Abstract
Pigmentation of gingiva not just has an impact on esthetics but also creates psychological negativity. Although a wide array of depigmentation techniques are available to manage this condition, there is a scarcity of literature that guides clinicians to choose the most appropriate technique. Hence, the aim of this review is to evaluate the available depigmentation therapeutic modalities with an emphasis on their merits and demerits. The databases of MEDLINE and Cochrane databases of systematic reviews were searched to collect relevant scientific literature. Cryosurgery followed by lasers has been reported to be the superior techniques with better esthetic results and low rate of recurrence. However, further randomized controlled longitudinal studies are warranted to elaborate the efficiency and effectiveness of available techniques.
Keywords: Depigmentation, gingival pigmentation, periodontal surgery, repigmentation
Introduction
Gingival tissue constitutes the macroelement of dentofacial esthetics along with face, lip, and teeth.[1] Gingiva participates in the harmony of smile with its pigmentation playing a crucial role. Pigmentation of gingiva is considered to be unaesthetic by patients, and it may have a psychological impact on them. This impact is aggravated in patients with “gummy smile” or excessive gingival display while smiling (high smile line).[2]
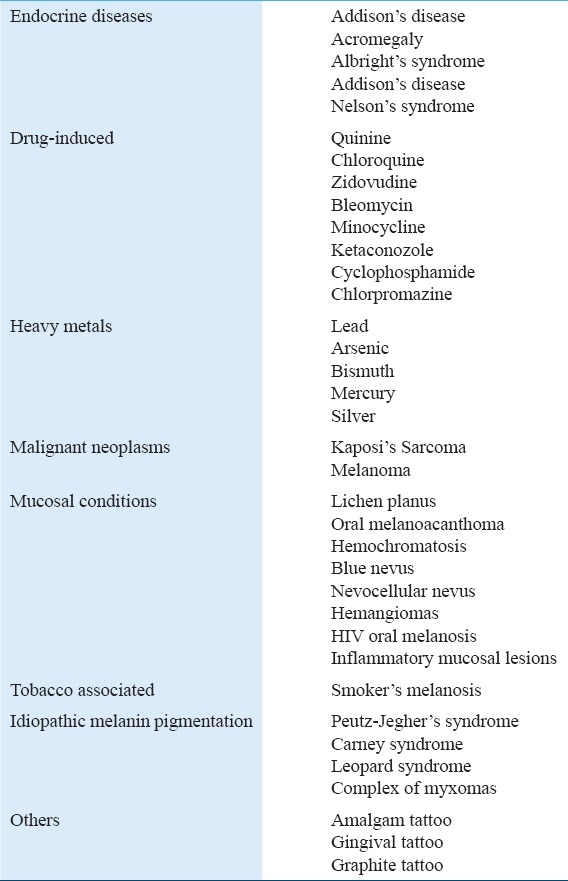
Gingival hyperpigmentation can be defined as a darker gingival color beyond what is normally expected.[3] Pigmentation is contributed by-products of the physiological process such as melanin, melanoid, carotene, oxyhemoglobin, reduced hemoglobin, bilirubin and iron[4] and/or pathological diseases, and conditions.[5] Melanin pigmentation results from melanin granules which are produced by melanoblasts.[6] Furthermore, environmental risk factors such as tobacco smoking contribute to the gingival hyperpigmentation in both active and passive form.[7-10] Ethnicity and age also influence the color of gingiva and has no sexual predilection.[11] Various pathological causes of gingival pigmentation are listed in Table 1. A wide range of procedures have been advocated for the removal of gingival pigmentation, i.e., depigmentation.
Table 1.
Represents the list of various pathological cause of gingival pigmentation
Gingival Depigmentation
Gingival depigmentation can be defined as a periodontal plastic surgical procedure whereby the gingival hyperpigmentation is removed or reduced by various techniques.[2] Depigmentation is not a clinical indication but a treatment of choice where esthetics is a concern and is desired by the patients.[12,13]
A variety of depigmentation techniques have been described in the literature which can be classified into the following groups:
Chemical methods: Using agents such as alcohols,[14,15] phenols,[14,15] and ascorbic acid.[16,17]
-
Surgical methods
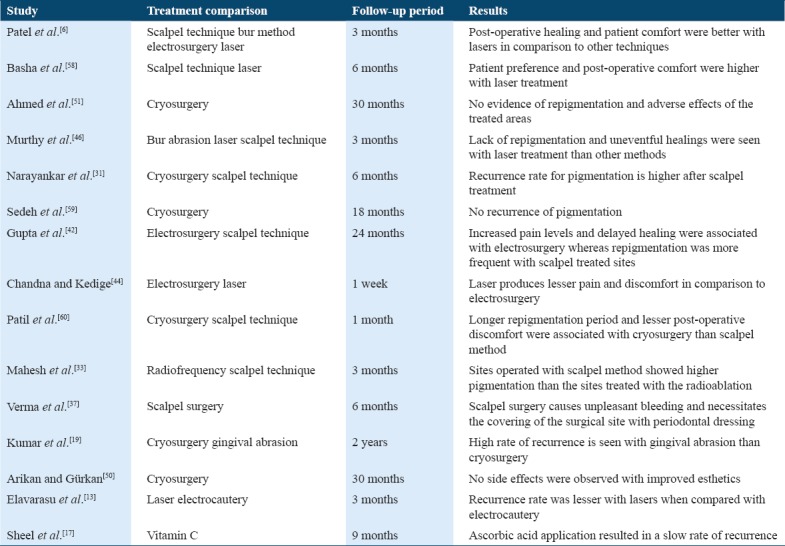
Table 2 summarizes the studies comparing the different depigmentation techniques.
Table 2.
Presents the various studies that compared the different depigmentation techniques
Criteria for Selection of Technique
Patient’s skin color, extent of gingival pigmentation, lip line, upper lip curvature, esthetic concern and expectation from the treatment, influence the orchestration of treatment plan, and selection of technique.[2,12,20]
However, the procedure adopted should be simple, cost-effective, and comfortable to the clinician as well as patient with less pain and minimal tissue loss.[36] Caution must be employed to avoid injury to soft tissues and adjacent teeth. Inappropriate technique or inadvertent application can result in a gingival recession, damage to attachment apparatus, underlying bone, as well as enamel.
Chemical Gingival Peeling
It is a treatment method used to destroy the overlying gingival epithelium using a chemical peeling agent. A variety of chemical agents are available such as phenols, salicylic acid, glycolic acid, and trichloroacetic acid.[36] The most commonly used are phenols and alcohols.[14] In a study by Hirschfield and Hirschfield in 1951, pigmented gingiva was burnt out by destroying tissue down to and slightly below the basal layer of mucous membranes using a mixture of 90% phenol and 95% alcohol.[15] However, repigmentation and relapse occurred in all cases shortly after the application of either agent.[15] As phenols may induce cardiac arrhythmias, cardiac monitoring is necessary.[23] The inability to control the depth of penetration and amount of destruction are the main drawbacks of this method. Thereby, these methods are no longer in use and are unacceptable to the clinicians as well as patients.
Ascorbic Acid
Ascorbic acid/Vitamin C has potential in the treatment of gingival melanin pigmentation.[16] It inhibits the melanin formation by suppressing the tyrosine activity which is essential for melanin biosynthesis.[16] Furthermore, ascorbic acid directly downregulates dopaquinone formation, a precursor in melanin synthesis, thus inhibiting the melanin formation. A study by Sheel et al. have reported the delay in repigmentation of gingiva with the local application of ascorbic acid following the depigmentation procedure.[17]
Gingival Abrasion
The first case using this technique was documented by Ginwalla et al. in 1966.[18] It involves the denuding of pigmented gingival epithelium by superficial abrasion using grit football shaped or doughnut-shaped coarse diamond burs in a low-speed handpiece.[14,19] Extra care should be taken to control the speed and pressure of handpiece, so as not to cause unwanted abrasions or pitting of the tissue.[23] It is a relatively a non-invasive and cost-effective technique and does not require any specific instruments.[14] However, it is associated with various drawbacks such as technique sensitivity, increased treatment duration, post-treatment pain, placement of periodontal dressing, and high recurrence rate.[14,19] Exposure of underlying alveolar bone can occur with high speed and/or increased pressure.
Scalpel Surgical Technique
It is also called as split thickness epithelial excision[14] and surgical stripping.[3] Conventional scalpel method involves the surgical excision of gingival epithelium using a scalpel and allowing the denuded connective tissue to heal by secondary intention.[20,21] It is simple, most economical and convenient to perform with minimum time and efforts.[4,23,37] Healing with this technique is faster in comparison to other surgical techniques.[23,4] Although lower cost and lower rate of recurrence favor the surgical stripping of gingiva,[3] it is associated with pain, post-operative discomfort, intra- and post-operative bleeding and requires placement of periodontal dressing.[21,25,37-39] Thinner gingival biotype and narrow papillary areas contraindicate the use of this technique.[40]
Free gingival grafting (FGG)
In this technique, an unpigmented free gingival autograft harvested from the patient’s palate is placed on the prepared recipient site.[22] This technique masks the pigmented gingival area rather than eliminating it.[2] Two surgical sites, post-operative discomfort due to pain, technique sensitivity, and ghost-like appearance of the treated site due to hypopigmentation are the drawbacks of this technique.[14,39]
ADMA
It can be used as a safe substitute for free gingival autograft in the treatment of gingival hyperpigmentation.[24] ADMA has benefits of elimination of second surgical procedure for donor site, decreased post-operative complications, availability of unlimited amount of graft material, and satisfactory esthetic results than the FGG.[23,24] However, it is technique sensitive, expensive and requires clinical expertise.[23]
Electrosurgery
In electrosurgical technique, heat generated by transmission of high-frequency electrical energy to the tissues leads to either cutting or coagulation of tissue.[26] Bleeding control, tissue contouring and less scar tissue formation favor the use of this technique for gingival depigmentation.[41] However, pain and patient discomfort during the initial healing period is more with this technique.[6,42] Furthermore, it requires more clinical expertise than the scalpel surgical method.[25,27] Prolonged or repeated application can induce heat accumulation and undesired tissue destruction.[25] Contact of the electrosurgical tip with the teeth, periosteum, or alveolar bone can cause their damage.[27]
Lasers
Laser therapy has optimal efficacy in the treatment of gingival hyperpigmentation.[28] Most commonly used lasers for gingival depigmentation are carbon dioxide (CO2, 10,600 nm) lasers, neodymium: Yttrium, aluminum, and garnet (Nd: YAG, 1,064 nm) and diode (980 nm) lasers.[29,30] Lasers exhibit enhanced hemostatic activity, good visibility at the surgical site and fewer post-operative complications such as pain, bleeding, edema, infection, and impaired wound healing.[28,43-47] It is an effective and safe treatment modality with ease of access to interdental papilla and low rate of recurrence.[28,38,46,48] Although better esthetic results can be achieved by lasers,[46] it requires sophisticated equipment, occupies large space and is expensive method.[25] Inappropriate application may damage gingiva and underlying alveolar bone which, in turn, can cause gingival recession, gingival fenestrations, and delayed wound healing.[14,19]
Cryosurgery
Cryosurgery is most widely accepted method of gingival depigmentation.[11,19,31,32] It involves freezing of gingiva with the application of different materials, i.e. cryogen such as liquid nitrogen at very low temperatures.[27] The effect of ultralow temperature of cryogen on gingival tissue causes the epithelium to undergo cryonecrosis, which helps to eliminate gingival pigmentation.[49] It is an inexpensive method with long-term superior esthetic results, rapid healing, and low recurrence rate.[19,50] Lack of bleeding, pain and scar formation, application without regional anesthesia, sutures or drugs, ease of application of cryogen at papillary areas and need of no complicated instruments, and prioritizes the cryosurgery over other depigmentation methods.[19,31,32,47,51,52] Post-operative swelling and difficulty in controlling the penetration depth constitute the disadvantages of this technique.[25,53]
Radiosurgery
It is a novel therapeutic modality for the gingival depigmentation that utilizes radiofrequency.[33] Electrically generated thermal energy from the radiofrequency apparatus influences the molecular disintegration of melanin cells present on the basal and suprabasal layers of gingival epithelium.[33] The latent heat of radiosurgery retards the development and migration of melanocytes, which makes it a more efficient method of depigmentation than the conventional methods.[33] Radiosurgery produces coagulation, thereby reduces the bleeding but it requires at least two sessions of treatment.[34,35] Papillary areas can be easily depigmented with radiosurgery.[14] Multiple sittings, technique sensitivity, and more expense are the limitations of this novel technique.[14,35]
Future Advancements
Plasma therapy
At present, ongoing research is focusing on utilizing plasma as a novel treatment technique for gingival hyperpigmentation and gummy smile.[54] Plasma refers to the fourth state of matter consisting of partially ionized gases with free electrons, generated at a low temperature.[54] The mechanism of action is based on the release of free radicals and reactive species.[55] It also produces ozone.[56]
Gingival repigmentation
A critical concern in the management of hyperpigmented gingiva is a relapse or gingival repigmentation.[3] Repigmentation refers to the clinical appearance of melanin pigment following a period of clinical depigmentation.[57] As it depends on methodology and follow-up period, the duration of repigmentation mentioned in literature remains controversial from one technique to other. Futhermore, factors such as smoking, sun exposure, and genetic determination of skin color, influence the duration of relapse. However, the majority of the available literature has shown lower recurrence rate for cryosurgery and lasers.
Conclusion
Demand for depigmentation therapy is mostly seen in patients with the excessive gingival display. Gingival biotype, clinician’s expertise, patient preferences, and recurrence rate, greatly determine the selection of a technique. Although a wide range of techniques have been employed, cryosurgery followed by lasers has been reported to be superior techniques with better esthetic results and low rate of recurrence. Relapse or repigmentation is a critical concern and depends on the technique employed and follow-up period. Majority of the available literature is comprised case reports. Hence, authors recommend the conduct of randomized controlled longitudinal studies to identify the efficiency and effectiveness of available techniques.
References
- 1.McLaren EA, Culp L. Smile analysis:The Photoshop smile design technique Part I. Spring. 2013;29:94–108. [Google Scholar]
- 2.Malhotra S, Sharma N, Basavaraj P. Gingival esthetics by depigmentation. J Periodontal Med Clin Pract. 2014;1:79–84. [Google Scholar]
- 3.El-Shenawy H, Fahd A, Ellabban M, Dahaba M, Khalifa M. Lasers for esthetic removal of gingival hyperpigmentation:A systematic review of randomized clinical trials. Int J Adv Res. 2017;5:1238–48. [Google Scholar]
- 4.Ozbayrak S, Dumlu A, Ercalik-Yalcinkaya S. Treatment of melanin-pigmented gingiva and oral mucosa by CO2 laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:14–5. doi: 10.1067/moe.2000.106396. [DOI] [PubMed] [Google Scholar]
- 5.Chatterjee A, Singh N, Malhotra P, Ajmera N. Gingival pigmentation and its treatment modalities. J Dent Scie Oral Rehab. 2011;2:11–4. [Google Scholar]
- 6.Patel KA, Patil SS, Agrawal C, Patel AP, Kalaria J. Gingival depigmentation:Case series. Int J Appl Dent Scien. 2015;1:37–9. [Google Scholar]
- 7.Multani S. Interrelationship of smoking, lip and gingival melanin pigmentation, and periodontal status. Addict Health. 2013;5:57–65. [PMC free article] [PubMed] [Google Scholar]
- 8.Hanioka T, Tanaka K, Ojima M, Yuuki K. Association of melanin pigmentation in the gingiva of children with parents who smoke. Pediatrics. 2005;116:e186–90. doi: 10.1542/peds.2004-2628. [DOI] [PubMed] [Google Scholar]
- 9.Tadakamadla J, Kumar S, Nagori A, Tibdewal H, Duraiswamy P, Kulkarni S, et al. Effect of smoking on oral pigmentation and its relationship with periodontal status. Dent Res J (Isfahan) 2012;9:S112–4. [PMC free article] [PubMed] [Google Scholar]
- 10.Moravej-Salehi E, Moravej-Salehi E, Hajifattahi F. Relationship of gingival pigmentation with passive smoking in women. Tanaffos. 2015;14:107–14. [PMC free article] [PubMed] [Google Scholar]
- 11.Ho DK, Ghinea R, Herrera LJ, Angelov N, Paravina RD. Color range and color distribution of healthy human gingiva:A Prospective clinical study. Sci Rep. 2015;5:18498. doi: 10.1038/srep18498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grover HS, Dadlani H, Bhardwaj A, Yadav A, Lal S. Evaluation of patient response and recurrence of pigmentation following gingival depigmentation using laser and scalpel technique:A clinical study. J Indian Soc Periodontol. 2014;18:586–92. doi: 10.4103/0972-124X.142450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elavarasu S, Thangavelu A, Alex S. Comparative evaluation of depigmentation techniques in split-mouth design with electrocautery and laser. J Pharm Bioallied Sci. 2015;7:S786–90. doi: 10.4103/0975-7406.163563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar S, Bhat GS, Bhat KM. Development in techniques for gingival depigmentation -an update. Indian J Dent. 2012;3:e213–21. [Google Scholar]
- 15.Hirschfeld I, Hirschfeld L. Oral pigmentation and method of removing it. Oral Surg Oral Med Oral Path. 1951;4:1012. doi: 10.1016/0030-4220(51)90448-3. [DOI] [PubMed] [Google Scholar]
- 16.Shimada Y, Tai H, Tanaka A, Ikezawa-Suzuki I, Takagi K, Yoshida Y, et al. Effects of ascorbic acid on gingival melanin pigmentationin vitroandin vivo. J Periodontol. 2009;80:317–23. doi: 10.1902/jop.2009.080409. [DOI] [PubMed] [Google Scholar]
- 17.Sheel V, Purwar P, Dixit J, Rai P. Ancillary role of vitamin C in pink aesthetics. BMJ Case Rep. 2015;2015 doi: 10.1136/bcr-2014-208559. pii:bcr2014208559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ginwalla TM, Gomes BC, Varma BR. Surgical removal of gingival pigmentation. (A preliminary study) J Indian Dent Assoc. 1966;38:147–50. passim. [PubMed] [Google Scholar]
- 19.Kumar S, Bhat GS, Bhat KM. Comparative evaluation of gingival depigmentation using tetrafluoroethane cryosurgery and gingival abrasion technique:Two years follow up. J Clin Diag Res. 2013;7:389–94. doi: 10.7860/JCDR/2013/4454.2779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dummett CO. Physiologic pigmentation of the oral and cutaneous tissues in the Negro. J Dent Res. 1946;25:421–32. doi: 10.1177/00220345460250060201. [DOI] [PubMed] [Google Scholar]
- 21.Dummett CO, Bolden TE. Post-surgical clinical repigmentation of the gingiva. Oral Surg Oral Med Oral Pathol. 1963;16:353–65. [Google Scholar]
- 22.Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int. 1996;27:555–8. [PubMed] [Google Scholar]
- 23.Kathariya R, Pradeep AR. Split mouth de-epithelization techniques for gingival depigmentation:A case series and review of literature. J Indian Soc Periodontol. 2011;15:161–8. doi: 10.4103/0972-124X.84387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Novaes AB, Jr, Pontes CC, Souza SL, Grisi MF, Taba M., Jr The use of acellular dermal matrix allograft for the elimination of gingival melanin pigmentation:Case presentation with 2years of follow-up. Pract Proced Aesthet Dent. 2002;14:619–23. [PubMed] [Google Scholar]
- 25.Prasad SS, Agrawal N, Reddy NR. Gingival depigmentation:A Case report. People's J Sci Res. 2010;3:27–30. [Google Scholar]
- 26.Prasad S, Agrawal N, Reddy N. Gingival depigmentation:A case report. People's J Sci Res. 2010;3:27–9. [Google Scholar]
- 27.Moneim RA, El Deeb M, Rabea AA. Gingival pigmentation (cause, treatment and histological preview) Future Dent J. 2017;3:1–7. [Google Scholar]
- 28.Khalilian F, Nateghi Z, Janbakhsh N. Gingival depigmentation using lasers:A literature review. Br J Med Med Res. 2016;12:1–7. [Google Scholar]
- 29.Atsawasuwan P, Greethong K, Nimmanon V. Treatment of gingival hyperpigmentation for esthetic purposes by ND:YAG laser:Report of 4 cases. J Periodontol. 2000;71:315–21. doi: 10.1902/jop.2000.71.2.315. [DOI] [PubMed] [Google Scholar]
- 30.El Shenawy HM, Nasry SA, Zaky AA, Quriba MA. Treatment of gingival hyperpigmentation by diode laser for esthetical purposes. Open Access Maced J Med Sci. 2015;3:447–54. doi: 10.3889/oamjms.2015.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Narayankar SD, Deshpande NC, Dave DH, Thakkar DJ. Comparative evaluation of gingival depigmentation by tetrafluroethane cryosurgery and surgical scalpel technique. A Randomized clinical study. Contemp Clin Dent. 2017;8:90–5. doi: 10.4103/ccd.ccd_1017_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lin YH, Tu YK, Lu CT, Chung WC, Huang CF, Huang MS, et al. Systematic review of treatment modalities for gingival depigmentation:A random-effects poisson regression analysis. J Esthet Restor Dent. 2014;26:162–78. doi: 10.1111/jerd.12087. [DOI] [PubMed] [Google Scholar]
- 33.Mahesh HV, Harish MR, Shashikumar BM, Ramya KS. Gingival pigmentation reduction:A novel therapeutic modality. J Cutan Aesthet Surg. 2012;5:137–40. doi: 10.4103/0974-2077.99458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim DG, Choe WJ, Paek SH, Chung HT, Kim IH, Han DH. Radiosurgery of intracranial cavernous malformations. Acta Neurochir. 2002;144:869–78. doi: 10.1007/s00701-002-0983-9. [DOI] [PubMed] [Google Scholar]
- 35.Sherman JA, Gürkan A, Arikan F. Radiosurgery for gingival melanin depigmentation. Dent Today. 2009;28:118. 120-1. [PubMed] [Google Scholar]
- 36.Sharath KS, Shah R, Thomas B, Madani SM, Shetty S. Gingival depigmentation:Case series for four different techniques. Nitte Univ J Health Sci. 2013;3:132–6. [Google Scholar]
- 37.Verma S, Gohil M, Rathwa V. Gingival depigmentation. Indian J Clin Pract. 2013;12:801–3. [Google Scholar]
- 38.Senthinathan S, Baskaran M, Thirumalai S, Naarayanen MB. A comparative study to evaluate gingival depigmentation using scalpel blade technique and CO2 lasers. J Oro Res. 2014;4:59–62. [Google Scholar]
- 39.Mokeem SA. Management of gingival hyperpigmentation by surgical abrasion:Report of three cases. Saudi Dent J. 2006;18:162–6. [Google Scholar]
- 40.Bergamaschi O, Kon S, Doine AI, Ruben MP. Melanin repigmentation after gingivectomy:A 5-year clinical and transmission electron microscopic study in humans. Int J Periodontics Restorative Dent. 1993;13:85–92. [PubMed] [Google Scholar]
- 41.Gupta ND, Agrawal A, Agrawal N, Yadav P. Gingival depigmentation by different technique:A case series. IOSR J Dent Med Sci. 2015;14:93–7. [Google Scholar]
- 42.Gupta G, Kumar A, Khatri M, Puri K, Jain D, Bansal M, et al. Comparison of two different depigmentation techniques for treatment of hyperpigmented gingiva. J Indian Soc Periodontol. 2014;18:705–9. doi: 10.4103/0972-124X.147404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nagati RR, Ragul M, Al-Qahtani NA, Ravi KS, Tikare S, Pasupuleti MK. clinical effectiveness of gingival depigmentation using conventional surgical scrapping and diode laser technique:A quasi experimental study. Global J Health Sci. 2017;9:296–303. [Google Scholar]
- 44.Chandna S, Kedige SD. Evaluation of pain on use of electrosurgery and diode lasers in the management of gingival hyperpigmentation:A comparative study. J Indian Soc Periodontol. 2015;19:49–55. doi: 10.4103/0972-124X.145823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Monteiro LS, Costa JA, da Câmara MI, Albuquerque R, Martins M, Pacheco JJ, et al. Aesthetic depigmentation of gingival smoker's melanosis using carbon dioxide lasers. Case Rep Dent. 2015;2015:510589. doi: 10.1155/2015/510589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Murthy MB, Kaur J, Das R. Treatment of gingival hyperpigmentation with rotary abrasive, scalpel, and laser techniques:A case series. J Indian Soc Periodontol. 2012;16:614–9. doi: 10.4103/0972-124X.106933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Roshna T, Nandakumar K. Anterior esthetic gingival depigmentation and crown lengthening:Report of a case. J Contemp Dent Pract. 2005;6:139–47. [PubMed] [Google Scholar]
- 48.Thangavelu A, Elavarasu S, Jayapalan P. Pink esthetics in periodontics-gingival depigmentation:A case series. J Pharm Bioallied Sci. 2012;4:S186–90. doi: 10.4103/0975-7406.100267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kumar S, Bhat GS, Bhat KM. Effectiveness of cryogen tetrfluoroethane on elimination of gingival epithelium and its clinical application in gingival depigmentation-histological findings and case series. J Clin Diagn Res. 2013;7:3070–2. doi: 10.7860/JCDR/2013/5353.3855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arikan F, Gürkan A. Cryosurgical treatment of gingival melanin pigmentation with tetrafluoroethane. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:452–7. doi: 10.1016/j.tripleo.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 51.Ahmed SK, George JP, Prabhuji ML, Lazarus M. Cryosurgical treatment of gingival melanin pigmentation-a 30-month follow-up case report. Clin Adv Perio. 2002;2:73–8. doi: 10.1902/cap.2011.100007. [DOI] [PubMed] [Google Scholar]
- 52.Yu CH, Chen HM, Chang CC, Hung HY, Hsiao CK, Chiang CP, et al. Cotton-swab cryotherapy for oral leukoplakia. Head Neck. 2009;31:983–8. doi: 10.1002/hed.21055. [DOI] [PubMed] [Google Scholar]
- 53.Almas K, Sadig W. Surgical treatment of melanin-pigmented gingiva;an esthetic approach. Indian J Dent Res. 2002;13:70–3. [PubMed] [Google Scholar]
- 54.Jha N, Ryu JJ, Wahab R, Al-Khedhairy AA, Choi EH, Kaushik NK, et al. Treatment of oral hyperpigmentation and gummy smile using lasers and role of plasma as a novel treatment technique in dentistry:An introductory review. Oncotarget. 2017;8:20496–509. doi: 10.18632/oncotarget.14887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma Y, Ha CS, Hwang SW, Lee HJ, Kim GC, Lee KW, et al. Non-thermal atmospheric pressure plasma preferentially induces apoptosis in p53-mutated cancer cells by activating ROS stress-response pathways. PLoS One. 2014;9:e91947. doi: 10.1371/journal.pone.0091947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haertel B, von Woedtke T, Weltmann KD, Lindequist U. Non-thermal atmospheric-pressure plasma possible application in wound healing. Biomol Ther (Seoul) 2014;22:477–90. doi: 10.4062/biomolther.2014.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Srivastava S, Shrivastava T, Dwivedi S, Yadav P. Gingival melanin pigmentation-a review and case report. J Orofac Res. 2014;4:50–4. [Google Scholar]
- 58.Basha MI, Hegde RV, Sumanth S, Sayyed S, Tiwari A, Muglikar S, et al. Comparison of ND:YAG laser and surgical stripping for treatment of gingival hyperpigmentation:A Clinical trial. Photomed Laser Surg. 2015;33:424–36. doi: 10.1089/pho.2014.3855. [DOI] [PubMed] [Google Scholar]
- 59.Sedeh SA, Badihi S, Esfahaniyan V. Comparison of recurrent rate of gingival pigmentation after treatment by liquid nitrogen and cryoprob in 18 months follows-up. Dent Res J (Isfahan) 2014;11:592–8. [PMC free article] [PubMed] [Google Scholar]
- 60.Patil KP, Joshi V, Waghmode V, Kanakdande V. Gingival depigmentation:A split mouth comparative study between scalpel and cryosurgery. Contemp Clin Dent. 2015;6:S97–S101. doi: 10.4103/0976-237X.152964. [DOI] [PMC free article] [PubMed] [Google Scholar]


