Abstract
The aim of our study was to compare the cost of preoperative empiric mupirocin treatment of all total joint arthroplasty patients with a standard Staphylococcus aureus screening and decolonization protocol. The cost of empiric mupirocin treatment is $24.65 per patient, whereas the cost of a standard S. aureus screening and decolonization protocol is $60.32 per patient. Given that more than 1,051,000 total joint arthroplasties are performed annually, the cost savings with empiric treatment is nearly $40 million per year. Empiric treatment allows for more efficient workflow, minimizes potential for clerical error, eliminates risk of undertreatment, and has not been shown to increase antibiotic resistance.
Keywords: Mupirocin, Infection, Staphylococcus, Hip, Knee, Arthroplasty
Introduction
Kalmeijer et al. [1] reported a 9-fold higher risk of Staphylococcus aureus prosthetic joint infection (PJI) after total joint arthroplasty (TJA) with S. aureus nasal colonization. Nearly 85% of S. aureus PJIs are caused by bacterial strains found in the patient's nares [2]. The efficacy of S. aureus screening and decolonization programs in preventing PJI and decreasing associated costs is well established [2].
Screening involves culturing swabs of the anterior nares of both nostrils. Decolonization is achieved by administering 2% mupirocin ointment intranasally twice daily for 5 days to all patients with nasal cultures positive for methicillin-sensitive S. aureus and methicillin-resistant S. aureus. Screening and decolonization protocols suffer from a false-negative S. aureus detection rate as high as 8% [3], clerical error in culture interpretation or selection of patients for decolonization, and added cost. There is a need for more accurate, efficient, and cost-effective S. aureus decolonization of TJA patients. Recently, universal S. aureus decolonization of TJA patients, regardless of S. aureus carrier status, has been shown to decrease the rate of PJI [4].
The aim of our study was to compare the cost of preoperative empiric mupirocin treatment of all TJA patients with a standard S. aureus screening and decolonization protocol.
Material and methods
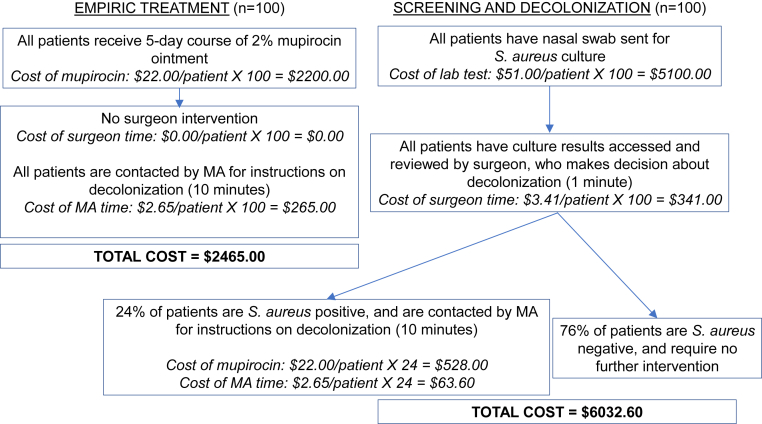
We calculated the costs of a 5-day course of 2% mupirocin topical ointment (Perrigo; Dublin, Ireland) applied intranasally twice daily to all TJA patients preoperatively (empiric treatment) and preoperative nasal swab of all TJA patients sent for S. aureus culture, review of culture results, and selective decolonization with mupirocin (screening and decolonization).
We made the following assumptions in our calculations. Based on a study of 912 patients by Hacek et al. [5], 24% of all patients are nasal culture positive for S. aureus. Based on 2011 Medical Group Management Association data, the average TJA surgeon's yearly salary is $589,267. With 4 weeks of vacation a year and a 60 hour work week, a TJA surgeon's wage is $204.61 per hour. Using our institutional average, a medical assistant's wage is $15.92 per hour. We used the costs of medications and laboratory tests at our institution in our calculations.
Workflow and cost for empiric treatment versus screening and decolonization of 100 TJA patients are illustrated in Figure 1. Costs common to both treatment protocols, such as chlorhexidine washes/showers, were not included in the cost analysis.
Figure 1.
Workflow and cost calculation for empiric mupirocin treatment versus screening and decolonization in 100 TJA patients.
Results
Over 1,051,000 TJAs are performed annually according to the Centers for Disease Control. As a result, the cost savings to our health-care system with empiric treatment over screening and decolonization is at least $37,489,170.00 per year, as follows:
Standard S. aureus screening and decolonization $60.32/patient × 1,051,000 = $63,396,320
Empiric mupirocin treatment $24.65/patient × 1,051,000 = $25,907,150
Cost difference $63,396,320−$25,907,150 = $37,489,170
Discussion
Mupirocin application is extremely safe, with a potential for reaction only in those patients hypersensitive to the drug class. In a multicenter study of 14,316 patients, there were no adverse events associated with mupirocin treatment [6]. The use of povidone-iodine (PI), instead of mupirocin, for nasal S. aureus decolonization has recently been investigated. PI ($27.21) is not only more expensive than mupirocin ($22.00), but also less efficacious [7]. S. aureus culture remains positive in 21% of PI-treated patients but only 2.8% of mupirocin-treated patients [8], [9].
There may be concern for increased mupirocin resistance with empiric treatment. However, to our knowledge, increased mupirocin resistance as a result of preoperative S. aureus decolonization has not been reported. In a study of approximately 7000 patients followed for 4 years after receiving a 5-day course of nasal mupirocin, there was no evidence of increased mupirocin resistance [10]. These findings were recapitulated by others who found no increase in low-level mupirocin resistance and no high-level mupirocin resistance after a 5-day course of nasal mupirocin [4].
Conclusions
Our results demonstrate that preoperative empiric mupirocin treatment of all TJA patients is approximately one-third the cost of S. aureus screening and decolonization. This amounts to savings of nearly $40 million annually. In addition, empiric treatment allows for more efficient workflow, minimizes potential for clerical error, eliminates risk of undertreatment due to false-negative screening results, has not been shown to increase antibiotic resistance, and may decrease the rate of PJI. Future work may examine the development or discovery of agents both less expensive and more efficacious than mupirocin for S. aureus eradication.
Footnotes
One or more of the authors of this article have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2017.11.011.
Appendix A. Supplementary data
References
- 1.Kalmeijer M.D., van Nieuwland-Bollen E., Bogaers-Hofman D., de Baere G.A. Nasal carriage of Staphylococcus aureus is a major risk factor for surgical-site infections in orthopedic surgery. Infect Control Hosp Epidemiol. 2000;21(5):319. doi: 10.1086/501763. [DOI] [PubMed] [Google Scholar]
- 2.Chen A.F., Wessel C.B., Rao N. Staphylococcus aureus screening and decolonization in orthopaedic surgery and reduction of surgical site infections. Clin Orthop Relat Res. 2013;471:2383. doi: 10.1007/s11999-013-2875-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yano K., Minoda Y., Sakawa A., Kuwano Y., Kondo K., Fukushima W., Tada K. Positive nasal culture of methicillin-resistant Staphylococcus aureus (MRSA) is a risk factor for surgical site infection in orthopedics. Acta Orthop. 2009;80(4):486. doi: 10.3109/17453670903110675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stambough J.B., Nam D., Warren D.K., Keeney J.A., Clohisy J.C., Barrack R.L., Nunley R.M. Decreased hospital costs and surgical site infection incidence with a universal decolonization protocol in primary total joint arthroplasty. J Arthroplasty. 2017;32(3):728. doi: 10.1016/j.arth.2016.09.041. [DOI] [PubMed] [Google Scholar]
- 5.Hacek D.M., Robb W.J., Paule S.M., Kudrna J.C., Stamos V.P., Peterson L.R. Staphylococcus aureus nasal decolonization in joint replacement surgery reduces infection. Clin Orthop Relat Res. 2008;466:1349. doi: 10.1007/s11999-008-0210-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Warren D.K., Liao R.S., Merz L.R., Eveland M., Dunne W.M. Detection of methicillin-resistant Staphylococcus aureus directly from nasal swab specimens by a real-time PCR assay. J Clin Microbiol. 2004;42(12):5578. doi: 10.1128/JCM.42.12.5578-5581.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Torres E.G., Lindmair-Snell J.M., Langan J.W., Bumikel B.G. Is preoperative nasal povidone-iodine as efficient and cost-effective as standard methicillin-resistant Staphylococcus aureus screening protocol in total joint arthroplasty? J Arthroplasty. 2016;31(1):215. doi: 10.1016/j.arth.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 8.Rezapoor M., Nicholson T., Tabatabaee R.M., Chen A.F., Maltenfort M.G., Parvizi J. Povidone-iodine-based solutions for decolonization of nasal staphylococcus aureus: a randomized, prospective, placebo-controlled study. J Arthroplasty. 2017;32:1. doi: 10.1016/j.arth.2017.04.039. [DOI] [PubMed] [Google Scholar]
- 9.Chen A.F., Heyl A.E., Xu P.Z., Rao N., Klatt B.A. Preoperative decolonization effective at reducing staphylococcal colonization in total joint arthroplasty patients. J Arthroplasty. 2013;28(8 Suppl):18. doi: 10.1016/j.arth.2013.03.036. [DOI] [PubMed] [Google Scholar]
- 10.Fawley W.N., Parnell P., Hall J., Wilcox M.H. Surveillance for mupirocin resistance following introduction of routine peri-operative prophylaxis with nasal mupirocin. J Hosp Infect. 2006;62:327. doi: 10.1016/j.jhin.2005.09.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.