Abstract
Stress is a core issue to be addressed in lifestyle medicine. Not only does it influence disease directly (eg, cardiovascular disease), it also indirectly affects health by having a negative influence on other behaviors such as sleep and physical activity. The importance of stress is further highlighted by the fact that it is one of the most highly ranked health risks for employees globally. Practitioners are encouraged to attend to both significant life stressors and those that are encountered daily. Stress reduction strategies are further discussed.
Keywords: stress, lifestyle, Type A behavioral pattern
‘Most would agree that it is far better to prevent heart disease, type 2 diabetes, or obesity than to treat them.’
A few salient concepts should be considered and addressed by any lifestyle practitioner regardless of the patient being treated. For example, a focus on prevention should be a major goal when dealing with a host of diseases that are treated through lifestyle changes. Most would agree that it is far better to prevent heart disease, type 2 diabetes, or obesity than to treat them.1,2 An ounce of prevention truly is worth a pound of cure.3 Optimal practice also addresses health from environmental, behavioral, medical, and motivational perspectives. In addressing disease from these multiple perspectives, we have the greatest chance to both treat and prevent it. Attending to factors that promote the development of disease, negatively affect treatment outcomes, and decrease the likelihood of patients adhering to recommended lifestyle change is also critical. Stress is an issue that meets each of these criteria.4
Stress can be described in a medical sense as the rate of wear and tear in the body,5 or more generally as an aversive event (ie, physical, mental, or emotional) that threatens the well-being of an individual. As discussed in this issue by Rossi et al,6 stress is one of the modifiable risk factors associated with infertility. Although its impact on infertility is a relatively new concept, the role that stress has on health behaviors in general has been studied for quite some time. Several of the first studies on stress observed its impact on cardiovascular disease. Seminal research by Friedman and Rosenman7 demonstrated that people who engage in a “chronic and incessant struggle to achieve more in less time” were at higher risk to have coronary heart disease. In time, this behavioral pattern became known as Type A personality.8 In current literature, it is referred to as Type A behavior pattern (TABP).9
Considerable debate regarding how well TABP predicts cardiovascular disease exists; however, there is a clear and consistent association between the two.10-12 Although several characteristics and moods are included in TABP (eg, hostility, impatience, irritability, frustration),13 compelling evidence suggests that stress (and one’s response to it) is the major factor driving the adverse health outcomes in these individuals.14,15 Even more concerning is that stressors are associated with cardiovascular risk factors beginning as early as childhood.16,17 Overall, the connection between stress and cardiovascular disease is both long-standing and strong.
Impact on Other Positive Health Behaviors
The role that stress has on health extends beyond that of cardiovascular disease and fertility. For example, stress has been shown to increase the length of time needed for injuries to heal,18 affect aging processes,19 and decrease immune function,20 and this is by no means an exhaustive list. Although stress has a direct consequence on health, it also has an indirect one. Stress likely has its most profound influence on health in its interaction with multiple other behaviors that support well-being. For example, high levels of stress affect the quality of sleep and make it less likely one will engage in physical activity.
Sleep
Stress has been shown to negatively affect sleep behaviors.21 Observational studies have produced an abundance of literature regarding this occurrence. Daily mental tasks requiring elevated tension have resulted in highly variable sleep patterns.22 Stressful life events in adolescents with and without major depressive disorder alter slow-wave sleep in both groups.23 Experimental studies confirm these observational findings. Presleep stress (ie, an aversive film) increased the number of awakenings and distorted overall sleep patterns.24 Furthermore, when an intellectually challenging test was given to university students that resulted in feelings of inferiority (ie, the stressor), students’ sleep patterns were heavily affected.25
Physical Activity and Exercise
A strong association has been found between higher levels of stress and physical activity (PA).26 Although a greater emphasis has been placed on how high levels of PA lead to lower levels of stress, a reverse relationship may exist.27,28 Observational studies have demonstrated this link. Specifically, chronically stressed populations, including medical school students,29 first-time mothers,30 and cancer survivors31 all have been shown to exhibit low levels of PA. Although numerous observational studies have provided a link between stress and PA, there is conflicting evidence regarding the association between the two.32,33
Observational studies have established a link between increased stress and decreased PA, and experimental studies have reaffirmed this inverse relationship. Phenomenon triggering acute stress has been shown to produce a significant reduction in PA.34-36 For example, children were randomized to a passive reading (control) or a public speaking (stress) condition. After participation in the respective condition, children were given the opportunity to exercise. Children in the public speaking condition were less likely to engage in PA.34 Case controlled studies have found a similar pattern between stress and PA. Parents of a child who had just received a cancer diagnosis reported lower levels of PA than parents of a healthy child,35 and parents of a child with a cancer diagnosis had lower levels of PA three months after diagnosis compared to matched controls.36
Far-Reaching Impact
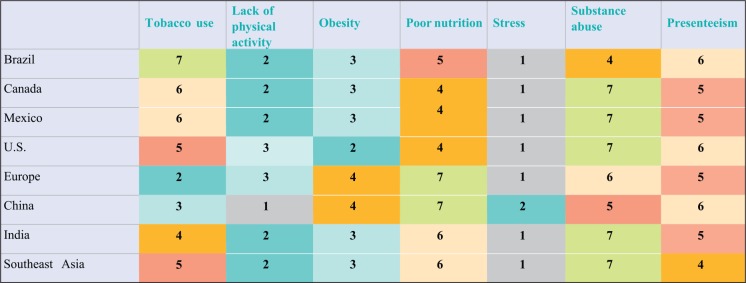
Given the clear and extensive impact of stress on health, the pervasiveness of stress is an area of considerable concern. Stress and life in a Westernized world have almost become synonymous. However, Westernized societies are not the only ones to deal with the issue of high levels of stress. In a recent global survey, employers overwhelmingly rank stress as the major health risk faced by their employees (see Figure 1). A significant increase in stress over the past few decades has been observed in the general population.37 This progression may be especially true for women, less-educated individuals, and those with lower incomes. Although sources of stress are extremely diverse and should be assessed at an individual level, some of the most common sources of stress include money, work, health concerns, and personal safety.38 The most reported behaviors used to cope with stress included watching TV, surfing the Internet, napping, eating, drinking alcohol, and smoking.38
Figure 1.
Lifestyle risk factors that are a workforce issue.
Note. Ranking by employers of most important issues affecting health of their employees. Ranking of 1 is the issue of greatest concern.
First reported in Staying@Work™ Report: The Business Value of a Healthy Workforce by ©Willis Towers Watson. Reprinted with permission.
Treatment
Practitioners in lifestyle medicine should be prepared to help their patients cope with issues that cause large amounts of stress suddenly (eg, divorce, birth of child) or chronic issues that create constant lower levels of stress (eg, work concerns, dealing with chronic illness). Stress management techniques are numerous and include relaxation (eg, diaphragmatic breathing, guided relaxation), behavioral approaches (eg, distraction, time management), or cognitive strategies (eg, humor, positive self-statements).39 Patients should identify which technique they feel would be the most effective and most likely to be used outside of the office. The chosen technique should be practiced before the stressful event occurs. It may be most beneficial for time in the office to be dedicated to practicing these techniques. Patients should demonstrate mastery with the chosen technique. The concept of “overlearning” may further increase the likelihood that the relaxation strategy will be effective when the stressor occurs.
Conclusion
Stress is a significant lifestyle issue that should be addressed in order to promote overall wellness. By attending to patients’ stress, practitioners not only address an issue that is directly associated with disease but also address behaviors that support health, such as sleep and exercise. However, stress reduction is often “tacked on” to existing interventions and often is not a primary focus.39 Given that stress has a negative impact on so many individuals, health care professionals should consider it a priority in providing treatment.
Acknowledgments
This work is a publication of the Department of Health and Human Performance, University of Houston (Houston, Texas).
References
- 1. Shenkin H. Is an ounce of prevention always worth a pound of cure? No: promoting prevention to contain costs is a logical fallacy. West J Med. 2001;174(2):85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Teutsch SM. Is an ounce of prevention always worth a pound of cure? Yes: clinical preventive services can provide excellent value. West J Med. 2001;174(2):84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Citizen O. An anonymous letter: Protection of towns from fire. Pennsylvania Gazette; February 4, 1735. [Google Scholar]
- 4. Johnson SL, Tandon SD, Cheng TL. Career readiness: a potential pathway through which urban youth exposure to stress influences adult health. J Community Psychol. 2015;43:321-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Selye H. The Stress of Life. Revised ed New York, NY: McGraw Hill; 1978. [Google Scholar]
- 6. Rossi BV, Abusief M, Missmer SA. Modifiable Risk Factors and Infertility: What are the connections? Am J Lifestyle Med. 2016;10:220-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Friedman M, Rosenman RH. Association of specific overt behavior pattern with blood and cardiovascular findings. J Am Med Assoc. 1959;169:1286-1296. [DOI] [PubMed] [Google Scholar]
- 8. Friedman M. Type A Behavior: Its Diagnosis and Treatment. New York, NY: Plenum Press, 1996. [Google Scholar]
- 9. Bokenberger K, Perderson NL, Gatz M, Dahl AK. The type A behavior pattern and cardiovascular disease as predictors of dementia. Health Psychol. 2014;33:1593-1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jamil G, Haque A, Namawar A, Jamil M. “Personality traits and heart disease in the Middle East.” Is there a link? Am J Cardiovasc Dis. 2013;3:163-169. [PMC free article] [PubMed] [Google Scholar]
- 11. Smith TW, Glazer K, Ruiz JM, Gallo LC. Hostility, anger, aggressiveness, and coronary heart disease: an interpersonal perspective on personality, emotion and health. J Pers. 2004;72:1217-1270. [DOI] [PubMed] [Google Scholar]
- 12. Smith TW, MacKenzie J. Personality and risk of physical illness. Annu Rev Clin Psychol. 2006;2:435-467. [DOI] [PubMed] [Google Scholar]
- 13. Rosenman RH, Friedman M, Jenkins CD, Strauss R, Wurm M, Kositchek R. Recurring and fatal myocardial infarction in the Western Collaborative Group Study. Am J Cardiol. 1967;19:771-775. [DOI] [PubMed] [Google Scholar]
- 14. Friedman M. Type A behavior pattern: some of its pathophysiological components. Bull N Y Acad Med. 1977;53:593-604. [PMC free article] [PubMed] [Google Scholar]
- 15. Rosmond R, Bjorntorp P. The hypothalamic-pituitary-adrenal axis activity as a predictor of cardiovascular disease, type 2 diabetes and stroke. J Intern Med. 2000;247:188-197. [DOI] [PubMed] [Google Scholar]
- 16. Roemmich JN, Lobarinas CL, Joseph PN, Lambiase MJ, Archer Iii FD, Dorn J. Cardiovascular reactivity to psychological stress and carotid intima-media thickness in children. Psychophysiology. 2009;46:293-299. [DOI] [PubMed] [Google Scholar]
- 17. Roemmich JN, Lambiase MJ, Balantekin KN, Feda DM, Dorn J. Stress, behavior, and biology: risk factors for cardiovascular disease in youth. Exerc Sport Sci Rev. 2014;42:145-152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kiecolt-Glaser JK, Marucha PT, Malarkey WB, Mercado AM, Glaser R. Slowing of wound healing by psychological stress. Lancet. 1995;346:1194-1196. [DOI] [PubMed] [Google Scholar]
- 19. Hawkley LC, Cacioppo JT. Stress and the aging immune system. Brain Behav Immun. 2004;18:114-119. [DOI] [PubMed] [Google Scholar]
- 20. Glaser R, Kiecolt-Glaser JK. Stress-induced immune dysfunction: implications for health. Nat Rev Immunol. 2005;5:243-251. [DOI] [PubMed] [Google Scholar]
- 21. Kim E, Dimsdale JE. The effect of psychosocial stress on sleep: a review of the polysomnographic evidence. Behav Sleep Med. 2007;5:256-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kobayashi T, Ishikawa T, Arakawa K. Effects of daytime activity upon the timing of REM sleep periods during a night. Psychiatry Clin Neurosci. 1998;52:130-131. [DOI] [PubMed] [Google Scholar]
- 23. Williamson DE, Dahl RE, Birmaher B, Goetz RR, Nelson B, Ryan ND. Stressful life events and EEG sleep in depressed and normal control adolescents. Biol Psychiatry. 1995;37:859-865. [DOI] [PubMed] [Google Scholar]
- 24. Baekeland F, Koulack D, Lasky R. Effects of a stressful presleep experience on electroencephalograph-recorded sleep. Pyschophysiology. 1968;4:436-443. [DOI] [PubMed] [Google Scholar]
- 25. Koulack D, Prevost F, De Koninck J. Sleep, dreaming, and adaptation to a stressful intellectual activity. Sleep. 1985;8:244-253. [DOI] [PubMed] [Google Scholar]
- 26. Stults-Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44:81-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Salmon P. Effects of physical exercise on anxiety, depression, and sensitivity to stress: a unifying theory. Clin Psychol Rev. 2001;21:33-61. [DOI] [PubMed] [Google Scholar]
- 28. Lutz RS, Lochbaum MR, Lanning B, Stinson LG, Brewer R. Cross-lagged relationships among leisure-time exercise and perceived stress in blue-collar workers. J Sport Exerc Psychol. 2007;29:687-705. [DOI] [PubMed] [Google Scholar]
- 29. Buchman BP, Sallis JF, Criqui MH, Dimsdale JE, Kaplan RM. Physical activity, physical fitness, and psychological characteristics of medical students. J Psychosom Res. 1991;35:197-208. [DOI] [PubMed] [Google Scholar]
- 30. Vernon MM, Young-Hyman D, Looney SW. Maternal stress, physical activity, and body mass index during new mothers’ first year postpartum. Women Health. 2010;50:544-562. [DOI] [PubMed] [Google Scholar]
- 31. Park CL, Edmondson D, Fenster JR, Blank TO. Positive and negative health behavior changes in cancer survivors: a stress and coping perspective. J Health Psychol. 2008;13:1198-1206. [DOI] [PubMed] [Google Scholar]
- 32. Allison KR, Adlaf EM, Ialomiteanu A, Rehm J. Predictors of health risk behaviours among young adults: analysis of the National Population Health Survey. Can J Public Health. 1999;90:85-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gadalla TM. Unhealthy behaviours among Canadian adolescents: prevalence, trends and correlates. Chronic Dis Inj Can. 2012;32:156-163. [PubMed] [Google Scholar]
- 34. Roemmich JN, Gurgol CM, Epstein LH. Influence of an interpersonal laboratory stressor on youths’ choice to be physically active. Obes Res. 2003;11:1080-1087. [DOI] [PubMed] [Google Scholar]
- 35. Smith AW, Baum A, Wing RR. Stress and weight gain in parents of cancer patients. Int J Obes (Lond). 2005;29:244-250. [DOI] [PubMed] [Google Scholar]
- 36. Vitaliano PP, Scanlan JM, Ochs HD, Syrjala K, Siegler IC, Snyder EA. Psychosocial stress moderates the relationship of cancer history with natural killer cell activity. Ann Behav Med. 1998;20:199-208. [DOI] [PubMed] [Google Scholar]
- 37. Cohen S, Janicki-Deverts D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42:1320-1334. [Google Scholar]
- 38. American Psychological Survey. Stress in America: The impact of discrimination. http://www.apa.org/news/press/releases/stress/2015/impact-of-discrimination.pdf. Published March 10, 2016. Accessed March 23, 2016.
- 39. Cox TL, Krukowski R, Love SJ, et al. Stress management-augmented behavioral weight loss intervention for African American women: a pilot, randomized controlled trial. Health Educ Behav. 2013;40:78-87. [DOI] [PubMed] [Google Scholar]