Abstract
Primary care physicians experience high rates of burnout, which results in diminished quality of life, poorer quality of care, and workforce attrition. In this randomized controlled trial, our primary aim was to examine the impact of a brief mindfulness-based intervention (MBI) on burnout, stress, mindfulness, compassion, and resilience among physicians. A total of 33 physicians completed the baseline assessment and were randomized to the Mindful Medicine Curriculum (MMC; n = 17) or waitlist control group (n = 16). Participants completed self-report measures at baseline, post-MBI, and 3-month follow-up. We also analyzed satisfaction with doctor communication (DCC) and overall doctor rating (ODR) data from patients of the physicians in our sample. Participants in the MMC group reported significant improvements in stress (P < .001), mindfulness (P = .05), emotional exhaustion (P = .004), and depersonalization (P = .01) whereas in the control group, there were no improvements on these outcomes. Although the MMC had no impact on patient-reported DCC or ODR, among the entire sample at baseline, DCC and ODR were significantly correlated with several physician outcomes, including resilience and personal achievement. Overall, these findings suggest that a brief MBI can have a positive impact on physician well-being and potentially enhance patient care.
Keywords: mindfulness, burnout, perceived stress, resilience
Physicians experience the highest rates of burnout among health care providers, with specialties on the frontline, such as family medicine and internal medicine, being at the greatest risk.1 Nearly 60% of physicians have reported symptoms of burnout, including emotional exhaustion, depersonalization of patients, and lost sense of personal accomplishment.2,3 Ultimately, this leads to diminished quality of care, increased medical errors, poorer adherence to treatment plans, and decreased satisfaction with care among patients.4,5 Furthermore, burnout is linked to lower productivity, early retirement, and higher rates of turnover, which have profound financial impacts;6,7 replacement costs are approximately $250 000 per physician.8 Therefore, there is a clear need for evidence-based methods to reduce burnout and mitigate its negative impact among physicians. One such approach may be mindfulness.
A form of mental training that enhances one’s ability to nonjudgmentally attend to the present moment, mindfulness is often translated as “to see with discernment.”9 Two salient components of mindfulness are (a) an intentional regulation of attention and awareness of the present moment and (b) a nonjudgmental and curious willingness to experience the content (thoughts, feelings, sensations) of the present moment.10 Ultimately, this practice redirects us away from habitual reactions to situations, and teaches new ways to respond that are more creative and less depleting. Mindfulness-based interventions (MBIs) have demonstrated effectiveness in reducing burnout, depression, anxiety, and perceived stress,11-13 and increasing well-being, resilience,14,15 and compassion for others16 among clinical and nonclinical populations. Additionally, in a meta-analysis, Shapiro et al17 found that MBIs are an effective and affordable way to reduce burnout and enhance quality of life among health care professionals, and in a randomized controlled trial (RCT) among primary care providers, an 8-week Mindfulness-Based Stress Reduction (MBSR) course enhanced mood, increased mindfulness and empathy, and decreased burnout.18
Although MBIs have been linked to a number of positive outcomes among health care professionals, a commonly reported issue is high attrition rates due to the intensive time requirement. To address this barrier, Fortney et al19 developed a substantially abbreviated weekend immersion MBI with 2 brief follow-up sessions for primary care providers. In an uncontrolled pilot study, 30 primary care providers reported reduced burnout, depression, anxiety, and perceived stress after attending the weekend program, and the effects were maintained over 9 months postintervention. These results suggest that time-limited initial training may be sufficient in teaching a mindfulness practice to physicians.
One limitation noted in the study by Fortney et al19 was the lack of a control group. Using an RCT design, we assessed the efficacy of the brief MBI developed by Fortney et al19 among primary care providers. Our primary aim was to explore whether a brief MBI, compared with a waitlist control group, would reduce burnout and stress and increase mindfulness, compassion, and resilience from baseline to 3-month follow-up in a group of physicians. Our secondary aim was to evaluate patient-reported satisfaction with their primary care physician—both its relationship to physician self-reported characteristics (burnout, stress, mindfulness, compassion, and resilience) at baseline, and how a brief MBI might affect these characteristics at 3-month follow-up.
Method
Participants
Participants were primary care physicians recruited from the family medicine and internal medicine departments at Providence Health and Services in Portland, Oregon. Recruitment emails were sent to all 204 physicians in these 2 departments. Inclusion criteria were (a) employed as a primary care physician by Providence Medical Group (PMG), (b) working at least 30% time in direct patient care, (c) aged between 25 and 75 years, (d) willing to be randomized to the intervention or waitlist control group, and (e) no prior participation in the same MBI offered at PMG. The Providence Health and Services Institutional Review Board approved the study and all participants provided informed consent.
Procedures
Recruitment and data collection occurred between December 2014 and May 2015. Potential participants were recruited via email for 3 weeks prior to the first MBI group (January 2015). Participants responded to the recruitment email by directing their browser to the study website, which was housed on Qualtrics, a secure web-based survey system. At baseline participants created unique identification codes based on responses to 2 innocuous questions to allow for tracking of responses over time. After completing the baseline measures, participants were randomized 1:1 into the intervention or a waitlist control.
Intervention
The intervention used in this study, Mindful Medicine Curriculum (MMC), is similar to the protocol used by Fortney et al19 MMC is a modified version of MBSR, with added elements of compassion skills training, brief mindfulness techniques designed to be used at work, and “SLO conversation” exercises where participants practice applying mindfulness to the core clinical skills of speaking, listening, and observing (SLO). Key to the MMC is an introduction to mindfulness that is relevant to the professional contexts in which physicians work, hence emphasizing the physicians’ ability to incorporate mindfulness and compassion into interpersonal relationships. Instructors present the MMC using secular, accessible language, and they have extensive experience in secular MBIs and familiarity with the culture of physicians. MMC is a 13-hour weekend training program plus 2-hour follow-up sessions scheduled at 2 and 4 weeks after the weekend.
Measures
Physician Self-Report
The Mindful Attention Awareness Scale20 (MAAS) is a 15-item measure of mindfulness in which respondents indicate, on a 6-point Likert-type scale, their level of awareness and attention to present events and experiences20; higher scores indicate greater mindfulness. The MAAS has good internal consistency (α = .87; present sample at baseline = .92) and test-retest reliability (r = .81).
The Brief Resilience Scale21 (BRS) is a 6-item measure designed to assess the ability to bounce back or recover from stress. Items are rated on a 5-point Likert-type scale; higher scores indicate greater resilience. The BRS has good internal consistency (α = .83; present sample at baseline = .92), a single factor structure, and demonstrated expected correlations with a variety of constructs, including perceived stress.
The Perceived Stress Scale–1022 (PSS-10) was used to assess the degree to which situations in life are perceived as stressful, and how unpredictable, uncontrollable, and overloaded participants find their lives. Items are rated on a 5-point Likert-type scale; higher scores indicate greater stress. The PSS-10 has good internal consistency (α = .88; present sample at baseline = .84) and has demonstrated expected correlations with a variety of constructs.
The Santa Clara Brief Compassion Scale23 (SCBCS) is a 5-item scale designed to measure compassion. The SCBCS is a brief version of the Compassionate Love Scale24, in which compassionate love is defined as an attitude toward others that is “focused on caring, concern, tenderness; and an orientation toward supporting, helping, and understanding others” (p. 630). Items are rated on a 7-point Likert-type scale; higher scores indicate greater compassion. The SCBCS has good internal consistency (α = .90; present sample at baseline = .88) and has demonstrated expected correlations with a variety of constructs.
The Maslach Burnout Inventory3 (MASL) is a 22-item scale designed to measure burnout and job satisfaction. The MASL consists of 3 subscales: emotional exhaustion, depersonalization, and personal accomplishment. Items are rated on a 7-point Likert-type scale; higher scores on each subscale indicate more of the construct. Each of the 3 subscales has adequate internal consistency: emotional exhaustion (α = .90; present sample at baseline = .88), depersonalization (α = .76; present sample at baseline = .78), and personal achievement (α = .76; present sample at baseline = .77).
Meditation Practice Questionnaire (MPQ): We developed 4 items to measure how much participants continued the practices they learned in the MMC. We asked participants: (a) how often they do formal mindfulness practices (eg, sitting meditation, yoga, body scan); (b) average duration of each formal mindfulness practice; (c) how often they do informal mindfulness practices (eg, mindfulness of daily activities like eating, walking, speaking, listening, journaling, etc); and (d) when engaged in daily activities (eg, eating, walking, speaking, listening, journaling, etc) what percent of the time they do them mindfully. All 4 items were rated on a 7-point Likert-type scale, and the 2 formal and 2 informal meditation items were summed to form a formal and informal meditation index, respectively.
All physician self-report measures were administered at baseline, post-MMC (within 7 days of the weekend-long MBI), and 3 months after the MMC, with the exception of the MPQ, which was only administered at 3-month follow-up.
Patient Self-Reported Satisfaction With Primary Care Physician
To examine patient self-reported satisfaction with their primary care physicians, we assessed archival Consumer Assessment of Healthcare Providers and Systems–Clinician and Group Adult Visit (CG-CAHPS) survey data. The CAHPS surveys were developed to elicit reports from consumers about their health care experiences. The CG-CAHPS Adult Visit Survey contains 42 items; we used the Doctor Communication Composite (DCC; 6 items), which asks patients whether the doctor explained things clearly, listened carefully, gave easy to understand instructions, knew important medical history about the patient, showed respect, and spent enough time with the patient. These questions reference the most recent visit and use a 3-point response scale (1 = no; 2 = yes, somewhat; 3 = yes, definitely). We also used the single item Overall Doctor Rating (ODR), which asks the patient to rate the doctor on a scale from 0 (worst doctor possible) to 10 (best doctor possible). The DCC has demonstrated adequate internal consistency (α = .82) and is significantly correlated with the ODR (r = .52).25 At PMG, every month 10 surveys per provider are mailed to a randomly selected group of patients after a visit. In addition, all patients with an email on file (who have not been surveyed within the past 90 days) receive an email with the invitation to complete a survey online. The response rate for both is approximately 20%. We included all available CG-CAHPS surveys for each physician in the study (per physician M = 95.24, SD = 47.59, range = 20-189), and calculated average DCC and ODR scores for the 12-month period preceding the intervention (January-December 2014) to get a baseline. To examine pre- to post-MMC change, we also calculated average DCC and ODR scores for the 3-month period following the intervention (February-April 2015; per physician number of CG-CAHPS surveys M = 23.24, SD = 10.74, range = 3-52).
Data Analysis
We used a multilevel modeling (MLM) approach with restricted maximum likelihood estimation (REML) to examine linear change in our physician self-report outcomes over time as a fixed effect. Outcome variables were treated as random effects that could vary within person and across time. MLM with REML allows for more accurate estimates with small sample sizes and missing data that are missing at random or completely at random.26,27 To test whether changes in mindfulness, stress, compassion, resilience, and burnout (emotional exhaustion, depersonalization, and personal achievement) occurred after the MMC, we conducted 2 (Group: control and intervention) by 3 (Time: baseline, post-MMC, 3-month follow-up) Mixed analyses of variance with each outcome as the dependent variable using the MLM framework with a first-order autoregressive covariance structure (with the exception of CG-CAHPS data, which had 2 time points). Significant Group × Time interaction effects indicated the effectiveness of MMC, compared with the waitlist control group. Follow-up analyses of variance using the MLM approach and a symmetric covariance structure were used to test hypotheses about within-group changes from pre- to 3-month postintervention scores among the MMC and control groups separately. Given the very brief nature of the intervention (2 days), we chose the 3-month follow-up as the postintervention outcome time point. Effect sizes were calculated using Cohen’s d (small effect = .20, medium effect = .50, and large effect = .80).28 Zero-order Pearson’s correlations were used to examine the relationship between meditation practice and physician self-report outcomes at 3-month follow-up, and to examine the relationships between patient-reported satisfaction with their physician and physician self-report variables at baseline. For all analyses, 2-tailed tests were used and α was set at .05.
Results
Thirty-five potential participants responded to the recruitment email; 1 person was excluded due to working less than 30% in direct patient care and 1 other endorsed already having participated in the MBI at PMG. The 33 baseline participants had a mean age of 42.76 ± 8.43 years (range 32-61 years); 73% (n = 24) of the sample was female. The mean number of years licensed as a physician was 13.27 ± 8.09 (range 3-31 years) and 12% (n = 4) endorsed a current meditation practice (3 waitlist control and 1 MBI). There were no significant differences between the intervention (n = 17) and waitlist control (n = 16) group on any demographic variables (all Ps >.05).
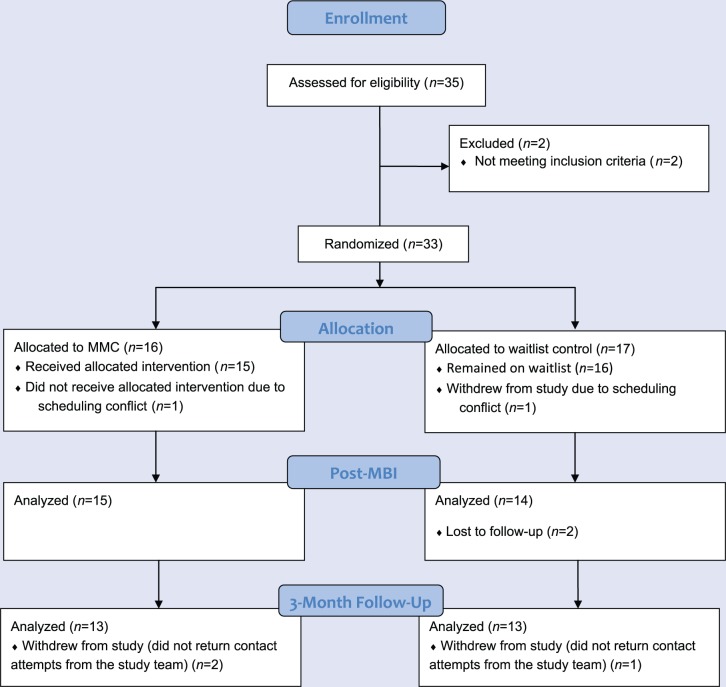
Figure 1 shows the participant flow. A total of 33 physicians provided written consent to enroll in the study, completed the baseline assessment, and were randomized to the MBI or waitlist control. Two participants (1 MBI and 1 waitlist control) withdrew (citing lack of time or scheduling conflicts) after randomization. Two waitlist control group participants withdrew from the study before postintervention assessment, and 2 MBI participants and 1 waitlist control group participant did not complete 3-month follow-up.
Figure 1.
Participant flow. MMC, Mindful Medicine Curriculum.
Change in Physician Self-Reported Outcomes Over Time
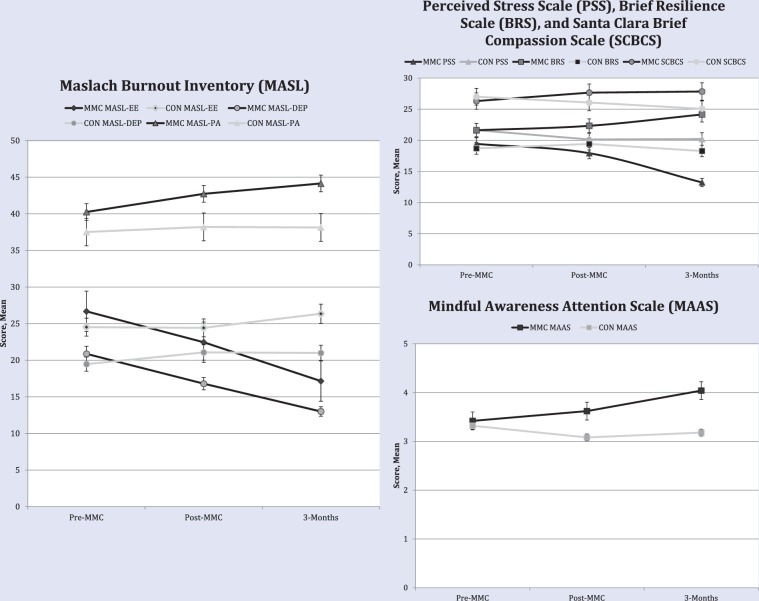
The intervention and control groups did not differ on any outcome measures at baseline (all Ps >.05). MLM analyses revealed significant Group × Time interactions for stress, mindfulness, emotional exhaustion, and depersonalization (see Table 1 and Figure 2). Participants in the MMC group reported significant improvements in stress (P < .001), mindfulness (P = .05), emotional exhaustion (P = .004), and depersonalization (P = .01) at 3-month follow-up relative to baseline; however, there was no significant improvement in resilience (P = .14), compassion (P = .66), or personal achievement (P = .06). In the control group, there were no statistically significant improvements on any physician self-report outcomes (Ps >.20).
Table 1.
Physician Self-Reported Outcomes by Group.
| Time × Group Interaction F-value, P-value | Pre-MMC CON M (SD) (n = 17) MMC M (SD) (n = 16) |
Post-MMC CON M (SD) (n = 14) MMC M (SD) (n = 15) |
3-Month Follow-up CON M (SD) (n = 13) MMC M (SD) (n = 13) |
CON Pre-MMC to 3-Month Follow-up ES, Percent Change (CI) MMC Pre-MMC to 3-Month Follow-up ES, Percent Change (CI) |
|
|---|---|---|---|---|---|
| MAAS | 3.98, .05 | 3.32 (0.76) 3.42 (0.96) |
3.08 (0.76) 3.62 (0.89) |
3.18 (0.58) 4.04 (1.02) |
−.23, –4.21% (–0.30, 0.41) 1.01, 18% (–1.18, –.47) |
| BRS | 1.45, .23 | 18.70 (5.13) 21.62 (4.45) |
19.42 (4.21) 22.33 (4.74) |
18.28 (5.32) 24.15 (5.47) |
−.10, –2.24% (–2.36, 2.50) .51, 11.70% (–5.72, .49) |
| PSS | 3.94, .05 | 21.64 (4.52) 19.43 (5.30) |
20.14 (5.99) 17.93 (5.27) |
20.21 (6.65) 13.23 (5.19) |
−.27, –6.60% (–1.83, 4.54) –1.30, –31.90% (3.96, 9.87) |
| SCBCS | 1.29, .25 | 27.00 (4.97) 26.31 (4.51) |
26.07 (4.73) 27.66 (3.22) |
25.07 (5.85) 27.84 (4.09) |
−.59, –7.14% (–1.31, 2.70) .57, 5.81% (–2.10, 2.26) |
| MASL-DEP | 5.76, .02 | 19.47 (7.90) 20.87 (8.42) |
21.07 (5.94) 16.80 (9.95) |
21.0 (7.52) 13.0 (8.14) |
.24, 7.85% (–3.24, 3.81) –1.12, –37.70% (3.15, 11.61) |
| MASL-EE | 6.15, .02 | 24.52 (10.57) 26.68 (8.48) |
24.42 (8.97) 22.46 (10.66) |
26.35 (8.06) 17.15 (9.0) |
.31, 3.25% (–4.14, 3.14) –1.57, –35.71% (6.24, 13.44) |
| MASL-PA | 1.15, .28 | 37.52 (6.43) 40.25 (5.92) |
38.21 (6.49) 42.73 (5.44) |
38.14 (6.08) 44.15(4.33) |
.18, 1.65% (–2.80, 1.22) 1.09, 9.68% (–7.06, –2.16) |
Abbreviations: CON, control group; MMC, Mindful Medicine Curriculum; ES, effect size; CI, difference score confidence interval; MAAS, Mindful Attention Awareness Scale; BRS, Brief Resiliency Scale; PSS, Perceived Stress Scale; SCBCS, Santa Clara Brief Compassion Scale; MASL-DEP, Maslach Burnout Inventory–Depersonalization; MASL-EE, Maslach Burnout Inventory–Emotional Exhaustion; MASL-PA, Maslach Burnout Inventory–Personal Achievement.
Figure 2.
Means of outcome variables assessed at baseline, postintervention, and 3-month follow-up.
Abbreviations: CON, control group; MMC, Mindful Medicine Curriculum group; MASL-EE, Maslach Burnout Inventory–Emotional Exhaustion; MASL-DEP, Maslach Burnout Inventory–Depersonalization; MASL-PA, Maslach Burnout Inventory–Personal Achievement.
Patient-Reported Satisfaction With Primary Care Physician
As shown in Table 2, among the entire sample (n = 33), baseline CG-CAHPS patient-reported DCC and ODR were significantly correlated with several baseline physician self-reported outcomes. However, as shown in Table 3, there were no significant Group × Time interactions for CG-CAHPS patient-reported DCC. Thus, the MMC had no impact on patient-reported satisfaction with their primary care physician at the 3-month follow-up.
Table 2.
Zero-Order Correlations between Physician Self-Report Measures and Patient-Reported Satisfaction with Primary Care Physician (CG-CAHPS) at Baseline (n= 33).
| MAAS | PSS | BRS | SCBCS | MASL-EE | MASL-DEP | MASL-PA | |
|---|---|---|---|---|---|---|---|
| CG-CAHPS—Doctor Communication | .22 | −.33* | .49** | −.03 | −.10 | −.04 | .37* |
| CG-CAHPS—Overall Doctor Rating | .11 | −.27† | .48** | .12 | −.05 | −.07 | .39* |
Avvreviations: CG-CAHPS—Doctor Communication, Consumer Assessment of Healthcare Providers and Systems–Clinician and Group Adult Visit—Doctor Communication Composite, Consumer Assessment of Healthcare Providers and Systems–Clinician and Group Adult Visit—Overall Doctor Rating; MAAS, Mindful Attention Awareness Scale; BRS, Brief Resiliency Scale; PSS, Perceived Stress Scale; SCBCS, Santa Clara Brief Compassion Scale; MASL-DEP, Maslach Burnout Inventory–Depersonalization; MASL-EE, Maslach Burnout Inventory–Emotional Exhaustion; MASL-PA, Maslach Burnout Inventory–Personal Achievement.
P < .10; *P < .05; **P < .01.
Table 3.
Patient-Reported Satisfaction With Primary Care Physician (CG-CAHPS) by Group.
| 12-Month Aggregate Baseline Pre-MMC | 3 Month Aggregate Post-MMC | |||||
|---|---|---|---|---|---|---|
| CON M (SD) (n = 17) | MMC M (SD) (n = 16) | CON M (SD) (n = 13) | MMC M (SD) (n = 13) | F | P | |
| CG-CAHPS—Doctor Communication | 17.23 (1.90) | 17.48 (1.40) | 17.29 (1.92) | 17.37 (1.65) | 1.30 | .27 |
| CG-CAHPS—Overall Doctor Rating | 9.01 (1.29) | 9.12 (1.36) | 9.04 (1.23) | 9.19 (1.44) | 0.77 | .44 |
Abbreviations: CON, control group; MMC, Mindful Medicine Curriculum Group; CG-CAHPS—Doctor Communication, Consumer Assessment of Healthcare Providers and Systems–Clinician and Group Adult Visit—Doctor Communication Composite, Consumer Assessment of Healthcare Providers and Systems–Clinician and Group Adult Visit—Overall Doctor Rating.
Ongoing Meditation Practice
As shown in Table 4, a large majority of the MMC group (92%; n = 12) endorsed ongoing formal (92%; n = 12; eg, sitting meditation, yoga, body scan) and informal (92%; n = 12; eg, mindfulness of daily activities like eating, walking, speaking, listening, journaling, etc) meditation practice at 3-month post-MMC. As shown in Table 5, there were a number of significant correlations between formal/informal meditation practice and physician self-report outcomes among MMC group participants at 3-month follow-up.
Table 4.
Formal and Informal Mindfulness Practice at Three-Month Follow-up Among Mindful Medicine Curriculum Group Participants (n = 13).
| Formal Practice Frequency | Average Formal Practice Duration (in Minutes) | |
|---|---|---|
| Never | 8% (n = 1) | 0-10 (n = 10) |
| <1 day per month | 15% (n = 2) | 11-20 (n = 2) |
| 1-10 days per month | 46% (n = 6) | 21-30 (n = 0) |
| 11-20 days per month | 23% (n = 3) | 31-40 (n = 0) |
| 21-29 days per month | 8% (n = 1) | 41-50 (n = 0) |
| Every day | 0% (n = 0) | 51-60 (n = 0) |
| Informal Practice Frequency | Percentage of Time Engaged in Daily Activities Mindfully | |
| Never | 8% (n = 1) | 0-10 (n = 4) |
| <1 day per month | 0% (n = 0) | 11-20 (n = 2) |
| 1-10 days per month | 54% (n = 7) | 21-30 (n = 0) |
| 11-20 days per month | 0% (n = 0) | 31-40 (n = 0) |
| 21-29 days per month | 30% (n = 4) | 41-50 (n = 3) |
| Every day | 8% (n = 1) | 51-60 (n = 1) 61-70 (n = 1) 71-80 (n = 1) 81-90 (n = 0) 91-100 (n = 0) |
Table 5.
Zero-Order Correlations Between Formal and Informal Mindfulness Practice and Outcomes among MMC Group at 3-Month Follow-up (n = 13).
| MAAS | PSS | BRS | SCBCS | MASL-EE | MASL-DEP | MASL-PA | |
|---|---|---|---|---|---|---|---|
| Formal mindfulness practice | .53* | −.56* | .26 | .08 | −.46† | −.55* | .11 |
| Informal mindfulness practice | .56* | −.46† | .49* | .34 | −.50* | −.34 | .49* |
Abbreviations: MMC, Mindful Medicine Curriculum; MAAS, Mindful Attention Awareness Scale; BRS, Brief Resiliency Scale; PSS, Perceived Stress Scale; SCBCS, Santa Clara Brief Compassion Scale; MASL-DEP, Maslach Burnout Inventory–Depersonalization; MASL-EE, Maslach Burnout Inventory–Emotional Exhaustion; MASL-PA, Maslach Burnout Inventory–Personal Achievement.
P < .10; *P < .05.
Discussion
Results from this RCT demonstrated that brief mindfulness training for primary care physicians reduced stress and burnout and increased mindfulness. Similar to Fortney et al,19 the current study utilized an abbreviated format—a mindfulness weekend retreat plus 2 follow-up sessions. The abbreviated format was intended to facilitate enrollment that might be detrimentally affected by a more traditional 8-week MBSR course. Physicians who completed the MMC reported enhanced mindfulness and reduced stress, emotional exhaustion, and depersonalization from baseline to 3-month follow-up when compared with the control group. Also notable, at baseline, physicians in this study reported lower mindfulness scores29 and higher depersonalization scores19,30 when compared with previously published psychometric data. This is concerning, considering that burnout is a significant threat to physician well-being and is associated with lower patient satisfaction and reduced adherence to treatment plans.31
Patients may also benefit from physician mindfulness training. Previous studies have noted that MBIs improve provider empathy and build communication and rapport between doctor and patient, which can lead to better patient satisfaction.25 Our results provide tentative support for this association; baseline correlations suggest that physicians who are more resilient and who cope better with stress—which are common outcomes of MBIs—are rated more positively by their patients. We did not find any significant differences over time in patient satisfaction between the MMC and control groups; however, the baseline scores on the CG-CAHPS were quite high, leaving little room for improvement. Despite our null findings, the hypothesis that mindfulness training can enhance patient-provider relationships and ultimately lead to improved health outcomes needs further investigation using higher powered RCTs.
In addition, participants in the MMC group were able to maintain their practices over a 3-month period, confirming that a brief weekend introduction to mindfulness practice is sustainable with minimal ongoing support. Furthermore, self-reports of formal meditation practice were significantly correlated with improvements in mindfulness, stress, and depersonalization, while self-reports of informal practices were significantly correlated with improvements in mindfulness, resilience, emotional exhaustion, and personal achievement. Additionally, most of the participants in this cohort were able to achieve these improvements with less than 10 minutes of formal meditation daily. This is noteworthy, as most MBIs among health care providers lack information regarding adherence to formal and informal practices conducted outside the weekly sessions. These results enhance our understanding of the differential effects of formal and informal practices among health care providers and provide more information regarding the frequency and intensity of mindfulness practice required to and sustain effects. This is especially important given the time constrictions of this population.
This study had a number of limitations. First, the small sample size reduced statistical power and multiple comparisons may have increased the likelihood of type I errors. The medium to large effect sizes for changes in nonsignificant outcomes (ie, compassion, resiliency, and personal achievement) in the MMC group from baseline to 3-month follow-up suggest the possibility that our sample size was too small to detect improvements on these outcomes. Second, the generalizability of the findings is limited because participants volunteered to participate in the study, introducing selection bias. Third, a potential variable that was not controlled for, but may have been influential, was enhanced social support. The mindfulness retreat provided an opportunity for practitioners to come together and discuss topics unique to patient care issues, which can be very depleting. Support from a group of like-minded physicians is likely partly responsible for some of the benefits, and may be more difficult to measure. While this is a separate component from traditional MBI teaching, the group interaction was considered an integral part of the practices and follow-up.32
In summary, burnout is a common consequence of the ever-increasing demands made of practicing physicians. Mindfulness is a promising approach to managing this concern. Among a group of primary care physicians, who at baseline endorsed relatively high burnout and low mindfulness, we found that a very brief MBI led to significant improvements in burnout, stress, and mindful awareness. Most of these physicians also maintained a mindfulness practice 3 months after the training. Physician burnout is a complex phenomenon with multiple causes. Medical systems contending with high physician burnout rates might consider offering brief mindfulness training as one potential remedy.
Acknowledgments
The authors thank the Providence Health System Clinical Transformation Council for funding this study (Principal Investigator: David A Schroeder).
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Informed Consent: Not applicable, because this article does not contain any studies with human or animal subjects.
Trial Registration: Not applicable, because this article does not contain any clinical trials.
References
- 1. Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172:1377-1385. [DOI] [PubMed] [Google Scholar]
- 2. McCray LW, Cronholm PF, Bogner HR, Gallo JJ, Neill RA. Resident physician burnout: is there hope? Fam Med. 2008;40:626-632. [PMC free article] [PubMed] [Google Scholar]
- 3. Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory manual. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 4. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet. 2009;374:1714-1721. [DOI] [PubMed] [Google Scholar]
- 5. Ratanawongsa N, Roter D, Beach MC, et al. Physician burnout and patient-physician communication during primary care encounters. J Gen Intern Med. 2008;23:1581-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dewa CS, Loong D, Bonato S, Thanh NX, Jacobs P. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res. 2014;14:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thorne SE, Bultz BD, Baile WF, Team SC. Is there a cost to poor communication in cancer care?: a critical review of the literature. Psycho-oncology. 2005;14:875-884. [DOI] [PubMed] [Google Scholar]
- 8. Waldman JD, Kelly F, Aurora S, Smith HL. The shocking cost of turnover in health care. Health Care Manage Rev. 2004;29:2-7. [DOI] [PubMed] [Google Scholar]
- 9. Goldstein J. The Experience of Insight: A Natural Unfolding. Boston, MA: Shambhala; 1980. [Google Scholar]
- 10. Bishop SR, Lau M, Shapiro S, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. 2004;11:230-241. [Google Scholar]
- 11. Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174:357-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: a comprehensive meta-analysis. Clin Psychol Rev. 2013;33:763-771. [DOI] [PubMed] [Google Scholar]
- 13. Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Altern Complement Med. 2009;15:593-600. [DOI] [PubMed] [Google Scholar]
- 14. Foureur M, Besley K, Burton G, Yu N, Crisp J. Enhancing the resilience of nurses and midwives: pilot of a mindfulness-based program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemporary Nurse. 2013;45:114-125. [DOI] [PubMed] [Google Scholar]
- 15. Sharma M, Rush SE. Mindfulness-based stress reduction as a stress management intervention for healthy individuals: a systematic review. J Evid Based Complementary Altern Med. 2014;19:271-286. [DOI] [PubMed] [Google Scholar]
- 16. Condon P, Desbordes G, Miller WB, DeSteno D. Meditation increases compassionate responses to suffering. Psychol Sci. 2013;24:2125-2127. [DOI] [PubMed] [Google Scholar]
- 17. Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manage. 2005;12:164-176. [Google Scholar]
- 18. Asuero AM, Queraltó JM, Pujol-Ribera E, Berenguera A, Rodriguez-Blanco T, Epstein RM. Effectiveness of a mindfulness education program in primary health care professionals: a pragmatic controlled trial. J Contin Educ Health Prof. 2014;34:4-12. [DOI] [PubMed] [Google Scholar]
- 19. Fortney L, Luchterhand C, Zakletskaia L, Zgierska A, Rakel D. Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. Ann Fam Med. 2013;11:412-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822-848. [DOI] [PubMed] [Google Scholar]
- 21. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15:194-200. [DOI] [PubMed] [Google Scholar]
- 22. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385-396. [PubMed] [Google Scholar]
- 23. Hwang JY, Plante T, Lackey K. The development of the Santa Clara Brief Compassion Scale: an abbreviation of Sprecher and Fehr’s compassionate love scale. Pastoral Psychol. 2008;56:421-428. [Google Scholar]
- 24. Sprecher S, Fehr B. Compassionate love scale for close others and humanity. J Soc Pers Relat. 2005;22:629-651. [Google Scholar]
- 25. Dyer N, Sorra JS, Smith SA, Cleary PD, Hays RD. Psychometric properties of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Clinician and Group Adult Visit Survey. Med Care. 2012;50(suppl):S28-S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Maas CJ, Hox JJ. Sufficient sample sizes for multilevel modeling. Methodology. 2005;1:86-92. [Google Scholar]
- 27. Snijders TA. Multilevel Analysis. New York, NY: Springer; 2011. [Google Scholar]
- 28. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 29. Beach MC, Roter D, Korthuis PT, et al. A multicenter study of physician mindfulness and health care quality. Ann Fam Med. 2013;11:421-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Krasner MS, Epstein RM, Beckman H, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA. 2009;302:1284-1293. [DOI] [PubMed] [Google Scholar]
- 31. Dyrbye LN, Shanafelt TD. Physician burnout: a potential threat to successful health care reform. JAMA. 2011;305:2009-2010. [DOI] [PubMed] [Google Scholar]
- 32. Beckman HB, Wendland M, Mooney C, et al. The impact of a program in mindful communication on primary care physicians. Acad Med. 2012;87:815-819. [DOI] [PubMed] [Google Scholar]