Abstract
Background
Limited research has documented an association between soil-transmitted helminth (STH) infections and child development. This has recently been identified as an important knowledge gap.
Methods
A longitudinal cohort study was conducted in Iquitos, Peru, between September 2011 and July 2016. A cohort of 880 children, recruited at 1 year of age, was followed up to 5 years. STH infection was measured annually and child development was measured with the Wechsler Preschool and Primary Scale of Intelligence III (WPPSI-III) at 5 years. Linear-regression models were used to investigate the effect of the number of detected STH infections between 1 and 5 years of age on WPPSI-III scores at 5 years of age. Bayesian latent class analysis was used to adjust for exposure misclassification.
Results
A total of 781 (88.8%) children were included in the analysis. In multivariable analysis, adjusted for STH misclassification, increasing numbers of Ascaris, Trichuris, hookworm and any STH infections were associated with lower WPPSI-III scores. Among the largest observed effects were those for the effect of Ascaris infection on verbal IQ scores [difference in IQ (95% CrI) for two, three, and four or five detected infections compared with zero or one infection: –8.27 (–13.85, –3.10), –6.69 (–12.05, –2.05) and –5.06 (–10.75, 0.05), respectively]. Misclassification of STH infection generally led to a bias towards the null.
Conclusions
These results document an association between STH infection and child development. The results highlight the importance of adjusting for STH misclassification; however, future research is needed to accurately determine the sensitivity of STH diagnostic techniques. STH control in preschool children may contribute to lowering the disease burden associated with poor child development.
Keywords: soil-transmitted helminth, child health, cohort study, epidemiology
Key Messages
This research documents a longitudinal association between STH infection and lower child-development scores.
This is the first longitudinal study conducted in preschool children specifically investigating the effect of STH infection on child development with appropriate adjustment for confounding variables.
This is the first study regarding STH infection and child development that has adjusted for bias due to STH misclassification, despite the fact that all previous research suffers from this bias.
This research makes a valuable contribution in terms of quantifying the developmental morbidity associated with STH infections and highlights the importance of accurate STH diagnostics.
These results can be used to motivate Ministries of Health in STH-endemic countries to prioritize STH control strategies, including mass deworming campaigns, in preschool children.
Introduction
The soil-transmitted helminths (STHs) (i.e. Ascaris lumbricoides, Trichuris trichiura and the two hookworm species, Ancylostoma duodenale and Necator americanus) are parasites that live in the human gut. A total of 103 countries around the world are endemic for STH infections1 and approximately 2 billion people are at risk of infection.2 Several microscopic techniques are available for diagnosing STH infections from stool specimens; however, no gold standard exists and all techniques are limited by imperfect sensitivities.3,4
It has been proposed that STH infections adversely affect child development primarily due to mediating factors including malnutrition and anemia.5 Because brain plasticity is greatest during the first few years of life, perturbations during this critical time of development could have long-term effects on brain development.6 It is therefore likely that the effect of STH infection on child development is more pronounced in preschool children compared with older children.7 Several observational studies have documented associations between STH infection and child development.8–20 The quality of this body of evidence, however, is limited by poor study designs,8–10,12–19 failure to adjust for critical confounding variables,8–11,19,20 small sample sizes10,15,18,20 and inappropriate statistical analyses.10,11,14,20 Most research has been done in school-aged children despite the fact that preschool children are more likely to be affected. No past research has adjusted for STH misclassification due to imperfect sensitivities of the diagnostic techniques used. The need for research to clarify the effects that STH infections may have on child development has recently been emphasized by both the STH and child-development scientific communities.5,21
The objective of the current research, therefore, was to determine the effect of the number of times a child was found STH-infected between 1 and 5 years of age on total IQ scores, verbal IQ scores and performance IQ scores at 5 years of age, adjusting for bias due to STH misclassification.
Methods
The original data source for this study was a parent randomized–controlled trial (RCT) conducted in Iquitos, Peru, between September 2011 and June 2013. This study has been described in detail elsewhere.22 Briefly, a population-based sample of 1760 children between 12 and 14 months of age were recruited and randomized to one of four deworming strategies [(i) deworming with mebendazole at 12 months of age and placebo at 18 months of age; (ii) deworming with mebendazole at 12 and 18 months of age; (iii) placebo at 12 months of age and deworming with mebendazole at 18 months of age; and (iv) placebo at 12 and 18 months of age]. These children were followed up at 18 and 24 months of age. Children were included in the trial regardless of their STH-infection status. The primary objective was to determine the effect of the timing and frequency of deworming during the second year of life on infant weight gain between 1 and 2 years of age.22 A secondary outcome was child development at 2 years of age.23 The RCT did not find a consistent effect of deworming compared with placebo on either weight gain or cognition at 2 years of age, and this was hypothesized to be due to the short follow-up period (i.e. only 1 year) and the relatively lower-than-expected baseline prevalence of STH infections.22,23 Following completion of the RCT, follow-up of the same children continued on an annual basis to 5 years of age. The current study uses data from the original RCT and the follow-up (i.e. from the 1-, 2-, 3-, 4- and 5-year time points).
The current study is a longitudinal cohort study. Data collection took place in the rural and peri-urban communities surrounding the city of Iquitos in the Peruvian Amazon. Inclusion and exclusion criteria were specified in the parent RCT.22 At each annual visit, a questionnaire was administered to the child’s primary caregiver; the child’s height and weight were measured; the child’s cognitive development was assessed; and a stool specimen was obtained.
At the 2- to 5-year visits, all stool specimens were analysed using the Kato-Katz technique within 24 hours of collection. Whereas this diagnostic test has near perfect specificity, a recent meta-analysis found the following sensitivity values from one stool specimen for Ascaris, Trichuris and hookworm, respectively: 63.8% (95% Credible Interval (CrI): 59.1–68.6%), 82.2% (95% CrI: 80.1–84.5%) and 59.5 (95% CrI: 56.9–62.2%).3 All children were treated with mebendazole at the 2-year visit and any child found infected at subsequent visits was referred for treatment.
Stool specimens collected at recruitment (when treatment allocation for the parent trial took place) required special processing because ethical guidelines required any individual found STH-infected to be treated. Due to sufficient clinical equipoise regarding the trial research question, it was deemed acceptable to collect stool specimens from all children participating in the RCT and only immediately analysing those specimens from children who were randomized to receive deworming using the Kato-Katz technique (this ensured that those found positive would be treated). Stool specimens from children randomized to receive placebo were stored in 10% formalin until they were analysed using the direct smear technique, following the trial end date (i.e. when all children were treated). (Note that it is not possible to analyse preserved stool specimens with the Kato-Katz technique.) Recent sensitivity estimates of the direct smear technique for diagnosis of Ascaris, Trichuris and hookworm infection are 52.1% (95% CrI: 46.6–57.7%), 62.8% (95% CrI: 56.9–68.9%) and 42.8% (95% CrI: 38.3–48.4%), respectively.3
Because no single high-quality scale of child development exists for both 1- and 5-year-old children, two separate scales were used to measure child development in this study. The Bayley Scales of Infant and Toddler Development, Third Edition (Bayley-III) was used up to 3 years of age and the Wechsler Preschool and Primary Scale of Intelligence, Third Edition (WPPSI-III) was used at 4 and 5 years. These two scales are widely used internationally.24 Both scales were administered by highly trained research assistants in a secluded area to avoid distractions. All research assistants were nurses or nurse-midwives with a minimum bachelor’s degree education. Research assistants were blinded to group assignment during the trial and were unaware of the current STH-infection status during follow-up visits. The Bayley-III was administered to all 1760 participants at 1 year of age. For feasibility reasons, at the 3-, 4- and 5-year visits, child development was measured in a random sample of 880 children.
Ethics
The study was approved by the Universidad Peruana Cayetano Heredia in Lima, Peru; the Instituto Nacional de Salud in Lima, Peru; and the Research Ethics Boards of the McGill University Health Centre in Montreal, Canada. Informed consent was obtained from parents/guardians of the participating children. Assent was obtained for any parent under 18 years, with informed consent requested from their parent or guardian over 18 years.
Statistical analyses
Double data entry was performed and data cleaning followed a comparison of the two databases. Summary statistics were generated to describe the study population at baseline.
Linear-regression models were used to investigate the effect of cumulative STH infections on child development. Cumulative STH infection was defined as the number of times a child was found infected between 1 and 5 years of age and was categorized as: never infected, infected once, infected twice, infected three times, infected four times and infected five times. Categories were combined, as necessary, in the case of sparse data. The effect of infection with any of the three STH infections (any STH infection) and with species-specific infections on total IQ score, verbal IQ score and performance IQ score at 5 years of age was estimated. IQ scores were generated by converting WPPSI-III raw scores to age-scaled scores and converting age-scaled scores to composite scores according to the scoring instructions and conversion tables (using a Mexican reference population) included in the WPPSI-III manual.25 The covariates included in the multivariable models were chosen based on theoretical knowledge (variables that are thought to be associated with both the exposure and outcome of interest without being mediators of this relationship) and statistical criteria. Variables that were considered during model selection are listed in the Supplementary Material, available as Supplementary data at IJE online. Univariable regression models were used to identify variables that were associated with the outcome and exposure. The final multivariable models included: socio-economic status (i.e. maternal education, using gas for cooking and having a toilet connected to public sewage in the home), baseline nutritional status (i.e. stunting), use of health care (i.e. number of routine growth and development visits attended at baseline), baseline development scores (i.e. Bayley-III cognitive raw scores) and number of years in preschool. Missing exposure data were imputed using multiple imputation (details described in the Supplementary Material, available as Supplementary data at IJE online).
Bayesian latent class linear-regression models were used to estimate the exposure effects while adjusting for misclassification of the exposure due to imperfect sensitivity and specificity of the STH diagnostic techniques. This methodology has been fully described previously.26 A brief description is included in the Supplementary Material, available as Supplementary data at IJE online. Diffuse, non-informative priors were used for all regression coefficients. Informative priors were specified for the sensitivity and specificity values of the two diagnostic tests (Table 1). Mean priors, as well as optimistic and pessimistic priors, were specified for comparison purposes and were assumed to follow a beta distribution. For comparison purposes, analyses were also run assuming that the sensitivity and specificity values were 100%. The prior ranges for the sensitivities and specificities of the direct smear and Kato-Katz techniques were developed based on previous research and expert opinion.3
Table 1.
Probability ranges and coefficients of the beta prior densities for the sensitivities and specificities of the Kato-Katz and direct smear techniques used in the Bayesian latent class analyses to adjust for misclassification of STH infection
| Mean priors |
Optimistic priors |
Pessimistic priors |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Range | Beta distribution coefficients |
Range | Beta distribution coefficients |
Range | Beta distribution coefficients |
|||||
| α | β | α | β | α | β | |||||
| Kato-Katz | Ascaris: | |||||||||
| Sensitivity | 0.55–0.75 | 55.86 | 29.63 | 0.70–0.80 | 214.34 | 70.81 | 0.50–0.60 | 208.45 | 170.38 | |
| Specificity | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | |
| Trichuris: | ||||||||||
| Sensitivity | 0.75–0.90 | 77.85 | 15.75 | 0.85–0.95 | 116.06 | 12.05 | 0.70–0.80 | 214.34 | 70.81 | |
| Specificity | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | |
| Hookworm: | ||||||||||
| Sensitivity | 0.52–0.68 | 85.65 | 56.78 | 0.63–0.73 | 226.28 | 105.98 | 0.47–0.57 | 198.73 | 183.37 | |
| Specificity | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | |
| Direct smear | Ascaris: | |||||||||
| Sensitivity | 0.40–0.60 | 47.30 | 47.30 | 0.55–0.65 | 220.49 | 146.68 | 0.35–0.45 | 146.68 | 220.49 | |
| Specificity | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | |
| Trichuris: | ||||||||||
| Sensitivity | 0.55–0.75 | 55.86 | 29.63 | 0.70–0.80 | 214.34 | 70.81 | 0.50–0.60 | 208.45 | 170.38 | |
| Specificity | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | |
| Hookworm: | ||||||||||
| Sensitivity | 0.35–0.55 | 42.02 | 51.57 | 0.50–0.60 | 208.45 | 170.38 | 0.30–0.40 | 121.41 | 226.29 | |
| Specificity | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | 0.95–0.99 | 231.95 | 6.26 | |
Sample size
A total of 880 of the original 1760 children were randomly sampled for this study. A difference in the mean IQ score of five points was considered the minimum clinically significant effect size. Assuming that the standard deviation of the outcome in all exposure groups would be 15,24 and assuming that approximately 20% of the population is unexposed (never STH-infected) and that 20, 25, 25 and 10% of the population would have been found STH-infected one, two, three, and four or five times, respectively (based on preliminary data), a sample size of 880 is able to detect a difference of five points between each infection category and the never-infected category, with a total 95% confidence interval width of 6.28, 5.95, 5.95 and 7.68 points for one, two, three, and four or five times found infected, respectively.
Statistical analyses were performed in Stata, version 13.1 and WinBUGS version 1.4.3.
Results
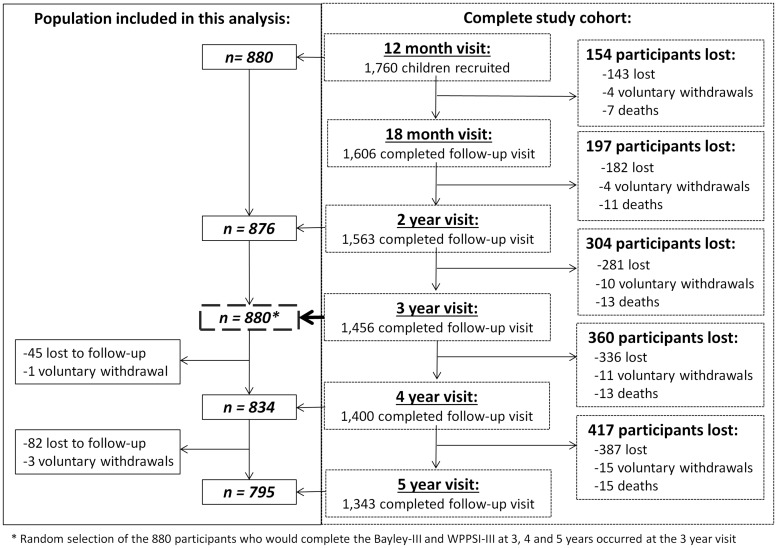
The study flowchart is presented in Figure 1. Of the 880 children, 795 (90.3%) completed the 5-year visit and 781 (88.8%) had valid WPPSI-III measurements and were included in this analysis. (WPPSI-III scores are considered invalid if a participant scores zero on two or more of the verbal or performance subtests.) Most children lost to follow-up moved outside the study area. The exposure variable—cumulative STH infection—was missing for 11 children. Of all stool specimens analysed throughout the study, 10.1% were analysed using the direct smear technique and 89.9% were analysed using the Kato-Katz technique.
Figure 1.
Study flowchart showing the entire study population from the parent study (N = 1760) and the random sample included in this analysis (n = 880).
Baseline characteristics of the trial and cohort populations were similar (Table 2). STH-infection prevalence increased from 12.4% at 1 year of age to 50.8% at 5 years of age (Table 3). Hookworm infection was relatively uncommon, with a prevalence of 0.34% at baseline and 4.7% at 5 years. Table 4 shows the frequencies of any STH and species-specific infection at each time point. At 5 years of age, WPPSI-III scores in this population were low. The mean (± sd) total IQ, verbal IQ and performance IQ scores were 77.1 (± 10.8), 77.0 (± 11.8) and 81.1 (± 11.9), respectively. At 5 years of age, the proportion of children considered to have below-average development was 87.8% and the proportion of children considered to have extremely low development was 20.6%.
Table 2.
Baseline characteristics of the entire study population (N = 1760) at 12 months of age and of the 880 children randomly selected for the cohort study, Iquitos, Peru (between September 2011 and July 2016)
| Random sample [Mean or % (SD or n)] | Entire cohort [Mean or % (SD or n)] | |
|---|---|---|
| N | 880 | 1760 |
| Child characteristics | ||
| Sex (males) [%, n] | 51.9 (457) | 52.3 (920) |
| Age (months) [mean, sd] | 12.1 (0.28) | 12.1 (0.30) |
| Birthweight (kg) [mean, sd] | 3.13 (0.48)a | 3.14 (0.47)b |
| Number of routine healthy growth visits attended between birth and 1 year of age [mean, sd] | 7.6 (3.5) | 7.6 (3.5) |
| Vaccinations up to date at 11 months of age [%, n]c | 74.3 (652)d | 73.8 (1296)e |
| Taking iron supplementation [%, n] | 35.7 (313)f | 33.1 (583)g |
| Ever received deworming [%, n] | 0.0 (0)h | 0.0 (0)i |
| Hospitalized in the past [%, n] | 9.6 (84) | 9.3 (164) |
| Walks without support [%, n] | 24.6 (216) | 24.6 (433)j |
| Stunted [%, n] | 24.0 (211) | 24.2 (425) |
| Underweight [%, n] | 7.5 (66) | 8.6 (151) |
| Wasted [%, n] | 1.7 (15) | 2.3 (40) |
| Bayley-IIIl Cognition raw score [mean, sd] | 42.6 (3.0) | 42.5 (3.0) |
| Bayley-IIIl Receptive language raw score [mean, sd] | 13.0 (1.6) | 12.9 (1.6) |
| Bayley-IIIl Expressive language raw score [mean, sd] | 13.6 (2.2) | 13.5 (2.1) |
| Bayley-IIIl Fine motor raw score [mean, sd] | 29.2 (1.5) | 29.2 (1.5) |
| Maternal characteristics | ||
| Maternal age (years) [mean, sd] | 27.1 (7.1) | 26.5 (7.1) |
| Married or common-law [%, n] | 81.9 (721) | 80.9 (1423) |
| Maternal education | ||
| Completed primary education [%, n] | 85.7 (754) | 85.9 (1511) |
| Completed secondary education [%, n] | 32.5 (286) | 31.1 (547) |
| Mother is employed [%, n] | 18.7 (164)j | 17.5 (307)d |
| Household characteristics | ||
| Number of persons living in the home [mean, sd] | 6.6 (2.7) | 6.6 (2.7) |
| Wood/earth house material [%, n] | 75.7 (666) | 76.9 (1354) |
| Cooking method | ||
| Gas [%, n] | 31.4 (276) | 31.5 (555) |
| Charcoal [%, n] | 28.1 (247) | 26.6 (468) |
| Firewood [%, n] | 40.1 (353) | 41.5 (730) |
| Other [%, n] | 0.5 (4) | 0.4 (7) |
| Electric energy in the home [%, n] | 91.0 (801) | 90.7 (1596) |
| Owns a working radio [%, n] | 53.2 (468) | 51.0 (897) |
| Owns a working television [%, n] | 75.0 (660) | 74.2 (1305) |
| Presence of running water in the home [%, n] | 51.3 (451) | 51.0 (898) |
| Type of toilet in the home | ||
| Latrine or pit without drainage [%, n] | 42.3 (372) | 41.6 (732) |
| Toilet with water and connection to public sewage [%, n] | 43.6 (384) | 42.9 (755) |
| Latrine or silo with drainage [%, n] | 10.0 (88) | 11.5 (203) |
| Other [%, n]k | 4.1 (36) | 4.0 (70) |
aMissing data for 79 participants.
bMissing data for 166 participants.
cUp-to-date vaccinations includes having received all of the following vaccines: one dose of Bacille Calmette-Guérin (BCG), one dose of hepatitis B, three doses of polio, three doses of pentavalent, two doses of rotavirus and two doses of pneumococcal.
dMissing data for two participants.
eMissing data for three participants.
fMissing data for four participants (respondent did not know).
gMissing data for five participants (respondent did not know).
hMissing data for 15 participants (respondent did not know).
iMissing data for 20 participants (respondent did not know).
jMissing data for one participant.
kOther includes: Directly in river, Open-air, Septic tank, Other.
lBayley-III: Bayley Scales of Infant and Toddler Development, Third Edition.
Table 3.
STH prevalence and intensity at each study time point, in preschool children in Iquitos, Peru, September 2011 to July 2016
| 1 yeara | 2 yearsb | 3 yearsb | 4 yearsb | 5 yearsb | |
|---|---|---|---|---|---|
| Ascaris | |||||
| Prevalence [% (n)] | 11.0 (97)c | 30.7 (269)e | 30.6 (269)c | 28.3 (236)f | 28.2 (224)g |
| Intensity (epgh) [mean (sd)] | 329.9 (1416.6)d | 2304.2 (11 987.5)e | 2009.9 (8566.4)c | 3468.4 (12 923.5)f | 6157.3 (23 596.1)g |
| Prevalence of moderate/heavy-intensity infection [% (n)] | 2.0 (9)d | 9.6 (84)e | 8.1 (71)c | 13.3 (111)f | 16.6 (132)g |
| Trichuris | |||||
| Prevalence [% (n)] | 2.5 (22)c | 21.8 (191)e | 26.5 (233)c | 34.4 (286)f | 38.6 (307)g |
| Intensity (epgh) [mean (sd)] | 26.5 (261.3)d | 46.7 (225.5)e | 66.4 (265.2)c | 171.5 (1214.6)f | 340.3 (1293.1)g |
| Prevalence of moderate/heavy-intensity infection [% (n)] | 0.7 (3)d | 0.7 (6)e | 1.3 (11)c | 2.8 (23)f | 7.8 (62)g |
| Hookworm | |||||
| Prevalence [% (n)] | 0.34 (3)c | 1.37 (12)e | 1.7 (15)c | 2.8 (23)f | 4.7 (37)g |
| Intensity (epgh) [mean (sd)] | 1.7 (26.8)d | 1.4 (17.6)e | 1.25 (13.3)c | 7.9 (72.3)f | 9.8 (66.9)g |
| Prevalence of moderate/heavy-intensity infection [% (n)] | 0 (0)d | 0 (0)e | 0 (0)c | 0 (0)f | 0 (0)g |
| Any STH | |||||
| Prevalence [% (n)] | 12.4 (109)c | 41.1 (360)e | 42.7 (376)c | 48.1 (401)f | 50.8 (404)g |
aAt the 1 year of age visit, 449 (51%) stool specimens were analysed using the Kato-Katz technique and 431 (49%) stool specimens were analysed using the direct smear technique.
bAt the 2–5 years of age visits, all available stool specimens were analysed using the Kato-Katz technique.
cData available for all 880 participants.
dData available for 449 participants (who had their stool specimen analysed with the Kato-Katz technique).
eData available for 876 participants.
fData available for 833 participants.
gData available for 795 participants.
hEggs per gram of stool.
Table 4.
Frequency of detected STH infections between 1 and 5 years of age for the 784 participants with complete STH data included in this analysis, Iquitos, Peru, September 2011 to July 2016
| Ascaris | Trichuris | Hookworm | Any STH | |
|---|---|---|---|---|
| No detected infections [% (n)] | 31.4 (246) | 40.6 (318) | 91.5 (717) | 19.9 (156) |
| One detected infection [% (n)] | 31.1 (244) | 22.5 (176) | 6.9 (54) | 21.7 (170) |
| Two detected infections [% (n)] | 20.0 (157) | 16.6 (130) | 1.0 (8) | 21.9 (172) |
| Three detected infections [% (n)] | 12.2 (96) | 12.4 (97) | 0.6 (5) | 18.8 (147) |
| Four detected infections [% (n)] | 4.2 (33) | 7.3 (57) | 0.0 (0) | 13.7 (107) |
| Five detected infections [% (n)] | 1.0 (8) | 0.8 (6) | 0.0 (0) | 4.1 (32) |
In univariable analyses, children with increasing numbers of detected STH infections had lower total IQ scores (Table 5), verbal IQ scores (Table 6) and performance IQ scores (Table 7). In multivariable analyses, effects were attenuated (Tables 5–7). The largest effect sizes were observed in the associations of any STH infection with verbal IQ scores. Compared with children who were never found infected with any STH infection, the adjusted difference [β (95% confidence interval (CI)] in verbal IQ scores was: –1.64 (–4.00, 0.72) for children found infected one time; –3.31 (–5.71, –0.90) for children found infected twice, –4.22 (–6.77, –1.68) for children found infected three times; and –2.57 (–5.24, 0.10) for children found infected four or five times. The effects for hookworm infection on IQ scores were inconclusive (Tables 5–7).
Table 5.
Univariable and multivariable linear-regression results for the effect of cumulative Ascaris infection, cumulative Trichuris infection, cumulative hookworm infection and cumulative any STH infection on total IQ score, in preschool children in Iquitos, Peru, September 2011 to July 2016
| Univariablea | Multivariable with multiple imputationb | |
|---|---|---|
| β (95% CI) | β (95% CI) | |
| # times found infected with Ascaris: | ||
| 0 | REF | REF |
| 1 | –3.56 (–5.44, –1.69) | –1.45 (–3.19, 0.30) |
| 2 | –5.78 (–7.90, –3.66) | –2.50 (–4.50, –0.51) |
| 3 | –6.81 (–9.30, –4.32) | –3.05 (–5.40. –0.70) |
| 4–5 | –6.22 (–9.69, –2.75) | –0.89 (–4.13, 2.36) |
| Mother completed secondary education | 7.95 (6.44, 9.47) | 4.81 (3.24, 6.38) |
| Cooking method: gas | 6.03 (4.46, 7.60) | 2.22 (0.64, 3.80) |
| Toilet in the home | 5.81 (4.34, 7.29) | 2.43 (0.92, 3.94) |
| Stunted at 1 year | –4.29 (–6.03, –2.56) | –2.48 (–4.09, –0.88) |
| Bayley-IIIc cognitive score at 1 year | 0.55 (0.31, 0.80) | 0.28 (0.05, 0.51) |
| # healthy growth visits from birth to 1 year of age | 0.58 (0.37, 0.79) | 0.23 (0.04, 0.43) |
| # years in preschool | 4.05 (2.93, 5.17) | 2.14 (1.05, 3.23) |
| # times found infected with Trichuris: | ||
| 0 | REF | REF |
| 1 | –3.35 (–5.29, –1.41) | –1.40 (–3.20, 0.41) |
| 2 | –4.88 (–7.04, –2.71) | –2.08 (–4.13, –0.03) |
| 3 | –7.45 (–9.83, –5.07) | –3.19 (–5.48, –0.90) |
| 4–5 | –6.15 (–8.98, –3.33) | –1.62 (–4.34, 1.10) |
| Mother completed secondary education | 7.95 (6.44, 9.47) | 4.79 (3.23, 6.35) |
| Cooking method: gas | 6.03 (4.46, 7.60) | 2.27 (0.69, 3.86) |
| Toilet in the home | 5.81 (4.34, 7.29) | 2.19 (0.65, 3.73) |
| Stunted at 1 year | –4.29 (–6.03, –2.56) | –2.46 (–4.08, –0.85) |
| Bayley-IIIc cognitive score at 1 year | 0.55 (0.31, 0.80) | 0.29 (0.06, 0.52) |
| # healthy growth visits from birth to 1 year of age | 0.58 (0.37, 0.79) | 0.23 (0.03, 0.43) |
| # years in preschool | 4.05 (2.93, 5.17) | 2.06 (0.98, 3.14) |
| # times found infected with hookworm: | ||
| 0 | REF | REF |
| 1–3 | –3.49 (–6.20, –0.78) | –1.92 (–4.35, 0.51) |
| Mother completed secondary education | 7.95 (6.44, 9.47) | 5.03 (3.47, 6.58) |
| Cooking method: gas | 6.03 (4.46, 7.60) | 2.34 (0.76, 3.93) |
| Toilet in the home | 5.81 (4.34, 7.29) | 2.80 (1.30, 4.30) |
| Stunted at 1 year | –4.29 (–6.03, –2.56) | –2.59 (–4.19, –0.98) |
| Bayley-IIIc cognitive score at 1 year | 0.55 (0.31, 0.80) | 0.28 (0.05, 0.51) |
| # healthy growth visits from birth to 1 year of age | 0.58 (0.37, 0.79) | 0.25 (0.06, 0.45) |
| # years in preschool | 4.05 (2.93, 5.17) | 2.09 (1.01, 3.18) |
| # times found infected with any STH: | ||
| 0 | REF | REF |
| 1 | –2.26 (–4.54, 0.03) | –0.83 (–2.95, 1.28) |
| 2 | –5.39 (–7.68, –3.10) | –2.48 (–4.62, –0.33) |
| 3 | –7.11 (–9.49, –4.73) | –3.14 (–5.41, –0.86) |
| 4–5 | –7.23 (–9.66, –4.86) | –1.85 (–4.24, 0.54) |
| Mother completed secondary education | 7.95 (6.44, 9.47) | 4.75 (3.18, 6.32) |
| Cooking method: gas | 6.03 (4.46, 7.60) | 2.26 (0.68, 3.85) |
| Toilet in the home | 5.81 (4.34, 7.29) | 2.35 (0.82, 3.88) |
| Stunted at 1 year | –4.29 (–6.03, –2.56) | –2.45 (–4.06, –0.84) |
| Bayley-IIIc cognitive score at 1 year | 0.55 (0.31, 0.80) | 0.28 (0.05, 0.50) |
| # healthy growth visits from birth to 1 year of age | 0.58 (0.37, 0.79) | 0.24 (0.04, 0.44) |
| # years in preschool | 4.05 (2.93, 5.17) | 2.10 (1.02, 3.18) |
aComplete data available for 770 participants.
b781 participants were included in the analyses (complete data were available for 770 participants and number of times found infected with any STH infection and species-specific infections was imputed for 11 participants with missing data).
cBayley III: Bayley Scales of Infant and Toddler Development Third Edition.
Table 6.
Univariable and multivariable linear-regression results for the effect of cumulative Ascaris infection, cumulative Trichuris infection, cumulative hookworm infection and cumulative any STH infection on verbal IQ score, in preschool children in Iquitos, Peru, September 2011 to July 2016
| Univariablea | Multivariable with multiple imputationb | |
|---|---|---|
| β (95% CI) | β (95% CI) | |
| # times found infected with Ascaris | ||
| 0 | REF | REF |
| 1 | –5.30 (–7.36, –3.24) | –3.20 (–5.15, –1.25) |
| 2 | –6.50 (–8.83, –4.17) | –3.21 (–5.46, –0.97) |
| 3 | –7.17 (–9.91, –4.44) | –3.40 (–6.01, –0.78) |
| 4–5 | –6.14 (–9.96, –2.33) | –0.84 (–4.47, 2.78) |
| Mother completed secondary education | 7.67 (5.98, 9.36) | 4.29 (2.53, 6.04) |
| Cooking method: gas | 6.28 (4.55, 8.00) | 2.57 (0.80, 4.34) |
| Toilet in the home | 5.78 (4.15, 7.41) | 2.26 (0.58, 3.95) |
| Stunted at 1 year | –4.69 (–6.60, –2.79) | –2.79 (–4.58, –0.99) |
| Bayley-IIIc cognitive score at 1 year | 0.67 (0.40, 0.94) | 0.40 (0.15, 0.65) |
| # healthy growth visits from birth to 1 year of age | 0.57 (0.34, 0.80) | 0.24 (0.02, 0.46) |
| # years in preschool | 3.67 (2.43, 4.91) | 1.81 (0.59, 3.03) |
| # times found infected with Trichuris: | ||
| 0 | REF | REF |
| 1 | –3.08 (–5.23, –0.94) | –1.18 (–3.21, 0.84) |
| 2 | –4.69 (–7.09, –2.30) | –1.99 (–4.30, 0.32) |
| 3 | –7.44 (–10.07, –4.81) | –3.35 (–5.94, –0.75) |
| 4–5 | –6.69 (–9.81, –3.57) | –2.19 (–5.24, 0.87) |
| Mother completed secondary education | 7.67 (5.98, 9.36) | 4.40 (2.64, 6.15) |
| Cooking method: gas | 6.28 (4.55, 8.00) | 2.61 (0.83, 4.39) |
| Toilet in the home | 5.78 (4.15, 7.41) | 2.06 (0.32, 3.79) |
| Stunted at 1 year | –4.69 (–6.60, –2.79) | –2.76 (–4.58, –0.94) |
| Bayley-IIIc cognitive score at 1 year | 0.67 (0.40, 0.94) | 0.41 (0.16, 0.67) |
| # healthy growth visits from birth to 1 year of age | 0.57 (0.34, 0.80) | 0.24 (0.01, 0.46) |
| # years in preschool | 3.67 (2.43, 4.91) | 1.65 (0.44, 2.87) |
| # times found infected with hookworm: | ||
| 0 | REF | REF |
| 1–3 | –3.18 (–6.16, –0.20) | –1.37 (–4.11, 1.37) |
| Mother completed secondary education | 7.67 (5.98, 9.36) | 4.64 (2.89, 6.39) |
| Cooking method: gas | 6.28 (4.55, 8.00) | 2.75 (0.97, 4.53) |
| Toilet in the home | 5.78 (4.15, 7.41) | 2.69 (1.01, 4.38) |
| Stunted at 1 year | –4.69 (–6.60, –2.79) | –2.92 (–4.73, –1.12) |
| Bayley-IIIc cognitive score at 1 year | 0.67 (0.40, 0.94) | 0.40 (0.15, 0.66) |
| # healthy growth visits from birth to 1 year of age | 0.57 (0.34, 0.80) | 0.26 (0.04, 0.48) |
| # years in preschool | 3.67 (2.43, 4.91) | 1.72 (0.50, 2.94) |
| # times found infected with any STH: | ||
| 0 | REF | REF |
| 1 | –2.96 (–5.48, –0.45) | –1.64 (–4.00, 0.72) |
| 2 | –6.13 (–8.65, –3.61) | –3.31 (–5.71, –0.90) |
| 3 | –7.99 (–10.61, –5.38) | –4.22 (–6.77, –1.68) |
| 4–5 | –7.81 (–10.45, –5.16) | –2.57 (–5.24, 0.10) |
| Mother completed secondary education | 7.67 (5.98, 9.36) | 4.26 (2.50, 6.01) |
| Cooking method: gas | 6.28 (4.55, 8.00) | 2.59 (0.82, 4.37) |
| Toilet in the home | 5.78 (4.15, 7.41) | 2.17 (0.46, 3.89) |
| Stunted at 1 year | –4.69 (–6.60, –2.79) | –2.72 (–4.52, –0.92) |
| Bayley-IIIc cognitive score at 1 year | 0.67 (0.40, 0.94) | 0.40 (0.14, 0.65) |
| # healthy growth visits from birth to 1 year of age | 0.57 (0.34, 0.80) | 0.24 (0.02, 0.46) |
| # years in preschool | 3.67 (2.43, 4.91) | 1.65 (0.44, 2.86) |
aComplete data available for 770 participants.
b781 participants were included in the analyses (complete data were available for 770 participants and number of times found infected with any STH infection and species-specific infections was imputed for 11 participants with missing data).
cBayley III: Bayley Scales of Infant and Toddler Development Third Edition.
Table 7.
Univariable and multivariable linear-regression results for the effect of cumulative Ascaris infection, cumulative Trichuris infection, cumulative hookworm infection and cumulative any STH infection on performance IQ score, in preschool children in Iquitos, Peru, September 2011 to July 2016
| Univariablea | Multivariable with multiple imputationb | |
|---|---|---|
| β (95% CI) | β (95% CI) | |
| # times found infected with Ascaris: | ||
| 0 | REF | REF |
| 1 | –2.35 (–4.43, –0.27) | –0.18 (–2.17, 1.80) |
| 2 | –5.56 (–7.91, –3.20) | –2.29 (–4.58, –0.003) |
| 3 | –6.09 (–8.86, –3.33) | –2.53 (–5.21, 0.14) |
| 4–5 | –6.08 (–9.93, –2.23) | –1.18 (–4.98, 2.61) |
| Mother completed secondary education | 8.10 (6.41, 9.79) | 5.27 (3.49, 7.06) |
| Cooking method: gas | 5.72 (3.97, 7.46) | 1.93 (0.13, 3.73) |
| Toilet in the home | 5.93 (4.29, 7.56) | 2.74 (1.02, 4.45) |
| Stunted at 1 year | –3.36 (–5.29, –1.43) | –1.66 (–3.49, 0.17) |
| Bayley-IIIc cognitive score at 1 year | 0.43 (0.16, 0.71) | 0.16 (–0.09, 0.42) |
| # healthy growth visits from birth to 1 year of age | 0.59 (0.36, 0.82) | 0.26 (0.03, 0.48) |
| # years in preschool | 3.80 (2.55, 5.05) | 1.82 (0.58, 3.06) |
| # times found infected with Trichuris: | ||
| 0 | REF | REF |
| 1 | –3.93 (–6.09, –1.78) | –1.92 (–3.98, 0.14) |
| 2 | –5.12 (–7.52, –2.71) | –2.46 (–4.80, –0.12) |
| 3 | –6.89 (–9.52, –4.25) | –2.78 (–5.38, –0.17) |
| 4–5 | –5.30 (–8.43, –2.17) | –0.77 (–3.89, 2.35) |
| Mother completed secondary education | 8.10 (6.41, 9.79) | 5.19 (3.41, 6.97) |
| Cooking method: gas | 5.72 (3.97, 7.46) | 2.03 (0.23, 3.84) |
| Toilet in the home | 5.93 (4.29, 7.56) | 2.51 (0.76, 4.26) |
| Stunted at 1 year | –3.36 (–5.29, –1.43) | –1.64 (–3.48, 0.20) |
| Bayley-IIIc cognitive score at 1 year | 0.43 (0.16, 0.71) | 0.17 (–0.08, 0.43) |
| # healthy growth visits from birth to 1 year of age | 0.59 (0.36, 0.82) | 0.26 (0.04, 0.49) |
| # years in preschool | 3.80 (2.55, 5.05) | 1.78 (0.55, 3.01) |
| # times found infected with hookworm: | ||
| 0 | REF | REF |
| 1–3 | –3.35 (–6.33, –0.37) | –2.27 (–5.05, 0.50) |
| Mother completed secondary education | 8.10 (6.41, 9.79) | 5.42 (3.65, 7.19) |
| Cooking method: gas | 5.72 (3.97, 7.46) | 2.03 (0.23, 3.82) |
| Toilet in the home | 5.93 (4.29, 7.56) | 3.07 (1.36, 4.77) |
| Stunted at 1 year | –3.36 (–5.29, –1.43) | –1.72 (–3.55, 0.11) |
| Bayley-IIIc cognitive score at 1 year | 0.43 (0.16, 0.71) | 0.17 (–0.09, 0.43) |
| # healthy growth visits from birth to 1 year of age | 0.59 (0.36, 0.82) | 0.28 (0.05, 0.50) |
| # years in preschool | 3.80 (2.55, 5.05) | 1.80 (0.57, 3.04) |
| # times found infected with any STH: | ||
| 0 | REF | REF |
| 1 | –2.01 (–4.55, 0.53) | –0.58 (–3.00, 1.84) |
| 2 | –5.48 (–8.02, –2.93) | –2.71 (–5.17, –0.25) |
| 3 | –6.26 (–8.90, –3.62) | –2.37 (–4.97, 0.24) |
| 4–5 | –6.63 (–9.30, –3.96) | –1.28 (–4.01, 1.45) |
| Mother completed secondary education | 8.10 (6.41, 9.79) | 5.20 (3.41, 6.99) |
| Cooking method: gas | 5.72 (3.97, 7.46) | 2.01 (0.21, 3.82) |
| Toilet in the home | 5.93 (4.29, 7.56) | 2.68 (0.93, 4.42) |
| Stunted at 1 year | –3.36 (–5.29, –1.43) | –1.62 (–3.45, 0.22) |
| Bayley-IIIc cognitive score at 1 year | 0.43 (0.16, 0.71) | 0.16 (–0.10, 0.42) |
| # healthy growth visits from birth to 1 year of age | 0.59 (0.36, 0.82) | 0.27 (0.05, 0.50) |
| # years in preschool | 3.80 (2.55, 5.05) | 1.88 (0.65, 3.11) |
aComplete data available for 770 participants.
b781 participants were included in the analyses (complete data were available for 770 participants and number of times found infected with any STH infection and species-specific infections was imputed for 11 participants with missing data).
cBayley III: Bayley Scales of Infant and Toddler Development Third Edition.
Results from the Bayesian latent class analyses adjusted for misclassification of STH infection and confounding are presented in Table 8. For all species and for any STH infection, the misclassification-adjusted results shift away from the null, suggesting that misclassification led to bias towards the null. Infection by all STH species was found to lead to lower development scores. In the analyses using mean sensitivity and specificity priors (see Table 1), cumulative Ascaris, Trichuris, hookworm and any STH infection were associated with lower total IQ scores; cumulative Ascaris, Trichuris and any STH infection were associated with lower verbal IQ scores; and cumulative Ascaris, Trichuris and any STH infection were associated with lower performance IQ scores. The largest effects found were for effects of cumulative Ascaris infection on verbal IQ score [β (95% CrI) for two, three, and four or five detected infections compared with zero or one infections: –8.27 (–13.85, –3.10), –6.69 (–12.05, –2.05) and –5.06 (–10.75, 0.05), respectively] and for effects of any STH infection on verbal IQ score [β (95% CrI) for two, three, and four or five detected infections compared with zero or one infections: –9.42 (–15.46, –3.04), –8.58 (–13.75, –3.90) and –7.59 (–12.81, –2.75), respectively]. The misclassification-adjusted results using optimistic and pessimistic priors for the sensitivity of the Kato-Katz and direct smear techniques show how dependent the results are on these prior specifications. In general, assuming that the sensitivities of the diagnostic tests are poorer led to larger main effect sizes.
Table 8.
Results from Bayesian Latent Class models adjusting for misclassification due to imperfect sensitivity and specificity of the Kato-Katz and direct smear techniques for identifying STH infection, in preschool children (n = 781) in Iquitos, Peru, September 2011 to July 2016a
| Perfect sensitivity/ specificity β (95% CrI) | Mean priors for sensitivity/ specificity β (95% CrI) | Optimistic priors for sensitivity/ specificity β (95% CrI) | Pessimistic priors for sensitivity/ specificity β (95% CrI) | |
|---|---|---|---|---|
| 1) Outcome: Total IQ Score | ||||
| # times found infected with Ascaris: | ||||
| 0–1 | REF | REF | REF | REF |
| 2 | –1.83 (–3.58, –0.07) | –5.50 (–9.92, –1.32) | –3.68 (–6.57, –0.74) | –7.05 (–11.59, –1.84) |
| 3 | –2.26 (–4.38, –0.14) | –5.33 (–9.43, –1.75) | –3.46 (–6.36, –0.51) | –7.01 (–11.11, –3.10) |
| 4–5 | –0.07 (–3.13, 3.00) | –3.75 (–8.33, 0.39) | –1.35 (–4.95, 2.32) | –5.83 (–10.14, –1.64) |
| # times found infected with Trichuris: | ||||
| 0 | REF | REF | REF | REF |
| 1 | –1.36 (–3.14, 0.43) | –3.02 (–6.40, 0.36) | –2.39 (–5.02, 0.26) | –3.66 (–7.49, 0.52) |
| 2 | –2.10 (–4.11, –0.07) | –2.80 (–5.83, 0.16) | –2.26 (–4.87, 0.31) | –3.48 (–6.80, –0.17) |
| 3 | –3.18 (–5.44, –0.88) | –4.27 (–7.44, –1.08) | –3.96 (–6.81, –1.14) | –4.63 (–8.16, –1.09) |
| 4–5 | –1.60 (–4.28, 1.09) | –2.58 (–6.55, 1.31) | –1.70 (–5.48, 1.97) | –3.47 (–7.58, 0.57) |
| # times found infected with hookworm: | ||||
| 0 | REF | REF | REF | REF |
| 1–3 | –1.80 (–4.20, 0.60) | –3.70 (–7.28, –0.20) | –3.63 (–7.19, –0.12) | –3.76 (–7.27, –0.24) |
| # times found infected with any STH: | ||||
| 0–1 | REF | REF | REF | REF |
| 2 | –2.04 (–3.84, –0.24) | –4.04 (–10.74, 10.80) | –3.60 (–7.11, 0.05) | –0.41 (–12.90, 13.52) |
| 3 | –2.71 (–4.64, –0.78) | –6.19 (–10.60, –1.60) | –4.52 (–7.34, –1.72) | –6.24 (–12.65, –0.18) |
| 4–5 | –1.30 (–3.34, 0.73) | –4.63 (–9.61, 1.54) | –2.83 (–5.57, –0.06) | –4.32 (–11.83, 3.18) |
| 2) Outcome: Verbal IQ Score | ||||
| # times found infected with Ascaris: | ||||
| 0–1 | REF | REF | REF | REF |
| 2 | –1.55 (–3.52, 0.43) | –8.27 (–13.85, –3.10) | –4.27 (–7.47, –1.10) | −10.01 (–14.67, –4.92) |
| 3 | –1.63 (–4.02, 0.76) | –6.69 (–12.05, –2.05) | –3.03 (–6.24, 0.18) | –8.29 (–12.92, –3.92) |
| 4–5 | 0.87 (–2.57, 4.31) | –5.06 (–10.75, 0.05) | –0.89 (–4.88, 3.10) | –6.99 (–11.63, –2.47) |
| # times found infected with Trichuris: | ||||
| 0 | REF | REF | REF | REF |
| 1 | –1.13 (–3.13, 0.88) | –2.67 (–6.91, 1.32) | –2.00 (–5.03, 0.97) | –3.57 (–8.44, 1.55) |
| 2 | –1.86 (–4.12, 0.42) | –2.09 (–5.48, 1.23) | –1.78 (–4.68, 1.12) | –2.55 (–6.32, 1.17) |
| 3 | –3.19 (–5.74, –0.66) | –3.95 (–7.59, –0.36) | –3.63 (–6.82, –0.45) | –4.36 (–8.39, –0.27) |
| 4–5 | –1.96 (–4.96, 1.05) | –3.27 (–7.75, 1.01) | –2.54 (–6.69, 1.48) | –4.14 (–8.80, 0.42) |
| # times found infected with hookworm: | ||||
| 0 | REF | REF | REF | REF |
| 1–3 | –1.53 (–4.23, 1.18) | –3.43 (–7.55, 0.69) | –3.36 (–7.42, 0.71) | –3.59 (–7.76, 0.55) |
| # times found infected with any STH: | ||||
| 0–1 | REF | REF | REF | REF |
| 2 | –2.32 (–4.32, –0.31) | –9.42 (–15.46, –3.04) | –4.79 (–8.73, –0.75) | −11.84 (–17.18, –5.40) |
| 3 | –3.21 (–5.37, –1.06) | –8.58 (–13.75, –3.90) | –5.01 (–8.20, –1.88) | −10.63 (–15.68, –5.75) |
| 4–5 | –1.40 (–3.68, 0.90) | –7.59 (–12.81, –2.75) | –3.38 (–6.50, –0.31) | –9.96 (–14.55, –5.29) |
| 3) Outcome: Performance IQ Score | ||||
| # times found infected with Ascaris: | ||||
| 0–1 | REF | REF | REF | REF |
| 2 | –2.36 (–4.36, –0.35) | –0.95 (–9.79, 16.11) | –3.84 (–7.26, –0.31) | 3.03 (–11.67, 16.37) |
| 3 | –2.49 (–4.90, –0.07) | –4.86 (–9.42, –0.42) | –3.84 (–7.18, –0.43) | –5.17 (–11.07, –0.16) |
| 4–5 | –0.80 (–4.29, 2.69) | –2.37 (–7.94, 3.97) | –1.61 (–5.74, 2.64) | –2.07 (–9.77, 4.71) |
| # times found infected with Trichuris: | ||||
| 0 | REF | REF | REF | REF |
| 1 | –1.89 (–3.92, 0.15) | –4.03 (–8.05, –0.06) | –3.33 (–6.46, –0.28) | –4.53 (–9.08, 0.51) |
| 2 | –2.41 (–4.71, –0.08) | –3.85 (–7.57, –0.31) | –2.87 (–5.95, 0.16) | –4.77 (–8.75, –0.85) |
| 3 | –2.64 (–5.21, –0.06) | –4.34 (–8.18, –0.62) | –3.87 (–7.23, –0.57) | –4.76 (–8.88, –0.61) |
| 4–5 | –0.94 (–3.98, 2.09) | –1.69 (–6.21, 2.74) | –0.58 (–4.81, 3.66) | –2.55 (–7.19, 2.04) |
| # times found infected with hookworm: | ||||
| 0 | REF | REF | REF | REF |
| 1–3 | –1.77 (–4.49, 0.97) | –3.36 (–7.37, 0.69) | –3.31 (–7.35, 0.69) | –3.41 (–7.40, 0.59) |
| # times found infected with any STH: | ||||
| 0–1 | REF | REF | REF | REF |
| 2 | –2.33 (–4.38, –0.28) | 2.68 (–9.13, 14.95) | –3.46 (–7.65, 1.07) | 10.61 (–4.16, 16.22) |
| 3 | –2.06 (–4.27, 0.14) | –5.16 (–9.67, –0.90) | –4.52 (–7.80, –1.26) | –4.31 (–8.82, –0.25) |
| 4–5 | –1.00 (–3.32, 1.33) | –1.70 (–7.42, 3.76) | –2.23 (–5.41, 0.89) | 0.25 (–5.59, 4.48) |
aAll effect estimates are adjusted for: maternal education, use of gas for cooking, ownership of a toilet connected to public sewage, stunting at 1 year of age, baseline cognitive raw score, number of routine growth and development visits attended from birth to 1 year of age and number of years in preschool.
Discussion
Our results document an association between STH infection and child development in a cohort of preschool children. From the STH misclassification-adjusted results, infection by each STH species was associated with lower IQ scores, with Ascaris infection having the largest effect. Cumulative Ascaris, Trichuris and any STH infections were found to be associated with lower total, verbal and performance IQ scores. Hookworm infection was found to be associated with lower total IQ scores but its effect on verbal and performance IQ scores was inconclusive. The relatively wide 95% credible intervals for these effects, however, led to some ambiguity regarding the exact sizes and clinical significance of these effects. In this study, we chose to look at the effect of the number of detected STH infections over a long time period instead of looking at one infection at one single time point, as in previous studies. We consistently found that the largest effect on IQ scores was for being found infected two or three times. Compared with children who were never found infected or were infected one time, children found infected two or three times had IQ scores that ranged, on average, from one to nine points lower, depending on the STH species and the IQ construct.
The exposure—cumulative STH infection—was measured by summing indicators of binary variables (i.e. STH infection) over time (i.e. between 1 and 5 years of age). This type of analysis has been referred to as an ‘accumulation hypothesis’ and requires the assumption that cumulative STH infection between 1 and 5 years of age affects child development irrespective of the specific timing of infection.27 Future research should also consider ‘critical period’ hypotheses, as STH infections may have a particularly important and irreversible effect on child development at a more precise time point during the first 5 years of life.27,28
We found low WPPSI-III scores, with over 85% of children scoring in the below-average range. These results are consistent with regional indicators (e.g. poverty, malnutrition and illiteracy rates)29; however, whereas the Spanish version of the WPPSI-III was validated in a Mexican population and used previously in Peru,30 it has not been previously validated in this specific population and generalizability may be limited.
This initial analysis investigates the effect of cumulative STH infections over time using STH-prevalence data. It would be valuable for future research to look at the effect of cumulative infection with moderate- or heavy-intensity STH infections (e.g. number of moderate- or heavy-intensity infections detected over time). Consideration of infection intensity would be useful because STH-related morbidity is usually associated with moderate- or heavy-intensity infections and less associated with light-intensity infections. This type of analysis, however, will likely suffer from bias due to measurement error for which adjustment metrics do not currently exist.
Our results inform the current debate surrounding the benefits of deworming on child health. A recent Cochrane Review investigating the effect of deworming on cognitive development in children concluded that deworming was unlikely to have an effect on cognitive development.31 Several researchers and public health experts have challenged this review32 and one of the specific criticisms is that many of the reviewed trials only provided a single dose of deworming. Considering the high probability of rapid re-infection following treatment, single-dose deworming is likely insufficient to produce an important effect on a potentially chronic condition.32 Whereas our results do not directly address the effect of deworming, they do show that a single infection at one time point is unlikely to have an important long-term effect on child development and that recurrent infections over time may have important effects. Therefore, to obtain an accurate understanding of the true burden of STH infection, future research must focus on the health effects of long-term infection and of repeated doses of deworming provided over several years.
This study is unique. A large cohort of children recruited at 1 year of age was followed to 5 years, with annual measurements of STH infection and child development. This allowed us to look at cumulative STH infections over time—a unique and possibly more relevant exposure that has not previously been studied. Additionally, to our knowledge, no previous study investigating the effect of STH infection on child development has adjusted for misclassification of STH infection. Since no gold-standard diagnostic technique exists, all research conducted on STH infections suffers from such misclassification bias. Ignoring this can lead to unpredictable bias in reported results.
Our results also show that the magnitude of the misclassification of STH infection can have an important effect on the adjusted results. There is little agreement regarding the sensitivity values of the Kato-Katz and other STH diagnostic techniques in the literature, with different publications reporting different sensitivity values.3,4 Our results highlight that it is important that additional research be conducted to determine the true sensitivity of the Kato-Katz and other STH diagnostic techniques.
This study has limitations. First, the exposure—cumulative STH infection over time—is a simple proxy measure. Ideally, stool specimens would be collected daily and the total amount of time that each child was STH-infected would be calculated. This is obviously infeasible. We believe, however, that the number of times detected as infected annually is a reasonable estimate of the relative burden of STH infection between 1 and 5 years of age. Second, this is an observational study and, therefore, residual confounding may explain some of the observed associations. Such confounding, however, would need to be strong to explain the magnitude of the observed associations. Finally, although the Bayley-III and WPPSI-III are among the best available scales to measure child development in preschool children, neither scale is perfect.24,33 The Bayley-III, for example, has been criticized for overestimating development34 and the WPPSI-III has been criticized for lacking a measure of short-term memory.24
The results of our study suggest that STH infection in preschool children contributes to impaired child development. Therefore, prevention of STH infection during this period of life, when the brain is rapidly developing, should be made a priority. WHO has set a goal of 75% national coverage of STH control programmes in all endemic countries by the year 2020.35 In 2016, however, the global coverage rate in preschool children was only 50.8%.1 Increased global efforts are still urgently needed to adequately address STH infection as a public health problem, especially in preschool children living in STH-endemic countries.
Conclusion
These results provide important empirical evidence regarding the effect of STH infection on child development. We have shown that, in preschool children, an association exists between cumulative STH infections up to 5 years of age and lower development scores, especially for Ascaris infection. The results also highlight the importance of adjusting for STH misclassification. Additional research on diagnostic technique parameters would enable researchers to obtain more precise and conclusive results from analyses adjusted for STH misclassification. The results, however, do suggest that prioritizing preschool children for STH interventions including deworming could lead to life-long improvements in cognition and may ultimately contribute to improving productivity in adulthood and reducing poverty levels in STH-endemic countries.
Funding
Research reported in this publication was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number P50AI098574. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This work was also supported by the Thrasher Research Fund (02832-2 to T.W.G) and the Canadian Institutes of Health Research (MOP-110969 to T.W.G.).
Conflict of interest: None declared.
Supplementary Material
References
- 1. WHO. Schistosomiasis and soil-transmitted helminthiases: number of people treated in 2016. Wkly Epidemiol Rec 2017;92:749–60. [PubMed] [Google Scholar]
- 2. WHO. Deworming for Health and Development. Geneva: World Health Organization, 2005. [Google Scholar]
- 3. Nikolay B, Brooker SJ, Pullan RL. Sensitivity of diagnostic tests for human soil-transmitted helminth infections: a meta-analysis in the absence of a true gold standard. Int J Parasitol 2014;44:765–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tarafder MR, Carabin H, Joseph L, Balolong E, Olveda R, McGarvey ST. Estimating the sensitivity and specificity of Kato-Katz stool examination technique for detection of hookworms, Ascaris lumbricoides and Trichuris trichiura infections in humans in the absence of a ‘gold standard’. Int J Parasitol 2010;40:399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Walker SP, Wachs TD, Gardner JM et al. . Child development: risk factors for adverse outcomes in developing countries. Lancet 2007;369:145–57. [DOI] [PubMed] [Google Scholar]
- 6. Grantham-McGregor S, Cheung YB, Cueto S et al. . Developmental potential in the first 5 years for children in developing countries. Lancet 2007;369:60–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kvalsvig J, Albonico M. Effects of geohelminth infections on neurological development. Handb Clin Neurol 2013;114:369–79. [DOI] [PubMed] [Google Scholar]
- 8. Kuong K, Fiorentino M, Perignon M et al. . Cognitive performance and iron status are negatively associated with hookworm infection in Cambodian schoolchildren. Am J Trop Med Hyg 2016;95:856–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Liu C, Luo R, Yi H et al. . Soil-transmitted helminths in southwestern China: a cross-sectional study of links to cognitive ability, nutrition, and school performance among children. PLoS Negl Trop Dis 2015;9:e0003877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shang Y, Tang L. Intelligence level and characteristics of cognitive structure in school-age children infected with soil-transmitted helminthes. Chinese J Parasitol Parasit Dis 2010;28:423–26. [PubMed] [Google Scholar]
- 11. Santos DN, Assis AMO, Bastos ACS et al. . Determinants of cognitive function in childhood: a cohort study in a middle income context. BMC Public Health 2008;8:202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ezeamama AE, Friedman JF, Acosta LP et al. . Helminth infection and cognitive impairment among Filipino children. Am J Trop Med Hyg 2005;72:540–48. [PMC free article] [PubMed] [Google Scholar]
- 13. Sakti H, Nokes C, Hertanto W, Hendratno S, Hall A, Bundy DA. Evidence for an association between hookworm infection and cognitive function in Indonesian school children. Trop Med Int Health 1999;4:322–34. [DOI] [PubMed] [Google Scholar]
- 14. Oberhelman RA, Guerrero ES, Fernandez ML et al. . Correlations between intestinal parasitosis, physical growth, and psychomotor development among infants and children from rural Nicaragua. Am J Trop Med Hyg 1998;58:470–75. [DOI] [PubMed] [Google Scholar]
- 15. Callender J, Walker SP, Grantham‐McGregor SM, Cooper ES. Growth and development four years after treatment for the Trichuris dysentery syndrome. Acta Paediatr 2007;87:1247–49. [DOI] [PubMed] [Google Scholar]
- 16. Hutchinson SE, Powell CA, Walker SP, Chang SM, Grantham-McGregor SM. Nutrition, anaemia, geohelminth infection and school achievement in rural Jamaican primary school children. Eur J Clin Nutr 1997;51:729–35. [DOI] [PubMed] [Google Scholar]
- 17. Simeon D, Callender J, Wong M, Grantham‐McGregor S, Ramdath DD. School performance, nutritional status and trichuriasis in Jamaican schoolchildren. Acta Paediatr 1994;83:1188–93. [DOI] [PubMed] [Google Scholar]
- 18. Callender JEM, Grantham-McGregor S, Walker S, Cooper ES. Trichuris infection and mental development in children. Lancet 1992;339:181. [DOI] [PubMed] [Google Scholar]
- 19. Waite JH, Neilson I. Effects of hookworm disease on mental development of North Queensland schoolchildren. JAMA 1919;73:1877–79. [PubMed] [Google Scholar]
- 20. Lobato L, Miranda A, Faria IM, Bethony JM, Gazzinelli MF. Development of cognitive abilities of children infected with helminths through health education. Rev Soc Bras Med Trop 2012;45:514–19. [DOI] [PubMed] [Google Scholar]
- 21. Campbell SJ, Nery SV, Doi SA et al. . Complexities and perplexities: A critical appraisal of the evidence for soil-transmitted helminth infection-related morbidity. PLoS Negl Trop Dis 2016;10:e0004566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Joseph SA, Casapía M, Montresor A et al. . The effect of deworming on growth in one-year-old children living in a soil-transmitted helminth-endemic area of Peru: a randomized controlled trial. PLoS Negl Trop Dis 2015;9:e0004020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Joseph SA, Casapía M, Lazarte F et al. . The effect of deworming on early childhood development in Peru: a randomized controlled trial. SSM Popul Health 2015;1:32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lichtenberger EO. General measures of cognition for the preschool child. Ment Retard Dev Disabil Res Rev 2005;11:197–208. [DOI] [PubMed] [Google Scholar]
- 25. Wechsler D. Escala Wechsler de inteligencia Para los niveles preescolar y primario—III: Manual Técnico. Mexico: El Manual Moderno, 2002. [Google Scholar]
- 26. MacLehose RF, Olshan AF, Herring AH, Honein MA, Shaw GM, Romitti PA. Bayesian methods for correcting misclassification: an example from birth defects epidemiology. Epidemiology 2009;20:27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mishra G, Nitsch D, Black S, De Stavola B, Kuh D, Hardy R. A structured approach to modelling the effects of binary exposure variables over the life course. Int J Epidemiol 2009;38:528–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kuh D, Shlomo YB. A Life Course Approach to Chronic Disease Epidemiology. Oxford, United Kingdom: Oxford University Press, 2004. [Google Scholar]
- 29. Instituto Nacional de Estadística e Informatica. Estadisticas Sociales 2017. https://www.inei.gob.pe/estadisticas/indice-tematico/sociales/ (4 July 2017, date last accessed). [Google Scholar]
- 30. Warthon-Medina M, Qualter P, Zavaleta N, Dillon S, Lazarte F, Lowe NM. The long term impact of micronutrient supplementation during infancy on cognition and executive function performance in pre-school children. Nutrients 2015;7:6606–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Taylor‐Robinson DC, Maayan N, Soares‐Weiser K, Donegan S, Garner P. Deworming drugs for soil‐transmitted intestinal worms in children: effects on nutritional indicators, haemoglobin, and school performance. Cochrane Database Syst Rev 2015;CD000371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Montresor A, Addiss D, Albonico M et al. . Methodological bias can lead the Cochrane Collaboration to irrelevance in public health decision-making. PLoS Negl Trop Dis 2015;9:e0004165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Frongillo EA, Tofail F, Hamadani JD, Warren AM, Mehrin SF. Measures and indicators for assessing impact of interventions integrating nutrition, health, and early childhood development. Ann Ny Acad Sci 2014;1308:68–88. [DOI] [PubMed] [Google Scholar]
- 34. Anderson PJ, Burnett A. Assessing developmental delay in early childhood—concerns with the Bayley-III scales. Clin Neuropsychol 2017;31:371–81. [DOI] [PubMed] [Google Scholar]
- 35. WHO. Soil-Transmitted Helminthiases: Eliminating Soil-Transmitted Helminthiases as a Public Health Problem in Children: Progress Report 2001–2010 and Strategic Plan 2011–2020. Geneva: World Health Organization, 2012. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.