Abstract
The application of distraction osteogenesis through the use of magnet-operated, remote-controlled intramedullary lengthening continues to provide new opportunities for accurate limb equalization. While limb-length discrepancy and deformity can be addressed by total hip arthroplasty alone, the magnitude of correction is limited by the soft-tissue envelope and complications such as sciatic nerve palsy. This 3-patient case series presents the combination of staged ipsilateral total hip arthroplasty and retrograde intramedullary femoral nail lengthening for the correction of both deformity and limb-length discrepancy. Our results report leg-length equalization, independent ambulation without assistive devices, and excellent bone and functional outcomes without complications, demonstrating that this combined technique can be used to achieve targeted lengthening and deformity correction.
Keywords: Limb lengthening, Limb-length discrepancy, Total hip arthroplasty, PRECICE, Deformity
Introduction
Distraction osteogenesis has been used to correct limb-length discrepancy (LLD) resulting from a wide range of etiologies including congenital shortening, growth plate arrest, open fractures with bone defects, nonunion, tumor, osteomyelitis, and achondroplasia. The application of a magnet-operated, remote-controlled intramedullary (IM) lengthening nail continues to provide new opportunities for accurate limb equalization with excellent functional outcomes and improved consolidation indices [1], [2], [3], [4], [5], [6]. Bone lengthening with internal devices provides decreased complication rates compared with external fixation, including pin tract infections, soft-tissue tethering, and joint stiffness [1], [4], [5]. The PRECICE nail system (NuVasive Specialized Orthopedics, Aliso Viejo, CA) is an IM, magnetic, telescopic rod that is activated through an external handheld controller. The rate and rhythm of distraction is programmed by the surgeon and transmitted to the device to allow for the desired daily distraction rate and rhythm. The advantages of the PRECICE nail system over previous models include the ability to either lengthen or shorten without the use of a cable or implanted subcutaneous antenna. Kirane et al [2] utilized the PRECICE system to perform a mean total lengthening of 35.0 mm with a range of 14.0-65.0 mm, while maintaining alignment and knee and ankle range of motion for 24 patients with femoral and tibial LLD.
While LLD and hip deformity can be addressed by total hip arthroplasty (THA) alone, the magnitude of achievable correction is limited by the soft-tissue envelope and concern over associated complications. Limb lengthening through THA is limited by the risk of sciatic, femoral, and peroneal nerve palsy, low back pain, and abnormal gait. There is no safe threshold for lengthening; however, it is agreed upon that progressively greater lengthening is associated with greater risk of injury [7]. Edwards et al [8] reviewed THA cases complicated by nerve palsy and found an average lengthening of 2.7 cm for peroneal nerve palsy and 4.4 cm for sciatic nerve palsy. Therefore, the general consensus on the amount of length that can be gained through THA at the time of surgery is 4.0 cm with careful monitoring and direct visualization of nerve tension with lengthening greater than 2.0 cm. It is important that the initial physical examination rules out other causes of deformity and LLD including flexion contracture and rigid scoliosis; the former is correctable with standing blocks on standing long-leg radiographs, whereas the latter is not [9]. Patients with an LLD undergoing THA are younger, tend not to use assist devices or shoe lifts, and are predominantly females. LLD can be addressed through THA by lowering the acetabulum toward an anatomic position or inserting a femoral component that is longer that the length of the femoral bone removed [10]. Although deformity correction through THA is possible, its limitations may prevent full correction of larger length discrepancies, and these individuals stand to benefit from a combined operative technique.
The use of IM limb lengthening in conjunction with THA has yet to be described. The present article presents a retrospective multicenter case review identifying 3 patients who underwent staged ipsilateral THA and retrograde IM femoral nail lengthening with the PRECICE nail for deformity and LLD. The mean age at surgery was 28.3 years (range, 17-40 years) and the minimum follow-up was 14 months from the index procedure (range, 14-40 months). The etiology of the original deformity was Perthes (n = 1) and neonatal septic arthritis (n = 2).
Assessment included preoperative and postoperative length and alignment radiographic measurements of LLD, mechanical axis deviation (MAD), medial proximal tibial angle (MPTA), and the medial lateral distal femoral angle (mLDFA) as defined by Paley [11] using long-standing radiographs of the entire lower extremity. The MAD was measured in the frontal plane from the center of the femoral head to the center of the ankle plafond; the normal mechanical axis line passes 8.0 ± 7.0 mm medial to the center of the knee joint line. The mLDFA was measured in the frontal plane as the lateral angle formed between the mechanical axis line of the femur and the knee joint line of the femur. The MPTA was measured in the frontal plane as the medial angle formed between the mechanical axis line of the tibia and the knee joint line of the tibia [11].
Outcomes were also evaluated according to the Association for the Study and Application of Methods of Ilizarov (ASAMI) bone and functional scores criteria [12], [13]. An excellent functional outcome is defined as being active, no limp, <15° loss of knee extension, no reflex sympathetic dystrophy (RSD), and insignificant pain. Good and fair functional outcomes defined as when patients continued to have 1-2 or 3 of the following: limp, stiffness, RSD, or significant pain. A poor outcome being inactivity resulting in unemployment or inability to perform activities of daily living, whereas amputation is defined as a functional failure. Excellent bone outcomes were defined as union, no infection, final residual deformity <7°, and a residual LLD <2.5 cm [13]. Good and fair bone outcomes were defined as union with any 2 or 3 of the following: absence of infection, deformity <7°, and a limb-length inequality of <2.5 cm. A poor bone outcome being nonunion, refractures, or union with infection, deformity >7°, or limb-length inequality >2.5 cm.
Case histories
Case 1
A 40-year-old female initially presented with left hip ankylosis. She had previously undergone left hip surgery at the age of 8 years in South America and was placed in a cast for 1 year for an unknown condition, presumed Legg-Calve Perthes disease, then subsequently developed avascular necrosis and fusion. Upon presentation, she had a 63.5-mm LLD, 40° hip flexion contracture, 15° of abduction, and 0° external rotation. She was able to ambulate with difficulty using a ½ inch shoe lift (Fig. 1). She underwent an uncomplicated THA by a fellowship-trained arthroplasty surgeon using an S-range of motion (ROM) modular hip system (DePuy Synthes Joint Reconstruction, Warsaw, IN). An S-ROM modular hip system was specifically selected to achieve stability through a press-fit metaphyseal sleeve with a fluted diaphyseal stem with differing lengths and configurations, while simultaneously controlling version with independent neck and sleeve options that can be dialed in separately. An intraoperative alignment guide was used to place the acetabular components in 45° abduction and 20° anteversion. Postoperatively the abduction angle was measured to be 46° based on anteroposterior pelvis radiographs taken in post-anesthesia care unit. Lengthening through the THA was approximately 1.5 inches. The estimated blood loss (EBL) was 500 cc, operative time was 280 minutes, and the length of hospital stay was 5 days. Postoperatively the patient ambulated with a half inch shoe lift and had a residual internal rotation deformity and LLD of 24.0 mm originating from the femur. Approximately 21 months after THA, the patient underwent a femoral derotational osteotomy, iliotibial band release, and retrograde PRECICE IM nailing using a 215.0 mm by 10.7 mm diameter rod by a fellowship-trained trauma and limb deformity surgeon. For the lengthening procedure, the EBL was 20 cc, operative time was 225 minutes, and the length of hospital stay was 2 days. She underwent 26 days of lengthening at 1.0 mm per day resulting in a total of 24.0 mm of lengthening through the PRECICE IM system. She was maintained at 50 lbs weight bearing until distraction was completed, and 3 of 4 cortices were healed then advanced to weight bearing as tolerated at approximately 16 weeks. At 11 months postoperatively, the patient was ambulating without a lift or any assist device, reported subjectively equivalent limb length, and achieved 0°-120° hip flexion and 10° of internal and external rotation. She underwent an uncomplicated removal of hardware approximately 16 months after nail insertion. During which the EBL was 10 cc and the operative time was 102 minutes, and the patient was discharged home from the post-anesthesia care unit. At the time of final follow-up, 19.5 months after IM nail insertion and 41 months after her original THA surgery, the patient's LLD was corrected.
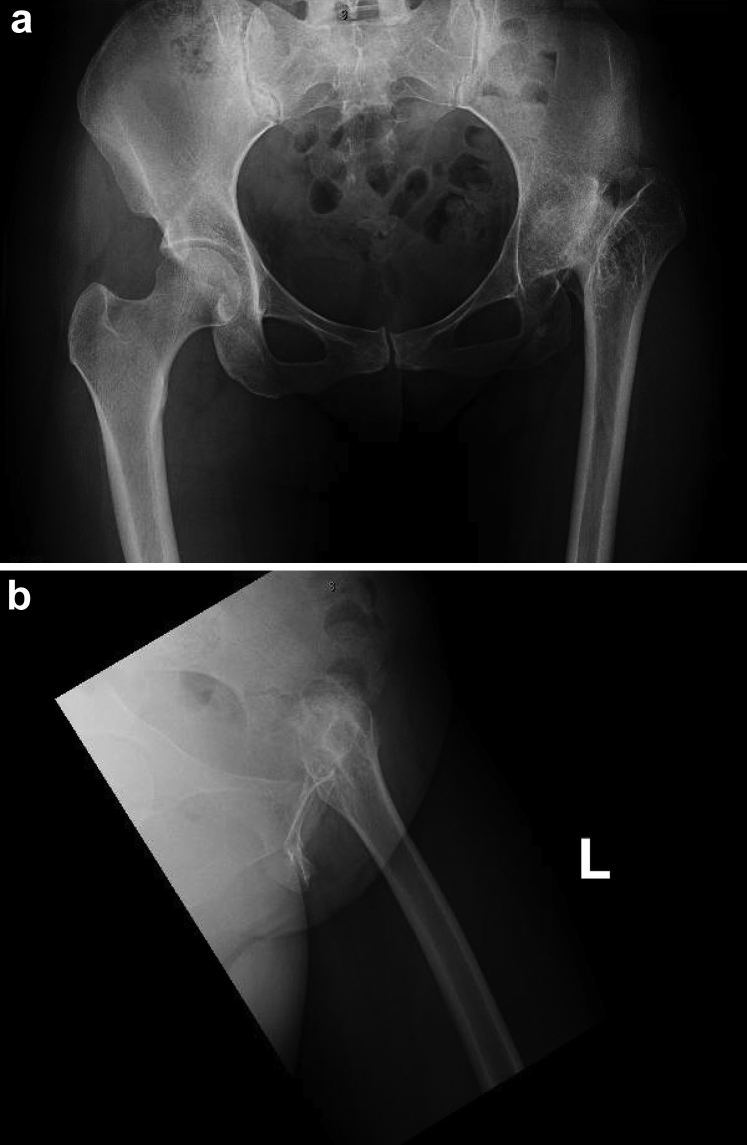
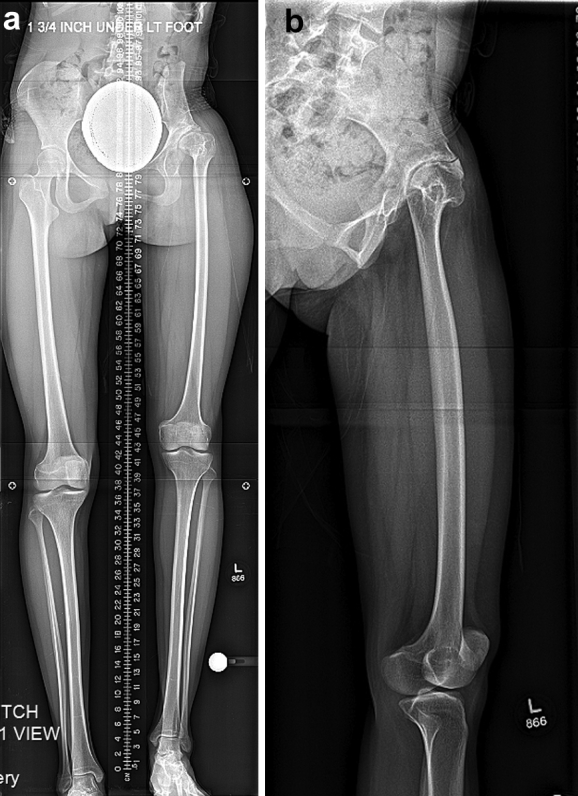
Figure 1.
(a and b) Case 1: Preoperative anteroposterior (AP) pelvis and frog-leg lateral radiographs.
Case 2
A 17-year-old female presented with a history of neonatal sepsis and a 43.0 mm LLD from the left femur (Figs. 2 and 3). She underwent an uncomplicated THA with 18.0 mm of intraoperative lengthening through the arthroplasty construct. For the THA, the EBL was 200 cc, the operative time was 150 minutes, and the length of hospital stay was 3 days. The acetabular component was placed in the pseudoacetabular region instead of the native hip center because it was determined intraoperatively to be the position with the best bone stock. Given her LLD with a planned second procedure, placement of the acetabular component in the pseudoacetabulum avoided the need for bone grafting and optimized available bone stock. The postoperative measurement for the acetabular components was 50° abduction and 20° anteversion. Her residual LLD was 25.0 mm (Figs. 4 and 5). Three and a half months after THA, the patient underwent an uncomplicated femoral osteoplasty and retrograde PRECICE IM nailing by a fellowship-trained trauma and limb lengthening surgeon. For the lengthening procedure, the EBL was 25 cc, the operative time was 120 minutes, and the length of hospital stay was 2 days. The patient then completed 30 days of lengthening at 1.0 mm per day with a total of 25.0 mm of lengthening through the PRECICE IM system. She was restricted to 50 lbs weight bearing for 16 weeks and underwent an uncomplicated removal of hardware 13 months after nail insertion (Figs. 6 and 7). At the final follow-up, 19.5 months after her index operation, her hip range of motion was 0°-100° flexion and 60° of abduction and she was able to ambulate independently without a lift or any assist device (Figs. 8 and 9).
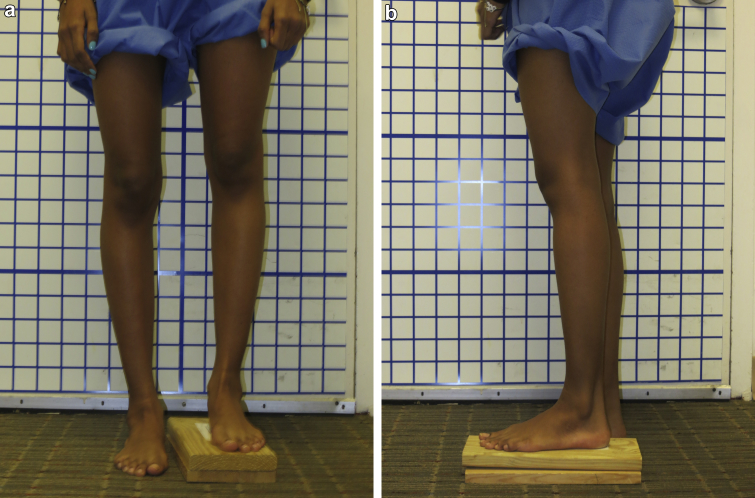
Figure 2.
(a and b) Case 2: AP and lateral clinical photographs at initial presentation.
Figure 3.
(a and b) Case 2: AP and lateral radiographs at initial presentation.
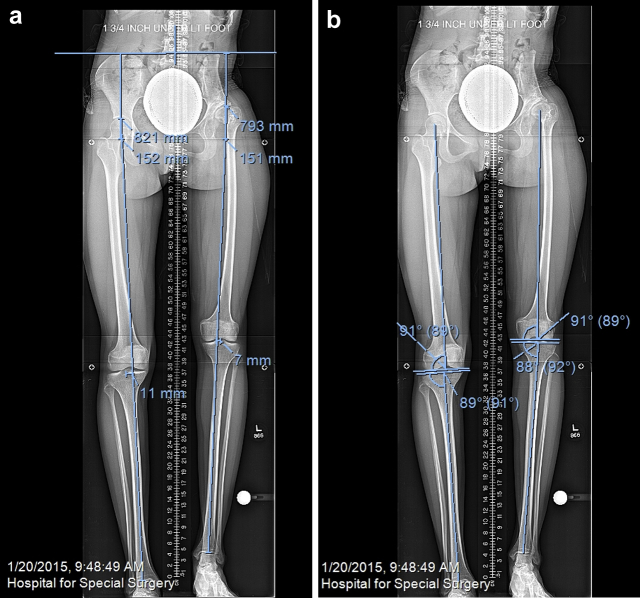
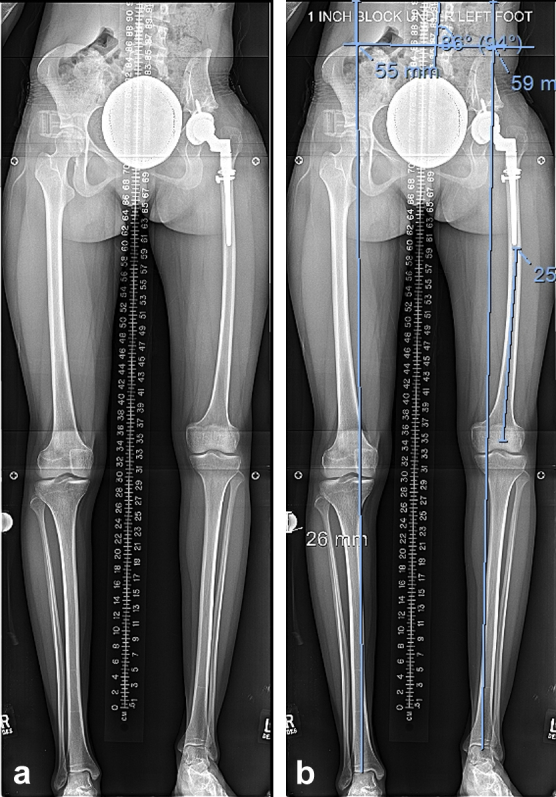
Figure 4.
(a and b) Case 2: full-length AP and lateral radiographs with preoperative planning measurements including LLD, mLDFA, and the MPTA.
Figure 5.
(a and b) Case 2: full-length AP radiograph after THA and preoperative planning before retrograde IM nail insertion.
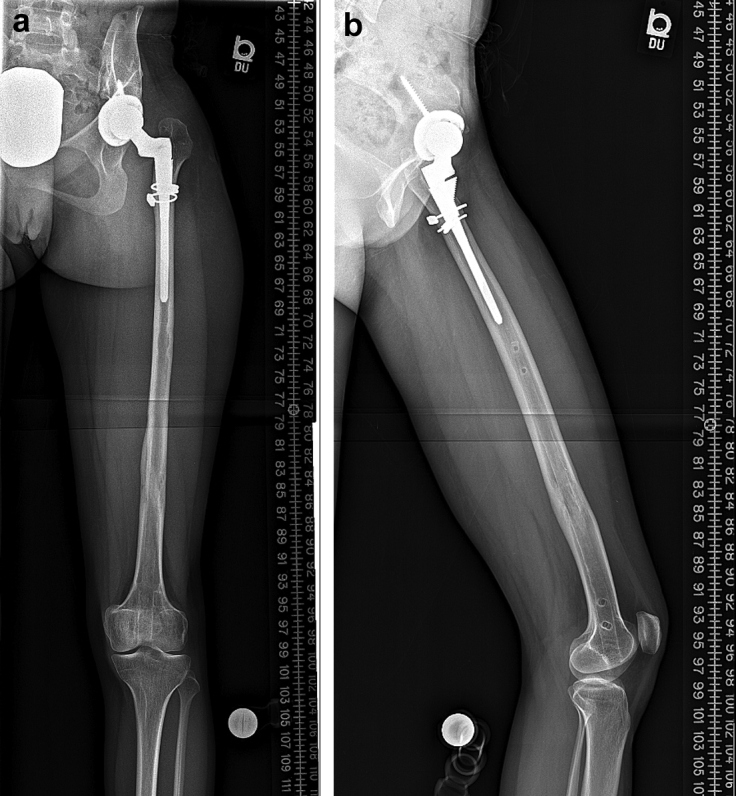
Figure 6.
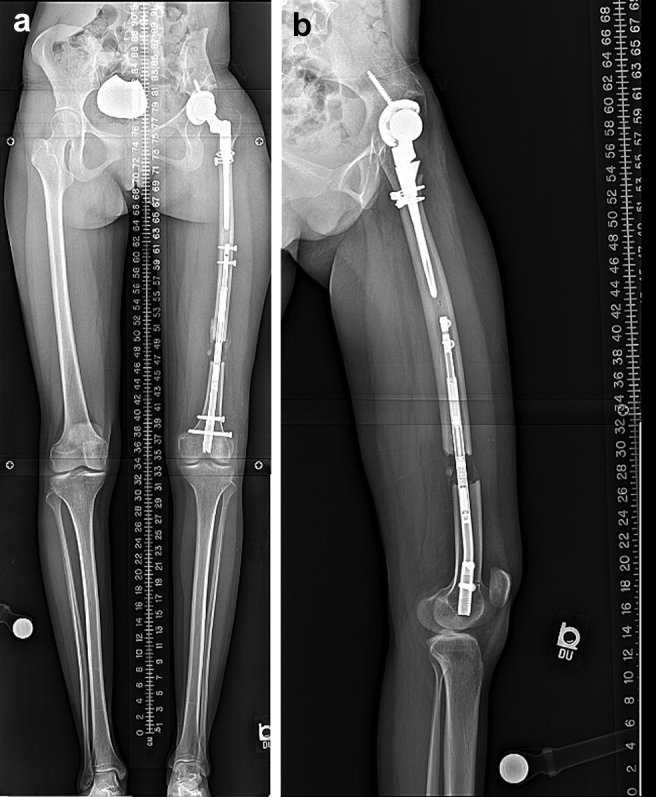
(a and b) Case 2: full-length AP and lateral radiographs at final lengthening.
Figure 7.
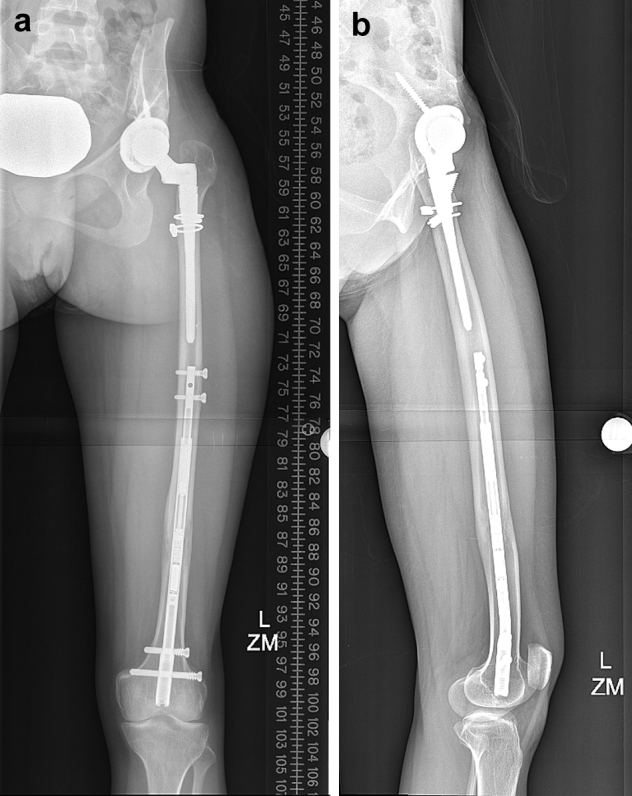
(a and b) Case 2: AP and lateral radiographs at final healing.
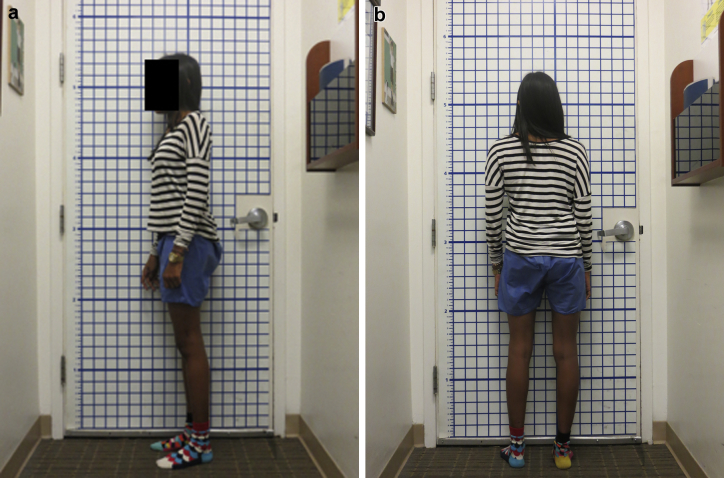
Figure 8.
(a and b) Case 2: AP and lateral clinical photographs at final follow-up.
Figure 9.
(a and b) Case 2: AP and lateral radiographs at final follow-up.
Case 3
A 28 year-old female presented with a history of neonatal sepsis and an 83.0 mm leg-length discrepancy from the left femur. Her preoperative range of motion revealed a 15° hip extension deficit and 60° of hip flexion. She underwent an uncomplicated femoral shortening osteotomy and THA at an outside hospital with 13.0 mm of overall intraoperative lengthening resulting in a residual leg-length discrepancy of 70.0 mm. The postoperative measurement for the acetabular components was 39° abduction and 20° anteversion. Eight months after her THA, the patient underwent a femoral osteotomy and insertion of a retrograde magnetically controlled lengthening rod (PRECICE) with a gradual 34-day lengthening period resulting in a gain of 40.0 mm of length. For the first lengthening procedure, the EBL was 20 cc, the operative time was 120 minutes, and the length of hospital stay was 3 days. Three and a half months later, she then underwent a second lengthening lasting 33 days and resulting in an additional 30.0 mm of length through the PRECICE IM system. Two separate lengthenings were performed because the maximum nail length for the first lengthening was less than 245 mm, therefore allowing a maximum stroke length of 50.0 mm. She was restricted to 50 lbs weight bearing for 24 weeks. At the final follow-up, 14 months after her index THA, her hip range of motion was 0° extension, 100° flexion, and 60° of abduction. The patient was ambulating without a lift or any assist device.
Discussion
In our case series, the mean original LLD was 63.2 mm (range, 43.0-83.0 mm). All patients underwent an uncomplicated THA. The mean total lengthening achieved through THA was 15.3 mm (range, 13.0-18.0 mm). The average post THA LLD was 39.0 mm (range, 22.0-70.0 mm) (Table 1). The mean total lengthening achieved through the retrograde IM femoral nail was 39.7 mm (range, 24.0-70.0 mm). The average number of days lengthening through was 41 days (range, 26-34 days). On final radiographic assessment, the mean final total LLD was 0.67-mm long (range, 0-2.0 mm) (Table 1). The average prelengthening MAD was 2.0 mm lateral (range, 1.0 mm lateral-7.0 mm medial). The average prelengthening mLDFA was 87° (range, 86-89) and the average prelengthening MPTA was 89.3° (range, 88-92). The average final MAD was 3.0 mm medial (range, 11.0 mm lateral-14.0 mm medial). The average final mLDFA was 87.3° (range, 84-93) and the average final MPTA was 89° (range, 87-92) (Table 2). Upon final assessment, all patients met criteria for excellent ASAMI bone and functional scores. No minor or major complications were observed. All patients reported leg-length equalization and were able to ambulate independently without assistive device or shoe lift.
Table 1.
Compiled data from initial presentation, THA, IM nail lengthening, and final outcomes of all 3 patient cases.
| Characteristic | Case 1 | Case 2 | Case 3 | Mean | Range |
|---|---|---|---|---|---|
| Gender | F | F | F | ||
| Age (y) | 40 | 17 | 28 | 28.3 | 17-40 |
| Diagnosis | Perthes | Neonatal sepsis | Neonatal sepsis | ||
| Original LLD (mm) | 63.5 | 43.0 | 83.0 | 63.2 | 43-83 |
| Amount of lengthening with THA (mm) | 15.3 | 18.0 | 13.0 | 15.3 | 13.0-18.0 |
| Post THA LLD (mm) | 22.0 | 25.0 | 70.0 | 39.0 | 22.0-70.0 |
| # Days lengthening (d) | 26 | 30 | 34 and 33 (67 total) | 41 | 26-67 |
| Nail lengthening (mm) | 24.0 | 25.0 | 40.0 and 30.0 (70.0 total) | 39.7 | 24.0-70.0 |
| Final total LLD (mm) | +2.0 | 0 | 0 | +0.67 | 0-2.0 |
| ASAMI bone | Excellent | Excellent | Excellent | Excellent | |
| ASAMI function | Excellent | Excellent | Excellent | Excellent |
Table 2.
Prelengthening and final follow-up MAD, mLDFA, and MPTA measurements.
| Characteristic | Case 1 | Case 2 | Case 3 | Mean | Range |
|---|---|---|---|---|---|
| Prelengthening MAD | 1 mm lateral | 7 mm medial | 8 mm lateral | 2 mm lateral | 8 mm lateral-7 mm medial |
| Prelengthening mLDFA | 86° | 89° | 86° | 87° | 86°-89° |
| Prelengthening MPTA | 88° | 88° | 92° | 89.3° | 88-92° |
| Final MAD | 11.0 mm lateral | 14.0 medial | 8.0 mm lateral | 5.0 mm lateral | 1.7 mm medial |
| Final mLDFA | 84° | 93° | 85° | 87.3° | 84°-93° |
| Final MPTA | 87° | 88° | 92° | 89° | 87°-92° |
Distraction osteogenesis has been used to treat complex long-bone nonunions associated with segmental defects and infection [14], [15]; however, the application of this technology has evolved to the correction of LLD secondary to many congenital, traumatic, and infectious etiologies [14], [16], [17]. IM lengthening nails provide new opportunities for limb equalization and deformity correction from conventional external fixation [18]. Former generations of nail systems include the Fitbone telescope active actuator system, Albizzia nail, and the IM skeletal kinectic distractor. Previous systems have experienced complications related to the dysfunction of the distraction mechanism of the nail [19], premature consolidation, run away acute lengthening, prominent hardware, limitation of osteotomy site positioning, and nail distortion [20], [21], resulting in either revision surgery or transition to a monolateral external fixator system. Many of these issues have been resolved as the technology has evolved with newer generations. The complications associated with external fixation (pin tract infections, pain, soft-tissue tethering, and joint stiffness) are minimized or eliminated [1], [4], [5], [22]. Kirane et al [2] utilized the PRECICE system to perform accurate lengthening while maintaining knee and ankle range of motion. Hawi et al [23] demonstrated that intramedullary nailing lengthening is superior to lengthening through an external fixator in controlling medial and lateral MAD and also identified risk factors for varus angulation, nail-medullary canal ratio <85% and a shorter distance between the lesser trochanter and the osteotomy site. However, there are situations in which IM lengthening with the PRECICE system is contraindicated, including infection, osteopenia, metal allergies, open physes, peripheral vascular disease, patients weighing in excess of the nail weight restriction by diameter, patients with IM canal diameter greater than the nail width restriction by diameter, and patients who are incapable of following lengthening instructions.
Before this series, there are no published reports of the PRECICE nail system being utilized in combination with other means of deformity correction. While LLD and deformity can be addressed by THA with cup placement in the native hip center combined with a subtrochanteric shortening osteotomy, the magnitude of achievable correction is limited by the surrounding soft-tissue structures and concern over associated complications, mainly nerve palsy. Therefore, the general consensus on the amount of length that can be gained through THA at the time of surgery is 4.0 cm.
In this unique multicenter case series, we present the combination of THA and PRECICE IM femoral nail lengthening for congenital hip deformity and LLD. This technique optimizes available bone stock and also allows for placement of a larger head and therefore greater ROM. It also avoids the need to perform 2 osteotomies because the first procedure utilizes the available bone stock while the second addresses the patient's LLD. Our study found that the combination of THA and IM femoral lengthening can safely and accurately allow for the correction of deformity and LLD. At the final follow-up, all patients exhibited leg-length equalization with a mean final total LLD of 0.67 mm. During femoral lengthening, the mLDFA and MPTA were maintained. Overall, the mechanical axis was medialized; range, 11.0 mm lateral to 14.0 mm medial. At the end of treatment, all 3 patients reported leg-length equalization and were able to ambulate independently without assistive devices or the use of a shoe lift. All 3 patients met criteria for excellent ASAMI functional outcomes given their activity level, minimum stiffness, insignificant pain, and lack of a limp or RSD. All 3 patients also met criteria for excellent ASAMI bone outcomes; they achieved union without infection, deformity <7°, and a LLD <2.5 cm. There were no patient complications. Specifically, there were no nerve palsies, dislocation events, nonunions, infections, or refracture.
This study had a number of limitations. The first limitation is the low patient volume, which is secondary to the nature of the deformity and LLD specific to these patients. The study only included patients who underwent a combination of THA and IM femoral nail lengthening with the PRECICE nail system, a technique which has never been described. Future studies would elucidate the ideal indication for the integration of these 2 surgical techniques. Second, this study is a retrospective chart review; the final radiographic and functional outcomes were recorded directly from radiographs and data that were present in the medical record. No patients were lost to follow-up, and the senior surgeons examined all patients. Therefore, a deficiency or inaccuracy of information should be minimal.
THA and the Ilizarov method are both widely accepted as viable treatment options to address deformity and LLD; however, they both carry specific limitations. In the present study, these 2 surgical techniques were safely combined for accurate limb-length equalization with excellent functional results. Future studies should aim to delineate the indications for this combined surgical technique and produce more generalizable conclusions in a prospective, multicenter design.
Summary
Targeted lengthening and deformity correction through combined THA and retrograde IM femoral nail lengthening was achieved in all 3 cases with excellent radiographic and clinical outcomes. As demonstrated in this small case series, combined THA and retrograde IM femoral nail lengthening can be used to safely and effectively correct cases of deformity and LLD.
Footnotes
One or more of the authors of this paper have disclosed potential or pertinent conflicts of interest, which may include receipt of payment, either direct or indirect, institutional support, or association with an entity in the biomedical field which may be perceived to have potential conflict of interest with this work. For full disclosure statements refer to https://doi.org/10.1016/j.artd.2018.03.001.
Appendix A. Supplementary data
References
- 1.Horn J., Grimsrud Ø., Dagsgard A.H., Huhnstock S., Steen H. Femoral lengthening with a motorized intramedullary nail. Acta Orthop. 2015;86(2):248. doi: 10.3109/17453674.2014.960647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirane Y.M., Fragomen A.T., Rozbruch S.R. Precision of the PRECICE® internal bone lengthening nail. Clin Orthop Relat Res. 2014;472(12):3869. doi: 10.1007/s11999-014-3575-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laubscher M., Mitchell C., Timms A., Goodier D., Calder P. Outcomes following femoral lengthening: an initial comparison of the precice intramedullary lengthening nail and the LRS external fixator monorail system. Bone Joint J. 2016:1382. doi: 10.1302/0301-620X.98B10.36643. [DOI] [PubMed] [Google Scholar]
- 4.Mahboubian S., Seah M., Fragomen A.T., Rozbruch S.R. Femoral lengthening with lengthening over a nail has Fewer complications than intramedullary skeletal kinetic distraction. Clin Orthop Relat Res. 2011;470(4):1221. doi: 10.1007/s11999-011-2204-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rozbruch S.R., Birch J.G., Dahl M.T., Herzenberg J.E. Motorized intramedullary nail for management of limb-length discrepancy and deformity. J Am Acad Orthop Surg. 2014;22(7):403. doi: 10.5435/JAAOS-22-07-403. [DOI] [PubMed] [Google Scholar]
- 6.Schiedel F.M., Vogt B., Tretow H.L. How precise is the PRECICE compared to the ISKD in intramedullary limb lengthening? Reliability and safety in 26 procedures. Acta Orthop. 2014;85(3):293. doi: 10.3109/17453674.2014.913955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clark C.R., Huddleston H.D., Schoch E.P., Thomas B.J. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg. 2006;14(1):38. doi: 10.5435/00124635-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Edwards B.N., Tullos H.S., Noble P.C. Contributory factors and etiology of sciatic nerve palsy in total hip arthroplasty. Clin orthop Relat Res. 1987;(218):136. [PubMed] [Google Scholar]
- 9.Ng V.Y., Kean J.R., Glassman A.H. Limb-length discrepancy after hip arthroplasty. J Bone Joint Surg Am. 2013;95(15):1426. doi: 10.2106/JBJS.L.00433. [DOI] [PubMed] [Google Scholar]
- 10.Jaroszynski G., Woodgate I.G., Saleh K.J., Gross A.E. Total hip replacement for the dislocated hip. Instr Course Lect. 2001;50:307. [PubMed] [Google Scholar]
- 11.Paley D. Normal lower limb alignment and joint orientation. In: Paley D., editor. Principles of deformity correction. Springer Berlin Heidelberg; Berlin, Heidelberg: 2002. p. 1. [Google Scholar]
- 12.Bernstein M., Fragomen A.T., Sabharwal S., Barclay J., Rozbruch S.R. Does integrated fixation provide benefit in the reconstruction of posttraumatic tibial bone defects? Clin Orthop Relat Res. 2015;473(10):3143. doi: 10.1007/s11999-015-4326-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paley D., Catagni M.A., Argnani F., Villa A., Benedetti G.B., Cattaneo R. Ilizarov treatment of tibial nonunions with bone loss. Clin Orthop Relat Res. 1989;241:146. [PubMed] [Google Scholar]
- 14.Seenappa H., Shukla M., Narasimhaiah M. Management of complex long bone nonunions using limb reconstruction system. Indian J Orthop. 2013;47(6):602. doi: 10.4103/0019-5413.121590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shahid M., Hussain A., Bridgeman P., Bose D. Clinical outcomes of the ilizarov method after an infected tibial non union. Arch Trauma Res. 2013;2(2):1. doi: 10.5812/atr.11300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamdy R.C., Bernstein M., Fragomen A.T., Rozbruch S.R. What's new in limb lengthening and deformity correction. J Bone Joint Surg Am. 2016;98(16):1408. doi: 10.2106/JBJS.16.00460. [DOI] [PubMed] [Google Scholar]
- 17.Shabtai L., Specht S.C., Standard S.C., Herzenberg J.E. Internal lengthening device for congenital femoral deficiency and fibular hemimelia. Clin Orthop Relat Res. 2014;472(12):3860. doi: 10.1007/s11999-014-3572-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muthusamy S., Rozbruch S.R., Fragomen A.T. The use of blocking screws with internal lengthening nail and reverse rule of thumb for blocking screws in limb lengthening and deformity correction surgery. Strategies Trauma Limb Reconstr. 2016;11(3):199. doi: 10.1007/s11751-016-0265-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dinçyürek H., Kocaoğlu M., Eralp I.L., Bilen F.E., Dikmen G., Eren I. Functional results of lower extremity lengthening by motorized intramedullary nails. Acta Orthop Traumatol Turc. 2012;46(1):42. doi: 10.3944/aott.2012.2671. [DOI] [PubMed] [Google Scholar]
- 20.Papanna M.C., Monga P., Al-Hadithy N., Wilkes R.A. Promises and difficulties with the use of femoral intra-medullary lengthening nails to treat limb length discrepancies. Acta Orthop Belg. 2011;77(6):788. [PubMed] [Google Scholar]
- 21.Simpson A.H.W.R., Shalaby H., Keenan G. Femoral lengthening with the intramedullary skeletal kinetic distractor. J Bone Joint Surg Br. 2009;91(7):955. doi: 10.1302/0301-620X.91B7.21466. [DOI] [PubMed] [Google Scholar]
- 22.Paley D. PRECICE intramedullary limb lengthening system. Expert Rev Med Devices. 2015;12(3):231. doi: 10.1586/17434440.2015.1005604. [DOI] [PubMed] [Google Scholar]
- 23.Hawi N., Kenawey M., Panzica M. Nail-medullary canal ratio affects mechanical axis deviation during femoral lengthening with an intramedullary distractor. Injury. 2015;46(11):2258. doi: 10.1016/j.injury.2015.05.040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.