Abstract
Background and aims
Macrophages play a significant role in chronic liver disease as reflected by elevated soluble (s)CD163 and mannose receptor (sMR) levels and associated with liver disease severity and prognosis. Extracellular matrix remodelling associated with fibrogenesis may be affected by systemic inflammation induced by bacterial translocation. Therefore, we aimed to investigate the effect of rifaximin-α, an antibiotic with effect on gut bacteria, on sCD163, sMR, and collagen metabolites.
Methods
Fifty-four clinically stable patients with decompensated cirrhosis were randomized to 4 weeks treatment with rifaximin-α (n = 36) or placebo (n = 18). Macrophage markers sCD163, sMR and markers of collagen fibrogenesis (C3M and C4M) and formation (PRO-C3 and P4NPS7) were analysed in plasma before and after treatment.
Results
sCD163 and sMR levels were associated with liver disease severity (MELD score, sCD163 rho = 0.47, p<0.001 and sMR rho = 0.37, p = 0.005). There was no effect of Rifaximin-α on sCD163 levels (median (range) sCD163 5.64(2.02 to 10.8) at baseline versus 4.42(1.98 to 8.92) at follow-up in the rifaximin-α group and 4.85 (2.29 to 12.1) at baseline versus 4.32 (1.98 to 12.4) at follow-up in the placebo-group), p = 0.34); nor sMR levels, p = 0.34.
Also in patients with elevated lipopolysaccharide binding protein (> 5.9 μg/ml, 38 patients) there was no effect of rifaximin-α on sCD163 (p = 0.49) or sMR levels (p = 0.32).
Conclusion
We confirmed that macrophage activation markers sCD163 and sMR are directly associated to liver disease severity (MELD score). However, rifaximin-α has no effect on sCD163, sMR or collagen markers in decompensated cirrhosis and does therefore not seem to interfere with macrophage activation or fibrogenesis.
Introduction
Portal hypertension (PH) in liver cirrhosis imposes a high risk of complications and increased mortality[1]. PH leads to oesophageal varices and risk of variceal bleeding, ascites formation and systemic vascular dysfunction, including peripheral vasodilation and a hyperdynamic circulation, which is involved in the hepatorenal syndrome and renal failure in cirrhosis [2, 3]. Several factors contribute to the development of PH. Formation of fibrosis in the liver parenchyma causes a mechanic disruption of the liver architecture, and endothelial dysfunction activates contractile properties in the hepatic stellate cell [4, 5]. Also, an increased inflammatory activity in cirrhosis adds to upregulation of innate immune cells and macrophage activation [6, 7]. The degree of macrophage activation can be determined by soluble (s) CD163 and soluble mannose receptor (sMR), which are shed from activated macrophages in the liver [8, 9]. Levels of sCD163 are related to the degree of PH, risk of variceal bleeding, and may be used as a prognostic marker in cirrhosis [9–11].
In liver fibrosis, extensive remodelling of the extracellular matrix such as the fibrillar type III collagens from the interstitial matrix is ongoing [12]. Type III collagen formation and degradation can be evaluated by the serological markers PRO-C3 and C3M respectively [13, 14]. Especially PRO-C3 is found to be associated with fibrosis stage and prognostic for progression of fibrosis [15, 16]. Type IV collagen is primarily found in the basement membrane and it is also subject to extensive remodelling in liver fibrosis. Changes in type IV collagen can be measured by the markers P4NPS7 and C4M being elevated in advanced fibrosis at least in hepatitis B and C [17]. These biomarkers may also be associated with PH, and has the potential to be non-invasive markers of portal hypertension [18]. Markers of fibrogenesis may also be affected by systemic inflammation induced by bacterial translocation [19]. Associations between sCD163 and fibrosis have been demonstrated in patients with cirrhosis due to viral hepatitis [20].
Rifaximin-α is a non-absorbable antibiotic used in the prevention of hepatic encephalopathy [21]. Due to its broad spectrum and effect on gut bacteria, studies have investigated its impact on gut bacteria and possible effects in prevention of bacterial translocation from the gut and thereby prevention of systemic inflammation [22, 23]. The pathophysiological mechanisms of rifaximin-α are still scarcely elucidated.
In this randomized trial (NCT01769040) we aimed to investigate the relations between intestinal decontamination with rifaximin-α and the markers of macrophage activation sCD163 and sMR, in addition to selected neoepitope markers reflecting type III (PRO-C3 and C3M) and IV (P4NPS7, C4M) collagen remodelling in patients with advanced liver cirrhosis. We hypothesized that rifaximin-α treatment would ameliorate both inflammatory and fibrosis markers.
Materials and methods
Patients
In a randomized, placebo controlled and double blind clinical trial fifty-four stable patients with liver cirrhosis and ascites were randomized to rifaximin-α (XIFAXAN, Norgine Denmark A/S, for Alfasigma S.p.A., Bologna, Italy) or placebo for 28 days.
Inclusion criteria were diagnosis of cirrhosis verified by clinical, biochemical, and ultrasound findings; clinical or ultrasound-verified ascites within the last three months; age 18 to 80 years; and portal hypertension with a hepatic venous pressure gradient ≥ 10 mmHg. Exclusion criteria were cardiac or respiratory failure, invasive cancer within the past five years, clinical or biochemical signs of infection, antibiotic treatment 14 days prior to inclusion, overt hepatic encephalopathy, kidney failure with serum creatinine above 200 μmol/l, transfusion-requiring bleeding within one week prior to inclusion, blood hemoglobin level below 5.5 mmol/l, continuous abuse of alcohol with symptoms of withdrawal; or expected survival of less than 3 months. In- and exclusion criteria, as well as basal characteristics of the subjects have been described previously [23, 24]. Patients were invasively characterized with liver vein catheterization and measurement of cardiac output and hepatic venous pressure gradient, along with glomerular filtration rate, assessment of hepatic encephalopathy and biochemistry. All had PH with a Hepatic Venous pressure Gradient (HVPG) of 12 mmHg or higher [24].
Thirty-six patients were randomized to rifaximin-α 550 mg twice daily and eighteen to placebo with identical tablets in shape and size.
During LVC, 25 ml of blood was collected from the femoral artery at baseline and follow-up. Blood was immediately placed on ice; a fraction was centrifuged and both samples of full blood and EDTA plasma were stored at -80 degrees Celsius until analysis.
All patients gave written consent to participation. The trial was approved by the Danish Health Authorities (EudraCT 2012-002890-71), and registered in clinicaltrialsregister.eu on August 16, 2012. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the Scientific Ethics Committee of the Capital Region of Denmark (H-1-2012-078) on August 20, 2012. The Good Clinical Practice unit (GCP unit) of Copenhagen University Hospital served as the external monitor of the trial, and initiated the trial on November 20, 2012.
The trial was further registered in clinicaltrials.gov (NCT1769040).
The first patient was enrolled and randomized on January 29, 2013. Last patient, last visit was performed on December 23, 2015 and the trial was closed as per protocol on December 30, 2015.
sCD163 and sMR assays
Concentrations of sCD163 and sMR were determined by in-house sandwich enzyme-linked immunosorbent assays (ELISA)s using a BEP-2000 ELISA-analyzer (Dade Behring) essentially as previously described [25, 26]. Reference intervals of 0.69 to 3.86 mg/l for sCD163 and 0.10–0.43 mg/L for sMR in healthy individuals have previously been established with the same assays [26, 27].
Both substances are resistant to repeated freezing and thawing, and are stable for prolonged freezing at -80 degrees Celsius.
Assays of PRO-C3, P4NP7S, C3M, and C4M
Neoepitope markers of collagen remodeling (type III and IV collagen, C3M and C4M) and collagen-formation (type III and IV, PRO-C3 and P4NPS7) were measured in plasma by well characterized assays as previously described [13, 14, 28, 29].
In brief, 96-well streptavidin plates were coated with biotinylated synthetic peptides specific for the fragments of interest and incubated for 30minutes at 20°C. 20ul of standard peptide or pre-diluted plasma were added to designated wells followed by addition of peroxidase-conjugated specific monoclonal antibodies and incubated for 1 hour at 20°C or 20 hours at 4°C (depending on the assay). Then, tetramethylbenzidine (TMB) was added to each well and plates were incubated for 15 minutes at 20°C. The enzymatic reaction was stopped by the addition of 0.18M H2SO4 and absorbance was measured at 450 nm with 650nm as a reference. All incubation steps included shaking of 300 rounds per minutes, and each incubation step was followed by five times washing with buffer (20mM Tris, 50mM NaCl, pH 7.2).
Lipopolysaccharide binding protein (LBP)
LBP was measured in ethylene diamine tetra-acetic acid plasma with a commercially available ELISA (Vaiomer SAS, Toulouse, France). Protease activity was assessed by recording absorbance at 405 nm. The minimal detection limit was 3.5 μg/mL.
Statistical analyses
Data was reported as median and range since data did not consequently follow a Gaussian normal distribution. Differences between rifaximin-α and placebo groups at baseline and follow-up were evaluated by Mann-Whitney test of delta values (the difference between follow up and baseline).P-values were calculated two-tailed, with four digits. Subgroup analyses were performed for participants with elevated LBP (n = 37). Spearman rank correlations on baseline values to identify associations between disease severity and biomarkers were performed. Data were handled using MedCalc Statistical Software (v 14.8.1 MedCalc Software bvba, Ostend, Belgium) and GraphPad (Software Prism 6.0.7, La Jolla, CA 92037 USA).
Results
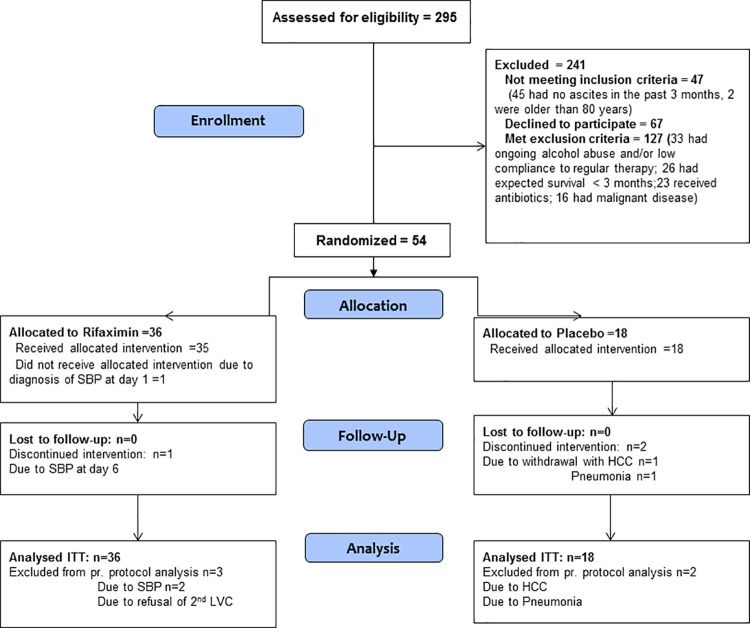
Baseline characteristics and demography in the two groups are shown in Table 1 and reported previously [23, 24]. Trial flow chart is reported previously and in Fig 1 [24].
Table 1. Demographic characteristics in the two groups (rifaximin-α and placebo) [24].
| Rifaximin-α | Placebo | p-value | |
|---|---|---|---|
| Sex (male/female) | 31/5 | 14/4 | N/A |
| Age | 58.5 (33–68) | 52.5 (34–74) | 0.2 |
| Child Class B/C | 27/9 | 17/1 | N/A |
| MELD | 12 (6–25) | 9.5 (6–15) | 0.007 |
| Albumin g/l | 28.5 (21–40) | 32 (24–43) | 0.16 |
| Bilirubin μmol/l | 24 (8–166) | 16.5 (5–40) | 0.002 |
| Creatinine μmol/l | 60 (43–171) | 73 (44–146) | 0.53 |
| Platelets 109/l | 131 (27–562) | 151.5 (56–275) | 0.87 |
| Hemoglobin mmol/l | 7.6 (5.3–9.6) | 7.85 (5–9.8) | 0.36 |
| Alanine transaminase U/l | 25.5 (10–153) | 28 (15–56) | 0.79 |
| Alkaline phosphatase U/l | 121.5 (53–1200) | 146 (47–459) | 0.82 |
Values are given in median and minimum and maximum values, as they do not follow normal distribution, unless otherwise stated. MELD: Modified end stage liver disease score
Fig 1. Trial flow diagram.
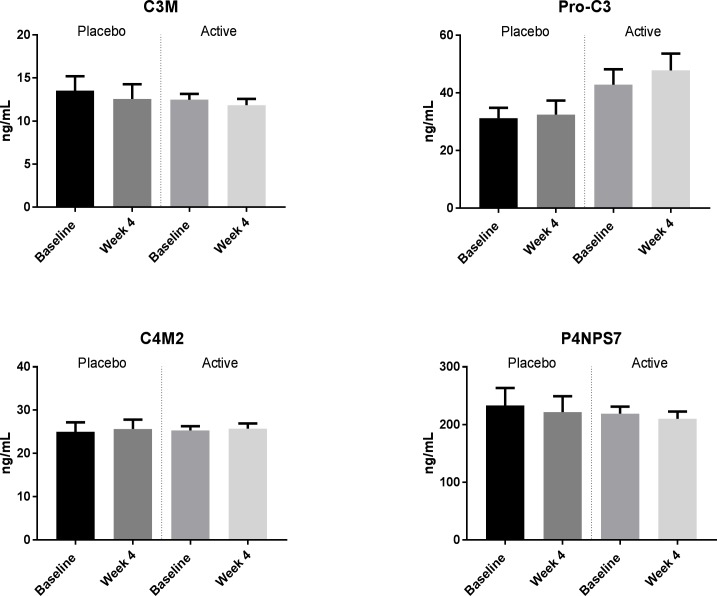
Rifaximin-α had no effect on sCD163 (median (range) sCD163 5.64(2.02 to 10.8) at baseline versus 4.42(1.98 to 8.92) at follow-up in the rifaximin-α group and 4.85 (2.29 to 12.1) at baseline versus 4.32 (1.98 to 12.4) at follow-up in the placebo-group), p = 0.34, and 95% Confidence Interval of difference in median values -2.61 to 1.16; and no effect on sMR, (median (range) sMR 0.56 (0.28 to 1.43) at baseline versus 0.47 (0.37 to 1.08) at follow-up in the rifaximin-α group and 0.59 (0.38 to 1.18) at baseline versus 0.59 (0.34 to 1.2) at follow-up in the placebo group), p = 0.34, and 95% Confidence Interval of difference in median values -0.214 to 0.055; Fig 2.
Fig 2. Levels of sCD163 and sMR in groups (rifaximin-α and placebo) before and after treatment.
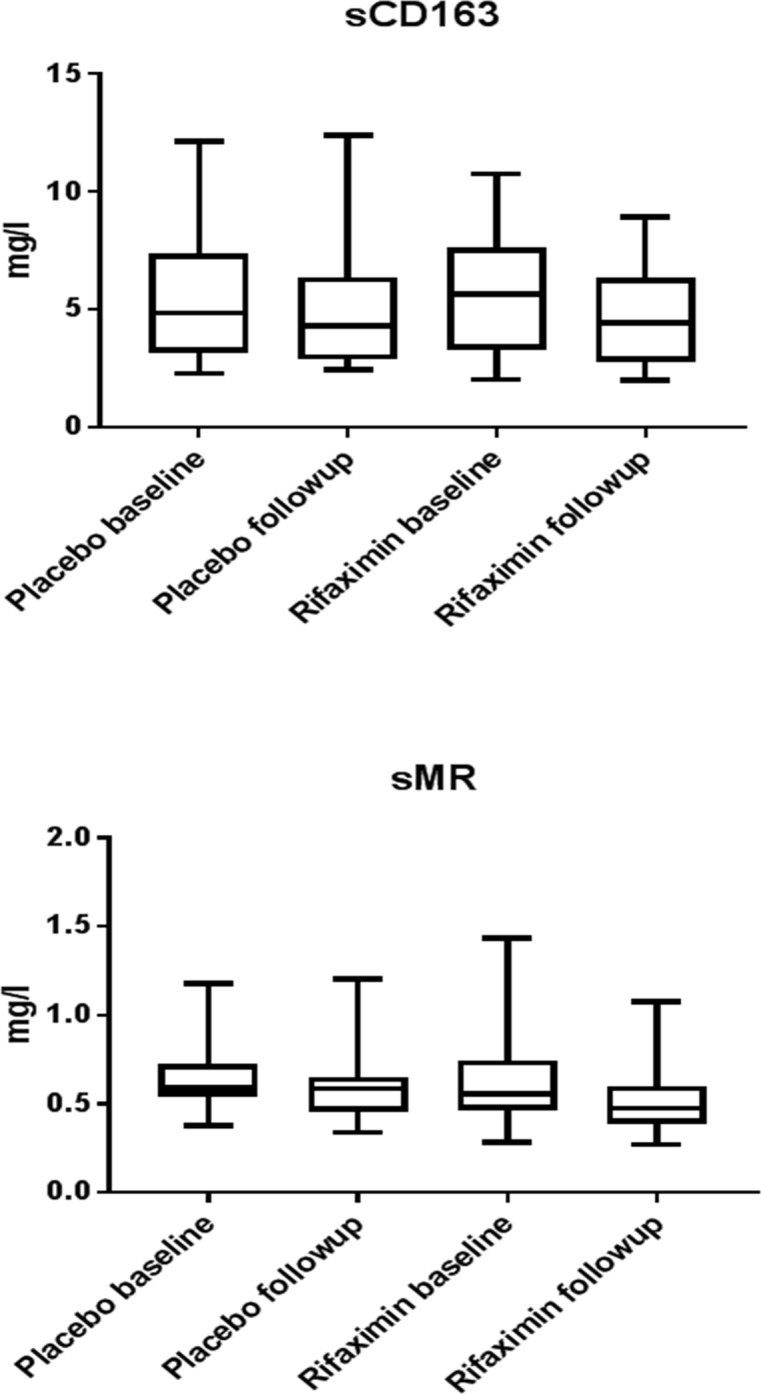
No significant differences in markers of collagen formation and fibrogenesis were observed between the rifaximin-α group and placebo group at baseline or at follow-up, Fig 3, Table 2.
Fig 3. Levels of neoepitope markers of collagen remodeling at baseline and after 4 weeks of treatment.
Table 2. Neoepitope markers of collagen remodeling before and after treatment.
| Placebo (n = 18) | p | Rifaximin-α (n = 18) | p | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Delta | Baseline | Follow-up | Delta | |||
| PRO-C3 (ng/ml) |
26.8 (20.6 – 40.1) | 30.6 (18.9 – 40.5) | -0.05 (-8.9–5.3) | 0.95 | 34.5 (25.6 – 41.1) | 35.9 (27.0 – 51.1) | 3.9 (-0.7–9.1) | 0.49 |
| P4NPS7 (ng/ml) |
182.3 (168.5 – 230.9) | 186.7 (146.7 – 257.7) | -14.1 (34.5–20.4) | 0.94 | 207.4 (186.5 – 246.1) | 179.4 (164.5 – 253.5) | -7.2 (-28.2–11.0) | 0.61 |
| C3M (ng/ml) |
11.5 (9.7 – 13.4) | 10.17 (8.8–14.1) | -0.15 (-2.0–0.97) | 0.63 | 12.5 (10.3 – 14.1) | 11.4 (9.0–13.7) | -0.7 (-2.0–0.5) | 0.53 |
| C4M (ng/ml) |
22.2 (19.38–28.9) | 21.2 (19.1 – 32.3) | 1.4 (-2.1–3.3) | 0.76 | 24.1 (22.7 – 28.4) | 25.1 (20.8 – 30.0) | -0.4 (-1.6–2.3) | 0.87 |
Values of the collagen markers are given as median +/- percentile range 95%.
SCD163 was associated with liver disease severity (MELD score, rho = 0.42, p = 0.001 and Child score, rho = 0,27, p = 0.05). Both sCD163 and sMR was associated with low albumin levels (sCD163 rho = -0.47, p = <0.001 and sMR rho = -0,43, p = 0.001). However, sCD163 and sMR were not associated to portal hypertension or markers of bacterial translocation (for sCD163: HVPG rho = -0.075, p = 0.59; LBP rho = -0.078, p = 0.57 and LPS, rho = -0.042, p = 0.08. For sMR: HPVG, rho = 0.021, p = 0.88, LBP, rho = 0.008, p = 0.95, and LPS, rho = -0.202, p = 0.14). The neoepitope markers were not associated to either disease severity or markers of bacterial translocation, S1 Table.
We found no effect of rifaximin-α on neither sCD163 (p = 0.49), sMR (p = 0.052) nor the neoepitope markers in the subgroup of patients with elevated LBP (n = 37, 25 rifaximin group, 12 placebo group), S2 Table.
Discussion
In this study the effects of rifaximin-α on macrophage activation markers sCD163 and sMR, and neoepitope markers of collagen remodeling were assessed in a randomized trial. We found no effect of rifaximin-α on any of the evaluated markers. However, increased levels of sCD163 were associated to disease severity and low albumin levels, but not to portal hypertension.
The macrophage activation marker sCD163 is associated with liver inflammation and fibrosis in chronic viral hepatitis B and C and is reduced after anti-viral treatment [8, 20, 30]. Further, sCD163 and sMR has been evaluated alone and in combination with fibrosis markers in predictive scores for clinically significant portal hypertension [9, 10], and also as a predictor of decompensation and mortality in cirrhosis [7, 31, 32]. Liver macrophages (Kupffer cells) express toll-like-receptors that respond to lipopolysaccharides (LPS) in blood. Presence of LPS and the LPS-binding protein LBP is supposed to be due to bacterial translocation and increased gut-blood permeability in patients with cirrhosis [33, 34]. In a previous study there was no association between sCD163 and LBP in patients selected for TIPS treatment. Interestingly, sCD163 levels were unchanged despite successful TIPS procedure and significant reductions in LBP levels [35]. A recently published study did contrariwise find an association between liver disease severity expressed as Child score and D’amico cirrhosis stage, and LBP and sCD14 [36]. In this cohort, levels of sCD163 and sMR were much higher in both patients with Child A, B and C, than demonstrated in the present study of 54 patients, and the prognostic value of sMR and sCD163 could not be confirmed. Further longitudinal studies in patients with progressing liver disease and with Child C are needed to explore this area. Basic studies have suggested that rifaximin-α may have a protective effect on bacterial translocation by increasing trans-epithelial resistance in the small intestine [37, 38].
If rifaximin-α prevents bacterial translocation, sCD163, as a marker of macrophage activation is expected to decrease during rifaximin-α treatment. However, our negative efforts to demonstrate such an effect is in line with our previous data from this randomized trial, where we found no effect of rifaximin-α on clinical parameters such as HVPG and cardiac output, no effect on biochemical parameters and inflammation markers (e.g. Tumor necrosis factor alpha and Interleukins 6, 10 and 18), and no effect on the composition of bacterial DNA in blood or stool [23, 24].
Previous studies have evaluated the significance of several neoepitope collagen markers as prognostic factors for portal hypertension in cirrhosis [16, 39]. Both C3M, C4M, PRO-C3 and P4NPS7 were reported to be associated with HVPG alone and in combination with the MELD score. These studies examined collagen markers in patients with varying severity of cirrhosis with MELD score in a range from 5 to 25. In the present study only P4NPS7 and C4M2 were significantly correlated to LPS, and none of the other markers of bacterial translocation or disease severity. We evaluated a homogenous group of patients with stable, but decompensated cirrhosis with a median MELD score of 12 (IQ range 7–16). Study participants were selected after presence of portal hypertension and the severely ill patients were excluded, which clearly narrowed the patient material to a highly selected group. This may explain the lack of association between neoepitope markers and disease severity in the present study. The pathophysiological mechanisms of rifaximin-α have been evaluated in several studies [40, 41]. Several factors may influence the lacking impact of rifaximin-α on collagen markers and fibrogenesis.
Patients were treated with rifaximin-α for 28 days and as previously reported we found no effect of rifaximin-α on systemic inflammation or bacterial composition in the gut, which indicates that the link between fibrogenesis and systemic inflammation is not affected by rifaximin-α. Also, in this patient cohort with stable but severe liver disease, the neo formation of fibrosis may have little influence on clinical and biochemical appearance of disease.
The beneficial effect of rifaximin-α in hepatic encephalopathy has been demonstrated in several studies, irrespective its unclear mechanism of action [21, 42]. In this randomized clinical trial of 54 patients with stable liver cirrhosis and ascites, we did not find a beneficial effect of rifaximin outside the current indication of overt hepatic encephalopathy. Future insight into the impact of bacterial translocation and leaky gut in cirrhosis on mechanisms of systemic inflammation is needed to evaluate indications for rifaximin-α outside hepatic encephalopathy and search for other treatment options in systemic inflammation. Also, further investigations into the possible effects of rifaximin on epithelial resistance and gut barrier functions as well as effects on fibrogenesis and fibrosis activity in liver disease is highly warranted.
This study was conducted as a double blind, placebo controlled randomized trial. The methodology may vouch for robust systematically collected data after applicable standards.
The study is of limited size though, and future trials may address selected areas of importance for systemic inflammation in the search for clinically relevant outcomes. Also assessment of drugs with different pharmacodynamics and targets may be applied in trials on systemic inflammation.
In conclusion, rifaximin-α treatment has no significant impact on macrophage activation in the liver as well as no effect on collagen markers. The effect of rifaximin-α on factors in the systemic inflammatory response theory is limited. Further studies to clarify both effects of rifaximin-α and the impact of the activated inflammation cascade in cirrhosis are in demand.
Supporting information
(DOC)
(DOCX)
(DOCX)
(PDF)
(PDF)
(PDF)
(DOC)
(XLSX)
Acknowledgments
The following participated in finding and evaluating patients eligible for screening:
Lise Lotte Gluud, Lone Madsen, Camilla Nøjgård, Sanne Dam-Larsen, Thomas Blixt, Karin Grønbæk, Flemming Tofteng, Srdan Novovic, Marianne Vester Andersen, Anne Wilkens Knudsen, Ida Vind, Astrid Naver, Niels Johansen, Stine Sloth, Mille Bækdal Nielsen, and Signe Wiese; all Gastro Unit, Medical Division, Copenhagen University Hospital Hvidovre.
Abbreviations
- HVPG
Hepatic venous pressure gradient
- LVC
Liver Vein Catheterization
- LPS
Lipopolysaccharide
- LBP
Lipopolysaccharide-binding protein
- MELD
Modified Endstage Liver Disease model
- PH
Portal Hypertension
- sCD163
soluble CD163
- sMR
soluble Mannose Receptor
Data Availability
Data are contained in the paper as Supporting Information files.
Funding Statement
This trial was funded by The Research Foundation of The Capital Region of Denmark, Novo Nordisk Foundation (NNF13OC0006561), Aase & Ejnar Danielsens Foundation, Amager and Hvidovre Hospital Research Foundation. The funders provided support in the form of salaries for authors (NK and JSP), but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. Norgine Denmark A/S delivered drugs (XIFAXAN, Norgine Denmark A/S, for Alfasigma S.p.A., Bologna, Italy) and the placebo as an unrestricted grant. This funder did not provide support in the form of salaries, and had no additional role in study design, data collection and analysis, decision to publish or preparation of the manuscript. Nordic Bioscience provided support in the form of salaries for authors NSG, DJL, MJN and MAK, and analyzed neoepitope markers free of charge. NSG, DJL, MJN, MAK did not have any role in the study design or data collection, but performed analysis, and participated in preparing the manuscript, writing discussion and revision of the manuscript.
References
- 1.Cardenas A, Gines P. Portal hypertension. Current opinion in gastroenterology 2009;25:195–201. [DOI] [PubMed] [Google Scholar]
- 2.Mindikoglu AL, Pappas SC. New Developments in Hepatorenal Syndrome. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piano S, Tonon M, Angeli P. Management of ascites and hepatorenal syndrome. Hepatology international 2017. [DOI] [PubMed] [Google Scholar]
- 4.Sethasine S, Jain D, Groszmann RJ, Garcia-Tsao G. Quantitative histological-hemodynamic correlations in cirrhosis. Hepatology 2012;55:1146–1153. 10.1002/hep.24805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iwakiri Y. Endothelial dysfunction in the regulation of cirrhosis and portal hypertension. Liver international: official journal of the International Association for the Study of the Liver 2012;32:199–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gandoura S, Weiss E, Rautou PE, Fasseu M, Gustot T, Lemoine F, et al. Gene- and exon-expression profiling reveals an extensive LPS-induced response in immune cells in patients with cirrhosis. Journal of hepatology 2013;58:936–948. 10.1016/j.jhep.2012.12.025 [DOI] [PubMed] [Google Scholar]
- 7.Gronbaek H, Rodgaard-Hansen S, Aagaard NK, Arroyo V, Moestrup SK, Garcia E, et al. Macrophage activation markers predict mortality in patients with liver cirrhosis without or with acute-on-chronic liver failure (ACLF). J Hepatol 2016;64:813–822. 10.1016/j.jhep.2015.11.021 [DOI] [PubMed] [Google Scholar]
- 8.Laursen TL, Wong GL, Kazankov K, Sandahl T, Moller HJ, Hamilton-Dutoit S, et al. Soluble CD163 and mannose receptor associate with chronic hepatitis B activity and fibrosis and decline with treatment. Journal of gastroenterology and hepatology 2017. [DOI] [PubMed] [Google Scholar]
- 9.Sandahl TD, McGrail R, Moller HJ, Reverter E, Moller S, Turon F, et al. The macrophage activation marker sCD163 combined with markers of the Enhanced Liver Fibrosis (ELF) score predicts clinically significant portal hypertension in patients with cirrhosis. Aliment Pharmacol Ther 2016;43:1222–1231. 10.1111/apt.13618 [DOI] [PubMed] [Google Scholar]
- 10.Gronbaek H, Sandahl TD, Mortensen C, Vilstrup H, Moller HJ, Moller S. Soluble CD163, a marker of Kupffer cell activation, is related to portal hypertension in patients with liver cirrhosis. Aliment Pharmacol Ther 2012;36:173–180. 10.1111/j.1365-2036.2012.05134.x [DOI] [PubMed] [Google Scholar]
- 11.Waidmann O, Brunner F, Herrmann E, Zeuzem S, Piiper A, Kronenberger B. Macrophage activation is a prognostic parameter for variceal bleeding and overall survival in patients with liver cirrhosis. J Hepatol 2013;58:956–961. 10.1016/j.jhep.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 12.Kirimlioglu H, Kirimlioglu V, Yilmaz S. Expression of matrix metalloproteinases 2 and 9 in donor liver, cirrhotic liver, and acute rejection after human liver transplantation. Transplantation proceedings 2008;40:3574–3577. 10.1016/j.transproceed.2008.09.033 [DOI] [PubMed] [Google Scholar]
- 13.Barascuk N, Veidal SS, Larsen L, Larsen DV, Larsen MR, Wang J, et al. A novel assay for extracellular matrix remodeling associated with liver fibrosis: An enzyme-linked immunosorbent assay (ELISA) for a MMP-9 proteolytically revealed neo-epitope of type III collagen. Clin Biochem 2010;43:899–904. 10.1016/j.clinbiochem.2010.03.012 [DOI] [PubMed] [Google Scholar]
- 14.Nielsen MJ, Nedergaard AF, Sun S, Veidal SS, Larsen L, Zheng Q, et al. The neo-epitope specific PRO-C3 ELISA measures true formation of type III collagen associated with liver and muscle parameters. American journal of translational research 2013;5:303–315. [PMC free article] [PubMed] [Google Scholar]
- 15.Karsdal MA, Henriksen K, Nielsen MJ, Byrjalsen I, Leeming DJ, Gardner S, et al. Fibrogenesis assessed by serological type III collagen formation identifies patients with progressive liver fibrosis and responders to a potential antifibrotic therapy. American journal of physiology Gastrointestinal and liver physiology 2016;311:G1009–G1017. 10.1152/ajpgi.00283.2016 [DOI] [PubMed] [Google Scholar]
- 16.Jansen C, Leeming DJ, Mandorfer M, Byrjalsen I, Schierwagen R, Schwabl P, et al. PRO-C3-levels in patients with HIV/HCV-Co-infection reflect fibrosis stage and degree of portal hypertension. PloS one 2014;9:e108544 10.1371/journal.pone.0108544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nielsen MJ, Kazankov K, Leeming DJ, Karsdal MA, Krag A, Barrera F, et al. Markers of Collagen Remodeling Detect Clinically Significant Fibrosis in Chronic Hepatitis C Patients. PLoS One 2015;10:e0137302 10.1371/journal.pone.0137302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veidal SS, Karsdal MA, Vassiliadis E, Nawrocki A, Larsen MR, Nguyen QH, et al. MMP mediated degradation of type VI collagen is highly associated with liver fibrosis—identification and validation of a novel biochemical marker assay. PloS one 2011;6:e24753 10.1371/journal.pone.0024753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arroyo V, Garcia-Martinez R, Salvatella X. Human serum albumin, systemic inflammation, and cirrhosis. Journal of hepatology 2014;61:396–407. 10.1016/j.jhep.2014.04.012 [DOI] [PubMed] [Google Scholar]
- 20.Kazankov K, Barrera F, Moller HJ, Bibby BM, Vilstrup H, George J, et al. Soluble CD163, a macrophage activation marker, is independently associated with fibrosis in patients with chronic viral hepatitis B and C. Hepatology 2014;60:521–530. 10.1002/hep.27129 [DOI] [PubMed] [Google Scholar]
- 21.Bass NM, Mullen KD, Sanyal A, Poordad F, Neff G, Leevy CB, et al. Rifaximin treatment in hepatic encephalopathy. The New England journal of medicine 2010;362:1071–1081. 10.1056/NEJMoa0907893 [DOI] [PubMed] [Google Scholar]
- 22.Bajaj JS, Heuman DM, Sanyal AJ, Hylemon PB, Sterling RK, Stravitz RT, et al. Modulation of the metabiome by rifaximin in patients with cirrhosis and minimal hepatic encephalopathy. PloS one 2013;8:e60042 10.1371/journal.pone.0060042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kimer N, Pedersen JS, Tavenier J, Christensen JE, Busk TM, Hobolth L, et al. Rifaximin has minor effects on bacterial composition, inflammation and bacterial translocation in cirrhosis; A randomized trial. Journal of gastroenterology and hepatology 2017. [DOI] [PubMed] [Google Scholar]
- 24.Kimer N, Pedersen JS, Busk TM, Gluud LL, Hobolth L, Krag A, et al. Rifaximin has no effect on hemodynamics in decompensated cirrhosis: A randomized, double-blind, placebo-controlled trial. Hepatology 2017;65:592–603. 10.1002/hep.28898 [DOI] [PubMed] [Google Scholar]
- 25.Moller HJ, Hald K, Moestrup SK. Characterization of an enzyme-linked immunosorbent assay for soluble CD163. Scandinavian journal of clinical and laboratory investigation 2002;62:293–299. [DOI] [PubMed] [Google Scholar]
- 26.Rodgaard-Hansen S, Rafique A, Christensen PA, Maniecki MB, Sandahl TD, Nexo E, et al. A soluble form of the macrophage-related mannose receptor (MR/CD206) is present in human serum and elevated in critical illness. Clin Chem Lab Med 2014;52:453–461. 10.1515/cclm-2013-0451 [DOI] [PubMed] [Google Scholar]
- 27.Moller HJ. Soluble CD163. Scandinavian journal of clinical and laboratory investigation 2012;72:1–13. 10.3109/00365513.2011.626868 [DOI] [PubMed] [Google Scholar]
- 28.Leeming DJ, Nielsen MJ, Dai Y, Veidal SS, Vassiliadis E, Zhang C, et al. Enzyme-linked immunosorbent serum assay specific for the 7S domain of Collagen Type IV (P4NP 7S): A marker related to the extracellular matrix remodeling during liver fibrogenesis. Hepatology research: the official journal of the Japan Society of Hepatology 2012;42:482–493. [DOI] [PubMed] [Google Scholar]
- 29.Sand JM, Larsen L, Hogaboam C, Martinez F, Han M, Rossel Larsen M, et al. MMP mediated degradation of type IV collagen alpha 1 and alpha 3 chains reflects basement membrane remodeling in experimental and clinical fibrosis—validation of two novel biomarker assays. PloS one 2013;8:e84934 10.1371/journal.pone.0084934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dultz G, Gerber L, Farnik H, Berger A, Vermehren J, Pleli T, et al. Soluble CD163 is an indicator of liver inflammation and fibrosis in patients chronically infected with the hepatitis B virus. Journal of viral hepatitis 2014. [DOI] [PubMed] [Google Scholar]
- 31.Rode A, Nicoll A, Moller HJ, Lim L, Angus PW, Kronborg I, et al. Hepatic macrophage activation predicts clinical decompensation in chronic liver disease. Gut 2013;62:1231–1232. 10.1136/gutjnl-2012-304135 [DOI] [PubMed] [Google Scholar]
- 32.Sandahl TD, Stoy SH, Laursen TL, Rodgaard-Hansen S, Moller HJ, Moller S, et al. The soluble mannose receptor (sMR) is elevated in alcoholic liver disease and associated with disease severity, portal hypertension, and mortality in cirrhosis patients. PLoS One 2017;12:e0189345 10.1371/journal.pone.0189345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paik YH, Schwabe RF, Bataller R, Russo MP, Jobin C, Brenner DA. Toll-like receptor 4 mediates inflammatory signaling by bacterial lipopolysaccharide in human hepatic stellate cells. Hepatology 2003;37:1043–1055. 10.1053/jhep.2003.50182 [DOI] [PubMed] [Google Scholar]
- 34.Wiest R, Lawson M, Geuking M. Pathological bacterial translocation in liver cirrhosis. J Hepatol 2014;60:197–209. 10.1016/j.jhep.2013.07.044 [DOI] [PubMed] [Google Scholar]
- 35.Holland-Fischer P, Gronbaek H, Sandahl TD, Moestrup SK, Riggio O, Ridola L, et al. Kupffer cells are activated in cirrhotic portal hypertension and not normalised by TIPS. Gut 2011;60:1389–1393. 10.1136/gut.2010.234542 [DOI] [PubMed] [Google Scholar]
- 36.Rainer F, Horvath A, Sandahl TD, Leber B, Schmerboeck B, Blesl A, et al. Soluble CD163 and soluble mannose receptor predict survival and decompensation in patients with liver cirrhosis, and correlate with gut permeability and bacterial translocation. Alimentary pharmacology & therapeutics 2018;47:657–664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Esposito G, Nobile N, Gigli S, Seguella L, Pesce M, d'Alessandro A, et al. Rifaximin Improves Clostridium difficile Toxin A-Induced Toxicity in Caco-2 Cells by the PXR-Dependent TLR4/MyD88/NF-kappaB Pathway. Front Pharmacol 2016;7:120 10.3389/fphar.2016.00120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wan YC, Li T, Han YD, Zhang HY, Lin H, Zhang B. Effect of Pregnane Xenobiotic Receptor Activation on Inflammatory Bowel Disease Treated with Rifaximin. J Biol Regul Homeost Agents 2015;29:401–410. [PubMed] [Google Scholar]
- 39.Leeming DJ, Karsdal MA, Byrjalsen I, Bendtsen F, Trebicka J, Nielsen MJ, et al. Novel serological neo-epitope markers of extracellular matrix proteins for the detection of portal hypertension. Alimentary pharmacology & therapeutics 2013;38:1086–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kalambokis GN, Tsianos EV. Rifaximin reduces endotoxemia and improves liver function and disease severity in patients with decompensated cirrhosis. Hepatology 2012;55:655–656. 10.1002/hep.24751 [DOI] [PubMed] [Google Scholar]
- 41.Bajaj JS. Review article: potential mechanisms of action of rifaximin in the management of hepatic encephalopathy and other complications of cirrhosis. Alimentary pharmacology & therapeutics 2016;43 Suppl 1:11–26. [DOI] [PubMed] [Google Scholar]
- 42.Kimer N, Krag A, Moller S, Bendtsen F, Gluud LL. Systematic review with meta-analysis: the effects of rifaximin in hepatic encephalopathy. Alimentary pharmacology & therapeutics 2014;40:123–132. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(DOCX)
(PDF)
(PDF)
(PDF)
(DOC)
(XLSX)
Data Availability Statement
Data are contained in the paper as Supporting Information files.