Abstract
Background: The relative value of universal compared to contingent approaches to communication and behavioral interventions for persons of low health literacy remains unknown. Objective: To examine the effectiveness of interventions that are tailored to individual health literacy level compared to nontailored interventions on health-related outcomes. Design: Systematic review. Data Sources: PubMed and Embase databases. Eligibility Criteria: Studies were eligible if they were in English, used an experimental or observational design, included an intervention that was tailored based on the individual’s level of education, health literacy or health numeracy, and had a comparator group in which the intervention was not tailored to individual characteristics. Review Methods: Databases were searched from inception to January 2016, and the retrieved reference lists hand searched. Abstracts that met PICOS criteria underwent dual review for data extraction to assess study details and study quality. A qualitative synthesis was conducted. Results: Of 2,323 unique citations, 458 underwent full review, and 9 met criteria for the systematic review. Five studies were positive and rated as good quality, 3 were negative with 2 of those of good quality, and 1 had mixed results (fair quality). Positive studies were conducted in the clinical domains of hypertension, diabetes, and depression with interventions including educational materials, disease management sessions, literacy training, and physician notification of limited health literacy among patients. Negative studies were conducted in the clinical domains of heart disease, glaucoma, and nutrition with interventions including medication reconciliation and educational materials. Conclusions: Tailoring communication and behavioral interventions to the individual level of health literacy may be an effective strategy to improve knowledge and indicators of disease control in selected clinical settings.
Keywords: health numeracy, health literacy, tailoring, systematic review
The construct of general health literacy and the domain of health numeracy have been well described and measures of the construct developed and validated.1–14 The strategy of screening patients for low health literacy and using literacy-specific strategies of communication and education in health has been suggested but its efficacy is unknown.15 A strategy of tailoring communication to the individual’s level of health literacy has potential advantages to a universal approach of clear communication. First, a strategy of limiting interventions to those who are determined by valid measures to have low literacy may be less costly than universal use of a resource-intensive intervention. Second, a universal approach that prioritizes the communication of information designed for persons with low literacy may not optimize the communication with persons of high literacy. Third, the increasing sophistication of health information technology increases the feasibility and scalability of a tailored approach to communication. Finally, modern psychometric measures of health literacy offer the potential to decrease respondent burden and usability of literacy assessments.16 The objective of this systematic review is to evaluate the efficacy of communication and behavioral interventions tailored to an individual’s level of health literacy or numeracy on knowledge, psychosocial, or health outcomes, compared to a control group where interventions are not individually tailored. As print and numeric health literacy are considered domains of the general health literacy construct and some measures of health literacy incorporate both domains, our design considers studies that measure and tailor to print, numeric, or a composite of print and numeric literacy as eligible for the systematic review. Furthermore, in order to capture all studies that could inform the research question, we considered studies that measured and tailored to education level to be eligible for inclusion.
Methods
Study Eligibility Criteria
Investigators were guided by PRISMA criteria for systematic reviews.17 In order for studies to be eligible, the authors had to report an intervention that was conducted in the primary language of the study population. Health literacy, health numeracy, or level of education must have been assessed at the individual level prior to the intervention. The study protocol had to include an experimental or cohort design with an intervention tailored to the individual’s level of print literacy, numeracy, or education. Inclusion criteria also required a comparator group (a pre-intervention assessment or a control group in which the intervention was not tailored to the person’s level of health literacy, numeracy, or education), a measurable outcome, and to be published in English.
Information Sources
We used PubMed and Embase from inception to January of 2016. The last search of the data was conducted in July 2016.
Search
We consulted a research librarian to create a search strategy. For PubMed we used the following terms to identify eligible observational or experimental study designs: observational study, crossover procedures, randomly allocated, placebos, clinical trials, multicenter study, controlled clinical trial, single blind method, experimental design. Working with a research librarian and guided by the goals of the systematic review, we identified search terms that reflect communication and behavioral interventions pertinent to the health care context. Terms used in the search included public education, consumer education, decision making, risk communication, teaching, decision support, patient education, notification, patient communication, tailored, or tailoring, or tailor. We then used the following terms to indicate if baseline health literacy, or health numeracy, or education was assessed: statistical literacy, statistics literacy, numeracy, educational attainment, science literacy, scientific literacy, graphic literacy, graph literacy, quantitative literacy, health numeracy, and health literacy. Finally, we used the following terms to identify if a baseline assessment or screen was made: screening, mass screening, measurement, testing, or test. We required that the study have one term in each of these four categories (study design, intervention, literacy, and screening). The search strategy was adapted to accommodate the Embase database search algorithm. We limited the search to articles published in English.
Study Selection
All abstracts that met our criteria were reviewed by one of the investigators. The initial review of abstracts identified all that were reporting original research. Each abstract that met this criterion was reviewed to assess the full PICOS criteria including the following: 1) the population must have a primary language that is the same as the intervention and screening tools used to assess literacy, numeracy, or education at baseline; 2) the intervention must include the use of a screening tool for literacy, numeracy, or education; 3) the intervention must be tailored or targeted to the individuals level of literacy or education; 4) a comparator must either be a pre-post design or if a separate control group is used it must be subject to the intervention but not tailored to literacy, numeracy, or education or be composed of usual care; and 5) a measurable outcome pertaining to health comprehension, health behavior, heath care services, morbidity or mortality, or other must be identified (see Online Appendix 1). The full article was reviewed if it was not clear from the abstract that the article met PICOS criteria. If there was uncertainty regarding the PICOS criteria, a second investigator reviewed the study and a decision was made by consensus. Those articles that met PICOS criteria had a full review by 2 independent reviewers to abstract methods, outcomes, and assess quality (see Online Appendix 2). Discrepancies in the reviews were discussed by the investigative team and consensus achieved regarding study elements and quality ratings.
Data Collection Process
We piloted the PICOS and Data Extraction Forms (see Online Appendixes 1 and 2) on several studies and revised the forms to increase clarity and usability. The revised forms were piloted on several additional studies until they were found to be working well with clear understanding and consensus among the investigative team regarding criteria. One investigator (MS) abstracted data from all studies. The other investigators divided the studies between them with each study abstracted by two investigators. Investigators sent completed forms to one investigator (MS) to review and identify discrepancies, which were then discussed in a conference and consensus reached.
Data Items
Data extracted included identifying data for the study, study design, subjects, literacy screening tool used, intervention group sample size at the start and end of the study, description of the intervention, control group sample size at the start and end of the study, study duration, outcomes including the name of the outcome, the measurement instrument, and a description of the outcome including direction of effect. We identified studies that had statistically significant changes in outcomes, those that had no statistically significant changes in outcomes, and those that had mixed findings. As each study varied in the outcome assessed, we did not combine data across the studies.
Quality criteria were adapted from an approach used by Berkman and others, to reflect elements of potential bias in the studies.18 Elements abstracted for the quality analysis included the method of randomization, allocation concealment, creation of comparable groups, maintenance of comparable groups, health literacy or numeracy measurement, outcome measurement, outcome measurement equally applied, blinding of patients and providers, blinding of outcome assessors, appropriate statistical testing, assessment of impact of loss to follow-up, control of confounding, sample sufficient for power analysis, and an overall study assessment (see Online Appendix 2). The overall study assessment in the quality measure was coded as good (conclusions are very likely to be correct given degree of bias), fair (conclusions are probably correct given degree of bias), or poor (conclusions are not certain given degree of bias).18,19
Results
Study Selection
Our search strategy yielded 2,323 unique citations. We excluded 1,865 citations based on screening of title and abstracts, mainly due to lack of a research design that met inclusion criteria or nonrelevant topics. There were 458 citations that met criteria for full article review. We subsequently excluded 440 articles that did not meet PICOS criteria, most because the intervention was not tailored to the individual level of print literacy, numeracy, or education. This left 18 citations for full review; two investigators independently reviewed each of the 18 full manuscripts. Nine of the 18 citations that underwent full review were subsequently excluded because they did not meet PICOS criteria. An additional citation was excluded because outcomes were measured in only one of two intervention arms leading to a poor quality rating. This yielded 8 citations with 9 studies (1 manuscript reported 2 studies) for final inclusion (Figure 1).
Figure 1.
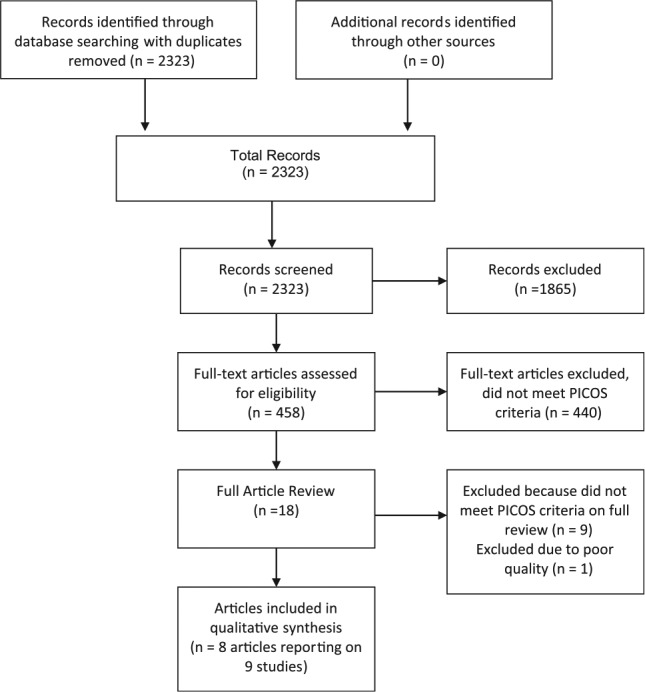
The flow diagram for article retrieval and review in the systematic review.
Study Characteristics and Quality
Of the nine studies identified, all were randomized controlled trials (Table 1). The studies varied with respect to the target population, clinical context, nature of the intervention, and primary outcomes. Eight studies involved patient or community member interventions and one study involved provider notification of patient health literacy level. Of the patient-focused interventions, three were among patients with hypertension (two in the emergency room setting and one in primary care), two among patients with diabetes, and one each of patients with the following diagnoses or presentations: glaucoma, heart disease, and depression. One study focused on nutrition education among community members in England. Outcomes evaluated included knowledge (n = 4), disease control indicators (n = 3), self-confidence (n = 1), medication adherence (n = 2), adverse drug events (n = 1), use of low literacy management strategies (n = 1), and clinician satisfaction and perceived effectiveness (n = 1). Of the nine studies reviewed, seven were rated as good quality and two as fair quality (Table 2). In the following, we summarize each study with additional study details provided in Table 1.
Table 1.
Summary of Included Studies
| Study | Population and Setting | Literacy Measure | Study Design | Intervention | Primary Outcome Domain | Primary Outcome Measure and Result | Quality Measure |
|---|---|---|---|---|---|---|---|
| Giuse and others (2012)20 | Patients with HTN presenting to the
emergency room; USA N = 93 |
S-TOFHLA3 | RCT |
Experiment 1 Control Group: Standard of care discharge instructions Intervention Group: Personalized hypertension materials Inadequate or marginal HL: core materials. Marginal: option of supplemental materials. Adequate HL: core and supplemental. |
Knowledge |
Positive Study 17-Item Hypertension Knowledge Test Greater improvement on posttest scores in intervention group versus control group (P < 0.001) |
Good |
| Giuse and others (2012)20 | Patients with HTN presenting to the
emergency room; USA N = 103 |
Chew Health Literacy Test21 | RCT |
Experiment 2 Control Group: Standard of care discharge instructions Intervention Group: (tailored to HL with additional tailoring to learning style as below) Visual learners: Handouts with pictures/charts Read/write learners: Maximize writing word Aural learners: Audio version Kinesthetic learners: card-sorting |
Knowledge |
Positive Study 17-Item Hypertension Knowledge Test Greater improvement on posttest versus pretest scores in intervention group (P < 0.001) |
Good |
| Rothman and others (2004)22 | Patients DM: 18 years or older with
poorly controlled DM (HbA1c > 8.0%) in general internal
medicine clinics practice; USA N = 217 |
REALM2 | RCT |
Control Group: Initial
management session by clinical pharmacist then continued
with usual care Intervention Group: Initial management session by clinical pharmacist then intensive disease management from a multidisciplinary team including 1) one-to-one educational sessions by pharmacist and DCC, 2) application of evidence-based treatment algorithms, and 3) strategies to address barriers. Pharmacist or DCC aware of patients’ health literacy status, use of techniques to enhance communication among those with low health literacy. |
Disease control indicators |
Positive Study Change in HbA1c Greater improvement in intervention group (−2.1%) versus control group (−1.3%), P = 0.001 Goal HbA1c: Greater in intervention versus control group (1.0, 95% CI = 1.0 to 3.8, P = 0.05) Goal Systolic BP: Greater in intervention versus control group, −7.6 mm, 95% CI = −12.0 to −2.2, P = 0.006 |
Good |
| Weiss and others (2006)23 | Patients with depression and limited HL N = 70 |
REALM2 | RCT |
Control Group: Standard
treatment for depression by PCP Intervention Group: Standard treatment for depression and literacy training at adult education program |
Disease indicator |
Positive Study PHQ-9 scores 1–3 months: Intervention versus control 8 versus 48, P = 0.25 PHQ-9 scores 3–6 months: Intervention versus control 6 versus 9, P = 0.03 PHQ-9 scores 6–12 months (median): Intervention versus control 6 versus 10, P = 0.04 |
Good |
| Bosworth and others (2005)27 | Veterans with HTN N = 588 |
REALM2 | RCT |
Control Group: Usual care Intervention Group: Nurse-administered HTN telephone tailored counseling. Patients identified with low literacy have medication regimen explained verbally at first phone call and then any time regimens altered. |
Self-confidence, knowledge, adherence |
Mixed Results 6-Month self-confidence with treatment: Increase in intervention group (0.33) versus usual care (−0.10), P < 0.007 6-Month HTN knowledge: No difference between groups 6-Month self-reported adherence: No difference between groups |
Fair |
| Seligman and others (2005)24 | Providers in primary care practice
and their patients with DM, 30 years or older, and limited
HL, English or Spanish speaking N = 63 providers N = 182 patients |
S-TOFHLA3 | RCT |
Control Group: No notification
of low HL level of patients Intervention Group): Notification to MDs of patients’ limited health literacy skill, note added to chart immediately prior to study visit |
Physician behavior, satisfaction, and perceived effectiveness |
Positive Study Management Strategies Intervention physicians more likely to use >3 recommended management strategies during the visit (21% v. 8%, OR = 3.2, P = 0.04) Visit-Specific Satisfaction of Clinician Intervention physicians less likely than control physicians to be satisfied with the visit (81% v. 93%, OR = 0.3, P = 0.01) Intervention physicians perceived themselves as somewhat less effective (38% v. 53%, OR = 0.5, P = 0.10) |
Good |
| Additional outcomes: HbA1c fell by 0.21% in intervention group and rose by 0.05% in control group (P = 0.26) | |||||||
| Additional outcomes: HbA1c fell by 0.21% in intervention group and rose by 0.05% in control group (P = 0.26) | |||||||
| Kripalani and others (2013)26 | Patients hospitalized patients with
ACS or heart failure, English or Spanish speaking N = 851 |
S-TOFHLA3 | RCT |
Control Group: Usual care Intervention Group: 4 components: pharmacist-assisted medication reconciliation, tailored inpatient counseling by pharmacist, provision of low literacy adherence aids, and individualized telephone follow-up after discharge. Intervention counseling was sensitive to the patients’ health literacy and cognition. |
Medication errors |
Negative Study Medication errors (mean) within 30 days of discharge similar between intervention (0.87 per patient) and usual care (0.95 per-patient) groups (unadjusted IRR = 0.92, 95% CI = 0.77 to 1.10). ADEs per patient similar in intervention (0.43) and control (0.40) groups |
Good |
| Muir and others (2013)27 | Veterans with medically treated
glaucoma; USA N = 127 |
TOFHLA1 | RCT |
Control Group: Usual care Intervention Group: 2- to 5-minute scripted video scripted at 4th-, 7th-, or 10th-grade level. Inadequate or marginal literacy groups also shown diagrams. Adequate HL received an American Academy of Ophthalmology brochure at the 10th-grade reading level. |
Medication adherence |
Negative Study Days without medication (DWM) in 6 months following enrollment was similar in the intervention (mean, SD: 63, 198) versus control (mean, SD 605, 198), P = 0.708 Similar results with outcome of Medical Possession Ration (MPR) |
Good |
| Fine and others (1994)28 | Nutrition education among women aged
25 to 34 years, lower socioeconomic class in England N = 264 |
7 items: math/education | RCT |
Test Group: Course in basic
nutrition counseling and tailored motivational materials;
low-ability group received training in a simplified format Control Group: Video and booklet with no motivational or simplified materials Baseline Group: No materials provided |
Knowledge |
Negative Study No difference in nutritional knowledge between groups at 1-week follow-up Test and control groups had greater improvement than baseline group |
Fair |
Note: HTN = hypertension; S-TOFHLA = Short Test of Functional Health Literacy in Adults; RCT = randomized controlled trial; HL = health literacy; DM = diabetes mellitus; REALM = Rapid Estimate of Adult Literacy in Medicine; DCC = drug consultative committee; CI = confidence interval; PCP = primary care provider; PHQ-9 = Patient Health Questionnaire–9; OR = odds ratio; ACS = acute coronary syndrome; IRR = incidence rate ratio. Quality criteria adapted from Berkman and others.19 Categories included method of randomization, allocation concealment, creation of comparable groups, maintenance of comparable groups, health literacy valid measurement, outcome measurement, equal measurement across groups, blinding, statistical testing, power, and control of confounding.
Table 2.
Quality Assessment of Included Studies
| Study | Randomization | Concealment | Comparable Groups | Maintenance of Group | Literacy | Outcome Measurement | Equal Across Groups | Blinded Patient/Provider | Blind Assessment | Statistical Testing | Loss of Follow-up | Confound | Power | Summary |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Guise #1, 2012 | Good | Poor | Fair | Good | Good | Good | Good | Poor | Poor | Good | Poor | Good | Fair | Good |
| Guise #2, 2012 | Good | Poor | Fair | Good | Good | Good | Good | Poor | Poor | Good | Poor | Good | Fair | Good |
| Rothman, 2004 | Fair | Fair | Good | Good | Good | Good | Good | Fair | Good | Good | Good | Good | Fair | Good |
| Weiss, 2006 | Good | Fair | Good | Good | Good | Good | Good | Poor | Poor | Good | Poor | Good | Fair | Good |
| Bosworth,2005 | Good | Fair | Good | Good | Good | Good | Good | Poor | Poor | Good | Good | Good | Poor | Fair |
| Seligman, 2005 | Good | Good | Good | Good | Good | Good | Good | Good | Poor | Good | Good | Good | Fair | Good |
| Kripalani, 2013 | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good | Good | Fair | Good |
| Muir, 2013 | Fair | Poor | Fair | Good | Good | Good | Good | Poor | Poor | Good | Good | Good | Fair | Good |
| Fine, 1994 | Poor | Poor | Fair | Fair | Fair | Good | Good | Poor | Poor | Fair | Poor | Good | Poor | Fair |
Note: Quality criteria adapted from Berkman and others. Categories included method of randomization, allocation concealment, creation of comparable groups, maintenance of comparable groups, health literacy or numeracy valid measurement, outcome measurement, equal measurement across groups, blinding, statistical testing, power, and control of confounding. Overall summary assessment presented.
Results of Individual Studies
Positive Studies
Five studies had positive findings. In a study by Giuse and others, 93 patients with hypertension presenting to an emergency room were randomized to an experimental intervention versus usual care.20 Health literacy was measured with the Short Test of Functional Health Literacy in Adults (S-TOFHLA).3 The experimental group was given hypertension education materials tailored to inadequate, marginal, or adequate health literacy levels. Investigators developed core and supplemental versions of patient education materials about hypertension, written at the fifth- and eighth-grade reading level, respectively. The core set (given to those with inadequate or marginal health literacy) included the minimal information needed to answer hypertension knowledge questions and the supplemental set (given to those with adequate health literacy) included elaboration of the concepts presented. Patients with inadequate or marginal health literacy were given core materials. Those with marginal health literacy had the option of receiving supplemental materials. Patients with adequate health literacy were given core and supplemental materials. The control group received standard discharge instructions. The primary outcome was hypertension knowledge. The study reported statistically significantly greater improvement in knowledge scores among the experimental versus control groups.
In a second experiment by Giuse and others,20 103 patients with hypertension presenting to the emergency room were randomized to receive an intervention tailored to both health literacy and learning style compared to usual discharge instructions. Health literacy was assessed with the Brief Health Literacy Test developed by Chew and others and categorized into inadequate, marginal, or adequate health literacy.21 The primary outcome was hypertension knowledge. The study was positive, demonstrating a greater increase in knowledge in the experimental versus control groups. In both Guise studies, the control arm reflected usual care rather than a strategy of universal precautions for low health literacy.
In a study by Rothman and others,22 217 patients with poorly controlled diabetes in a primary care clinic were randomized to a clinical pharmacist information session followed by an intensive disease management intervention from a diabetic care coordinator. The comparator group received only the initial clinical pharmacist information session followed by usual care. Health literacy was assessed with the Rapid Estimate of Adult Literacy in Medicine (REALM).2 Both the pharmacist and team members were aware of the patient’s health literacy status with communication individualized by utilizing techniques to enhance communication among those with low health literacy. These techniques included predominant use of verbal education with simplified explanations of critical behaviors and goals, teach back techniques to assess patient comprehension, and use of picture-based materials. Of note, all literacy levels of the intervention arm received an enhanced intervention compared to usual care. The control arm received the initial clinical pharmacist information session followed by usual care but was not exposed to a strategy of universal precautions for low health literacy. The primary outcome was HbA1c. The study was positive, finding a greater improvement in HbA1c level, and achieving goal HbA1c systolic blood pressure in the experimental versus control groups.
In a study by Weiss and others,23 70 patients with limited health literacy defined by a REALM score of less than or equal to 60 (indicating less than a high school reading level) and a diagnosis of depression were randomized to standard treatment of depression plus health literacy training or standard treatment of depression alone. Health literacy was measured by the REALM.2 The health literacy skill training was provided by a detailed assessment of skills and the development of a learning plan that involves computer-assisted instruction, traditional text-based instruction, and self-paced learning modules. The program also offered employment skill training. The control arm received standard treatment but did not reflect a strategy of universal precautions for low health literacy. The primary outcome was control of depression as measured by the Patient Health Questionnaire–9. The study was positive with the experimental group demonstrating improved control of depression compared to the control group.
In a study by Seligman and others,24 63 primary care providers were randomized to receive notification of the health literacy level of 182 patients with limited health literacy and diabetes or to not receive this notification. The notification including the following statement:
Your patient, Mr./Ms.____ has undergone a screening measure of functional health literacy in (English/Spanish) and was found to have (inadequate/marginal) health literacy. Patients with low levels of functional health literacy may be more likely to have difficulties understanding written health materials, following prescribed treatment regimens, or processing oral communication.
During the study period, some of the physicians had attended a local lecture on limited health literacy but there was no systematic training to improve physicians’ management of patients with limited health literacy. Health literacy was measured with the S-TOFHLA.1 The primary outcome was the use of management strategies designed for low-literacy patients including involving patient family members or friends, referring to a diabetes educator, referring to a nutritionist, using pictures or diagrams, reviewing understanding of medications, or spending time educating about diabetes. These behaviors were used as a primary outcome because of evidence that physician visit–based behaviors are the most proximate intermediate endpoint through which screening for health literacy might affect patient outcomes.25,26 The control arm received usual care and was not exposed to a strategy of universal precautions for low health literacy. Secondary physician outcomes included visit-specific satisfaction and perceived effectiveness. The providers in the experimental group were found more likely to use three or more of the six recommended management strategies during the patient visit than those in the control group. Secondary outcomes indicated that providers in the intervention group were less satisfied with the visit and perceived the visit to be less effective than providers in the control group (Table 1).
Mixed Results (Positive and Negative Primary Outcomes) Study
In a study by Bosworth and others,27 588 veterans with hypertension were enrolled in a randomized controlled trial. The study had mixed results with positive findings for the outcome of self-confidence but negative findings for the outcomes of hypertension knowledge or self-reported medication adherence. Baseline health literacy was measured with the REALM.2 The experimental group received a nurse-administered hypertension counseling session administered by telephone. The patients identified as having low health literacy had their hypertension medication regimen explained verbally by the nurse at the first phone call and then anytime the regimen was altered. In addition, the patient’s regimen is explained to a family member/friend, the nurse reinforced the medication instructions, and provided information on the purpose of medications and the potential side effects. The control group received usual care and did not use a strategy of universal precautions to address low health literacy. Outcomes included knowledge, self-confidence, and self-reported adherence to medications. This study had mixed results. At the 6-month assessment, the experimental group had a greater increase in self-confidence with the treatment group that the control group. However, there was no difference between groups in hypertension knowledge or self-reported medication adherence.
Negative Studies
Three studies had negative results. In a study by Kripalani and others,28 851 patients who were hospitalized with acute coronary syndrome or heart failure were randomized to receive pharmacist-assisted medication reconciliation, tailored inpatient counseling by a pharmacist, low literacy adherence aids, and individualized telephone follow-up after discharge. Intervention counseling was described as sensitive to the patient’s health literacy level. The control group received usual care and did not use a strategy of universal precautions to address low health literacy. The primary outcome was clinically important medication errors within 30 days. Health literacy was measured with the S-TOFHLA.3 There was no difference in clinically significant medication errors within 30 days of discharge between groups
In a study by Muir and others,29 127 veterans with glaucoma treated in ophthalmology clinic were randomized to receive videos scripted at the 4th-, 7th-, or 10th-grade level. Subjects who scored less than 60 on the TOFHLA (inadequate literacy) saw a video scripted at the 4th-grade reading level, subjects who scored 60 to 74 (marginal health literacy) at a 7th-grade level, and those who scored >74 (adequate health literacy) at a 10th-grade level and received an American Academy of Ophthalmology educational brochure at the 10th-grade level. The intervention group also received training in how to use the eye drops and a phone call once a month to ask if the patient had questions about the medication. The control group received standard care and did not include a strategy of universal precautions to address low health literacy. Health literacy was measured with the TOFHLA.1 The primary outcome was medication adherence as measured by days without medication. There was no difference between groups in days without medication at 6 months.
Finally, in a study by Fine and others,30 264 women aged 25 to 34 and of lower socioeconomic class in England were randomized to 3 groups: 1) video and booklet about nutrition, motivational material, and training materials in a simplified format if the patient was of low education and mathematical ability; 2) video and booklet only; and 3) no intervention. Education and math ability was measured at baseline. The primary outcome was nutrition knowledge. There was no difference found between groups in gains in nutrition knowledge before and after the intervention.
Discussion
In summary, of the nine studies identified, five were positive and rated as good quality, three were negative with two of those of good quality, and one had mixed results. A large number of studies have evaluated interventions that are designed for persons of low health literacy.19 However, our review highlights that relatively few have both measured individual-level literacy at baseline and had a study design that tailored the intervention to the individuals’ level of health literacy. Furthermore, our review found no studies that compared an intervention arm tailored to individual level health literacy to universal precautions for persons of low literacy. Despite the limited studies identified, our analysis provides some support for a strategy of testing for and tailoring interventions to the level of health literacy. Furthermore, our findings provide insight regarding the efficacy of this approach across clinical contexts, target populations, and outcomes of interest.
Our review indicates that a strategy of tailoring communication to an individual’s level of health literacy may be effective in primary care settings when outcomes of disease knowledge and self-management of chronic disease are of interest. Study designs that focused on improving patient knowledge and disease management skills were positive or demonstrated mixed results. In the two experiments conducted by Giuse and others,20 hypertension knowledge scores improved more in the group receiving educational materials tailored to health literacy level than the control group receiving standard discharge instructions. Previous research has found that discharge instructions are often written at a higher literacy level than the literacy skills of patients receiving the instructions.31,32 Of interest, 14% and 20% of the study population had inadequate or marginal health literacy in experiments 1 and 2, respectively. In the study conducted by Rothman and others,22 the addition of educational sessions that were tailored to level of health literacy to a single clinical pharmacist consultation led to a significant improvement in HbA1c among diabetic patients. In this study, 38% of the study population had low literacy. The study by Bosworth and others27 reports an increase in self-efficacy regarding hypertension management among the group that received nurse-administered counseling tailored to health literacy and other patient factors compared to a control group, although the study failed to demonstrate a difference in hypertension knowledge and adherence. The proportion of low health literacy in the Bosworth study population was not reported although 17% had a high school or less level of education. As a group, these studies suggest that tailoring the content of education and counseling interventions to the individual health literacy level of the patient may improve knowledge about chronic disease or indicators of chronic disease control.
The study by Weiss takes a very different approach than the other studies evaluated. Rather than an intervention designed to provide communication or education tailored to the patient’s level of skill, this study had an intervention designed to improve patient literacy. This strategy was found to have a positive impact on disease management of depression. Although health literacy is often analyzed as a trait, the field of adult learning suggests that both print and numeracy skills can be improved with education and training.33 This study suggests that a strategy of testing for health literacy in the clinical setting and referral to adult literacy programs may have a positive impact on health outcomes.
Studies in our review that focused on medication adherence or adverse effects of medications were negative.28,29 These include the large study (n = 851) by Kripalani and others28 that evaluated a literacy-sensitive pharmacy intervention among patients hospitalized with acute coronary syndrome or heart failure. The primary outcomes were clinically important medication errors including nonadherence, assessed by interview and self-report. One factor that may limit the generalizability of this finding is the low percentage (10%) of persons with inadequate health literacy in the study sample. This was lower than the estimated prevalence of low health literacy of 26% (95% confidence interval = 22% to 29%) in a systematic review.34 A subset analysis indicates that participants with inadequate health literacy were more likely to incur a benefit from the intervention but the finding did not reach statistical significance and the study was not powered to measure this heterogeneity effect. A second negative study conducted by Muir and others29 evaluated a literacy tailored educational intervention about glaucoma medication with a primary outcome of medication adherence assessed by review of pharmacy records and determination of days without medication. This study was negative, although 36% of participants had inadequate or marginal health literacy. This study also reports indications of heterogeneity with greater response to the intervention in the low-literacy subgroups but differences did not reach statistical significance. In summary, these studies indicate that medication adherence may less responsive to literacy-tailored educational interventions compared to knowledge and other behavioral outcomes.
One study in our systematic review targeted the physician.24 The intervention involved clinician notification of low literacy in a patient.24 The Seligman study indicates that notifying of patients with low health literacy increases their use of management strategies appropriate for low-literacy persons.24 However, the study also identified unintended adverse outcomes including decreased satisfaction and perceived effectiveness of the visit.
This systematic review has some limitations. First, publication bias may lead to an overrepresentation of positive studies in the literature. Second, our study design sought to include interventions targeted to either print or numeric health literacy. These domains may differ in response to tailored approaches to communication. However, they each comprise domains of the general health literacy construct. Furthermore, several validated measures of health literacy are composite measures of print and numeric domains.35 Inclusion of both print and numeric literacy in this systematic review was consistent with the objectives of this study. Third, we found no studies where the comparator arm used a universal approach to communication and behavioral interventions for low-literacy persons. The optimal study design to test a universal versus contingent strategy of providing health literacy–appropriate interventions would include arms with identical strategies with the addition of a tailored intervention for the experimental arm. Our design required a contingent strategy in the experimental arm but allowed for usual care in the control arm. Despite these limitations, this is the first systematic review to provide evidence supporting a contingent approach to low health literacy interventions. Additional studies including direct comparisons of contingent versus universal approaches are needed to determine optimal strategies for communication and behavioral interventions among persons with low health literacy.
In conclusion, we find a modest degree of evidence that tailoring health communication strategies to patient level of health literacy can improve knowledge, proximal indicators of disease control (such as A1c level in patients with diabetes), and disease control (depression). These outcomes may lead to a decrease in morbidity and mortality associated with chronic disease. The efficacy of a contingent approach to low literacy may vary with clinical context (primary care v. hospitalization), target of the intervention (patient v. physician), and outcomes evaluated (cognitive, behavioral, disease indicators, or adverse effects). This review highlights the need for evaluating not only proximal effects of communication but more distal effects on health outcomes. Our findings also identify the lack of head to head studies that evaluate a contingent versus universal strategy to address communication and behavioral interventions for persons of low health literacy. Given the potential to use health information technology to tailor interventions, selected use of literacy contingent strategies is one option to consider in the design of effective health care communication strategies.
Supplementary Material
Footnotes
Financial support for this study was provided in part by a grant from the American Cancer Society. The funding agreement ensured the authors’ independence in designing the study, interpreting the data, writing, and publishing the report.
The online appendixes for this article are available on the Medical Decision Making Policy & Practice Web site at http://journals.sagepub.com/doi/suppl/10.1177/2381468317714474.
References
- 1. Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10:537–41. [DOI] [PubMed] [Google Scholar]
- 2. Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391–5. [PubMed] [Google Scholar]
- 3. Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. [DOI] [PubMed] [Google Scholar]
- 4. Apter AJ, Cheng J, Small D, et al. Asthma numeracy skill and health literacy. J Asthma. 2006;43:705–10. [DOI] [PubMed] [Google Scholar]
- 5. Nurss JR, Parker R, Williams MV, Baker DW. TOFHLA: Test of Functional Health Literacy in Adults. Hartford (MI): Peppercorn Books and Press; 1995. [DOI] [PubMed] [Google Scholar]
- 6. Johnson TV, Abbasi A, Kleris RS, et al. Assessment of single-item literacy questions, age, and education level in the prediction of low health numeracy. JAAPA. 2013;26:50–4. [DOI] [PubMed] [Google Scholar]
- 7. Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–72. [DOI] [PubMed] [Google Scholar]
- 8. Schapira MM, Walker CM, Cappaert KJ, et al. The numeracy understanding in medicine instrument: a measure of health numeracy developed using item response theory. Med Decis Making. 2012;32:851–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schapira MM, Fletcher KE, Gilligan MA, et al. A framework for health numeracy: how patients use quantitative skills in health care. J Health Commun. 2008;13:501–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Osborn CY, Wallston KA, Shpigel A, Cavanaugh K, Kripalani S, Rothman RL. Development and validation of the General Health Numeracy Test (GHNT). Patient Educ Couns. 2013;91:350–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Med Decis Making. 2001;21:37–44. [DOI] [PubMed] [Google Scholar]
- 12. Jacobs EA, Walker CM, Miller T, et al. Development and validation of the Spanish Numeracy Understanding in Medicine Instrument. J Gen Intern Med. 2016;31:1345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. Am J Prev Med. 2005;29:375–6. [DOI] [PubMed] [Google Scholar]
- 14. Apter AJ, Paasche-Orlow MK, Remillard JT, et al. Numeracy and communication with patients: they are counting on us. J Gen Intern Med. 2008;23:2117–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hamm RM, Bard DE, Hsieh E, Stein HF. Contingent or universal approaches to patient deficiencies in health numeracy. Med Decis Making. 2007;27:635–7. [DOI] [PubMed] [Google Scholar]
- 16. Nguyen TH, Paasche-Orlow MK, Kim MT, Han HR, Chan KS. Modern measurement approaches to health literacy scale development and refinement: overview, current uses, and next steps. J Health Commun. 2015;20(suppl 2):112–5. [DOI] [PubMed] [Google Scholar]
- 17. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–41. [DOI] [PubMed] [Google Scholar]
- 18. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. [DOI] [PubMed] [Google Scholar]
- 19. Berkman ND, Sheridon SL, Donahue KE, et al. Health Literacy Interventions and Outcomes: An Updated Systematic Review (Report No. 11-E006). Rockville (MD): Agency for Healthcare Research and Quality; 2011. [PMC free article] [PubMed] [Google Scholar]
- 20. Giuse NB, Koonce TY, Storrow AB, Kusnoor SV, Ye F. Using health literacy and learning style preferences to optimize the delivery of health information. J Health Commun. 2012;17(suppl 3):122–40. [DOI] [PubMed] [Google Scholar]
- 21. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36:588–94. [PubMed] [Google Scholar]
- 22. Rothman RL, DeWalt DA, Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;292:1711–6. [DOI] [PubMed] [Google Scholar]
- 23. Weiss BD, Francis L, Senf JH, Heist K, Hargraves R. Literacy education as treatment for depression in patients with limited literacy and depression: a randomized controlled trial. J Gen Intern Med. 2006;21:823–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Seligman HK, Wang FF, Palacios JL, et al. Physician notification of their diabetes patients’ limited health literacy. A randomized, controlled trial. J Gen Intern Med. 2005;20:1001–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004;52:315–23. [DOI] [PubMed] [Google Scholar]
- 26. Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163:83–90. [DOI] [PubMed] [Google Scholar]
- 27. Bosworth HB, Olsen MK, Gentry P, et al. Nurse administered telephone intervention for blood pressure control: a patient-tailored multifactorial intervention. Patient Educ Couns. 2005;57:5–14. [DOI] [PubMed] [Google Scholar]
- 28. Kripalani S, Roumie CL, Dalal AK, et al. Effect of a pharmacist intervention on clinically important medication errors after hospital discharge: a randomized trial. Ann Intern Med. 2012;157:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Muir KW, Ventura A, Stinnett SS, Enfiedjian A, Allingham RR, Lee PP. The influence of health literacy level on an educational intervention to improve glaucoma medication adherence. Patient Educ Couns. 2012;87:160–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Fine GA, Conning DM, Firmin C, et al. Nutrition education of young women. Br J Nutr. 1994;71:789–98. [DOI] [PubMed] [Google Scholar]
- 31. Spandorfer JM, Karras DJ, Hughes LA, Caputo C. Comprehension of discharge instructions by patients in an urban emergency department. Ann Emerg Med. 1995;25:71–4. [DOI] [PubMed] [Google Scholar]
- 32. Williams DM, Counselman FL, Caggiano CD. Emergency department discharge instructions and patient literacy: a problem of disparity. Am J Emerg Med. 1996;14:19–22. [DOI] [PubMed] [Google Scholar]
- 33. Beder H. Adult Literacy: Issues for Policy and Practice. Malabar (FL): Krieger; 1991. [Google Scholar]
- 34. Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20:175–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21:878–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


