Highlights
-
•
H-reflex is a well known neurophysiological test used to evaluate S1 root.
-
•
As a single tool, H-reflex cannot be used intraoperatively to assess motor deficit.
-
•
IONM with H-reflex can be useful in patients with preexisting neurological deficits.
Keywords: Intraoperative neurophysiological monitoring, TcMEP, H-reflex, Scoliosis, Hypotension
Abstract
Objective
H-reflex is a well known neurophysiological test used to evaluate sensory afferent and motor efferent impulses of S1 root. Despite its simplicity and feasibility, it is not used very often in the operating room.
Methods
We report the case of a 16-year-old male patient who undergoes a surgical correction for a severe paralytic scoliosis (160°). On account of previous deficits, intraoperative neurophysiological monitoring was achieved through TcMEP and H-reflex.
Results
Intraoperative neurophysiological monitoring (IONM) showed a transient and simultaneous loss of bilateral TcMEP and H-reflex, coinciding with an abrupt hypotension during pedicle screw placement. After having dismissed mechanical injury and after increasing blood pressure, TcMEP and H-reflex were equivalent to those at baseline.
Conclusions
The H-reflex is a classic neurophysiological test not used very frequently in the operating room. It is a feasible and reliable technique that can be helpful during spine surgery IONM, especially in patients with preexisting neurological deficits. Although simultaneous TcMEP and H-reflex monitoring has been previously described, to our knowledge, this is the first recorded case of a decline in both associated with abrupt hypotension.
1. Introduction
Spine surgery carries a low but devastating risk of neurologic damage. The main purpose of intraoperative neuromonitoring is to continuously assess the functional integrity of the spinal cord and nerve roots during these procedures. Initially somatosensory evoked potentials (SSEP) (Nash et al., 1977) and later transcranial electrical motor evoked potentials (TcMEP) (Merton and Morton, 1980), have been regarded by many as gold standard techniques to achieve this goal.
H-reflex is a well-known neurophysiological test not so much used in the operating room. In clinical practice, it is used to assess the reflex arc of the ascending posterior tibial nerve afferent activity, the synaptic connections at the S1 level, and the descending homonymous nerve efferent activity to the triceps surae muscle. Any motor neuron involved in H-reflex has several synapses, receiving information from sensory input, descending suprasegmental systems and propriospinal connections. Thus, it allows the H-reflex to give information not only about the reflex pathway but it also may attest interruption of the descending and/or of the intraspinal activity (Slimp, 2004).
Although the nature of the reflex largely depends on monosynaptic excitation, it is not exclusively a monosynaptic reflex. The earliest part of the reflex is mediated by monosynaptic fast Ia afferents, whereas the later portions of the reflex probably include contributions of slow Ia afferent pathways (Misiaszek, 2003, Burke, 2016). The H-reflex reliability depends on the balance of the integrated summated synaptic excitatory and inhibitory effect of the peripheral input, descending suprasegmental and propriospinal systems on the interneurons and motor neurons involved in the reflex (Leppanen, 2012). It is assumed that when acute or chronic spinal cord injury occurs, the subsequent hyperpolarization of the motor neurons will result in a significant decrease in the amplitude of the H-reflex (Walmsley and Tracey, 1983)
2. Case report
A 16-year-old male, weighing 17 kg with a history of neonatal cerebral palsy, progressive multifocal leukoencephalopathy and a severe paralytic scoliosis (160°) underwent surgical correction. In the preoperative examination, somatosensory evoked potentials (SSEP) were absent and central motor conduction through magnetic transcranial stimulation (MTS) was feasible despite a severe tetraparesis (normal latencies for the age of the patient, low amplitudes predominantly in lower extremities). The patient underwent a total intravenous anesthesia (TIVA) regime with propofol (4–5 mg/kg/h) and remifentanil (0.04–0.06 μg/kg/min).
His scoliosis was partially corrected after pedicle screws from T2 to S1 were placed.
IONM was performed with a Cadwell Cascade IONM 16 channel device (Kennewick, WA, USA). Motor evoked potentials were elicited by transcranial stimulation (corkscrew electrodes on C1-C2, train of 5 stimuli, duration 0.05 ms, interstimulus interval 4 ms, intensity 400 V) and were recorded by needle electrodes (12 mm) on abductor digiti minimi, tibialis anterior, triceps surae and abductor hallucis muscles bilaterally. The H-reflex was evoked by stimulation to the tibial nerve at the popliteal fossa (surface electrodes, stimulus duration 1 ms, submaximal intensity for the M wave) and recorded by needle electrodes (12 mm) on triceps surae muscle bilaterally.
Accordingly to the severe tetraparesis and the preoperative examination, TcMEP were difficult to obtain, and the most stable responses were recorded on bilateral abductor hallucis, right tibialis anterior and left triceps surae.
The alarm criteria used for TcMEP and H-reflex monitoring were an amplitude decrease larger than 75–80% and 90% respectively (Legatt et al., 2016, Leppanen, 2012).
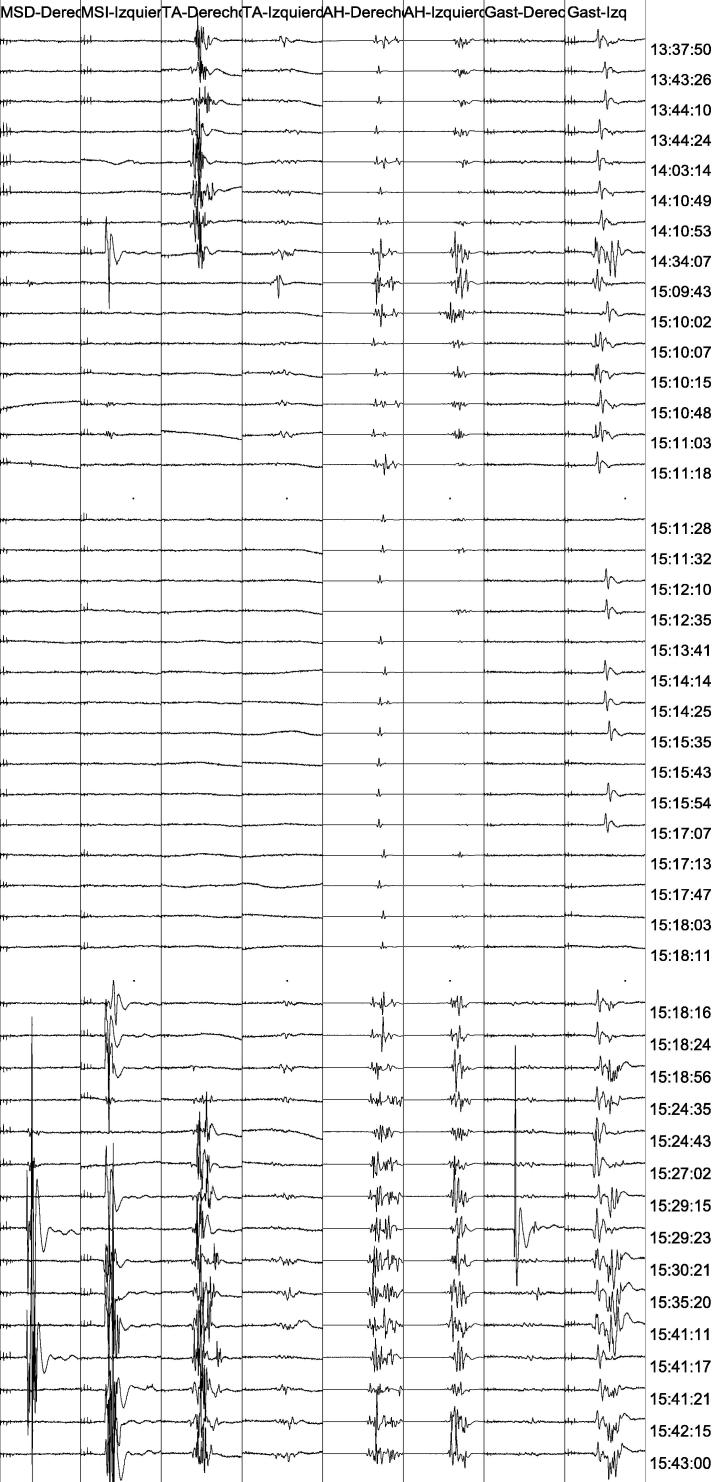
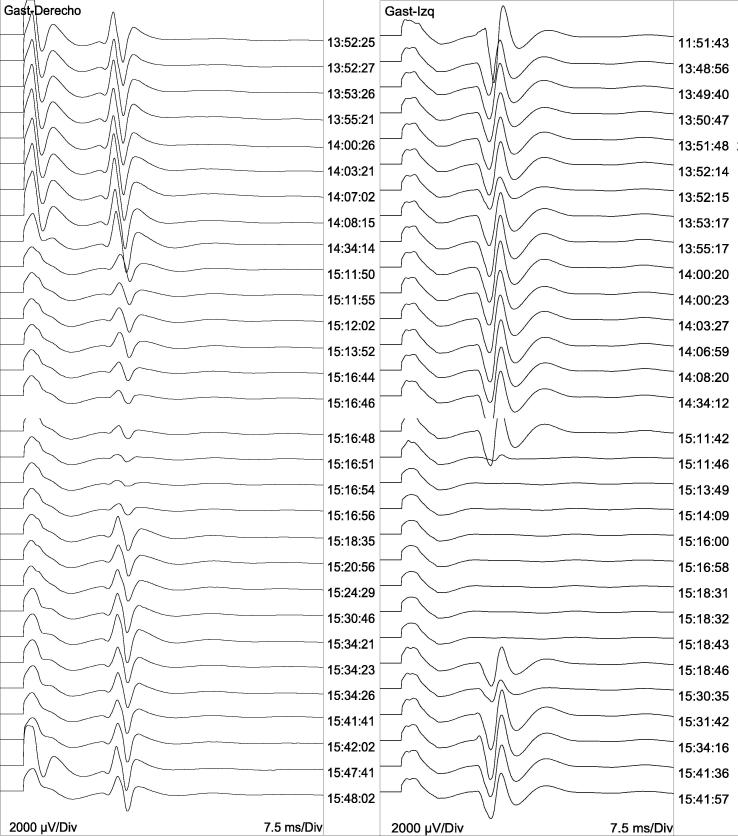
At a certain point of the intervention, concretely during pedicle screws placement between L1 and L2 levels, we observed a progressive loss of the TcMEP (Fig. 1) as well as the H-reflexes (Fig. 2), which started to fall simultaneously. This event coincided with an abrupt hypotension (mean blood pressure 45 mmHg, departing from 75 mmHg), and the responses decreased in amplitude almost to disappearance. After increasing the intensity and the number of pulses without having any improvement, we advised the anesthesiologist. Procedures to increase the blood pressure were applied (saline solution 20 ml/kg/h, blood 250 ml, ephedrine 24 mg within the 2 h after warning to maintain a proper blood pressure). 7–8 min later, blood pressure raised to basal values and TcMEP and H-reflexes were obtained, equal to those at baseline. Surgery went on until the end without any further disturbances. The patient woke up without any additional neurological deficit.
Fig. 1.
Transcranial motor evoked potentials (from left to right: Right and left abductor digiti minimi, right and left tibialis anterior, right and left abductor hallucis, right and left triceps surae – listed as gastrocnemius) Scale 10 ms/Div; 100 μV/Div on ADM, tibialis anterior and triceps surae, 2000 μV/Div on AH. Note progressive loss of TcMEP at 15:09:43 coinciding with an abrupt hypotension and recovery at 15:18:16 after procedures to increase blood pressure were applied.
Fig. 2.
Right (first column) and left (second column) H-reflexes. Scale 7.5 ms/Div; 2000 μV/Div. Synchronously to TcMEP loss between 15:11:46 and 15:18:35, as showed in Fig. 1, it can be noted a slightly progressive drop in amplitude of the right H-reflex, and a complete disappearance of the left H-reflex.
3. Discussion
This case report illustrates the potential usefulness of the H-reflex in spine surgery above S1 level when motor evoked potentials of more rostral motor neuron pools are lost, as a way to optimize IONM, especially in those patients whom SSEP or TcMEP are difficult to evoke or not obtainable.
In addition to TcMEP, F-responses and H-reflexes are a feasible and complementary approach that could be useful, even more so if they asses the integrity of different or overlapping populations of motor neurons (Leppanen, 2006). Unlike TcMEP, these techniques could be performed continuously during the surgery without disturbing the surgeon.
H-reflex can be elicited under TIVA. The impact of propofol in depressing motor neuron excitability may be solved increasing the stimulus intensity (von Dincklage et al., 2006).
The effect of hypotension on TcMEP and SSEP has been widely described (Dong et al., 2002, Polo et al., 2000, Owen, 1999). Although it is not the first report in literature about TcMEPs and H-reflexes being lost during thoracic spine surgery (Leppanen, 2004), to our knowledge, our case is the first in which transient drop in amplitude of both responses has been related to hypotension. Other potential causes to explain these findings – such as surgical damage to the spinal cord – were immediately dismissed since TcMEP amplitude dropped from upper and lower extremities.
Intraoperatively, it has been proved that rostral cord injury rapidly suppresses H-reflex (Leis et al., 1996). Post-operative deficits are correlated with an amplitude drop exceeding 90% of baseline but not a 50% drop in amplitude or transient changes (Leppanen, 2012). It has been hypothesized that slow suppression of H-reflexes may reflect ischemic spinal cord compromise while abrupt suppression may be secondary to mechanical injury (Feyissa and Tummala, 2015). In our case, there was a slightly progressive decrement in amplitude in the right H-reflex and a sudden disappearance in the left one (Fig. 2). In this context, literature (Leppanen, 2012) remains controversial as it is stated that ischemic insult might cause slow suppression instead of abrupt one.
4. Conclusion
H-reflex is a non specific methodology, and it cannot be used as a single monitoring tool to assess intraoperative motor deficit. Performing TcMEP in combination with H-reflex in the operating room could be useful as a complementary method to assess functional integrity of the spinal cord, especially in patients with preexisting neurological damage.
Conflict of interest statement
The authors declare no conflict of interest.
References
- Burke D. Clinical uses of H reflexes of upper and lower limb muscles. Clin. Neurophysiol. Pract. 2016;1:9–17. doi: 10.1016/j.cnp.2016.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong C.C., MacDonald D.B., Janusz M.T. Intraoperative spinal cord monitoring during descending thoracic and thoracoabdominal aneurysm surgery. Ann. Thorac. Surg. 2002;74:1873–1876. doi: 10.1016/s0003-4975(02)04137-1. [DOI] [PubMed] [Google Scholar]
- Feyissa A.M., Tummala S. Intraoperative neurophysiologic monitoring with Hoffmann reflex during thoracic spine surgery. J. Clin. Neurosci. 2015;22:990–994. doi: 10.1016/j.jocn.2015.01.008. [DOI] [PubMed] [Google Scholar]
- Legatt A.D., Emerson R.G., Epstein C.M., MacDonald D.B., Deletis V., Bravo R.J., López J.R. ACNS guideline: transcranial electrical stimulation motor evoked potential monitoring. J. Clin. Neurophysiol. 2016;33:42–50. doi: 10.1097/WNP.0000000000000253. [DOI] [PubMed] [Google Scholar]
- Leis A.A., Zhou H.H., Mehta M., Harkey H.L., 3rd, Paske W.C. Behavior of the H-reflex in humans following mechanical perturbation or injury to rostral spinal cord. Muscle Nerve. 1996;19:1373–1382. doi: 10.1002/(SICI)1097-4598(199611)19:11<1373::AID-MUS1>3.0.CO;2-9. [DOI] [PubMed] [Google Scholar]
- Leppanen R.E. From the electrodiagnostics lab: where transcranial stimulation, H-reflexes and F-responses monitor cord function intraoperatively. Spine J. 2004;4:601–603. doi: 10.1016/j.spinee.2003.11.006. [DOI] [PubMed] [Google Scholar]
- Leppanen R.E. Intraoperative applications of the H-reflex and F-response: a tutorial. J. Clin. Monit. Comput. 2006;20:267–304. doi: 10.1007/s10877-006-9036-x. [DOI] [PubMed] [Google Scholar]
- Leppanen R.E. Monitoring spinal nerve function with H-reflexes. J. Clin. Neurophysiol. 2012;29:126–139. doi: 10.1097/WNP.0b013e31824ceec5. [DOI] [PubMed] [Google Scholar]
- Merton P.A., Morton H.B. Stimulation of the cerebral cortex in the intact human subject. Nature. 1980;285:227. doi: 10.1038/285227a0. [DOI] [PubMed] [Google Scholar]
- Misiaszek J.E. The H-reflex as a tool in neurophysiology: its limitations and uses in understanding nervous system function. Muscle Nerve. 2003;28:144–160. doi: 10.1002/mus.10372. [DOI] [PubMed] [Google Scholar]
- Nash C.L., Lorig R.A., Schatzinger L.A., Brown R.H. Spinal cord monitoring during operative treatment of the spine. Clin. Orthop. Relat. Res. 1977;126:100–105. [PubMed] [Google Scholar]
- Owen J.H. The application of intraoperative monitoring during surgery for spinal deformity. Spine. 1999;24:2649–2662. doi: 10.1097/00007632-199912150-00012. [DOI] [PubMed] [Google Scholar]
- Polo A., Tercedor A., Paniagua-Soto J., Acosta F., Cañadas A. Neurophysiological monitoring during scoliosis surgery using control hypotension. Rev. Esp. Anestesiol. Reanim. 2000;47:367–370. [PubMed] [Google Scholar]
- Slimp J.C. Electrophysiologic intraoperative monitoring for spine procedures. Phys. Med. Rehabil. Clin. North Am. 2004;15:85–105. doi: 10.1016/s1047-9651(03)00106-2. [DOI] [PubMed] [Google Scholar]
- von Dincklage F., Reiche J., Rehberg B., Baars J.H. H-reflex depression by propofol and sevoflurane is dependent on stimulus intensity. Clin. Neurophysiol. 2006;117:2653–2660. doi: 10.1016/j.clinph.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Walmsley B., Tracey D.J. The effect of transection and cold block of the spinal cord on synaptic transmission between Ia afferents and motoneurones. Neuroscience. 1983;9:445–451. doi: 10.1016/0306-4522(83)90307-x. [DOI] [PubMed] [Google Scholar]