Abstract
Spirituality measures often show positive associations with preferred mental health outcomes in the general population; however, research among American Indians (AIs) is limited. We examined the relationships of mental health status and two measures of spirituality – the Midlife Development Inventory (MIDI) and a tribal cultural spirituality measure – in Northern Plains AIs, aged 15–54 (n = 1636). While the MIDI was unassociated with mental health status, the tribal cultural spirituality measure showed a significant relationship with better mental health status. Mental health conditions disproportionately affect AIs. Understanding protective factors such as cultural spirituality that can mitigate mental health disorders is critical to reducing these health disparities.
Keywords: American Indian, Native American, mental health, spirituality, SF-36, Mental Component Summary (MCS)
Introduction
Spirituality and religiosity, measured by variables as diverse as religious affiliation, church attendance, ritual participation, practices, beliefs, and attitudes, commonly appear as protective and resilience factors for mental health disorders in the general population (Bonelli & Koenig, 2013; Koenig, King, & Carson, 2012; Koenig, McCullough, & Larson, 2001).1 Two recent systematic reviews of the literature reported that the majority of studies relating spirituality to mental health showed improved mental health states (AbdA-leati, Mohd Zaharim, & Mydin, 2016; Bonelli & Koenig, 2013). One of these reviews demonstrated that 72% of the 43 studies linked spirituality to improved mental health (Bonelli & Koenig, 2013). Research reviews that summarise the use of spirituality for conditions such as anxiety disorders (Koenig, 2015), substance use disorders (Koenig, 2015; Walton-Moss, Ray, & Woodruff, 2013), and traumatic stress (Weaver, Flannelly, Garbarino, Figley, & Flannelly, 2003) demonstrate a pattern of positive associations with preferred mental health outcomes. Spirituality is also associated with a decrease in suicide and suicidality (Koenig, 2015; Koenig et al., 2001).
Relationships between spirituality and mental health have been examined among a number of racial and ethnic populations, and the results suggest similar positive relationships (Assari, 2013; Levin & Taylor, 1998; McRae, Carey, & Anderson-Scott, 1998; Musick, Koenig, Hays, & Cohen, 1998; Reinert, Campbell, Bandeen-Roche, Sharps, & Lee, 2015). Yet only a few such studies focus on, or even included, American Indians (AIs). This small but growing body of work illustrates that beliefs and practices related to both tribally specific cultural spirituality and Christianity may be related to positive mental health outcomes. For instance, East Coast AIs 65 years and older, who placed a great importance on faith and prayed more frequently had better scores on the mental health subscale of the Short Form-36 compared to those who did not practice these behaviours (Meisenhelder & Chandler, 2000). Another study conducted on four reservations in the Midwestern US and five Canadian First Nation reserves discovered spiritual activities, defined as traditional to one’s tribe, were related to alcohol cessation (Stone, Whitbeck, Chen, Johnson, & Olson, 2006). Still another study revealed, while Christian beliefs were protective against alcohol use, affiliation with the Native American Church – a spiritual tradition that combines aboriginal practices with Christian elements – was protective against alcohol and polysubstance use among urban AI youth (Kulis, Hodge, Ayers, Brown, & Marsiglia, 2012).
Finally, a study of Northern Plains (NP) tribes participating in the American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project (AISUPERPFP) found mixed results. It investigated the relationship of two, spirituality measures with one important mental health outcome, suicidality (Garroutte et al., 2003). It found no significant relationship with spirituality as measured by the Midlife Development Inventory (MIDI), an instrument in common use among the general population. However, a measure created in consultation with AI research participants that resonated with their cultural perspectives was associated with lower suicidality (Garroutte et al., 2003).
The pattern of findings in this later study draws attention to the probable importance of measuring AI spirituality in ways meaningful to this population. We returned to variables collected during the AI-SUPERPFP study to examine the association of a general measure of mental health status, the Mental Component Summary (MCS) score of the SF-36, and two measures of spirituality, the MIDI and a tribal cultural spirituality measure. We expected to find a pattern of relationships between our general measure of mental health status and the spirituality measures that resembled the earlier findings of the NP suicidality study cited above (Garroutte et al., 2003). Specifically, we hypothesised that spirituality as measured by the MIDI, the conventional measure developed for use with the general population, would not show a significant association with mental health status. At the same time, we also hypothesised that the tribal cultural spirituality measure would have a significant and positive relationship with mental health status. We expected these relationships to persist after controlling for demographic and socioeconomic variables, and the number of physical and mental health conditions.
Methods
Data source
The data for this secondary analysis came from the AI-SUPERPFP, a large community-based, cross-sectional survey. The AI-SUPERPFP assessed the prevalence of alcohol, drugs, and mental disorders as well as service utilisation in two distinct AI populations located in the NP and Southwest. Study approval was obtained from the Colorado Multiple Institutional Review Board (COMIRB) and was supported by tribal resolution from participating tribal governments. Tribal governments provided the names, dates of birth, tribal enrollment numbers, and last known addresses of tribal members. Researchers identified individuals to be located using stratified random sampling procedures (Kish, 1965). Individuals were eligible to participate if they lived on or within 20 miles of their home reservations. Seventy-seven per cent of the located individuals consented to participate. After receiving intensive training in research and interviewing procedures, tribal community members collected the data from 1997 to 1999 via computer-assisted personal interviews. For a more detailed description of the AI-SUPERPFP methods, see Beals, Manson, Mitchell, and Spicer (2003).
The analyses reported here focused on the NP sample (n = 1636). The COMIRB determined that our project, which was limited to secondary analyses, did not constitute human subjects research. We obtained formal tribal approvals either through the relevant tribal Research Review Board or tribal resolution.
Measures
Outcome measure
The MCS of the SF-36 (Ware, 1994) was the outcome variable and measured self-reported mental health status. Prior to data collection, focus groups of tribal members reviewed this instrument for cultural acceptability, as they did all AI-SUPERPFP measures, and recommended necessary adaptations. Focus group members asked us to modify one MCS question, “During the past four weeks, how much has your physical health or emotional problems interfered with your normal social activities with family, friends, neighbors, or groups?” Focus group members recommended breaking this question into two questions, one focused on physical health and the other on emotional problems. This change was implemented and upon scoring we combined responses to the two questions which did affect the overall scoring.
The SF-36 consists of eight subscales with four subscales comprising the majority of the MCS score: vitality, social functioning, role-emotional, and mental health (Ware, 1994). The Vitality Scale includes four questions related to energy and fatigue. Social functioning includes two items that assess the impact of health problems on social activities. The Role Functioning-Emotional Scale includes three items that address limitations due to emotional problems. The Mental Health Scale comprises five items related to four major mental health dimensions: anxiety, depression, loss of behavioural/emotional control, and psychological well-being (Ware, 2000). The remaining scales include physical functioning, role functioning-physical, bodily pain, and general health. The MCS score was derived using established algorithms and was standardised to allow for meaningful comparison with other studies (Ware, 1994). The MCS score ranges from 0 to 100 (mean = 50, standard deviation = 10 in the original standardised population) with higher scores indicating better mental health status. Previous analyses using the AI-SUPERPFP sample demonstrated that the MCS performed well among the NP Tribes (Cronbach’s α = .88) (Jiang et al., 2009; Mitchell & Beals, 2011).
Primary independent variable(s)
The MIDI was chosen in consultation with focus groups that were drawn from our sample (Institute on Aging, 2004; MacArthur Foundation Network on Successful Midlife Development, 1997). The MIDI was selected from several commonly used measures in the general population as the most appropriate. Focus groups suggested splitting question 3 into two questions to enhance comprehensibility. The change was made and did not affect scoring. The following items assessed the overall importance of spirituality in everyday life: (1) “How important is religion/spirituality in your life?” (2) “How often do you spend time on religious or spiritual practice?” (3) “How important is it to you that your children participation in some kind of religious or spiritual practice? Or if no children, how important would it be to you that they participated in some kind of religious or spiritual practice?” and (4) “How often do you seek comfort or guidance through religious or spiritual means?” Responses ranged from 0 (“not at all important”) to 3 (“very important”) and were combined to form an average score; Cronbach’s alpha for the sample was .76.
In addition to advising researchers on the necessary modifications to the MIDI, tribal focus groups directed the creation of the tribal cultural spirituality measure. In the context of the review of the MIDI, focus group members indicated that the MIDI did not adequately reflect the perceptions, experiences, knowledge, and actions tribal members themselves associate with spirituality (Garroutte et al., 2003). The research team then worked with focus group members to develop a measure which included the following eight items, participants were asked to “agree” or “disagree”: (1) “There is balance and order in the universe”, (2) “I am in harmony with all living things”, (3) “I feel connected with other people in life”, (4) “I follow the Red Road”, (5) “When I need to return to balance-I know what to do”, (6) “I feel like I am living the right way”, (7) “I give to others and receive from them in return”, and (8) “I am a person of integrity”. These questions, while quite specific to AI spirituality in our sample, resemble content of other measures (Underwood & Teresi, 2002). A mean score provides the proportion of items endorsed; Cronbach’s alpha for the sample was .74.
Other independent variables
Demographic variables included age as a continuous variable and gender.
Socioeconomic variables included married/cohabitating (living as though married), high school completion or the equivalent, unemployed at the time of the interview, and living below the US Federal poverty level, which was based upon household income and size. Besides age, the other demographic and socioeconomic variables were dichotomous with (yes/no) responses; “no” used as the reference category.
Health Variables included the number of physical health problems and the number of DSM-IV disorders. The number of health problems included a count of 31 common chronic physical health problems diagnosed by a doctor and experienced within the last year. These included but were not limited to conditions such as arthritis, diabetes, high blood pressure, heart disease, kidney problems, stroke, and high cholesterol, among others. A culturally adapted version of the Composite International Diagnostic Interview (Andrews & Peters, 1998; Kessler & Ustun, 2004; Kessler et al., 1998) assessed the presence of psychiatric disorders using DSM-IV criteria (American Psychiatric Association, 1994). Nine disorders were assessed: major depressive episode, dysthymia, generalised anxiety disorder, panic disorder, post-traumatic stress disorder, alcohol abuse, alcohol dependence, drug abuse, and drug dependence.
Statistical analysis
We used descriptive statistics to characterise the sample. Means and standard deviations are presented for continuous variables; for categorical variables, the number of participants endorsing the items and percentages are provided. Linear regression was used to estimate the bivariate relationships of the mental health status score with each variable. Mean values, 95% confidence intervals, and statistical significance are reported. Sample weights were used in all analyses to account for the differential probability of selection into the sample (Cochran, 1977).
To test our hypotheses, we used Mplus (Muthén & Muthén, 1998–2014) estimating nested linear regression models, progressively adding in blocks of variables beginning with the relationship of the spirituality indicators to the MCS (Model 1). In the next block, we added demographic indicators (Model 2), followed by socioeconomic variables (Model 3). Examining the health variables, we first added in the number of physical health problems (Model 4), followed by the number of DSM-IV disorders (Model 5). Improvements in the fit of models were assessed by R-squared, the amount of variance explained, and are reported for each of the five models.
A comparison of Models 4 and 5 suggested that the number of DSM-IV disorders may have mediated the relationship of the tribal cultural spirituality measure and the MCS. We used the definitions of full and partial mediation to assess potential mediation (Baron & Kenny, 1986). Full mediation occurs when a statistically significant relationship between the MCS (outcome) and the tribal cultural spirituality indicator (independent variable) is no longer statistically significant when the number of DSM-IV disorders (mediating variable) is included in the model, while partial mediation occurs when relationships are greatly reduced once the number of DSM-IV disorders (mediator) is included in the model. Mediation was tested using Mplus (Muthén & Muthén, 1998–2014) and the indirect, direct, and total results are reported.
The proportion of missing data in the dataset used for these analyses was less than 2%. Full information maximum likelihood was used to handle missing data allowing us to retain the entire sample for all nested models (Muthén & Muthén, 1998–2014).
Results
Sample characteristics appear in Table 1. The average MCS score was 54.4 (SD = 8.1). The average age was 33.8 years (SD = 10.7); 51% were female; 51% were married or living as married; 47% had a high school education or equivalent; 32% were unemployed, and 62% were living below the US federal poverty level. The average number of physical health problems in the past year was 1.6 (SD = 2.2), while the average number of DSMIV disorders in the past year was .35 (SD = .72).
Table 1.
Sample characteristics and bivariate associations of MCS with each variable.
| n = 1638 | Entire sample | MCS score | ||
|---|---|---|---|---|
| n/mean | %/sd | Mean | 95%CI | |
| Mental Component Summary Score | 54.4 | 8.1 | ||
| Spirituality measures | ||||
| MIDI | 1.95 | .77 | 52.9 | 53.9, 54.4 |
| Tribal cultural spirituality | .79 | .23 | 56.0 | 53.9, 58.1† |
| Demographics | ||||
| Age | 33.8 | 10.7 | 53.9 | 53.9, 53.9 |
| Female | 835 | 51% | 53.7 | 52.9, 54.6** |
| Socioeconomic variables | ||||
| Married/cohabitating | 835 | 51% | 54.4 | 54.4, 55.2 |
| High school graduate or GED | 770 | 47% | 55.0 | 54.2, 55.8** |
| Unemployed | 524 | 32% | 53.6 | 52.7, 54.9* |
| Living below federal poverty level | 1016 | 62% | 53.7 | 52.8, 56.5† |
| Health variables (past year) | ||||
| Number self-reported health problems diagnosed by doctor | 1.6 | 2.2 | 54.8 | 54.6, 56.0† |
| Number of DSM-IV disorders | .35 | .72 | 51.5 | 50.8, 52.3† |
Note: MCS = Mental Component Summary Score, n = number, sd = standard deviation, % = per cent, CI = confidence interval.
p value ≤ .05,
p value ≤ .01,
p value ≤ .001.
Table 2 depicts the results of the nested linear regression Models 1 through 5. Model 1 shows the relationship of the spirituality indicators to the MCS. The results indicate no association between the MIDI and the MCS and also indicated those with higher tribal cultural spirituality scores had higher mental health status scores. Models 2 through 4 show that the tribal cultural spirituality estimates were similar to Model 1, though in each block the magnitude of the relationship attenuates as other variables account for some of the variation in the MCS. Comparing Models 4 and 5, Model 5 shows a marked reduction in the tribal cultural spirituality estimate, suggesting the number of DSM-IV disorders may be acting as a mediating variable.
Table 2.
Nested linear regression models predicting Mental Component Summary Scores with spirituality indicators as primary independent variables.
| n=1638 | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | 95% Cl | Est. | SE | 95% Cl | Est. | SE | 95% Cl | Est. | SE | 95% Cl | Est. | SE | 95% Cl | |
| Spirituality | |||||||||||||||
| MIDI | −.08 | .29 | −.65, .49 | −.04 | .29 | −.61, .53 | −.11 | .29 | −.67, .45 | −.03 | .28 | −.58, .52 | .07 | .28 | −.57, .61 |
| Tribal cultural spirituality | 7.75† | 1.21 | 5.50, 9.43 | 7.77† | 1.21 | 5.58, 9.97 | 7.49† | 1.11 | 5.32, 9.67 | 7.07† | 1.07 | 4.97, 9.17 | 4.99† | 1.03 | 2.98, 7.00 |
| Demographics | |||||||||||||||
| Age | −.01 | .02 | −.04, .03 | −.01 | .02 | −.05, .02 | .04* | .02 | .01, .08 | .03 | .02 | −.01, .06 | |||
| Female | −1.34† | .41 | −2.15,−.52 | −1.08** | .41 | −1.89, −.28 | −.71 | .41 | −1.50, .09 | −.97* | .39 | −1.73,−.21 | |||
| Socioeconomic variables | |||||||||||||||
| Married/cohabitating | −.20 | .42 | −1.02, .61 | −.10 | .41 | −.90, .70 | −.22 | .39 | −.98, .54 | ||||||
| High school graduate or GED | 1.15** | .41 | .34,1.96 | .96* | .41 | .17, 1.76 | .69 | .39 | −.07, 1.45 | ||||||
| Unemployed | −.56 | .49 | −1.52, .41 | −.14 | .48 | −1.08, .80 | −.07 | .46 | −.97, .83 | ||||||
| Living below federal poverty level | −1.45** | .50 | −2.27, −.49 | −1.32** | .44 | −2.19, −.46 | −1.25** | .43 | −2.09, −.42 | ||||||
| Health variables (past year) | |||||||||||||||
| Number self-reported health problems | −.73† | .13 | −.98, −.47 | −.53† | .13 | −.78, −.28 | |||||||||
| Number of DSM-IV disorders | −3.69† | .38 | −4.42,−2.93 | ||||||||||||
| R-squared | .05 | .05 | .07 | .10 | .20 | ||||||||||
Note: MIDI = Midlife Development Inventory, Est = estimate, SE = standard error, CI = confidence interval.
p value ≤ .05,
p value ≤ .01,
p value ≤ .001.
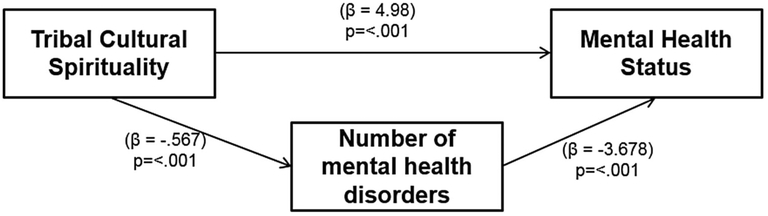
Figure 1 and Table 3 present the path analysis showing the mediation results. The number of DSM-IV disorders partially mediated the relationship between the tribal cultural spirituality measure and the MCS. Results indicated that higher tribal cultural spirituality scores were associated with fewer mental health disorders, and a greater number of mental health disorders were associated with lower mental health status. In addition, the tribal cultural spirituality score had a direct relationship to mental health status; higher scores indicate higher mental health status scores. Total results that combine the indirect and direct relationships (2.09 + 4.99 = 7.07) of the culturally oriented spirituality measure and MCS indicated higher tribal cultural spirituality scores are associated with higher mental health status scores.
Figure 1.
Direct relationship of the tribal cultural spirituality and mental health status, and the indirect relationship through the number of mental health disorders.
Table 3.
Mental Component Summary score mediated by number of DSM-IV disorders with spirituality variables as primary independent variables.
| n = 1638 | Indirect relationship to MCS mediated by DSM-IV disorders8 | Direct relationship to MCS | Total (indirect and direct) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Est. | SE | 95% Cl | Est. | SE | 95% Cl | Est. | SE | 95% Cl | |
| Spirituality | |||||||||
| MIDI | −.11 | .09 | −.28, .07 | .07 | .28 | −.47, .61 | −.04 | .28 | −.58, .51 |
| Culturally oriented spirituality | 2.09† | .47 | 1.17,3.00 | 4.99† | 1.03 | 2.98, 7.00 | 7.07† | 1.07 | 4.98,9.17 |
| Demographics | |||||||||
| Age | .01* | .01 | .001, .02 | .03 | .02 | −.01, .06 | .04* | .02 | .01, .08 |
| Female | .26 | .14 | −.01,.53 | −.97* | .39 | −1.73,−.21 | −.71 | .41 | −1.50, .08 |
| Sotioeconomic status | |||||||||
| Married/cohabitating | .12 | .14 | −.15, .40 | −.22 | .39 | −.98, .54 | −.10 | .41 | −.90, .70 |
| High school graduate or GED | .26 | .15 | −.02, .55 | .69 | .39 | −.07, 1.45 | .95* | .41 | .16, 1.75 |
| Unemployed | −.08 | .15 | −.37, .22 | −.07 | .46 | −.97, .83 | −.15 | .48 | −1.09, .79 |
| Living below federal poverty level | −.08 | .15 | −.36, .21 | −1.25** | .43 | −2.09, −.42 | −1.33** | .44 | −2.19, −.47 |
| Health variables (past year) | |||||||||
| Number self-reported health problems diagnosed by doctor | −.20† | .04 | −.29,−.12 | −.53† | .13 | −.77, −.28 | −.73† | .13 | −.99, −.47 |
| R-squared | .20 | ||||||||
Note: Est. = estimate, CI = confidence interval, SE = standard error.
aNumber of DSM-IV disorders within the last year.
p value < .05,
p value < .01,
p value < .001.
Discussion
AIs suffer pronounced mental health disparities. Previous analyses of the AI-SUPERPFP data found that NP AIs had 2.82 times the odds of lifetime post-traumatic stress disorder compared to the general population and were 37% more likely to have an anxiety disorder (Beals et al., 2005). Other research shows that lifetime rates of substance use disorders are also higher compared to the US general population (45.3% versus 35.4%) (Beals et al., 2005), as are rates of completed suicides (22.4 versus 10.6 per 100,000) (Indian Health Service, Office of Public Health Support, & Division of Program Statistics, 2008). Such disparities necessitate the investigation of protective factors that may mitigate mental health disorders among AIs. Substantial evidence suggests that spirituality may function as a protective factor in the generation population.
Compared to what is known about other subpopulations in the US, considerably less is known about the relationship of spirituality and mental health among AIs. This scarcity of research is surprising, given the central role that spirituality plays in AI life. Data from AISUPERPFP show that NPs AIs assign high salience to religion and spirituality at rates that exceed those of other Americans. Ninety-five per cent of men and 98% of women reported that spiritual and/or religious beliefs are either “very important” or “somewhat important” in their lives (Garroutte et al., 2009). When this question was asked among the US general population, 73% of men and 82% of women give the same responses (Pew Research Center, 2016).
We hypothesised the tribal cultural spiritually measure would be associated with a general measure of mental health status (MCS), while the more conventional measure (MIDI) would not be related. This hypothesis was suggested by focus group work preceding AI-SUPERPFP data collection, which led us to suspect that a culturally grounded measure would be more powerful than a conventional measure of spirituality. A prior study (Garroutte et al., 2003) supported this hypothesis in the case of one particular mental health outcome, suicidality. The current study is consistent with the conclusion that tribal cultural spiritualty is an important factor contributing to better overall mental health in NP AIs.
As mentioned previously, when spirituality measures were reviewed by focus groups of tribal members in preparation for AI-SUPERPFP, the MIDI with its inquiries about the importance of spirituality for oneself and one’s children, frequency of practice, and the use of spirituality for comfort and guidance was determined the most appropriate. In addition, focus groups noted AI spirituality pertained more to how one sees oneself in the larger universe, and/or how one sees oneself within the morals of this broader universal perspective. In this research study, spirituality was only associated with mental health status when measured in a way that reflected the research participants’ own cultural perspectives. This underscores the importance of conceptualising spirituality in a manner meaningful to AI people themselves. Our findings suggest that there is reason to believe that the spirituality measures commonly used among the general population may not work well with all AIs. This may complicate efforts to understand exactly how spirituality relates to mental health. Little research attention has been given to the measurement of AI spirituality. We would argue that careful conceptualisation and measurement of spirituality in culturally resonant ways will be critically important for future AI investigations and interventions (Hodge, Limb, & Cross, 2009).
Although not hypothesised, we found the number of DSM-IV disorders acted as a partial mediator from the tribal cultural spirituality measure to mental health status. Specifically, we found the tribal cultural spirituality measure was associated with fewer mental health disorders and that fewer mental health disorders were related to higher mental health status scores. This seems reasonable since the mental health subscale of the MCS enquires about the symptoms of depression and anxiety. The count of DSM-IV disorders variable denotes whether participants met the specific criteria for the nine disorders in the past year. One would expect disorders, both current and within the last year, to be related to current mental health status. Other studies demonstrate that variables such as self-efficacy, stressful life events, and social support mediated the relationship of spirituality and health (physical and mental) (Hayward, Owen, Koenig, Steffens, & Payne, 2012; Konopack & McAuley, 2012; Smith, McCullough, & Poll, 2003). Although our mediation analysis was post hoc, it contributes to the body of work that demonstrates the complexity of spirituality and mental health. In our analyses, mental health disorders negatively influence mental health status, while tribal cultural spirituality at the same time positively affects mental health status.
Confirmatory factor analytic approaches were used to test alternative models for these data. A two-factor model emerged that differentiated the MIDI and the tribal cultural spirituality measures and also proved to be the best fit. The resulting scales had internal consistencies of .80 and .76, respectively. We assessed the correlation of the tribal cultural spiritual measure and the MIDI and found a low correlation of .26. Post hoc we also assessed whether a statistical interaction existed between these two measures and found it was not statistically significant.
The use of spirituality in the treatment of AI mental health disorders may be an important factor worthy of consideration. Although there are distinct differences in tribal cultural spirituality among AIs, the Indian Health Service (IHS) recognises that many AIs share a common view of disease etiology. Good health is a holistic approach of balance in various aspects: mental, spiritual, emotional, physical, and social states (IHS, 2015a). In recognising the importance of spirituality in the health and well-being of AIs, IHS incorporates aspects of cultural spirituality into the delivery of some care such as cancer (Witte, Begay, & Coe, 2011) and substance abuse treatment (IHS, 2015b). The expansion of these practices into more mental health services within IHS and other health care settings will likely benefit AIs.
The Joint Commission also supports the integration of spirituality into medical care. In 2010, the Joint Commission implemented standards for spirituality care that include assessment, accommodation, and the support of spiritual needs in ways that are important and meaningful to patients (Joint Commission, 2010). The use of assessments like those recommended by the Joint Commission will assist providers in accommodating the spirituality and health needs of all people (Hodge, 2015).
These analyses have both limitations and strengths. First, we focused exclusively on NP tribes; attempts to generalise to other regions must be done with caution. While the dataset is over 15 years old, its unusual size, scope, and methodological sophistication have allowed it to remain among the best for studying the relationship of spirituality and mental health status among AIs – relationships that are likely to have remained consistent over time. Because mediation was not hypothesised but uncovered during our analyses, we did not include constructs shown elsewhere to mediate the relationship of spirituality and health such as self-efficacy, stressful life events, and social support (Hayward et al., 2012; Konopack & McAuley, 2012; Smith et al., 2003).
These analytic limitations are counterbalanced by strengths. Given that even the largest studies rarely include sufficient data on AIs to permit separate analysis (Kosmin & Keysar, 1990, 2009), our work contributes to knowledge about a population whose mental health disparities are great and whose needs are poorly understood. Our work also complements and builds upon other spirituality work in this NP AI sample (Garroutte et al., 2009; Garroutte et al., 2003; Garroutte et al., 2014) and the broader spirituality literature. Although these analyses focused on an overall measure of mental health status, it nonetheless adds to research in AI samples finding that spirituality is protective against poor mental health (Garroutte et al., 2003; Puchala, Paul, Kennedy, & Mehl-Madrona, 2010; Stone et al., 2006). Not examined here but worthy of future investigation is whether the MIDI may be related to mental health status in certain AI subpopulations such as those who primarily identify with Christianity.
Conclusion
We investigated the association of mental health status with two measures of spirituality, the MIDI and a measure of tribal cultural spirituality. Though the MIDI was not associated, the tribal cultural spirituality measure was associated with higher mental health status scores. This is consistent with prior research in this NP population and suggests that spirituality is a protective factor in AI mental health. These finding also suggest that attention to appropriate spirituality measurement is needed. It further attests to the need for collaborative interventions with AI communities on effective methods to combat mental health disparities by harnessing the power of spirituality. Given that NP AIs contend with high rates of mental health disorders, understanding factors that mitigate these conditions is critical, as is support for the integration of spirituality into health care planning and practice.
Acknowledgments
Funding
This work was supported by National Institute of Mental Health [grant number MH048174 (SM Manson)]; National Institute on Minority Health and Health Disparities [grant number MD000507 (SM Manson), U54MD008164 (A Elliott)].
Footnotes
Note
Following the work of others, we define spirituality as attitudes and feelings about individual relationships with the transcendent and sacred (Koenig et al., 2001). We treat religiosity as a subtype of spirituality (Hill & Pargament, 2003; Kudel, Cotton, Szaflarski, Holmes, & Tsevat, 2011; Piderman, Schneekloth, Pankratz, Stevens, & Altchuler, 2008).
Disclosure statement
No potential conflicts of interest were reported by the authors.
References
- AbdAleati NS, Mohd Zaharim N, & Mydin YO (2016). Religiousness and mental health: Systematic review study. Journal of Religion and Health, 55(6), 1929–1937. doi: 10.1007/s10943-014-9896-1 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (DSM IV) (4th ed.). Washington, DC: Author. [Google Scholar]
- Andrews G, & Peters L (1998). The psychometric properties of the composite international diagnostic interview. Social Psychiatry and Psychiatric Epidemiology, 33(2), 80–88. doi: 10.1007/s001270050026 [DOI] [PubMed] [Google Scholar]
- Assari S (2013). Race and ethnicity, religion involvement, church-based social support and subjective health in United States: A case of moderated mediation. International Journal of Preventive Medicine, 4(2), 208–217. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3604855/ [PMC free article] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. doi: 10.1037/0022-3514.51.6.1173 [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Mitchell CM, & Spicer P, & and the AI-SUPERPFP Team. (2003). Cultural specificity and comparison in psychiatric epidemiology: Walking the tightrope in American Indian research. Culture, Medicine and Psychiatry, 27(3), 259–289. doi: 10.1023/A:1025347130953 [DOI] [PubMed] [Google Scholar]
- Beals J, Novins DK, Whitesell NR, Spicer P, Mitchell CM, & Manson SM,... & and the AI SUPERPFP Team. (2005). Prevalence of mental disorders and utilization of mental health services in two American Indian reservation populations: Mental health disparities in a national context. American Journal of Psychiatry, 162(9), 1723–1732. doi: 10.1176/appi.ajp.162.9.1723 [DOI] [PubMed] [Google Scholar]
- Bonelli RM, & Koenig HG (2013). Mental disorders, religion and spirituality 1990 to 2010: A systematic evidence-based review. Journal of Religion and Health, 52(2), 657–673. doi: 10.1007/s10943-013-9691-4 [DOI] [PubMed] [Google Scholar]
- Cochran WG (1977. Sampling techniques (3rd ed.). New York, NY: John Wiley & Sons. [Google Scholar]
- Garroutte E, Beals J, Kaufman CE, Spicer P, Henderson JA, & Nez-Henderson P, … and the AI-SUPERPFP Team. (2009). Religiosity and spiritual engagement in two American Indian populations. Journal for the Scientific Study of Religion, 48(3), 480–500. doi: 10.1111/j.1468-5906.2009.01461.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garroutte EM, Beals J, Orton HD, Henderson JA, Nez Henderson P, & Thomas JF, ... The AI-SUPERPFP Team. (2014). Religio-spiritual participation in two American Indian populations. Journal for the Scientific Study of Religion, 53(1), 17–37. doi: 10.1111/jssr.12084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garroutte EM, Goldberg J, Beals J, Herrell R, Manson SM, & Team A-S (2003). Spirituality and attempted suicide among American Indians. Social Science & Medicine, 56(7), 1571–1579. doi: 10.1016/S0277-9536(02)00157-0 [DOI] [PubMed] [Google Scholar]
- Hayward RD, Owen AD, Koenig HG, Steffens DC, & Payne ME (2012). Longitudinal relationships of religion with posttreatment depression severity in older psychiatric patients: Evidence of direct and indirect effects. Depression Research and Treatment, 58(3), 1–8. doi: 10.1155/2012/745970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PC, & Pargament KI (2003). Advances in the conceptualization and measurement of religion and spirituality: Implications for physical and mental health research. American Psychologist, 58(1), 64–74. doi: 10.1037/0003-066X.58.1.64 [DOI] [PubMed] [Google Scholar]
- Hodge DR (2015). Spiritual assessment in social work and mental health practice. New York, NY: Columbia University Press. [Google Scholar]
- Hodge DR, Limb GE, & Cross TL (2009). Moving from colonization toward balance and harmony: A native American perspective on wellness. Social Work, 54(3), 211–219. doi: 10.1093/sw/54.3.211 [DOI] [PubMed] [Google Scholar]
- Indian Health Service. (2015a). Native American disease etiology. Retrieved from https://www.ihs.gov/chr/career/etiology/
- Indian Health Service. (2015b). Youth regional treatment centers. Retrieved from https://www.ihs.gov/yrtc/
- Indian Health Service, Office of Public Health Support, & Division of Program Statistics. (2008). Indian health service regional differences in Indian health. Washington, DC: Government Printing Office. [Google Scholar]
- Institute on Aging. (2004). MIDUS, midlife in the United States, A national study of health & well-being, documentation of scales in MIDUS I. Madison, WI: Institute on Aging. [Google Scholar]
- Jiang L, Beals J, Whitesell NR, Roubideaux Y, Manson SM, & Team T. A.-S. (2009). Health-related quality of life and help seeking among American Indians with diabetes and hypertension. Quality of Life Research, 18(6), 709–718. doi: 10.1007/s11136-009-9495-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint Commission on Accreditation of Healthcare Organizations. (2010). Joint commission guide to allied health professionals. Oakbrook Terrace, IL: Author. [Google Scholar]
- Kessler RC, & Ustun TB (2004). The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). International Journal of Methods in Psychiatric Research, 13(2), 93–121. doi: 10.1002/mpr.168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Wittchen H-U, Abelson JM, McGonagle KA, Kendler KS, Knauper B, & Zhao S (1998). Methodological studies of the composite international diagnostic interview (CIDI) in the US National Comorbidity Survey. International Journal of Methods in Psychiatric Research, 7(1), 33–55. doi: 10.1002/mpr.33 [DOI] [Google Scholar]
- Kish L (1965). Survey sampling. New York, NY: John Wiley and Sons. [Google Scholar]
- Koenig HG (2015). Religion, spirituality, and health: A review and update. Advances in Mind-body Medicine, 29(3), 19–26. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/26026153 [PubMed] [Google Scholar]
- Koenig HG, King D, & Carson VB (2012). Handbook of religion and health (2nd ed.). Oxford: Oxford University Press. [Google Scholar]
- Koenig HG, McCullough ME, & Larson DB (2001). Handbook of religion and health. Oxford: Oxford University Press. [Google Scholar]
- Konopack JF, & McAuley E (2012). Efficacy-mediated effects of spirituality and physical activity on quality of life: A path analysis. Health & Quality of Life Outcomes, 10: 57. doi: 10.1186/1477-7525-10-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosmin BA, & Keysar A (1990). National Survey of Religious Identification codebook. New York, NY: The Graduate School and University Center of the City University of New York. [Google Scholar]
- Kosmin BA, & Keysar A (2009). American Religious Identification Survey (ARIS 2008) summary report. Hartford, CI: Institute for the Study of Secularism in Society and Culture. [Google Scholar]
- Kudel I, Cotton S, Szaflarski M, Holmes WC, & Tsevat J (2011). Spirituality and religiosity in patients with HIV: A test and expansion of a model. Annals of Behavioral Medicine, 41(1), 92–103. doi: 10.1007/s12160-010-9229-x [DOI] [PubMed] [Google Scholar]
- Kulis S, Hodge DR, Ayers SL, Brown EF, & Marsiglia FF (2012). Spirituality and religion: Intertwined protective factors for substance use among urban American Indian youth. American Journal of Drug and Alcohol Abuse, 38(5), 444–449. doi: 10.3109/00952990.2012.670338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin JS, & Taylor RJ (1998). Panel analyses of religious involvement and well-being in African Americans: Contemporaneous vs. longitudinal effects. Journal for the Scientific Study of Religion, 37(4), 695–709. doi: 10.2307/1388151 [DOI] [Google Scholar]
- MacArthur Foundation Network on Successful Midlife Development. (1997). Midlife Development Inventory. Chicago, IL: Author. [Google Scholar]
- McRae MB, Carey PM, & Anderson-Scott R (1998). Black churches as therapeutic systems: A group process perspective. Health Education & Behavior, 25(6), 778–789. doi: 10.1177/109019819802500607 [DOI] [PubMed] [Google Scholar]
- Meisenhelder JB, & Chandler EN (2000). Faith, prayer, and health outcomes in elderly native Americans. Clinical Nursing Research, 9(2), 191–203. doi: 10.1177/105477380000900207 [DOI] [PubMed] [Google Scholar]
- Mitchell CM, & Beals J (2011). The utility of the Kessler Screening Scale for psychological distress (K6) in two American Indian communities. Psychological Assessment, 23(3), 752–761. doi: 10.1037/a0023288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musick MA, Koenig HG, Hays JC, & Cohen HJ (1998). Religious activity and depression among community-dwelling elderly persons with cancer: The moderating effect of race. The Journals of Gerontology: Series B: Psychological Sciences and Social Sciences, 53B(4), S218–S227. doi: 10.1093/geronb/53B.4.S218 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (1998–2014). Mplus user’s guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Pew Research Center. (2016). Religious landscape study, gender composition. Importance of religion in one’s life by gender. Retrieved from http://www.pewforum.org/religious-landscape-study/gender-composition/
- Piderman KM, Schneekloth TD, Pankratz VS, Stevens SR, & Altchuler SI (2008). Spirituality during alcoholism treatment and continuous abstinence for one year. The International Journal of Psychiatry in Medicine, 38(4), 391–406. doi: 10.2190/PM.38.4.a [DOI] [PubMed] [Google Scholar]
- Puchala C, Paul S, Kennedy C, & Mehl-Madrona L (2010). Using traditional spirituality to reduce domestic violence within aboriginal communities. The Journal of Alternative and Complementary Medicine, 16(1), 89–96. doi: 10.1089/acm.2009.0213 [DOI] [PubMed] [Google Scholar]
- Reinert KG, Campbell JC, Bandeen-Roche K, Sharps P, & Lee J (2015). Gender and race variations in the intersection of religious involvement, early trauma, and adult health. Journal of Nursing Scholarship, 47(4), 318–327. doi: 10.1111/jnu.12144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith TB, McCullough ME, & Poll J (2003). Religiousness and depression: Evidence for a main effect and the moderating influence of stressful life events. Psychological Bulletin, 129(4), 614–636. doi: 10.1037/0033-2909.129.4.614 [DOI] [PubMed] [Google Scholar]
- Stone RA, Whitbeck LB, Chen X, Johnson K, & Olson DM (2006). Traditional practices, traditional spirituality, and alcohol cessation among American Indians. Journal of Studies on Alcohol, 67(2), 236–244. doi: 10.15288/jsa.2006.67.236 [DOI] [PubMed] [Google Scholar]
- Underwood LG, & Teresi JA (2002). The Daily Spiritual Experience Scale: Development, theoretical description, reliability, exploratory factor analysis, and preliminary construct validity using health-related data. Annals of Behavioral Medicine, 24(1), 22–33. doi: 10.1207/S15324796ABM2401_04 [DOI] [PubMed] [Google Scholar]
- Walton-Moss B, Ray EM, & Woodruff K (2013). Relationship of spirituality or religion to recovery from substance abuse: A systematic review. Journal of Addictions Nursing, 24(4), 217–226. doi: 10.1097/JAN.0000000000000001 [DOI] [PubMed] [Google Scholar]
- Ware JE Jr. (1994). SF-36 Physical and Mental Health Summary Scales: A user’s manual. Boston, MA: The Health Institute. [Google Scholar]
- Ware JE Jr. (2000). SF-36 Health Survey update. Spine, 25(24), 3130–3139. doi: 10.1097/00007632-200012150-00008 [DOI] [PubMed] [Google Scholar]
- Weaver AJ, Flannelly LT, Garbarino J, Figley CR, & Flannelly KJ (2003). A systematic review of research on religion and spirituality in the Journal of Traumatic Stress: 1990–1999. Mental Health, Religion & Culture, 6(3), 215–228. doi: 10.1080/1367467031000088123 [DOI] [Google Scholar]
- Witte C, Begay TD, & Coe K (2011). Spiritual care within oncology care: Development of a spiritual care program at an Indian health service hospital. Journal of Health Disparities Research and Practice, 4(3), 54–60. Retrieved from https://digitalscholarship.unlv.edu/jhdrp/vol4/iss3/7 [Google Scholar]