Short abstract
Objective
Diagnosis of pulmonary cryptococcosis is difficult. In this study, we examined the clinical and radiological features that increase the diagnostic accuracy for pulmonary cryptococcosis.
Methods
This retrospective study included clinical data from 68 patients with pulmonary cryptococcosis from 2012 to 2016 in 3 tertiary hospitals.
Results
Among the 68 patients, 39 (57.35%) had no complications, 39 (57.35%) had clinical symptoms, 6 (8.82%) had a history of occupational exposure, 27 (39.71%) had a single nodule/mass (the most common type of pulmonary cryptococcosis) on chest computed tomography images, 21 (30.88%) had multiple nodules/masses, 16 (23.53%) had ground glass opacity with or without nodules, 2 (2.94%) had miliary nodules, and 2 (2.94%) had enlarged mediastinal lymph nodes. Fifty-three (77.94%) patients had lesions with irregular margins, 33 (48.53%) had spiculated lesions, 32 (47.06%) had air bronchograms, 9 (13.24%) had cavities, and 4 (5.88%) had calcifications. Twenty-four patients underwent surgery, 35 received antifungal treatment, and 9 received both treatments.
Conclusion
The clinical features and computed tomography signs found in this study are not specific for a diagnosis of pulmonary cryptococcosis. Therefore, an increased awareness of pulmonary cryptococcosis is needed among clinicians.
Keywords: Pulmonary cryptococcosis, chest computed tomography, single nodule/mass, multiple nodules/masses, miliary nodules, enlarged mediastinal lymph nodes
Introduction
Cryptococcal disease (cryptococcosis) is caused by Cryptococcus spp., which are basidiomycetes. Each year worldwide, approximately 1 million patients with human immunodeficiency virus (HIV) develop cryptococcosis and approximately 625,000 HIV/acquired immunodeficiency syndrome (AIDS)-associated deaths occur.1 The number of HIV-negative patients is currently increasing.
Cryptococcal disease may be pulmonary; it may also present as cryptococcal meningoencephalitis or skin/subcutaneous, ophthalmic, bone, or prostatic disease. Inhalation of cryptococcal aerosol particles into the respiratory tract is the most common route of infection.2,3 , Pulmonary cryptococcosis is often misdiagnosed as tuberculosis or lung cancer because of the similar clinical features (coughing, expectoration, chest tightness, fever, or absence of symptoms) and radiological characteristics (nodules, cavities, and enlarged lymph nodes). The main diagnostic methods are culturing of clinical samples, detection of cryptococcal antigen in body fluids, and histopathological examination of tissue sections.4 However, these methods may be invasive depending on the specimen collection and culture techniques. Chest computed tomography (CT) is a noninvasive and repeatable method that can be used to evaluate the overall course of pulmonary disease. Few studies have focused on the chest CT characteristics of pulmonary cryptococcosis. In the present study, we retrospectively reviewed multiple clinical and chest CT findings of patients with pulmonary cryptococcosis to improve the diagnosis of this type of pulmonary infectious disease.
Patients and methods
We reviewed the clinical data of patients with pulmonary cryptococcosis from January 2012 to December 2016 in three tertiary hospitals. All patients’ diagnoses were confirmed by pathological examination after pulmonary segmentectomy/wedge resection or CT-guided percutaneous biopsy, and cerebrospinal fluid was collected from a small proportion of the patients. This study was approved by the Research Ethics Committee of Beijing Shijitan Hospital affiliated to Capital Medical University.
All patients were scanned by 64-row multi-slice spiral CT. The patients were placed in the supine position and asked to hold their breath during scanning. The scans were obtained at 1.25-mm intervals throughout the chest using 1.5-mm collimation and were reconstructed with a high-spatial-frequency algorithm. The images were photographed at window settings appropriate for assessing the lung parenchyma (window level, –600 Hounsfield units; window width, 1,600 Hounsfield units). The CT images were retrospectively reviewed by two independent experienced radiologists. The size, number, location, border, and internal characteristics of any pulmonary nodules or masses were recorded. The presence of air bronchograms, the halo sign, cavities, calcification, and pleural effusions was also noted. The CT attenuation values of the nodules or masses were measured in the largest parts of the lesions, which were located away from the air density area. The mean attenuation values were calculated from three randomly selected nodule locations.
The patients’ complications, clinical manifestations, radiological images, and therapeutic effects were retrospectively analyzed. Because this was a retrospective study, the three hospital ethics committees did not seek informed consent from patients.
Results
This study included 68 patients (46 male, 22 female; 3 children, 4 adolescents, 20 young adults, 30 middle-aged patients, and 11 elderly patients). The clinical and radiological features of the patients are shown in Table 1. The diagnosis was confirmed by pulmonary segmentectomy or wedge resection in 35 patients and CT-guided percutaneous biopsy in 33 patients. Cerebrospinal fluid was collected from five patients.
Table 1.
Demographics and clinical information of patients with pulmonary cryptococcosis
| Target68 | Single nodule/mass(n = 27) | Multiple nodules/masses(n = 21) | GGO/GGO with nodules(n = 16) | Miliary nodules(n = 2) | Enlarged mediastinal lymph nodes(n = 2) |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 21 | 15 | 8 | 1 | 1 |
| Female | 6 | 6 | 8 | 1 | 1 |
| Age (years) | |||||
| 0–12 | 0 | 0 | 0 | 1 | 2 |
| 13–20 | 1 | 1 | 1 | 1 | 0 |
| 21–44 | 9 | 6 | 5 | 0 | 0 |
| 45–59 | 14 | 9 | 7 | 0 | 0 |
| ≥60 | 3 | 5 | 3 | 0 | 0 |
| Symptoms | |||||
| None | 17 | 9 | 3 | 0 | 0 |
| Cough | 4 | 5 | 5 | 0 | 0 |
| Fever | 2 | 1 | 2 | 0 | 0 |
| Cough, fever | 2 | 1 | 4 | 2 | 2 |
| Chest pain | 2 | 5 | 2 | 0 | 0 |
| History | |||||
| Diabetes | 1 | 1 | 2 | 0 | 0 |
| Tuberculosis | 1 | 1 | 0 | 0 | 0 |
| Malignant tumor | 1 | 4 | 1 | 1 | 0 |
| Liver cirrhosis | 0 | 1 | 2 | 0 | 0 |
| Glucocorticoid therapy | 2 | 0 | 6 | 0 | 0 |
| Occupational exposure | 1 | 1 | 1 | 1 | 2 |
| CT characteristics | |||||
| Irregular margin | 21 | 17 | 11 | 2 | 2 |
| Spiculated | 18 | 9 | 6 | 0 | 0 |
| Air bronchogram | 14 | 5 | 12 | 0 | 1 |
| Halo sign | 7 | 6 | 9 | 0 | 0 |
| Cavity | 3 | 4 | 1 | 1 | 0 |
| Calcifications | 2 | 2 | 0 | 0 | 0 |
| Primary diagnosis | |||||
| Lung cancer | 17 | 8 | 2 | 0 | 0 |
| Tuberculosis | 1 | 3 | 0 | 1 | 2 |
| Bacterial infection | 3 | 7 | 12 | 1 | 0 |
| Treatment | |||||
| Surgery | 19 | 4 | 1 | 0 | 0 |
| Antifungals | 4 | 14 | 13 | 2 | 2 |
| Surgery combined with antifungals | 4 | 3 | 2 | 0 | 0 |
| Prognosis | |||||
| CNS cryptococcosis | 2 | 0 | 1 | 2 | 0 |
| Significantly small | 4 | 4 | 3 | 1 | 1 |
| No recurrence | 22 | 15 | 11 | 1 | 1 |
| Unknown | 1 | 2 | 2 | 0 | 0 |
GGO, ground glass opacity; CT, computed tomography; CNS, central nervous system
The most common symptoms were cough (5.8%), fever (2.9%), and chest pain (2.9%); however, most patients had an asymptomatic infection (25.0%). Four patients (5.8%) had diabetes, 2 (2.9%) had pulmonary tuberculosis, 7 (10.2%) had malignant tumors (breast cancer, n = 2; malignant lymphoma, n = 3; liver cancer, n = 1; and yolk sac tumor, n = 1), 3 (4.4%) had liver cirrhosis, and 8 (11.8%) were taking glucocorticoids (pituitary adenoma, n = 2; psoriasis, n = 2; rheumatoid disease, n = 3; and optic neuritis, n = 1). Six patients (8.8%) had a history of occupational exposure (raising chickens and pigeons, n = 4; contact with live poultry n = 1; and working in a live poultry market, n = 1).
The diameter of 44.44% of lesions ranged from 1.1 to 2.0 cm. Lesions with an irregular margin (77.78%), spiculated lesions (66.67%), air bronchograms (51.85%), and the halo sign (25.93%) were more common than calcification (7.41%) and cavities (11.11%). The cavities in pulmonary cryptococcosis lesions were usually small and smooth. The largest lesions of 47.61% of the multiple nodules/masses had a diameter of 1.1 to 2.0 cm. A total of 61.90% of lesions were 2.0 to 4.0 cm, and a fusion trend was found. Most of the lesions were circular and distributed along the bronchial bundle, without the tree-in-bud pattern. The largest lesions were characterized by irregular margins (80.95%) and spiculation (42.86%). Calcification (19.05%) and cavities (9.52%) were rare. GGO/GGO with nodules were associated with irregular margins (68.75%), air bronchograms (75.00%), and the halo sign (56.25%). Cavities (6.25%) were rare, and calcification was not found. The edges of the miliary nodules were not smooth and calcified. The enlarged mediastinal lymph nodes had irregular margins. Pleural effusion was often found in young children.
Chest CT images showed that the lesions of 66 patients were in the peripheral region of the lung. Cavities were seen in nine patients, six of whom had complications. A single nodule/mass was seen in 27 patients (39.71%) (Figure 1): the diameters were 0.1 to 1.0 cm in 2 patients, 1.1 to 2.0 cm in 12 patients, 2.1 to 3.0 cm in 8 patients, and >3.0 cm in 1 patient. The characteristics of the single nodules/masses were an irregular margin (21/27), spiculation (18/27), air bronchograms (14/27), the halo sign (7/27), cavities (3/27), and calcification (2/27). Multiple nodules/masses were present on the CT scans of 21 patients (30.88%) (Figure 2). The diameter of the largest lesion in was 0.1 to 1.0 cm in 2 patients, 1.1 to 2.0 cm in 10 patients, 2.1 to 3.0 cm in 6 patients, and >3.1 cm in 3 patients. The number of lesions ranged from 2 to 4 in 13 patients, 5 to 7 in 6 patients, and 8 to 10 in 2 patients. The characteristics of the maximal lesion were an irregular margin (17/21), spiculation (9/21), air bronchograms (5/21), the halo sign (6/21), cavities (4/21), and calcification (2/21). Ground glass opacity (GGO)/GGO with nodules were present on the CT scans of 16 patients (23.53%) (Figure 3). The characteristics of these lesions were an irregular margin (11/16), spiculation (6/16), air bronchograms (12/16), the halo sign (9/16), cavities (1/16), and pleural effusion (1/16). Miliary nodules were present on the CT scans of two patients (2.94%) (Figure 4). One of these two patients also had enlarged mediastinal lymph nodes. The characteristics of these lesions were an irregular margin (1/2) and cavities (1/2). The lesions of the remaining two patients were enlarged mediastinal lymph nodes (Figure 5) with characteristics of an irregular margin (2/2), air bronchograms (1/2), and pleural effusion (1/2).
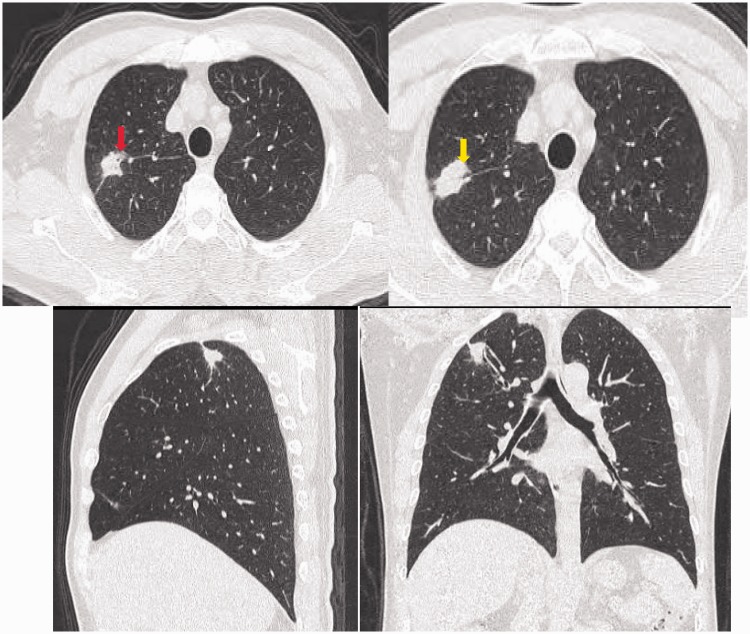
Figure 1.
Representative case of a 54-year-old immunocompetent man with pulmonary cryptococcosis. Computed tomography (lung window) demonstrated a nodule with a clear boundary, a cavity (red arrow), and an air bronchogram (yellow arrow).
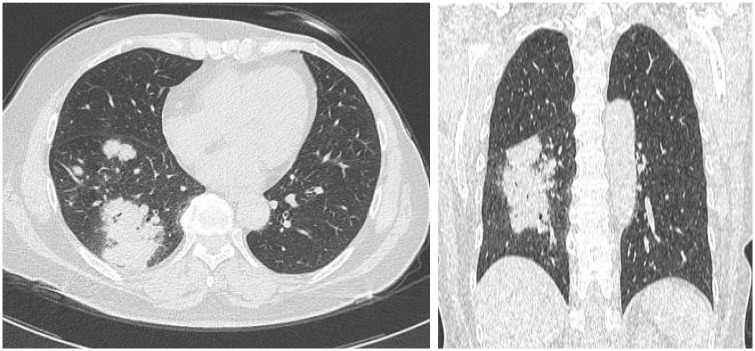
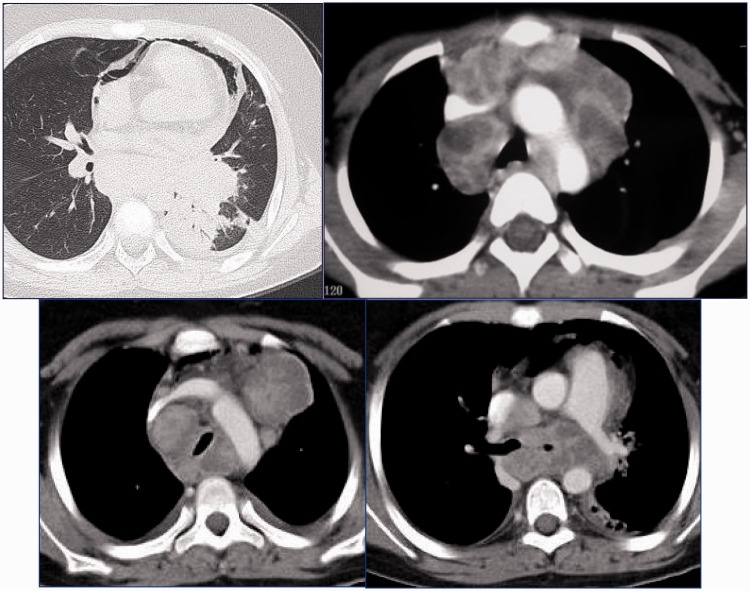
Figure 2.
Representative case of a 58-year-old woman after surgical treatment of breast cancer who developed pulmonary cryptococcosis. Computed tomography (lung window) demonstrated multiple nodules and masses.
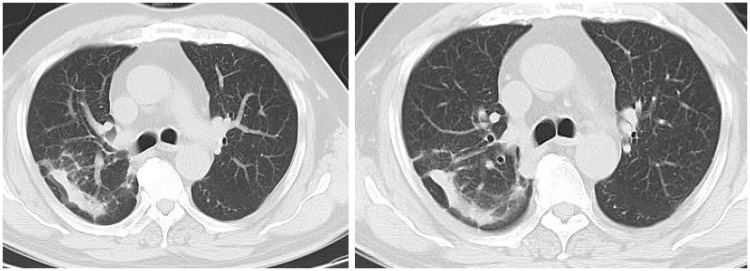
Figure 3.
Representative case of a 72-year-old man with pulmonary cryptococcosis. Computed tomography (lung window) demonstrated ground glass opacity.
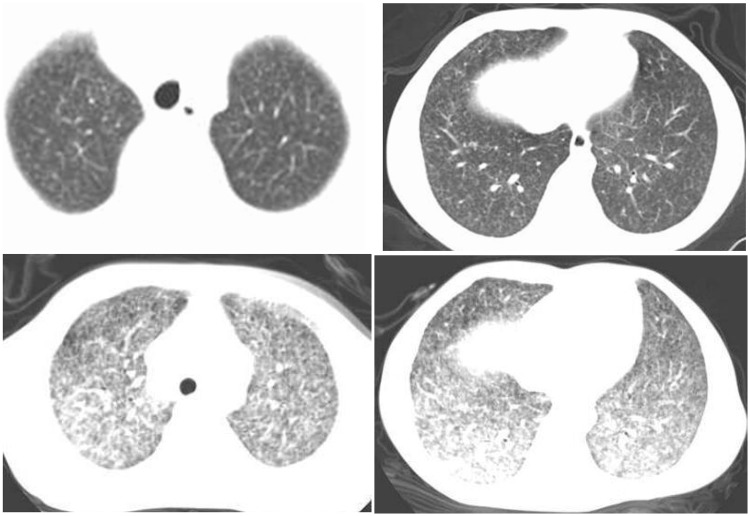
Figure 4.
Representative case of an 11-year-old boy with pulmonary cryptococcosis. Computed tomography (lung window) demonstrated miliary nodules.
Figure 5.
Representative case of a 3-year-old girl with pulmonary cryptococcosis. Computed tomography (lung window) demonstrated enlarged lymph nodes.
Comprehensive analysis of the CT images and clinical data showed that 27 patients (39.71%) were misdiagnosed with lung cancer, 7 (10.29%) were misdiagnosed with tuberculosis, and 23 (33.82%) were misdiagnosed with bacterial pneumonia. Twenty-four patients underwent surgical treatment, 35 received antifungal treatment, and 9 underwent surgery combined with antifungal therapy (of these 9 patients, 3 had a malignant tumor history, 2 were taking hormones, 2 had diabetes, and 1 had tuberculosis). Forty-three patients were treated for 3 to 15 months; 5 patients (patients with central systemic infection) received amphotericin B and flucytosine for 4 weeks, and these drugs were then replaced by voriconazole for 6 to 12 months. Five patients had a central nervous system infection as shown by Cryptococcus spp. in their cerebrospinal fluid. Five patients were lost to follow-up. Finally, the lesions disappeared in 13 patients and no recurrence was found in 50 patients.
Discussion
In recent years, the incidence of Cryptococcus infection has been increasing on an annual basis, especially in immunosuppressed patients such as those with AIDS, those who have undergone organ transplantation, and those with a hematologic malignancy; Cryptococcus neoformans is often detected in such patients.5 However, Cryptococcus infection in AIDS-negative patients is not rare. A previous study showed that Cryptococcus gattii is more likely to cause disease in healthy people.6 As in the present study, 64.71% of patients had no complications in that study.6 The use of glucocorticoids is an important predisposing factor. When cellular immune function is decreased, macrophages cannot efficiently clear away the Cryptococcus microorganisms, leading to dissemination in the lungs and the development of multiple lesions or central nervous system infection. Only six patients in the present study had a history of occupational exposure, suggesting that environmental exposure is not the main clue to diagnosis of this disease.
In addition, 67.65% patients in the present study were male, and this proportion is consistent with other studies.7 Children and adolescents were predisposed to the development of miliary nodules and enlarged mediastinal lymph nodes because of their immature immune systems. In these patients, Cryptococcus often spreads along the lymphatic routes, easily causing enlarged lymph nodes or interlobular septal thickening in the lungs. According to one study most patients with pulmonary cryptococcosis have normal immune function.8 A total of 42.65% of patients had no symptoms in that study, which was inconsistent with the CT findings.8
In the present study, nodules/masses with an irregular margin were often located in the peripheral region of the lung without pleural effusion. The lesions of 13.24% of patients had cavities, especially those with complications, indicating that the formation of cavities is associated with complications. The CT images were difficult to differentiate from lung cancer, tuberculosis, and bacterial infection. The radiological findings suggest that patients with complications are susceptible to GGO/GGO with nodules, while patients with no complications are susceptible to single or multiple nodules/masses. A single nodule/mass (39.7%) was more common than multiple nodules/masses (30.8%), consistent with previous findings.9
The American Thoracic Society recommends fluconazole for treatment of mild to moderate pulmonary cryptococcosis.10 Amphotericin B and fluorouracil are recommended for severe pulmonary cryptococcosis or pulmonary cryptococcosis combined with central nervous system infection. We suggest the use of antifungal drugs to prevent systemic infection after surgery in patients with complications. No consensus has been reached on the course of antifungal treatment after surgery. Our treatment time was 3 months in this study, and no recurrence was found. For patients who are unwilling to undergo surgical treatment, the use of voriconazole alone is effective. Voriconazole shows a certain advantage in the treatment of pulmonary cryptococcosis.
The limitations of this study include the lack of blood laboratory test results. Antigen detection of Cryptococcus is also important for the diagnosis of cryptococcal disease, but such tests were not performed. We did not culture and type the cryptococcal strains; thus, the distributions of C. neoformans and C. gattii in 68 patients and their relationship with the patients’ immune status remain unknown.
In summary, pulmonary cryptococcosis has particular clinical and CT features, but it is often misdiagnosed as lung cancer, tuberculosis, or bacterial pneumonia. Pulmonary cryptococcosis should be considered when patients have predisposing factors and the specific clinical syndromes and CT characteristics discussed herein.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This study was supported by Beijing Outstanding Young Talent Fund (2014000021469G253) and National Natural Science Fund Youth Project (81700007). Additionally, the study was supported by a special fund from the Railway Head Corporation (J2015C001-B).
References
- 1.Park BJ, Wannemuehler KA, Marston BJ, et al. Estimation of the current global burden of cryptococcal meningitis among persons living with hiv/aids. AIDS 2009; 23: 525–530. [DOI] [PubMed] [Google Scholar]
- 2.Brown GD, Denning DW, Gow NA, et al. Hidden killers: Human fungal infections. Sci Transl Med 2012; 4: 165rv113. [DOI] [PubMed] [Google Scholar]
- 3.Chang CC, Sorrell TC, Chen SC. Pulmonary cryptococcosis. Semin Respir Crit Care Med 2015; 36: 681–691. [DOI] [PubMed] [Google Scholar]
- 4.Espinel-Ingroff A, Kidd SE. Current trends in the prevalence of cryptococcus gattii in the united states and canada. Infect Drug Resist 2015; 8: 89–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith IM, Stephan C, Hogardt M, et al. Cryptococcosis due to cryptococcus gattii in germany from 2004-2013. Int J Med Microbiol 2015; 305: 719–723. [DOI] [PubMed] [Google Scholar]
- 6.Teodoro VL, Gullo FP, Sardi Jde C, et al. Environmental isolation, biochemical identification, and antifungal drug susceptibility of cryptococcus species. Rev Soc Bras Med Trop 2013; 46: 759–764. [DOI] [PubMed] [Google Scholar]
- 7.Brizendine KD, Baddley JW, Pappas PG. Predictors of mortality and differences in clinical features among patients with cryptococcosis according to immune status. PloS One 2013; 8:e60431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xie LX, Chen YS, Liu SY, et al. Pulmonary cryptococcosis: Comparison of ct findings in immunocompetent and immunocompromised patients. Acta Radiol 2015; 56: 447–453. [DOI] [PubMed] [Google Scholar]
- 9.Xie X, Xu B, Yu C, et al. Clinical analysis of pulmonary cryptococcosis in non-hiv patients in south China. Int J Clin Exp Med 2015; 8: 3114–3119. [PMC free article] [PubMed] [Google Scholar]
- 10.Limper AH, Knox KS, Sarosi GA, et al. An official american thoracic society statement: Treatment of fungal infections in adult pulmonary and critical care patients. Am J Respir Crit Care Med 2011; 183: 96–128. [DOI] [PubMed] [Google Scholar]