Abstract
Objective:
Mechanical neck pain (NP) with referred pain to upper limb is a common problem and often leads to functional impairment of common activities of daily living. The present study is undertaken to study and compare the effect of gross myofascial release (MFR) of upper limb and neck alone with conventional physiotherapy against only conventional treatment in subjects with mechanical NP referred to upper limb in terms of cervical endurance, pain, range of motion, and function.
Methods:
Design: This was a experimental study; a total of 40 subjects clinically diagnosed with mechanical NP along with referred pain between the age group of 20 and 50 years. Intervention: Control group was given conventional treatment of hot moist pack, TENS, and stretching and strengthening exercise, and experimental group was given gross MFR of the neck and upper limb in addition to conventional therapy. Treatment was given for 6 consecutive days. Outcome measures used were pressure biofeedback to measure cervical endurance, goniometer for cervical ROM, Northwick Park NP questionnaire, and disabilities of arm, shoulder, and hand questionnaire.
Results:
Statistically significant change was present for pain, cervical flexure endurance, ROM, and functional abilities with P < 0.05 for both the groups except for neck flexor endurance in control group.
Conclusion:
Gross MFR of upper limb and neck is an effective technique for subjects with mechanical NP and has a faster rate of improvement.
Keywords: Cervical flexor endurance, gross myofascial release technique, mechanical neck pain, myofascial release, referred pain
Introduction
Neck pain (NP) is considered to occur insidiously[1] and is multifactorial in origin. It includes one or more of the following causes such as poor posture, anxiety, depression, neck strain, and sporting or occupational activities.[2,3] NP appears to be more persistent than low back pain, and it is second only to lumbar pain as the causal factor for time missed from work.[13] In one of the systematic reviews for the incidence of NP in populations around the world, the point prevalence was from 5.9% to 38.7%. The incidence of NP is higher in women (15%) than men (9%). Women have the highest incidence at the age of 45 and men at the age of 60.[2] High prevalence of NP was reported in desk job workers. 1-year prevalence of NP and work-related NP was reported as 43.3% and 28.3%, respectively.[4]
Based on the duration of NP, the International Association for the Study of Pain proposed a classification as: Acute NP which usually lasts <7 days, subacute NP lasting for more than 7 days but <3 months, and chronic NP with the duration of 3 months or more.[5]
NP can be of two types: Specific NP and nonspecific or mechanical NP. Mechanical NP is defined as generalized NP provoked by sustained neck postures, neck movement, and pain on palpation of cervical musculature without pathologies. Movement of the neck feels restricted and moving the neck may make the pain worse. It develops in the neck and may spread to the shoulder, arm, or base of the skull.[6]
The mechanical NP may spread down to an arm and even into the fingers giving a sensation of “pins and needles” in part of an arm or hand, crunching sound when bending or turning the neck, stiff neck, restricted movement of the neck, and pain when moving the neck. This referred pain may be due to two factors. First, there is irritation of the nerve going to arm from the spinal cord in the neck.[7,8] Mechanical loading of the upper limbs may cause NP as a direct consequence of increasing the mechanical loading to the articular and ligamentous structures of the neck or by creating protective spasm.[9] This may result in pain, decreased range of motion, and functioning.[10] Second, the upper limb is further mechanically attached to the neck through the brachial plexus which extends from the neck into the upper limb. A survey which was done on mechanical NP patients found that 67% of patients presented with associated upper limb pain without neurological deficit.[11]
Assessment of mechanical NP with referred pain to upper limb is based mainly on clinical findings which include history, symptomatology, and objective assessment. It is done by assessing for pain, cervical range of motion, and functional disability along with special tests such as craniocervical flexion test, deep neck flexor endurance test, upper limb tension test, Spurling’s test, and distraction test. Clinically, the patients with non-specific NP report problems with upper limb function. Literature suggests that baseline NP/disability measured using Northwick park neck pain questionnaire (NPQ) and baseline upper limb disability which is measured using disability of the arm, shoulder, and hand (DASH) are both valid and reliable tools in measuring upper limb disability in non-specific NP.[12-17] Transcutaneous electrical nerve stimulation (TENS) is considered to be simple, non-invasive analgesic technique that is used extensively in health-care settings by physiotherapists.[18,19] To be of benefit, a stretching and strengthening exercise program should concentrate on the musculature of the cervical, shoulder-thoracic area, or both.[5,13,19-23]
One of the basic gross myofascial release (MFR) techniques involves gross stretch of the upper quarter called as the “arm pull technique” and gross stretch of posterior cervical spine. These techniques are over an advantage in reducing muscle soreness, relieving joint stress, decreasing neuromuscular hypertonicity, increasing extensibility of musculotendinous junction, improving neuromuscular efficiency, and correcting muscle imbalance along with the maintenance of normal functional muscular length.[24]
Gross MFR with upper quarter pull techniques has been assessed for its effectiveness in a previous study done on fascial release effects and proved to improve or restore normal tissue mobility and function and to decrease pain perception.[25] Another study was done using ultrasonography where gross MFR was given in chronic non-specific NP and was found to be effective.[26]
Two more studies were done, one on non-specific NP referred to upper limb and other on cervical radiculopathy using gross MFR with upper quarter pull technique.[18,27] The effects were assessed and concluded as an effective technique. However, both the studies were non-randomized clinical trials with small sample size and with no objective outcome measures.
Hence, the literature review suggests paucity in a high-quality controlled studies using gross MFR with upper quarter pull technique been used in mechanical NP patients with referred pain to upper limb. Hence, this study was undertaken with the aim to find the effect of gross MFR of upper limb and neck in subjects with mechanical NP along with referred pain to unilateral upper limb.
Methods
The study design was a double-blinded randomized controlled trial, where the assessor and the therapist were blinded to the groups. The study was conducted in Physiotherapy Outpatient Department of KLE Hospital, Belagavi, Karnataka, India, on local residents restricted to Belgaum city. The Ethical Committee approval was obtained from Institutional Ethical Review Committee, and written informed consents were also taken from all participants. All subjects clinically diagnosed with mechanical NP along with referred pain to unilateral upper limb were screened based on the following criteria.
Inclusion criteria
The following criteria were included in the study:
Subjects clinically diagnosed with mechanical NP along with referred pain to unilateral upper limb between the age group of 20 and 50 years of both genders.
Willingness to participate in the study.
Exclusion criteria
The following criteria were excluded from the study:
Specific causes of NP (conditions with neurological involvement such as myelopathy with weakness, numbness and sensory loss, cervical disc prolapse, and cervical spinal stenosis)
Previous neck and upper limb surgery.
History of cervical trauma (whiplash disorder), fractures, dislocations.
History of congenital torticollis.
Frequent migraine.
Carcinoma.
Pregnancy.
Sample size
The sample size was 40
SD of group A (S1) = 10.68
SD of group B (S2) = 9.97
Formula:
where s = S1 + S2/2
Hence, n = 20 in each group, under 5% alpha error, 80% power, with d = 9.0540.
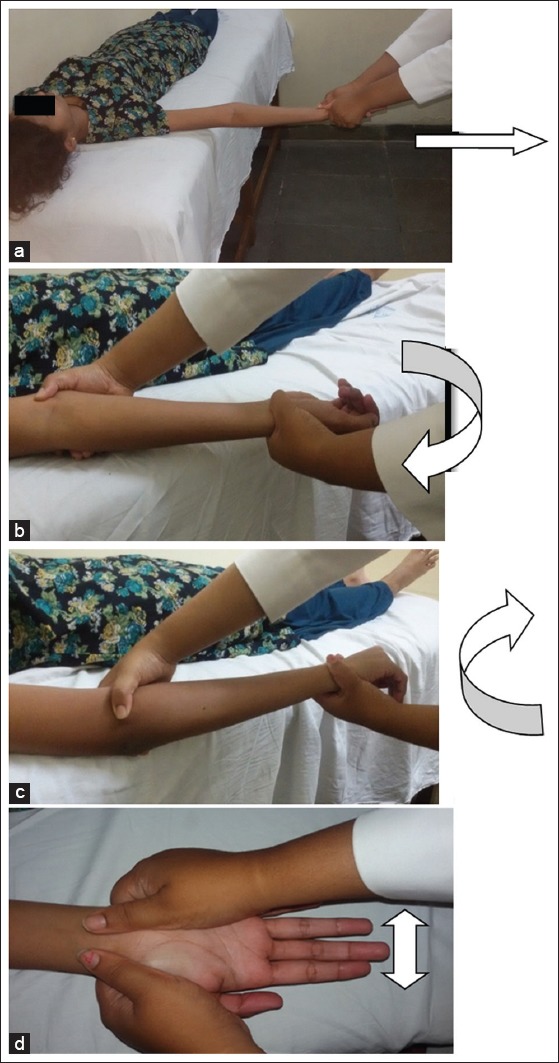
Before the commencement of the procedure, written informed consent was obtained from the subjects. The purpose of the study was explained following which demographic data were collected from the subjects. The setting where the subjects were recruited was physiotherapy OPD, tertiary health care setup, Belagavi, India. The assessment was done at the beginning (1st day) and at the end (6th day) of the protocol so as to find the significant changes. Subjects were randomly allotted to two groups using the envelope method.
Group A: Experimental group.
Group B: Control group.
Procedure
Step 1: A brief demographic data were noted from the subjects.
Step 2: Pre- and post-assessment were done using four outcome measures: Cervical flexor endurance (CFE) score.[28] [Figure 1], cervical ROM, NPQ,[29] and DASH.[12,30]
Step 3: Using envelope method, the subjects were segregated into two groups, i.e. Group A - experimental group and Group B - control group.
Step 4: Control group: Hot moist pack (HMP) was applied for the duration of 20 min with patient in sitting and head rested on the forearm and table. It was followed by TENS for 15 min. Conventional TENS, rectangular waveform with pulse frequency of 10–200 Hz, pulse width 100–250 µs, and two electrodes given along the referred pain with the intensity as tolerated by the subject. Subjects were advised home program of stretching and strengthening exercises of cervical musculature which are stated below and ergonomic advice was given.
Figure 1.

Measuring cervical flexor endurance
Stretching and strengthening exercise protocol [Figures 2 and 3]
Figure 2.

Stretching exercise-Home exercise protocol
Figure 3.

Strengthening exercise-Home exercise protocol
Active ROM exercises
Subjects in sitting position actively performed neck rotations and side bending on both sides, forward bending, neck extension, and shoulder rolls. These were repeated 5 times.
Neck isometrics
In sitting position, subject performed an isometric push against the hand to strengthen the neck. Subject was told to hold the left palm against the left side of the head. Push the left hand against the head while also pushing your head toward your left hand at about half strength. Hold for 30 s. The same was repeated with the right hand on the right side of the head and using either hand, with the back of the head, and the forehead. This was repeated 5 times.
Neck retraction exercise
While lying faceup or sitting, bring the head straight back, without bending the neck. Hold for 10 s. Then, return to neutral. Repeat 10 times.
Neck stretches
Subject in sitting position is told to reach the right arm over the head so that palm is on top of the skull with fingers resting just above the left ear. Along with light fingertip pressure, the weight of the arm is allowed to gently bend the head toward the right shoulder with shoulders relaxed. Subject is looking forward. The position is held for 30 s. Then, the fingers are moved toward the back left corner of your skull, this time allow your head to bend forward and to the right, about 45° in front of your shoulder, and held for 30 s. Then, fingers are placed at the back of the skull and head is gently pulled straight forward, toward the chest, held for 30 s. Hands switched and the stretches are repeated in reverse order: Pull forward, then 45° in front of the left shoulder, and directly over the left shoulder. This was repeated 5 times.
Experimental group
Subjects in the experimental group were given HMP on the neck region for 15 min after which they underwent a manual intervention of gross MFR technique for posterior cervical musculature[26] and gross stretch of upper quarter: Arm pull[26] for the duration of 10–15 min.
Gross stretch of posterior cervical musculature [Figure 4]
Figure 4.

(a-c) Gross stretch of posterior cervical musculature
Both hands were placed at the base of the occiput and stretching up toward the top of the subject’s head. The thumbs were rested slightly on the lateral neck musculature. The other hand was over the upper thoracic spine. Gross stretch was performed by stretching upward at the base of the occiput and downward at the upper thoracic spine.
The initial traction should just counterbalance the weight of the subject’s head. Stretch was hold for 90 s until release and was stretched again by increasing traction. With each release, capital extension should increase. This release sequence was repeated until an end feel was reached.
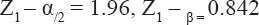
Gross stretch of the upper quarter: Arm pull [Figure 5]
Figure 5.
(a-d) Gross stretch of upper quarter: Arm pull
The arm pull is a straight plan stretch parallel to the floor. Arm was in a neutral position as the initial stretch was applied. With the subject in supine, therapist comfortably grasped the subject’s hand and kept his shoulders relaxed and moved toward the subject’s feet until the elbow was in full extension. Most of the weight was placed on the back foot, and therapist stood slightly backward to apply the initial stretch on the subject’s entire upper extremity. The line of stretch was parallel to the floor and down toward the subject’s feet in line with the deltoid fibers. Only enough traction was used to counterbalance the weight of the patient’s arm. Stretch was hold until the fibers were released, and then, stretch was given again by increasing traction. This sequence was repeated until an end feel was reached. The subject’s elbow must be in full extension during the arm pull.
Traction was maintained and forearm was rotated into supination until restriction was felt. Traction was maintained and stretched again by increasing supination. If full supination was not possible, subject’s forearm returned to neutral position and palm was stretched by placing one hand on thenar eminence and the other on hypothenar eminence. Subject’s arm was spread laterally until tightness or restriction was felt. This position was held, released, and stretched again.
Gross stretch of posterior cervical musculature [Figure 4] is prepended before gross stretch of upper quarter: Arm Pull [Figure 5]
Dosage
One session per day for 6 days for both the groups was delivered by an experienced physiotherapy practitioner. This was followed by TENS with a frequency ranging from 10 to 200 Hz and pulse width 100–250 µs for a maximum duration of 20 min. During the therapy, the subject was instructed to lie in the supine position stay relaxed not sleep during procedure. The subjects were also instructed to report the therapist if any discomfort or pain was felt during the procedure.
Consort Chart
Data analysis
The data of the study were statistically analyzed using SPSS software version 20.0. Statistical analysis was performed using independent t-test and dependent t-test. A significance level of P < 0.05 was used for all statistical analyses. All parameters for day 1 and day 6 scores followed a normal distribution. Therefore, the parametric tests were applied. The pre- and post-comparison within the group was done using dependent t-test and between the groups was done by independent t-test.
Results
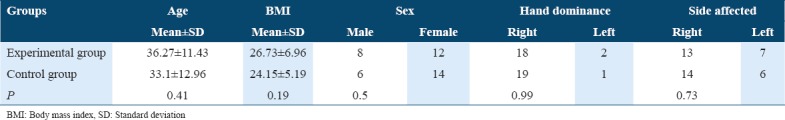
A total of 40 patients were participated in this study. Table 1 summarizes their general characteristics.
Table 1.
Demographic distribution of parameters in two study groups
CFE score (mmHg)
There was a significant improvement in CFE for experimental group with P = 0.001 for within-group analysis, but there was no significant improvement for control group with P = 0.30 [Tables 2 and 3]. Furthermore, for between-group analysis, there was no significant difference for pre-intervention score, while post-intervention score and the mean difference scores resulted in statistically significant values (P = 0.0005 and P = 0.0001) [Table 4].
Table 2.
Pre–post comparison for experimental group#
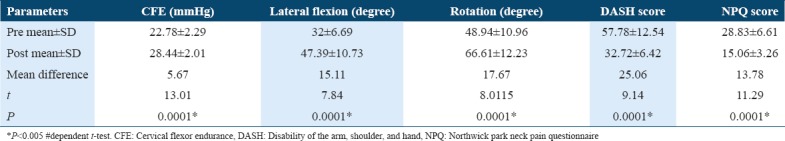
Table 3.
Pre–post comparison for control group#
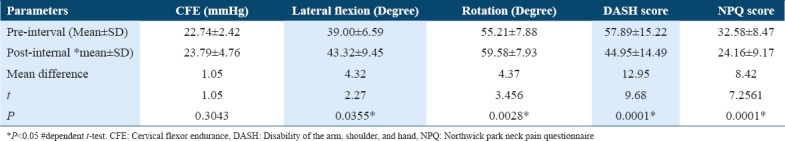
Table 4.
Between-group comparison of experimental and control groups#
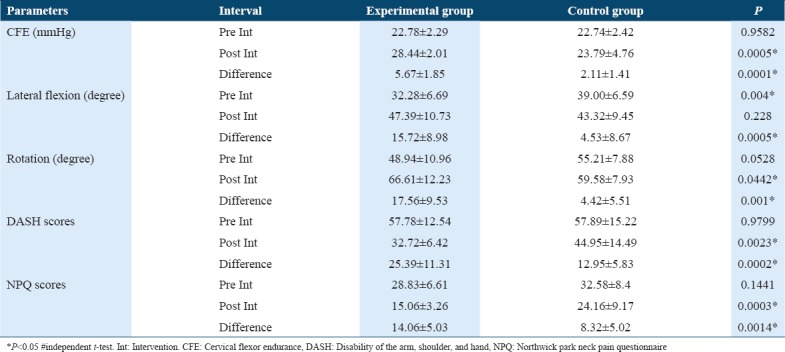
ROM of cervical spine
Lateral flexion
For within-group analysis, there was significant improvement in lateral flexion range of motion for experimental group (P = 0.0001) [Table 2] and also for control group (P = 0.0355) [Table 3]. For between-group analysis, it showed a significant difference for pre-intervention score and mean difference scores (P = 0.004, P = 0.0005), while post-intervention scores were not statistically significant (P = 0.228) [Table 4].
Rotation
For within-group analysis, significant improvement was present in rotation range for experimental group (P = 0.0001) [Table 2] and control group (P = 0.0028) [Table 3]. The between-group comparison for both the study groups did not show significant difference for pre-intervention score (P = 0.0528), while post-intervention score and the mean difference score indicate statistically significant values (P = 0.0442 and P = 0.001) [Table 4].
DASH scores
For within-group analysis, there was a significant improvement in DASH scores for experimental group (P = 0.0001) [Table 2] and control group (P = 0.0001) [Table 3]. The between-group comparison for both the study groups did not show a significant difference for pre-intervention score (P = 0.9799), while post-intervention score and the mean difference score showed statistically significant values (P = 0.0023 and P = 0.0002) [Table 4].
NPQ scores
Within-group analysis showed significant improvement in NPQ scores for experimental group (P = 0.0001) [Table 2] and control group (P = 0.0001) [Table 3]. The between-group comparison for both the study groups did not show significant difference for pre-intervention score (P = 0.1441), while post-intervention score and the mean difference score revealed statistically significant values (P = 0.0003 and P = 0.0014) [Table 4].
Overall, the gross MFR of neck and quarter arm pull technique was more beneficial than the control group in terms of CFE, cervical ROM, NPQ, and DASH, although both the treatment groups proved to be effective in treating mechanical NP referred to unilateral upper limb except that the control group did not show any significant improvement in CFE.
Discussion
The present randomized controlled trial was done to study the effect of MFR of the upper limb and neck in subjects with mechanical NP with referred pain to unilateral upper limb.
The results from the statistical analysis of the present study support the alternate hypothesis that gross MFR of neck and quarter arm pull technique was more beneficial in experimental group, although both the treatment groups proved to be effective in treating mechanical NP referred to unilateral upper limb except that the control group did not show any significant improvement in CFE.
In the present study, the age of patient ranged from 20 to 50 years with mean age of 30.2 ± 12.1 years indicating the occurrence of mechanical NP being predominant during second to third decade of life. Age group between 20 and 50 years was taken as an inclusion criteria as several prevalence studies have shown an increase in the occurrence of mechanical NP in the above-mentioned working age group.[18,31,32] High incidence was found in women (15%) than men (9%) for developing mechanical NP. According to BMI, the subjects in the present study fall in the category of borderline overweight for India, Asia population.[25]
The present study reveals that 90% of the subjects were right handed and around 67.5% of subjects had the same side affected, which infers that mechanical NP may give rise to referred pain mostly on the dominant side. The occurrence of pain referral more on the dominant side was probably related to their difficult work positions, repetitive precision-demanding handgrips, and overuse of dominant side.[33]
Mechanical NP leads to upper limb involvement due to a reduction in the use of upper limb and referred pain.[21,27] Upper limb and neck are mechanically connected, and movement of upper limb causes elongation of mechanical structures which in turn leads to pain, irritation of the nerve, decreased range of motion, and functional disability.[34,35]
The treatment protocols used in the control group and the experimental group both proved to be effective in improving cervical ROM, NPQ scores, and DASH scores. The initial treatment in the conventional therapy included modalities to relieve pain and spasm. Hence, the improvement in pain, ROM, and function was achieved prior than the improvement in the endurance scores.
In the experimental group, the MFR showed improvement in CFE at the end of 6-day protocol (P = 0.30), while the control group showed no improvement. The possible reasoning of failure to show improvement can be that the 6-day intervention period might not have been sufficient to show the changes in the endurance after treating with the conservative treatment. The stretching strengthening protocol given was as a home program and hence was not supervised. This might have led to the failure. This is in contrary with the previous research studies which have proved that strengthening exercise, with or without combination with other techniques, appears to be more beneficial to patients with chronic NP.[14,31]
In agreement with Chiu et al.,[19] conventional exercise therapy in the present study might have helped in improving ROM, pain reduction, and function in patients with mechanical NP.
The experimental group proved to be more beneficial in all terms in treating mechanical NP referred to upper limb. This can be attributed first because MFR is an approach that focuses on freeing restrictions of movement that originates in the soft tissues of the body. Second, by applying pressure and administering fascial release to areas of the body, this therapy aims to improve the health of fascia tissue. Fascia is a connective tissue along with tendons, ligaments, bone, and muscle. A slow gentle pressure allows the body’s tissue to reorganize, release physical restrictions, and release the body’s unconscious holding and bracing patterns. As this technique produces heat and increases blood flow which releases tension from fibrous band of connective tissue, it thus results in softening, elongating, and realigning the fascia and removing restrictions or blockages in the fascia.[29]
Gross MFR of the neck with arm pull technique is a form of indirect technique which is suggested for acute cases. A non-randomized clinical trial with no control group determined the effect of Gross MFR on upper limb and neck in subjects with mechanical NP to reduce pain and improve functional abilities.[18] The subjects showed a significant reduction in pain which was only subjective outcome measures, i.e., visual analog scale and improvement in functional activities according to NPQ and DASH with P < 0.001 in all domains proving its effectiveness in reducing mechanical NP and in improving functional abilities. The present study has both objective and subjective outcome measures and found results similar to the above study with statistical significance in all domains.
Another randomized controlled trial study found out the effect of MFR technique on chronic non-specific NP on 30 subjects. It concluded that MFR is one of the effective manual therapy techniques in reducing pain and disability and improving the isometric extension strength of neck in patients with non-specific chronic NP.[26] The MFR techniques used in this study included skin rolling, cross hand, compression, and combination techniques, which are completely different from the technique used in the present study which comprises of gross MFR of posterior cervical musculature and upper quarter arm pull technique and are done in more acute condition. Furthermore, the present study included larger number of subjects as compared to the above study.
Yet another study evaluated the effect of MFR with arm pull technique in decreasing neck disability (NDI) in patients with cervical radiculopathy and found that MFR with arm pull reduces the neck disability and hence helps the patients to return to their previous normal life and might be used as an effective treatment technique for the patients with cervical radiculopathy.[27] The technique used in the present study and the above study is the same and found to be effective in NP individuals with referred pain in the upper limb although the patient population differs. However, the population was cervical radiculopathy and the outcome measures used were subjective in comparison to the present study.
In the present study, experimental group which was treated with gross MFR of posterior cervical musculature and upper quarter arm pull technique showed more improvement in reducing pain, improving neck flexor endurance, range of motion, and functional abilities in subjects with mechanical NP referred to unilateral upper limb with gross MFR when compared to control group.
Limitations
This was a single-centric study and carry over or long-term follow-up effect was not monitored. Furthermore, the effect of only six sessions was assessed. If more number of sessions were included, the patients would get completely recovered. Acute and chronic cases based on the duration of symptoms were not separately categorized.
Scope of the study
Trigger point assessment and ultrasound screening can be assessed. Long-term outcomes can be investigated. Effect of gross MFR in acute and chronic cases can be studied separately. Number of sessions can be increased to 10–12 sessions.
Conclusion
The study concluded that the interventions given to each of the groups showed an improvement in terms of pain intensity, CFE, range of motion, and functional levels in the neck, except for CFE in control group which did not show significance.
Gross MFR of upper limb and neck showed significantly more improvement in terms of all outcome measures such as pain intensity, CFE, cervical range of motion, and functional outcomes.
Gross MFR of upper limb and neck showed improvement with early and lesser treatment sessions, i.e. only 5–6 sessions were enough.
Thus, the study suggests that gross MFR of upper limb can be implemented into rehabilitation protocols for the treatment of mechanical NP with referred pain to upper limb and should not be only seen as an adjunct or complementary therapy.
Acknowledgment
We express our sincere gratitude to all the patients who participated in this study. We are grateful to the management and staff of KLE University for Institute of Physiotherapy for supporting this study.
References
- 1.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine (Phila Pa 1976) 1994;19:1307–9. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population:A systematic critical review of the literature. Eur Spine J. 2006;15:834–48. doi: 10.1007/s00586-004-0864-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharan d. A Prevalence study of neck disorders in Bangalore. [[Last accessed on 2016 Jan 10]];Deccan Heralds. 2004-2005 2:23–35. Available from: http://www.deepak.sharan.com/toicolumn . [Google Scholar]
- 4.Darivemula SB, Goswami K, Gupta SK, Salve H, Singh U, Goswami AK, et al. Work-related neck pain among desk job workers of tertiary care hospital in New Delhi, India:Burden and determinants. Indian J Community Med. 2016;41:50–4. doi: 10.4103/0970-0218.170967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.International Association for the Study of Pain (Iasp) Pain Terminology. Seattle: IASP; 2004. Iasp Task Force for Taxonomy. [Google Scholar]
- 6.Hamilton L, Boswell C, Fryer G. The effects of high-velocity, low-amplitude manipulation and muscle energy technique on sub-occipital tenderness. Int J Osteopath Med. 2007;10:42–9. [Google Scholar]
- 7.Mechanical-neck-pain. [[Last accessed on 2016 January 14]]. Available from: http://www.backandneck.ca/mechanical-neck-pain/
- 8.Merskey H. Pain terms:A list with definitions and notes on usage. Recommended by the IASP subcommittee on taxonomy. Pain. 1979;6:249. [PubMed] [Google Scholar]
- 9.Duncan R. What is Myofascial Release and How Does it Work? Integrated Myofascial Therapy. 2007. [[Last accessed on 2016 Jan 11]]. pp. 18–20. Available from: http://www.Myofascialrelease.co.uk .
- 10.Webb R, Brammah T, Lunt M, Urwin M, Allison T, Symmons D, et al. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine (Phila Pa 1976) 2003;28:1195–202. doi: 10.1097/01.BRS.0000067430.49169.01. [DOI] [PubMed] [Google Scholar]
- 11.Greening J, Lynn B. Minor peripheral nerve injuries:An underestimated source of pain. Man Ther. 1998;3:187–94. [Google Scholar]
- 12.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure:The DASH (disabilities of the arm, shoulder and hand) [corrected] The upper extremity collaborative group (UECG) Am J Ind Med. 1996;29:602–8. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.Leak AM, Cooper J, Dyer S, Williams KA, Turner-Stokes L, Frank AO, et al. The Northwick park neck pain questionnaire, devised to measure neck pain and disability. Br J Rheumatol. 1994;33:469–74. doi: 10.1093/rheumatology/33.5.469. [DOI] [PubMed] [Google Scholar]
- 14.Levangie PK, Norkin CC. Joint Structure and Function:A Comprehensive Analysis. Philadelphia, PA: FA Davis; 2011. [Google Scholar]
- 15.Sim J, Jordan K, Lewis M, Hill J, Hay EM, Dziedzic K, et al. Sensitivity to change and internal consistency of the Northwick park neck pain questionnaire and derivation of a minimal clinically important difference. Clin J Pain. 2006;22:820–6. doi: 10.1097/01.ajp.0000210937.58439.39. [DOI] [PubMed] [Google Scholar]
- 16.Tozzi P, Bongiorno D, Vitturini C. Fascial release effects on patients with non-specific cervical or lumbar pain. J Bodyw Mov Ther. 2011;15:405–16. doi: 10.1016/j.jbmt.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 17.Walker MJ, Boyles RE, Young BA, Strunce JB, Garber MB, Whitman JM, et al. The effectiveness of manual physical therapy and exercise for mechanical neck pain:A randomized clinical trial. Spine (Phila Pa 1976) 2008;33:2371–8. doi: 10.1097/BRS.0b013e318183391e. [DOI] [PubMed] [Google Scholar]
- 18.Nitsure P, Welling A. Effect of gross myofascial release of upper limb and neck on pain and function in subjects with mechanical neck pain with upper limb radiculopathy:A clinical trial. Int J Dental Med Res. 2014;1:8–16. [Google Scholar]
- 19.Chiu TT, Hui-Chan CW, Chein G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin Rehabil. 2005;19:850–60. doi: 10.1191/0269215505cr920oa. [DOI] [PubMed] [Google Scholar]
- 20.Chivate D. Comparative Effectiveness of Static and Dynamic Neck Strengthening Exercise in Chronic Neck Pain-a Randomized Clinical Trial (Doctoral dissertation, KLE University, Belgaum, Karnataka) [Google Scholar]
- 21.Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J, et al. Treatment of neck pain:Noninvasive interventions:Results of the bone and joint decade 2000-2010 task force on neck pain and its associated disorders. Spine (Phila Pa 1976) 2008;33:S123–52. doi: 10.1097/BRS.0b013e3181644b1d. [DOI] [PubMed] [Google Scholar]
- 22.Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Bronfort G, et al. Exercises for mechanical neck disorders. Cochrane Database Syst Rev. 2005;3:CD004250. doi: 10.1002/14651858.CD004250.pub3. [DOI] [PubMed] [Google Scholar]
- 23.La touché R, Ostergreen P, Hansen P. Bilateral mechanical sensitivity over the trigeminal region in patients with chronic mechanical neck pain. J Musculomed. 2010;26:264–80. doi: 10.1016/j.jpain.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 24.Manheim CJ. The Myofascial Release Manual. Charlesten SC: Slack Incorporated; 2008. pp. 40–3. 98-101. [Google Scholar]
- 25.Mäkelä M, Heliövaara M, Sievers K, Impivaara O, Knekt P, Aromaa A, et al. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 1991;134:1356–67. doi: 10.1093/oxfordjournals.aje.a116038. [DOI] [PubMed] [Google Scholar]
- 26.Hosseinifar M. Effect of myofascial release technique on pain, disability, maximum isometric contraction of the extensor muscles, and pressure pain threshold in patients with chronic nonspecific neck pain:Double blinded randomized clinical trial. Health Sci. 2016;5:500–6. [Google Scholar]
- 27.Sambyal R, Moitra M, Samuel AJ, Kumar SP. Does myofascial Release technique contribute to cervical radiculopathy treatment? Cues from a noncontrolled experimental design study. Revista Pesquisaem Fisioterapia. 2016;6:599–605. [Google Scholar]
- 28.Harris KD, Heer DM, Roy TC, Santos DM, Whitman JM, Wainner RS, et al. Reliability of a measurement of neck flexor muscle endurance. Phys Ther. 2005;85:1349–55. [PubMed] [Google Scholar]
- 29.Hou CR, Tsai LC, Cheng KF, Chung KC, Hong CZ. Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Arch Phys Med Rehabil. 2002;83:1406–14. doi: 10.1053/apmr.2002.34834. [DOI] [PubMed] [Google Scholar]
- 30.Huisstede BM, Feleus A, Bierma-Zeinstra SM, Verhaar JA, Koes BW. Is the disability of arm, shoulder, and hand questionnaire (DASH) also valid and responsive in patients with neck complaints. Spine (Phila Pa 1976) 2009;34:E130–8. doi: 10.1097/BRS.0b013e318195a28b. [DOI] [PubMed] [Google Scholar]
- 31.Nachemson AL, Jonsson E, Englund L, Evers S, Gibson JN, Goossens M, et al. Neck and Back Pain:The Scientific Evidence of Causes, Diagnosis, and Treatment. Philadelphia, PA: Lippincott Williams and Wilkins; 2000. [Google Scholar]
- 32.Norkin CC, White DJ. Measurement of Joint Motion:A Guide to Goniometry. Philadelphia, PA: FA Davis; 2016. [Google Scholar]
- 33.Falla D, Jull G, Rainoldi A, Merletti R. Neck flexor muscle fatigue is side specific in patients with unilateral neck pain. Eur J Pain. 2004;8:71–7. doi: 10.1016/S1090-3801(03)00075-2. [DOI] [PubMed] [Google Scholar]
- 34.Gross AR, Hoving JL, Haines TA, Goldsmith CH, Kay T, Aker P, et al. Acochrane review of manipulation and mobilization for mechanical neck disorders. Spine (Phila Pa 1976) 2004;29:1541–8. doi: 10.1097/01.brs.0000131218.35875.ed. [DOI] [PubMed] [Google Scholar]
- 35.Guez M, Hildingsson C, Nilsson M, Toolanen G. The prevalence of neck pain. Acta Orthopaedica Scandinavica. 2002 Jan 1;73(4):455–9. doi: 10.1080/00016470216329. [DOI] [PubMed] [Google Scholar]


