Abstract
Objectives:
Pediatric diaphyseal forearm fractures are common injuries of childhood. Conservative modality of treatments is usually preferred when they are possible. We identified factors that may affect closed reduction success or lead to redisplacement in forearm diaphyseal fractures in children.
Methods:
This was a retrospective study from a level I trauma center on patients up to 18 years of age who presented with forearm diaphyseal fractures from January 1, 2007, to December 31, 2015. Cases were obtained from medical records. Data were collected and confirmed by plain films and medical files.
Results:
We included 145 patients in this study. The majority (86.2%) were boys. Around 29% of trials of closed reduction failed, and the patients were subsequently treated surgically. Following trials of closed reduction, 82.4% of both bone cases were successfully reduced compared to 42.9% of radius shaft cases (P = 0.006). Redisplacement following non-surgical treatment in the first follow-up was found in 32% of both bone cases and 13.3% of radial shaft cases. All Galeazzi cases that were successfully treated with closed reduction presented with no redisplacement on follow-up.
Conclusion:
Immediate surgical management might be considered in older children, especially above 12 years of age since they have a higher failure rate of closed reduction than younger ones. Fracture site should be taken into account when following pediatric diaphyseal forearm fractures following conservative treatments as cases with both bone involvement have a high success rate of closed reduction and considerably high rate of redisplacement compared to others.
Keywords: Childhood injuries, children fractures, diaphyseal fractures, forearm fractures, pediatric fractures
Introduction
Fractures in children are common scenarios facing physicians.[1] Forearm fractures in childhood account for 25% of all other injuries.[2] Some authors believe it accounts for 30%–50% of all pediatric fractures.[3-6] Forearm diaphyseal fractures constitute around 6% of all other children’s fractures.[7] Children between 5 and 14 years of age have the highest fracture incidence.[8] The risk of fracture for children <16 years of age is 42% in boys compared to 27% among girls.[2] Although conservative treatment, depending on the case presentation, is usually preferred to avoid complications of surgical treatment, several studies showed that treatment of diaphyseal forearm fractures has increasingly become surgical.[9-12] The increased rate was attributed due to immediate complications of non-surgical treatment such as redisplacement and loss of mobility.[13] The focus on this subject in the literature varies when it comes to forearm shaft fractures treatment and outcome.[14] Treatment of forearm shaft fractures can be divided as non-surgical or conservative (cast only or closed reduction and cast application) or surgical (percutaneous intramedullary nails or plate and screws fixation). Loss of reduction is the most common complication of pediatric forearm fractures.[8] Redisplacement rate during follow-up ranges from 7 to 27%.[15-18]
Recognition of potential predictors of redisplacement may improve the effectiveness of cast immobilization and identify patients who need surgical intervention rather than conservative management. Our aim in this study is to identify factors that lead to failure of closed reduction or redisplacement in children with diaphyseal forearm fractures.
Methods
A retrospective study was done in a level I trauma center after the approval from the ethical committee. All patients up to age 18 years who presented with complete fractures of radius and/or ulna bone diaphysis from January 1, 2007, to December 31, 2015, who were treated and followed up in outpatient clinics until discharge were included in the study. We did not include any pathological fracture case. Moreover, patients who had no follow-up after their initial presentation in the emergency department were excluded from the study. 167 patients had presented with diaphyseal forearm fractures. Twenty-two cases were excluded, 21 were due to the absence of follow-up, and a case due to pathological fracture secondary to end-stage renal disease.. The aim of this study is to determine potential predictive factors that may lead to redisplacement or failure of closed reduction which are demographics (age and gender), affected bone (radius, ulna, or both bone), fracture pattern (proximal, middle, and distal third), degree of initial angulation, and involvement of radioulnar joint (RUJ). Angle measurements were obtained from X-ray films, and patients’ demographic data, treatment type, and follow-up information were obtained from medical files. Data collected using X-ray films were degree and direction of angulation, site of fracture, and proximal or distal RUJ involvement. Regarding information taken from medical files, we obtained age, gender, hospital course on presentation (cast immobilization, closed reduction, or operative reduction), and time of follow-up from initial presentation. In our institution, orthopedic residents manage all orthopedic cases in ER with senior supervision. All closed reductions were done under conscious sedation. All patients were scheduled for follow-up 1 week after the emergency room (ER) presentation. Above elbow full cast was used in all cases that were managed non-surgically. SPSS software (Version 21.0, IBM Corp., Armonk, NY) was used for data analysis. Descriptive analyses were carried out in terms of frequencies and percentages for categorical variables and mean and standard deviation for continuous variables. Statistical differences between groups were tested using the Chi-square test. P < 0.05 was considered to be statistically significant.
Results
The average age of the patients was 10.16 years (SD: 4.82). We found 125 male cases and 20 female cases with a ratio of (6.25:1). Most fractures involved the distal 1/3 of the diaphysis of both bones (45.5%). Left-sided fractures were 103 (61.68%), right-sided were 62 (37%) review, and bilateral diaphyseal fractures were seen in two cases (1.2%). Seventy-two (49.7%) cases were successfully managed by open reduction and internal fixation by plating and screws, and 25 (17.2%) were managed with closed reduction and intramedullary nails without any further redisplacement. 24 (16.6%) cases were managed with cast only, and another 24 (16.6%) were managed with closed reduction and cast application in the ER.
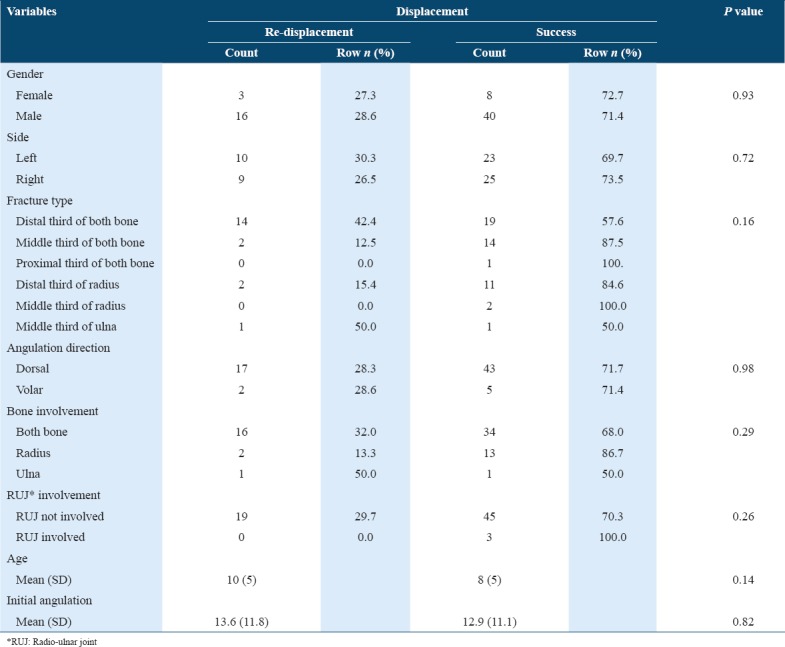
Of 48 patients who had a trial of closed reduction in the ER, 14 (29.2%) patients had unsuccessful closed reduction and were subsequently treated surgically. Thirty-four (70.8%) had initial successful closed reduction, of which 10 (29.41%) cases had their fractures redisplaced in the first follow-up visit (after 1 week) and were subsequently treated surgically. The average age was 9 years (SD: 4) in successful closed reduction group and 12 years (SD: 3) in the failed closed reduction group with statistical significant difference between the two groups (P = 0.02). The average initial angulation was 20.3° (SD: 10.8) in the successful closed reduction group and 24.9° (SD: 8.2) in the failed closed reduction group. Of 34 both bone fractures, which were managed initially with a closed reduction in the ER, 82.4% (n = 28) were successfully reduced while 42.9% (n = 6) of radial shaft fractures were successfully reduced with statistical significant difference (P = 0.006). Successful closed reduction was achieved in 70.7% (n = 29) of dorsally displaced fractures and in 71.4% (n = 5) of fractures with volar displacement. In cases with distal RUJ involvement, 62.5% (n = 5) had failure of closed reduction compared with cases that were successfully treated with closed reduction 37.5% (n = 3) with statistical significant difference (P = 0.02). Successful closed reduction was achieved in 90.9% of middle third fractures of both bone, 78.3% of distal third fractures of both bone, 60% of middle third fractures of the radius, and 33.3% of distal third fractures of the radius diaphyseal fractures with statistical significant difference (P = 0.02) [Table 1]. Sixty-seven patients had non-surgical treatment initially, 33 (49.3%) were treated with cast only while 34 (50.7%) were treated with closed reduction and cast immobilization. Of the 67 patients who were managed conservatively, 19 (28.4%) presented with redisplacement on follow-up. In patients who presented with redisplacement, the average age of presentation was 10.5 years (SD: 5), male-to-female ratio was 16:3, and the average initial angulation was 13.6° (SD: 11.8). Out of both bone diaphyseal fractures, 32% (n = 16) presented with redisplacement while 13.3% (n = 2) of radial diaphyseal fractures presented with redisplacement. There were three Galeazzi cases successfully managed with closed reduction and cast in the ER, none of which redisplaced and they achieved proper alignment. Of all cases in the study, we found 28.6% (n = 2) of volar displacement cases presented with redisplacement and 28.3% (n = 17) of dorsal displacement cases presented with redisplacement [Table 2].
Table 1.
Closed reduction failure versus success
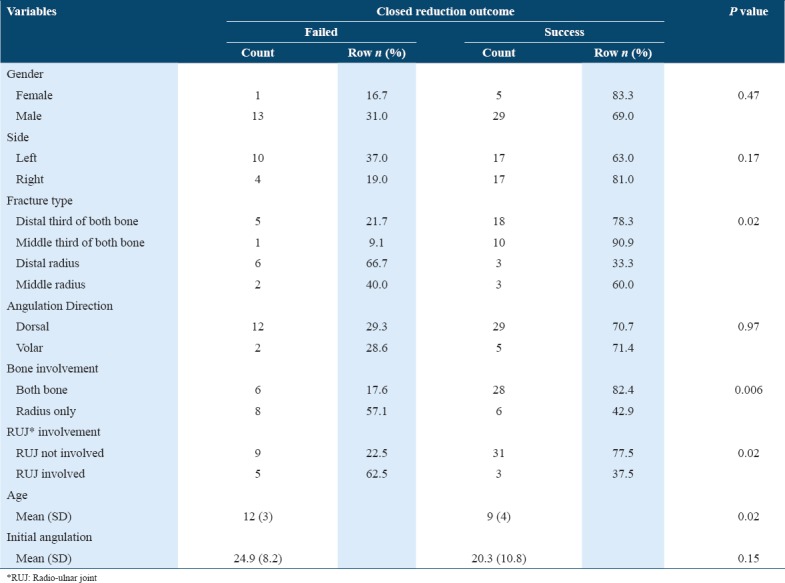
Table 2.
Cases who presented with redisplacement in comparison with stable cases
Discussion
Recently, diaphyseal forearm fractures in children have become increasingly common.[19] Some studies showed that there is an increased interest in surgical treatment of diaphyseal forearm fractures.[9-12] It was reported that there is an increase in the rate of complications following non-operative treatment compared with operative treatment which could be the reason that they have become more surgical.[13] Complications included redisplacement, decreased in range of motion, delayed union, residual deformity, and refracture.[13,20] Of these complications, redisplacement was our main concern along with failure of closed reduction and factors that lead to them. Sinikumpu et al.[21] did not support the recent trend that forearm fractures are becoming more surgical as they found a good long-term outcome following non-operative treatment. Sinikumpu et al.[8] found that the incidence of plating in pediatric diaphyseal of forearm fractures to be 5% compared with 30% incidence of elastic medullary nailing. We found that around 50% of the cases were managed by rigid fixation with plating making it the major treatment modality compared with 17% of the cases managed by intramedullary nailing. In our population, 97 (67%) of all cases were treated operatively, around 34% (n = 33) of them were treated initially with non-surgical treatment modalities (closed reduction and cast or cast only) but failed due to initial closed reduction failure or redisplacement on follow-up. We support the recent trend of surgical treatment as we found a considerably high rate of surgically treated cases primarily or due to failure of conservative treatment modalities. Closed reduction and cast immobilization are considered the gold standard in the treatment of pediatric forearm fractures.[16] Due to higher tendency for fractures to remodel in children, closed reduction is the recommended choice of treatment, especially in children aged 9 years or younger even with high degree of displacement in both radius and ulna fractures as some authors suggested.[22,23] Closed reduction is indicated in patients whose age is 0–8 years with fracture angulation of >15° if they are in the middle and distal third, and more than 10° if it is in the proximal third.[24] Loss of reduction is the most common complication in pediatric forearm fractures and especially in both bone involvement.[8] 29% of cases who underwent closed reduction in the ER failed in our study. We found that they had a higher average of initial angulation degree, higher average age at presentation, had more RUJ involvement, and there were a higher number of cases involving distal third of radius fractures when we compared them to successful closed reduction group with statistical significant difference (P < 0.05). More than half of the distal third of radial diaphyseal fractures were not successfully treated with closed reduction alone, unlike the other sites.
The usual treatment modality used for Galeazzi fracture-dislocation is surgical in adults and conservative in children.[25,26] Closed reduction has shown good outcome in pediatric cases with Galeazzi fracture.[27,28] We found that 62.5% (n = 5) of Galeazzi cases had failure of closed reduction alone, while the rest were successful, with no redisplacement that necessitated surgical treatment with good functional outcome until discharge. Eberl et al.[29] found that only 15% of pediatric Galeazzi cases needed further surgical treatment, which is more satisfactory than what we found (62.5%).
Average age and average initial angulation were found to be higher in failed closed reduction than successful closed reduction groups. Tarmuzi et al.[30] concluded that children with forearm diaphyseal fractures younger than 10 years of age with up to 20° of angulation are acceptable to be treated conservatively. In comparison to our study, we found that the average age of cases who had failure of closed reduction treatment was significantly higher than successful cases (mean = 12 years with SD: 3 versus mean = 9 years with SD: 4) (P value: 0.02). The average initial angulation was higher in failed closed reduction group 24.9° (SD: 8.2) compared to 20.3° (SD:10.8) in successful closed reduction group with no statistical significance (P = 0.15).
Colaris et al.[31] found that redisplacement was seen in 27% of the cases who had a diaphyseal fracture of the forearm, which is close to what we found (28.4%). In the literature, the chance of redisplacement is between 7% and 27% of the cases presented with diaphyseal forearm fractures during follow-up.[15-18] Both bone fractures are believed to be less stable than a single bone fracture.[17,32,33] Admittedly, we found that 32% of both bone diaphyseal fractures in our study showed redisplacement compared to 13.33% of radial diaphyseal cases. There were only two cases of ulna diaphyseal fractures treated conservatively, a case presented with redisplacement. Both bone distal third diaphyseal fractures showed the highest rate of redisplacement compared to other sites in the radius or both bone. To make sure that the fracture is stable and needs no further intervention, we usually follow-up a child with a forearm fracture after 1 week from their initial presentation to the ER following a non-surgical treatment. Half of the cases who presented with redisplacement presented later than 1 week in the initial follow-up which might indicate incompliance with instructions of the treating physicians. Initial angulation is not believed to be a risk factor for redisplacement by some authors.[31,34,35] There is no statistically significant difference in average initial angulation between the redisplaced and the non-redisplaced groups (P = 0.82). However, some authors believe that the initial displacement is an important factor that might lead to redisplacement.[10,16,23] Fractures in older children tend to redisplace more than younger ones.[36,37] We found that the average age of children who presented with redisplacement is more than those who had stable fractures but with no statistically significant difference (P = 0.14).
Our findings are generalizable as all presented patients with follow-up visits were included in the study. Future studies should be focused on the long-term outcome of children with diaphyseal forearm fractures to assess complications following all treatment modalities.
Limitations
The data involved a single-center and it would have been better if more centers were involved for more representative data.
Conclusion
Fracture site should be taken into account with patients following up. Closer follow-up is essential, especially in both bone fracture cases, since they were found to have a higher rate of redisplacement on follow-up as well as a higher rate of initial successful closed reduction in comparison to radial diaphyseal fractures with or without distal RUJ involvement. In addition, immediate surgical management might be considered in older children, especially above 12 years of age, since they have a higher rate of closed reduction failure than younger patients. Dorsal and volar angulations were nearly similar regarding the prevalence rate of close reduction failure, success, and redisplacement. Our study supports the recent trend of operative treatment in pediatric diaphyseal forearm fractures since we found a high rate of cases treated surgically as the primary treatment or secondary to failure of conservative treatments modalities.
Acknowledgments
The authors would like to thank Dr. Rizwan Suliankatchi Abdulkader for his statistical analysis of the study.
References
- 1.Cheng JC, Shen WY. Limb fracture pattern in different pediatric age groups:A study of 3,350 children. J Orthop Trauma. 1993;7:15–22. doi: 10.1097/00005131-199302000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Landin LA Fracture patterns in children. Analysis of 8,682 fractures with special reference to incidence, etiology and secular changes in a Swedish Urban population 1950-1979. Acta Orthop Scand Suppl. 1983;202:1–09. [PubMed] [Google Scholar]
- 3.Bailey DA, Wedge JH, McCulloch RG, Martin AD, Bernhardson SC. Epidemiology of fractures of the distal end of the radius in children as associated with growth. J Bone Joint Surg Am. 1989;71:1225–31. [PubMed] [Google Scholar]
- 4.Jones IE, Cannan R, Goulding A. Distal forearm fractures in New Zealand children:Annual rates in a geographically defined area. N Z Med J. 2000;113:443–5. [PubMed] [Google Scholar]
- 5.Kramhoft M, Bodtker S. Epidemiology of distal forearm fractures in Danish children. Acta Orthop Scand. 1988;59:557–9. doi: 10.3109/17453678809148784. [DOI] [PubMed] [Google Scholar]
- 6.Worlock P, Stower M. Fracture patterns in Nottingham children. J Pediatr Orthop. 1986;6:656–60. doi: 10.1097/01241398-198611000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Landin LA. Epidemiology of children's fractures. J Pediatr Orthop B. 1997;6:79–83. doi: 10.1097/01202412-199704000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Sinikumpu JJ, Pokka T, Serlo W. The changing pattern of pediatric both-bone forearm shaft fractures among 86,000 children from 1997 to 2009. Eur J Pediatr Surg. 2013;23:289–96. doi: 10.1055/s-0032-1333116. [DOI] [PubMed] [Google Scholar]
- 9.Cheng JC, Ng BK, Ying SY, Lam PK. A 10-year study of the changes in the pattern and treatment of 6,493 fractures. J Pediatr Orthop. 1999;19:344–50. [PubMed] [Google Scholar]
- 10.Altay M, Aktekin CN, Ozkurt B, Birinci B, Ozturk AM, Tabak AY, et al. Intramedullary wire fixation for unstable forearm fractures in children. Injury. 2006;37:966–73. doi: 10.1016/j.injury.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Carmichael KD, English C. Outcomes assessment of pediatric both-bone forearm fractures treated operatively. Orthopedics. 2007;30:379–83. doi: 10.3928/01477447-20070501-08. [DOI] [PubMed] [Google Scholar]
- 12.Smith VA, Goodman HJ, Strongwater A, Smith B. Treatment of pediatric both-bone forearm fractures:A comparison of operative techniques. J Pediatr Orthop. 2005;25:309–13. doi: 10.1097/01.bpo.0000153943.45396.22. [DOI] [PubMed] [Google Scholar]
- 13.Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. Complications and radiographic outcome of children's both-bone diaphyseal forearm fractures after invasive and non-invasive treatment. Injury. 2013;44:431–6. doi: 10.1016/j.injury.2012.08.032. [DOI] [PubMed] [Google Scholar]
- 14.Cooper C, Dennison EM, Leufkens HG, Bishop N, van Staa TP. Epidemiology of childhood fractures in Britain:A study using the general practice research database. J Bone Miner Res. 2004;19:1976–81. doi: 10.1359/JBMR.040902. [DOI] [PubMed] [Google Scholar]
- 15.Voto SJ, Weiner DS, Leighley B. Redisplacement after closed reduction of forearm fractures in children. J Pediatr Orthop. 1990;10:79–84. [PubMed] [Google Scholar]
- 16.Jones K, Weiner DS. The management of forearm fractures in children:A plea for conservatism. J Pediatr Orthop. 1999;19:811–5. [PubMed] [Google Scholar]
- 17.Monga P, Raghupathy A, Courtman NH. Factors affecting remanipulation in paediatric forearm fractures. J Pediatr Orthop B. 2010;19:181–7. doi: 10.1097/BPB.0b013e3283314646. [DOI] [PubMed] [Google Scholar]
- 18.Bochang C, Jie Y, Zhigang W, Weigl D, Bar-On E, Katz K, et al. Immobilisation of forearm fractures in children:Extended versus flexed elbow. J Bone Joint Surg Br. 2005;87:994–6. doi: 10.1302/0301-620X.87B7.15774. [DOI] [PubMed] [Google Scholar]
- 19.Sinikumpu JJ, Lautamo A, Pokka T, Serlo W. The increasing incidence of paediatric diaphyseal both-bone forearm fractures and their internal fixation during the last decade. Injury. 2012;43:362–6. doi: 10.1016/j.injury.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 20.Flynn JM, Jones KJ, Garner MR, Goebel J. Eleven years'experience in the operative management of pediatric forearm fractures. J Pediatr Orthop. 2010;30:313–9. doi: 10.1097/BPO.0b013e3181d98f2c. [DOI] [PubMed] [Google Scholar]
- 21.Sinikumpu JJ, Victorzon S, Antila E, Pokka T, Serlo W. Nonoperatively treated forearm shaft fractures in children show good long-term recovery:A population-based matched case-control study with mean 11 years of follow-up. Acta Orthop. 2014;85:620–5. doi: 10.3109/17453674.2014.961867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zionts LE, Zalavras CG, Gerhardt MB. Closed treatment of displaced diaphyseal both-bone forearm fractures in older children and adolescents. J Pediatr Orthop. 2005;25:507–12. doi: 10.1097/01.bpo.0000158005.53671.c4. [DOI] [PubMed] [Google Scholar]
- 23.Franklin CC, Robinson J, Noonan K, Flynn JM. Evidence-based medicine:Management of pediatric forearm fractures. J Pediatr Orthop. 2012;32:S131–4. doi: 10.1097/BPO.0b013e318259543b. [DOI] [PubMed] [Google Scholar]
- 24.Price CT. Acceptable alignment of forearm fractures in children:Open reduction indications. J Pediatr Orthop. 2010;30:S82–4. [Google Scholar]
- 25.Bhan S, Rath S. Management of the galeazzi fracture. Int Orthop. 1991;15:193–6. doi: 10.1007/BF00192292. [DOI] [PubMed] [Google Scholar]
- 26.Giannoulis FS, Sotereanos DG. Galeazzi fractures and dislocations. Hand Clin. 2007;23:153–63. doi: 10.1016/j.hcl.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Mikic ZD. Galeazzi fracture-dislocations. J Bone Joint Surg [Am] 1975;57:1071–80. [PubMed] [Google Scholar]
- 28.Walsh HP, McLaren CA, Owen R. Galeazzi fractures in children. J Bone Joint Surg [Br] 1987;69:730–3. doi: 10.1302/0301-620X.69B5.3680332. [DOI] [PubMed] [Google Scholar]
- 29.Eberl R, Singer G, Schalamon J, Petnehazy T, Hoellwarth ME. Galeazzi lesions in children and adolescents:Treatment and outcome. Clin Orthop Relat Res. 2008;466:1705–9. doi: 10.1007/s11999-008-0268-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tarmuzi NA, Abdullah S, Osman Z, Das S. Paediatric forearm fractures:Functional outcome of conservative treatment. Bratisl Lek Listy. 2009;110:563–8. [PubMed] [Google Scholar]
- 31.Colaris JW, Allema JH, Reijman M, Biter LU, de Vries MR, van de Ven CP, et al. Risk factors for the displacement of fractures of both bones of the forearm in children. Bone Joint J. 2013;95-B:689–93. doi: 10.1302/0301-620X.95B5.31214. [DOI] [PubMed] [Google Scholar]
- 32.Zamzam MM, Khoshhal KI. Displaced fracture of the distal radius in children:Factors responsible for re-displacement after closed reduction. J Bone Joint Surg [Br] 2005;87(B):841–3. doi: 10.1302/0301-620X.87B6.15648. [DOI] [PubMed] [Google Scholar]
- 33.Bohm ER, Bubbar V, Yong Hing K, Dzus A. Above and below-the-elbow plaster casts for distal forearm fractures in children. A randomized controlled trial. J Bone Joint Surg Am. 2006;88:1–8. doi: 10.2106/JBJS.E.00320. [DOI] [PubMed] [Google Scholar]
- 34.Proctor MT, Moore DJ, Paterson JM. Re-displacement after manipulation of distal radial fractures in children. J Bone Joint Surg[Br] 1993;75 B:453–4. doi: 10.1302/0301-620X.75B3.8496221. [DOI] [PubMed] [Google Scholar]
- 35.Boyer BA, Overton B, Schrader W, Riley P, Fleissner P. Position of immobilization for pediatric forearm fractures. J Pediatr Orthop. 2002;22:185–7. [PubMed] [Google Scholar]
- 36.Asadollahi S, Pourali M, Heidari K. Predictive factors for re-displacement in diaphyseal forearm fractures in children-role of radiographic indices. Acta Orthop. 2017;88(1):101–8. doi: 10.1080/17453674.2016.1255784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodríguez-Merchán EC. Pediatric fractures of the forearm. Clin Orthop Relat Res. 2005;432:65–72. [PubMed] [Google Scholar]


