Abstract
Orthodontic records are one of the main milestones in orthodontic therapy. Records are essential not only for diagnosis and treatment planning but also for follow-up of the case, communicating with colleagues, and evaluating the treatment outcomes. Recently, two-dimensional (2D) imaging technology, such as cephalometric and panoramic radiographs and photographs, and plaster models were routinely used. However, after the introduction of three-dimensional (3D) technologies (laser scanner, stereophotogrammetry, and computed tomography) into dentistry, 3D imaging systems are more and more commonly preferred than 2D, especially in cases with craniofacial deformities. In fact, 3D imaging provided more detailed and realistic diagnostic information about the craniofacial hard as well as soft tissue and allowed to perform easier, faster, and more reliable 3D analyses. The purpose of this review is to provide an overview of the 3D imaging techniques, including their advantages and disadvantages, and to outline the indications for 3D imaging.
Keywords: Three-dimensional, imaging, orthodontics, laser scanner, stereophotogrammetry, computed tomography
INTRODUCTION
Orthodontic records are one of the main milestones in orthodontic therapy. Records are essential not only for diagnosis and treatment planning but also for follow-up of the case, communicating with colleagues, and evaluating the treatment outcomes. Recently, two-dimensional (2D) imaging technology, such as cephalometric and panoramic radiographs and photographs, and plaster models were used routinely. However, there are some limitations of 2D imaging systems as significant amount of radiographic projection error, enlargement, distortion, exposure to radiation, weaknesses of landmark identification, inaccurate duplication of measurements, significant variation in the position of reference points, such as sella turcica, and extreme limitations in assessing soft tissue balance (1). When the clinician uses 2D imaging to view three-dimensional (3D) anatomical craniofacial structures, some cephalometric structures and landmarks that do not exist in the patient appear such as mandibular symphysis, articulare, pterygoid fossa, and “key ridges.” Averaging bilateral structures (such as the right and left inferior borders of the mandible) to create a unified anatomic outline (mandibular plane) results in loss of parasagittal information and, if present, asymmetry of the patient. In summary, 2D imaging systems are not able to overcome the fact that reduction of a 3D object to a 2D view will cause data loss (2).
After the introduction of 3D imaging systems, it was possible to evaluate structures in real three anatomical dimensions. In addition, not only the hard but also the soft tissues of the craniofacial region can be observed in three dimensions. These new systems have several other advantages. First, most of these systems are non-invasive, and, therefore, repeat of images are not of ethical matter. Second, all images may also be stored in digital forms, consequently archiving is much more practical, and extra space need for storage is handled in this way. The development of software programs enables to precisely and reliably analyze the 3D data. Furthermore, thanks to opportunities such as zooming and rotation function, software programs are really user-friendly (3, 4).
3D imaging systems are especially favorable for patients with craniofacial syndromes and anomalies such as cleft lip and palate (CLP) (Table 1). This patient group is frequently treated for a long period starting in infancy and not finishing until adulthood, undergoes several surgeries, and requires treatment from specialists of several disciplines or, in other words, interdisciplinary approaches.
Table 1.
Comparison of cost, radiation dose, and indications of 3D imaging systems
| Imaging techniques | Cost | Radiation dose | Indications |
|---|---|---|---|
| CBCT | High | Dentoalveolar 11-674 μSv Maxillofacial 30-1073 μSv |
Craniofacial deformities (other indications with caution) |
| Laser scanner | High | Non-invasive | May be recommended in every patient |
| Stereophotogrammetry | High | Non-invasive | May be recommended in every patient |
| MRI | High | Non-invasive | Airway assessment |
| Intraoral scanner | High | Non-invasive | May be recommended in every patient |
The treatment plans have to involve the dentition, the hard tissue jaw position, as well as the facial bone position, and the covering soft tissue. Although the Eurocleft and Americacleft studies proposed documentation at certain time periods, the guidelines are based on 2D records except the 3D dental casts. However, more and more studies have been published about the introduction, the advantages over 2D, and the indications of 3D imaging systems of craniofacial patient treatment teams. However, compared with 2D systems, the cost and also radiation dose of some of these 3D imaging systems are high and should be considered by the specialists before indicating (Table 2). Therefore, the aim of the present review is to summarize the 3D imaging system in daily orthodontic practice and to emphasize the indication areas especially in patients with craniofacial anomalies.
Table 2.
Comparison of 2D and 3D imaging systems
| Imaging techniques | Effective dose (μSv) | Cost |
|---|---|---|
| Periapical radiograph | <1.5* | X |
| Panoramic radiograph | 2.7–24.3 | 2X |
| Cephalometric radiograph | <6 | 2X |
| CBCT | ||
| Dentoalveolar CBCT | 11–674 (61) | |
| Maxillofacial CBCT | 30–1073 | 10-20X |
| MSCT maxillo-mandibular | 280 – 1410 | 10-20X |
To be able to understand 3D imaging systems, some of the terminology should be familiarized. There are two axes (the vertical and the horizontal axes) in 2D images. In 3D images, the Cartesian coordinate system is used, and it consists of the x-axis (or the transverse dimension), y-axis (or the vertical dimension), and the z-axis (the anteroposterior dimension “depth axis”). There are several steps in generating 3D models. The first one is “modeling”. Mathematics is used in this step in order to describe the physical properties of an object. After this step, the modeled object is called as a “wireframe” (or a “polygonal mesh”).
In the modeling procedure, surface is added to the object by placing a layer of pixels. This is called “image” or “texture mapping”. In the second step, to bring more realism to the 3D object, some shading and lighting is applied. “Rendering” is the final step. The anatomical data collected from the patient are converted into a lifelike 3D object by the computer, and it can be viewed on the computer screen (5).
3D imaging methods can be summarized as follows:
conventional computed and cone-beam computerized tomography (CT/CBCT)
laser scanning (3D laser scanning)
vision-based scanning techniques
3D orthognathic surgery planning
intraoral scanning
magnetic resonance imaging (MRI) and surface scanning
video camera (four-dimensional (4D) imaging and video stereophotogrammetry).
CT
CT, also named computerized axial tomography, consists of a 3D view using cross-sectional images of the body. This scan contains 3D information about especially hard but also soft tissues. Tomography is divided into fan beam and CBCT. Traditional tomography is fan beam tomography and has a high radiation dose. Additionally, it is expensive and not available in every health care hospital. Hence, the high radiation dose, it is not suitable for routine orthodontic applications. However, owing to the informative data about orofacial pathologies, maxillary sinus, temporomandibular joint (TMJ), orofacial trauma and fractures, airway volumes, anatomical variations, and craniofacial syndromes, it is used widely in dentistry (Figure 1).
Figure 1.
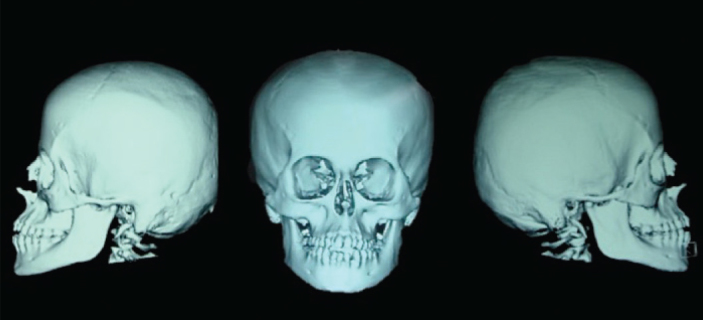
3D fan beam computerized tomography (CT) image
Craniofacial CBCT was introduced approximately 20 years ago and was designed to overcome some of the limitations of conventional CT scanning (6). The cost of CBCT imaging is very low compared with CT, and more importantly, the 3D visualization with much more less radiation dose is possible. However, the lower radiation dose is still much higher than conventional 2D imaging systems (Table 2).
CBCT allows realignment of 2D images in coronal, sagittal, oblique, and various inclined planes. With CBCT devices, all raw data are obtained in a single turn. In this way, the patient’s length of hospital stay is reduced, and the device increases patient satisfaction. The most important advantage of CBCT is its possibility to display and arrange 3D data in personal computers. Various comprehensive softwares for orthodontic measurements are available.
CBCT can be used for several approaches in orthodontic patients. According to Kapila and Nervina (7), CBCT should be preferred:
- if it enhances diagnosis such as identification of the location of impacted (8, 9, 10) and supernumerary teeth (10–12) (Figure 2)
- if it quantifies the magnitude of the defect such as in patients with CLP (13, 14) (Figure 3, 4)
- if it improves differential diagnosis of malocclusions such as craniofacial anomalies and syndromes (15)
- if determination whether the discrepancy is uni- or bilateral is required such as facial asymmetry especially for patients with orthognathic surgery (16) (Figure 5)
- if it helps to identify the etiology of the malocclusion such as TMJ disorders (17)
- if it helps to assess treatment outcomes such as rapid maxillary expansion (18–20) and root angulations (21)
- if determination of the quality and quantity of bone and the anatomical structures is required for orthodontic device placement such as miniscrews
- if determination of alveolar boundary conditions is needed (22)
- if 3D airway morphology is needed especially for the therapy of obstructive sleep apnea (23).
Figure 2.
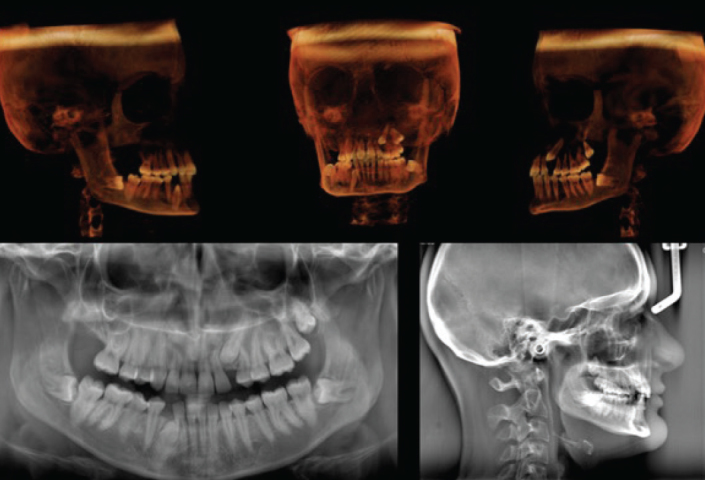
3D cone beam computerized tomography (CBCT) image and 2D panoramic and lateral cephalometric radiography of a patient with impacted teeth
Figure 3.

2D intraoral photographs of a patient with right unilateral CLP
Figure 4.
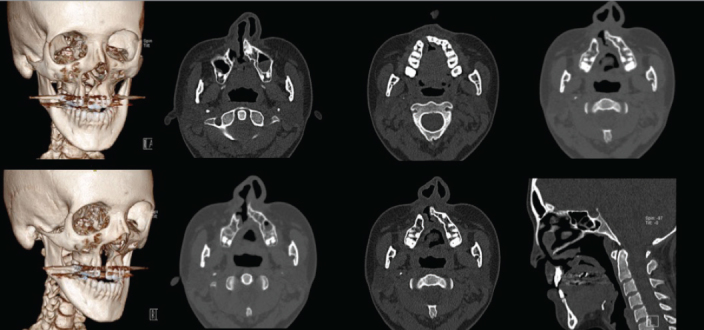
3D and 2D axial images to identify the defect in a patient with unilateral CLP
Figure 5.
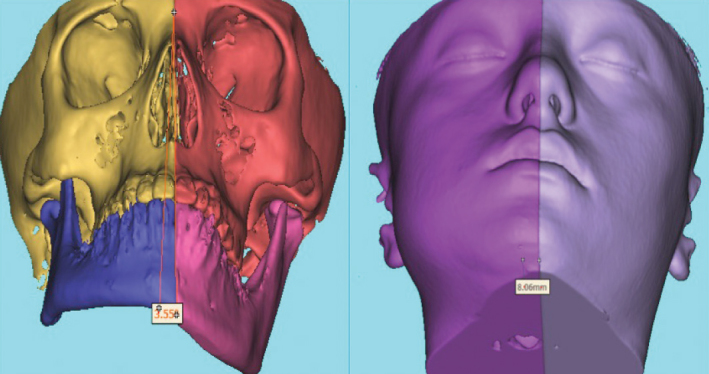
3D CBCT images to evaluate hard and soft tissue facial asymmetries
CBCT has been usually used for diagnosis and treatment planning of impacted teeth (8–10). According to Lai et al. (10), CBCT improves exact localization of the impacted canines, assessment of the proximity to other structures and teeth, determining the existence of any pathology, and root resorption associated with impacted teeth and adjacent teeth. Furthermore, CBCT aids treatment planning of the impacted teeth, helps to determine surgical access and extrusion of the impacted teeth into the oral cavity. In addition, it is shown that CBCT scans contribute to more accurate image over 2D radiographs for root resorption associated with impacted teeth. In supernumerary teeth cases, the position of supernumerary teeth especially if it is impacted and describing the morphology of the supernumerary teeth is the most important points in treatment of these cases. CBCT provides the required 3D information involving the shape and position of the supernumerary tooth, any irregularities around the tooth, and root resorption of adjacent permanent teeth (10–12).
Even though the correlation between orthodontic treatment and TMJ has not been supported by most of the studies, examination of TMJ before beginning the orthodontic treatment is always advised. Studies showed that CBCT provides more specific anatomic imaging than 2D radiographs, and it is more effective than CT and MRI in detecting osseous changes (17). Using CBCT images when placing temporary anchorage devices (TADs) can be helpful for judgment of the surrounding tissues and anatomical structures such as tooth roots, sinuses, and nerves, preventing any complications (7). CBCT is not only used for treatment planning or diagnosis but also used for evaluating treatment outcomes. CBCT has been used in several studies for assessment of dental and skeletal effects of maxillary expansion (18, 19) and comparison of the periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion devices (20), determining how expansion forces affect different regions of the maxilla (18).
After orthodontic treatment, root parallelism and angulations can be determined by using CBCT to aid post-treatment stability (22). CBCT imaging has been used to investigate the efficacy of rapid maxillary expansion (RME) and surgery as treatment options for a constricted airway (7). In summary, CBCT examination is recommended for evaluating airway volume (23). CBCT was also preferred in airway evaluation studies to evaluate the nose and sinuses as well as volumes of airway spaces at different levels; however, none of these studies had high-quality scores, and therefore, a real indication could not be stated according to Kujipers et al. (24).
In patients with craniofacial syndromes, impacted or supernumerary teeth are considerably prevalent; CBCT images have been found supportive in planning orthodontic treatment of the patient with syndrome who has impacted and supernumerary teeth (15).
3D imaging is especially usable for pre-treatment evaluation of the patients with craniofacial deformities such as patients with CLP, orthognathic surgery, syndromes, and facial asymmetries. De Moraes et al. (25) emphasized that CBCT provides better evaluation of craniofacial morphology than 2D images. Nur et al. (16) outlined that CBCT is a favorable diagnosis method in facial asymmetry to compare the right and left facial hard and also limits soft tissue measurements. Recent studies showed that CBCT provides valuable information in patients with CLP for determining the volume of the alveolar defect, location, proximity, eruption status, and paths of the teeth near the cleft site (13, 14). Therefore, CBCT improves the ability to understand the precise volume of the post-expansion defect and enables optimally planning and evaluating of outcomes of bone grafting. Overall, the SEDENTEXCT Consortium stated that CLP is one of the main reasonable indications for taking CBCT from the patients in dentistry and recommended to consider the other indications with caution (26).
Laser Scanning (3D Laser Scanning)
Laser scanning is a non-invasive technique for capturing facial morphology and soft tissue (Table 1). Validity of the method was proven in many studies (27, 28). According to Kau and Richmond (29), besides producing accurate 3D facial models, laser scanning devices are less expensive and easily handled.
Laser scanning can be used for the following reasons (Figure 6):
Figure 6.
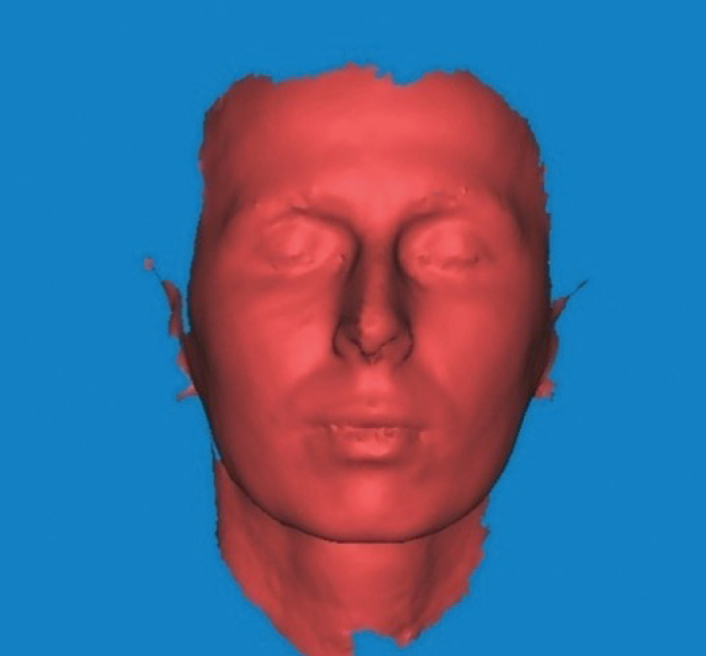
3D laser scanning image
– cross-sectional growth changes (32)
– assessment of treatment outcomes (33)
– evaluating clinical outcomes for surgical cases (34)
– evaluating patients with CLP (31)
– soft tissue changes (35)
– scanning dental casts (36).
Laser scanning has been used for quantitatively evaluating facial symmetry in adolescents (30) and patients with cleft lip palate as well as the soft tissue changes after treatment (31). Moreover, Kujipers et al. (24) reported that laser scanner and stereophotogrammetry are reliable soft tissue imaging systems with a maximum measurement error of <1 mm.
The capturing time in this technique is the most prominent disadvantage. Therefore, it is inconvenient for pediatric cases (37). On the other hand, a study concluded that laser scanning might be a suitable method for pre-school children as long as they are well prepared (31). Apart from these, some other shortcomings of the method have been reported such as inability to capture soft tissue surface texture and safety issues due to exposing the eyes to the laser beam (5).
Vision-Based Scanning Techniques
Vision-based scanning techniques such as Moiré topography, structured light, stereophotogrammetry, and 3D facial morphometry are non-invasive and quite user-friendly techniques. Stereophotogrammetry has been shown to be the most frequently used in the orthodontic practice among vision-based scanning techniques.
Stereophotogrammetry
Stereophotogrammetry is based on photographing objects by a pair of configured cameras and combining photos taken from two different directions to create 3D models. Studies showed that stereophotogrammetry has many advantages:
– It is non-invasive and non-contact technique with no radiation exposure.
– It is good at capturing facial morphology and soft tissue changes (38–40).
– It has a short acquisition time and user-friendly (in pediatric patients especially infants).
– It can be combined with CBCT images.
– 3D images can be viewed on a personal computer and can be used as communication tool between clinicians.
– 3D images can be rotated and viewed from any direction, thus stereophotogrammetry is very useful for orthognathic surgery and (5, 41) patients with craniofacial anomalies (CLP) (24, 42, 43) (Figure 7, 8).
Figure 7.
Different views of 2D photographs and 3D stereophotogrammetric images of an infant with bilateral CLP by multiple and one capture, respectively
Figure 8.
Different views of 2D photographs and 3D stereophotogrammetric images of a patient with right unilateral CLP by multiple and one capture, respectively
In a thesis, stereophotogrammetry has also been used for scanning dental casts to evaluate the intraoral changes after nasoalveolar therapy (44). It was concluded that 3D data enabled rotating and zooming into the image, so that models can be viewed from any direction desired and hence performing more accurate measurement on the model (42). It is quite efficient in capturing facial morphology (38–40); however, tissue reflections, hair, eyebrow, and curved surfaces such as the eyes and ears can influence the image process (45). Stereophotogrammetry allows orthodontists to evaluate the face from every direction with only one capture, and this makes stereophotogrammetry useful for patients with orthognathic surgery and craniofacial deformities (5, 41). Stereophotogrammetry has also been preferred for making superimpositions after orthognathic surgery (5).
Stereophotogrammetry is the most frequently used 3D techniques in patients with CLP for soft tissue evaluation. As it is a non-invasive technique and patients are not exposed to radiation, it can be safely used in pediatric patients. Another reason for preferring stereophotogrammetry on little children is short capturing time and simple utilization of the device. Hence, it is favorable in the infancy period as the infants receive pre-surgical orthopedic treatment to document the follow-ups as well as the outcomes of the treatment. The digital archiving of the soft tissue data at the first surgery enables the follow-up of soft tissue growth differentiations due to the surgical approaches. By this way, the techniques and approaches may be enhanced and developed to overcome determined surgical side effects. Recently, to distinguish the physiological- from approached-based growth, several studies were performed on babies using stereophotogrammetry to establish superimpositions (42–44).
MRI and Surface Scanning
MRI and surface scanning are non-invasive imaging techniques. MRI provides accurate and detailed information on abnormalities and disorders of craniofacial hard and soft tissues, especially the TMJ (46), and it has been used in craniofacial imaging for several years. MRI is mostly used for upper airway analysis and 3D imaging of TMJ morphology. Kujipers et al. (24) reported that studies about velopharyngeal function using MRI were scored high quality and, therefore, may be indicated for measuring airway space, motion, and function especially in patients with cleft to determine velopharyngeal incompetence. MRI has been thought to have some limitations due to limited usage area in dentistry, cost of the device, and orthodontists’ lack of experience in application (47). However, recent studies showed that MRI is useful in many orthodontic fields and compared MRI with conventional 3D imaging techniques (CBCT and CT) (Table 1). Detterbeck et al. (48) compared mesio-distal tooth width by using 3D imaging techniques with and without ionizing radiation and concluded that MRI offers equivalent measurements compared with CBCT, and tooth germs are better illustrated than erupted teeth on MRI. Whether MRI is comparable with cephalometric radiographs in cephalometric analysis was evaluated and confirmed that orthodontic treatment planning without radiation exposure is possible by using MRI technique (49). In conclusion, MRI has huge potential for usage in clinical practice in orthodontics with its benefits such as good contrast ratio and absence of ionizing radiation.
Video Camera (4D Imaging and Video Stereophotogrammetry)
The aforementioned methods are used to evaluate the facial morphology either two- or three-dimensionally. However, the human face is a dynamic structure especially the nose, lip, and mouth areas. The newest method is 4D video capturing, which can record dynamic movements of the human face and enable to analyze the dynamics of facial expressions (50). Several studies used 4D imaging in patients with CLP and orthognathic surgery to demonstrate asymmetry while making facial expressions, and differences in facial motion between individuals with and without CLP were evaluated (50). With these new technologies, new attempts have been performed to create virtual patients by superimposing facial skeleton, soft tissue, and/or dentition (51). Future planned studies to create a real-time 4D virtual patient in motion are needed in the literature.
3D Planning in Orthognathic Surgery
Facial soft tissues, facial skeleton, and dentition are the main elements of orthognathic surgery planning. Capturing these three important tissue groups can only be achieved by “image fusion” (52). 3D facial image capture and CBCT images can be combined to create a “virtual 3D patient” so the orthodontists and surgeons can evaluate the patient’s craniofacial skeleton and the soft tissue together. These 3D models are interactive and can be rotated to any view for more complete diagnosis and treatment planning. All collected data can be stored in the computer files which can be easily managed online. It also helps orthodontists and surgeons to communicate and make interdisciplinary treatment plans.
Accurate treatment planning is vital for orthognathic surgery to achieve optimum aesthetic and occlusal results. 3D surgical planning can be performed on this virtual patient through the software programs. In addition, surgical splints can be manufactured by using Computer Aided Design/Computer Aided Manufacturing (CAD/CAM) technology (53). With these surgical guides, the virtual planning can be transferred to the operating room (52). It is possible to make predictions of the postoperative outcomes in soft and hard tissues by 3D surgery simulations. According to Centenero et al. (53), postoperative predictions are reliable in some areas, but further development is needed in representing the postoperative changes in facial soft tissue. This technology is available to:
- repositioning of osteotomized bony structures
- control intercuspation
- control interferences between osteotomized bony structures and regions at the base of the skull (53)
- perform virtual distraction osteogenesis (54)
- make multiple simulations of different osteotomies and skeletal movements (5)
- data management
- communication between orthodontists and surgeons
- manufacturing surgical splints.
However, 3D image fusion process is an expensive method, which requires equipment and time (approximately 1 hour to generate virtual patient) (52).
Intraoral Scanning
Intraoral scanner is an equipment that consists of an intraoral camera, computer, and software. It creates a digital 3D model of scanned objects that can be teeth, impression, or dental cast. With the introduction of intraoral scanning technique, disadvantages of conventional impression techniques such as dimensional changes of impression materials, storage problem, and dental stone errors are overcome. In addition, it is easier to take impressions from the patients with gag reflexes by using intraoral camera. The development of digital models allows to obtain 3D diagnostic information, communicate between laboratory and orthodontists, create virtual set-ups and treatment planning, and fabricate custom-made fixed or removable appliances. Orthodontists are able to plan the treatment on the digital model, control the bracket positioning, and superimpose the before and after models.
Intraoral scanning can provide:
- archiving study casts
- examine intra- and inter-arch relationships
- treatment planning
- virtual treatment and virtual set-ups
- 3D prefabrication of arch wires
- construction of 3D aligners
- CAD/CAM retainer
- fabricated lingual brackets
- indirect bracket bonding.
However, according to a systematic review, inter-arch measurements such as overjet, overbite, molar relationship, and canine relationship need to be verified on virtually occluded digital models (55). Moreover, the time requirement for full arch scanning in routine practice can be counted as disadvantage of this technique.
CONCLUSION
3D imaging techniques are very supportive for routine orthodontic practice. These techniques enhance treatment options enabling more detailed diagnostic information on the specific cases such as patients with craniofacial anomalies. CBCT has quite wide usage area especially to evaluate craniofacial skeleton and related pathologies; however, owing to the high radiation dose, it is recommended to consider the indications with caution. As aforementioned, CBCT use in patients with cleft is one of the main supportable indications. Although the non-invasive systems such as stereophotogrammetry, laser scanner, intraoral scanner, and MRI are suitable for every patient, the high cost has to be considered. Stereophotogrammetry is suggested for patients with craniofacial deformities (involving patients with CLP), and it is highly recommended especially in pediatric patients (infancy period) who are very hard to capture due to movements with conventional photographs. Some weaknesses of laser scanning, such as poorness of capturing soft tissue surface texture, make this technique more suitable for scanning dental casts. Digital dental casts are user-friendly tools to evaluate the dentition. MRI presented high reliability and may be indicated to determine velopharyngeal functions and airway space. Overall, as all 3D imaging techniques are developed and became a routine, chair time for full orthodontic records, record loss, and storage problem will be reduced, and the interdisciplinary communication enhanced. Whereas still evidence-based guidelines for 3D imaging were required to cooperate it into standard orthodontic record collecting phase, the future of 3D imaging offers clinicians dynamic 4D virtual patient in motion to recognize functional recovery after treatment.
Footnotes
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - O.E., B.N.Y.; Design - O.E., B.N.Y.; Supervision - B.N.Y.; Resources - O.E., B.N.Y.; Materials - O.E., B.N.Y; Data Collection and/or Processing - O.E., B.N.Y.; Analysis and/or Interpretation - O.E., B.N.Y.; Literature Search - O.E., B.N.Y.; Writing Manuscript - O.E., B.N.Y.; Critical Review - B.N.Y.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Jacobson A. Radiographic Cephalometry: From basics to videoimaging. Chicago: Quintessence; 1995. [Google Scholar]
- 2.Palomo JM, Yang C, Hans MG. Clinical Application of Three-Dimensional Craniofacial Imaging in Orthodontics. J Med Sci. 2005:269–78. [Google Scholar]
- 3.Lane C, Harrell W., Jr Completing the 3-dimensional picture. Am J Orthod Dentofacial Orthop. 2008;133:612–20. doi: 10.1016/j.ajodo.2007.03.023. [DOI] [PubMed] [Google Scholar]
- 4.Germec-Cakan D, Canter HI, Nur B, Arun T. Comparison of Facial Soft Tissue Measurements on 3D Images and Models Obtained with Different Methods. J Craniofac Surg. 2010;21:1393–9. doi: 10.1097/SCS.0b013e3181ec6976. [DOI] [PubMed] [Google Scholar]
- 5.Hajeer MJ, Millett DT, Ayoub AF, Siebert JP. Applications of 3D imaging in orthodontics: Part I. J Orthod. 2004;31:62–70. doi: 10.1179/146531204225011346. [DOI] [PubMed] [Google Scholar]
- 6.Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the conebeam technique: preliminary results. Eur Radiol. 1998;8:1558–64. doi: 10.1007/s003300050586. [DOI] [PubMed] [Google Scholar]
- 7.Kapila SD, Nervina JM. CBCT in orthodontics: assessment of treatment outcomes and indications for its use. Dentomaxillofac Radiol. 2015;44:20140282. doi: 10.1259/dmfr.20140282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Botticelli S, Verna C, Cattaneo PM, Heidmann J, Melsen B. Two- versus three-dimensional imaging in subjects with unerupted maxillary canines. Eur J Orthod. 2011;33:344–9. doi: 10.1093/ejo/cjq102. [DOI] [PubMed] [Google Scholar]
- 9.Katheria BC, Kau CH, Tate R, Chen JW, English J, Bouquot J. Effectiveness of impacted and supernumerary tooth diagnosis from traditional radiography versus cone beam computed tomography. Pediatr Dent. 2010;32:304–9. [PubMed] [Google Scholar]
- 10.Lai CS, Bornstein MM, Mock L, Heuberger BM, Dietrich T, Katsaros C. Impacted maxillary canines and root resorptions of neighbouring teeth: a radiographic analysis using cone-beam computed tomography. Eur J Orthod. 2013;35:529–38. doi: 10.1093/ejo/cjs037. [DOI] [PubMed] [Google Scholar]
- 11.Toureno L, Park JH, Cederberg RA, Hwang EH, Shin JW. Identification of supernumerary teeth in 2D and 3D: review of literature and a proposal. J Dent Educ. 2013;77:43–50. [PubMed] [Google Scholar]
- 12.Mossaz J, Kloukos D, Pandis N, Suter VG, Katsaros C, Bornstein MM. Morphologic characteristics, location, and associated complications of maxillary and mandibular supernumerary teeth as evaluated using cone beam computed tomography. Eur J Orthod. 2014;36:708–18. doi: 10.1093/ejo/cjt101. [DOI] [PubMed] [Google Scholar]
- 13.Garib DG, Yatabe MS, Ozawa TO, Filho OG. Alveolar bone morphology in patients with bilateral complete cleft lip and palate in the mixed dentition: cone beam computed tomography evaluation. Cleft Palate Craniofac J. 2012;49:208–14. doi: 10.1597/10-198. [DOI] [PubMed] [Google Scholar]
- 14.Oberoi S, Gill P, Chigurupati R, Hoffman WY, Hatcher DC, Vargervik K. Three-dimensional assessment of the eruption path of the canine in individuals with bone-grafted alveolar clefts using cone beam computed tomography. Cleft Palate Craniofac J. 2010;47:507–12. doi: 10.1597/08-171. [DOI] [PubMed] [Google Scholar]
- 15.Dalessandri D, Laffranchi L, Tonni I, Zotti F, Piancino MG, Paganelli C, et al. Advantages of cone beam computed tomography (CBCT) in the orthodontic treatment planning of cleidocranial dysplasia patients: a case report. Head Face Med. 2011;7:6. doi: 10.1186/1746-160X-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nur RB, Çakan DG, Arun T. Evaluation of Facial Hard and Soft Tissue Asymmetry using Cone Beam Computed Tomography. Am J Orthod Dentofacial Orthop. 2016;149:225–37. doi: 10.1016/j.ajodo.2015.07.038. [DOI] [PubMed] [Google Scholar]
- 17.Ilguy D, Ilguy M, Fisekcioglu E, Dolekoglu S, Ersan N. Articular eminence inclination, height, and condyle morphology on cone beam computed tomography. ScientificWorldJournal. 2014;2014 doi: 10.1155/2014/761714. 761714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Habeeb M, Boucher N, Chung CH. Effects of rapid palatal expansion on the sagittal and vertical dimensions of the maxilla: a study on cephalograms derived from cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2013;144:398–403. doi: 10.1016/j.ajodo.2013.04.012. [DOI] [PubMed] [Google Scholar]
- 19.Kanomi R, Deguchi T, Kakuno E, Takano-Yamamoto T, Roberts WE. CBCT of skeletal changes following rapid maxillary expansion to increase arch-length with a development- dependent bonded or banded appliance. Angle Orthod. 2013;83:851–7. doi: 10.2319/082012-669.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Toklu MG, Germec-Cakan D, Tozlu M. Periodontal, dentoalveolar, and skeletal effects of tooth-borne and tooth-bone-borne expansion appliances. Am J Orthod Dentofacial Orthop. 2015;148:97–109. doi: 10.1016/j.ajodo.2015.02.022. [DOI] [PubMed] [Google Scholar]
- 21.Bouwens DG, Cevidanes L, Ludlow JB, Phillips C. Comparison of mesiodistal root angulation with posttreatment panoramic radiographs and cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2011;139:126–32. doi: 10.1016/j.ajodo.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson DP. MSc thesis. University of Michigan, School of Dentistry; 2011. Effects of curve of Wilson correction and pretreatment boundary conditions on quantitative changes in alveolar bone morphology. [Google Scholar]
- 23.Feng X, Li G, Qu Z, Liu L, Näsström K, Shi XQ. Comparative analysis of upper airway volume with lateral cephalograms and cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2015;147:197–204. doi: 10.1016/j.ajodo.2014.10.025. [DOI] [PubMed] [Google Scholar]
- 24.Kuijpers MA, Chiu YT, Nada RM, Carels CE, Fudalej PS. Three-dimensional imaging methods for quantitative analysis of facial soft tissues and skeletal morphology in patients with orofacial clefts: a systematic review. PLoS One. 2014;9:e93442. doi: 10.1371/journal.pone.0093442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Moraes ME, Hollender LG, Chen CS, Moraes LC, Balducci I. Evaluating craniofacial asymmetry with digital cephalometric images and cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2011;139:523–31. doi: 10.1016/j.ajodo.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 26.European Comission. Radiation protection no 172. Cone beam CT for dental and maxillofacial radiology (evidence-based guidelines) 2012. (cited 2017 Nov 17). Available from: URL: http:/www.sedentexct.eu/files/radiation_protection_172.pdf.
- 27.Kau CH, Richmond S, Zhurov AI, Knox J, Chestnutt I, Hartles F, et al. Reliability of measuring facial morphology with a 3-dimensional laser scanning system. Am J Orthod Dentofacial Orthop. 2005;128:424–30. doi: 10.1016/j.ajodo.2004.06.037. [DOI] [PubMed] [Google Scholar]
- 28.Kovacs L, Zimmermann A, Brockmann G, Baurecht H, Schwenzer-Zimmerer K, Papadopulos NA, et al. Accuracy and precision of the three-dimensional assessment of the facial surface using a 3-D laser scanner. IEEE Trans Med Imaging. 2006;25:742–54. doi: 10.1109/TMI.2006.873624. [DOI] [PubMed] [Google Scholar]
- 29.Kau CH, Richmond S. Three-dimensional imaging for orthodontics and maxillofacial surgery. Iowa: Willey-Blackwell; 2010. [DOI] [Google Scholar]
- 30.Djordjevic J, Pirttiniemi P, Harila V, Heikkinen T, Toma AM, Zhurov AI, et al. Three-dimensional longitudinal assessment of facial symmetry in adolescents. Eur J Orthod. 2011;35:143–51. doi: 10.1093/ejo/cjr006. [DOI] [PubMed] [Google Scholar]
- 31.Djordjevic J, Lewis BM, Donaghy CE, Zhurov AI, Knox J, Hunter L, et al. Facial shape and asymmetry in 5-year-old children with repaired unilateral cleft lip and/or palate: an exploratory study using laser scanning. Eur J Orthod. 2012;36:497–505. doi: 10.1093/ejo/cjs075. [DOI] [PubMed] [Google Scholar]
- 32.Nute SJ, Moss JP. Three-dimensional facial growth studied by optical surface scanning. J Orthod. 2000;27:31–8. doi: 10.1093/ortho/27.1.31. [DOI] [PubMed] [Google Scholar]
- 33.Moss JP, Ismail SF, Hennessy RJ. Three-dimensional assessment of treatment outcomes on the face. Orthod Craniofac Res. 2003;6:126–31. doi: 10.1034/j.1600-0544.2003.245.x. [DOI] [PubMed] [Google Scholar]
- 34.Meehan M, Teschner M, Girod S. Three-dimensional simulation and prediction of craniofacial surgery. Orthod Craniofac Res. 2003;6:102–7. doi: 10.1034/j.1600-0544.2003.242.x. [DOI] [PubMed] [Google Scholar]
- 35.Jeon H, Lee SJ, Kim TW, Donatelli RE. Three-dimensional analysis of lip and perioral soft tissue changes after debonding of labial brackets. Orthod Craniofac Res. 2013;16:65–74. doi: 10.1111/ocr.12006. [DOI] [PubMed] [Google Scholar]
- 36.Kusnoto B, Evans CA. Reliability of a 3D surface laser scanner for orthodontic applications. Am J Orthod Dentofacial Orthop. 2002;122:342–8. doi: 10.1067/mod.2002.128219. [DOI] [PubMed] [Google Scholar]
- 37.Devlin MF, Ray A, Raine P, Bowman A, Ayoub AF. Facial symmetry in unilateral cleft lip and palate following alar base augmentation with bone graft: a three-dimensional assessment. Cleft Palate Craniofac J. 2007;44:391–5. doi: 10.1597/06-179.1. [DOI] [PubMed] [Google Scholar]
- 38.Plooij JM, Swennen GR, Rangel FA, Maal TJ, Schutyser FA, Bronkhorst EM, et al. Evaluation of reproducibility and reliability of 3D soft tissue analysis using 3D stereo- photogrammetry. Int J Oral Maxillofac Surg. 2009;38:267–73. doi: 10.1016/j.ijom.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 39.Kim YK, Lee NK, Moon SW, Jang MJ, Kim HS, Yun PY. Evaluation of soft tissue changes around the lips after bracket debonding using three-dimensional stereophotogrammetry. Angle Orthod. 2015;85:833–40. doi: 10.2319/090414.622.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Baysal A, Ozturk MA, Sahan AO, Uysal T. Facial soft-tissue changes after rapid maxillary expansion analyzed with 3-dimensional stereophotogrammetry: A randomized, controlled clinical trial. Angle Orthod. 2016;86:934–42. doi: 10.2319/111315-766.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ayoub AF, Siebert P, Moos KF, Wray D, Urquhart C, Niblett TB. A vision based 3D capture system for maxillofacial assessment and surgical planning. Br J Oral Maxillofac Surg. 1998;36:353–57. doi: 10.1016/S0266-4356(98)90646-5. [DOI] [PubMed] [Google Scholar]
- 42.Wong JY, Oh AK, Ohta E, Hunt AT, Rogers GF, Mulliken JB, et al. Validity and reliability of craniofacial anthropometric measurement of 3D digital photogrammetric images. Cleft Palate Craniofac J. 2008;45:232–9. doi: 10.1597/06-175. [DOI] [PubMed] [Google Scholar]
- 43.Bugaighis I, Tiddeman B, Mattick CR, Hobson R. 3D comparison of average faces in subjects with oral clefts. Eur J Orthod. 2012;36:365–72. doi: 10.1093/ejo/cjs060. [DOI] [PubMed] [Google Scholar]
- 45.Karatas OH, Toy E. Three-dimensional imaging techniques: A literature review. Eur J Dent. 2014;8:132–40. doi: 10.4103/1305-7456.126269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hall RK. The role of CT, MRI and 3D imaging in the diagnosis of temporomandibular joint and other orofacial disorders in children. Aust Orthod J. 1994;13:86–94. [PubMed] [Google Scholar]
- 47.Mah J, Hatcher D. Current status and future needs in craniofacial imaging. Orthod Caniofacial Res. 2003;6:10–6. doi: 10.1034/j.1600-0544.2003.230.x. [DOI] [PubMed] [Google Scholar]
- 48.Detterbeck A, Hofmeister M, Haddad D, Weber D, Schmid M, Hölzing A, et al. Determination of the mesio-distal tooth width via 3D imaging techniques with and without ionizing radiation: CBCT, MSCT, and μCT versus MRI. Eur J Orthod. 2017;39:310–9. doi: 10.1093/ejo/cjw047. [DOI] [PubMed] [Google Scholar]
- 49.Heil A, Gonzalez EL, Hilgenfeld T, Kickingereder P, Bendszus M, Heiland S, et al. Lateral cephalometric analysis for treatment planning in orthodontics based on MRI compared with radiographs: A feasibility study in children and adolescents. PLoS One. 2017;12:e0174524. doi: 10.1371/journal.pone.0174524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hallac RR, Feng J, Kane AA, Seaward JR. Dynamic facial asymmetry in patients with repaired cleft lip using 4D imaging (video stereophotogrammetry) J Craniomaxillofac Surg. 2017;45:8–12. doi: 10.1016/j.jcms.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 51.Joda T, Brägger U, Gallucci G. Systematic literature review of digital three-dimensional superimposition techniques to create virtual dental patients. Int J Oral Maxillofac Implants. 2015;30:330–7. doi: 10.11607/jomi.3852. https://doi.org/10.11607/jomi.3852. [DOI] [PubMed] [Google Scholar]
- 52.Plooij JM, Maal TJ, Haers P, Borstlap WA, Kuijpers-Jagtman AM, Bergé SJ. Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery. A systematic review. Int J Oral Maxillofac Surg. 2011;40:341–52. doi: 10.1016/j.ijom.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 53.Aboul-Hosn Centenero S, Hernández-Alfaro F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results–our experience in 16 cases. J Craniomaxillofac Surg. 2012;40:162–8. doi: 10.1016/j.jcms.2011.03.014. [DOI] [PubMed] [Google Scholar]
- 54.Swennen GR, Schutyser FAC. Three-dimensional virtual approach to diagnosis and treatment planning of maxillofacial deformity. In: Bell WH, Guerrero CA, editors. Distraction osteogenesis of the facial skeleton. chapter 06 Hamilton: BC Decker Inc; 2006. [Google Scholar]
- 55.Goracci C, Franchi L, Vichi A, Ferrari M. Accuracy, reliability, and efficiency of intraoral scanners for full-arch impressions: a systematic review of the clinical evidence. Eur J Orthod. 2016;38:422–8. doi: 10.1093/ejo/cjv077. [DOI] [PubMed] [Google Scholar]




