Abstract
Lumbar stenosis is a common radiographic finding that sometimes can be symptomatic. It usually results from a degenerative process of hypertrophic facets, ligamentum flavum hypertrophy, and disc involvement. A prominence of fat in the epidural space, epidural lipomatosis, can also be a contributing factor. This case report presents a 55-year-old man with radiographic improvement of epidural lipomatosis and stenosis from dietary weight loss. Given the rising obesity epidemic, practitioners should be cognizant of epidural lipomatosis and consider weight loss as a possible treatment option.
Keywords: lipomatosis, back pain, complementary therapies, spinal stenosis
‘Lumbar spinal stenosis is a common radiographic finding that can become symptomatic in some individuals.”’
Lumbar spinal stenosis is a common radiographic finding that can become symptomatic in some individuals. This commonly originates as a degenerative process with contribution from hypertrophic facets, thickened ligamentum flavum, and disc involvement.1 A prominence of the epidural fat, epidural lipomatosis, can also be a contributing cause to spinal canal stenosis. In some individuals, this can be the predominant cause of stenosis.2 We present a patient with lumbar stenosis related to epidural lipomatosis who lost weight and had radiographic improvement of his stenosis.
Presentation
A 55-year-old obese man with a past medical history of chronic low back pain, peripheral neuropathy, hypertension, hyperlipidemia, gastroesophageal reflux disease, alcohol abuse, and methicillin-resistant Staphylococcus aureus empyema with decortication who presented to an academic spine center because of lumbar complaints. He had a long-standing history of axial back pain that had notably worsened over the prior year to include complaints of back, gluteal, and thigh pain. Symptoms began to worsen gradually without an inciting incident. Although he also had an electromyography proven peripheral neuropathy with symptoms in a stocking glove distribution, his spinal complaints were clearly different. His gluteal and thigh pain worsened with standing and walking and was alleviated with sitting. To help with ambulation he used a single point cane. Pain became severe and limited his ambulation. Prior to being seen at the academic spine center, he had been through physical therapy, nonsteroidal anti-inflammatories, muscle relaxants, and opiates.
On physical examination, he had diminished vibration and light touch that was symmetrical in both feet in a stocking glove distribution consistent with his peripheral neuropathy. Additionally, he had 0/5 strength of bilateral extensory hallucis longus but otherwise strength 5/5 more proximally. Muscle stretch reflexes were 2+ and symmetrical at bilateral patellar but absent at the Achilles tendons bilaterally.
A magnetic resonance imaging (MRI) was performed on July 10, 2013, which showed epidural lipomatosis with congenital canal narrowing. This combination lead to multilevel severe spinal canal stenosis notably from L1-4. There was a component of congenitally short pedicles but clearly significant dorsal epidural fat was the major contributor to the stenosis. After discussion with Neurosurgery about treatment options he was referred to Psychiatry for trial of conservative therapy to improve his pain complaints. Given he had no history of endocrinopathies or steroid exposure to explain findings of lipomatosis on imaging, facet steroid injections for his back pain and later epidural steroid injections for radicular pain were trialed. Injections provided great relief but only for 2-day duration each and were not continued. Through dietary measures he was able to lose 39 pounds (17.7 kg), going from 221 pounds (body mass index [BMI] 31.7 kg/m2) to 182 pounds (BMI 26.1 kg/m2) over a 21-month period. However, because of continued pain complaints, he had an updated MRI of the lumbar spine in April 2015, which revealed improvement in the degree of stenosis because of less epidural lipomatosis. This improvement is displayed in Figures 1 and 2. The official radiology impression stated the following: “Significantly decreased epidural lipomatosis with improved central stenosis at multiple levels. . . . There is persistent, severe central stenosis at L3-L4 due to disc bulge.”
Figure 1.
Before and after axial T1 images on magnetic resonance imaging showing less epidural lipomatosis after a 39-pound (17.7 kg) weight loss from July 2013 to April 2015.
Figure 2.
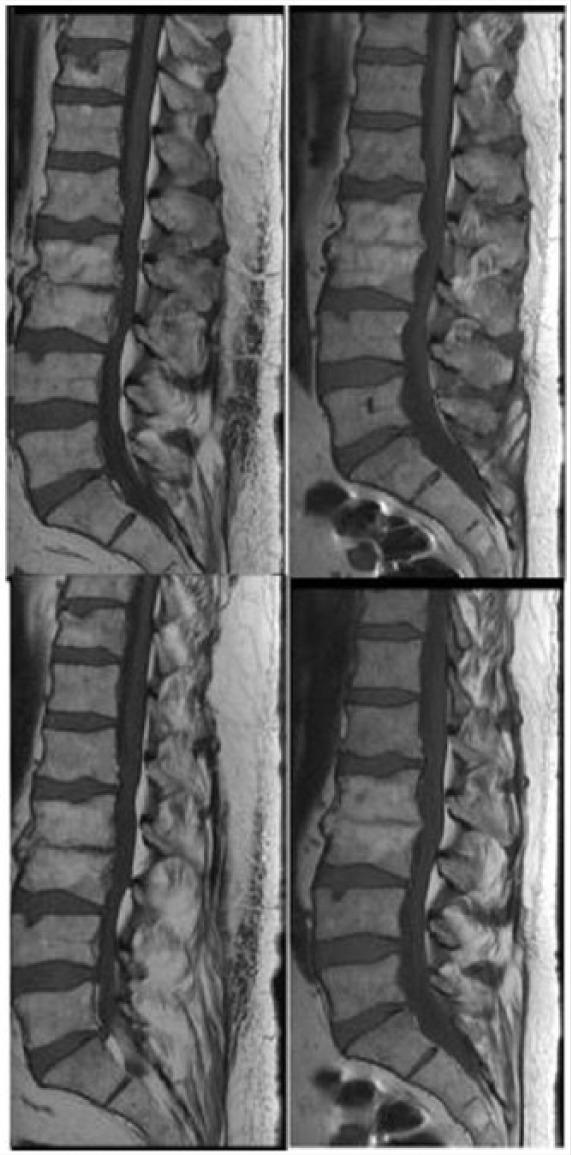
Sagittal T1 images (closest images to midline) comparing from July 2013 (left) to April 25 (right) showing less epidural lipomatosis.
Despite the radiographic improvement after weight loss, he continued to have neurogenic claudication and ultimately had a L1-5 laminectomy on April 14, 2015. Postoperatively he did well with resolution of his lower limb pain and neurogenic claudication. Although he eventually underwent surgery, this does give support to the fact that epidural lipomatosis may improve with weight loss.
Discussion
Degenerative changes are the most common etiology for spinal stenosis typically with facet hypertrophy, ligamentum flavum thickening and disc involvement contributing to a narrowed spinal canal.1 Epidural lipomatosis can be a contributing factor to stenosis and occasionally the predominant cause of the stenosis. The exact frequency of epidural lipomatosis is not known.2
Epidural lipomatosis has been divided into idiopathic and secondary etiologies.3 Secondary etiologies are typically due to increased steroid exposure, whether exogenous or endogenous. Less commonly there have been reports of epidural lipomatosis secondary to pituitary tumors4 and HIV patients using protease inhibitors with a lipid dystrophy.5,6 In both idiopathic and secondary cases, males are affected more commonly (80%-90%) and obesity is very common in both groups (70%). This brings into question whether reported idiopathic cases are truly idiopathic or simply weight related. Idiopathic cases more commonly are located in the lumbar region (65%) and secondary cases are more common in the thoracic region (73%).
Epidural lipomatosis can be an asymptomatic radiographic finding on MRIs. Typically, diagnosis of epidural lipomatosis with MRI requires the thickness be greater than 7 mm at the level of compression.7 A system for grading epidural lipomatosis was reported by Borré et al8 in 2004 and reevaluated by Pinkhardt et al9 in 2007. Borré et al8 graded epidural lipomatosis as 0 (no lipomatosis), I (mild), II (moderate), and III (severe). Using anteroposterior measurements on the axial plane, grade III was defined as epidural fat occupying ≥75% of the spinal canal diameter or a ratio of the dural sac diameter to epidural fat of ≤0.33. Borré et al8 found that all patients with grade III (severe) epidural lipomatosis were symptomatic.
There have been other case reports showing that weight loss improves spinal stenosis related to epidural lipomatosis.10-12 Thus, this case report adds to the growing evidence that weight loss should be the first line of treatment in patients with epidural lipomatosis where excess weight is felt to be an underlying issue. Of course, this does not negate the need to evaluate for an underlying endocrinopathy or if they are on steroids wean them if possible. For patients who fail conservative measures or have progressive neurologic deficits, surgical decompression with a laminectomy is an effective option.3
In summary, spinal stenosis is caused by a number of factors. Commonly, it is related to degenerative changes, but epidural lipomatosis can be a contributing factor and occasionally the primary cause. With the growing obesity epidemic in the United States, we should be cognizant of epidural lipomatosis. Lifestyle choices could potentially play a big role in the prevention and treatment of many cases of epidural lipomatosis.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976). 1978;3:319-328. [DOI] [PubMed] [Google Scholar]
- 2. Fassett DR, Schmidt MH. Spinal epidural lipomatosis: a review of its causes and recommendations for treatment. Neurosurg Focus. 2004;16:E11. [PubMed] [Google Scholar]
- 3. Al-Khawaja D, Seex K, Eslick GD. Spinal epidural lipomatosis—a brief review. J Clin Neurosci. 2008;15:1323-1326. [DOI] [PubMed] [Google Scholar]
- 4. Fujisawa H, Hasegawa M, Tachibana O, Yamashita J. Spinal epidural lipomatosis associated with pituitary macroprolactinoma. Acta Neurochir (Wien). 2002;144:213-214. [DOI] [PubMed] [Google Scholar]
- 5. Cersósimo MG, Lasala B, Folgar S, Micheli F. Epidural lipomatosis secondary to indinavir in an HIV-positive patient. Clin Neuropharmacol. 2002;25:51-54. [DOI] [PubMed] [Google Scholar]
- 6. Vince GH, Brucker C, Langmann P, Herbold C, Solymosi L, Roosen K. Epidural spinal lipomatosis with acute onset of paraplegia in an HIV-positive patient treated with corticosteroids and protease inhibitor: case report. Spine (Phila Pa 1976). 2005;30:E524-E527. [DOI] [PubMed] [Google Scholar]
- 7. Kumar K, Nath RK, Nair CP, Tchang SP. Symptomatic epidural lipomatosis secondary to obesity. Case report. J Neurosurg. 1996;85:348-350. [DOI] [PubMed] [Google Scholar]
- 8. Borré DG, Borré GE, Aude F, Palmieri GN. Lumbosacral epidural lipomatosis: MRI grading. Eur Radiol. 2003;13:1709-1721. [DOI] [PubMed] [Google Scholar]
- 9. Pinkhardt EH, Sperfeld AD, Bretschneider V, Unrath A, Ludolph AC, Kassubek J. Is spinal epidural lipomatosis an MRI-based diagnosis with clinical implications? Acta Neurol Scand. 2008;117:409-414. [DOI] [PubMed] [Google Scholar]
- 10. Beges C, Rousselin B, Chevrot A, et al. Epidural lipomatosis. Interest of magnetic resonance imaging in a weight-reduction treated case. Spine (Phila Pa 1976). 1994;19:251-254. [PubMed] [Google Scholar]
- 11. Borstlap AC, van Rooij WJ, Sluzewski M, Leyten AC, Beute G. Reversibility of lumbar epidural lipomatosis in obese patients after weight-reduction diet. Neuroradiology. 1995;37:670-673. [DOI] [PubMed] [Google Scholar]
- 12. Pouchot J, Si-Hassen C, Damade R, Bayeux MC, Mathieu A, Vinceneux P. Cauda equina compression by epidural lipomatosis in obesity. Effectiveness of weight reduction. J Rheumatol. 1995;22:1771-1775. [PubMed] [Google Scholar]



