Abstract
High-intensity interval training (HIIT) has emerged as an attractive alternative to traditional continuous exercise training (CT) programs for clinical and healthy populations who find that they can achieve equal or greater fitness benefits in less time. Land-based HIIT may not be an appropriate choice for some participants. Few studies have explored the acute responses and chronic adaptations of HIIT in an aquatic environment, and no study has compared the cardiometabolic responses of an aquatic-based program to a land-based HIIT program. Shallow-water aquatic exercise (AE) programs utilizing HIIT have elicited comparable and, in some cases, greater physiological responses compared with constant-intensity or continuous AE regimens. Factors that may explain why HIIT routines evoke greater cardiometabolic responses than CT protocols may be based on the types of exercises and how they are cued to effectively manipulate hydrodynamic properties for greater intensities. Favorable aquatic HIIT protocols such as the S.W.E.A.T. system may serve as a beneficial alternative to land-based HIIT programs for clinical, and athletic populations, potentially reducing the likelihood of associated musculoskeletal and orthopedic complications. Hence, the purpose of this review is to examine the role of AE as an alternative safe and effective HIIT modality.
Keywords: aquatic exercise, water fitness, HIIT, cardiometabolic training
‘High-intensity interval training (HIIT) has emerged as an attractive exercise alternative for clinical and healthy populations who may be more likely to incorporate brief bouts of vigorous physical activity into a busy day.’
Introduction
As a cardioprotective lifestyle intervention, structured aerobic exercise training (AET), increased lifestyle physical activity, or both, have been widely promoted for the prevention and treatment of cardiovascular disease and other cardiometabolic risk factors.1,2 Independent of dietary intervention, AET improves central and peripheral cardiovascular function and all the risk factors associated with the development of metabolic syndrome.3-6 Furthermore, improvements in cardiorespiratory (CR) fitness from AET are associated with reduced cardiovascular and all-cause mortality in men and women across the life span.7-9 Despite the overwhelming evidence to support the benefits of regular AET, less than half of adults meet the US recommendations of at least 150 min/wk of moderate-intensity or 75 min/wk of vigorous-intensity aerobic exercise.1,4,10 Because the most commonly reported barrier to AET is “lack of time,” it seems reasonable to suggest that effective, time-saving exercise regimens may be more likely to be embraced by habitually sedentary individuals seeking improved health and fitness.11-13 High-intensity interval training (HIIT) has emerged as an attractive exercise alternative for clinical and healthy populations who may be more likely to incorporate brief bouts of vigorous physical activity into a busy day.14 HIIT is characterized by short bursts of exercise performed at a high intensity. This type of exercise is performed as work-rest intervals with exercise intensities approximately 85% to 95% of maximal heart rate (HR) or >90% maximal oxygen consumption (VO2max) followed by periods of rest or moderate-intensity active recovery.3,15,16 Regardless of the conditioning status, the recovery period following a work interval is designed to allow an individual to perform repeated bouts at an intensity that could not be maintained during a continuous exercise training (CT) session.
HIIT is focused on the inverse relationship between intensity and duration of training. Previous studies supported 75 min/wk of vigorous exercise as sufficient to maintain cardiovascular health17-20; therefore, short-term sprint or high-intensity intermittent training is considered an ideal standard for the vigorous-intensity model.17-20 The HIIT method is considered a time-efficient way to obtain similar and, in some cases, greater physiological and clinical benefits than those observed with traditional aerobic CT programs.3,17,21-24 When HIIT is prescribed at intensities near an individual’s VO2max, central CR and peripheral adaptations will promote increased aerobic capacity and endurance performance. Improvements in blood pressure, endothelial function, lipid profiles, and myocardial function have been observed with HIIT programs.14,25-28 However, further research is needed to compare the effects of HIIT and CT using both land-based and aquatic-based modalities for athletic, mainstream, and clinical populations. Specifically, the purpose of this review is to examine current evidence in order to evaluate the viability of aquatic exercise (AE) as a safe and effective type of HIIT modality.
Selected Land-Based Evidence
Among patients with cardiometabolic disorders (including those with chronic heart failure) who have undergone land-based HIIT compared with traditional CT forms, greater relative improvements in VO2max, resting HR, ejection fraction, brachial artery flow-mediated dilation, and peak oxygen pulse have been reported.25,29-32 Moreover, reduced lactate accumulation and lower ratings of perceived exertion (RPE), reflecting peripheral metabolic adaptations, have also been observed.33 It is believed that the brief, repeated near-maximum-intensity stimuli in a HIIT program are primarily responsible for the greater improvements in VO2max, mitochondrial biogenesis, and cardiovascular autonomic function versus traditional CT programs.34-36 Studies examining endothelial function following a HIIT program compared with CT have shown mixed results. Whereas some studies suggest that favorable changes in cardiovascular disease risk will be seen in training programs that are greater than 8 weeks in duration,3 improvements in oxidative capacity of trained skeletal muscles have been observed in as little as 2 weeks for older adults.14 Furthermore, despite the lower volume of total work performed and training time undertaken in HIIT compared with CT groups, greater improvements in left ventricular function with similar improvements in plasma volume, cardiac output, and stroke volume have been observed after only 6 HIIT cycling sessions in healthy young men.28 Collectively these results are clinically significant, promoting the effectiveness of HIIT for both clinical and healthy populations.
HIIT is often perceived as more enjoyable than moderate-intensity CT programs because it can offer both a physiologically and psychologically novel and challenging approach to complement an existing exercise regimen.37 Although greater motivation may be required to perform HIIT, numerous studies of selected clinical and nonclinical populations have reported high adherence rates and less boredom because of varied protocols compared with CT programs.37,38 Moreover, although originally developed to further enhance athletic performance, HIIT has now been increasingly adopted by mainstream and clinical populations.32,39,40 Despite its growing popularity, each subgroup should be informed of potential risks prior to the onset of a HIIT program. This primarily includes the increased risk of injuries that may occur in those who perform work bouts beyond their maximal-intensity threshold.41 However, when clinical populations perform HIIT under supervision and within the guidelines of an appropriately prescribed exercise or workout plan, this form of training may be considered a safe and well-tolerated form of AET.3,37,42,43
HIIT in an Aquatic Environment
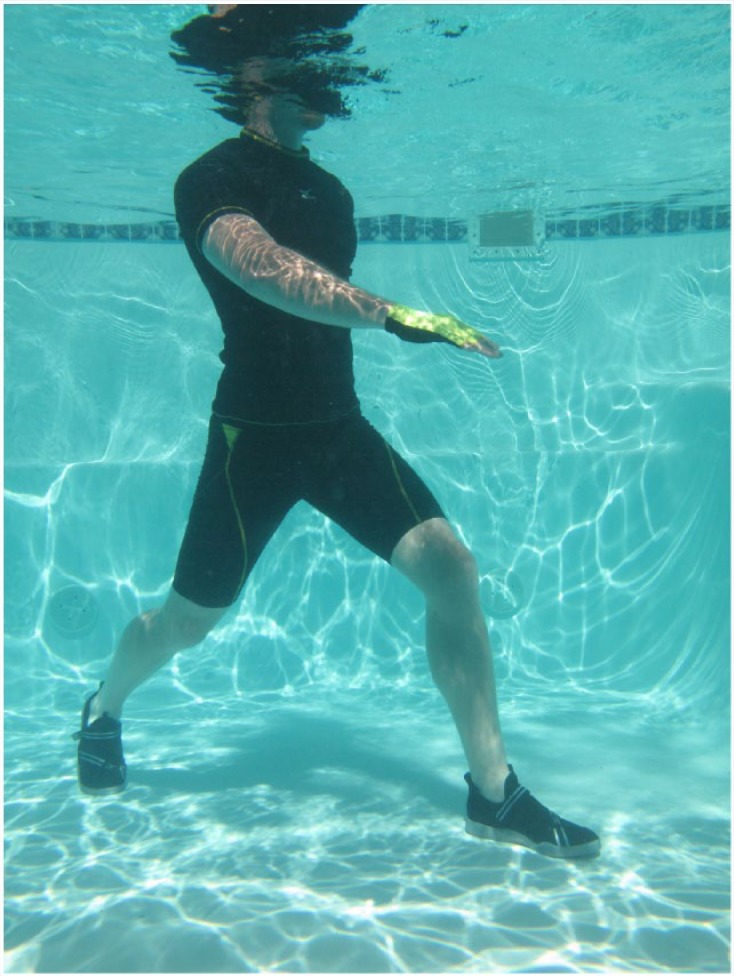
Because of the unique hydrodynamic properties, HIIT performed in an aquatic environment presents individuals with a safe and lower weight-bearing aerobic alternative to land-based interval training programs.44 Previous studies of clinical populations in AE regimens and interval training swimming programs have reported significant aerobic, metabolic, musculoskeletal, CR, and psychological benefits.1,45-62 AE performed primarily in an upright stance, is considered an adaptation of land-based physical activity (ie, walking, jogging, calisthenics, and locomotor/resistive movements) to a water medium63 (Figure 1). Similar to land-based protocols, aquatic HIIT regimens instruct participants to complete alternating “very-hard” segments with “easy” recovery periods using an interval approach. Because of the viscosity and density of water, major movements aimed at increasing velocity will result in greater resistance to flow, creating an ideal environment for augmenting work output and energy expenditure.64-66
Figure 1.

Shallow-Water Running (Photo by Kataqua; Courtesy of WaterFit).
The same hydrodynamic properties that influence velocity of movement also affect HR responses.67 Accordingly, traditional land-based methods to prescribe exercise intensity such as HRs or velocity are considered less accurate in an aquatic environment depending on water depth and temperature.68-71 Recent studies have reported a more accurate self-regulated approach to prescribing intensity during aquatic resistance exercises through visual and verbal perceptual cuing systems that include a RPE scale.72 To elicit these intensity-dependent physiological responses during aquatic HIIT, systematic manipulation of several potential modulators are recommended and may include the following: (1) changing body position; (2) segmental actions of upper and lower limbs;73 (3) increasing speeds and surface area of the movement patterns that are executed;73-75 or (4) adding equipment such as gloves, paddles, bands, or other resistive devices74,76,77 (refer to Sidebar 1).
Sidebar 1 Selected Physiological Characteristics of Upright Immersion.
During immersion, the majority of physiological effects are a result of the unique properties of water, including buoyancy, hydrostatic pressure, viscosity, and thermodynamics.78 The effects on a body during immersion are described below.
Buoyancy
Because a human is less dense than water, the body will be individually offloaded, depending on body composition and the depth of immersion.
Hydrostatic Pressure
Immersion results in enhanced venous return, displacing blood upward through the venous and lymphatic systems, finally reaching the chest and into the heart.
Cardiac volume increases 27% to 30% with immersion to neck level, resulting in a 35% mean stroke volume increase even at rest.78
Standing in water that is about neutral temperature (33.5°C-35.5°C) at xiphoid depth, a person’s cardiac filling and stroke volume increases. This response typically results in a 12% to 15% decrease in HR.78
In warm water (36°C-38°C), the HR and corresponding cardiac filling rise to a greater extent.78
At chest depth, hydrostatic pressure compresses the chest wall resulting in an increase in the total work of breathing by approximately 60%, especially during inspiration.78,79
Viscosity
Moving through water feels “heavy” because of the friction of the moving fluid. Drag forces and turbulence create resistance to a limb or body moving through water.
Resistance increases exponentially as more force is applied and drops to 0 almost immediately when the force (movement) stops. Participants can fully control the level of resistance overload by simply changing speed of the movement.78,80
At a given speed, when the surface area of the limb or added equipment is increased, resistance overload increases.81 Simple webbed gloves can provide additional overload to achieve higher intensity. The combination of speed and surface area provides a broad intensity progression.
Thermodynamics
Water is an efficient conductor of heat, transferring heat 25 times faster than air, and affects HR and oxygen consumption.78,82
Exercising in warm water (30°C-35.5°C) results in HRs similar to that on land.
Aquatic cycling and running in cold to cool water (18°C-25°C) produces HRs that are 10 to 15 beats/min lower than what is typical for land exercise.82 Water temperature needs to be considered for HIIT design. Neutral temperatures (33.5°C-35.5°C) may provide both a safe and comfortable environment for vigorous exercise.
Acute Physiological Responses to Immersion
Although only a limited number of studies have explored the benefits of HIIT in an aquatic environment, shallow-water AE programs utilizing HIIT have reported similar and, in some cases, greater acute CR responses compared with constant-intensity or continuous AE protocols.47,62,68,70,71,81 Using a 32-minute upper- and lower-body water HIIT routine, investigators observed greater oxygen uptake (VO2), HR, and energy expenditure (EE) as compared with a continuous-intensity comparison group.70 Similarly, researchers evaluated a shallow-water aquatic HIIT protocol that included 15-s alternating very hard/easy intervals, measuring the EE during 12 separate 3- to 5-minute CR and muscular endurance segments.63,83 Overall, greater VO2, HR, and EE occurred during the CR segments as compared with traditional CT protocols.2,63,66,67,84,85 Of note, the hover jog segment, which involved repeated jumping and jogging whole body exercise, elicited the greatest cardiometabolic response of the 12 segments examined (8.3 kcal/min; 7.3 metabolic equivalents, and 79% age-predicted maximum HR).
Collectively, these studies are provocative, given the fact that HR responses in water are typically lower than those observed during land-based exercise.86 Because the effects of hydrostatic pressure on the CR system cause a redistribution of blood to the thoracic region, a subsequent increase in preload and larger stroke volume should result in a reduction in HR.87 Factors such as increased water temperatures, water submersion levels, and relative workloads may also serve as aerobic and chronotropic modulators.67,88-90 Accordingly, aquatic HIIT appears to offer an effective CR stimulus when greater movement velocities are performed to overcome the hydrodynamic and increased resistive forces of water.63,65 This has been substantiated by acute shallow-water HIIT responses >90% HRmax, supporting this training modality as a bonafide stimulus to improve CR fitness.1,4,51,63,68,71
Several conditions may help explain how water-based HIIT routines can elicit greater cardiometabolic responses as compared with conventional CT protocols. These include the following: (1) as compared with deep-water exercise, shallow-water exercise elicits greater VO2 and HR responses because of increased ground reaction forces and decreased effects of hydrostatic pressure, particularly on the lungs68,89,91; (2) increased velocity of movements result in greater speeds that further increase intensity and, thus, the energy cost of movement86,92; (3) engagement in vigorous full range of motion whole-body exercises that involve varied movement patterns, anatomical planes, joint angles, and muscle groups result in increased drag force,62 frictional resistance, and work output63,84; and (4) inclusion of a verbal and visual cueing system that allows participants to maximize speed needed to achieve individual overload (instead of working to a set beat of music or pace) can facilitate higher-intensity work bouts.63,70
Additionally, an important and often overlooked benefit of aquatic HIIT is the opportunity to achieve higher intensities along with a reduction in force and joint compression that occurs compared with traditional land-based exercise.65 It is estimated that immersion to the xiphoid process decreases limb loading by ≥60%.78 Given a lesser stress on the body, aquatic HIIT may be perceived as less strenuous and, therefore, a more enjoyable form of exercise.48,52,93 Furthermore, favorable adaptations and improvements from aquatic HIIT have also been documented in elderly and obese individuals as well as those with chronic conditions such as osteoarthritis and fibromyalgia.33,51,76,94-99 For these clinical populations, aquatic HIIT may attenuate other participation barriers, including poor coordination or fear of injury.63
Cardiometabolic Adaptations to HIIT During Upright AE
Although few interventions have explored the cardiometabolic effects of HIIT in water, positive outcomes have noted similar, and in some cases, distinct adaptations previously not identified in land-based studies.100-104 Table 1 demonstrates the efficacy of shallow and deep water, shallow-water treadmill, and traditional swimming training programs. Table 2 illustrates 2 single-bout studies that reflect higher-intensity training responses using 2 different exercise designs. One utilizes a variety of movements typically performed during AE group classes, whereas the other includes a single movement involving deep-water running. Both methods show promise that HIIT can be achieved under different conditions. Participants can choose the type of exercise they prefer and apply water-specific HIIT methods to reach their intensity goals (Figures 2 and 3).
Table 1.
Selected Aquatic HIIT Training Studies.
| Author (Year) | Participants and Sample Size | Program Design | Intensity/Duration | Key Findings |
|---|---|---|---|---|
| Broman et al105 (2006) | Elderly healthy women | Deep-water running HIIT: 2 times/wk, 8 weeks | AHIIT: 15-s to 3-minute intervals, at 75% heart rate (HR) maximum, for 10 minutes, with 2-minute rest between each interval | AHIIT: Increased VO2max (10%; P <.01) and maximal VE (14%; P <.01); lower resting HR (8%; P < .01) and submaximum HR (3%; P < .01) |
| AHIIT (12) | CON: No exercise | CON: No change | ||
| CON (9) | ||||
| Martin et al100 (1987) | Sedentary middle aged men and women | Swimming + land-based circuit training; swim: combination of continuous and HIIT; 3 times/wk, 12 weeks | AHIIT: 2 miles/session, continuous + interval training; land-based circuit, 15 exercises, targeting muscle endurance | AHIIT: Increase in peak supine VO2 (10%; P < .05) and peak supine left end-diastolic volume (18%); decrease: upright and supine resting HR (P < .005) |
| AHIIT (15) | CON: No exercise | CON: No change | ||
| CON (9) | ||||
| Mohr et al101 (2014) | Sedentary, premenopausal women with mild hypertension | Swimming; HIIT swim or moderate-pace swim; 3 times/wk, 15 weeks | AHIIT: 6-10 rounds of sprint freestyle, 30 s each, 2 minute passive recovery in between, for 25 minutes | AHIIT: Greater improvements (P < .05): systolic BP, mean arterial pressure, resting HR versus Moderate and CON |
| AHIIT (21) | Moderate: 1 hour continuous swim | |||
| Moderate (21) | CON: No exercise | |||
| CON (21) | ||||
| Rebold et al104 (2013) | Young, healthy, men and women | Shallow-water treadmill running; HIIT Tabata intervals (20 s work/10 s rest); 2 times/wk, 8 weeks | AHIIT: Treadmill running with all out sprints, 8 rounds, for 20 minutes | AHIIT: Increase in mean aerobic power, flexibility (P < .05) |
| AHIIT (13) | CON: No exercise | CON: No change | ||
| CON (12) | ||||
| Wilber et al103 (1996) | Young, trained male runners | Deep-water running or land-based treadmill running HIIT combination; 5 times/wk, 6 weeks | Both groups combined HIIT and moderate intensity running for 30 minutes per session | During HIIT, both groups achieved 90%-100% VO2max |
| AHIIT (8) | ||||
| Land treadmill HIIT (8) |
Abbreviations: HIIT, high-intensity interval training; AHIIT, aquatic HIIT; CON, control group; BP, blood pressure.
Table 2.
Selected Single-Bout Aquatic HIIT Studies.
| Author (Year) | Participants and Sample Size | Program Design | Intensity/Duration | Key Findings |
|---|---|---|---|---|
| Nagle et al63 (2013) | Young healthy women | Shallow-water HIIT full-body exercises for cardio + arms only for muscular conditioning | AHIIT: 15 s moderate/15 s hard-very hard/15 s easy; 2-4 rounds each exercise, 30 minutes, single bout | AHIIT: Cardio + muscular segments (30 minutes): 65%-87% heart rate maximum (HRM) |
| AHIIT (21) | Cardio only (20 minutes): 82%-87% HRM; highest was 90% HRM | |||
| Wilder et al107 (1993) | Healthy men and women | Deep-water running, single-bout graded exercise test using leg cadence speed to predict HR response | AHIIT: 5 sets, 2 minutes each at somewhat hard; 30 s rest; 8 sets, 1 minute at hard; 30 s rest; repeat set 1 for total time 37 minutes | AHIIT: High correlation; cadence and HR |
| AHIIT (20) | Mean HR: slow, 51% HRM; very fast, 86% HRM |
Abbreviations: HIIT, high-intensity interval training; AHIIT, aquatic HIIT.
Figure 2.

Shallow-Water Treadmill Running (Courtesy of Hydroworx).
Figure 3.

Deep-Water Running (Photo by Tracy Frankel; Courtesy of WaterFit).
In a cohort of older women, Broman et al105 studied the effects of an 8-week deep-water running interval training program on CR outcomes and found that submaximal work rates, aerobic capacity, and maximal minute ventilation improved during a postconditioning land-based cycle ergometer test. Aerobic power measured throughout cycle exercise improved 10% across 8 weeks, suggesting possible transfer effects to land-based exercise. It was felt that the peripheral adaptations observed were attributed to the effects of increased hydrostatic pressure and ability to stimulate capillary proliferation and oxidative enzyme activities. Of note, in this elderly sample, maximal ventilatory capacity improved by 14%, revealing the potency of water’s immersive qualities and ability to create compressive forces on the body. Likewise, Wilber et al103 used deep water to examine water run training and ability to maintain aerobic performance in a younger sample. By comparing deep-water with traditional treadmill-based training, a combination of high- and moderate-intensity training methods was used by both groups. Although this study did not exclusively offer an aquatic or land-based experimental HIIT-only group, results showed no differences between groups in terms of improvements in oxygen uptake, ventilatory threshold, running economy, or plasma norepinephrine. Results showed deep-water run training as an ideal alternative to land-based forms, with the additional benefits of reduced musculoskeletal stress and ability to recruit additional upper-body musculature. Improved anaerobic power and flexibility, with reduced lower-extremity musculoskeletal stress, was also shown in young men and women following an 8-week aquatic HIIT treadmill running program when compared with a nonexercise control.104 This is encouraging because some land-based HIIT studies resulted in up to a 50% injury rate, whereas aquatic HIIT programs have reported no injuries by participants in the programs.63,99,106 Collectively, results of previous aquatic deep- and shallow-water training studies suggest that aquatic HIIT can be an effective CR stimulus without the risks of land-based HIIT exercise. Furthermore, this may be particularly valuable to athletes who need to maintain their CR fitness while undergoing rehabilitation, postrehabilitation, or while cross-training or for those unable to engage in a land-based running program.103
Cardiometabolic Adaptations to HIIT During Swimming
Two investigations have studied the cardiometabolic effects of aquatic HIIT using swimming while performed in a prone or supine body position. In contrast to exercising in water in an upright position, a supine body position will enhance venous return and preload and require a greater energy cost of breathing because of the greater hydrostatic pressure of water.78 Martin et al100 studied a group of 12 sedentary men and women who underwent a 12-week intensive interval swim plus land-based circuit training program and found improvements in skeletal muscle circulatory responses and increased cardiac output. Using a land-based upright cycling protocol, improvements in VO2peak, end-diastolic volume, and hyperemic blood flow were noted, whereas left ventricular ejection fraction was unchanged, suggesting that physiological effects of swim training are transferable to other forms of exercise.
Similarly, Mohr et al101 found that a 15-week HIIT swimming program reduced systolic blood pressure and improved water- and land-based exercise capacities in a sample of mildly hypertensive women. Although improvements were not significantly greater than that in the moderate-intensity CT group, the HIIT training protocol was accomplished in 50% less total time per week. Of interest was the greater decline in resting systolic and mean arterial pressure of the HIIT group only in contrast to previous results reported during land-based HIIT programs.38,42,108 Given that previous swimming CT interventions have demonstrated hypertensive effects through changes in endothelial function, arterial compliance, and cardiovagal baroreflex sensitivity,56 it is possible that the hydrostatic forces exerted while maintaining a supine body position compounded by a greater intensity stimulus of HIIT may, in part, be associated with the positive changes in systolic blood pressure and mean arterial pressure observed in this study. Although the aquatic HIIT studies described included control groups, none of the research designs incorporated a land-based HIIT comparison group. However, a closer examination of the physical properties of water and how they might affect central and peripheral CR adaptations during a high-intensity AE or swimming program holds promise and should be investigated further.
AE HIIT Program Design
AE HIIT has increased in popularity and shows promise as an effective, time-efficient training method across apparently healthy, clinical, and athletic populations. A programming challenge of aquatic HIIT is to create opportunities for participation, especially for those who may have mobility limitations, poor balance, or inability to achieve higher intensities during land-based exercise. This may also appeal to athletes who want to engage in a cross-training program that provides a challenging CR stimulus with reduced impact on the musculoskeletal system. Similar to adopting any lifestyle behavior, a desire and readiness to begin an aquatic HIIT is the first prerequisite. Although aquatic HIIT may appeal to all ages, the above-referenced subgroups may have special needs or objectives, necessitating modifications in program design.
Healthy and Athletic Populations
It is important to first determine the goals and outcomes desired from an aquatic HIIT program (eg, fat loss, improved CR fitness), including the energy system to be targeted. Aquatic HIIT training can provide a conditioning stimulus for a particular energy system based on the manipulation of several variables: (1) intensity and duration of work interval, (2) nature and duration of rest interval, (3) number of intervals repeated, (4) number of sets (series) completed, (5) nature and duration of recovery between sets, and (6) modality chosen.109 For example, shorter intervals (10-15 s) performed at extremely high intensities for short periods followed by longer rest periods (1:4 work to rest ratio) will target the adenosine triphosphate-phosophocreatine and anaerobic glycolytic systems. This approach also limits the associated magnitude of neuromuscular fatigue, allowing the athlete to continue to focus on other (ie, tactile) training components. Longer intervals (30 s to 2 minutes) performed at >70% to 95% HRmax with brief rest periods (1:1 or less) will challenge the aerobic system and promote greater EE. Furthermore, for healthy adults or athletes to achieve a desired outcome (ie, cross-training, rehabilitation), aquatic HIIT may be especially beneficial at a particular time of year, complementing a seasonal training regimen.
Clinical Populations
Prior to undertaking an aquatic HIIT program, particular clinical subgroups may require an assessment of risk factors, medical history, symptomatology, and/or diagnostic testing for evidence of exercise-induced myocardial ischemia, threatening arrhythmias, or coexisting musculoskeletal and/or metabolic disorders.5,15 Previous concerns regarding the appropriateness of HIIT have focused on water’s immersive effects on the body, a reduction in vascular capacitance, translocation of blood volume to the thoracic region with concomitant increases in cardiac preload and central venous pressure, and a resulting risk of decreased stroke volume. However, recent studies have indicated that patients with severely reduced left ventricular function (but clinically stable) as well as patients with coronary disease are able to increase cardiac output adequately during controlled water immersion and swimming.15,110,111
Other prescriptive considerations for older or deconditioned adults prior to starting an aquatic HIIT program include the following76,106: (1) acquiring the skills needed for proper alignment and stabilization in water; (2) exercising for a minimum of 20 minutes at 70% to 85% of HRmax; (3) using proper progression of frequency and intensity of workouts, interspersed with recovery days; and (4) employing appropriate warm-up and cool-down exercises.
Aquatic HIIT Programming Considerations
Although numerous AE training programs have become widely available, the S.W.E.A.T. method is particularly noteworthy for its ability to achieve HIIT-related CR responses in both shallow and deep water.63 The S.W.E.A.T. method developed by WaterFit has been found to be an effective training method in shallow and deep water, resulting in improved cardiovascular and muscular endurance for young women, for a woman diagnosed with muscular dystrophy, and one with severe physical disabilities.63,83,112,113
The primary types of exercises performed during HIIT studies have typically involved walking or running in shallow or deep water. However, the S.W.E.A.T. method encompasses a variety of movements designed to improve fitness as well as functional mobility on land.106 The method incorporates functional movement patterns such as push and pull, rise and lower, rotation, and locomotion, into full-body exercises. These elements are then combined with 6 basic movements, including walking, jogging, kicking, jumping, rocking, and scissors (Figure 4) or a combination of jump and jog called “hover jogs” (Figure 5). These functional patterns are performed as intervals by coaching participants to regulate intensity using a series of cues defined by the S.W.E.A.T. acronym. The cues are used to coach changes in the following: speed of cadence using pushing and pulling effort; the working positions of the body vertically, targeting rise and lower; enlarging a move to full range of motion for functional flexibility; work the limbs around the body or joint using multidimensional planes for rotation; and travel through water for locomotion. These coaching cues create waves of continuous high- and low-intensity intervals that allow participants to gear up or gear down intensity based on specific interval times or RPE. This method provides hundreds of exercise variety options within a wide range of interval intensities. Participants are encouraged to individualize the effort needed to achieve their goals by choosing a self-regulated intensity using RPE in order to set their own pace. Studies using this method have reported high program adherence (94%), perhaps because of the wide variety in movements and interval options.83,106,113
Figure 4.
Scissors Basic Move Using the S.W.E.A.T. Method (photo by Tracy Frankel; Courtesy of WaterFit).
Figure 5.

Hover Jogs, S.W.E.A.T. Method (Photo by Kataqua; Courtesy of WaterFit).
An important advantage of the S.W.E.A.T. method is that it effectively uses the physical properties of water to achieve a conditioning stimulus for healthy and clinical populations. By using a method of cues that coach participants to perform movements that maximize workloads by individualizing changes, the S.W.E.A.T. method describes speed, surface area, impact, range of motion, planes of movement, and travel through the water and is designed to include the following cues:
S: Changes in Surface area and Speed
W: Changes in impact by using the Working positions of rebound (jumping), neutral (chest submerged, feet touch lightly), suspended (buoyant work performed without feet touching bottom), and extended (standing tall, feet grounded on the bottom)
E: Enlarge the movement (extending to fuller range of motion)
A: Work Around the body or joint by changing planes (sagittal, transverse, and multiplanar)
T: Traveling through water forward, backward, and on diagonal
Webbed gloves are used during the program to enhance the surface area and to provide additional overload to achieve higher intensity as needed. Each variable when applied changes how the properties of water are engaged against the body for varied and interval-based training. A sample segment can be found in Sidebar 2.
Sidebar 2 Sample S.W.E.A.T. Segment.
The following S.W.E.A.T. sample protocol is a shallow-water HIIT segment that can be added to a water workout or performed on its own. Participants are asked to find the depth that reaches approximately to the xiphoid, then practice the skills at slow speeds and check for proper alignment (ears, shoulders, hips aligned). Participants gradually increase speed and effort to adapt progressively to the higher resistance. They are reminded to breathe fully, strengthening the muscles working against hydrostatic pressure. The intensity cues to follow include the following:
- Choose a coordinated basic move. Arms and legs must work together for stabilization and movement efficiency. Webbed gloves can assist with stabilization and can help “grip” the water for better movement quality. For example, choose scissors for 3 minutes then the hover jogs for 2 minutes:
Apply the S.W.E.A.T. cues for intensity variations. Recommended intervals are the following: 15 s at moderate pace, 15 s hard to very hard (increase speed), 15 s easy. Repeat the intervals using a different variation, or change the basic move until the desired interval segment is completed.
Conclusion
HIIT appears to offer similar cardiometabolic benefits as CT, with the advantage of providing a challenging, novel, highly effective, and time-saving approach to AET. More important, HIIT may represent a safe and effective exercise alternative for clinical, healthy, and athletic populations who desire a low-impact physical conditioning program to achieve a cardiovascular training effect, health fitness objectives, or rehabilitative goals. Although additional research is warranted, aquatic HIIT appears to convey training benefits similar to that of land-based HIIT, with the added hydrodynamic advantage of reduced musculoskeletal stress as a result of the aquatic medium.2,100,104,107 Future studies of aquatic versus land-based HIIT are needed to compare respective central and peripheral adaptations as well as the incidence of associated metabolic, musculoskeletal, and cardiovascular complications. Specifically, the S.W.E.A.T. program shows potential as an effective aquatic HIIT method that provides a wide variety of movements to keep participants motivated. Further study is warranted to determine the most effective components of an aquatic-based HIIT regimen, which may challenge or even exceed the physiological and clinical adaptations achieved during land-based programs.
Acknowledgments
The authors would like to acknowledge Dr Jacquelyn Nagle for her editorial assistance, hard work, and support.
References
- 1. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 9th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 2. Campbell JA, D’Acquisto LJ, D’Acquisto DM, Cline MG. Metabolic and cardiovascular response to shallow water exercise in young and older women. Med Sci Sports Exerc. 2003;35:675-681. [DOI] [PubMed] [Google Scholar]
- 3. Kessler HS, Sisson SB, Short KR. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports Med. 2012;42:489-509. [DOI] [PubMed] [Google Scholar]
- 4. Garber CE, Blissmer B, Deschenes MR, et al. American College of Sports Medicine position stand: quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334-1359. [DOI] [PubMed] [Google Scholar]
- 5. Franklin BA. Preventing exercise-related cardiovascular events: is a medical examination more urgent for physical activity or inactivity? Circulation. 2014;129:1081-1084. [DOI] [PubMed] [Google Scholar]
- 6. Carroll S, Dudfield M. What is the relationship between exercise and metabolic abnormalities? A review of the metabolic syndrome. Sports Med. 2004;34:371-418. [DOI] [PubMed] [Google Scholar]
- 7. Lee D-c, Artero EG, Sui X, Blair SN. Review: mortality trends in the general population: the importance of cardiorespiratory fitness. J Psychopharmacol. 2010;24(4, suppl):27-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality: a prospective study of healthy and unhealthy men. JAMA. 1995;273:1093-1098. [PubMed] [Google Scholar]
- 9. Blair SN, Kohl HW, Paffenbarger RS, Clark DG, Cooper KH, Gibbons LW. Physical fitness and all-cause mortality: a prospective study of healthy men and women. JAMA. 1989;262:2395-2401. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. Physical activity. http://www.cdc.gov/physicalactivity/everyone/guidelines/adults.html. Accessed April 16, 2015.
- 11. Korkiakangas EE, Alahuhta MA, Laitinen JH. Barriers to regular exercise among adults at high risk or diagnosed with type 2 diabetes: a systematic review. Health Promot Int. 2009;24:416-427. [DOI] [PubMed] [Google Scholar]
- 12. Reichert FF, Barros AJ, Domingues MR, Hallal PC. The role of perceived personal barriers to engagement in leisure-time physical activity. Am J Public Health. 2007;97:515-519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sherwood NE, Jeffery RW. The behavioral determinants of exercise: implications for physical activity interventions. Annu Rev Nutr. 2000;20:21-44. [DOI] [PubMed] [Google Scholar]
- 14. Klonizakis M, Moss J, Gilbert S, Broom D, Foster J, Tew GA. Low-volume high-intensity interval training rapidly improves cardiopulmonary function in postmenopausal women. Menopause. 2014;21(10):1099-1105. [DOI] [PubMed] [Google Scholar]
- 15. Keteyian SJ. High intensity interval training in patients with cardiovascular disease: a brief review of physiologic adaptations and suggestions for future research. J Clin Exerc Phys. 2013;2:13-19. [Google Scholar]
- 16. Lunt H, Draper N, Marshall HC, et al. High intensity interval training in a real world setting: a randomized controlled feasibility study in overweight inactive adults, measuring change in maximal oxygen uptake. PLoS One. 2014;9:e83256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Burgomaster KA, Howarth KR, Phillips SM, et al. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. J Physiol. 2008;586:151-160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gibala MJ. High-intensity interval training: a time-efficient strategy for health promotion? Curr Sports Med Rep. 2007;6:211-213. [PubMed] [Google Scholar]
- 19. Nybo L, Sundstrup E, Jakobsen MD, et al. High-intensity training versus traditional exercise interventions for promoting health. Med Sci Sports Exerc. 2010;42:1951-1958. [DOI] [PubMed] [Google Scholar]
- 20. Metcalfe RS, Babraj JA, Fawkner SG, Vollaard NB. Towards the minimal amount of exercise for improving metabolic health: beneficial effects of reduced-exertion high-intensity interval training. Eur J Appl Physiol. 2012;112:2767-2775. [DOI] [PubMed] [Google Scholar]
- 21. Gillen JB, Gibala MJ. Is high-intensity interval training a time-efficient exercise strategy to improve health and fitness? Appl Physiol. 2014;39:409-412. [DOI] [PubMed] [Google Scholar]
- 22. Burgomaster KA, Hughes SC, Heigenhauser GJ, Bradwell SN, Gibala MJ. Six sessions of sprint interval training increases muscle oxidative potential and cycle endurance capacity in humans. J Appl Physiol. 2005;98:1985-1990. [DOI] [PubMed] [Google Scholar]
- 23. Boutcher SH. High-intensity intermittent exercise and fat loss. J Obes. 2011;2011:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. LaForgia J, Withers RT, Gore CJ. Effects of exercise intensity and duration on the excess post-exercise oxygen consumption. J Sports Sci. 2006;24:1247-1264. [DOI] [PubMed] [Google Scholar]
- 25. Molmen-Hansen HE, Stolen T, Tjonna AE, et al. Aerobic interval training reduces blood pressure and improves myocardial function in hypertensive patients. Eur J Prev Cardiol. 2012;19:151-160. [DOI] [PubMed] [Google Scholar]
- 26. Wisloff U, Stoylen A, Loennechen JP, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115:3086-3094. [DOI] [PubMed] [Google Scholar]
- 27. Moholdt T, Aamot IL, Granoien I, et al. Aerobic interval training increases peak oxygen uptake more than usual care exercise training in myocardial infarction patients: a randomized controlled study. Clin Rehabil. 2012;26:33-44. [DOI] [PubMed] [Google Scholar]
- 28. Esfandiari S, Sasson Z, Goodman JM. Short-term high-intensity interval and continuous moderate-intensity training improve maximal aerobic power and diastolic filling during exercise. Eur J Appl Physiol. 2014;114:331-343. [DOI] [PubMed] [Google Scholar]
- 29. Munk PS, Staal EM, Butt N, Isaksen K, Larsen AI. High-intensity interval training may reduce in-stent restenosis following percutaneous coronary intervention with stent implantation: a randomized controlled trial evaluating the relationship to endothelial function and inflammation. Am Heart J. 2009;158:734-741. [DOI] [PubMed] [Google Scholar]
- 30. Schjerve I, Tyldum G, Tjonna A, et al. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clin Sci. 2008;115:283-293. [DOI] [PubMed] [Google Scholar]
- 31. Moholdt TT, Amudsen BH, Rustad LA, et al. Aerobic interval training versus continuous moderate exercise after coronary artery bypass surgery: A randomized study of cardiovascular effects and quality of life. Am Heart J. 2009; 158: 1031-1037. [DOI] [PubMed] [Google Scholar]
- 32. Tjonna AE, Stolen TO, Bye A, et al. Aerobic interval training reduces cardiovascular risk factors more than a multitreatment approach in overweight adolescents. Clin Sci. 2009;116:317-326. [DOI] [PubMed] [Google Scholar]
- 33. Alkahtani SA, King NA, Hills AP, Byrne NM. Effect of interval training intensity on fat oxidation, blood lactate and the rate of perceived exertion in obese men. Springerplus. 2013;2:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gibala MJ, McGee SL, Garnham AP, Howlett KF, Snow RJ, Hargreaves M. Brief intense interval exercise activates AMPK and p38 MAPK signaling and increases the expression of PGC-1α in human skeletal muscle. J Appl Physiol. 2009;106:929-934. [DOI] [PubMed] [Google Scholar]
- 35. Kiviniemi AM, Tulppo MP, Eskelinen JJ, et al. Cardiac autonomic function and high-intensity interval training in middle-age men. Med Sci Sports Exerc. 2014;46:1960-1967. [DOI] [PubMed] [Google Scholar]
- 36. Little JP, Safdar A, Bishop D, Tarnopolsky MA, Gibala MJ. An acute bout of high-intensity interval training increases the nuclear abundance of PGC-1α and activates mitochondrial biogenesis in human skeletal muscle. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1303-R1310. [DOI] [PubMed] [Google Scholar]
- 37. Bartlett JD, Close GL, MacLaren DP, Gregson W, Drust B, Morton JP. High-intensity interval running is perceived to be more enjoyable than moderate-intensity continuous exercise: implications for exercise adherence. J Sports Sci. 2011;29:547-553. [DOI] [PubMed] [Google Scholar]
- 38. Tjonna AE, Lee SJ, Rognmo O, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation. 2008;118:346-354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Keteyian SJ, Hibner BA, Bronsteen KM, et al. Greater Improvement in Cardiorespiratory Fitness Using Higher-Intensity Interval Training in the Standard Cardiac Rehabilitation Setting. J. Cardiopulmonary Rehab & Prev. 2014;34:98-105. [DOI] [PubMed] [Google Scholar]
- 40. Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol. 2012;590(pt 5):1077-1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Shiraev T, Barclay G. Evidence based exercise: clinical benefits of high intensity interval training. Aust Fam Physician. 2012;41:960-962. [PubMed] [Google Scholar]
- 42. Rognmo Ø, Moholdt T, Bakken H, et al. Cardiovascular risk of high-versus moderate-intensity aerobic exercise in coronary heart disease patients. Circulation. 2012;126:1436-1440. [DOI] [PubMed] [Google Scholar]
- 43. Cornish AK, Broadbent S, Cheema BS. Interval training for patients with coronary artery disease: a systematic review. Eur J Appl Physiol. 2011;111:579-589. [DOI] [PubMed] [Google Scholar]
- 44. Batterham SI, Heywood S, Keating JL. Systematic review and meta-analysis comparing land and aquatic exercise for people with hip or knee arthritis on function, mobility and other health outcomes. BMC Musculoskelet Disord. 2011;12:123-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Alves da, Silva MH, Maranhão Neto GdA. Development of the running test in shallow water for women engaged in water exercises: reliability and norms for evaluation of the distance covered. Rev Bras Med Esporte. 2006;12:206-210. [Google Scholar]
- 46. Cadmus L, Patrick MB, Maciejewski ML, Topolski T, Belza B, Patrick DL. Community-based aquatic exercise and quality of life in persons with osteoarthritis. Med Sci Sports Exerc. 2010;42:8-15. [DOI] [PubMed] [Google Scholar]
- 47. Colado JC, Triplett NT, Tella V, Saucedo P, Abellan J. Effects of aquatic resistance training on health and fitness in postmenopausal women. Eur J Appl Physiol. 2009;106:113-122. [DOI] [PubMed] [Google Scholar]
- 48. Cox KL, Burke V, Beilin LJ, Grove JR, Blanksby BA, Puddey IB. Blood pressure rise with swimming versus walking in older women: the Sedentary Women Exercise Adherence Trial 2 (SWEAT 2). J Hypertens. 2006;24:307-314. [DOI] [PubMed] [Google Scholar]
- 49. Ishikawa-Takata K, Ohta T, Tanaka H. How much exercise is required to reduce blood pressure in essential hypertensives: a dose–response study. Am J Hypertens. 2003;16:629-633. [DOI] [PubMed] [Google Scholar]
- 50. Jennings GL. Exercise and blood pressure: walk, run or swim? J Hypertens. 1997;15:567-569. [DOI] [PubMed] [Google Scholar]
- 51. Melton-Rogers S, Hunter G, Walter J, Harrison P. Cardiorespiratory responses of patients with rheumatoid arthritis during bicycle riding and running in water. Phys Ther. 1996;76:1058-1065. [DOI] [PubMed] [Google Scholar]
- 52. Nagle EF, Robertson RJ, Jakicic JJ, Otto AD, Ranalli JR, Chiapetta LB. Effects of aquatic exercise and walking in sedentary obese women undergoing a behavioral weight-loss intervention. Int J Aquat Res Educ. 2007;1:43-56. [Google Scholar]
- 53. Saavedra JM, De La, Cruz E, Escalante Y, Rodriguez FA. Influence of a medium-impact aquaerobic program on health-related quality of life and fitness level in healthy adult females. J Sports Med Phys Fitness. 2007;47:468-474. [PubMed] [Google Scholar]
- 54. Sideraviciute S, Gailiuniene A, Visagurskiene K, Vizbaraite D. The effect of long-term swimming program on body composition, aerobic capacity and blood lipids in 14-19-year aged healthy girls and girls with type 1 diabetes mellitus. Medicina. 2006;42:661-666. [PubMed] [Google Scholar]
- 55. Tanaka H. Swimming exercise: impact of aquatic exercise on cardiovascular health. Sports Med. 2009;39:377-387. [DOI] [PubMed] [Google Scholar]
- 56. Tanaka H, Bassett DR, Jr, Howley ET, Thompson DL, Ashraf M, Rawson FL. Swimming training lowers the resting blood pressure in individuals with hypertension. J Hypertens. 1997;15:651-657. [DOI] [PubMed] [Google Scholar]
- 57. Tanaka H, Bassett DR, Jr, Howley ET. Effects of swim training on body weight, carbohydrate metabolism, lipid and lipoprotein profile. Clin Physiol. 1997;17:347-359. [DOI] [PubMed] [Google Scholar]
- 58. Volaklis KA, Spassis AT, Tokmakidis SP. Land versus water exercise in patients with coronary artery disease: effects on body composition, blood lipids, and physical fitness. Am Heart J. 2007;154:560.e561-566. [DOI] [PubMed] [Google Scholar]
- 59. Greene NP, Martin SE, Crouse SF. Acute exercise and training alter blood lipid and lipoprotein profiles differently in overweight and obese men and women. Obesity. 2012;20:1618-1627. [DOI] [PubMed] [Google Scholar]
- 60. Perraton L, Machotka Z, Kumar S. Components of effective randomized controlled trials of hydrotherapy programs for fibromyalgia syndrome: a systematic review. J Pain Res. 2009;2:165-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Takeshima N, Rogers ME, Watanabe E, et al. Water-based exercise improves health-related aspects of fitness in older women. Med Sci Sports Exerc. 2002;34:544-551. [DOI] [PubMed] [Google Scholar]
- 62. D’Acquisto LJ, D’Acquisto DM, Renne D. Metabolic and cardiovascular responses in older women during shallow-water exercise. J Strength Cond Res. 2001;15:12-19. [DOI] [PubMed] [Google Scholar]
- 63. Nagle EF, Sanders ME, Shafer A, et al. Energy expenditure, cardiorespiratory, and perceptual responses to shallow-water aquatic exercise in young adult women. Phys Sportsmed. 2013;41:67-76. [DOI] [PubMed] [Google Scholar]
- 64. Di Prampero P. The energy cost of human locomotion on land and in water. Int J Sports Med. 1986;7:55-72. [DOI] [PubMed] [Google Scholar]
- 65. Miller MG, Cheatham CC, Porter AR, Ricard MD, Hennigar D, Berry DC. Chest-and waist-deep aquatic plyometric training and average force, power, and vertical-jump performance. Int J Aquat Res Educ. 2007;1:145-155. [Google Scholar]
- 66. Kanitz AC, Delevatti RS, Reichert T. Effects of two deep water training programs on cardiorespriatory and muscular strength responses in older adults. Exp Gerontology. 2015;64:55-61. [DOI] [PubMed] [Google Scholar]
- 67. Kruel LF, Peyre-Tartaruga LA, Coertjens M, Dias AB, Da Silva RC, Rangel AC. Using heart rate to prescribe physical exercise during head-out water immersion. J Strength Cond Res. 2014;28:281-289. [DOI] [PubMed] [Google Scholar]
- 68. Benelli P, Ditroilo M, De Vito G. Physiological responses to fitness activities: a comparison between land-based and water aerobics exercise. J Strength Cond Res. 2004;18:719-722. [DOI] [PubMed] [Google Scholar]
- 69. Graef FI, Pinto RS, Alberton CL, de Lima WC, Kruel LF. The effects of resistance training performed in water on muscle strength in the elderly. J Strength Cond Res. 2010;24:3150-3156. [DOI] [PubMed] [Google Scholar]
- 70. Kruel LFM, Posser MS, Alberton CL, Pinto SS, Oliveira AS. Comparison of energy expenditure between continuous and interval water aerobic routines. Int J Aquat Res Educ. 2009;3:186-196. [Google Scholar]
- 71. Cassady SL, Nielsen DH. Cardiorespiratory responses of healthy subjects to calisthenics performed on land versus in water. Phys Ther. 1992;72:532-538. [DOI] [PubMed] [Google Scholar]
- 72. Colado JC, Tella V, Triplett NT. A method for monitoring intensity during aquatic resistance exercises. J Strength Cond Res. 2008;22:2045-2049. [DOI] [PubMed] [Google Scholar]
- 73. Alberton CL, Olkoski MM, Becker ME, et al. Cardiorespiratory responses of postmenopausal women to different water exercises. Int J Aquat Res Educ. 2007. 2007;1:363-372. [Google Scholar]
- 74. Matsumoto I, Araki H, Tsuda K, et al. Effects of swimming training on aerobic capacity and exercise induced bronchoconstriction in children with bronchial asthma. Thorax. 1999;54:196-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Pinto SS, Cadore EL, Alberton CL, et al. Cardiorespiratory and neuromuscular responses during water aerobics exercise performed with and without equipment. Int J Sports Med. 2011;32:916-923. [DOI] [PubMed] [Google Scholar]
- 76. Sanders M, Takeshima N, Rogers M, Colado J, Borreani S. Impact of the S.W.E.A.T. water exercise method on activities of daily living for older women. J Sports Sci Med. 2013;12:707-715. [PMC free article] [PubMed] [Google Scholar]
- 77. Masumoto K, Takasugi S, Hotta N, et al. Electromyographic analysis of walking in water in healthy humans. J Physiol Anthropol Appl Hum Sci. 2004;23:119-127. [DOI] [PubMed] [Google Scholar]
- 78. Becker B. Aquatic therapy: scientific foundations and clinical rehabilitation applications. Am Acad Phys Med Rehabil. 2009;1:859-872. [DOI] [PubMed] [Google Scholar]
- 79. Gulick D.T., Geigle P.R. Physiological responses to immersion and aquatic exercise. Aquat Exerc Rehabil Training. 1st ed. Champaign, IL: Human Kinetics; 2009: 35-42. [Google Scholar]
- 80. Brancazio PJ, Holmes B. SportScience. Am J Phys. 1985;53:506-507. [Google Scholar]
- 81. Colado JC, Tella V, Triplett NT, Gonzalez LM. Effects of a short-term aquatic resistance program on strength and body composition in fit young men. J Strength Cond Res. 2009;23:549-559. [DOI] [PubMed] [Google Scholar]
- 82. Sanders ME. YMCA Water Fitness Program for Health. Champaign, IL: Human Kinetics; 2000. [Google Scholar]
- 83. Sanders ME. Selected Physiological Responses to a Water Exercise Program Called Wave Aerobics. Reno, NV: University of Nevada; 1993. [Google Scholar]
- 84. Cassady SL, Nielsen DH. Cardiorespiratory responses of healthy subjects to calisthenics performed on land versus in water. Phys Ther. 1992;72:532-538; discussion 539. [DOI] [PubMed] [Google Scholar]
- 85. Phillips VK, Legge M, Jones LM. Maximal physiological responses between aquatic and land exercise in overweight women. Med Sci Sports Exerc. 2008;40:959-964. [DOI] [PubMed] [Google Scholar]
- 86. Pendergast DR, Lundgren CE. The underwater environment: cardiopulmonary, thermal, and energetic demands. J Appl Physiol. 2009;106:276-283. [DOI] [PubMed] [Google Scholar]
- 87. Chu KS, Rhodes EC, Taunton JE, Martin AD. Maximal physiological responses to deep-water and treadmill running in young and older women. J Aging Phys Act. 2002;10:306-313. [Google Scholar]
- 88. Connelly TP, Sheldahl LM, Tristani FE, et al. Effect of increased central blood volume with water immersion on plasma catecholamines during exercise. J Appl Physiol. 1990;69:651-656. [DOI] [PubMed] [Google Scholar]
- 89. Silvers WM, Rutledge ER, Dolny DG. Peak cardiorespiratory responses during aquatic and land treadmill exercise. Med Sci Sports Exerc. 2007;39:969-975. [DOI] [PubMed] [Google Scholar]
- 90. Kruel LF, Tartaruga LA, Coertjens M, et al. Using heart rate to prescribe physical exercise during head-out water immersion. J Strength Cond Res. 2014;28:281-289. [DOI] [PubMed] [Google Scholar]
- 91. Moening D, Scheidt A, Shepardson L, Davies GJ. Biomechanical comparison of water running and treadmill running. Isokinet Exerc Sci. 1993;3:207-215. [Google Scholar]
- 92. Barbosa TM, Garrido MF, Bragada J. Physiological adaptations to head-out aquatic exercises with different levels of body immersion. J Strength Cond Res. 2007;21:1255-1259. [DOI] [PubMed] [Google Scholar]
- 93. Gappmaier E, Lake W, Nelson AG, Fisher AG. Aerobic exercise in water versus walking on land: effects on indices of fat reduction and weight loss of obese women. J Sports Med Phys Fitness. 2006;46:564-569. [PubMed] [Google Scholar]
- 94. Altan L, Bingol U, Aykac M, Koc Z, Yurtkuran M. Investigation of the effects of pool-based exercise on fibromyalgia syndrome. Rheumatol Int. 2004;24:272-277. [DOI] [PubMed] [Google Scholar]
- 95. Assis MR, Silva LE, Alves AM, et al. A randomized controlled trial of deep water running: clinical effectiveness of aquatic exercise to treat fibromyalgia. Arthritis Rheum. 2006;55:57-65. [DOI] [PubMed] [Google Scholar]
- 96. Berger BG, Owen DR. Mood alteration with swimming: swimmers really do “feel better.” Psychosom Med. 1983;45:425-433. [DOI] [PubMed] [Google Scholar]
- 97. Hall J, Grant J, Blake D, Taylor G, Garbutt G. Cardiorespiratory responses to aquatic treadmill walking in patients with rheumatoid arthritis. Physiother Res Int. 2004;9:59-73. [DOI] [PubMed] [Google Scholar]
- 98. Cuesta-Vargas AI, García-Romero JC, Arroyo-Morales M, Diego-Acosta ÁM, Daly DJ. Exercise, manual therapy, and education with or without high-intensity deep-water running for nonspecific chronic low back pain: a pragmatic randomized controlled trial. Am J Phys Med Rehabil. 2011;90:526-538. [DOI] [PubMed] [Google Scholar]
- 99. Bressel E, Wing JE, Miller AI, Dolny DG. High-intensity interval training on an aquatic treadmill in adults with osteoarthritis: effect on pain, balance, function, and mobility. J Strength Cond Res. 2014;28:2088-2096. [DOI] [PubMed] [Google Scholar]
- 100. Martin W, Montgomery J, Snell PG, et al. Cardiovascular adaptations to intense swim training in sedentary middle-aged men and women. Circulation. 1987;75:323-330. [DOI] [PubMed] [Google Scholar]
- 101. Mohr M, Nordsborg NB, Lindenskov A, et al. High-intensity intermittent swimming improves cardiovascular health status for women with mild hypertension. BioMed Res Int. 2014;2014:1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Broman G, Quintana M, Engardt M, Gullstrand L, Jansson E, Kaijser L. Older women’s cardiovascular responses to deep-water running. J Aging Phys Act. 2006;14:29-40. [DOI] [PubMed] [Google Scholar]
- 103. Wilber RL, Moffatt RJ, Scott BE, Lee DT, Cucuzzo NA. Influence of water run training on the maintenance of aerobic performance. Med Sci Sports Exerc. 1996;28:1056-1062. [DOI] [PubMed] [Google Scholar]
- 104. Rebold MJ, Kobak MS, Otterstetter R. The influence of a tabata interval training program using an aquatic underwater treadmill on various performance variables. J Strength Cond Res. 2013;27:3419-3425. [DOI] [PubMed] [Google Scholar]
- 105. Broman G, Quintana M, Lindberg T, Jansson E, Kaijser L. High intensity deep water training can improve aerobic power in elderly women. Eur J Appl Physiol. 2006;98:117-123. [DOI] [PubMed] [Google Scholar]
- 106. Sanders ME. Higher intensity interval training. J Active Aging. 2013;12:66-73. [Google Scholar]
- 107. Wilder RP, Brennan D, Schotte DE. A standard measure for exercise prescription for aqua running. Am J Sports Med. 1993;21:45-48. [DOI] [PubMed] [Google Scholar]
- 108. Wallman K, Plant LA, Rakimov B, Maiorana AJ. The effects of two modes of exercise on aerobic fitness and fat mass in an overweight population. Res Sports Med. 2009;17:156-170. [DOI] [PubMed] [Google Scholar]
- 109. Buchheit M, Laursen PB. High-intensity interval training, solutions to the programming puzzle. Sports Med. 2013;43:313-338. [DOI] [PubMed] [Google Scholar]
- 110. Schmid JP, Noveanu M, Morger C, et al. Influence of water immersion, water gymnastics and swimming on cardiac output in patients with heart failure. Heart. 2007;93:722-727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Schega L, Claus G, Almeling M, Niklas A, Daly DJ. Cardiovascular responses during thermoneutral, head-out water immersion in patients with coronary artery disease. J Cardiopulm Rehabil Prev. 2007;27:76-80. [DOI] [PubMed] [Google Scholar]
- 112. Sanders ME, Escobar L. The story of Laura Sos, Castellon, Spain. ACSM Health Fitness J. 2010;16:35-41. [Google Scholar]
- 113. Escobar Torres L, Sanders ME, Lawson D, Belenguer Benitez CA. A case study: mobility & health impact of an aquatic fitness program for a woman with intellectual and physical disabilities. Int J Aquat Res Educ. 2013;7:147-153. [Google Scholar]


