In this retrospective study of 285 patients receiving outpatient parenteral antibiotic therapy (OPAT), the duration of antibiotic, use of double-lumen catheters, and receipt of penicillin G and cloxacillin appeared to increase the risk of peripherally inserted central catheter (PICC) occlusion. Physicians should consider these factors when prescribing long-term antibiotic therapy.
KEYWORDS: peripherally inserted central catheter, outpatient parenteral antimicrobial therapy, occlusion
ABSTRACT
In this retrospective study of 285 patients receiving outpatient parenteral antibiotic therapy (OPAT), the duration of antibiotic, use of double-lumen catheters, and receipt of penicillin G and cloxacillin appeared to increase the risk of peripherally inserted central catheter (PICC) occlusion. Physicians should consider these factors when prescribing long-term antibiotic therapy. Further studies are needed to evaluate methods to reduce PICC occlusion, particularly when double-lumen PICCs are necessary and when cloxacillin or penicillin G are the preferred treatment.
TEXT
Peripherally inserted central catheter (PICC) occlusions are a frequently encountered complication, resulting in treatment interruptions, hospital visits, and catheter replacements (1). We conducted a retrospective cohort study to identify the factors associated with PICC occlusion in the outpatient parenteral antibiotic therapy (OPAT) setting.
Sunnybrook Health Sciences Centre is a 627-bed academic health sciences center located in Toronto, Ontario, Canada. Patients undergo PICC insertion in the interventional radiology department via ultrasound and fluoroscopy. Lumen selection was left to the discretion of the ordering physician up until 21 February 2017, at which point all PICCs ordered for inpatients in noncritical care units were defaulted to single lumen in the absence of an appropriate indication (two long-term intravenous antibiotics, total parenteral nutrition, intravenous chemotherapy, or use in medical assistance in dying). Prior to discharge, the patients are referred to the institutional OPAT clinic for follow-up. Outpatient antibiotic administration and PICC care are coordinated by local health integration networks, either through an infusion clinic, or by a nurse at home. The catheter care protocol includes flushes with normal saline once daily.
A retrospective review was conducted from 1 June 2016 to 31 October 2017 of patients discharged with a PICC for antibiotic therapy and seen in an OPAT clinic for follow-up. Patient, PICC, antibiotic, and occlusion information were collected from the electronic health record. Occlusion was defined as the inability to infuse medication through the PICC in the absence of line malposition or intraluminal administration of alteplase. Only the first course of intravenous antibiotic therapy per patient was included. PICCs inserted for nonadmitted patients and inpatients admitted to critical care units were excluded. Research ethics board approval was obtained.
A bivariate analysis was conducted to determine the association of each variable with PICC occlusion. Wilcoxon signed-rank tests and chi-square tests (or Fisher's exact tests) were used to assess continuous and categorical variables, respectively. A multivariable logistic regression analysis was used to identify factors associated with PICC occlusion and included the following prespecified variables: age, sex, comorbidities (active malignancy, current tobacco use, venous thromboembolic history, diabetes, and obesity), PICC characteristics (lumen number and side of insertion), and intravenous antibiotic (type and duration). The analysis was performed using R statistical software version 3.4.3 (Foundation for Statistical Computing, Vienna, Austria).
Over 17 months, 285 patients were discharged from the hospital with a PICC for antibiotic therapy. The most commonly treated infections were osteomyelitis (107/285 [37.5%]), septic arthritis (34/285 [11.9%]), and Staphylococcus aureus bacteremia (31/285 [10.9%]). The most commonly administered antibiotics were vancomycin (24.9%), cefazolin (22.5%), and ceftriaxone (22.5%). Of the 285 patients, 79 (27.7%) developed a PICC occlusion. Most PICC occlusions (57/79 [72.2%]) occurred after hospital discharge, prompting 23 emergency department visits and 20 catheter replacements. In the 70 occlusion events where the specific time of occlusion was available, the median (interquartile) time to occlusion from insertion was 14.5 (7 to 27) days.
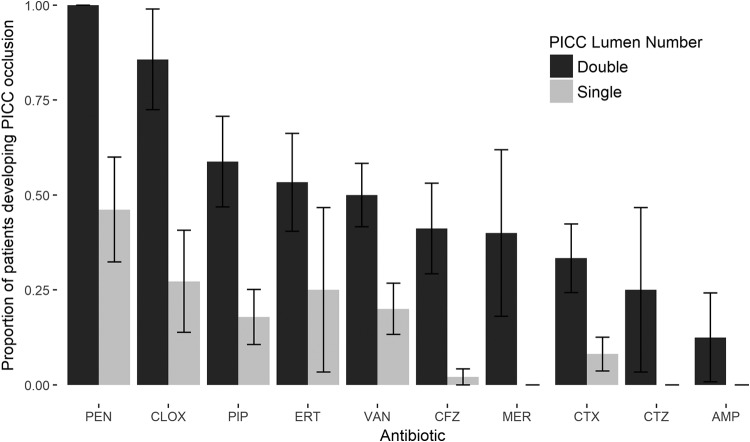
In the bivariate analysis, a longer antibiotic duration (5.7 versus 5.3 weeks, P = 0.01), use of a double-lumen PICC compared to single-lumen PICC (50.0% versus 12.9%, respectively; P < 0.001), and use of penicillin G compared to other antibiotics (61.1% versus 25.5%, respectively; P = 0.002) were associated with an increased occlusion risk (Table 1). In the multivariable logistic regression analysis, the duration of antibiotic (adjusted odds ratio [aOR], 1.25 per week of therapy; 95% confidence interval [CI], 1.06 to 1.47; P = 0.009), use of a double-lumen PICC (aOR, 11.33; 95% CI, 5.45 to 24.25; P < 0.0001), use of cloxacillin (aOR, 5.91; 95% CI, 1.04 to 33.64; P = 0.045) and penicillin G (aOR, 11.45; 95% CI, 2.10 to 63.38; P = 0.005) were associated with increased occlusion risk (Table 1). The proportions of patients developing PICC occlusions stratified by antibiotic and lumen numbers are summarized in Fig. 1.
TABLE 1.
Patient and treatment characteristics associated with occlusion of peripherally inserted central catheters
| Characteristic | No. (%) or median (IQR) |
Multivariable logistic regression analysis |
||||
|---|---|---|---|---|---|---|
| Total (n = 285) | Bivariate analysis |
|||||
| No occlusion (n = 206) | Occlusion (n = 79) | P value | Adjusted odds ratio (95% CI) | P value | ||
| Age (yrs) | 65 (51–73) | 66 (51–74) | 63 (52–71) | 0.44 | 1.01 (0.98–1.03) | 0.64 |
| Sex | ||||||
| Male | 170 (59.6) | 129 (62.6) | 41 (51.9) | Reference | 0.42 (0.20–0.90) | 0.03 |
| Female | 115 (40.4) | 77 (37.4) | 38 (48.1) | 0.13 | ||
| Current tobacco use | 52 (18.2) | 35 (17.0) | 17 (21.5) | 0.48 | 2.03 (0.80–5.17) | 0.14 |
| Active malignancy | 42 (14.7) | 30 (14.6) | 12 (15.2) | 1.00 | 1.07 (0.42–2.73) | 0.88 |
| Diabetes | 89 (31.2) | 63 (30.6) | 26 (32.9) | 0.81 | 1.09 (0.48–2.49) | 0.83 |
| Obesity | 54 (18.9) | 36 (17.5) | 18 (22.8) | 0.39 | 1.21 (0.49–3.02) | 0.68 |
| VTEa history | 15 (5.3) | 13 (6.3) | 2 (2.5) | 0.25 | 0.39 (0.07–2.10) | 0.14 |
| PICCb site of insertion | ||||||
| Right | 40 (14.0) | 27 (13.1) | 13 (16.5) | Reference | 1.78 (0.68–4.75) | 0.24 |
| Left | 245 (86.0) | 179 (86.9) | 66 (83.5) | 0.59 | ||
| No. of lumina for PICC | ||||||
| 1 | 171 (60.0) | 149 (72.3) | 22 (27.8) | Reference | ||
| 2 | 114 (40.0) | 57 (27.7) | 57 (72.2) | <0.001 | 11.33 (5.45–24.25) | <0.0001 |
| Antibiotic duration (wks) | 5.4 (4.0–6.1) | 5.3 (3.6–6.1) | 5.7 (4.9–6.4) | 0.01 | 1.25 (1.06–1.47) | 0.009 |
| No. of antibiotics | ||||||
| 1 | 247 (86.7) | 181 (87.9) | 66 (83.5) | Reference | ||
| 2 | 38 (13.3) | 25 (12.1) | 13 (16.5) | 0.44 | ||
| Antibiotic | ||||||
| Ampicillin | 11 (3.9) | 10 (4.9) | 1 (1.3) | 0.30 | 0.13 (0.01–1.39) | 0.09 |
| Cefazolin | 64 (22.5) | 56 (27.2) | 8 (10.1) | 0.001 | 0.47 (0.11–2.00) | 0.31 |
| Ceftazidime | 9 (3.2) | 8 (3.9) | 1 (1.3) | 0.45 | 0.12 (0.01–1.51) | 0.10 |
| Ceftriaxone | 64 (22.5) | 52 (25.2) | 12 (15.2) | 0.08 | 0.64 (0.18–2.19) | 0.47 |
| Cloxacillin | 18 (6.3) | 9 (4.4) | 9 (11.4) | 0.05 | 5.91 (1.04–33.64) | 0.045 |
| Ertapenem | 19 (6.7) | 10 (4.9) | 9 (11.4) | 0.06 | 1.00 (0.22–4.57) | 1.00 |
| Meropenem | 9 (3.2) | 7 (3.4) | 2 (2.5) | 1.00 | 0.33 (0.04–2.73) | 0.31 |
| Penicillin G | 18 (6.3) | 7 (3.4) | 11 (13.9) | 0.002 | 11.55 (2.10–63.38) | 0.005 |
| Piperacillin-tazobactam | 45 (15.8) | 30 (14.6) | 15 (19.0) | 0.37 | 1.74 (0.41–7.45) | 0.46 |
| Vancomycin | 71 (24.9) | 46 (22.3) | 25 (31.6) | 0.13 | 1.75 (0.62–4.97) | 0.29 |
VTE, venous thromboembolism.
PICC, peripherally inserted central catheter.
FIG 1.
Proportions of patients developing PICC occlusions stratified by lumen number and antibiotic. Error bars represent the standard errors. PEN, penicillin G; CLOX, cloxacillin; PIP, piperacillin-tazobactam; ERT, ertapenem; VAN, vancomycin; CFZ, cefazolin; MER, meropenem; CTX, ceftriaxone; CTZ, ceftazidime; AMP, ampicillin.
In patients with single-lumen PICCs, changing from cloxacillin to cefazolin could result in a potential absolute risk reduction (ARR) in occlusions of 25.1% (27.2% versus 2.1%, respectively; number needed to treat [NNT], 4). Similarly, changing from penicillin G to ceftriaxone could result in a potential ARR of 38.0% (46.1% versus 8.1%, respectively; NNT, 2.6).
We identified several modifiable factors associated with increased PICC occlusion risk. The use of double-lumen PICCs (compared to single-lumen PICCs) was associated with an increased risk of occlusion. This finding highlights the importance of choosing the minimum number of lumina required for antibiotic administration. Interventions aimed at optimizing single-lumen PICC use have successfully reduced PICC-related complications (2–4). Second, the use of intravenous cloxacillin and penicillin G was associated with an increased risk of occlusion. This risk was not inconsequential, as our data suggest that for every four patients prescribed cefazolin instead of cloxacillin, and for every 2.6 patients prescribed ceftriaxone instead of penicillin G, one PICC occlusion might be avoided. Although cloxacillin has been identified by nursing experts as an antibiotic likely to cause occlusion (5), there is a paucity of data quantifying this risk. One other study compared the risk of occlusion for three different antibiotics (piperacillin-tazobactam, cefepime, and vancomycin) and identified similar risks for all three (6). We suspect that cloxacillin and penicillin G form a greater antibiotic precipitate within the catheter lumen, resulting in an increased occlusion risk. If this hypothesis is true, interventions to reduce antibiotic precipitation should be explored, such as modifying antibiotic reconstitution techniques, infusion times, and catheter flushing protocols.
These findings have important implications for antibiotic selection in certain clinical scenarios in the OPAT setting. For example, the lower risk of PICC occlusion with cefazolin than with cloxacillin may favor the outpatient use of cefazolin for S. aureus bacteremia. Two retrospective studies have suggested improved safety with cefazolin compared to that with antistaphylococcal penicillins but did not account for PICC-related complications (7, 8). Likewise, the use of ceftriaxone instead of penicillin G for the treatment of endocarditis caused by highly penicillin-susceptible viridans group streptococci may result in fewer PICC occlusions, but this should be weighed against the potential harms of selecting a broader-spectrum agent, such as Clostridium difficile infection (9).
There are several limitations to our study. First, the single-center nature of this study may influence the generalizability of these results to other OPAT treatment models. Second, occlusion risk could not be evaluated for antibiotics marketed outside Canada, such as other antistaphylococcal penicillins (flucloxacillin, oxacillin, and nafcillin). Finally, it is possible that other confounding variables influencing occlusion risk were unaccounted for in this study.
The duration of the antibiotic, the use of double-lumen catheters, and the receipt of penicillin G and cloxacillin appear to increase the risk of PICC occlusion in the OPAT setting. Physicians should consider these factors when prescribing long-term antibiotic therapy. Further studies are needed to evaluate methods to reduce PICC occlusion, particularly when double-lumen PICCs are necessary and when cloxacillin or penicillin G is the preferred treatment.
ACKNOWLEDGMENTS
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sector.
None of the authors have any relevant conflicts of interest to disclose.
REFERENCES
- 1.Moureau N, Poole S, Murdock MA, Gray SM, Semba CP. 2002. Central venous catheters in home infusion care: outcomes analysis in 50,470 patients. J Vasc Interv Radiol 13:1009–1016. doi: 10.1016/S1051-0443(07)61865-X. [DOI] [PubMed] [Google Scholar]
- 2.O'Brien J, Paquet F, Lindsay R, Valenti D. 2013. Insertion of PICCs with minimum number of lumens reduces complications and costs. J Am Coll Radiol 10:864–868. doi: 10.1016/j.jacr.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Swaminathan L, Flanders S, Rogers M, Calleja Y, Snyder A, Thyagarajan R, Bercea P, Chopra V. 2018. Improving PICC use and outcomes in hospitalised patients: an interrupted time series study using MAGIC criteria. BMJ Qual Saf 27:271–278. doi: 10.1136/bmjqs-2017-007342. [DOI] [PubMed] [Google Scholar]
- 4.Lam PW, Volling C, Chan T, Wiggers JB, Castellani L, Wright J, Peckham K, Shadowitz S, Tasker S, MacFadden DR, Daneman N, Gold WL, Pugash R, Leis JA. 9 April 2018. Impact of defaulting to single lumen peripherally inserted central catheter on patient outcomes: an interrupted time series study. Clin Infect Dis doi: 10.1093/cid/ciy301. [DOI] [PubMed] [Google Scholar]
- 5.Hill J, Broadhurst D, Miller K, Cook C, Dumanski J, Friesen N, Karrei I, Logan R, Paquet F, Pittendreigh L, Whynot A. 2013. Occlusion management guideline for central venous access devices. Vasc Access 7:22. [Google Scholar]
- 6.Smith SN, Moureau N, Vaughn VM, Boldenow T, Kaatz S, Grant PJ, Bernstein SJ, Flanders SA, Chopra V. 2017. Patterns and predictors of peripherally inserted central catheter occlusion: the 3P-O study. J Vasc Interv Radiol 28:749.e2–756.e2. doi: 10.1016/j.jvir.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Youngster I, Shenoy ES, Hooper DC, Nelson SB. 2014. Comparative evaluation of the tolerability of cefazolin and nafcillin for treatment of methicillin-susceptible Staphylococcus aureus infections in the outpatient setting. Clin Infect Dis 59:369–375. doi: 10.1093/cid/ciu301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J, Echevarria KL, Hughes DW, Cadena JA, Bowling JE, Lewis JS II. 2014. Comparison of cefazolin versus oxacillin for treatment of complicated bacteremia caused by methicillin-susceptible Staphylococcus aureus. Antimicrob Agents Chemother 58:5117–5124. doi: 10.1128/AAC.02800-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown KA, Khanafer N, Daneman N, Fisman DN. 2013. Meta-analysis of antibiotics and the risk of community-associated Clostridium difficile infection. Antimicrob Agents Chemother 57:2326–2332. doi: 10.1128/AAC.02176-12. [DOI] [PMC free article] [PubMed] [Google Scholar]