 | 2710 (32.4%) | 2664 (31.8%) | .038 | 0.012 |
| Comorbidities | ||||||||
| AIDS | 9 (0.1%) | 46 (0.0%) | <.0001 | 0.036 | 9 (0.1%) | 4 (0.0%) | .166 | 0.021 |
| Alcohol abuse | 201 (2.4%) | 2490 (0.9%) | <.0001 | 0.115 | 201 (2.4%) | 148 (1.8%) | <.001 | 0.044 |
| Deficiency anemia | 1049 (12.5%) | 29,855 (11.1%) | <.0001 | 0.043 | 1048 (12.5%) | 1055 (12.6%) | .730 | 0.003 |
| Rheumatoid arthritis | 458 (5.5%) | 11,102 (4.1%) | <.0001 | 0.062 | 457 (5.5%) | 414 (4.9%) | .008 | 0.023 |
| Chronic blood loss anemia | 92 (1.1%) | 3227 (1.2%) | .388 | 0.010 | 92 (1.1%) | 90 (1.1%) | .821 | 0.002 |
| Congestive heart failure | 203 (2.4%) | 6289 (2.3%) | .635 | 0.005 | 203 (2.4%) | 170 (2.0%) | .019 | 0.027 |
| Chronic pulmonary disease | 2100 (25.1%) | 38,992 (14.5%) | <.0001 | 0.267 | 2100 (25.1%) | 2056 (24.6%) | .055 | 0.012 |
| Coagulopathy | 163 (1.9%) | 5493 (2.0%) | .520 | 0.007 | 163 (1.9%) | 134 (1.6%) | .025 | 0.026 |
| Depression | 1676 (20.0%) | 34,767 (13.0%) | <.0001 | 0.191 | 1675 (20.0%) | 1658 (19.8%) | .416 | 0.005 |
| Diabetes | 2179 (26.0%) | 57,641 (21.5%) | <.0001 | 0.107 | 2179 (26.0%) | 2152 (25.7%) | .222 | 0.007 |
| Peripheral vascular disorders | 101 (1.2%) | 6613 (2.5%) | <.0001 | 0.094 | 101 (1.2%) | 67 (0.8%) | <.001 | 0.041 |
| Drug abuse | 257 (3.1%) | 1437 (0.5%) | <.0001 | 0.191 | 256 (3.1%) | 194 (2.3%) | <.001 | 0.046 |
| Weight loss | 47 (0.6%) | 1130 (0.4%) | .053 | 0.020 | 47 (0.6%) | 42 (0.5%) | .553 | 0.008 |
| Infection | 118 (1.4%) | 1977 (0.7%) | <.0001 | 0.065 | 118 (1.4%) | 114 (1.4%) | .728 | 0.004 |
McNemar's test (a chi-square test for paired proportions). The difference in paired proportions is small for all covariates but statistically significant for several covariates because of the large sample size.
A standardized difference less than 0.10 suggests negligible difference in the mean or prevalence of a covariate between the 2 insurance groups.
Table 2.
Overall readmissions in propensity score–matched Medicaid vs non-Medicaid patients.
| Readmitted (Medicaid) | Not readmitted (Medicaid) | Total | |
|---|---|---|---|
| Readmitted (non-Medicaid) | 251a | 919b | 1170 |
| Not readmitted (non-Medicaid) | 1287c | 5915d | 7202 |
| Total | 1538 | 6834 | 8372 pairs(n) |
| Paired proportion Pm: a+c/n | 1538/8372 (0.1837) |
| Paired proportion P0: a+b/n | 1170/8372 (0.1398) |
| RR = (a+c)/(a+b) = 1.31 | |
| RR (95% confidence interval) | 1.31 (1.23, 1.41) P = <.001 |
Sum of Medicaid and non-Medicaid readmitted patients.
Sum of Medicaid not readmitted and non-Medicaid readmitted.
Sum of Medicaid readmitted and non-Medicaid not readmitted.
Sum of Medicaid and non-Medicaid not readmitted.
Table 3.
Ninety-day readmissions in propensity score–matched Medicaid vs non-Medicaid patients.
| Readmitted (Medicaid) | Not readmitted (Medicaid) | Total | |
|---|---|---|---|
| Readmitted (non-Medicaid) | 96a | 525b | 621 |
| Not readmitted (non-Medicaid) | 741c | 7010d | 7751 |
| Total | 837 | 7535 | 8372 pairs(n) |
| Paired proportion Pm: a+c/n | 837/8372 (0.1000) |
| Paired proportion P0: a+b/n | 621/8372 (0.0742) |
| RR = (a+c)/(a+b) = 1.35 | |
| RR (95% confidence interval) | 1.35 (1.22, 1.48) P = <0.001 |
Sum of Medicaid and non-Medicaid readmitted patients.
Sum of Medicaid not readmitted and non-Medicaid readmitted.
Sum of Medicaid readmitted and non-Medicaid not readmitted.
Sum of Medicaid and non-Medicaid not readmitted.
Table 4.
Comparison of total cost after TKA between Medicaid and non-Medicaid patients (n = 8372).
| Total cost | Medicaid (95% CI) | Other insurance (95% CI) | Difference (95% CI) | P-value |
|---|---|---|---|---|
| Median | 54,983 (54,107-55,783) | 51,463 (50,785-52,092) | 2194 (1216-3113) | <.0001a |
| Mean | 64,487 (63,575-65,398) | 61,021 (60,232-61,809) | 3466 (2274-4657) | <.0001b |
| STD | 41,654 | 36,027 | 54,442 | |
| IQR | 41,245 | 35,536 | 50,899 |
CI, confidence interval; IQR, interquartile range; STD, standard deviation.
P-value from Wilcoxon signed-rank test.
P-value from paired t-test.
Table 5.
Comparison of length of stay after TKA between Medicaid and non-Medicaid patients (n = 8372).
| Length of stay | Medicaid (95% CI) | Other insurance (95% CI) | Difference (95% CI) | P-value |
|---|---|---|---|---|
| Mean | 3.98 (3.91-4.06) | 3.34 (3.29-3.39) | 0.64 (0.55-0.73) | <.0001a |
| STD | 3.58 | 2.39 | ||
| IQR | 1 | 1 |
CI, confidence interval; IQR, interquartile range.
P-value from paired t-test.
Discussion
With continued health-care reform and the ACA, it is expected that Medicaid will expand to millions of uninsured Americans [21]. With this growth, it is expected that the states will be required to fund approximately 10% of the expansion by 2020. In an effort to decrease cost, APMs, such as bundled payments, may become more prevalent. Although the ACA has allowed APMs for Medicaid patients in some states, these models have not been readily adopted for arthroplasty patients as cost data for Medicaid patients are sparse. This study demonstrates that Medicaid payer status is independently associated with increased morbidity and resource utilization following TKA after adjusting for comorbidities and potential confounders. Specifically, Medicaid payer status is associated with increased 90-day and overall readmission rates, length of stay, and direct cost. These findings are consistent with previous orthopaedic literature [22], [23], [24], [25] and is the largest patient sample size evaluating Medicaid patients and TKA from a national standpoint. There are a few small retrospective cohort studies evaluating Medicaid status with increased 90-day readmission and 1 large national inpatient sample study looking at Medicaid inpatient reporting only [1], [25]. This study is the first to assess a large national database on the impact of Medicaid payer status on resource utilization via 90-day and overall readmission rates, length of stay, and direct cost in TKA patients.
The differences in 90-day outcomes after total knee replacement persist after matching Medicaid patients to non-Medicaid patients. This study design accounts for a wide range of confounding patient demographics and comorbidities that may be encountered in patients with Medicaid payer status. Previous studies have revealed several disparities in preoperative patient characteristics that could influence outcomes. For example, Medicaid patients who undergo total knee replacements are typically younger, positive for smoking history, and have increased medical comorbidities. These are potential confounders that were accounted for in this analysis. Previous studies on this population have been underpowered and lacked confounding variable control.
With the increased prevalence of bundled payment programs, health-care stakeholders have a financial incentive to provide high-quality care to patients at the lowest cost. With postdischarge care accounting for a significant portion of the overall cost, patients who are at increased risk to be discharged to rehabilitation center or be readmitted within 90 days will significantly increase cost per episode of care [9]. Because of increased cost per episode of care in patients with Medicaid status, providers may be hesitant to take on financial risks associated with Medicaid insurance, thus potentially increasing disparities in patient access to care. This study justifies further investigation into adjusting reimbursement models for TKA patients based on Medicaid payer status.
The strength of the study is the ability to analyze a large number of patient records and control for confounding variables through matching. This is a nationwide sample and is representative of clinical practice. This is the first study to include administrative data on payer status, for 90 days, with sufficient sample size to avoid beta error. The limitations are those inherent in the analysis of large administrative databases, such as incomplete data collection, inaccurate diagnostic and procedural coding, and lack of detailed clinical information or clinical outcomes. There are also limitations inherent to propensity score matching analysis. Specifically, propensity score methods only provide the expectation that measured baseline covariates will be balanced between Medicaid and non-Medicaid groups but make no claim to balance unmeasured covariates. Psychosocial factors such as income, education level, employment status, and race are not available in the NRD and thus not available for propensity score matching. Finally, the insufficient clinical detail prevents conclusions based on preoperative functional status or the severity of joint disease that can vary inside of International Classification of Diseases-9 code 8154.
Although this study shows that Medicaid status is an independent risk factor for complications, readmission, and increased resource utilization, it does not explain why the association exists nor does it suggest causation or provide reasons for readmissions. The influence of socioeconomic factors on 90-day readmissions and complications is complex, and all potential factors cannot be captured in a study of administrative data. Further studies are needed to identify other possible psychosocial variables that may impact readmission and cost of care. These factors should be considered along with medical comorbidities in reimbursement models, and these models need to be critically evaluated at a continuum to allow policymakers and providers to implement strategies that will improve care and access for a spectrum of patients.
Conclusions
With the continued growth of APMs including bundled payments, access to care for individuals with increased risk of complications, readmission, and discharge to a nursing facility will continue to be an issue. Physicians and hospitals may potentially have a disincentive on patient populations who require increased resource utilization. Medicaid status in this study was predictive of increased 90-day and overall readmission rates, length of stay, and direct cost after TKA. Risk adjustment models accounting for Medicaid status are necessary to avoid decreased access to care for this patient population and avoid financial penalty for physician and hospital alike.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
No author associated with this paper has disclosed any potential or pertinent conflicts which may be perceived to have impending conflict with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2018.05.001.
Appendix A. Supplementary data
References
- 1.Browne J.A., Novicoff W.M., D'Apuzzo M.R. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. J Bone Joint Surg Am. 2014;96(21):e180. doi: 10.2106/JBJS.N.00133. [DOI] [PubMed] [Google Scholar]
- 2.Medicaid Eligibility Criteria. http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Eligibility/Eligibility.html
- 3.Congressional Budget Office Estimates for the insurance coverage provisions of the Affordable Care Act updated for the recent Supreme Court decision. 2012. http://cbo.gov/sites/default/files/cbofiles/attachments/43472-07-24-2012-CoverageEstimates.pdf
- 4.Kurtz S.M., Lau E., Ong K. Projections of primary and revision hip and knee arthroplasty in the United States from 2005-2030. Clin Orthop Relat Res. 2009;467(10):2606. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare and Medicaid Services New Medicare data available to increase transparency on hospital utilization. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2015-Fact-sheets-items/2015-06-01.html accessed February 25, 2018.
- 6.Iorio R., Clair A.J., Slover J. Early results of CMS bundled payment initiative for a 90 day total joint replacement episode of care. J Arthroplasty. 2016;31(2):343. doi: 10.1016/j.arth.2015.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Mechanic R.E. Mandatory Medicare bundled payments: is it ready for prime time. N Engl J Med. 2015;373:1291. doi: 10.1056/NEJMp1509155. [DOI] [PubMed] [Google Scholar]
- 8.Iorio R., Bosco J., Slover J., Sayeed Y., Zuckerman J.D. Single institution early experience with the bundled payments for care improvement initiative. J Bone Joint Surg Am. 2017;99:e2. doi: 10.2106/JBJS.16.00066. [DOI] [PubMed] [Google Scholar]
- 9.Slover D. Want a successful bundle: what about post-discharge care? J Arthroplasty. 2016;31(5):936. doi: 10.1016/j.arth.2016.01.056. [DOI] [PubMed] [Google Scholar]
- 10.Iorio R. Strategies and tactics for successful implementation of bundled payments: bundled payment for care improvement at a large, urban, academic medical center. J Arthroplasty. 2015;30:349e50. doi: 10.1016/j.arth.2014.12.031. [DOI] [PubMed] [Google Scholar]
- 11.Kamath A.F., Courtney P.M., Bozic K.J. Bundled payment in total joint care: survey of AAHKS membership attitudes and experience with alternative payment models. J Arthroplasty. 2015;30(12):2045. doi: 10.1016/j.arth.2015.05.036. [DOI] [PubMed] [Google Scholar]
- 12.Calvillo-King L., Arnold D., Eubank K.J. Impact of social factors on risk of readmission or mortality in pneumonia and heartfailure: systematic review. J Gen Intern Med. 2013;28(2):269. doi: 10.1007/s11606-012-2235-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LaPar D.J., Bhamidipati C.M., Mery C.M. Primary payer status affects mortality for major surgical operations. Ann Surg. 2010;252(3):544. doi: 10.1097/SLA.0b013e3181e8fd75. discussion 550-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lyon S.M., Benson N.M., Cooke C.R., Iwashyna T.J., Ratcliffe S.J., Kahn J.M. The effect ofinsurance status on mortality and procedural use in critically ill patients. Am J Respir Crit Care Med. 2011;184(7):809. doi: 10.1164/rccm.201101-0089OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stone M.L., LaPar D.J., Mulloy D.P. Primary payer status is significantly associated with postoperative mortality, morbidity, and hospital resource utilization in pediatric surgical patients within the United States. J Pediatr Surg. 2013;48(1):81. doi: 10.1016/j.jpedsurg.2012.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inneh I.A. The combined influence of sociodemographic, preoperative comorbid and intraoperative factors on longer length of stay after elective primary total knee arthroplasty. J Arthroplasty. 2015;30(12):2092. doi: 10.1016/j.arth.2015.05.032. [DOI] [PubMed] [Google Scholar]
- 17.Rosenbaum P.R., Rubin D.B. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41. [Google Scholar]
- 18.Rubin D.B. The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med. 2007;26:20. doi: 10.1002/sim.2739. [DOI] [PubMed] [Google Scholar]
- 19.Bergstralh E.J., Konsanke J.L. Technical reports series, number 56. Mayo Clinic Department of Health Sciences Research; Rochester, MN: 1995. Computerized matching of cases to controls. [Google Scholar]
- 20.Austin P.C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ayanian J.Z., Ehrlich G.M., Grimes D.R., Levy H. Economic effects of Medicaid expansion in Michigan. N Engl J Med. 2017;376:407e10. doi: 10.1056/NEJMp1613981. [DOI] [PubMed] [Google Scholar]
- 22.Freburger J.K., Holmes G.M., Ku L.E., Cutchin M.P., Heatwole-Shank K., Edwards L.J. Disparities in post-acute rehabilitation care for joint replacement. Arthritis Care Res. 2011;63:1020e30. doi: 10.1002/acr.20477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Courtney P.M., Huddleston J.I., Iorio R., Markel D.C. Socioeconomic risk adjustment models for reimbursement are necessary in primary total joint arthroplasty. J Arthroplasty. 2017;32:1. doi: 10.1016/j.arth.2016.06.050. [DOI] [PubMed] [Google Scholar]
- 24.Rozell J.C., Courtney P.M., Dattilo J.R., Wu C.H., Lee G.C. Should all patients be included in alternative payment models for primary total hip arthroplasty and total knee arthroplasty? J Arthroplasty. 2016;31(9 Suppl):45. doi: 10.1016/j.arth.2016.03.020. [DOI] [PubMed] [Google Scholar]
- 25.Courtney P.M., Edmiston T., Batko B., Levine B.R. Can bundled payments Be successful in the Medicaid population for primary joint arthroplasty? J Arthroplasty. 2017;32(11):3263. doi: 10.1016/j.arth.2017.05.035. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.