Neutrophil removal from inflammatory sites is regulated by lipid mediator signals between macrophages and neutrophils.
Abstract
Neutrophils are the first immune cells recruited to a site of injury or infection, where they perform many functions. Having completed their role, neutrophils must be removed from the inflammatory site—either by apoptosis and efferocytosis or by reverse migration away from the wound—for restoration of normal tissue homeostasis. Disruption of these tightly controlled physiological processes of neutrophil removal can lead to a range of inflammatory diseases. We used an in vivo zebrafish model to understand the role of lipid mediator production in neutrophil removal. Following tailfin amputation in the absence of macrophages, neutrophillic inflammation does not resolve, due to loss of macrophage-dependent handling of eicosanoid prostaglandin E2 (PGE2) that drives neutrophil removal via promotion of reverse migration. Knockdown of endogenous PGE synthase gene reveals PGE2 as essential for neutrophil inflammation resolution. Furthermore, PGE2 is able to signal through EP4 receptors during injury, causing an increase in Alox12 production and switching toward anti-inflammatory eicosanoid signaling. Our data confirm regulation of neutrophil migration by PGE2 and LXA4 (lipoxin A4) in an in vivo model of inflammation resolution. This pathway may contain therapeutic targets for driving inflammation resolution in chronic inflammatory disease.
INTRODUCTION
Inflammation is a critical process that maintains normal tissue homeostasis following injury or infection, by removing potential pathogens and beginning the process of wound repair and healing. Neutrophils are the first immune cells recruited to a site of injury or infection, where they carry out a number of functions (1). They destroy foreign pathogens, control the spread of infection, and thereby minimize tissue damage. Neutrophils engulf bacteria and cell debris at the site of inflammation through phagocytosis and release antimicrobial molecules by degranulation. Along with the release of reactive oxygen species, this activity aids in the destruction of pathogens (2) and permits neutrophil penetration into otherwise inaccessible tissues (3). Having completed their role, neutrophils must then be removed from the inflammatory site for successful inflammation resolution to occur. If this tightly controlled physiological process is disrupted, then failure of inflammation resolution can lead to inflammatory diseases such as chronic obstructive pulmonary disease.
There are several mechanisms by which neutrophils can be removed from sites of inflammation. Caspase-dependent neutrophil apoptosis and subsequent efferocytosis by macrophages have been shown to contribute to the successful resolution of inflammation in mouse (4), human (5), and zebrafish (6). Natural killer cells can also induce granulocyte apoptosis as a proresolving mechanism (7). Neutrophil apoptosis is tightly coupled to uptake by macrophages to prevent tissue damage (8). Macrophages phagocytose pathogens and apoptotic cells and contribute to inflammation resolution (9), tissue remodeling, and regeneration (9, 10); however, their influence on inflammation resolution is incompletely defined.
More recently, it has been demonstrated that neutrophils can also undergo reverse migration away from sites of inflammation, which, in some circumstances, might contribute to the dissipation of the inflammatory burden and hence to inflammation resolution (11, 12). In the zebrafish, reverse migration is anti-inflammatory and is suppressed by proinflammatory stimuli such as hypoxia (13). Variations on this process have also been seen in mouse models (14, 15) and in human neutrophils (16, 17). Understanding the molecular mechanisms that govern neutrophil removal, either via efferocytosis or via reverse migration, is essential to developing new therapeutics for inflammation resolution.
Macrophages are well known to be key mediators in determining the outcome of the inflammatory response (18). Macrophages and neutrophils secrete a range of pro- and anti-inflammatory cytokines, dependent on the local inflammatory environment. Studies in mammalian systems (19, 20) have shown that upon uptake of apoptotic cells, macrophages regulate pro- and anti-inflammatory cytokine production (21). When fed with apoptotic neutrophils, lipopolysaccharide-stimulated human monocyte-derived macrophages down-regulate key proinflammatory cytokines and up-regulate anti-inflammatory mediators transforming growth factor–β1 (TGFβ1), prostaglandin E2 (PGE2), and platelet activating factor (PAF). Prostaglandins, such as PGE2, are not stored in cells, but rather produced following arachidonic acid metabolism and therefore can be produced by almost all cells in the body (22). PGE2 is the most abundant prostaglandin in humans (23) generated via the action of cyclooxygenase enzymes. While PGE2 is known to have proinflammatory properties under defined conditions (24), it has also been shown to have anti-inflammatory functions (25). In zebrafish cancer models, inhibition of PGE2 production led to a change in macrophage behavior and enhanced proinflammatory activity (26), consistent with PGE2 directing macrophages toward an anti-inflammatory phenotype (27). In human peripheral blood neutrophils, PGE2 switches lipid mediator biosynthesis from predominantly proinflammatory leukotriene B4 [LTB4; 5-lipoxygenase (5-LO)–initiated pathway] to lipoxin A4 (LXA4), which reduces neutrophil infiltration into exudates (28). These studies support a role for PGE2 in influencing immune cell phenotype and led us to ask whether macrophages might be altering local lipid mediator signaling as a mechanism for influencing inflammation resolution in vivo.
Using a zebrafish model of in vivo inflammation resolution, we examined the potential role of the lipid mediator PGE2 in driving inflammation resolution. We demonstrate that macrophage uptake of apoptotic cells is necessary for successful inflammation resolution; PGE2 is produced and acts via EP4 receptors to drive inflammation resolution by reverse migration.
RESULTS
Macrophage clearance of apoptotic cells is necessary for successful resolution of neutrophilic inflammation in vivo
Inflammation requires the presence and activity of both neutrophils and macrophages. To test whether neutrophil dynamics were influenced by the presence of macrophages, we ablated macrophages using tissue-specific bacterial nitroreductase expression and by treatment with metronidazole as previously described (29, 30). Injury was performed on 3 days post fertilization (dpf) macrophage-ablated larvae, and neutrophil and macrophage numbers were assessed at the time points indicated (Fig. 1A). In control larvae, neutrophil numbers peaked between 4 and 6 hours post injury (hpi), with numbers returning to basal levels by 24 hpi, demonstrating spontaneous resolution of inflammation. Macrophages were recruited to the site of injury at a lower rate, with numbers plateauing at 12 hpi and remaining high until at least 24 hpi. In metronidazole-treated larvae, macrophages were not seen at the wound throughout the inflammatory time course, confirming successful ablation. Neutrophil numbers at the wound site were significantly increased at 24 hpi in macrophage-depleted larvae compared to control larvae, suggesting failed inflammation resolution (Fig. 1, A and B). In contrast to wound-site neutrophils, whole-body neutrophil counts were unaltered (Fig. 1C). These data demonstrate that macrophages are necessary at the site of tissue injury for normal inflammation resolution to occur.
Fig. 1. Macrophage clearance of apoptotic cells is necessary for successful resolution of neutrophilic inflammation in an in vivo zebrafish model.

(A) Neutrophil and macrophage counts at the wound in triple transgenic Tg(cfms:Gal4)i186;Tg(UAS:nfsB-mCherry)i149;Tg(mpx:EGFP)i114 larvae in the presence or absence of metronidazole. Neutrophil numbers are significantly higher at the wound in the absence of macrophages at 24 hpi, ***P < 0.0001. Statistics: Two-tailed nonpaired t test comparing neutrophil counts at 24 hpi with or without macrophage present. All data are n = 18 from three individual experiments plotted as means ± SEM. (B) Representative photomicrographs at 24 hpi showing increased neutrophil numbers at the site of injury in metronidazole-treated larvae compared to control. Wound area classed as area to the right of the yellow dashed line. Images were taken using ×10 magnification on a TE2000U inverted microscope (Nikon). (C) Total neutrophil numbers are not affected in the absence of macrophages. Data are n = 17 individual larvae. (D) Dual fluorescein isothiocyanate (FITC)–TSA and Rhodamine-TUNEL–positive cell counts in 8 dpf larvae at 24 hpi in the presence or absence of metronidazole show no significant difference (ns) in the percentage of apoptotic neutrophils. (E) Total apoptotic cell counts of TUNEL-positive cells in 8 dpf larvae at 24hpi. Macrophage-depleted larvae have significantly more apoptotic bodies at the wound, P = 0.0021. All data are presented as means ± SEM, n = 12, from two individual experiments for (D) and (E). (F) Representative photomicrographs of 8 dpf larvae at 24 hpi treated with either dimethyl sulfoxide (DMSO) control or metronidazole and dual-stained with FITC-TSA to label neutrophils and Rhodamine-TUNEL to label apoptotic cells at the wound (white arrow head). Images were taken using ×10 magnification on a TE2000U inverted microscope (Nikon).
In many models of inflammation, including the zebrafish, apoptosis of neutrophils contributes to inflammation resolution (6, 31). It might therefore be expected that macrophage depletion would leave apoptotic neutrophils at the wound site. To test whether the persistence of apoptotic corpses explained the increase in neutrophil numbers, we ablated macrophages by treating transgenic zebrafish with metronidazole at 7 dpf, injuring the tailfin as before at 8 dpf and then fixing at 24 hpi in 4% paraformaldehyde for TUNEL (terminal deoxynucleotidyl transferase–mediated deoxyuridine triphosphate nick end labeling) staining. Older larvae were used to increase cell numbers involved in the inflammatory response and to increase our ability to detect apoptotic events. We costained for endogenous peroxidase activity of neutrophils using a modification of the tyramide signal amplification (TSA) system (6). Double-stained cells corresponding to apoptotic neutrophils were then counted in macrophage-depleted larvae. Although the number of neutrophils was higher in the metronidazole-treated fish, the percentage of these neutrophils that were apoptotic was not different in the metronidazole-treated group (Fig. 1D), suggesting that persisting apoptotic neutrophil corpses did not account for the increase in neutrophil numbers in the absence of macrophages. During analysis of these images, we did notice a striking and unexpected increase in TUNEL-positive, TSA–negative cells in macrophage-depleted larvae (Fig. 1E), corresponding to apoptotic cells from nonneutrophil lineages. Representative images of stained cells are shown in Fig. 1F. This finding demonstrates that macrophages have an important role in removing apoptotic cells arising from tissue injury and that neutrophil persistence is not due to uncleared apoptotic neutrophils. This suggested to us that the majority of neutrophils might be removed from the wound by an alternative mechanism, such as reverse migration (12).
Inflammation resolution is not exclusively dictated by direct macrophage-neutrophil interaction
Neutrophil-macrophage interaction has been observed during the inflammatory response (32) and, under some circumstances, this has been shown to alter neutrophil migratory behavior in ways that could explain the observed failure of inflammation resolution in the absence of macrophages. We therefore sought to analyze neutrophil migration before and after interaction with macrophages to see whether that interaction caused neutrophils to migrate away from the wound, thereby dissipating the inflammatory burden. We tracked individual transgenically labeled macrophages and neutrophils, monitoring their interaction with other inflammatory cells. We tracked neutrophils and macrophages during an inflammatory response and plotted their x,y coordinates (Fig. 2A). Interaction between red (macrophage) and green (neutrophil) tracks was identified, and for each interaction, we identified whether contact between a macrophage and a neutrophil induced a significant change in behavior of the neutrophil. Direct cell contact was defined as when membranes of both cell types could be seen to touch. Interaction with a macrophage made no significant difference in the neutrophil meandering index (Fig. 2B), suggesting that interaction did not lead to a change in migratory behavior. Moreover, analysis of vector maps of neutrophils before and after interaction with a macrophage showed no clear difference between the two vector maps. The vector maps show the overall direction a neutrophil takes during the analyzed period (Fig. 2C). When analyzed, the percentage of reverse-migrated neutrophils that did not interact with a macrophage was 71%, compared to 65% of neutrophils reverse-migrating following a macrophage interaction (Fig. 2D). There was no significant difference in reverse migration behavior following macrophage interaction (P = 0.78, Fisher’s exact test). Direct contact between macrophages and neutrophils is therefore not sufficient to completely explain the observed changes in neutrophil direction, suggesting that an additional soluble factor is involved.
Fig. 2. Inflammation resolution is not exclusively dictated by direct macrophage-neutrophil interaction.

(A) Neutrophil (eight green lines) and macrophage (six magenta lines) tracks during an inflammatory response are plotted using their x,y coordinates. Larval caudal fin outline superimposed over tracks to indicate position at wound. (B) The meandering index (migration pattern) of neutrophils before and after contact with a macrophage shows no significant difference. Number of cells tracked: 14. Two-tailed paired t test. (C) Representative vector maps of overall neutrophil direction pre (green) and post macrophage (magenta) interaction. (D) Neutrophils (65%) that interacted with a macrophage reverse-migrated, whereas 71% neutrophils without a macrophage interaction also reverse-migrated away from the wound site. Chi-squared Fisher’s exact test indicated no significant difference in reverse migration with or without macrophage contact. P = 0.78.
The eicosanoid PGE2 is necessary for timely inflammation resolution
Previous studies in vitro have shown that, following uptake of apoptotic cells, macrophages can alter both their profile of cytokine production and their phenotype, from pro- to anti-inflammatory (21). It has been reported that levels of TGFβ1 and PGE2 increase following phagocytosis of apoptotic cells, whereas levels of cytokines such as interleukin-10 and tumor necrosis factor–α fail to increase further. When PGE2 production was blocked by indomethacin, TGFβ1 levels remained low, suggesting that PGE2 might be an upstream regulator of macrophage phenotype following uptake of apoptotic cells (21). We therefore sought to establish whether PGE2 could be a potential mediator in enhancing inflammation resolution following tail injury in vivo.
Microsomal PGE synthase, Ptges, is necessary for the conversion of prostaglandin H2 into PGE2 (33). PGE2 levels can be significantly reduced when Ptges expression is inhibited through the use of a morpholino antisense oligo (34). We used a previously published morpholino to knock down ptges to test the effect of reduced PGE2 levels on neutrophil behavior during inflammation. Reverse transcription polymerase chain reaction (PCR) demonstrated a significant reduction in correctly spliced ptges transcript at 4 dpf (fig. S1). Neutrophil counts throughout the inflammatory response revealed a significant increase in neutrophil recruitment to the wound site. At the later time points, during the resolution phase, significantly more neutrophils were retained at the site of injury (Fig. 3A). Since PGE2 has been shown to be critical in hematopoiesis (35), we looked at total neutrophil number in ptges morphants. Knockdown of ptges significantly reduced the number of neutrophils in the whole zebrafish (Fig. 3B), demonstrating that the increase in neutrophil numbers seen during inflammation is not due to an overall increase in neutrophils within the zebrafish. These data demonstrate that Ptges activity plays an important role in the resolution of inflammation.
Fig. 3. In vivo effects of PGE2 on neutrophils during an inflammatory response through genetic manipulation and PGE2 supplementation.
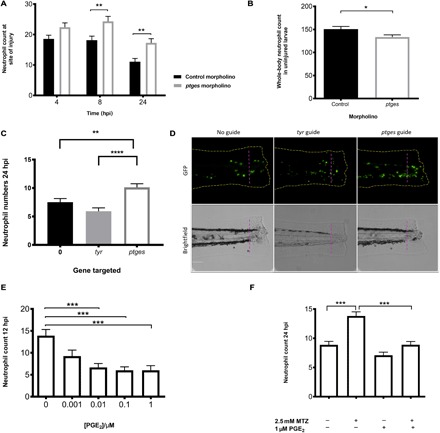
(A) Morpholino knockdown of endogenous ptges shows the necessity of PGE2 during inflammation resolution, with a significant increase in neutrophil numbers at the wound site at 8 and 24 hpi. *P < 0.01, two-way analysis of variance (ANOVA) with Bonferonni’s posttest. Data are n = minimum 30 from three experimental repeats. (B) Total neutrophil numbers in unstimulated larvae are reduced (P < 0.05, n = 24 larvae) in the absence of ptges, indicating that the increase during an inflammatory response is not due to increased neutrophils numbers overall. (C) Recapitulation of morphant phenotype in crispant. Three days post fertilization larvae with CRISPR/Cas9-mediated knockdown of ptges display significantly more neutrophils at the wound site at 24 hpi compared to a control-injected guide group targeting tyr. Injured crispants phenocopy ptges morphants. **P < 0.01, ****P < 0.0001, one-way ANOVA with Bonferroni posttest. Data are plotted as means ± SEM with a combined minimum of 40 larvae per group from three experimental repeats. (D) Representative images of crispant larvae at 24 hpi. Area to the right of the magenta dashed line indicates the wound site where GFP neutrophils are counted. Brightfield images demonstrate successful tyr knockdown as a reduction in pigmentation is visible. (E) Dose-response showing increasing concentrations of PGE2 significantly drive neutrophilic inflammation resolution. PGE2 was added at 8 hpi with neutrophil counts performed at 12 hpi. Neutrophil numbers at the site of injury are significantly reduced between 0.01 and 1 μM. (F) In the absence of macrophages, exogenous PGE2 is able to significantly reduce neutrophil numbers back to basal levels at 24hpi. ***P < 0.001, one-way ANOVA with Bonferroni posttest. Minimum of 32 larvae from three repeats. MTZ, metronidazole.
Genetic knockdown of ptges by morpholino has indicated that PGE2 production is essential for successful inflammation resolution. Because of the well-documented nonspecific effects of some morpholinos (36), we wanted to confirm our findings using a second approach. To address this, we have used CRISPR/Cas9 technology to support our findings (37). We designed a guide RNA (gRNA) that targets the ATG of ptges. Successful mutation by Cas9 protein deletes an MwoI restriction site, allowing the efficiency of the guide to be assessed and the larvae to be genotyped (fig. S4) with an uncut mutant band present at 293 base pairs (bp). Using our tailfin injury model, we have injected Tg(mpx:EGFP)i114 embryos at the one-cell stage with transactivating crRNA (tracrRNA) and Cas9 protein alone or in combination with a control gRNA, targeting tyrosinase (tyr) or a gRNA targeting ptges. Tyrosinase is the gene required for converting tyrosine into the pigment melanin, enabling visual identification of successful Cas9 knockdown (38). Genetic knockdown of ptges using Cas9 protein also leads to persisting neutrophils at the wound site compared to tyr-injected larvae (Fig. 3C), phenocopying the ptges morphant. Representative images were taken of each group to show this (Fig. 3D). These data strongly support the essential role of PGE2 for successful neutrophil removal from wound sites.
PGE2 is sufficient to drive inflammation resolution
PGE2 has both anti- (39) and proinflammatory effects dependent on the timing of its production and concentration (24, 40). To test whether PGE2 is sufficient to drive inflammation resolution, we immersed 3 dpf transgenic zebrafish larvae in a range of PGE2 concentrations at 8 hours after tailfin transection, after peak neutrophil recruitment had occurred. Wound neutrophil numbers were then assessed at 12 hpi to look for accelerated inflammation resolution. Twelve hours post injury is a time point where untreated larvae still have relatively high neutrophil numbers, and therefore, an enhanced reduction in neutrophil numbers would be detectable. Neutrophil numbers were significantly decreased in a dose-dependent manner when treated with PGE2, with 1 μM chosen as the optimal concentration (Fig. 3E). Exogenous PGE2 was able to rapidly enhance neutrophil removal from the site of injury to return neutrophil numbers to basal levels, thereby promoting successful inflammation resolution. As PGE2 reduced neutrophil numbers at the site of injury, we tested whether PGE2 accelerated neutrophil apoptosis at the wound site. Three days post fertilization larvae were injured, treated with PGE2, and fixed at 12 hpi for dual TUNEL (apoptosis) and TSA (neutrophil) staining. There was no difference in apoptotic cell numbers in larvae treated with PGE2 compared to control (fig. S2A). This suggests that neutrophils are removed through a mechanism other than apoptosis.
Since exogenous PGE2 could enhance inflammation resolution in our model, we investigated whether PGE2 could rescue the persisting neutrophil phenotype observed with macrophage ablation. Zebrafish larvae with nitroreductase-expressing macrophages and green fluorescent protein (GFP)–expressing neutrophils were treated with metronidazole at 2 dpf, injured at 3 dpf, and treated with PGE2 at 8 hpi. Cell counts were performed at 12 and 24 hpi. PGE2 was able to significantly reduce neutrophil numbers at the wound in metronidazole-treated larvae at 12 hpi compared to metronidazole-only larvae, with means of 4.6 ± 0.4 and 9.6 ± 0.8, respectively (fig. S2B). At 24 hpi, neutrophil numbers remained significantly reduced (Fig. 3F). These data demonstrate that PGE2 can drive inflammation resolution in the absence of macrophages, thus correcting the resulting inflammatory phenotype.
Neutrophil migration pattern, but not speed, is modulated by PGE2
During inflammation resolution, neutrophils can be removed through multiple mechanisms, including neutrophil apoptosis (41) and reverse migration (13, 42). Macrophage depletion did not result in a detectable difference in apoptotic neutrophil numbers compared to control, due to either residual macrophage activity or the infrequency of neutrophil apoptosis in the zebrafish model. Nonetheless, PGE2 can still reduce neutrophil numbers in these larvae, implying that neutrophils involved in the inflammatory response are being removed from the site of injury through a mechanism other than efferocytosis. We therefore investigated whether PGE2 could enhance inflammation resolution by acceleration of neutrophil reverse migration in tail-transected zebrafish larvae. Using well-established photoconversion protocols (43, 44) in transgenic zebrafish expressing the photoconvertable fluorophore kaede in neutrophils, we labeled neutrophils at the wound site at 8 hours after tailfin transection and observed the effects of addition of PGE2. Neutrophils at the wound site were tracked during the resolution phase of inflammation for 2 hours, from 10 to 12 hpi. Red, photoconverted neutrophils could be seen migrating away from the site of injury more readily in PGE2-treated larvae (Fig. 4, A to C). PGE2 significantly increased the number of neutrophils moving away from the wound area (Fig. 4D). This equates to there being a 50% difference in the number of reverse-migrated neutrophils in the PGE2-treated fish at 140 min after conversion, with a significant P value of 0.0015. These data show that PGE2 drives inflammation resolution by enhanced reverse migration away from the injury site.
Fig. 4. PGE2 drives accelerated reverse migration through EP4 receptor signaling.
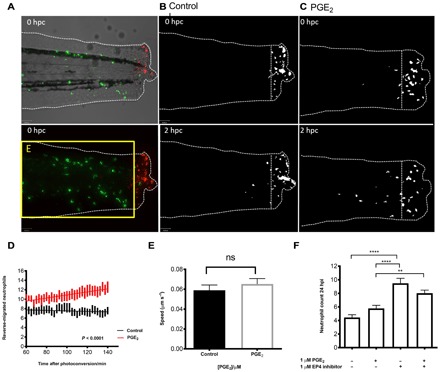
(A) Representative photomicrographs of control or PGE2-treated 3 dpf Tg(mpx:gal4)sh267;Tg(UAS:kaede)i222 larvae following photoconversion. The area to the right of the white dashed vertical line indicates wound site, where cells were photoconverted from green to red fluorescence. The yellow box E indicates the area into which the photoconverted cells migrate and corresponds to data in (D). (B) The red channel only is shown as a binary image of a control larva at 0 and 2 hours post conversion (hpc). Very little migration away from the wound site occurs between 10 and 12 hpi. (C) Binary images of the red channel of a PGE2-treated larva at 0 and 2 hpc. At 12 hpi, neutrophils have migrated away from the wound site, when treated with PGE2. (D) Plot showing the number of neutrophils moving away from the wound over 10 to 12 hpi, preincubated with or without PGE2 from 8 to 9 hpi. PGE2-treated neutrophils migrate away from the site of injury between 10 and 12 hpi more readily. Line of best fit shown is calculated by linear regression. P value shown is for the difference between the two slopes. (E) The speed of neutrophils moving away from the site of injury is not significantly different in the presence of exogenous PGE2, indicating that neutrophils migrate away sooner rather than at a greater speed in PGE2-treated larvae. (F) Neutrophil counts at 24 hpi show a significant increase in neutrophil number when EP4 signaling is blocked using the antagonist AH23848 **P < 0.01, ****P < 0.0001. Addition of PGE2 does not lead to significant abrogation of this effect, implying PGE2 signals through the EP4 receptor to promote neutrophil removal. All data are presented as means ± SEM, from n = 18 larvae for (D) and (E) and n = 53 for (F) from three experimental repeats. Images were taken using ×10 magnification on a TE2000U inverted microscope (Nikon).
We then asked whether this enhanced migration from the wound could be due to an increased migration speed of the neutrophils or to them leaving the site of injury sooner. Neutrophil migration speed away from the site of injury was measured in the same reverse migration assays described above (Fig. 4E). There was no significant difference in migration speed, implying that PGE2 may enhance release of neutrophils from their patrolling behavior at the wound site. The timing of PGE2 release is therefore critical to allow neutrophils to perform their role and then drive them away without compromising the inflammatory response.
Signaling through EP4 receptors contributes to inflammation resolution
PGE2 can signal through four prostanoid receptors: EP1, EP2, EP3, and EP4 (45). The expression and distribution of these receptors vary between different tissues and cell types. EP4 is considered a stimulatory receptor and is expressed on human macrophages, with studies showing that blockage of EP4 signaling inhibits cytokine release by macrophages (46). All four EP receptors are present in zebrafish, with multiple paralogs of each receptor (47). EP4b is the most abundant in adult zebrafish and is closest to human EP4 phylogenetically (48). To test whether PGE2 could be signaling in vivo through EP receptors, we used a previously published antagonist, AH23848, to inhibit EP4 receptor signaling (49). As we were assessing endogenous PGE2 signaling during a natural inflammatory response, where neutrophil numbers reduce from around 6 hpi, we performed 24 hpi counts for inhibitor assays to be able to detect neutrophil persistence over normal basal levels. Neutrophil counts at 24 hpi showed a significant increase in number when EP4 signaling was blocked, suggesting that endogenous PGE2 may act via this receptor. Addition of PGE2 at standard doses did not lead to significant abrogation of this effect (Fig. 5F). These data suggest that PGE2 signals predominantly through the EP4 receptor, contributing significantly to inflammation resolution. However, it remained unclear how EP4 signaling might lead to altered neutrophil behavior.
Fig. 5. EP receptor signaling and downstream activation of LOXs by PGE2 lead to lipid mediator class switching and inflammation resolution.
(A) Downstream activity of 15-LO was inhibited using the antagonist PD146176, also causing a significant delay in neutrophil removal from the wound site at 24 hpi. ****P < 0.0001. Data represent three replicates with a minimum of 30 fish per replicate. T test was performed. (B) Varying doses of PD146176 increase neutrophil numbers at the wound site at 24 hpi in a dose-dependent manner. (C) Exogenous PGE2 is unable to significantly decrease neutrophil numbers in the presence of the 15-LO inhibitor PD146176 at 24 hpi. ***P < 0.001. (D) qPCR expression analysis of alox12 following injury shows a significant increase up to the peak of inflammation. Fold change of expression to the reference gene represents the means ± SEM of four replicate experiments per time point, with a minimum of 50 larvae per replicate, therefore n = 200 individual larvae. P = 0.04, r 2 = 0.91.
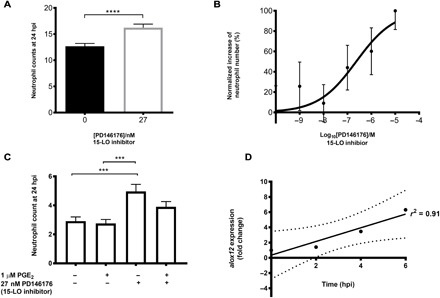
Up-regulation of lipoxygenase by PGE2 is necessary for inflammation resolution
The metabolism of the membrane lipid arachidonic acid is a complex pathway, producing not only prostaglandins but also other eicosanoids such as proresolving lipoxins and proinflammatory leukotrienes. Lipoxygenases (LOXs) are essential for the production of these metabolites, with select isozymes being key for particular pathways. Previous studies have shown that arachidonate 12-lipoxygenase (12-LO) or 15-lipoxygenase (15-LO) activity, in combination with arachidonate 5-lipoxygenase (5-LO), can produce lipoxins, and 5-LO activity alone forms leukotrienes (50). Increasing concentrations of PGE2 inhibit 5-LO translocation from the cytoplasm to the nucleus, abrogating leukotriene synthesis (51) and skewing the balance between pro- and anti-inflammatory mediators toward increased lipoxin synthesis—a process termed “lipid mediator class switching” (28). Zebrafish have the three key LOX genes for lipid mediator synthesis: alox12, alox5, and alox15b genes (52–54). To assess the contribution of lipoxin production during inflammation resolution in the zebrafish, we immersed injured transgenic larvae in PD146176, a specific 15-LO inhibitor (55). Again, as we hypothesized that there would be a delay in inflammation resolution, we performed 24 hpi counts for inhibitor assays to be able to detect neutrophil persistence over normal basal levels. We found that inhibiting 15-LO activity during inflammation led to a significant increase in neutrophil numbers at 24 hpi compared to control larvae (Fig. 5A), indicating persisting inflammation at the wound site. This effect was dose-dependent (Fig. 5B). Addition of exogenous PGE2 following 15-LO inhibition was unable to abrogate this effect, with neutrophil numbers remaining high at the wound site 24 hpi (Fig. 5C), supporting a mechanism of PGE2 acting upstream of 15-LO in this pathway.
The oxygenation of arachidonic acid by LOXs can occur at varying positions along the fatty acid carbon chain (50) and can determine the functionality of the protein according to which carbon is oxygenated and which amino acid residue is present at specific sites. In zebrafish, LOX genes are annotated in Ensembl as alox12 and alox15b; we predict that zebrafish Alox12 should function predominantly in the role of a 15-LO due to the presence of phenylalanine (F) at position 353 and a bulky valine (V) at position 418 [in comparison to the rabbit leukocyte 12-LO protein sequence (56) and associated with predominantly 15-LO activity in mammalian LOXs (57); fig. S3]. We therefore assessed alteration of expression of alox12 (the zebrafish putative 15-LO) by quantitative PCR (qPCR) during injury-induced inflammation. There was a significant linear increase in 12-LO expression up to 6 hpi (Fig. 5D), demonstrating that inflammation caused by injury induces a change in LOX activity. This suggests a plausible mechanism for the induction of reverse migration through increased lipoxin production during inflammation resolution.
Lipoxin A4 drives inflammation resolution via reverse migration
LXA4 is a proresolving product of arachidonic acid metabolism that inhibits neutrophil chemotaxis, transmigration, superoxide generation, and the production of proinflammatory cytokines (58). Because alox12 expression was increased during injury-induced inflammation, we next determined whether its key product LXA4 plays a role in inflammation in the zebrafish model. First, we added exogenous LXA4 to the injured larvae and assessed neutrophil number at 6 hpi. Our data demonstrate a protective effect of LXA4 acting to inhibit neutrophil chemotaxis, significantly reducing neutrophil recruitment to the wound site (Fig. 6A). This provides evidence that exogenous LXA4 is able to promote a response in our in vivo model. If PGE2 production following injury increases alox12 activity during inflammation resolution, and thereby increases endogenous LXA4 production, we would predict that LXA4 could allow removal of neutrophils already present at the wound site due to loss of sensitivity to local wound signals. To assess this, we performed reverse migration experiments in the presence of exogenous LXA4. LXA4 caused neutrophils to move away from the wound earlier than in untreated larvae (Fig. 6B), without altering neutrophil migration speed (Fig. 6C) or the path that the neutrophils take (Fig. 6D). Our data are best explained by proposing that production of endogenous LXA4 by Alox12 following injury-induced PGE2 production is the mechanism that promotes inflammation resolution in vivo.
Fig. 6. LXA4 drives inflammation resolution via reverse migration.
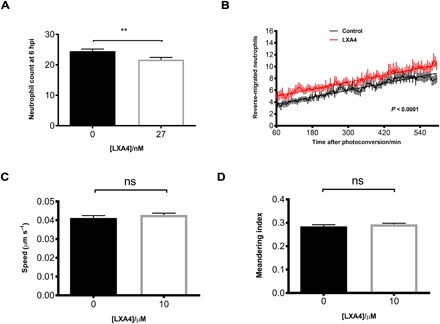
(A) Injection of LXA4 into zebrafish larvae causes a small but significant reduction in neutrophil numbers at the wound site at 6 hpi. n = 120 larvae. (B) Plot showing the number of neutrophils reverse-migrating away from the wound over a time course of 6 to 15 hpi, preinjected at 4 hpi with or without LXA4. LXA4-treated neutrophils migrate away from the site of injury sooner than control neutrophils. Line of best fit shown is calculated by linear regression. P value shown is for the difference between the two slopes. n = 21 larvae. (C) The speed of neutrophils moving away from the site of injury was measured and is not significantly different in the presence of exogenous LXA4. (D) The path the neutrophils take (meandering index) when moving away from the wound was also not significantly different when supplemented with LXA4. All data are presented as means ± SEM, from three experimental repeats.
DISCUSSION
Restoration of tissue homeostasis following infection or injury requires successful resolution of inflammation. Inflammation resolution should not occur before the threat is ablated, nor should inflammation persist longer than necessary. The process is therefore tightly regulated. Neutrophils and macrophages as a population are well positioned to assess the threat to the organism and determine the duration of the inflammatory response. Once the resolution is decided, neutrophils can either die at inflammatory sites by apoptosis and be cleared by macrophages (5) or can be removed from inflammatory sites by altered migratory patterns (reverse migration) (42). If this tightly controlled inflammatory process is disrupted, failure of inflammation resolution can lead to the tissue damage seen in chronic inflammatory diseases (59). The molecular mechanisms controlling the decisions on duration of inflammation are complex and yet to be fully determined. Existing evidence indicates that lipid mediator secretion is likely to be important in signaling inflammation resolution (60), but it is unknown which mediators regulate neutrophil removal from sites of inflammation in vivo. We have shown, for the first time, that the lipid mediator signaling molecule PGE2 is essential for determining the outcome of neutrophil inflammation in response to tissue injury. Moreover, our data suggest that alterations in LOX activity lead to production of LXA4. This lipid mediator class switching appears to be the critical mechanistic step by which macrophage PGE2 release after uptake of apoptotic cells promotes inflammation resolution in vivo.
Previous in vitro studies have suggested that phagocytosis of apoptotic neutrophils by macrophages might contribute toward successful inflammation resolution (21, 61). Ingestion of apoptotic cells by macrophages promotes an anti-inflammatory environment, suppressing proinflammatory cytokine production and promoting LXA4 production (21). While mice lacking macrophages and neutrophils show healing without excessive inflammation or scar formation, in macrophage-only depleted mice, neutrophils populated the wound area, with impaired wound morphology and delayed healing (62). We have shown that in the absence of macrophages, apoptotic bodies accumulate at the wound site, resulting in neutrophil persistence and prolonged inflammation. This finding demonstrates the importance of understanding macrophage-neutrophil interactions during inflammation resolution to prevent further damage to healing tissues.
Recent work has shown that reverse migration is a contributor to neutrophil removal from inflammatory sites (13, 15, 42, 63). It has been shown that macrophage recruitment and redox-SFK (Src family kinase) signaling play key roles in neutrophil-mediated inflammation resolution (32). These studies also suggest a direct contact mechanism between neutrophils and macrophages, which may direct neutrophil reverse migration; however, in the absence of macrophage contact, neutrophils are still able to reverse-migrate, suggesting that other, unknown factors may be involved. Tracking analysis of macrophage and neutrophil contact in our model of inflammation demonstrates that direct contact is not an essential requirement for reverse migration. Furthermore, our studies support the importance of a soluble factor, the lipid mediator PGE2, for successful inflammation resolution. Our data suggest that this lipid mediator is a key signaling molecule between macrophages and neutrophils during inflammation, leading to production of LXA4, enhancing neutrophil reverse migration and, hence, speeding inflammation resolution.
PGE2 is known to be involved in many cellular processes, including cell proliferation, apoptosis, angiogenesis, inflammation, and immune surveillance (64). The production of PGE2 from prostaglandin synthases is essential for the development of organisms past the gastrulation stage (34) and is crucial for hematopoietic stem cell homeostasis (35). However, to our knowledge, PGE2 has not been shown to be necessary for resolution of neutrophilic inflammation. We have shown by genetic and pharmacological approaches that the production of PGE2 is essential for inflammation to resolve and that PGE2 is sufficient to drive neutrophil removal from wound sites. PGE2 can promote neutrophil removal from wound sites in the absence of macrophages, implying an important connection between macrophages and the lipid mediator PGE2. This could prove to be a useful target for therapeutic intervention in chronic inflammatory disease.
PGE2 acts via EP receptors present on a range of cell types, including neutrophils, macrophages, and epithelial and endothelial cells. Neutrophils predominantly express EP2 and EP4 (65), both of which, upon activation, cause an increase in adenosine 3′,5′-monophosphate (cAMP) levels within the cell. An increase in intracellular cAMP can “reprogram” the cell to switch from 5-LO products to the production of 15-LO products (28). Our studies show PGE2 signaling through EP4 receptors to be important in the resolution of neutrophilic inflammation and that this activity is mediated via 15-LO products, most likely the anti-inflammatory mediator LXA4.
Human polymorphonuclear leukocytes in vitro markedly increase expression of 15-LO mRNA in the presence of PGE2 (28). Our data from whole animals show a significantly increased expression of the annotated zebrafish 12-LO mRNA following tailfin injury relative to time. Human blood neutrophils exposed to PGE2 inhibit LTB4 biosynthesis and demonstrate reduced neutrophil migration (66). Our data confirm the regulation of neutrophil migration by PGE2 and LXA4 in an in vivo model of inflammation resolution. Neutrophils more readily migrate away from the wound site when exposed to exogenous PGE2 or LXA4. The addition of PGE2 after the maximum recruitment of neutrophils to the wound is able to markedly enhance the reverse migration of neutrophils. The mechanism of this step is still unknown, but PGE2 alteration of LO activity would fit with its known role in inhibiting neutrophil recruitment (67). In our studies, exogenous LXA4 causes neutrophils to leave the wound sooner. LXA4 has been shown to inhibit chemokine signaling in neutrophils in vitro (68), suggesting a mechanism by which LXA4 facilitates neutrophil reverse migration from sites of inflammation. Mathematical modeling data from in vivo neutrophil migration following zebrafish tailfin wounding suggest that neutrophil reverse migration is a phenomenon of stochastic redistribution of neutrophils in the tissues (69). This suggests a model whereby neutrophils are retained at wounds by a molecular “retention signal” and that decay of this signal leads to reverse migration (12). Chemokine receptor desensitization would be a strong candidate for explaining how these retention signals might be initiated and subsequently decayed. LXA4 interference with these signals might be a potential mechanism by which PGE2 ultimately alters neutrophil migration patterns, leading to inflammation resolution.
In this context, an in vivo reporter would be useful to further elucidate the presence and activity of PGE2. Understanding the molecular mechanisms involved in neutrophil removal from wound sites, specifically during reverse migration, would greatly improve our understanding of inflammatory disease and provide potential strategies and targets for much needed therapeutic intervention.
MATERIALS AND METHODS
Maintenance and breeding of zebrafish
To visualize both macrophages and neutrophils within the same zebrafish larva, triple transgenic fish Tg(cfms:Gal4)i186;Tg(UAS:nfsB-mCherry)i149;Tg(mpx:EGFP)i114, as previously described (29), were incrossed. Tg(mpx:gal4)sh267;Tg(UASkaede)i222 zebrafish were used for photoconversion and neutrophil tracking experiments, subsequently termed mpx:kaede. Tg(mpx:EGFP)i114 zebrafish were used to study neutrophils during inflammation. Zebrafish strains were maintained according to standard protocols. Adult fish were maintained on a 14:10-hour light/dark cycle at 28°C in UK Home Office–approved facilities in The Bateson Centre aquaria at the University of Sheffield, under AWERB (Animal Welfare and Ethical Review Bodies) and UK Home Office–approved protocols.
Inflammation assay
Inflammation was induced in zebrafish embryos by tail transection as described previously (70). Embryos were anesthetized at 3 or 8 dpf by immersion in tricaine (0.168 mg/ml; Sigma-Aldrich), and tail transection was performed using a microscalpel (World Precision Instruments). Neutrophils and macrophages were counted at the site of transection at various time points including 2, 4, 6, 8, and 24 hpi using a fluorescence dissecting stereomicroscope (Leica).
In vivo cell-specific ablation
Metronidazole (Sigma-Aldrich) was dissolved to a concentration of 2.5 mM in E3 with 0.2% DMSO. Solutions of metronidazole were made fresh on the day of use with vigorous agitation until fully dissolved. Tg(cfms:Gal4)i186;Tg(UAS:nfsB-mCherry)i149;Tg(mpx:EGFP)i114 were immersed in metronidazole or E3 and 0.2% DMSO at 2 or 7 dpf overnight at 28°C for 15 hours. Larvae were wrapped in foil during the experiment. At 3 or 8 dpf, larvae were checked for macrophage depletion on a fluorescence dissecting stereomicroscope (Leica).
Neutrophil and apoptotic cell labeling
Rates of neutrophil apoptosis were assessed by dual staining with Rhodamine-TUNEL and FITC-TSA. Transgenic zebrafish larvae were injured at 8 dpf and fixed at 24 hpi in 4% paraformaldehyde. TUNEL (ApopTag Red; Millipore Corp.) staining labeled apoptotic cells with red fluorescence, and TSA (TSAplus kit; Fluorescence Systems, PerkinElmer Life and Analytical Sciences) staining labeled neutrophils with fluorescein green fluorescence. Neutrophils at the wound were imaged on an Eclipse TE2000-U inverted compound fluorescence microscope (Nikon), and neutrophil-specific apoptosis was assessed by the percentage of TSA-positive neutrophils labeled with TUNEL. Red TUNEL–positive–only cells were assessed for total apoptosis rates.
Cell tracking
To assess neutrophil migration behavior before and after interaction with a macrophage, transgenic larvae Tg(mpx:EGFP)i114 were crossed to Tg(mpeg1:mCherry-CAAX)sh378. Three days post fertilization larvae were injured, and images were taken every 3 min between 0 and 12 hpi using an Eclipse TE2000-U inverted compound fluorescence microscope (Nikon). Direct contact was defined as when cell membranes could be seen to touch. Comparisons of migration behavior were made over a 30-min period before and after interaction.
Compound treatment of zebrafish larvae
Following tail transection at 3 dpf, zebrafish larvae were screened at 4 hpi for neutrophil recruitment. Selected larvae were immersed in 1 μM PGE2 (Sigma-Aldrich) at 8 hpi with counts performed at 12 hpi to look for accelerated inflammation resolution and 24 hpi for correction of phenotype assays. Concentrations of PGE2 ranged from 0.01 to 10 μM for dose-response assays. The EP4 antagonist AH23848 (Cayman Chemicals) was used at a final concentration of 1 μM. Fish were incubated at 2 dpf, and tail transection was performed at 3 dpf. PD146176, a 15-LO inhibitor (Sigma-Aldrich), was injected at 6 hpi into the Duct of Cuvier to a final concentration of 27 nM in 2 dpf larvae. LXA4 (Cayman Chemicals) was injected into the Duct of Cuvier to a final concentration of 27 nM at 2 dpf, followed by tail transection and 6 hpi counts.
Reverse migration assay
Tail transection of Tg(mpx:gal4)sh267;Tg(UAS:kaede)i222 larvae was performed at 3 dpf. Embryos were raised to 8 hpi, incubated in 1 μM PGE2 for 1 hour, and mounted in 0.8% low-melting-point agarose (Sigma-Aldrich). An UltraVIEW PhotoKinesis device on an UltraVIEW VoX spinning disk confocal microscope (PerkinElmer Life and Analytical Sciences) was used to photoconvert Kaede-labeled cells at the wound site using 120 pulses of the 405-nm laser at 40% laser power. Embryos were transferred to an Eclipse TE2000-U inverted compound fluorescence microscope (Nikon), where a 1394 ORCA-ERA camera (Hamamatsu Photonics Inc) was used to capture a time-lapse series with 2.5-min intervals for 2 hours. Tracking analysis of red-fluorescing neutrophils was performed in Volocity 6 (Improvision; PerkinElmer Life and Analytical Sciences), using the intensity of fluorescence to identify individually labeled neutrophils over time. LXA4 was injected at 4 hpi at a final concentration of 27 nM, neutrophils at the wound site was photoconverted at 5 hpi, and larvae were time-lapsed between 6 and 15 hpi. Speed data were calculated using tracking time lapses, where larvae were incubated in 10 μM LXA4. We refer to the track a neutrophil takes as the meandering index of the neutrophil, where a direct movement in a straight line from A to B is given the value of 1. Tracks that are not a straight line fall between zero and 1.
Morpholino studies
All morpholinos were obtained from GeneTools LLC. ptges splice blocking morpholino is described by Feng et al. (26). Standard control morpholino (CoMo; 0.5 nl of 0.4mM) or ptges morpholino was injected into embryos at the one-cell stage previously described (26). Injected larvae were incubated in 5 μM PGE2 at the onset of epiboly to compensate for the PGE2 required for normal development up to 42 hours post fertilization (hpf ). PGE2 was then withdrawn from the larvae at 48 hpf. At 3 dpf, larvae were injured, and neutrophil counts were performed at 4, 8, and 24 hpi. Knockdown was assessed in the same fish at 48 hpf and 4 dpf using reverse transcription PCR, and primer sequences were PTGESF1 5′-CTCGGGAGCGACATACAGTT-3′ and PTGESR1 5′-AGCAGATATGCAACGCTGTG-3′. ptges splice blocking morpholino leads to deletion of exon 2 and a loss of 83 bp.
Quantitative PCR
Three days post fertilization larvae were injured, and total RNA was extracted using TRIzol at various time points after injury. Complementary DNA synthesis was performed using SuperScript II (Thermo Fisher Scientific), and qPCR experiments using a DyNAmo Flash SYBR green qPCR kit (Thermo Fisher Scientific) were carried out. ΔCT was calculated using elongation factor 1 alpha as a reference gene. Relative expression levels were plotted after determining ΔΔCt by normalizing to a single sample with a high ΔCT value. Primer sequences for alox12 gene were alox12F ccacggaatatcaccagatgga and alox12R attcagagtcgttgtgggtatc.
gRNA design and CRISPR/Cas9 injection
The online web tool CHOPCHOP was used to design a specific gRNA spanning the ATG of ptges. Purified gRNA, Cas9 protein, and tracrRNA were purchased from Sigma-Aldrich. The ptges guide sequence is gauagaggcucaagaugcucguuuuagagcuaugcuguuuug, targeting sequence gatagaggctcaagatgctcggg of the gene. Each embryo was injected with 1 nl of 6.6 nM gRNA, tracrRNA, and Cas9 protein at the one-cell stage. Genomic DNA was extracted from injected larvae, and PCR amplification was performed, generating a 345-bp product spanning the ATG of the ptges gene (ENSDARG00000020136). Primers used were ptges guide F1 gccaagtataatgaggaatggg and ptges guide R1 aatgtttggattaaacgcgact. Genotype was determined by digestion with MwoI. Wild-type PCR products produce 184-, 109-, and 52-bp bands. Mutant forms produce 293- and 52-bp bands.
Statistical analysis
Data were analyzed (Prism 7.0; GraphPad Software) using unpaired, two-tailed t tests for comparisons between two groups and one-way ANOVA (with appropriate posttest adjustment) for other data. A χ2 Fisher’s exact test was used to assess statistical significance in Fig. 2. Linear regression analysis was performed on qPCR data in Fig. 6.
Supplementary Material
Acknowledgments
We are grateful for the use of The Bateson Centre aquarium at the University of Sheffield and their support. The authors would like to thank M. Dunning of the Sheffield Bioinformatics Core for bioinformatic support. Sheffield Bioinformatics Core is supported by the Faculty of Sciences and Faculty of Medicine, Dentistry and Health at the University of Sheffield and the National Institute for Health Research Sheffield Biomedical Research Centre. Funding: This work was supported by a Medical Research Council (MRC) Senior Clinical Fellowship with Fellowship-Partnership Award and MRC Programme Grants to S.A.R (G0701932 and MR/M004864/1) and an MRC Centre Grant (G0700091). F.E. was funded by a CJ Martin Fellowship from the Australian National Health and MRC (grant 1054664). Funding for Y.F. was provided by Wellcome Trust Sir Henry Dale Fellow 100104AIA. Funding for B.D.L. is an NIH grant (P01GM095467). Author contributions: S.A.R. planned the study and designed the experiments with contribution from C.A.L., F.E., and B.D.L. C.A.L., J.A.L., A.L.R., M.J.G.S., and F.E. performed the experiments. Y.F., B.D.L., and M.K.B.W. provided scientific expert knowledge. C.A.L. and S.A.R. analyzed the data. C.A.L. and S.A.R. wrote the manuscript with assistance from all the other authors. Competing interests: The authors declare that they have no competing interests. Data and materials availability: All data needed to evaluate the conclusions in the paper are present in the paper and/or the Supplementary Materials. Additional data related to this paper may be requested from the authors. Materials can be obtained through a material transfer agreement.
SUPPLEMENTARY MATERIALS
Supplementary material for this article is available at http://advances.sciencemag.org/cgi/content/full/4/9/eaar8320/DC1
Fig. S1. Reverse transcription PCR demonstrates successful exon deletion.
Fig. S2. PGE2 drives resolution of inflammation in the absence of macrophages by 12 hpi and does not alter neutrophil apoptosis.
Fig. S3. Amino acid positions 353 and 418 determine LOX functionality.
Fig. S4. Genotyping method for ptges crispant.
REFERENCES AND NOTES
- 1.Amulic B., Cazalet C., Hayes G. L., Metzler K. D., Zychlinsky A., Neutrophil function: From mechanisms to disease. Annu. Rev. Immunol. 30, 459–489 (2012). [DOI] [PubMed] [Google Scholar]
- 2.Babior B. M., Kipnes R. S., Curnutte J. T., Biological defense mechanisms. The production by leukocytes of superoxide, a potential bactericidal agent. J. Clin. Invest. 52, 741–744 (1973). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mittal M., Siddiqui M. R., Tran K., Reddy S. P., Malik A. B., Reactive oxygen species in inflammation and tissue injury. Antioxid. Redox Signal. 20, 1126–1167 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cox G., Crossley J., Xing Z., Macrophage engulfment of apoptotic neutrophils contributes to the resolution of acute pulmonary inflammation in vivo. Am. J. Respir. Cell Mol. Biol. 12, 232–237 (1995). [DOI] [PubMed] [Google Scholar]
- 5.Grigg J. M., Silverman M., Savill J. S., Sarraf C., Haslett C., Neutrophil apoptosis and clearance from neonatal lungs. Lancet 338, 720–722 (1991). [DOI] [PubMed] [Google Scholar]
- 6.Loynes C. A., Martin J. S., Robertson A., Trushell D. M. I., Ingham P. W., Whyte M. K. B., Renshaw S. A., Pivotal advance: Pharmacological manipulation of inflammation resolution during spontaneously resolving tissue neutrophilia in the zebrafish. J. Leukoc. Biol. 87, 203–212 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barnig C., Cernadas M., Dutile S., Liu X., Perrella M. A., Kazani S., Wechsler M. E., Israel E., Levy B. D., Lipoxin A4 regulates natural killer cell and type 2 innate lymphoid cell activation in asthma. Sci. Transl. Med. 5, 174ra26 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khanna S., Biswas S., Shang Y., Collard E., Azad A., Kauh C., Bhasker V., Gordillo G. M., Sen C. K., Roy S., Macrophage dysfunction impairs resolution of inflammation in the wounds of diabetic mice. PLOS ONE 5, e9539 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Savill J., Fadok V., Corpse clearance defines the meaning of cell death. Nature 407, 784–788 (2000). [DOI] [PubMed] [Google Scholar]
- 10.Murray P. J., Wynn T. A., Protective and pathogenic functions of macrophage subsets. Nat. Rev. Immunol. 11, 723–737 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robertson A. L., Holmes G. R., Bojarczuk A. N., Burgon J., Loynes C. A., Chimen M., Sawtell A. K., Hamza B., Willson J., Walmsley S. R., Anderson S. R., Coles M. C., Farrow S. N., Solari R., Jones S., Prince L. R., Irimia D., Rainger G. E., Kadirkamanathan V., Whyte M. K. B., Renshaw S. A., A zebrafish compound screen reveals modulation of neutrophil reverse migration as an anti-inflammatory mechanism. Sci. Transl. Med. 6, 225ra29 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nourshargh S., Renshaw S. A., Imhof B. A., Reverse migration of neutrophils: Where, when, how, and why? Trends Immunol. 37, 273–286 (2016). [DOI] [PubMed] [Google Scholar]
- 13.Elks P. M., van Eeden F. J., Dixon G., Wang X., Reyes-Aldasoro C. C., Ingham P. W., Whyte M. K. B., Walmsley S. R., Renshaw S. A., Activation of hypoxia-inducible factor-1α (Hif-1α) delays inflammation resolution by reducing neutrophil apoptosis and reverse migration in a zebrafish inflammation model. Blood 118, 712–722 (2011). [DOI] [PubMed] [Google Scholar]
- 14.Woodfin A., Voisin M.-B., Beyrau M., Colom B., Caille D., Diapouli F.-M., Nash G. B., Chavakis T., Albelda S. M., Rainger G. E., Meda P., Imhof B. A., Nourshargh S., The junctional adhesion molecule JAM-C regulates polarized transendothelial migration of neutrophils in vivo. Nat. Immunol. 12, 761–769 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang J., Hossain M., Thanabalasuriar A., Gunzer M., Meininger C., Kubes P., Visualizing the function and fate of neutrophils in sterile injury and repair. Science 358, 111–116 (2017). [DOI] [PubMed] [Google Scholar]
- 16.Buckley C. D., Ross E. A., McGettrick H. M., Osborne C. E., Haworth O., Schmutz C., Stone P. C. W., Salmon M., Matharu N. M., Vohra R. K., Nash G. B., Rainger G. E., Identification of a phenotypically and functionally distinct population of long-lived neutrophils in a model of reverse endothelial migration. J. Leukoc. Biol. 79, 303–311 (2006). [DOI] [PubMed] [Google Scholar]
- 17.Hamza B., Wong E., Patel S., Cho H., Martel J., Irimia D., Retrotaxis of human neutrophils during mechanical confinement inside microfluidic channels. Integr. Biol. 6, 175–183 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li L., Yan B., Shi Y.-Q., Zhang W.-Q., Wen Z.-L., Live imaging reveals differing roles of macrophages and neutrophils during zebrafish tail fin regeneration. J. Biol. Chem. 287, 25353–25360 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McDonald P. P., Fadok V. A., Bratton D., Henson P. M., Transcriptional and translational regulation of inflammatory mediator production by endogenous TGF-β in macrophages that have ingested apoptotic cells. J. Immunol. 163, 6164–6172 (1999). [PubMed] [Google Scholar]
- 20.Michlewska S., Dransfield I., Megson I. L., Rossi A. G., Macrophage phagocytosis of apoptotic neutrophils is critically regulated by the opposing actions of pro-inflammatory and anti-inflammatory agents: Key role for TNF-α. FASEB J. 23, 844–854 (2009). [DOI] [PubMed] [Google Scholar]
- 21.Fadok V. A., Bratton D. L., Konowal A., Freed P. W., Westcott J. Y., Henson P. M., Macrophages that have ingested apoptotic cells in vitro inhibit proinflammatory cytokine production through autocrine/paracrine mechanisms involving TGF-beta, PGE2, and PAF. J. Clin. Invest. 101, 890–898 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith W. L., The eicosanoids and their biochemical mechanisms of action. Biochem. J. 259, 315–324 (1989). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Serhan C. N., Levy B., Success of prostaglandin E2 in structure–function is a challenge for structure-based therapeutics. Proc. Natl. Acad. Sci. U.S.A. 100, 8609–8611 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tchetina E. V., Di Battista J. A., Zukor D. J., Antoniou J., Poole A. R., Prostaglandin PGE2 at very low concentrations suppresses collagen cleavage in cultured human osteoarthritic articular cartilage: This involves a decrease in expression of proinflammatory genes, collagenases and COL10A1, a gene linked to chondrocyte hypertrophy. Arthritis Res. Ther. 9, R75 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scher J. U., Pillinger M. H., The anti-inflammatory effects of prostaglandins. J. Invest. Med. 57, 703–708 (2009). [DOI] [PubMed] [Google Scholar]
- 26.Feng Y., Renshaw S., Martin P., Live imaging of tumor initiation in zebrafish larvae reveals a trophic role for leukocyte-derived PGE2. Curr. Biol. 22, 1253–1259 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nakanishi Y., Nakatsuji M., Seno H., Ishizu S., Akitake-Kawano R., Kanda K., Ueo T., Komekado H., Kawada M., Minami M., Chiba T., COX-2 inhibition alters the phenotype of tumor-associated macrophages from M2 to M1 in ApcMin/+ mouse polyps. Carcinogenesis 32, 1333–1339 (2011). [DOI] [PubMed] [Google Scholar]
- 28.Levy B. D., Clish C. B., Schmidt B., Gronert K., Serhan C. N., Lipid mediator class switching during acute inflammation: Signals in resolution. Nat. Immunol. 2, 612–619 (2001). [DOI] [PubMed] [Google Scholar]
- 29.Gray C., Loynes C. A., Whyte M. K. B., Crossman D. C., Renshaw S. A., Chico T. J. A., Simultaneous intravital imaging of macrophage and neutrophil behaviour during inflammation using a novel transgenic zebrafish. Thromb. Haemost. 105, 811–819 (2011). [DOI] [PubMed] [Google Scholar]
- 30.Prajsnar T. K., Renshaw S. A., Ogryzko N. V., Foster S. J., Serror P., Mesnage S., Zebrafish as a novel vertebrate model to dissect enterococcal pathogenesis. Infect. Immun. 81, 4271–4279 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fox S., Leitch A. E., Duffin R., Haslett C., Rossi A. G., Neutrophil apoptosis: Relevance to the innate immune response and inflammatory disease. J. Innate Immun. 2, 216–227 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tauzin S., Starnes T. W., Becker F. B., Lam P.-y., Huttenlocher A., Redox and Src family kinase signaling control leukocyte wound attraction and neutrophil reverse migration. J. Cell Biol. 207, 589–598 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Claar D., Hartert T. V., Peebles R. S. Jr, The role of prostaglandins in allergic lung inflammation and asthma. Expert Rev. Respir. Med. 9, 55–72 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cha Y. I., Kim S.-H., Sepich D., Buchanan F. G., Solnica-Krezel L., DuBois R. N., Cyclooxygenase-1-derived PGE2 promotes cell motility via the G-protein-coupled EP4 receptor during vertebrate gastrulation. Genes Dev. 20, 77–86 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.North T. E., Goessling W., Walkley C. R., Lengerke C., Kopani K. R., Lord A. M., Weber G. J., Bowman T. V., Jang I.-H., Grosser T., FitzGerald G. A., Daley G. Q., Orkin S. H., Zon L. I., Prostaglandin E2 regulates vertebrate haematopoietic stem cell homeostasis. Nature 447, 1007–1011 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stainier D. Y. R., Raz E., Lawson N. D., Ekker S. C., Burdine R. D., Eisen J. S., Ingham P. W., Schulte-Merker S., Yelon D., Weinstein B. M., Mullins M. C., Wilson S. W., Ramakrishnan L., Amacher S. L., Neuhauss S. C. F., Meng A., Mochizuki N., Panula P., Moens C. B., Guidelines for morpholino use in zebrafish. PLOS Genet. 13, e1007000 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hwang W. Y., Fu Y., Reyon D., Maeder M. L., Tsai S. Q., Sander J. D., Peterson R. T., Yeh J.-R. J., Joung J. K., Efficient genome editing in zebrafish using a CRISPR-Cas system. Nat. Biotechnol. 31, 227–229 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jao L.-E., Wente S. R., Chen W., Efficient multiplex biallelic zebrafish genome editing using a CRISPR nuclease system. Proc. Natl. Acad. Sci. U.S.A. 110, 13904–13909 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fukunaga K., Kohli P., Bonnans C., Fredenburgh L. E., Levy B. D., Cyclooxygenase 2 plays a pivotal role in the resolution of acute lung injury. J. Immunol. 174, 5033–5039 (2005). [DOI] [PubMed] [Google Scholar]
- 40.Osma-Garcia I. C., Punzón C., Fresno M., Díaz-Muñoz M. D., Dose-dependent effects of prostaglandin E2 in macrophage adhesion and migration. Eur. J. Immunol. 46, 677–688 (2016). [DOI] [PubMed] [Google Scholar]
- 41.El Kebir D., Filep J. G., Role of neutrophil apoptosis in the resolution of inflammation. ScientificWorldJournal 10, 1731–1748 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mathias J. R., Perrin B. J., Liu T.-X., Kanki J., Look A. T., Huttenlocher A., Resolution of inflammation by retrograde chemotaxis of neutrophils in transgenic zebrafish. J. Leukoc. Biol. 80, 1281–1288 (2006). [DOI] [PubMed] [Google Scholar]
- 43.Dixon G., Elks P. M., Loynes C. A., Whyte M. K. B., Renshaw S. A., A method for the in vivo measurement of zebrafish tissue neutrophil lifespan. ISRN Hematol. 2012, 915868 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ellett F., Elks P. M., Robertson A. L., Ogryzko N. V., Renshaw S. A., Defining the phenotype of neutrophils following reverse migration in zebrafish. J. Leukoc. Biol. 98, 975–981 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kalinski P., Regulation of immune responses by prostaglandin E2. J. Immunol. 188, 21–28 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ikegami R., Sugimoto Y., Segi E., Katsuyama M., Karahashi H., Amano F., Maruyama T., Yamane H., Tsuchiya S., Ichikawa A., The expression of prostaglandin E receptors EP2 and EP4 and their different regulation by lipopolysaccharide in C3H/HeN peritoneal macrophages. J. Immunol. 166, 4689–4696 (2001). [DOI] [PubMed] [Google Scholar]
- 47.Iwasaki R., Tsuge K., Morimoto K., Inazumi T., Kawahara O., Kawahara A., Tsuchiya S., Sugimoto Y., Molecular and pharmacological characterization of zebrafish ‘contractile’ and ‘inhibitory’ prostanoid receptors. Biochem. Biophys. Res. Commun. 438, 353–358 (2013). [DOI] [PubMed] [Google Scholar]
- 48.Tsuge K., Iwasaki R., Morimoto K., Inazumi T., Kawahara O., Kawahara A., Tsuchiya S., Sugimoto Y., Molecular and pharmacological characterization of zebrafish ‘relaxant’ prostanoid receptors. Biochem. Biophys. Res. Commun. 436, 685–690 (2013). [DOI] [PubMed] [Google Scholar]
- 49.Jin D., Ni T. T., Sun J., Wan H., Amack J. D., Yu G., Fleming J., Chiang C., Li W., Papierniak A., Cheepala S., Conseil G., Cole S. P. C., Zhou B., Drummond I. A., Schuetz J. D., Malicki J., Zhong T. P., Prostaglandin signalling regulates ciliogenesis by modulating intraflagellar transport. Nat. Cell Biol. 16, 841–851 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Serhan C. N., Hamberg M., Samuelsson B., Lipoxins: Novel series of biologically active compounds formed from arachidonic acid in human leukocytes. Proc. Natl. Acad. Sci. U.S.A. 81, 5335–5339 (1984). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rael E. L., Lockey R. F., Interleukin-13 signaling and its role in asthma. World Allergy Organ. J. 4, 54–64 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Adel S., Heydeck D., Kuhn H., Ufer C., The lipoxygenase pathway in zebrafish. Expression and characterization of zebrafish ALOX5 and comparison with its human ortholog. Biochim. Biophys. Acta 1861, 1–11 (2016). [DOI] [PubMed] [Google Scholar]
- 53.Chatzopoulou A., Heijmans J. P. M., Burgerhout E., Oskam N., Spaink H. P., Meijer A. H., Schaaf M. J. M., Glucocorticoid-induced attenuation of the inflammatory response in zebrafish. Endocrinology 157, 2772–2784 (2016). [DOI] [PubMed] [Google Scholar]
- 54.Haas U., Raschperger E., Hamberg M., Samuelsson B., Tryggvason K., Haeggström J. Z., Targeted knock-down of a structurally atypical zebrafish 12S-lipoxygenase leads to severe impairment of embryonic development. Proc. Natl. Acad. Sci. U.S.A. 108, 20479–20484 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tobin D. M., Vary J. C. Jr, Ray J. P., Walsh G. S., Dunstan S. J., Bang N. D., Hagge D. A., Khadge S., King M.-C., Hawn T. R., Moens C. B., Ramakrishnan L., The lta4h locus modulates susceptibility to mycobacterial infection in zebrafish and humans. Cell 140, 717–730 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Berger M., Schwarz K., Thiele H., Reimann I., Huth A., Borngräber S., Kühn H., Thiele B.-J., Simultaneous expression of leukocyte-type 12-lipoxygenase and reticulocyte-type 15-lipoxygenase in rabbits. J. Mol. Biol. 278, 935–948 (1998). [DOI] [PubMed] [Google Scholar]
- 57.Borngräber S., Kuban R.-J., Anton M., Kühn H., Phenylalanine 353 is a primary determinant for the positional specificity of mammalian 15-lipoxygenases. J. Mol. Biol. 264, 1145–1153 (1996). [DOI] [PubMed] [Google Scholar]
- 58.Basil M. C., Levy B. D., Specialized pro-resolving mediators: Endogenous regulators of infection and inflammation. Nat. Rev. Immunol. 16, 51–67 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lawrence T., Gilroy D. W., Chronic inflammation: A failure of resolution? Int. J. Exp. Pathol. 88, 85–94 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Serhan C. N., Novel lipid mediators and resolution mechanisms in acute inflammation: To resolve or not? Am. J. Pathol. 177, 1576–1591 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bratton D. L., Henson P. M., Neutrophil clearance: When the party is over, clean-up begins. Trends Immunol. 32, 350–357 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goren I., Allmann N., Yogev N., Schürmann C., Linke A., Holdener M., Waisman A., Pfeilschifter J., Frank S., A transgenic mouse model of inducible macrophage depletion: Effects of diphtheria toxin-driven lysozyme M-specific cell lineage ablation on wound inflammatory, angiogenic, and contractive processes. Am. J. Pathol. 175, 132–147 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Starnes T. W., Huttenlocher A., Neutrophil reverse migration becomes transparent with zebrafish. Adv. Hematol. 2012, 398640 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nakanishi M., Rosenberg D. W., Multifaceted roles of PGE2 in inflammation and cancer. Semin. Immunopathol. 35, 123–137 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yamane H., Sugimoto Y., Tanaka S., Ichikawa A., Prostaglandin E(2) receptors, EP2 and EP4, differentially modulate TNF-alpha and IL-6 production induced by lipopolysaccharide in mouse peritoneal neutrophils. Biochem. Biophys. Res. Commun. 278, 224–228 (2000). [DOI] [PubMed] [Google Scholar]
- 66.Turcotte C., Zarini S., Jean S., Martin C., Murphy R. C., Marsolais D., Laviolette M., Blanchet M.-R., Flamand N., The endocannabinoid metabolite prostaglandin E2 (PGE2)-glycerol inhibits human neutrophil functions: Involvement of its hydrolysis into PGE2 and EP receptors. J. Immunol. 198, 3255–3263 (2017). [DOI] [PubMed] [Google Scholar]
- 67.Rossaint J., Nadler J. L., Ley K., Zarbock A., Eliminating or blocking 12/15-lipoxygenase reduces neutrophil recruitment in mouse models of acute lung injury. Crit. Care 16, R166 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gewirtz A. T., McCormick B., Neish A. S., Petasis N. A., Gronert K., Serhan C. N., Madara J. L., Pathogen-induced chemokine secretion for model intestinal epithelium is inhibited by lipoxin A4 analogs. J. Clin. Invest. 101, 1860–1869 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Holmes G. R., Dixon G., Anderson S. R., Reyes-Aldasoro C. C., Elks P. M., Billings S. A., Whyte M. K. B., Kadirkamanathan V., Renshaw S. A., Drift-diffusion analysis of neutrophil migration during inflammation resolution in a zebrafish model. Adv. Hematol. 2012, 792163 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Renshaw S. A., Loynes C. A., Trushell D. M. I., Elworthy S., Ingham P. W., Whyte M. K. B., A transgenic zebrafish model of neutrophilic inflammation. Blood 108, 3976–3978 (2006). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material for this article is available at http://advances.sciencemag.org/cgi/content/full/4/9/eaar8320/DC1
Fig. S1. Reverse transcription PCR demonstrates successful exon deletion.
Fig. S2. PGE2 drives resolution of inflammation in the absence of macrophages by 12 hpi and does not alter neutrophil apoptosis.
Fig. S3. Amino acid positions 353 and 418 determine LOX functionality.
Fig. S4. Genotyping method for ptges crispant.


