Sir,
A 51-year-old female, came to the skin outpatient department with a single discharging growth over the cheek, which was gradually increasing and was relatively asymptomatic. Cutaneous examination showed a single 2 cm×2 cm-sized well-defined exophytic nodule over the right cheek lateral to the ala of the nose with crusting, ulcer and blood vessels were running from the periphery [Figure 1]. No history of weight loss, abdominal pain, and pulmonary or neurological symptoms had been reported. No regional lymphadenopathy was seen. Systemic examination revealed no abnormalities. No significant family history was elicited. Routine investigations and chest X-rays were normal. Dermoscopy was done, showed a heterogeneous yellowish background with peripheral blood vessels and areas of ulceration [Figure 2]. An excisional biopsy was done keeping keratoacanthoma, basal cell carcinoma (BCC), and squamous cell carcinoma (SCC) as clinical differentials. Histopathology showed changes suggestive of sebaceous cell carcinoma. The depth of the tumor was 0.3 cm which composed of the irregular lobular formation with variation in size. The epidermis was ulcerated focally with an infiltrative growth of tumor in dermis [Figure 3a]. Many undifferentiated cells and few sebaceous cells with foamy cytoplasm were present in lobules [Figure 3b]. The undifferentiated cells have round-to-oval pleomorphic nuclei with dispersed chromatin and eosinophilic cytoplasm [Figure 3c]. Foci of atypical keratinizing cells and secondary neutrophilic exudates were seen.
Figure 1.

Single nodule over the right side of cheek lateral to the ala of the nose with crusting, ulcer, and blood vessels running from the periphery
Figure 2.
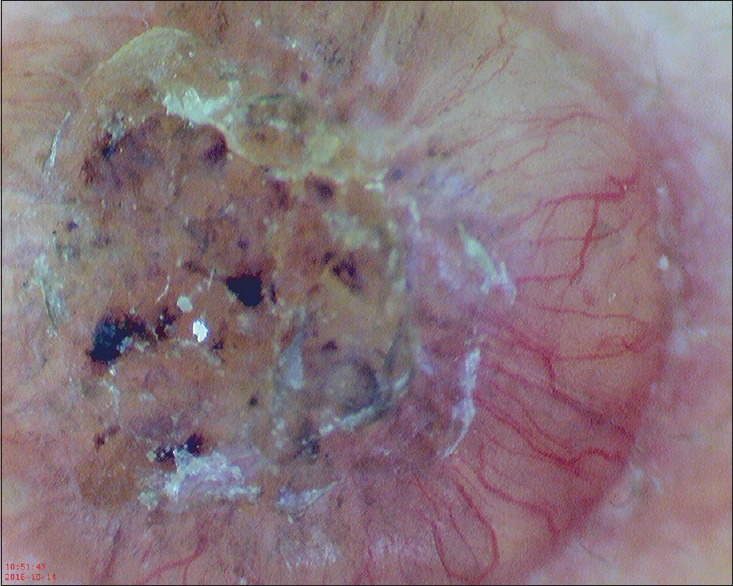
Dermatoscopy showing heterogeneous yellowish background with peripheral blood vessels and areas of ulceration
Figure 3.
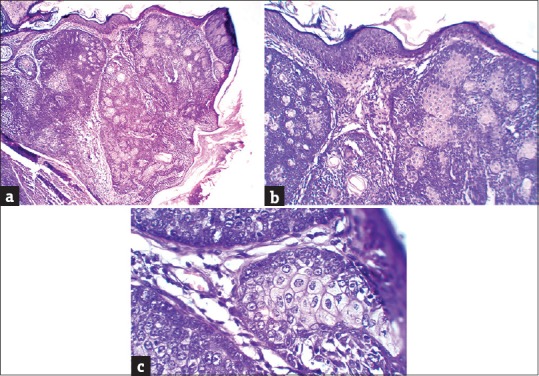
(a) Ulcerated epidermis focally with an infiltrative growth pattern of tumor in dermis (H and E, ×40) (b) Many undifferentiated cells with sebaceous cells having foamy cytoplasm (H and E, ×100) (c) The undifferentiated cells have round-to-oval pleomorphic nuclei with dispersed chromatin and eosinophilic cytoplasm (H and E, ×400)
Sebaceous carcinoma (SC) is a rare aggressive adnexal tumor arising from sebaceous glands with frequency varying from 0.2% to 4.6% of all malignant cutaneous neoplasms.[1] The majority of SCs occur in the periocular region, over the eyelid. Extraocular SC (EOSC) accounts for only 25% of all reported cases of SC.[2] The site of EOSC is head and neck, with parotid glands being the most common followed by nose, face, and neck. It is also reported over external genitalia, external auditory canal, axilla, trunk, and upper extremity.[2]
EOSC shows nearly equal gender distribution and takes varied morphological and histological appearance, leading to delayed diagnosis or misdiagnosis. SC is traditionally classified into two groups: tumors arising from the ocular adnexa particularly the meibomian glands and glands of Zeis and those arising in extraocular sites. Three-quarters of cases occur in the periocular region, particularly on the eyelids, arising especially from the meibomian glands.[2]
The exact etiology of SC is not known. Most of the SCs arise de novo; however, some tumors have been shown to originate from benign tumors such as actinic keratosis, nevus sebaceous, mature cystic teratoma, or pleomorphic adenoma.[3]
A higher frequency of SC in the Asian population without documented causes is reported.[2] Genetic factors are involved in its pathogenesis. SC can be sporadic or associated with Muir–Torre syndrome (MTS). Factors associated with sporadic histogenesis include older age, female sex, ultraviolet exposure, previous radiation therapy in the tumor site, and immunosuppression.[4]
Clinically, EOSC presents as a pink-to-red-yellow slowly enlarging firm dermal or subcutaneous nodule ranging from 6 mm to 20 cm in size.[2] Tendency for ulceration and spontaneous bleeding is seen in one-third of the cases. It can also present as pedunculated lesion, irregular mass, or diffuse thickening of the skin.
The morphological and histological findings for EOSC may resemble those of basal cell carcinoma, squamous cell carcinoma, melanoma, or other less common glandular or adnexal tumors, thereby leading to delay in the diagnosis, inappropriate treatment, and an increase in morbidity and mortality.[2]
Dermoscopic evaluation of suspected SC lesions helps differentiating them from benign sebaceous proliferations. Malignant lesions tend to have irregular abruptly ending border, various colors in a single dermoscopic field, pleomorphic vessels, and presence of ulceration. Benign tumors have homogeneous background with yellow, ovoid structures and regularly distributed crown vessels around a central crater, while SC exhibits heterogeneous yellowish background with irregular and polymorphous vessels, with areas of ulceration,[5] as was seen in our case.
The difference with a benign sebaceous lesion is the vascular pattern, which is regular in sebaceous hyperplasia and sebaceous adenoma but irregular and widely distributed in SC. The key to differentiate SC from other cutaneous carcinomas would be characteristic yellow background.[6]
BCC with sebaceous differentiation may display yellowish areas; however along with yellow areas, other features specific to BCC are also seen in dermoscopy, for example, superficial fine telangiectasia, blue-gray ovoid nests, and spoke wheel areas.[7] SCC on dermoscopy shows glomerular vessels with scaly surface, and keratoacanthoma shows central structureless keratin with arborizing vessels.[8] In both conditions, yellow areas are absent which were characteristically seen in our case.
Histopathologically, SCs are often poorly differentiated neoplasms mainly in dermis. Multiple lobules of basaloid undifferentiated cells are present in the dermis. In the central portion of lobules, more mature cells are present. Marked nuclear atypia, pleomorphism, and mitoses are common.[2]
EOSC has shown to have a better prognosis than ocular variant. However, a review of the recent literature has revealed that EOSC has a tendency to be locally aggressive, to develop cutaneous recurrence, and to metastasize widely,[9] the risk of metastasis from sporadic SC seems to be higher than one associated with Muir–Torre syndrome.
The most common site of metastasis is in the draining lymph node.[10] Distant metastases have been reported in <10% of all EOSC cases, which may occur in the abdomen lung, brain, bone, and subcutaneous soft tissue.[10]
Histochemically, the clear cells of SC are negative with periodic acid-Schiff and Alcian-blue stainings. Immunohistochemically, the tumor cells of SC show positive reactions for epithelial membrane antigen and cytokeratin. The positivity for human milk fat globules subclasses 1 and 2 (HMFG1 and HMFG2) helps to distinguish it from BCC.[11]
The treatment of choice for SC is surgical, with complete excision verified by negative margins. Radiotherapy and chemotherapy are used with metastatic disease or with a high risk of recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bassetto F, Baraziol R, Sottosanti MV, Scarpa C, Montesco M. Biological behavior of the sebaceous carcinoma of the head. Dermatol Surg. 2004;30:472–6. doi: 10.1111/j.1524-4725.2004.30025.x. [DOI] [PubMed] [Google Scholar]
- 2.Nelson BR, Hamlet KR, Gillard M, Railan D, Johnson TM. Sebaceous carcinoma. J Am Acad Dermatol. 1995;33:1–5. doi: 10.1016/0190-9622(95)90001-2. [DOI] [PubMed] [Google Scholar]
- 3.Mariem M, Lobna B, Abdlefaddeh S, Mohamed D, Colandane B, Bedreddine S, et al. Extra-ocular sebaceous carcinoma of the skin: A report of five cases and a review of the literature. Am J Med Case Rep. 2015:91–6. [Google Scholar]
- 4.Buitrago W, Joseph AK. Sebaceous carcinoma: The great masquerader: Emgerging concepts in diagnosis and treatment. Dermatol Ther. 2008;21:459–66. doi: 10.1111/j.1529-8019.2008.00247.x. [DOI] [PubMed] [Google Scholar]
- 5.Miyamoto D, Wang B, Miyamoto C, Aoki V, Lim LA, et al. Sebaceous cell carcinoma: A persistent challenge in clinical and histopathological diagnosis. J Clin Exp Dermatol Res. 2016;7:353. [Google Scholar]
- 6.Satomura H, Ogata D, Arai E, Tsuchida T. Dermoscopic features of ocular and extraocular sebaceous carcinomas. J Dermatol. 2017;44:1313–6. doi: 10.1111/1346-8138.13905. [DOI] [PubMed] [Google Scholar]
- 7.Longo C, Lallas A, Kyrgidis A, Rabinovitz H, Moscarella E, Ciardo S, et al. Classifying distinct basal cell carcinoma subtype by means of dermatoscopy and reflectance confocal microscopy. J Am Acad Dermatol. 2014;71:716–24. doi: 10.1016/j.jaad.2014.04.067. [DOI] [PubMed] [Google Scholar]
- 8.Rosendahl C, Cameron A, Argenziano G, Zalaudek I, Tschandl P, Kittler H, et al. Dermoscopy of squamous cell carcinoma and keratoacanthoma. Arch Dermatol. 2012;148:1386–92. doi: 10.1001/archdermatol.2012.2974. [DOI] [PubMed] [Google Scholar]
- 9.Moreno C, Jacyk WK, Judd MJ, Requena L. Highly aggressive extraocular sebaceous carcinoma. Am J Dermatopathol. 2001;23:450–5. doi: 10.1097/00000372-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Duman DG, Ceyhan BB, Celikel T, Ahiskali R, Duman D. Extraorbital sebaceous carcinoma with rapidly developing visceral metastases. Dermatol Surg. 2003;29:987–9. doi: 10.1046/j.1524-4725.2003.29268.x. [DOI] [PubMed] [Google Scholar]
- 11.Mari Y, Norito I, Shoji N, Takekuni N, Osamu M, Takashi H. Two cases of extraocular sebaceous carcinoma. Nishinihon J Dermatol. 2000;62:199–203. [Google Scholar]


