Abstract
Background. The results presented from a practice survey include cases of interest, demonstrating improvements in cardiometabolic risk factors utilizing a Nutrient-Dense, Plant-Rich (NDPR) diet. It includes changes in weight, blood pressure, and lipids parameters derived from the survey and retrospective chart review. Methods. Practice records and interviews were used for case history descriptions. Participants’ data were collected via an online survey. Results. Adherence to a NDPR dietary protocol resulted in reduced low-density lipoprotein cholesterol and serum triglycerides. Compliance of greater than 80% with the target diet resulted in an average sustained weight loss of over 50 pounds in 75 obese subjects. There was a corresponding average reduction of 27.8 mm Hg in systolic blood pressure for the 127 survey responders with untreated hypertension at baseline, and a 42.2 mg/dL average decrease in low-density lipoprotein cholesterol for the 328 survey responders, not on cholesterol reducing medications. Conclusion. The outcomes from both the survey responders and cases demonstrate the potential for the NDPR dietary intervention to improve weight, blood pressure, lipids, and even reverse severe cardiovascular disease. Though this is a report of cases and self-reported benefits, it adds evidence to support the need for further studies investigating the potential of this dietary intervention.
Keywords: diet therapy, hypertension, lipids, nutrient dense
“It is critically important to identify dietary patterns that are most effective that can be utilized therapeutically for patients with CAD willing to make dietary modifications.”
Coronary artery disease (CAD) is the leading cause of morbidity and mortality in the United States and is responsible for a major toll on the health care system. The human suffering resulting from cardiovascular disease (CVD) and its related comorbidities is compounded by economic considerations that total an estimated $315.4 billion dollars spent on hospitalizations and treatment.1 Despite significant resource allocations for prevention and treatment, CVD remains the primary cause of death in the United States. The American Heart Association’s 2014 Update on Heart Disease and Stroke Statistics indicates that CVD prevalence in the United States is 83.6 million, or 35.3% of the population, with a mortality rate that accounted for 31.9% of all deaths in 2010. Current evidence supports the association of Western dietary patterns, low intake of vegetables and fruits, tobacco consumption, and sedentary lifestyle with increased incidence of CVD, obesity, metabolic syndrome, diabetes mellitus, and other chronic diseases.2-6 It is critically important to identify dietary patterns that are most effective that can be utilized therapeutically for patients with CAD willing to make dietary modifications.
Higher vegetable consumption, as a percentage of total calories, demonstrates increasing protection against heart disease and strokes, as shown in multiple studies and in meta-analyses.7-9 The benefits from the synergistic effects of phytochemicals and whole-food constituents occur beyond the isolated effects of these compounds.10-13 Many studies document this effect, some particularly convincing. For example, one such study, published in the Journal of Epidemiology & Community Health, followed a random sample of over 65 000 people in England and found that vegetables had the strongest protective effect from CVD, with each daily portion reducing overall risk of death by 16%. A raw vegetable salad contributed to a 13% cardiovascular risk reduction per portion, and each portion of fresh fruit was associated with a smaller but still significant 4% reduction.14 These studies support the concept that increased fruit and vegetable consumption is associated with decreased mortality. Other studies have had similar conclusions: the higher the percentage of vegetables in the diet (and to a lesser degree, fruit), the lower the risk of death, and enhancement of lifespan.7 The take-home message from these studies is that it requires a large consumption of these foods to see dramatic benefits.
A limited number of interventional studies have demonstrated that plant-rich nutritional interventions can not only prevent but also arrest and reverse advanced CAD.15,16 However, those interventions have focused on fat avoidance, in spite of evidence that seeds and nuts may add a significant degree of cardiovascular protection.17 The Nutrient-Dense, Plant-Rich (NDPR) diet likewise focuses on whole plant foods but, in contrast, allows the liberal use of raw nuts and seeds, and so is not fat-avoidant.
This survey study intends to show that when utilized as a primary intervention, such a rigorous nutritional protocol can be an acceptable therapeutic choice for many people and can result in dramatic improvements in cardiovascular health, not typically obtainable from traditional medical management. The only previous research on the NDPR diet-style has been to demonstrate short-term benefits on cholesterol and metabolic markers of disease18 and to demonstrate improvements in body weight19 and to modify the perception of hunger reducing overeating behavior.20 There are no long-term investigations on cardiovascular benefits using the NDPR diet-style. This preliminary investigation surveys a large number of participants who have adopted this intervention for numerous years within a private medical practice. Furthermore, identifying and examining individuals, within this group, with advanced disease that have demonstrated dramatic improvements and/or reversal of atherosclerosis, is an important initial step to encourage further research into this therapeutically effective intervention.
Materials and Methods
Dietary Intervention
An NDPR diet-style, also called a nutritarian diet, represents a significant departure from the typical American diet, where the majority of calories come from processed foods and animal products. A nutritarian diet is a vegetable-based diet that emphasizes the consumption of greens, beans/legumes, and other vegetables and includes fruits, nuts, seeds, and whole grains. It minimizes the consumption of refined grains, vegetable oils, processed foods, and animal products. Though it is not necessarily vegan, animal products, such as chicken and fish, are limited to 3 (small to moderate) servings a week. A nutritarian diet is designed to be micronutrient-rich (particularly high in plant-derived phytochemicals), nutritionally complete, and hormonally favorable, avoiding high glycemic index carbohydrates. Foods with the highest micronutrient density are vegetables, beans, and berries, whereas processed foods and animal products are comparatively low in micronutrients, especially antioxidants and phytochemicals. The small amount of animal products allowed also assures low exposure to saturated fats; moreover, the diet is naturally very high in fiber.
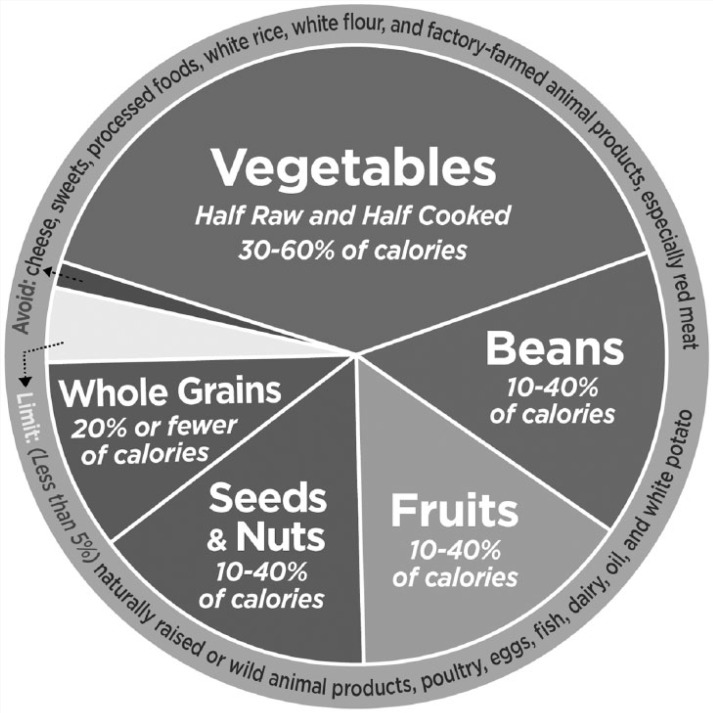
The use of a multivitamin containing B12, iodine, zinc, and vitamin D was also encouraged as well as a relatively small amount of EPA-DHA from algae, to assure comprehensive nutrient adequacy, considering the lack of or low amount of animal products recommended and utilized (see Figure 1).
Figure 1.
A Nutritarian Food Plate.
“Nutritarian” Food Consumption Guidelines
Consume unlimited quantities of raw vegetables; strive for a half pound daily.
Eat at least half a pound of cooked green vegetables daily.
Consume beans/legumes as a preferred carbohydrate food, at least half a cup daily.
Consume 3 to 5 servings of fresh fruit daily.
Limit cooked starches to 1 serving (approximately 1 cup) daily until reaching ideal body mass index.
Limit animal products to <8 oz weekly or eliminate until health goals reached.
Consume at least 1 ounce of raw nuts and seeds daily, only with meals, not as snacks.
Minimize salt (less than 1000 mg a day recommended) and avoid processed foods, refined carbohydrates, oils, dairy, sugar, soda, fruit drinks/juices, white rice, white potatoes, white flour.
No restriction on calories or portions are required, though snacking is not recommended, total calories should be consumed within the 3 meals.
Data Collection
A variable-length survey was administered online through the e-mail mailing list of our family practice office and online health community. Respondents to the survey were presented with a 42-item, recall-dependent questionnaire assessing duration and percentage adherence to an NDPR diet-style, and they answered queries encompassing cardiovascular testing and changes to weight, vital signs, lipid panel, and medication usage prior to and after undertaking dietary intervention. Though 2273 individuals completed the survey, many of the responders did not have medical issues to report, so only those with a history of high blood pressure, high cholesterol, or a body mass index (BMI) greater than 25 were included in this analysis. Respondents who gave permission to share their medical records with us for confirmation of self-reported responses were contacted to provide e-signatures on a digital version of OCA Official Form #960. These participants’ HIPAA-compliant releases were then faxed to their primary care physicians, if records were not already in our office files. Medical records received within the study time frame were compiled, and weight, BMI, blood pressure, total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides, and values salient to the self-reported dietary intervention period were extracted from the records and coded for analysis. Pre- and postintervention values were delineated based on self-reported intervention duration and medical record data within 3 months on either side of the window. Due to the incomplete quantity and quality of received records, precise time frames for all blood pressure changes, medication cessation, and intervention duration were unavailable and so were derived from self-reported survey responses. This study was approved by the Winthrop University Hospital Institutional Review Board, Mineola, New York (IRB# 14319), and it is in accordance with all ethical standards of the responsible committee on human experimentation.
The cases were from our family practice records, or case histories and records submitted from individuals who utilized our books and website to follow the dietary approach. If the patient was not seen in recent years, they were contacted by a registered nurse to corroborate and update details. The case histories presented were chosen based on their cardiovascular medical history of informative significance. Several of the cases were also chosen because of the long-term follow-up data available from our records, a few from 10 to 20 years ago, who have continued to remain patients, demonstrating long-term outcomes and clinical significance utilizing this approach.
Results
Survey Results
Participants’ ages ranged from 28 to 84. They were 91% Caucasian and 65% female. The average time utilizing this dietary approach of the responders was 3.8 years. Out of the 2273 individuals who completed the survey, 1303 (57%) reported adhering to the NDPR diet by 90% or more, 445 (20%) were 80% to 89% adherent, and 514 (23%) were less than 80% adherent. The data below excludes those whose adherence was less than 80%.
Weight Loss
There were 685 individuals that had a pre-intervention BMI greater than 30 kg/m2, and for this entire group the average weight loss at 1 year was 49 pounds (see Table 1). Only 75 of these individuals had data that were available for 3 years or more. These 75 lost an average of 49.3 ± 3.6 (P < .001) pounds at 1 year, and that degree of weight loss was maintained through years 2 and 3. The average weight loss at 2 years was 53.7 ± 3.9 pounds (P < .001), and at year 3, the average weight loss was 55.2 ± 4.0 pounds (P < .001). There were 310 individuals whose prediet weight had a BMI between 25 and 30 kg/m2 had an average 1-year weight loss of 14.4 ± 0.7 (P < .001) pounds, which on the average was maintained through years 2 and 3.
Table 1.
Weight Loss Results.
| BMI > 30 (N = 75) | BMI 25-30 (N = 310) | |
|---|---|---|
| Before | 225 | 149 |
| 1 Year | 175 | 134 |
| 2 Years | 171 | 134 |
| 3 Years | 169 | 135 |
| Average weight loss = 55.2 lbs | Average weight loss = 14 lbs |
Abbreviation: BMI, body mass index.
Blood Pressure
There were 443 respondents who were diagnosed with hypertension; this total included those who were on medication, never on medication, and those that discontinued their medication after the dietary intervention was initiated (see Table 2). The pre and post results represent an average of 1-year duration of dietary intervention. The 443 respondents reduced their systolic blood pressure by 26.4 ± 1.0 mm Hg (P < .001, 95% confidence interval [CI] = 1.95) and their diastolic blood pressure by 14.7 ± 0.6 mm Hg (P < .001, 95% CI = 1.14). Isolating the 127 individuals not on blood pressure–lowering medication at the start had their total systolic blood pressure dropped 27.8 ± 2.1 mm Hg (P < .001, 95% CI = 4.14) and their diastolic blood pressure dropped 15.8 ± 1.1 mm Hg (P < .001, 95% CI = 2.07). The 136 individuals whose blood pressure medications were stopped during the dietary intervention had an average reduction in systolic blood pressure of 28.6 ± 1.5 mm Hg (P < .001, 95% CI = 3.01) and diastolic blood pressure of 22.0 ± 6.1 mm Hg (P < .001, 95% CI = 11.88).
Table 2.
Blood Pressure Results.
| Total (N = 443) | No Medication (n = 127) | Discontinued Medication (n = 136) | Remained on Medication (n = 180) | |
|---|---|---|---|---|
| Before systolic | 147 | 149 | 149 | 144 |
| After systolic | 121 | 121 | 120 | 122 |
| Difference | 26.4 | 27.8 | 28.6 | 21.8 |
| Before diastolic | 89 | 90 | 97 | 87 |
| After diastolic | 74 | 74 | 75 | 74 |
| Difference | 14.7 | 15.8 | 11.9 | 13.2 |
Of note is also the number of people whose blood pressure medications were not discontinued. This may reflect some who still require medication, or it may reveal individuals who have earned a reduction or discontinuation of medication, but did not have physician contact to reduce or discontinue the medications or whose physician did not recognize a dose reduction was indicated. In this group of 180, the systolic blood pressure dropped 21.8 ± 1.5 mm Hg (P < .001, 95% CI = 2.98) on the average and the diastolic blood pressure dropped 13.2 ± 1.0 mm Hg (P < .001, 95% CI = 2.04). However, the average final blood pressure was 122/74 mm Hg, indicating that these subjects were potentially eligible for medication cessation but continued pharmacological treatment.
Serum Lipids
LDL cholesterol levels dropped dramatically as predicted by prior studies of this dietary portfolio.16 The pre and post results represent and average of 1-year duration of dietary intervention (see Table 3). In the 328 participants not taking cholesterol-lowering medications, the average LDL cholesterol level dropped from an average of 170.5 ± 3.1 mg/dL (P < .001) to 128.3 ± 2.3 mg/dL (P < .001), an average drop of 42.2 ± 2.3 mg/dL (P < .001, 95% CI = 4.57). The 69 individuals on statins experienced an LDL cholesterol decrease of 48.3 ± 6.5 mg/dL (P < .001, 95% CI = 12.69), from a baseline of 146.8 ± 8.3 mg/dL (P < .001) to a final reading of 98.6 ± 5.1 mg/dL (P < .001). Only 7 individuals discontinued their statins after the dietary intervention, and the average rise in LDL cholesterol was 15.7 ± 27.9 mg/dL (ns).
Table 3.
Low-Density Lipoprotein (LDL) Cholesterol and Triglycerides Results.
| LDL | No Medication (n = 328) | On Medication (n = 69) | Discontinued Medication (n = 7) |
|---|---|---|---|
| Before | 171 | 147 | NS |
| After | 128 | 99 | NS |
| Difference | 42.2 | 48.3 | |
| Triglycerides | No Medication (n = 166) | On Medication (n = 16) | Discontinued Medication (n = 33) |
| Before | 205 | 218 | 239 |
| After | 126 | 141 | 132 |
| Difference | 79.5 | 77.1 | 106.6 |
Of the 166 individuals not on statins, triglyceride levels dropped an average of 79.5 ± 7.2 mg/dL (P < .001, 95% CI = 14.14) from a baseline of 205.5 ± 8.0 mg/dL (P < .001) to 126.0 ± 4.6 mg/dL (P < .001). Thirty-three individuals discontinued their statins, with an average lowering of triglycerides of 106.6 ± 19.0 mg/dL (P < .001, 95% CI = 37.26), from a baseline of 238.5 ± 19.0 mg/dL (P < .001) to 132.0 ± 11.2 mg/dL (P < .001). Sixteen people continued their statin medications, and the average triglyceride level reduction in this group was 77.1 ± 26.7 mg/dL (P < .05, 95% CI = 52.33), from 217.7 ± 28.9 mg/dL (P < .05) at baseline to 140.6 ± 15.8 mg/dL (P < .05).
Eight Selected Case Histories
Case 1
A 48-year-old male had a past medical history significant for obesity, alcohol abuse, and CAD. He was 6’0” tall, and since his home weight scale only went up to 300 pounds, his starting weight was at least 300 pounds, putting him in the morbidly obese category with a BMI of >40 kg/m2. After having a 4-vessel coronary artery bypass graft in September 2005, the patient resumed his poor diet, along with smoking 2 to 3 packs per day, and occasional binge drinking. In July 2008, the patient awoke with severe angina, which subsequently resulted in the placement of 3 non-drug-eluding cardiac stents in one of the coronary arteries that had not been bypassed. Shortly after the procedure, he continued with severe angina experienced at the slightest exertion and was unable to work. His medication list included metoprolol succinate XL 200 mg daily, irbesartan 300 mg once daily, atorvastatin 20 mg once daily, clopidogrel bisulfate 75 mg once daily, and aspirin 325 mg once daily. He had a poor prognosis and was forced to be sedentary, secondary to angina even on minimal walking.
He adopted a nutritarian diet-style that he learned about via an Internet search. He also quit smoking. He received further guidance via website forums and discussion groups. He lost 35 pounds in the first month and 47 pounds in 9 weeks. At this point, his angina improved dramatically, but he still had morning angina symptoms with mild exertion that resolved during the day. After 6 months, he had lost 100 pounds and had no further angina symptoms, even with exercise. At that time, he had stopped all medications other than aspirin 81 mg daily. After 1 year, his weight, lipid parameters, glucose concentration, and blood pressure were dramatically lower (see Table 4).
Table 4.
Case 1 Summary Results.
| Parameters | July 2008 | July 2009 |
|---|---|---|
| Weight (lbs) | 300+ | 160 |
| Blood pressure (mm Hg) | 161/110 | 110/68 |
| Total cholesterol (mg/dL) | 270 | 120 |
| Low-density lipoprotein (mg/dL) | 148 | 75 |
| Triglyceride (mg/dL) | 300+ | 63 |
| Fasting glucose (mg/dL) | 100-120 | 80-90 |
| Medication | Irbesartan 300 mg qd; metoprolol succinate XL 200 mg qd; atorvastatin 20 mg qd; clopidogrel bisulfate 75 mg qd; aspirin 81 mg qd | None |
During year 1, he gradually regained his ability to exercise, and by the end of the year he was able to exercise fully, without angina and irregular palpitations. He also stopped smoking and binge alcohol use. Now, 5 years later, he maintains his superior health without any medications or further cardiac symptoms.
Case 2
A 60-year-old male with no significant past medical history was following a diet style for 10 years that included vegetables, fruits, whole grains, olive and flax oil, butter, salmon, and chicken. He was 5’7” tall with a weight of 155 pounds, and his BMI was 24 kg/m2, placing him in the “normal weight” category. In March 2006, he began a power walking exercise program and experienced exertional chest pain. A visit to the cardiologist office revealed a normal physical exam, electrocardiogram, echocardiogram, and a lipid panel showing an LDL concentration of 126 mg/dL, HDL concentration of 39 mg/dL, and a triglyceride concentration of 80 mg/dL. In June 2006, the patient had a positive thallium exercise stress test and a computed tomography (CT) angiogram, which revealed multifocal disease in the left anterior descending artery with low-density obstructive plaque. The patient was started on aspirin 81 mg and clopidogrel bisulfate 75 mg daily, but declined a statin medication. However, he did agree to niacin to reduce his Lp(a) levels. Starting in May 2006, the patient began following a nutritarian diet-style. After 3 months, the patient stopped experiencing exertional angina. In January 2007, all medications were discontinued by his primary physician, including niacin. The patient discontinued the aspirin on his own. Table 5 shows 1-year improved parameters.
Table 5.
Case 2 Summary Results.
| Parameters | June 2006 | June 2007 |
|---|---|---|
| Weight (lbs) | 155 | 135 |
| Waistline (in.) | 35 | 30.5 |
| Blood pressure (mm Hg) | 130/90 | 96/60 |
| Resting heart rate (bpm) | 72 | 55 |
| Low-density lipoprotein (mg/dL) | 126 | 63 |
| High-density lipoprotein (mg/dL) | 39 | 47 |
| Triglycerides (mg/dL) | 80 | 50 |
| Lp(a) (mg/dL) | 144 | 72 |
| Medication | Aspirin 81 mg qd; clopidogrel 75 mg qd; niacin 500 mg qd | None |
In June 2007, the patient also had a repeat CT angiogram revealing that the plaque in his left anterior descending (LAD) artery was now nonobstructive and had changed from low density to mixed density. In August 2008, the patient had an magnetic resonance angiogram showing a complete reversal of his coronary plaque, with no detectable disease, 2 years after beginning the NDPR diet. Now, 8 years later, he continues to be off all medications and angina-free.
Case 3
A 44-year-old male (6’0”, 216 pounds, BMI 29 kg/m2) with a history of hyperlipidemia was diagnosed with hypertension, with blood pressure measurements in the 140/90 mm Hg range. He also complained of night sweats and chest tightness on exertion for 6 to 12 months, as well as shortness of breath while exercising. At that time he did not seek medical attention and he refused to start antihypertensives and statins. Rather, he decided to commit to a nutritarian diet-style in August 2011. Over the next 2 months, he lost 35 pounds (181 pounds, BMI 24 kg/m2), and his blood pressure normalized to the 110/60 mm Hg range. His hyperlipidemia resolved with his total cholesterol decreasing from 216 to 161 mg/dL. Also, his night sweats, chest tightness, and shortness of breath resolved. Three years later, the patient continues to be symptom-free, has normal blood pressure and cholesterol, and does not take any medications.
Case 4
A 70-year-old female (5’10”, 240 pounds, BMI 34 kg/m2) with a history of hypertension, hypothyroidism, osteoarthritis, and low back pain had a history of angina while walking briskly or climbing stairs, for almost 10 years. She took valsartan 160 daily, hydrochlorothiazide 50 mg daily, atenolol 100 mg twice daily, rosuvastatin 20 mg daily, levothyroxine sodium 125 mg, potassium chloride 10 mEq daily, and aspirin 81 mg daily. Six months after starting a nutritarian diet-style in June 2012, she had lost 52 pounds (188 pounds, BMI 27). Her angina resolved, and she was able to walk and exercise at the gym without complaints. Her arthritis pains in her knees, ankles, and feet resolved as well. With a blood pressure of 119/59 mm Hg, she was able to discontinue her atenolol and is currently working with her physician to titrate off her valsartan and hydrochlorothiazide, whose dosages have been lowered already.
Case 5
A 53-year-old male with unstable angina for several months had never been evaluated by a medical provider and refused medical evaluations due to philosophical and religious reasons. Initially, he had complained of chest pressure with exertion but this had worsened over time, occurring even with minimal activity and then eventually even while at rest. At 5’10” with a weight of 183 pounds, his BMI was 26 kg/m2 and his blood pressure was 160/108 mm Hg. He was strongly advised to receive medical care urgently, but he refused. He did agree to adopt a nutritarian diet-style. Within 1 week of starting, his chest pain at rest (unstable angina) had resolved. After 2 to 3 weeks, he was able to walk a few blocks without experiencing chest pain. After 8 weeks, the patient was able to jog without symptoms. Moreover, after 12 weeks, the patient was able to do any amount of physical activity without any signs of angina. After 1 year, his weight remains at 154 pounds with a BMI of 22 kg/m2. His blood pressure is 112/75 mm Hg, and he continues to live without any angina symptoms in excellent health and continues to follow the nutritarian diet-style.
Case 6
A 60-year-old male (5’8”, 205 pounds, BMI 31 kg/m2) had a history of atrial fibrillation, hyperlipidemia, degenerative disc disease, and osteoarthritis. He also had chronic episodes of symptomatic atrial fibrillation during moderate exercise, with dizziness and fatigue. He complained of shortness of breath while climbing stairs and was unable to walk more than 15 minutes due to back pain. He had chronic indigestion requiring over-the-counter antacids at bedtime for the past 20 years. His medication list included metoprolol 100 mg twice daily, atorvastatin 20 mg daily, aspirin 81 mg, warfarin 5 mg, and fish oil 3 g daily.
In June 2012, the patient began a nutritarian diet-style. After a few weeks, he was able to discontinue his antacids. He lost 15 pounds in the first 7 weeks. By September 2012, he had lost 25 pounds. By March 2013, he weighed 168 pounds (BMI 25 kg/m2). His arthritis pains have resolved. His exercise tolerance has improved, allowing him to run stairs, cycle for 30 minutes, and lift weights without fatigue or shortness of breath. The patient’s episodes of atrial fibrillation have become very rare and without symptoms, allowing him to exercise without restriction, and he is not sure if they still occur. He has discontinued all his medications, except aspirin. His lipid profile and blood pressure have also improved significantly (see Table 6).
Table 6.
Case 6 Summary Results.
| Parameters | May 2012 | March 2013 |
|---|---|---|
| Weight (lbs) | 205 | 168 |
| Total cholesterol (mg/dL) | 226 | 188 |
| Low-density lipoprotein (mg/dL) | 156 | 119 |
| High-density lipoprotein (mg/dL) | 51 | 52 |
| Triglyceride (mg/dL) | 96 | 83 |
| Blood pressure (mm Hg) | 140/90 | 110/62 |
| Medication | Metoprolol 50 bid; atorvastatin 20 mg qd; warfarin 5 mg qd; aspirin 81 mg qd; fish oil 3 g qd | Aspirin 81 mg qd |
Case 7
A 72-year-old male presented with a history of CAD, seeking nutritional management of his angina. One month prior to presentation, in May 1994, the patient complained of chest pain radiating to bilateral arms while walking. He had a thallium stress test demonstrating multi-vessel CAD, and a cardiac catheterization documented with a demonstrated 95% stenosis of his LAD artery. He refused angioplasty and bypass surgery, requesting aggressive nutritional management. The patient was taking diltiazem 180 mg daily, aspirin 81 mg daily, and sublingual nitroglycerin as needed. With medication, his blood pressure was 136/64 mm Hg.
On his own, the patient had started a grain-based vegan diet prior to presenting to the office, which resulted in a 14 pound weight loss from 180 to 166 pounds, and his total cholesterol lowered from 240 to 218 with an LDL concentration of 146 mg/dL. His angina was already starting to improve. Two months after starting the nutritarian diet-style, the patient had lost an additional 14 pounds, lowering his blood pressure to 120/70 mm Hg on diltiazem, which was discontinued gradually, and his blood pressure remained favorable at future visits. In this short time, his chest pain resolved and he did not require any further sublingual nitroglycerin. His lipid profile also dramatically improved, with a total cholesterol of 177 mg/dL and LDL concentration of 107 mg/dL. His cardiologist supported his decision at this point to continue with nutritional management instead of angioplasty. In 2000, at the age of 78, he had a repeat exercise stress test that showed increased exercise tolerance, improved heart rate, improved blood pressure, and apparent regression of disease when compared with the previous stress test results. His lipid profile continued to decrease with total cholesterol concentration of 189 mg/dL and LDL concentration of 81 mg/dL. Now 20 years later, in his 90s, he has continued to be free of high cholesterol, high blood pressure, and angina, and he has remained medication-free in good health.
Case 8
A 63-year-old female (5’2”, 205 pounds, BMI 37.5 kg/m2) had a history of CAD, migraines, and polycythemia. The patient presented in 2003 for nutritional management of her persistent angina that occurred with the slightest exertion, making it difficult for her to ambulate. She was essentially homebound and in a wheelchair. >From 1999 to 2000, the patient suffered from 3 myocardial infarctions and underwent 5 angioplasties. She had one stent placed, which became occluded 3 months later. She took clopidogrel bisulfate 75 mg daily and aspirin 81 mg daily, verapamil 120 mg twice daily, sublingual nitroglycerin, acetaminophen and hydrocodone for migraines, lorazepam for anxiety, and hydroxyurea for polycythemia. Her blood pressure was 125/80 mm Hg on medication. Within the first 3 months after starting the nutritarian diet-style, she had lost 32 pounds, decreasing from 205 to 174 pounds. Her angina had almost resolved, and she was able to walk 2 miles without suffering any angina symptoms. Seven months after starting the diet, she had lost 90 pounds and was completely angina-free. Now, over 10 years later, she has remained chest-pain-free, without angina or any further cardiac symptoms. She requires no medications for high blood pressure, migraines, or anxiety, and her LDL cholesterol concentration remains around 65 mg/dL without medications.
Discussion
This study presents the surveyed data and medical records from people variably adherent to a NDPR diet from a 2-physician family practice, recommending the NDPR diet-style for more than 20 years. Though compliance and recruitment with such an aggressive dietary program can be an issue, those patients who were informed and motivated sufficiently to make these lifestyle modifications demonstrated impressive results in arresting and reversing cardiovascular risk factors and symptomatic atherosclerosis. The illustrated cases represented both short-term improvements noted in a relatively rapid fashion and more long-term benefits that were retained even into advanced years, for people remaining compliant with this diet-style. These data support the view that eating fruits, vegetables, beans, nuts, and seeds is generally recognized as healthy, but the size of the effect is staggering when increased to comprise the vast majority of calories consumed.
These data also support the epidemiological and interventional studies documenting the beneficial effects from utilizing nuts, and seeds in the diet as a source of fat, at the expense of oils and animal fats. An almost identical dietary approach studied over a 6-week period by Jenkins et al18 examined the impact of these dietary components and found that, compared to the American Heart Association low-fat diet and a grain-based vegan diet, a high-fiber vegetable diet with beans, seeds, and nuts resulted in significantly greater LDL reduction (33%) with no unfavorable changes to serum HDL or triglycerides. The effect of this high-fiber, vegetable diet on (high-sensitivity) C-reactive protein and homocysteine levels was found to be more profound than the change induced by statins in another study by the same research center.21 The results of this approach has also been reported in a pilot study of diabetes patients with dramatically favorable results, and a larger controlled trial is beginning shortly.22
The effectiveness of this approach corroborates the many studies indicating a reduction in CAD mortality from the inclusion of these fat-rich whole foods.23-25 In addition to providing fiber, protein, phytosterols, antioxidants, vitamins, and minerals, nuts and seeds are also a source of beneficial fatty acids, which enhance phytochemical and antioxidant absorption from other foods. At least 5 large prospective studies (the Adventist Health Study, the Iowa Women Health Study, the Nurses’ Health Study, the Physicians’ Health Study, and the CARE Study) have found an inverse association between nut consumption and the risk of CAD. Nuts have been found to reduce cholesterol and inflammatory markers, improve insulin sensitivity and endothelial function, and reduce the risk of sudden cardiac death and infarction.26-30 As calories from fruits, vegetables, beans, mushrooms, whole grains, nuts, and seeds increase in one’s diet, animal product calories are typically reduced accordingly. Apparently, it is the combination of increased plants with decreased animal products that synergistically offers the highest degree of protection/effect.
One of the similarities with the NDPR diet-style and others with documented cardiovascular benefits is the cautious use of oils, because of their caloric density. More olive oil in the diet is associated with more weight gain and obesity.31 Even back in 1965, a study demonstrated that heart patients given olive oil and corn oil had a higher risk of heart attack and death rate than the control, lower-fat diet.32 Modern studies are inconsistent, confounded by replacement foods, but some have confirmed that more of these (omega-6) oils in the diet are associated with higher mortality from heart disease.33 Our recommendation is that oil should be omitted or carefully controlled, such as under a teaspoon a day (40 calories), not a tablespoon, as allowed in the standard DASH diet, since most patients with heart disease and metabolic syndrome are overweight too. It is logical to assume that dietary intervention will be most effective and protective if fats are limited to whole foods, such as seeds and walnuts, shown to offer significant mortality benefits when used as a fat source in place of oil.34 Using oils liberally, with the addition of seeds and nuts would be calorically unfavorable.
There are numerous weaknesses in this data. Primary is that those that chose to respond to a survey may selectively favor those who have achieved favorable results. Also, a voluntary response survey does not examine what percentage of people presented with this information would choose to follow this rigorous dietary approach. Only a randomized controlled trial can answer those questions. Nevertheless, this is not a study that accurately determines acceptability or percent willing to be compliant, but rather a preliminary study demonstrating efficacy with willing, properly educated, and motivated patients.
The survey results reported may also have a self-reporting bias. The validity of “self-reported” BMI, calculated from self-reported height and weight, has been assessed in several populations, including the Adventist Health Study 2, which has the closest demographics to the population studied here.35 They chose a representative sample of 911 individuals and compared measured height and weights with self-reported values. It was found that 0.2 kg underestimation of weight and a 1.6 overestimation of height. They concluded that self-reported weight and height data from a cohort of Adventists in the United States and Canada is valid enough to be used in epidemiological studies, although it can lead to some underestimation of obesity.
Conclusion
Over 25 years of experience as a primary care physician teaching and motivating the public utilizing these methods has demonstrated the consistent effectiveness of this approach for weight reduction to dramatically lower blood pressure, treat/reverse type 2 diabetes,22 and even help resolve food addictions.20
The relatively large number of participants makes these results important for demonstrating the beneficial response following an NDPR diet to ameliorate CVD. With proper information, motivation, and support, this study demonstrates the potential of this intervention to effect behavioral change with significant benefits. The dramatic beneficial results achieved by individuals utilizing this dietary approach further supported their long-term, sustained adherence.
Nutritional interventions show promising potential as prophylactic and adjunctive treatment modalities in CVD. Due to the widespread prevalence of this condition and its contribution to extensive morbidity, mortality, cost, and access-of-care in the United States and international health systems, further investigations on the preventative impact of aggressive dietary intervention on cardiometabolic and cardiovascular disease are warranted.
Footnotes
Authors’ Note: Dr Fuhrman is the author of books and other educational materials teaching the NDPR dietary intervention.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation. 2014;129:e28-e292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Fung TT, Schulze M, Manson JE, Willet WC, Hu FB. Dietary patterns, meat intake, and the risk of type 2 diabetes in women. Arch Intern Med. 2004;164:2235-2240. [DOI] [PubMed] [Google Scholar]
- 3. Schulze MB, Liu S, Rimm EB, Manson JE, Willett WC, Hu FB. Glycemic index, glycemic load, and dietary fiber intake and incidence of type 2 diabetes in younger and middle-aged women. Am J Clin Nutr. 2004;80:348-356. [DOI] [PubMed] [Google Scholar]
- 4. Liu S, Willett WC. Dietary glycemic load and atherothrombotic risk. Curr Atheroscler Rep. 2002;4:454-461. [DOI] [PubMed] [Google Scholar]
- 5. Mursu J, Virtanen JK, Rissanen TH, et al. Glycemic index, glycemic load, and the risk of acute myocardial infarction in Finnish men: the Kuopio Ischaemic Heart Disease Risk Factor Study. Nutr Metab Cardiovasc Dis. 2011;21:144-149. [DOI] [PubMed] [Google Scholar]
- 6. Sieri S, Krogh V, Berrino F, et al. Dietary glycemic load and index and risk of coronary heart disease in a large Italian cohort: the EPICOR study. Arch Intern Med. 2010;170:640-647. [DOI] [PubMed] [Google Scholar]
- 7. Wang X, Ouyang Y, Liu J, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2014;349:g4490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136:2588-2593. [DOI] [PubMed] [Google Scholar]
- 9. He FJ, Nowson CA, MacGregor GA. Fruit and vegetable consumption and stroke: meta-analysis of cohort studies. Lancet. 2006;367:320-326. [DOI] [PubMed] [Google Scholar]
- 10. Fuhrman B, Volkova N, Rosenblat M, Aviram M. Lycopene synergistically inhibits LDL oxidation in combination with vitamin E, glabridin, rosmarinic acid, carnosic acid, or garlic. Antioxid Redox Signal. 2000;2:491-506. [DOI] [PubMed] [Google Scholar]
- 11. Hadad N, Levy R. The synergistic anti-inflammatory effects of lycopene, lutein, β-carotene, and carnosic acid combinations via redox-based inhibition of NF-κB signaling. Free Radic Biol Med. 2012;53:1381-1391. [DOI] [PubMed] [Google Scholar]
- 12. Böhm F, Edge R, McGarvey DJ, Truscott TG. β-Carotene with vitamins E and C offers synergistic cell protection against NOx. FEBS Lett. 1998;436:387-389. [DOI] [PubMed] [Google Scholar]
- 13. Soory M. Nutritional antioxidants and their applications in cardiometabolic diseases. Infect Disord Drug Targets. 2012;12:388-401. [DOI] [PubMed] [Google Scholar]
- 14. Oyebode O, Gordon-Dseagu V, Walker A, Mindell JS. Fruit and vegetable consumption and all-cause cancer and CVD mortality: analysis of Health Survey for England data. J Epidemiol Community Health. doi: 10.1136/jech-2013-203500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Esselstyn CB, Jr, Gendy G, Doyle J, Golubic M, Roizen MF. A way to reverse CAD. J Fam Pract. 2014;63:256-264b. [PubMed] [Google Scholar]
- 16. Ornish D, Scherwitz LW, Billings JH. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280:2001-2007. [DOI] [PubMed] [Google Scholar]
- 17. Hu FB, Stampfer MJ. Nut consumption and risk of coronary heart disease: a review of epidemiologic evidence. Curr Atheroscler Rep. 1999;1:204-209. [DOI] [PubMed] [Google Scholar]
- 18. Jenkins DJ, Kendall CW, Popovich DG, et al. Effect of a very-high-fiber vegetable, fruit, and nut diet on serum lipids and colonic function. Metabolism. 2001;50:494-503. [DOI] [PubMed] [Google Scholar]
- 19. Sarter BS, Fuhrman J. Effect of a high nutrient density diet on long-term weight loss: a retrospective chart review. Altern Ther Health Med. 2008;14(3):48-53. [PubMed] [Google Scholar]
- 20. Fuhrman J, Sarter B, Glaser D, Acocella S. Changing perceptions of hunger on a high nutrient density diet. Nutr J. 2010;9:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jenkins DJ, Kendall CW, Marchie A, et al. Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA. 2013;290:502-510. [DOI] [PubMed] [Google Scholar]
- 22. Dunaief D, Fuhrman J, Dunaief J, Ying G. Glycemic and cardiovascular parameters improved in type 2 diabetes with the high nutrient density (HND) diet. Open J Prev Med. 2012;2:364-371. [Google Scholar]
- 23. Megias-Rangil I, Garcia-Lorda P, Torres-Moreno M, Bullo M, Salas-Salvado J. Nutrient content and health effects of nuts. Arch Latinoam Nutr. 2004;54:83-86. [PubMed] [Google Scholar]
- 24. Hu FB, Stampfer MJ, Manson JE, et al. Frequent nut consumption and risk of coronary heart disease in women: prospective cohort study. BMJ. 1998;317:1341-1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jiang R, Jacobs DR, Mayer-Davis E, et al. Nut and seed consumption and inflammatory markers in the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2006;163:222-231. [DOI] [PubMed] [Google Scholar]
- 26. Kendall CW, Esfahani A, Truan J, Srichaikul K, Jenkins DJ. Health benefits of nuts in prevention and management of diabetes. Asia Pac J Clin Nutr. 2010;19:110-116. [PubMed] [Google Scholar]
- 27. Kendall CW, Josse AR, Esfahani A, Jenkins DJ. Nuts, metabolic syndrome and diabetes. Br J Nutr. 2010;104:465-473. [DOI] [PubMed] [Google Scholar]
- 28. Kris-Etherton PM, Hu FB, Ros E, Sabate J. The role of tree nuts and peanuts in the prevention of coronary heart disease: multiple potential mechanisms. J Nutr. 2008;138:1746S-1751S. [DOI] [PubMed] [Google Scholar]
- 29. Martinez-Gonzalez MA, Bes-Rastrollo M. Nut consumption, weight gain and obesity: epidemiological evidence. Nutr Metab Cardiovasc Dis. 2011;21(suppl 1):S40-S45. [DOI] [PubMed] [Google Scholar]
- 30. Sabate J, Ang Y. Nuts and health outcomes: new epidemiologic evidence. Am J Clin Nutr. 2009;89:1643S-1648S. [DOI] [PubMed] [Google Scholar]
- 31. Calle-Pascual AL, Saavedra A, Benedi A, et al. Changes in nutritional pattern, insulin sensitivity and glucose tolerance during weight loss in obese patients from a Mediterranean area. Horm Metab Res. 1995;27:499-502. [DOI] [PubMed] [Google Scholar]
- 32. Rose GA, Thompson WB, Williams RT. Corn oil treatment of ischaemic heart disease. BMJ. 1965;1:1531-1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ramsden CE, Zamora D, Leelarthaepin B, et al. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. BMJ. 2013;346:e8707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Guasch-Ferré M, Bulló M, Martínez-González MÁ, et al. Frequency of nut consumption and mortality risk in the PREDIMED nutrition intervention trial. BMC Med. 2013;11:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bes-Rastrollo M, Sabate J, Jaceldo-Siegl K, Fraser GE. Validation of self-reported anthropometrics in the Adventist Health Study 2. BMC Public Health. 2001;11:213. [DOI] [PMC free article] [PubMed] [Google Scholar]