Abstract
Background
Early sepsis diagnosis is crucial for the correct management of burn patients, and it clearly influences outcomes. The systemic inflammatory response triggered by burns mimics sepsis presentation and complicates early sepsis diagnosis. Biomarkers were advocated to aid the diagnosis of early sepsis. Serum procalcitonin (PCT) exhibits fair accuracy and good correlation with sepsis severity, being used in diverse clinical settings. However, few studies have evaluated perioperative changes in PCT levels in burn patients. The present study evaluated PCT kinetics during the first days after burn injury and subsequent surgical interventions to assess PCT utility in distinguishing septic from non-septic inflammatory responses.
Methods
This study was a retrospective observational study of all burn patients admitted to the Coimbra Burns Unit (Portugal) between January 2011 and December 2014 who presented with a total burn surface area ≥ 15% and who underwent subsequent surgery. PCT kinetics were investigated a) during the first five days after burn injury and b) preoperatively during the five days after surgery in three subsets of patients, including those with no preoperative and no postoperative sepsis (NN), no preoperative but postoperative sepsis (NS), and preoperative and postoperative sepsis (SS). A total of 145 patients met the selection criteria and were included in the analysis.
Results
PCT levels in the first five days after burn injury were significantly higher in patients who developed at least one sepsis episode (n = 85) compared with patients who did not develop sepsis (n = 60). PCT values > 1.00 ng/mL were clearly associated with sepsis. Study participants (n = 145) underwent a total of 283 surgical interventions. Their distribution by preoperative/postoperative sepsis status was 142 (50.2%) in NN; 62 (21.9%) in NS; and 79 (27.9%) in SS. PCT values exhibited a parallel course in the three groups that peaked on the second postoperative day and returned to preoperative levels on the third day or later. The lowest PCT values were found in NN, and the highest values were observed in SS; the NS values were intermediate.
Conclusions
PCT kinetics coupled with a clinical examination may be helpful for sepsis diagnosis during the first days after burn injury and burn surgery.
Electronic supplementary material
The online version of this article (10.1186/s12871-018-0585-6) contains supplementary material, which is available to authorized users.
Keywords: Burns, Sepsis, Procalcitonin, Surgery
Background
An early diagnosis of sepsis is of the utmost importance for the correct management of burn patients because it has a marked impact on treatment outcomes and survival [1]. Sepsis can lead to multiple organ dysfunction syndrome (MODS), which is the cause of most deaths in burn units [2]. Therefore, a prompt sepsis diagnosis and the immediate initiation of antimicrobial therapy are needed to reduce morbidity and mortality. However, the unnecessary administration of antimicrobials is often associated with adverse effects, increased costs and the emergence and spread of antimicrobial resistance.
It is clinically difficult to identify patients who are developing sepsis because the overwhelming systemic inflammatory response triggered by burn trauma mimics the signs and symptoms of sepsis [3]. A definitive diagnosis of sepsis requires microbiological cultures, but the results are not available for 24 to 48 h, and false negative results are found in 20–30% of cases. Therefore, the development of complementary tools for sepsis diagnosis, such as the use of biomarkers, is necessary [4].
Biomarkers and their kinetics may aid the clinical examination in the differentiation of infectious from non-infectious inflammatory responses [5, 6]. Numerous sepsis biomarkers are described in the literature [7], and procalcitonin (PCT) is one of the most studied biomarkers. PCT exhibits the best discriminative power of all of the biomarkers that are available at most hospital facilities [8, 9]. Thyroid C cells primarily secrete PCT in healthy subjects, and it is barely detected in blood (< 0.01 ng/mL). Many other cell types (liver, kidney, adipocytes, etc.) secrete PCT in response to direct or indirect infectious stimuli during septic episodes, and it is massively released into the bloodstream at concentrations that reach 1000 times its normal values [10]. Increased PCT is noticeable 2–4 h after sepsis onset and peaks at 24–48 h. PCT levels decrease by 50% every 1–1.5 days (half-life) when the infectious process is controlled [11]. PCT levels are highly correlated with bloodstream infections [12], and a recent meta-analysis demonstrated that elevated PCT levels and PCT non-clearance were related with an increased risk of sepsis and a higher mortality rate [13]. PCT is accurate for sepsis diagnosis, and its kinetics exhibit good correlation with sepsis severity [14]. Therefore, PCT is recommended in diverse clinical settings, including the exclusion of a bacterial cause in lower respiratory infections [15] as well as the diagnosis, stratification, prognosis [16, 17] and antimicrobial administration guidance in septic patients [18] and the diagnosis of postoperative infections [19, 20]. However, the utility of PCT in burn patients was questioned because of the high rate of false-positive results from the systemic inflammatory response induced by burn injury and subsequent surgical interventions [21, 22].
The present study evaluated PCT kinetics after a burn episode and the surgical intervention(s) needed for its treatment to assess its utility in the differential diagnosis between septic and non-septic inflammatory responses.
Methods
Study plan
This retrospective observational study used clinical and laboratory data collected from the health records of all burn patients admitted to Coimbra Burns Unit (CBU), a department of Coimbra Hospital and University Centre (CHUC), a tertiary referral hospital in Portugal, between January 2011 and December 2014, who presented with a 15% or more total burn surface area (TBSA) and who underwent subsequent surgery during their hospitalization. A total of 145 patients met the selection criteria, and their data were available for analysis.
Sepsis was diagnosed according to the American Burn Association (ABA) criteria [23]: presence, in at least one of the initial five days, of a clinical suspicion of infection coupled with at least three of the following findings: temperature > 39 °C or < 36.5 °C, tachycardia > 110 beats/min, tachypnea > 25 breaths/min or minute ventilation > 12 L/min, thrombocytopenia < 100,000/mL, hyperglycaemia (untreated plasma glucose > 200 mg/dL or intravenous glucose requirement > 7 U/h over 24 h), and enteral feeding intolerance (abdominal distension or gastric residuals more than two times feeding rate or diarrhoea > 2500 mL).
Serum PCT concentrations were measured using TRACE© (time-resolved amplified cryptate emission) technology (Kryptor© PCT; Brahms© AG; Hennigsdorf, Germany).
PCT kinetics were evaluated in the first five days after burn injury in the entire study population, preoperatively and during the five days after surgery in three subsets of patients: no preoperative and no postoperative sepsis (NN), no preoperative but postoperative sepsis (NS), and preoperative and postoperative sepsis (SS).
Statistical analysis
The maximum value of PCT on each day of the study was used for statistical analyses.
Qualitative variables (e.g., gender and mortality) are described as counts, and quantitative variables (e.g., TBSA and ABSI - Abbreviated Burn Severity Index: see Additional file 1) are described as the means and corresponding standard deviations. The number of surgical interventions and PCT values by subgroup are described as medians and interquartile ranges (IQR). Comparisons between sepsis and no sepsis groups were performed using the Mann-Whitney test for quantitative variables and the Fisher’s exact test for qualitative variables. Time comparisons of PCT levels were performed using Friedman’s test.
Receiver operating characteristic (ROC) curves and comparative analysis of the area under the curve (AUC) were performed to evaluate the discriminatory power of PCT levels on consecutive days.
Statistical analysis was performed using SPSS© 23.0 IBM© for Windows©, and a p-value ≤0.05 was considered significant.
Results
Table 1 presents the primary demographic and baseline characteristics of the study population, which consisted of 84 males and 61 females. The sepsis (n = 85) and non-sepsis (n = 60) groups showed no significant differences in terms of gender or age, but they were significantly different in terms of ABSI score, TBSA and mortality.
Table 1.
Study population
| Characteristics | No Sepsis | Sepsis# | p-value |
|---|---|---|---|
| Number of patients | 85 | 60 | |
| Gender (male/female) | 45/40 | 39/21 | 0.115 |
| Age (years)$ | 56.49 (±18.15) | 58.43(±21.89) | 0.517 |
| ABSI scorea | 7.69 (±2.82) | 9.17 (±2.20) | 0.000* |
| TBSA (%)$ | 29.97 (±19.94) | 34.6 (±17.26) | 0.000* |
| Mortality (No/Yes) | 84/1 | 24/36 | 0.004* |
*p-values < 0.05
$Values are Median (Q1-Q3)
#At least one day with sepsis in the first five days after burn episode
aDescription in Annex I
The analysis of PCT levels during the first five days after the burn episode showed a statistically significant difference between the group of patients who developed at least one sepsis episode during that time and the group of patients who did not develop sepsis (Fig. 1). PCT values over 1.00 ng/mL were clearly associated with septic processes (p < 0.001, Mann-Whiney U test, Table 2). ROC curves and the AUC were performed to evaluate the discriminatory power of PCT over consecutive days. These results demonstrated that the discriminatory power of PCT levels increased over time (Table 3 and Fig. 2).
Fig. 1.
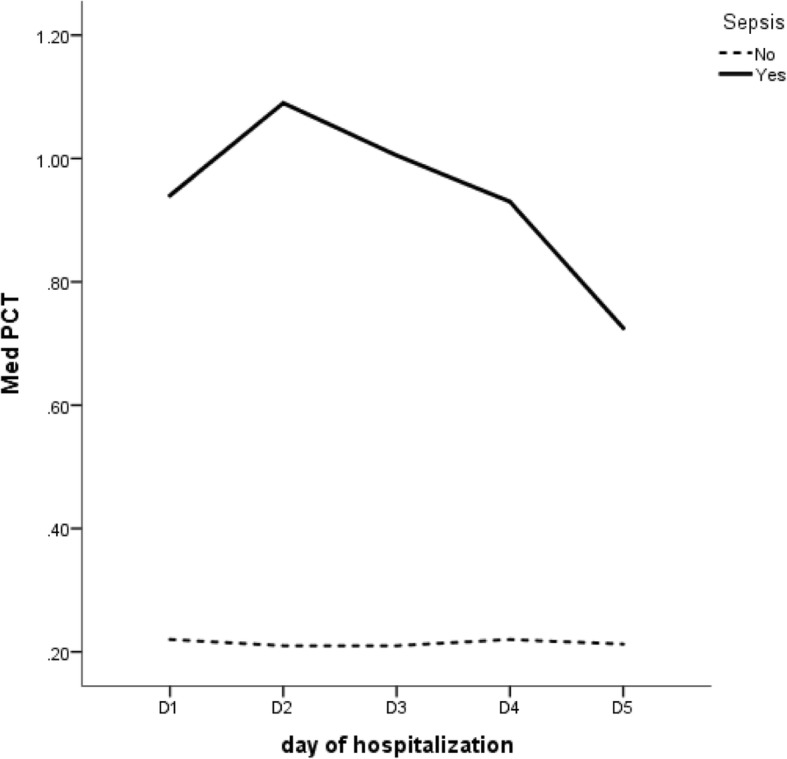
Median PCT levels observed in in the first five days after burn injury in septic (Yes) and non-septic (No) patients
Table 2.
Statistical analysis of PCT kinetics in the first five days after burn injury in septic and non-septic patients
| Sepsis | Statistic | D1 | D2 | D3 | D4 | D5 | p-value* |
|---|---|---|---|---|---|---|---|
| No | n | 64 | 70 | 72 | 69 | 62 | |
| Median [IQR] | 0.215 [0.090–0.578] | 0.205 [0.09–0.723] | 0.210 [0.08–0.668] | 0.215 [0.102–0.695] | 0.213 [0.118–0.618] | 0.557 | |
| n | 50 | 53 | 52 | 53 | 52 | ||
| Yes | Median [IQR] | 1.085 [0.188–5.440] | 1.650 [0.235–4.010] | 1.130 [0.335–2.920] | 1.060 [0.355–2.927] | 0.725 [0.340–2.105] | 0.288 |
| p-value** | 0.001 | 0.000 | 0.000 | 0.000 | 0.000 |
*Friedman test
**Mann-Whiney U test
Table 3.
ROC curves for the discriminatory power of PCT levels between septic and non-septic patients in the first five days after burn injury
| Area Under the Curve (AUROC) | |||
|---|---|---|---|
| Day | Area | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||
| D1 | 0.646 | 0.532 | 0.759 |
| D2 | 0.704 | 0.598 | 0.810 |
| D3 | 0.746 | 0.647 | 0.845 |
| D4 | 0.752 | 0.654 | 0.850 |
| D5 | 0.741 | 0.641 | 0.841 |
Fig. 2.
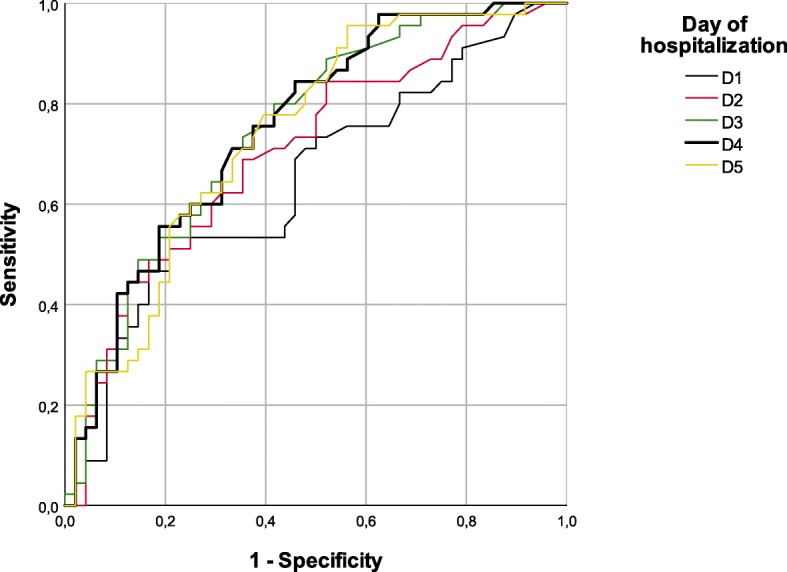
ROC Curves for the discriminatory power of PCT levels between septic and non-septic patients in the first five days after burn injury
All patients (n = 145) underwent at least one surgical intervention, with a cumulative 283 surgical interventions. Each patient was subjected to a median of three interventions, with an IQR of [2.00–5.25]. All interventions were performed under general anaesthesia and were classified as clean-contaminated. The interventions consisted primarily of escharectomies, skin autografts and flaps, and digits/limb amputations to a lesser extent.
To assess the influence of surgical trauma on PCT concentrations, PCT evolution from the day before the operation (D0) until the fifth postoperative day (D5) was analysed. Differences in the time evolution of PCT between the sepsis and non-sepsis groups were statistically significant (Table 4), and the discriminatory power increased over time as shown by the ROC curve analysis (Table 5 and Fig. 3).
Table 4.
Statistical analysis of PCT kinetics from preoperative day (D0) till the fifth postoperative day (D5) for NN, NS and SS groups
| Sepsis | Statistic | D0 | D1 | D2 | D3 | D4 | D5 | p-value* |
|---|---|---|---|---|---|---|---|---|
| NN | n | 212 | 208 | 198 | 186 | 163 | 149 | |
| Median [IQR] | 0.190 [0.110–0.560] | 0.200 [0.101–0.615] | 0.280 [0.120–0.758] | 0.223 [0.118–0.553] | 0.195 [0.110–0.430] | 0.180 [0.100–0.360] | 0.000 | |
| NS | n | 104 | 103 | 102 | 100 | 87 | 80 | |
| Median [IQR] | 0.405 [0.219–0.935] | 0.510 [0.240–1.360] | 0.640 [0.313–1.590] | 0.625 [0.283–1.438] | 0.540 [0.260–1.970] | 0.515 [0.273–2.045] | 0.000 | |
| SS | n | 74 | 74 | 74 | 69 | 65 | 62 | |
| Median [IQR] | 0.653 [0.233–2.193] | 0.790 [0.288–2.518] | 1.115 [0.413–2.990] | 0.880 [0.380–3.115] | 0.710 [0.300–1.950] | 0.580 [0.248–1.520] | 0.000 | |
| p-value** | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| Multiple comparison (p-value***) | ||||||||
| (NN,NS) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| (NN,SS) | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||
| (NS,SS) | 0.339 | 0.225 | 0.135 | 0.294 | 1 | 1 | ||
*Friedman test
**Kruskal Wallis test
***Mann-Whiney U test with Bonferroni correction
Table 5.
ROC curves for the discriminatory power of PCT levels between septic and non-septic patients preoperatively and in the first five days after burn surgery
| Area Under the Curve (AUROC) | |||
|---|---|---|---|
| Day | Area | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | ||
| D0 | 0.662 | 0.591 | 0.733 |
| D1 | 0.701 | 0.633 | 0.770 |
| D2 | 0.717 | 0.649 | 0.784 |
| D3 | 0.752 | 0.686 | 0.815 |
| D4 | 0.760 | 0.696 | 0.824 |
| D5 | 0.771 | 0.708 | 0.834 |
Fig. 3.
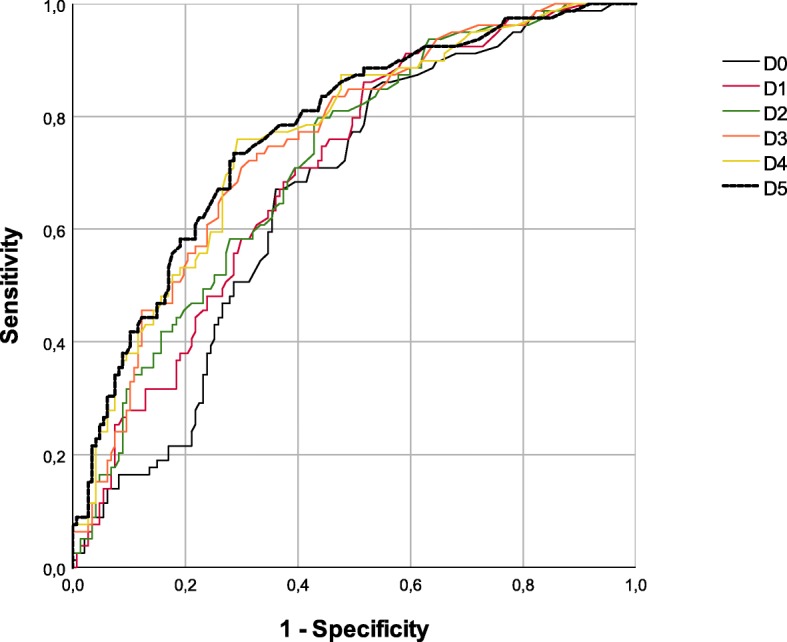
ROC Curves for the discriminatory power of PCT levels between septic and non-septic patients preoperatively and in the first five days after burn surgery
Regarding the preoperative/postoperative sepsis status, median values had a parallel course in the three groups (Fig. 4). Values peaked in the second postoperative day and returned to preoperative levels on the third day or later. The lowest values were found in the NN group, which included 142 surgical interventions in patients without preoperative sepsis and who did not develop postoperative sepsis through D5 (50.2%). The highest values were observed in the SS group, which included 62 surgical interventions in patients with pre- and postoperative sepsis (21.9%). Group NS exhibited PCT values roughly in the middle range between the other two groups and included 79 surgical interventions in patients who did not exhibit septic processes preoperatively but developed sepsis on at least one of the five days after surgery (27.9%). The kinetics of the PCT levels within each group (Table 3) were significantly different between days after surgery in the absence (NN) or presence of sepsis (NS and SS).
Fig. 4.
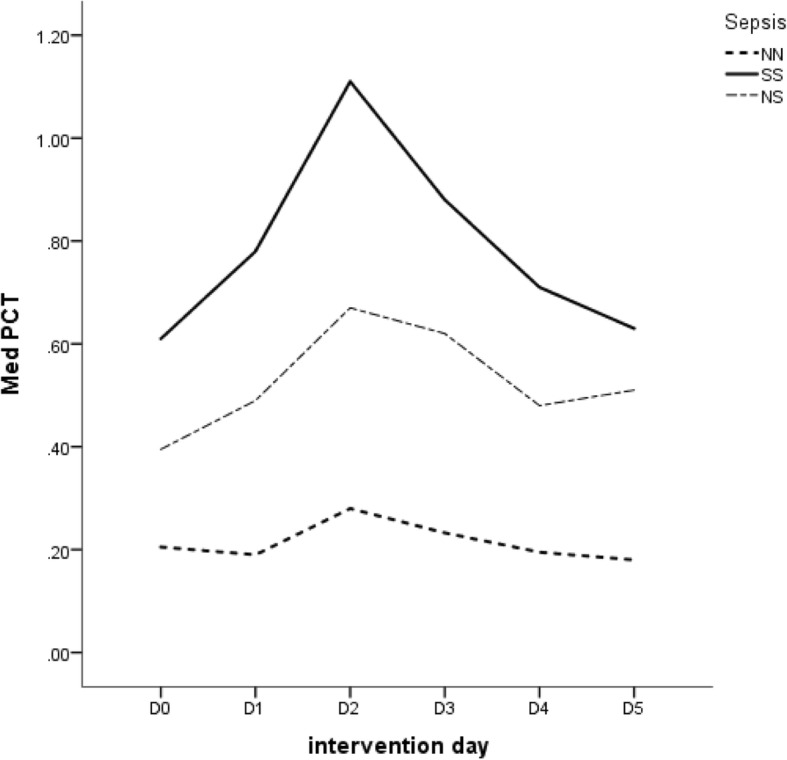
Median PCT levels observed from preoperative day (D0) till the fifth postoperative day (D5) for NN, NS and SS groups
Discussion
The present study included a sample of 145 burn patients from the CBU, and PCT levels were significantly different between septic and non-septic patients during the first five days after burn injury. The results indicate that PCT values evolved in parallel with sepsis development and the antimicrobial therapy effect. In this important population, PCT consistently showed good potential to discriminate between septic and non-septic patients, particularly when frequent PCT assays were performed and when its kinetics were dynamically assessed.
To evaluate PCT performance after surgical interventions and to investigate whether surgical trauma alone could reduce the accuracy of the diagnosis of postoperative sepsis, this study included a substantial and diversified number of interventions performed in the three subsets of patients who were organized according to the existence or absence of preoperative sepsis and the development or worsening of sepsis after surgery. PCT levels increased modestly and rapidly returned to basal levels after the second postoperative day in patients with no preoperative or postoperative sepsis episodes. Patients with increased preoperative PCT values that corresponded to preoperative sepsis exhibited PCT kinetics with a higher peak on the second postoperative day, which was presumably related to the additive increment of PCT of surgical trauma. PCT values returned to the initial values when antimicrobial therapy was administered. PCT levels in patients who only developed sepsis after surgery exhibited a parallel evolution to the already septic patients but generally with lower absolute values. Therefore, PCT is useful for sepsis diagnosis in cases of surgical intervention when preoperative PCT values are known because PCT kinetics follow the same pattern of evolution in cases of sepsis as in other critical patients.
The search for sepsis biomarkers is an exciting and never-ending story [24, 25]. Diverse approaches were used to identify more precise, practical, quicker, safer and cheaper chemicals or physical changes that may indicate the urgent need and adequacy of antimicrobial therapy or its redundancy to reduce adverse events, microbial resistance and financial costs. Current research is more focused on molecular (PCR, MALDI-TOF) and/or system-based (genomics, transcriptomics, proteonomics, metabolomics) methods for sepsis diagnosis [26–29], but these techniques are not fully developed, practical or widely available.
An ideal biomarker is not developed, and the use of PCT as an early distinction between actual septic patients and patients with merely systemic inflammatory signals and symptoms during the first days after hospital admission has been largely discussed in the medical literature in the last two decades [30–35]. PCT is a useful but not ideal biomarker, particularly due to its negative predictive power [36], which led to its inclusion in algorithms for sepsis management [37, 38]. The use of serial measurements instead of a single observation reinforces the predictive power of PCT and reduces the risks of false negatives and false positives [39–43]. The same considerations are valid for the use of PCT in the investigation of suspected postoperative sepsis [44], which is currently performed after many types of surgical procedures [45–49].
PCT accuracy in burn patients is controversial [21, 22, 50, 51]. Burn patients are generally excluded from sepsis studies and clinical trials based on the simplistic assumption that PCT levels are always elevated in burn patients as a result of the non-septic inflammatory systemic response related to burn trauma. However, several studies consistently demonstrated different PCT kinetics in burn patients based on the presence or absence of systemic infection [52–55]. Three recent meta-analysis also validated the use of PCT for sepsis diagnosis in these patients [56–58]. PCT evolution is predictable in both cases, and it provides a reliable means to identify septic processes, which was first referred to by von Heimburg et al. in 1998 [59]. The immediate inflammatory burst elevates PCT levels after burn injury, independent of infection, and grossly correlates with TBSA, but it rarely surpasses 2.0 ng/mL [60, 61]. The maximum PCT value is reached within 24–48 h in the absence of sepsis and returns to normal values (1.0–1.5 ng/mL or less) by the end of the third day. PCT levels continue increasing in the presence of sepsis and rapidly reach values greater than 5–100 ng/mL. PCT levels only diminish with antimicrobial therapy or terminal immunosuppression, as observed in other forms of severe trauma [62]. Lavrentieva et al. analysed a sample of 145 burn patients and found increased PCT levels during the first 24 h after a burn episode, which subsided in non-septic patients and continued increasing in septic patients. These authors demonstrated an inverse relationship of PCT level tendency with antimicrobial therapy efficacy. They proposed a cut-off of 1.5 ng/mL to distinguish between septic and non-septic patients [63]. Egea-Guerrero et al. [64] and Kim et al. [65] found the same PCT kinetics and approximate cutoffs.
PCT exhibited a similar kinetics pattern after surgical intervention [66], but preoperative PCT levels must be known to use these levels to discriminate between the postoperative physiological inflammatory response and postoperative sepsis. Preoperative PCT levels are related to the presence or absence of an ongoing sepsis process and possible ongoing antimicrobial therapy, which naturally influence baseline values [67]. To the best of our knowledge, the present study is the first study to specifically address PCT kinetics after surgical procedures in burn patients and demonstrate that this biomarker maintains its performance in this particular set of patients, even in the presence of preoperative sepsis.
PCT levels coupled with rigorous clinical monitoring and blood cultures as the diagnostic cornerstone [68] may help confirm or exclude sepsis in patients during the acute phase after burn trauma and ascertain the presence of postoperative sepsis in burn patients. Neither immunodepression [69] nor corticotherapy [70] affected the diagnostic performance of PCT, as opposed to other biomarkers, and PCT also distinguishes contamination from actual bloodstream infection [71]. The use of PCT dosing may inclusively reduce healthcare costs and avoid the superfluous use of antimicrobials and consequent increments on microbial resistance [72, 73].
The present study also presents some limitations. First, it was a single-centre, retrospective observational study, and the results require confirmation using prospective multicentre trials. Second, the precise influence of antimicrobial therapy in septic patients could not be evaluated because of ethical considerations that naturally prevent antimicrobial denial in face of septic episodes. Third, subgroup analyses according to the total burned surface area (TBSA) and the severity of patients’ attainment, for instance, using the Abbreviated Burn Severity Index (ABSI), was not performed. However, the use of defined and internationally accepted criteria for the clinical suspicion of burn sepsis, the homogeneity of therapeutic procedures, and the use of a standard methodology for the collection, recording and statistical analysis of the data are clearly strengths of the present study.
Conclusion
The present study was performed in 145 burn patients who underwent a high and diversified number of surgical interventions. The results allow us to conclude that 1) PCT kinetics may aid in the differential diagnosis between true sepsis and the normal inflammatory response to burn trauma in the first days after burn injury; and 2) PCT kinetics may be used to identify postoperative sepsis in burn patients who undergo surgical interventions during their stay in burn units.
Prospective multicentre studies in adult and paediatric burn patients are needed to confirm these findings and compare PCT and other biomarkers in these contexts.
Additional file
Abbreviated Burn Severity Index. (DOCX 17 kb)
Acknowledgments
The authors are grateful for the support received from Dr. Fernando Rodrigues, Director of the Department of Clinical Pathology of Coimbra University Hospital Centre, especially the prompt availability of the laboratory data used in the study. We also thank the generous help provided by Dr. Helena Donato, Director of the Documentation Service of the same hospital for the bibliographic research.
Funding
VA work was supported by Portuguese funds through the CIDMA - Center for Research and Development in Mathematics and Applications by the Portuguese Foundation for Science and Technology (FCT - Fundação para a Ciência e a Tecnologia), within project ID/MAT/04106/2013.
On behalf of all the other authors, the corresponding author states that none of the authors received any funding for this work.
Availability of data and materials
The data that support the findings of this study are available from the datasets of the Clinical Pathology Department and the Informatics Department of Coimbra University Hospital Centre, but restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available. However, data are available from the authors upon reasonable request and after permission of the Ethics Committee from Coimbra University Hospital Centre.
Abbreviations
- ABA
American Burn Association
- ABSI
Abbreviated Burn Severity Index
- AUC
Area Under the Curve
- CBU
Coimbra Burn Unit
- CHUC
Coimbra University Hospital Centre (Centro Hospitalar e Universitário de Coimbra)
- CIDMA
Center for Research and Development in Mathematics and Applications, Department of Mathematics, University of Aveiro
- CIOMS
Council for International Organizations of Medical Sciences
- iBiMED
Institute for Biomedicine, Department of Mathematics, University of Aveiro
- IBM
International Business Machines
- IQR
Interquartile Range
- MALDI-TOF
Matrix-Assisted Laser Desorption Ionization – Time of Flight
- MedinUP
Department of Pharmacology and Therapeutics, Faculty of Medicine, University of Porto
- MODS
Multiple Organ Dysfunction Syndrome
- PCR
Polymerase Chain Reaction
- PCT
Procalcitonin
- ROC
Receiver Operating Characteristic
- SACS
Autonomous Section of Health Sciences (Secção Autónoma de Ciências da Saúde), University of Aveiro
- SPSS
Statistical Package for the Social Sciences
- TBSA
Total Burn Surface Area
- TRACE
Time-Resolved Amplified Cryptate Emission
Authors’ contributions
All authors read the manuscript and agreed to its content. All authors are accountable for all aspects of the accuracy and integrity of the manuscript in accordance with ICMJE criteria and provided their consent for publication. LC, VA, MM and IT designed the study, interpreted data and drafted the manuscript. VA was responsible for most of the statistical analyses. RM, MV and CC were responsible for data acquisition and literature search and offered suggestions for citation integration in the manuscript. CC also made substantial intellectual contributions for the Introduction and Discussion sections of the manuscript. LA and JAP reviewed the manuscript and provided useful suggestions for the Discussion and Conclusion sections.
Ethics approval and consent to participate
This study has got the formal approval from the Ethics Committee of Coimbra University Hospital Centre (CHUC) to its realization. The Ethics Committee of Coimbra University Hospital Centre (CHUC) also waived the need for informed consent according to Declaration of Helsinki and CIOMS International Ethics Guidelines because this study was a retrospective observational study of patients from an anonymized dataset that only involved recording data from medical records.
Consent for publication
All data was anonymized, and this study does not contain any individual person’s data in any form (including individual details, images or videos). Therefore, consent for publication was waived.
Competing interests
On behalf of all authors, the corresponding author states that they have have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Luís Cabral, Email: jlacabral@gmail.com.
Vera Afreixo, Email: vera@ua.pt.
Rita Meireles, Email: rita_meireles@hotmail.com.
Miguel Vaz, Email: miguelpessoavaz@gmail.com.
Margarida Marques, Email: margaridammm1@gmail.com.
Isabel Tourais, Email: itmbedugo@gmail.com.
Catarina Chaves, Email: catichaves@yahoo.co.uk.
Luís Almeida, Email: lalmeida@blueclinical.pt.
José Artur Paiva, Email: jarturpaiva@gmail.com.
References
- 1.Nunes Lopez O, Cambiaso-Daniel J, Branski LK, Norbury WB, Herndon DH. Predicting and managing sepsis in burn patients: current perspectives. Ther Clin Risk Manag. 2017;13:1107–1117. doi: 10.2147/TCRM.S119938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenhalgh DG. Sepsis in the burn patient: a different problem than sepsis in the general population. Burns & Trauma. 2017;5:23–33. doi: 10.1186/s41038-017-0089-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Norbury W, Herndon DH, Tanksley J, Jeschke M, et al. Infections in burns. Surg Infect. 2016;17:250–255. doi: 10.1089/sur.2013.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin H. Liu z, Xiao Y, fan X et al. prediction of sepsis in trauma patients. Burns & Trauma. 2014;2:106–113. doi: 10.4103/2321-3868.135479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruíz-Caestilla M, Roca O, Masclans JR, Barret JP. Recent advances in biomarkers in severe burns. Shock. 2016;45:117–125. doi: 10.1097/SHK.0000000000000497. [DOI] [PubMed] [Google Scholar]
- 6.Arora R, Campbell JP, Simon G, Sahni N. Does serum procalcitonin aid in the diagnosis of bloodstream infection regardless of whether patients exhibit the systemic inflammatory response syndrome? Infection. 2017;45:291–298. doi: 10.1007/s15010-016-0965-0. [DOI] [PubMed] [Google Scholar]
- 7.Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Crit Care. 2010;14:R15. doi: 10.1186/cc8872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charles PE, Kus E, Aho S, et al. Serum procalcitonin for the early recognition of nosocomial infection in the critically ill patients: a preliminary report. BMC Infect Dis. 2009;9(49) 10.1186/1471-2334-9-4. [DOI] [PMC free article] [PubMed]
- 9.Marik PE. Don’t miss the diagnosis of sepsis! Crit Care. 2014;18:529–530. doi: 10.1186/s13054-014-0529-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vincent JL, van Nuffelen M, Lelubre C. Host response biomarkers in sepsis: the role of procalcitonin. In: Mancini N, editor. Sepsis: Diagnostic Methods and Protocols, Methods Mol Biol. New York: © Springer Science+Business Media; 2015. [DOI] [PubMed] [Google Scholar]
- 11.Meisner M. Update on procalcitonin measurements. Annals of Laboratory Medicine. 2014;34:263–273. doi: 10.3343/alm.2014.34.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoeboer SH, van der Geest PJ, Nieboer D, Groeneveld AB. The diagnostic accuracy of procalcitonin for bacteraemia: a systematic review and meta-analysis. Clin Microbiol Infect. 2015;21:474–481. doi: 10.1016/j.cmi.2014.12.026. [DOI] [PubMed] [Google Scholar]
- 13.Liu D, Su L, Han G, et al. Prognostic value of procalcitonin in adult patients with sepsis: a systematic review and meta-analysis. PLoS One. 2015;10:e0129450. doi: 10.1371/journal.pone.0129450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vincent JL, Teixeira L. Sepsis biomarkers. Value and limitations. Am J Respir Crit Care Med. 2014;190:1081–1082. doi: 10.1164/rccm.201410-1895ED. [DOI] [PubMed] [Google Scholar]
- 15.Schuetz P, Müller B, Christ-Crain M, Stolz D, et al. Procalcitonin to initiate or discontinue antibiotics in acute care respiratory tract infections. Evid-Based Child Health. 2013;8:1297–1371. doi: 10.1002/ebch.1927. [DOI] [PubMed] [Google Scholar]
- 16.Schuetz P, Maurer P, Punjabi V, Desai A, et al. Procalcitonin decrease over 72 hours in US critical care units predicts fatal outcome in sepsis patients. Crit Care. 2013;17:R115. doi: 10.1186/cc12787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryu JA, Yang JH, Lee D, Suh GY, et al. Clinical uselfulness of procalcitonin and C-reactive protein as outcome predictors in critically patients with severe sepsis and septic schock. PLoS One. 2015;10:e0138150. doi: 10.1371/journal.pone.0138150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bouadma L, Luyt CE, Tubach F, Cracco C, et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet. 2010;375(9713):463–474. doi: 10.1016/S0140-6736(09)61879-1. [DOI] [PubMed] [Google Scholar]
- 19.Mokart D, Merlin M, Sannini A, Brun JP, et al. Procalcitonin, Interleucin 6 and systemic inflammatory response syndrome (SIRS): early markers of sepsis after major surgery. Br J Anaesth. 2005;94:767–773. doi: 10.1093/bja/aei143. [DOI] [PubMed] [Google Scholar]
- 20.Meyer ZC, Schreinemakers JM, de Waal RA, van der Laan L. Searching for predictors of surgical complications in critically ill surgery patients in the intensive care unit: a review. Surg Today. 2015;45:1091–1101. doi: 10.1007/s00595-015-1159-6. [DOI] [PubMed] [Google Scholar]
- 21.Seoane L, Pertega S, Galeiras R, Astola I, Bouza T. Procalcitonin in the burn unit and the diagnosis of infection. Burns. 2014;40:223–229. doi: 10.1016/j.burns.2013.11.018. [DOI] [PubMed] [Google Scholar]
- 22.Honore PM, Spapen HD. The struggle to differentiate inflammation from infection in severely burned patients: time to send better biomarkers into the arena? Crit Care. 2016;20:13. doi: 10.1186/s13054-016-1194-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenhalgh DG, Saffle JR, Holmes JH, et al. American burn association consensus conference to define sepsis and infection in burns. J Burn Care Res. 2007;17:R115. doi: 10.1097/BCR.0b013e3181599bc9. [DOI] [PubMed] [Google Scholar]
- 24.Kibe S. Diagnostic and prognostic biomarkers of sepsis in critical care. J Antimicrob Chemother. 2011;66(Suppl.2):ii33–ii40. doi: 10.1093/jac/dkq523. [DOI] [PubMed] [Google Scholar]
- 25.Long B, Koyfman A. Ready for prime time? Biomarkers in Sepsis. Emerg Med Clin North Am. 2017;35:109–122. doi: 10.1016/j.emc.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Sandquist M, Wong HR. Biomarkers of sepsis and their potential value in diagnosis, prognosis and treatment. Expert Rev Clin Immunol. 2014;10:1349–1356. doi: 10.1586/1744666X.2014.949675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yan S, Tsurumi A, Que YA, Ryan CM, et al. Prediction of multiple infections after severe burn trauma: a prospective cohort control. Ann Surg. 2015;261:781–791. doi: 10.1097/SLA.0000000000000759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hazeldine J, Hampson P, Lord JM. The diagnostic and prognostic value of systems biology research in major traumatic and thermal injury: a review. Burns & Trauma. 2016;4:33. doi: 10.1186/s41038-016-0059-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.David VL, Ercisli MF, Rogobete AF, Boia ES, et al. Early prediction of sepsis incidence in critically ill patients using specific genetic polymorphisms. Biochem Genet. 2017;55:193–203. doi: 10.1007/s10528-016-9785-2. [DOI] [PubMed] [Google Scholar]
- 30.Harbarth S, Holeckova K, Froidevaux C, Pittet D, et al. Diagnostic value of procalcitonin, interleukin-6 and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med. 2001;164:396–402. doi: 10.1164/ajrccm.164.3.2009052. [DOI] [PubMed] [Google Scholar]
- 31.Tang BM, Eslick GD, Craig JC, McLean AS. Accuracy of procalcitonin for sepsis diagnosis in critically ill patients: systemic review and meta-analysis. Lancet Infect Dis. 2007;7:210–217. doi: 10.1016/S1473-3099(07)70052-X. [DOI] [PubMed] [Google Scholar]
- 32.Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker of sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13:426–435. doi: 10.1016/S1473-3099(12)70323-7. [DOI] [PubMed] [Google Scholar]
- 33.Garnacho-Montero J, Huici-Moreno MJ, Gutierrez-Pizarraya A, López I, et al. Prognostic and diagnostic value of eosinopenia, C-reactive protein, procalcitonin and circulating cell-free DNA in critically ill patients admitted with suspicion of sepsis. Crit Care. 2014;18:R116. doi: 10.1186/cc13908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lippi G, Montagnana M, Balboni F, Bellone A, et al. Academy of emergency medicine and Care-Society of Clinical Biochemestry and Clinical Molecular Biology consensus recommendations for clinical use of sepsis biomarkers in the emergency department. Emergency Care Journal. 2017;13:6877. [Google Scholar]
- 35.Sager R, Kutz A, Mueller B, Schuetz P. Procalcitonin-guided diagnosis and antibiotic stewardship revisited. BMC Med. 2017;15(15) 10.10186/s12916-017-0795-7. [DOI] [PMC free article] [PubMed]
- 36.Vincent JL. The clinical challenge of sepsis identification and monitoring. PLoS Med. 2016;13:e10012022. doi: 10.1371/journal.pmed.1002022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.de Jong E, van Oers JA, Beishuizen A, et al. Efficacy and safety of procalcitonin guidance in reducing the duration of antibiotic treatment in critically ill patients: a randomised, controlled, open-label trial. Lancet Infect Dis. 2016;16:819–827. doi: 10.1016/S1473-3099(16)00053-0. [DOI] [PubMed] [Google Scholar]
- 38.Schuetz P, Chiappa V, Briel M, Greenwald JL. Procalcitonin algorithms for antibiotic therapy decisions: a systematic review of randomized controlled trials and recommendations for clinical algorithms. Arch Intern Med. 2011;171:1322–1331. doi: 10.1001/archinternmed.2011.318. [DOI] [PubMed] [Google Scholar]
- 39.Molnár Z, Bogár L. Let’s go dynamic with procalcitonin. Crit Care Med. 2006;34:2687–2688. doi: 10.1097/01.CCM.0000240788.00292.F1. [DOI] [PubMed] [Google Scholar]
- 40.Vincent JL. Sepsis biomarkers – values and limitations. Am J Respir Crit Care Med. 2014;190:1081–1082. doi: 10.1164/rccm.201410-1895ED. [DOI] [PubMed] [Google Scholar]
- 41.Lipinska-Gediga M, Mierzchata-Pasierb M, Durek G. Procalcitonin kinetics – prognostic and diagnostic significance in septic patients. Arch Med Sci. 2016;12:112–119. doi: 10.5114/aoms.2016.57587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Trasy D, Molnar Z. Procalcitonin – assisted antibiotic strategy in sepsis. J Int Fed Clin Chem. 2017;28:104–113. [PMC free article] [PubMed] [Google Scholar]
- 43.Schuetz P, Robert Birkhahn R, Robert Sherwin R, Jones AE, et al. Serial procalcitonin predicts mortality in severe sepsis patients: results from the multicenter procalcitonin monitoring sepsis (MOSES) study. Crit Care Med. 2017;45:781–789. doi: 10.1097/CCM.0000000000002321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schüttler J. Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med. 1998;24:680–684. doi: 10.1007/s001340050644. [DOI] [PubMed] [Google Scholar]
- 45.Sponholz C, Sakr Y, Reinhart K, Brunkhorst F. Diagnostic value and prognostic implications of serum procalcitonin after cardiac surgery: a systematic review of the literature. Crit Care. 2006;10:R145. doi: 10.1186/cc5067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Friederichs J, Hutter M, Hierholzer C, Novotny A, et al. Procalcitonin as a predictor of successful surgical treatment of severe necrotizing soft tissue infections. Am J Surg. 2013;206:368–373. doi: 10.1016/j.amjsurg.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 47.Muñoz JL, Ruiz-Tovar J, Miranda E, Berrio DL, et al. C-reactive protein and procalcitonin as early markers of septic complications after laparoscopic sleeve gastrectomy in morbidly obese patients with an enhanced recovery after surgery program. J Am Coll Surg. 2016;222:831–837. doi: 10.1016/j.jamcollsurg.2016.01.059. [DOI] [PubMed] [Google Scholar]
- 48.Varetto G, Castagno C, Trucco A, Frola E, et al. Serum procalcitonin as a valuable diagnostic tool in the early detection of infectious complications after abdominal aortic repair. Ann Vasc Surg. 2016;34:111–118. doi: 10.1016/j.avsg.2016.01.012. [DOI] [PubMed] [Google Scholar]
- 49.Spoto S, Valeriani E, Caputo D, Cella E, et al. The role of procalcitonin in the diagnosis of bacterial infection after major abdominal surgery - advantage from daily measurement. Medicine. 2018;3(e9496):97. doi: 10.1097/MD.0000000000009496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bargues L, Chancerelle Y, Catineau J, Jault P, Carsin H. Evaluation of serum procalcitonin concentration in the ICU following severe burn. Burns. 2007;33:860–864. doi: 10.1016/j.burns.2006.10.401. [DOI] [PubMed] [Google Scholar]
- 51.Schultz L, Walker SA, Elligsen M, Walker SE. Identification of predictors of early infection in acute burn patients. Burns. 2013;39:1355–1366. doi: 10.1016/j.burns.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 52.Lavrentieva A, Kontakiotis T, Lazaridis L, et al. Inflammatory markers in patients with severe burn injury: What is the best indicator of sepsis. Burns. 2007;33:189. doi: 10.1016/j.burns.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 53.Barati M, Alinejad F, Bahar MA, et al. Comparison of WBC, ESR, CRP and PCT serum levels in septic and non-septic burn cases. Burns. 2008;34:770–774. doi: 10.1016/j.burns.2008.01.014. [DOI] [PubMed] [Google Scholar]
- 54.Mokline A, Garsallah L, Rahmani I, Jerbi K, et al. Procalcitonin: a diagnostic and prognostic biomarker of sepsis in burned patients. Ann Burns Fire Disasters. 2015;28:116–120. [PMC free article] [PubMed] [Google Scholar]
- 55.Cabral L, Afreixo V, Santos S, Almeida L, Paiva JA. Procalcitonin for the early diagnosis of sepsis in burn patients; a retrospective study. Burns. 2017;43:1427–1434. doi: 10.1016/j.burns.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 56.Mann EA, Wood GL, Wade CE. Use of procalcitonin for the detection of sepsis in the critically ill burn patient: a systematic review of the literature. Burns. 2011;37:549–558. doi: 10.1016/j.burns.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 57.Ren H, Li Y, Han C, Hu H. Serum procalcitonin as a diagnostic biomarker for sepsis in burn patients: a meta-analysis. Burns. 2015;41:502–509. doi: 10.1016/j.burns.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 58.Cabral, V Afreixo, L Almeida, Paiva JA. The use of procalcitonin (PCT) for diagnosis of sepsis in burn patients: a meta-analysis. PLoS One 2016;11: e0168475. DOI:10.1371/journal.pone.0168475. [DOI] [PMC free article] [PubMed]
- 59.von Heimburg D, Stieghorst W, Khorram-Sefat R, Pallua N. Procalcitonin – a sepsis parameter in severe burn injuries. Burns 1998;24:745–750. PMID:9915676. [DOI] [PubMed]
- 60.Sachse C, Machens HG, Felmerer G, Berger A, Henkel E. Procalcitonin as a marker for the early diagnosis of severe infection after thermal injury. J Burn Care Rehabil. 1999;20:354–360. doi: 10.1097/00004630-199909000-00004. [DOI] [PubMed] [Google Scholar]
- 61.Ciriello V, Gudipati S, Stavrou PZ, Kanakaris NK, et al. Biomarkers predicting sepsis in polytrauma patients: current evidence. Injury. 2013;44:1680–1692. doi: 10.1016/j.injury.2013.09.024. [DOI] [PubMed] [Google Scholar]
- 62.Billeter A, Turina M, Seifert B, Mica L, et al. Early serum procalcitonin, interleukin-6 and 24-hour lactate clearance: useful indicators of septic infections in severely traumatized patients. World J Surg. 2009;33:558–566. doi: 10.1007/s00268-008-9896-y. [DOI] [PubMed] [Google Scholar]
- 63.Lavrentieva A, Papadopoulou S, Kioumis J, Kaimakamis E, Bitzani M. PCT as a diagnostic and prognostic tool in burn patients - whether time course has a role in monitoring sepsis treatment. Burns. 2012;38:356–363. doi: 10.1016/j.burns.2011.08.021. [DOI] [PubMed] [Google Scholar]
- 64.Egea Guerrero JJ, Martínez-Fernandez C, Rodríguez-Rodríguez A, Bohorquez-López A, et al. The utility of C-reactive protein and procalcitonin for sepsis diagnosis in critically burned patients: a preliminary study. Plastic Surgery. 2015;23:239–243. doi: 10.1177/229255031502300412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kim HS, Yang HT, Hur J, Chun W, et al. Procalcitonin levels within 48 hours after burn injury as a prognostic factor. Ann Clin Lab Sci. 2012;42:57–64. [PubMed] [Google Scholar]
- 66.Dahaba AA, Hagara B, Fall A, Rehak PH, et al. Procalcitonin for early prediction of survival outcome in postoperative critically ill patients with severe sepsis. Br J Anaesth. 2006;97:503–508. doi: 10.1093/bja/ael181. [DOI] [PubMed] [Google Scholar]
- 67.Ljungström L, Pernestig A-K, Jacobsson G, Andersson R, Usener B, Tilevik D. Diagnostic accuracy of procalcitonin, neutrophil-lymphocyte count ratio, C-reactive protein, and lactate in patients with suspected bacterial sepsis. PLoS One. 2017;12:e0181704. doi: 10.1371/journal.pone.0181704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Riedel S. Procalcitonin and the role of biomarkers in the diagnosis and management of sepsis. Diagn Microbiol Infect Dis. 2012;73:221–227. doi: 10.1016/j.diagmicrobio.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 69.Bele N, Darmon M, Coquet I, Feugeas JP, et al. Diagnostic accuracy of procalcitonin in critically ill immunocompromised patients. BMC Infect Dis. 2011;11:224. doi: 10.1186/1471-2334-11-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schuetz P, Albrich W, Christ-Crain M, Chastre J, Mueller B. Procalcitonin for guidance of antibiotic therapy. Expert Rev Anti-Infect Ther. 2010;8:575–587. doi: 10.1586/eri.10.25. [DOI] [PubMed] [Google Scholar]
- 71.Hattori T, Nishiyama H, Kato H, Ikegami S, et al. Clinical value of procalcitonin for patients with suspected bloodstream infections. Am J Clin Pathol. 2014;141:43–51. doi: 10.1309/AJCP4GV7ZFDTANGC. [DOI] [PubMed] [Google Scholar]
- 72.Steuten L, Mantjes G. Economic value of procalcitonin guidance. Lancet Infect Dis. 2016;16(9):1000. doi: 10.1016/S1473-3099(16)30258-4. [DOI] [PubMed] [Google Scholar]
- 73.Balk RA, Kadri SS, Cao Z. Effect of procalcitonin testing on health-care utilization costs in critically ill patients in the United States. Chest. 2017;151:23–33. doi: 10.1016/j.chest.2016.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Abbreviated Burn Severity Index. (DOCX 17 kb)
Data Availability Statement
The data that support the findings of this study are available from the datasets of the Clinical Pathology Department and the Informatics Department of Coimbra University Hospital Centre, but restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available. However, data are available from the authors upon reasonable request and after permission of the Ethics Committee from Coimbra University Hospital Centre.


