Abstract
Objectives:
The objectives of this study were to determine the safety of the Plastibell device (PD) circumcision in neonates, infants, and older children.
Patients and Methods:
A prospective, descriptive study was conducted in private clinics of district Poonch and district Sudhanuti Azad Kashmir, Pakistan, during the period from November 2014 to August 2017. Research was conducted in light of guidelines set by Helsinki declaration. Healthy male babies free of any clinical signs of illness and congenital anomaly were included in the study. The babies having weight <3 kg at the time of surgery were excluded from the study. The parents/guardian were explained about the procedure and informed consent was taken. The complications that developed postoperatively were recorded. The record of all cases was analyzed retrospectively for safety outcome and complications developed in neonates, infants, and older children.
Results:
A total of 1000 cases including 655 (65.5%) neonates, 241 (24.1%) infants, and 104 (10.4%) children between 1 and 5 years of age were selected. The PD circumcision was done in all these cases. Of these, 93.5% neonates, 89.6% infants, and 66.3% children older than 1 years of age had no complications postoperatively. The complication rate was highest among the children between 1 and 5 years of age as compared to neonates and infants. The complications such as bleeding prepuce, hematoma, and swelling prepuce were higher in infants than neonates while superficial infection and buried glans were noted more in neonates than infants.
Conclusion:
It may be inferred from our findings that Plastibell circumcision is safer if done in the 1st year of life and younger the age better is prognosis in healthy male babies.
Keywords: Bleeding, circumcision, infants, infection, neonates, Plastibell
Introduction
After Christianity, Islam is the largest religion of the world. Total Muslim population is approximately 1.6 billion, approximately 23.2% of world population.[1] Every Muslim male child needs circumcision due to religious obligations. All famous books of hadiths mention circumcision as Sunnah/fitra.[2,3] History of circumcision dates back to prehistoric era. The Egyptian mummies crafted on walls explored in 19th century provide earliest records of circumcision, dating this procedure back to 6000 years BC. Islamic history of circumcision dates back to prophet Ibrahim who did circumcision at the age of 80 years.[4] Circumcision is not only related to Muslim but Jews also practice it routinely due to religious bonding.[5] It is also done in other parts of world as a protective, prophylactic, or curative procedure.[6] Infantile circumcision has been attributed to decrease the risk of penile carcinoma in future, by American Academy of Pediatrics.[7] In uncircumcised children, incidence of urinary tract infection has been reported to be much higher.[8] It is one of the most common surgical procedure done in the world with different techniques.[9] Circumcision is still considered “A Gold Standard” treatment for phimosis.[10] Every method of circumcision has its own benefits and risks but as the medical knowledge is expanding, safer techniques are available, old traditional way of circumcision is decreasing day by day. In underdeveloped world like Pakistan, most of the population lives in rural areas. In these areas, healthcare facilities are rare so circumcision is being done by untrained local practitioners by clamp method (bone cutter), which leads to many complications.[11] The most common hitches of cultural circumcisions are bleeding which has been documented up to 35% in the previous literature.[12] Plastibell device (PD) circumcisions are reported to be superior than conventional methods, but bleeding was notable significantly unless several modifications were evolved to minimize this risk. PD slippage and bleeding have been overcome using silk 0 ligature which offer better knotting and hemostatic qualities.[13]
Another less precarious reason for bleeding has been injury to the frenulum by the piercing edges of the holder of the PD when separating it from the ring. This threat is curtailed by orientation of the holder of PD in such a way that it is vertical to the frenulum while applying the hemostatic knots. The surgeons operating alone may have severe difficulty during the application of the ligatures so a skilled assistant is required to do so when prompted by the operating surgeon. The suitable sized PD is crucial for successful circumcision and trying slightly larger than the smaller device is sensible. The Plastibell ring usually disengages within 5–7 days, but surgical evaluation is required if separation does not occur by 2 weeks. The retained device may be detached just by applying traction on the ring. Rarely, if it fails than dividing the device with strong scissors may be required, which is done under mild sedation of subject and by applying topical anesthetic cream.[14-16]
Patients and Methods
It was a retrospective analysis of circumcision done in private setup. We studied safety of Plastibell method in rural areas of district Poonch and Sudhanuti, Azad Kashmir, Pakistan, from November 2014 to August 2017. The research was conducted in light of guidelines set by Helsinki declaration. Healthy male babies free of any clinical signs of illness were included in the study. The study was also in concordance with guidelines set by Ethical Review Committee Poonch Medical College, Rawalakot, AJK, and official permission was obtained. The babies having weight <3 kg at the time of surgery were not included in the study. The babies having any congenital anomaly, hypospadias, undescended testis, and hernia were excluded from the study. Only healthy babies were enrolled in the study. The parents/guardian were fully explained about the surgical procedure and related complications. Only those subjects were included in the study whose parents/guardian signed the consent form. The complications that developed postoperatively were recorded. During this period, 1000 circumcisions were performed using PD. During this study, 655 neonates, 241 infants, and 104 older children were circumcised using PD. Different sizes of plastic devices ranging from 1.1 to 1.7 were used. The surgical procedure was done under local anesthesia with a ring block using 2% lignocaine in insulin syringe to the base of the penis. Surgical duration, perioperative bleeding, time of PD separation, and use of analgesic medications, early and late complications in the post-operative period for neonates, infants, and older children were evaluated.
Results
A total of 1000 cases of PD circumcision meeting the inclusion criteria were surgically operated and the post-circumcision complications were monitored and analyzed. Of the total cases, 655 (65.5%) were neonates, 241 (24.1%) were infants, and 104 (10.4%) were old children 1–5 years of age [Graph 1]. The average age of the neonates was 15 days while the minimum age was 7 days. The mean age of infants was 3.0 months, and for older children, it was 2.3 years. PD circumcision devoid of any complication was noted in 897 (89.7%) cases. Remaining 103 (10.3%) developed post-circumcision complications which were easily managed without any significant long-term consequences. The percentage of various complications is depicted in Graph 2.
Graph 1.
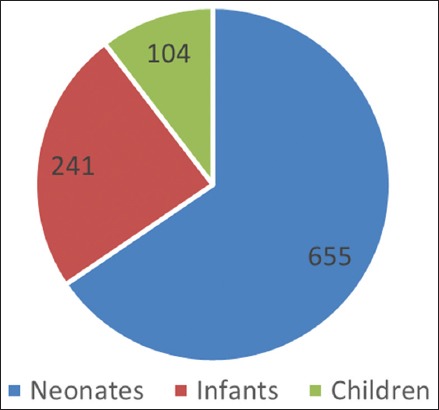
Number of neonates, infants, and children included in the study
Graph 2.
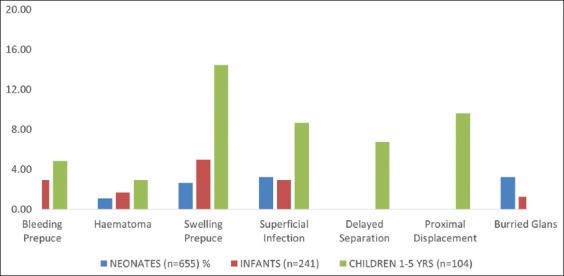
Complications among neonates, infants, and children
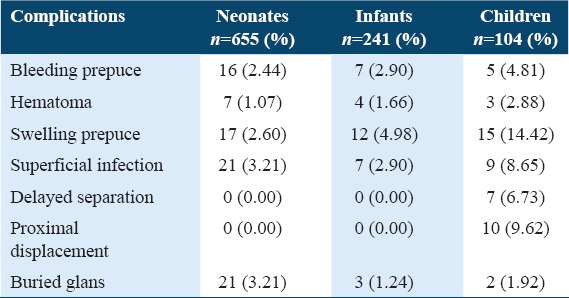
Most common complication noted in neonates was bleeding 16 (2.9%) cases, 4 cases had significant bleed due to edge slippage requiring stitching and device removal, and other 12 neonates had minor ooze from raw surface of glans and were managed by mild compression. Only 7 (0.45%) neonates developed post-PD hematoma for which evacuation of hematoma done along with compression of bleeding area and stitching was done. Swelling prepuce was seen in 17 (2.6%) neonates and buried glans in 21 (3.2%) neonates. In infants, 7 (2.9%) cases developed bleeding; only one needed stitching to stop bleed rest of them were managed by simple compression. Hematoma developed in only four infants while superficial infection was seen in only 7 (2.6%) infants. In older children, swelling prepuce was detected in 14 (14.4 %) cases and proximal displacement in 10 (9.6%). Complications of delayed separation of ring were seen in 7 (6.7%) children but in none of neonates and infants [Table 1].
Table 1.
Complications resulting post-operative circumcision in neonates, infants, and children
Discussion
In our study, the major indication for PD circumcision was religious. Most of the parents were interested for early circumcision during neonatal age. Child illness in early age was the reason for children brought late for circumcision. The overall complication rate was similar to that of surgeries carried out by expert surgeons.[12] The bleeding was seen in only 2.8% of total cases in our study with Plastibell method while bleeding rate up to 35% has been reported in literature by convention techniques.[17] Our results are in consistent with other studies which depict better outcomes with PD circumcision.[13] The PD circumcision is quicker to perform as compared to conventional techniques which are consistent with results of other studies.[18]
The percentage of complications such as bleeding, hematoma, swelling prepuce, superficial infection, and delayed separation was highest among the children more than 1 year as compared to infants and neonates. These results are consistent with results of other studies.[19-21] The cases of erythematous swelling emerged as a result of foreign body reaction (PD) because the redness and swelling subsided promptly (within a day or two) after detachment of the PD. The superficial infection was seen more in neonates as compared to infants. It may be due to the fact that immune response is not well developed in neonates.[22] The buried glans was also reported more in neonates as compared to infants which may be due to small size of penis and adhesions. The complications such as bleeding, swelling, and hematoma were seen more in infants than neonates which are similar to another study conducted at a private hospital in Karachi.[23]
In Muslim societies, circumcision is cultural and religious practice, but there are many benefits of it as well. According to the American Academy of Pediatrics, the circumcision done before the 1st year of life decreases the danger of urinary tract infection as well as risk of penile carcinoma.[8] In our study, the parents and guardians have been very satisfied at large and the complication rate was very minimal and overall acceptable.
Conclusion
The Plastibell circumcision has good safety profile with few certainly correctable early impediments. Plastibell circumcision is safe, quick, easily manageable, and acceptable technique for parents. Complications are low in neonates and infants than older age group.
References
- 1.Stonawski M, Skirbekk V, Hackett C, Potančoková M, Connor P, Grim B, et al. Yearbook of International Religious Demography. Washington, DC: BRILL; 2015. Global population projections by religion: 2010-2050; pp. 99–116. [Google Scholar]
- 2.AAAMiIīiIia-MiBa-Jf A, Al-Bukhari S. Sahih Al-Bukhari (Arabic-English). Vol. 7. Book 77-Hadith 106. 846 AD. Riyadh-Saudi Arabia: DARUSSALAM; 2017. p. 5889. [Google Scholar]
- 3.AAAMiIīiIia-MiBa-Jf A, Al-Bukhari S. Sahih Al-Bukhari (Arabic-English). Vol. 4. Book 60-Hadith 36. 846 AD. Riyadh-Saudi Arabia: DARUSSALAM; 2017. p. 3356. [Google Scholar]
- 4.Laumann EO, Masi CM, Zuckerman EW. Circumcision in the United States. Prevalence, prophylactic effects, and sexual practice. JAMA. 1997;277:1052–7. [PubMed] [Google Scholar]
- 5.Rizvi SA, Naqvi SA, Hussain M, Hasan AS. Religious circumcision:A Muslim view. BJU Int. 1999;83(Suppl 1):13–6. doi: 10.1046/j.1464-410x.1999.0830s1013.x. [DOI] [PubMed] [Google Scholar]
- 6.Hargreave T. Male circumcision:Towards a world health organisation normative practice in resource limited settings. Asian J Androl. 2010;12:628–38. doi: 10.1038/aja.2010.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ozsahin M, Jichlinski P, Weber DC, Azria D, Zimmermann M, Guillou L, et al. Treatment of penile carcinoma:To cut or not to cut? Int J Radiat Oncol Biol Physics. 2006;66:674–9. doi: 10.1016/j.ijrobp.2006.05.053. [DOI] [PubMed] [Google Scholar]
- 8.Kwak C, Oh SJ, Lee A, Choi H. Effect of circumcision on urinary tract infection after successful antireflux surgery. BJU Int. 2004;94:627–9. doi: 10.1111/j.1464-410X.2004.05014.x. [DOI] [PubMed] [Google Scholar]
- 9.Holman JR, Lewis EL, Ringler RL. Neonatal circumcision techniques. Am Fam Physician. 1995;52:511–8. 519-20. [PubMed] [Google Scholar]
- 10.Singh-Grewal D, Macdessi J, Craig J. Circumcision for the prevention of urinary tract infection in boys:A systematic review of randomised trials and observational studies. Arch Dis Child. 2005;90:853–8. doi: 10.1136/adc.2004.049353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiss HA, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants and children:A systematic review. BMC Urol. 2010;10:2. doi: 10.1186/1471-2490-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mousavi SA, Salehifar E. Circumcision complications associated with the Plastibell device and conventional dissection surgery:A trial of 586 infants of ages up to 12 months. Adv Urol. 2008:606123. doi: 10.1155/2008/606123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hammed A, Helal AA, Badway R, Goda SH, Yehya A, Razik MA, et al. Ten years'experience with a novel modification of plastibell circumcision. Afr J Paediatr Surg. 2014;11:179–86. doi: 10.4103/0189-6725.132832. [DOI] [PubMed] [Google Scholar]
- 14.Lazarus J, Alexander A, Rode H. Circumcision complications associated with the Plastibell device. S Afr Med J. 2007;97:192–3. [PubMed] [Google Scholar]
- 15.Sörensen SM, Sörensen MR. Circumcision with the Plasti bell device. A long-term follow-up. Int Urol Nephrol. 1988;20:159–66. doi: 10.1007/BF02550667. [DOI] [PubMed] [Google Scholar]
- 16.Quayle SS, Coplen DE, Austin PF. The effect of health care coverage on circumcision rates among newborns. J Urol. 2003;170:1533–6. doi: 10.1097/01.ju.0000091215.99513.0f. [DOI] [PubMed] [Google Scholar]
- 17.Taeusch HW, Martinez AM, Partridge JC, Sniderman S, Armstrong-Wells J, Fuentes-Afflick E, et al. Pain during mogen or plastiBell circumcision. J Perinatol. 2002;22:214–8. doi: 10.1038/sj.jp.7210653. [DOI] [PubMed] [Google Scholar]
- 18.Magoha GA. Circumcision in various Nigerian and Kenyan hospitals. East Afr Med J. 1999;76:583–6. [PubMed] [Google Scholar]
- 19.Krieger JN, Bailey RC, Opeya J, Ayieko B, Opiyo F, Agot K, et al. Adult male circumcision:Results of a standardized procedure in Kisumu district, Kenya. BJU Int. 2005;96:1109–13. doi: 10.1111/j.1464-410X.2005.05810.x. [DOI] [PubMed] [Google Scholar]
- 20.Bhat BA, Menon K, Jimenez R. Early discharge after neonatal circumcision. Ann Saudi Med. 2001;21:133–4. doi: 10.5144/0256-4947.2001.133. [DOI] [PubMed] [Google Scholar]
- 21.Jan IA. Circumcision in babies and children with plastibell technique:An easy procedure with minimal complications-Experience of 316 cases. Pak J Med Sci. 2004;20:175–80. [Google Scholar]
- 22.Klein JO, Remington JS. Current concepts of infections of the fetus and newborn infant. In: Remington JS, Klein JO, editors. Infectious Diseases of the Fetus and Newborn Infant. Philadelphia: WB Saunders; 2002. pp. 234–43. [Google Scholar]
- 23.Moosa FA, Khan FW, Rao MH. Comparison of complications of circumcision by 'Plastibell Device Technique'in male neonates and infants. J Pak Med Assoc. 2010;60:123–8. [PubMed] [Google Scholar]


