Abstract
Objective:
To evaluate the blood pressure (BP) effects of a yearlong e-health solution designed to interrupt prolonged occupational sitting time.
Methods:
BP data of 228 desk-based employees (45.1 ± 10.5 years) were analyzed at baseline, 3, 6, 9, and 12 months.
Results:
Systolic BP significantly reduced from baseline for the first 9 months (1.0 to 3.4 mmHg; P < 0.01) while diastolic and mean arterial pressure decreased for the full 12-months (4 to 5 mmHg for diastolic pressure and 3.6 to 4.2 mmHg for MAP; all P < 0.01).
Participants used the e-health solution 5.5 ± 2.0 times/day in the first 3 months which reduced to 4.2 ± 2.5 times/day by the end of the study (P < 0.05).
Conclusions:
An e-health solution designed to increase non-exercise physical activity by interrupting sitting time in the workplace is feasible and produced long-term reductions in blood pressure.
Keywords: e-health, hypertension, preventative medicine, public health, workplace health
Daily sitting is ubiquitous for the majority of desk-based employees. In recent decades the number of work tasks that can be performed while sitting at a workstation has increased markedly,1 contributing to the absence of regular movement throughout the workday. It is estimated that desk-based employees are exposed to work-based norms (ie, computer use) which cause them to sit on average 80,000 hours over their working life.2–4 Most of this sitting behavior is performed for prolonged uninterrupted periods of time exceeding 30 minutes.5–7 Thus, there is a confluence of factors which contribute to adverse health for desk-based workers, prolonged sitting and an increasingly sedentary-based workplace. This is problematic because it contributes to the public health concern of cumulative sedentary behavior.
Time spent sitting is positively associated with premature all-cause and cardiovascular disease mortality and elevated biomarkers of cardiometabolic risk, including waist circumference, serum triglycerides, and blood glucose.8–11 Sedentary behaviors are also associated with high resting blood pressure, adiposity, and aging.12–14 These adverse health outcomes from regular and consistent sedentary behavior might be independent of moderate-to-vigorous physical activity.15 Therefore, exclusively meeting recommended physical activity guidelines through traditional exercise might be insufficient to counteract the detrimental effects of prolonged sitting.
A potential solution advocated by a number of researchers16,17 is to reintroduce non-exercise physical activity (NEPA) back into the workday.18,19 This could be in the form of standing (eg, while talking on the phone) or slow/normal paced walking (eg, a walking meeting). For example, desk-based employees who interrupted their sitting every 20 minutes by engaging in light intensity walking over a month experienced a decrease in blood pressure.20 Despite advocacy for the implementation of NEPA into the workday,21 to date research on its impact on cardiometabolic risk has been reported for periods of less than 6 months, an insufficient timeframe to reflect meaningful behavior change.22 In the field, researchers have utilized prompting protocols to influence sedentary behavior change in the workplace.5,23 More recently, researchers utilized the very equipment that contributes to prolonged sitting, the computer, to prompt desk-based workers every 45 minutes during the workday to increase NEPA during work hours.24 In a field-based randomized controlled trial, desk-based workers, who were exposed to an e-health solution designed to interrupt prolonged occupational sitting showed a reduction (>10 mmHg) in mean arterial pressure (MAP) over a 13-week period.25 These participants self-reported interrupting their sitting time with an average of 8 minutes of NEPA per workday when prompted at hourly intervals. Moreover, the benefit of using regular computer prompts to encourage participants to complete their choice of short duration NEPA throughout the workday did not require specialized equipment and promoted adherence because it redefined participants’ perceptions of beneficial exercise.26
The current study builds upon this previous research with the primary aim to determine any changes in blood pressure due to participation in an e-health solution designed to interrupt sitting time by prompting employees to engage in NEPA movement breaks over a 12-month period. The secondary aim was to determine the impact of the intervention for those people with clinically elevated blood pressure results at baseline. Feasibility of this e-health solution was also investigated in terms of adherence over the yearlong trial period.
METHOD
Study Design and Setting
As part of an overall strategy to improve the health of state government workers, employees from the Tasmanian State Department of Health and Human Services (DHHS), Tasmania, Australia were invited to participate in this time series research study designed to interrupt the sedentary behavior of office workers. Blood pressure data were collected at five time points (baseline, 3, 6, 9, and 12 months) during this yearlong study.
Recruitment
Occupational health and safety (OHS) managers at the DHHS were sent an email informing them of the free availability of an e-health intervention and the possible multiple health benefits associated with its use for desk-based workers. After correspondence with OHS managers, permission was gained to email 3992 desk-based employees across the organization. Potential participants were asked to register their interest via a weblink to gain access to the e-health intervention. Before deployment of the e-health software, a second email was sent to all registered interested employees inviting them to orientation sessions conducted either face-to-face or online. These sessions offered information about the possible health effects associated with prolonged sitting, general strategies for performing appropriate workplace physical activity, and a practical instructional session on how to use the e-health solution, followed by a question and answer session with the research team. Those who chose the online induction option viewed the same information via pre-recorded video material and were encouraged to submit any questions that they had about the session through email communication to the research team.
At the end of the orientation sessions, participants were asked to consider to volunteer to participate in the yearlong study approved by the Tasmania Social Science Human Research Ethics Committee (reference no: H0018075). Interested individuals were informed of their rights and informed consent was taken. Data collection commenced in March 2013 and finished in September 2015, with a staged starting date for different worksites because of the field-based nature of the study.
Data Collection
All participants completed a baseline online-questionnaire and provided demographic data including sex, age, height, weight, desired weight, current chronic conditions, and medications. Baseline blood pressure measurements were taken and the e-health solution was installed on the participants’ work computers. Participants’ engagement with the software was logged through self-report of daily use through the e-health solution for the duration of the study. Participants were sent reminder emails every 13 weeks for subsequent blood pressure measurements (3, 6, 9, and 12 months) and completion of online-questionnaires on any change in body weight and medication. The DHHS agreed to not initiate any other workplace health promotion campaigns during the duration of the study. Participants were advised to not engage in any new exercise and/or diet programmes outside of work hours. These requests were made to reduce potential confounders that may affect blood pressure.
Blood Pressure Measurements
All blood pressure readings were collected in the workplace in a quiet room in a seated position after 5 minutes of rest. A team of certified nurses that worked within the DHHS collected brachial blood pressure with a calibrated Welch Allyn Sphygmomanometer Platinum Series—DS58–11 (Welch Allyn Australia Pty. Ltd., New South Wales, Australia). A standard care of blood pressure was utilized with three consecutive readings collected 5 minutes apart.27 The last two readings were averaged and used for the analysis.
Intervention
Once the baseline measures were complete the e-health solution, Exertime, was centrally deployed by the DHHS computer services team on the participant's work computer to begin the next workday. Once participants logged onto their computer each morning the Exertime prompting sequence, described below, first initiated after 45 minutes of computer work. The sequence begins with a prompt bubble in the bottom right hand corner of the computer screen. Once this small prompt bubble is presented on the computer screen a decision needed to be made by the user; choosing to perform a movement break comprised of self-selected NEPA, by clicking on the “Exertime now” button, or click the “Postpone” button for 5, 10, or 15 minutes to remove the prompt bubble from the computer screen for the selected amount of time. The prompt could only be ignored for a maximum of 15 minutes, then the Exertime sequence automatically initiated. Once the Exertime sequence was initiated, either by choice (clicking “Exertime Now”) or by force (“Postpone” time-out), users must click through the scheduled five movement break screens. These sequential screens allowed the users to choose a movement break, time their movement break, and record their progress with the number of repetitions they performed. There were no instructional requirements placed on participants in terms of activity choice, repetitions, duration, or intensity. During the entirety of this five screen movement break prompting sequence, participants are prevented from accessing the other computer work on their screen. Once participants click through the sequence, their computer screen becomes available again, and the prompt time initiation resets to 45 minutes.
To aid in their NEPA movement break decision-making process, users were able to view over 60 office-appropriate movement break video demonstrations of a model performing each activity in an office environment (for more detail on the intervention see Pedersen et al.,24). During the workday, each time a user responded to the prompting sequence a time and date stamp was recorded by the software indicating the NEPA movement break selected and the individual progress was self-reported. The dependent variable used to measure adherence was the number of movement breaks employees’ recorded per workday. For encouragement purposes only, the self-reported daily progress was graphically presented to employees indicating the frequency and the amount of time they had spent out of their chairs to engage in the movement break activities each day. The time was calculated automatically from when the Exertime sequence was initiated until the exit button was clicked by the employee at the end of the sequence. Despite best intentions, we were unable to analyze time spent in NEAT during work due to inherent shortcomings of the software used in the intervention. For example, at times participants chose to quickly click through the Exertime sequence resulting in 0 seconds logged for that movement break. In contrast, at other times participants may have chosen to initiate the sequence prior to leaving their desk for an office meeting and thereby not completing the sequence until they returned resulting in a movement break that registered for times greater than 1 or 2 hours. Unfortunately, therefore, these unreliable duration data were not utilized for further analyses.
Data Manipulation and Statistical Analyses
Mean arterial pressure (MAP) was calculated ([systolic blood pressure + 2∗ diastolic blood pressure]/3) from each blood pressure reading. To determine the impact of the intervention for those people with clinically elevated blood pressure, participants were categorized into normotensive (blood pressure <120/80 mmHg), prehypertensive (systolic 120 to 139 and/or diastolic 80 to 89 mmHg) and hypertensive (systolic ≥140 and/or diastolic 90 mmHg) based on their baseline blood pressure.28
Intention to treat, mixed effects regression analyses were conducted using STATA statistical software (STATA SE 14x, StataCorpLP, College Station, TX) used to determine differences in blood pressure (systolic, diastolic, and MAP) over time as well as changes to the number of times the e-health solution was utilized during the workday.29 Blood pressure data were adjusted for age, BMI, and sex during analyses. P values were adjusted for multiple comparisons using Holm test. Data were graphically plotted using Prism version 7.00 for Windows, GraphPad Software, La Jolla, CA.30
RESULTS
Of the 3922 eligible employees in DHHS, 595 employees expressed an interest and 370 consented and asked for the e-health solution to be installed on their computer. Nonetheless, only 228 (85% women; aged 45.1 ± 10.5 years) employees completed the baseline measures and subsequently began the intervention phase of the study. Only 94 participants (41.2%) came for the final (12-month) data collection point (Fig. 1). From the 228 participants who commenced the study, 78 (34.2%) were normotensive, 91 (39.9%) pre-hypertensive, and 59 (25.9%) hypertensive. The overall drop-out from each of the three groups was similar. Of the 94 participants who completed the yearlong study, 32 (34%) were from the normotensive group, 37 (39.4%) from the pre-hypertensive group, and 25 (26.6%) from the hypertensive group. The general categories for participant withdrawal for the yearlong study included: long- and short-term leave from work (n = 35), no reasons provided (n = 32), intervention-related stress (n = 28), switched work roles (n = 19), left the job (n = 11), work-related stress (n = 9), and non-sedentary job types (n = 4).
FIGURE 1.
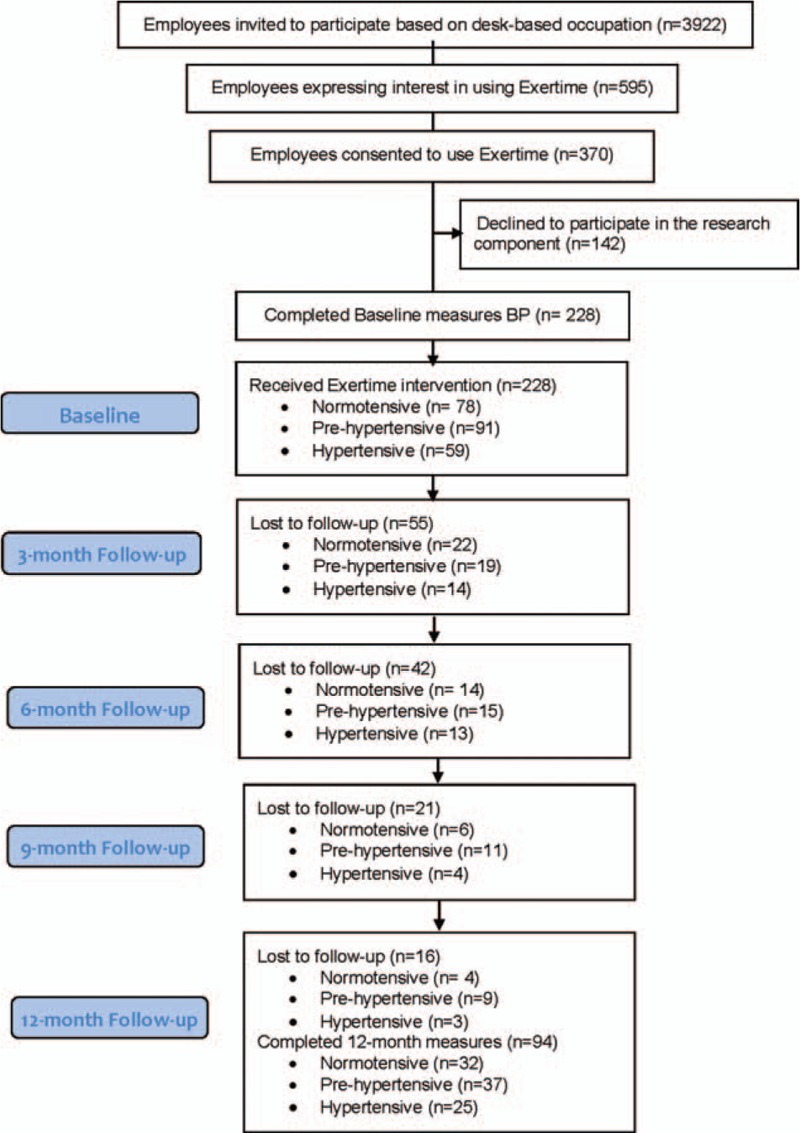
Participant flow through the study.
At study commencement, participants reported to be living with the following diseases/disorders: chronic pain (34.6%); respiratory diseases (28%); gastro-intestinal issues (20.2%); 46 with metabolic diseases (20.1%); cancer (2%); arthritis (15.8%); cardiovascular disease including hypertension (8.8%); and osteoporosis (2.2%). Eighty-two percent of the participants indicated that they wished to lose weight with 33% indicating a desire to lose more than 10 kg. Eighteen participants were taking antihypertensive medications at the commencement of the study, with eight medicated participants categorized as hypertensive, four as prehypertensive and the remaining six as normotensive, based on baseline blood pressure. Four of these participants (two hypertensive and two normotensive) did not complete the study, but this was not due to poor health or mortality.
Results for the Complete Sample
Diastolic blood pressure and MAP were significantly lower (by 4 to 5 mmHg for diastolic pressure and 3.6 to 4.2 mmHg for MAP; all P < 0.01; Table 1) at each time point, compared with baseline, however, there was no significant difference between the 3, 6, 9, and 12-month data-points. There was a slight but significant reduction (1.0 to 3.4 mmHg) in systolic blood pressure at 3, 6, and 9 months compared with baseline (all P < 0.01). There was no difference between 3, 6, 9, and 12 months. Work hours remained the same for the participants for the 12-month study period. Participants used the e-health solution 5.5 ± 2.0 times/day in the first 3 months. Workday movement breaks decreased throughout the study to 4.2 ± 2.5 times/day by the end of the study (P < 0.05 for all time points compared with 3 months). There were minimal (all P > 0.2) changes in self-reported weight and body mass index (BMI) of the participants during the 12-month study.
TABLE 1.
Demographic, Blood Pressure and Exertime Use Per Day for the Whole Group Throughout the Study
| Variable (Mean ± SD) | Baseline (n = 228) | 3-month (n = 173) | 6-month (n = 131) | 9-month (n = 110) | 12-month (n = 94) |
| Age, yr | 45.1 ± 10.5 | 45.6 ± 10.0 | 46.1 ± 10.1 | 46.5 ± 10.0 | 47.0 ± 10.0 |
| BMI, kg/m2 | 28.2 ± 6.3 | 28.3 ± 6.3 | 28.3 ± 6.2 | 28.4 ± 6.5 | 28.5 ± 6.5 |
| Gender (% F) | 85.4 | 82.3 | 80.9 | 79.1 | 82.1 |
| Work hours per week‡ | 36.1 ± 10.9 | 36.2 ± 11.1 | 35.7 ± 8.2 | 35.9 ± 9.5 | 36.5 ± 10.0 |
| Systolic blood pressure, mmHg | 122.9 ± 15.8 | 120.3 ± 13.4* | 120.3 ± 14.1* | 121.3 ± 14.7* | 122.0 ± 16.6 |
| Diastolic blood pressure, mmHg | 81.2 ± 10.2 | 77.4 ± 9.3* | 76.7 ± 9.1* | 76.9 ± 10.8* | 76.5 ± 9.8* |
| MAP, mmHg | 95.1 ± 11.1 | 91.7 ± 9.6* | 91.2 ± 9.8* | 91.7 ± 9.8* | 91.8 ± 11.0* |
| Exertime use, times/day‡ | 5.5 ± 2.0 | 5.0 ± 2.1† | 4.5 ± 2.3† | 4.2 ± 2.5† |
Data presented as means and standard deviations of the raw data; all data analyzed with intention to treat, mixed effects regression analyses corrected for any effect of BMI, sex, and age.
*Significantly different from baseline.
†Significantly different from 3 months data.
‡In Australia, the average full time work week equates to 37.5 hours per week or 7.5 hours per day.
Results for the Hypertensive Group
In the most at-risk group MAP significantly decreased by 8.0 to 11.0 mmHg during the duration of the study (all P < 0.001). Similarly, diastolic blood pressure reduced between 8.0 and 11.1 mmHg at each time-point compared with baseline (all P < 0.001). Further, there was a significant (all P < 0.001) reduction of 8.5 to 11.5 mmHg in systolic blood pressure in the hypertensive group during the course of the study compared with baseline (Fig. 2). Adherence to the e-health solution (Fig. 3) dropped from 5.1 times/day (95% CI 4.6 to 5.6 times/day) at 3 months to 4.1 times/day (95% CI 3.5 to 4.7 times/day) at 12 months and was significantly lower at 6, 9, and 12-months compared with the 3-month reading (all P < 0.01).
FIGURE 2.
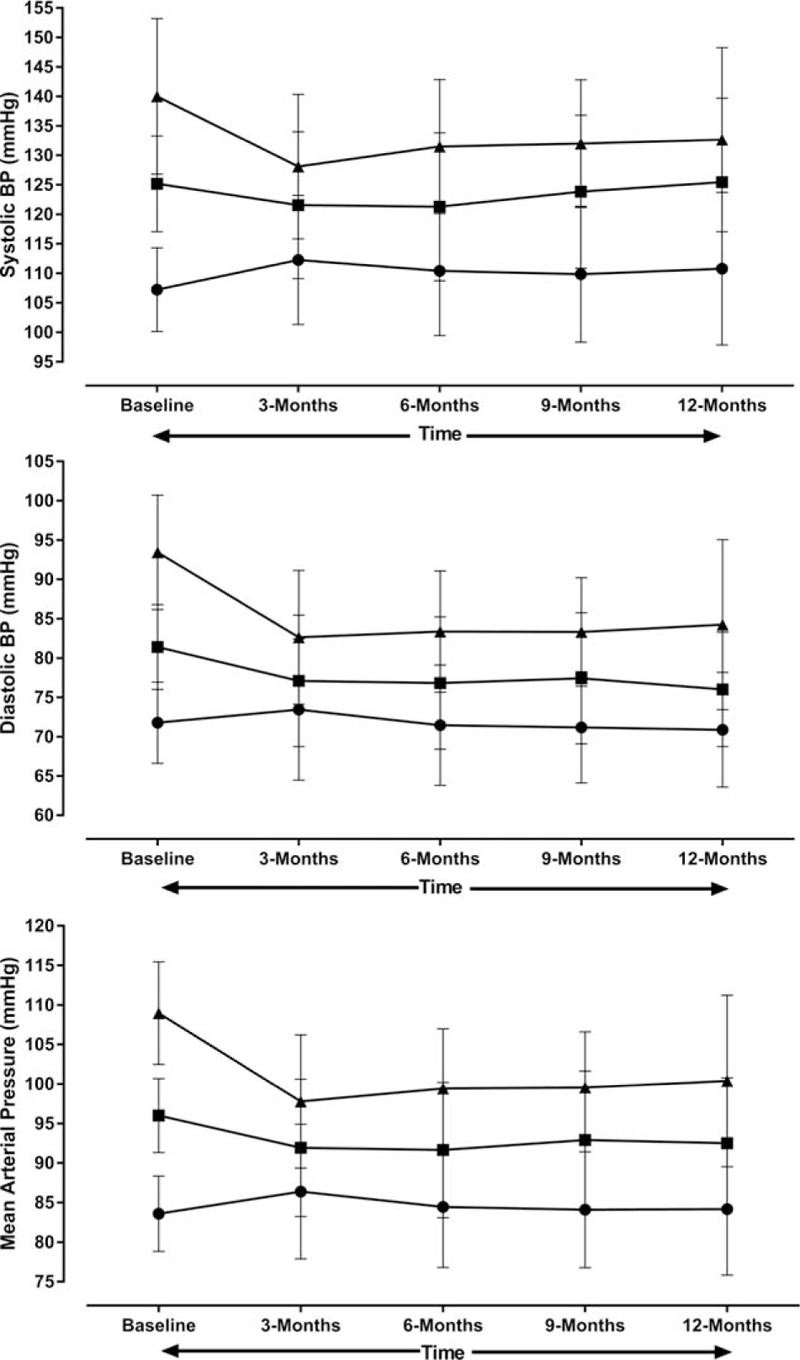
Blood pressure (mean ± SD) over the course of study separated into normotensive (circle; n = 78), pre-hypertensive (square; n = 91), and hypertensive (triangle; n = 59) categories based on baseline results.
FIGURE 3.
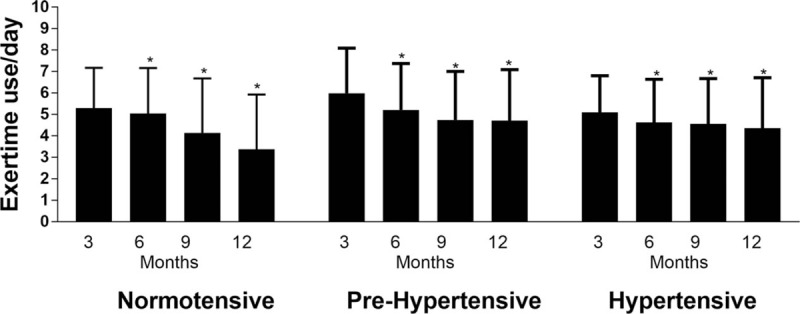
Adherence to the e-health solution separated into normotensive, pre-hypertensive, and hypertensive categories based on baseline results. ∗Indicates significantly different from 3-month data.
Results for the Pre-Hypertensive Group
For the pre-hypertensive group MAP decreased by 4 to 5 mmHg during the duration of the study (P < 0.001). Diastolic blood pressure was significantly lower by 4.5 to 6.0 mmHg at each time-point compared with baseline (all P < 0.001). Although systolic blood pressure reduced by 1.5 to 4.5 mmHg during the course of the study, the results were statistically significant (both P < 0.01) only at 3 and 6-months compared with the baseline (Fig. 2). The use of the e-health solution (Fig. 3) reduced gradually during the course of the study from 6.0 times/day (95% CI 5.6 to 6.4 times/day) at 3 months to 4.6 times/day (95% CI 4.0 to 5.1 times/day) at 12-months and was significantly lower at 6, 9, and 12-months compared with the 3-month reading (all P < 0.01).
Results for the Normotensive Group
Although there was a slight increase (1 to 3 mmHg) in MAP during the course of the study for the normotensive group, only the 3-month result was significantly higher than the baseline (P = 0.01; P > 0.3 for other time-points). As can be seen in Fig. 2 this was a result of no change in diastolic blood pressure during the course of the study (all P > 0.1), and a 3 to 5 mmHg increase in systolic blood pressure compared with baseline (all P ≤ 0.05). Mean adherence to the e-health solution (Fig. 3) dropped from 5.3 ± 1.9 times/day at 3 months to 3.4 ± 2.6 times/day at 12 months and was significantly lower at 6, 9, and 12months compared with the 3-month reading (all P < 0.01).
DISCUSSION
The primary aim of this study was to assess the blood pressure outcomes of an e-health intervention that consisted of a computer prompt designed to re-engage desk-based workers in the decision-making process to remain seated at their desk. The recorded instances participants logging their movements using the software indicate that the prompt was successful in having participants interrupt prolonged bouts of sitting and engage in small amounts of free-choice movement activities throughout their workdays. An outcome of this added movement for pre- hypertensive and hypertensive participants was a reduction in resting blood pressures sufficient to reduce their blood pressure category. Moreover, for those who experienced a change in resting blood pressure, and who maintained compliance, the result persisted over a yearlong trial. These results have several implications.
First, our results demonstrate that it is possible to achieve a clinically meaningful reduction in blood pressure through regular movement breaks. Changes in blood pressure values of 4 to 5 mmHg have been determined to be large enough to account for natural variation in measures and be clinically important.31 We achieved changes of this magnitude in systolic, diastolic, and MAP in the pre-hypertensive group and double this magnitude in the hypertensive group at the 3-month time point. Furthermore, of those initially classified as hypertensive at baseline 64% had moved to a lower category at 12 months. Of those categorized as pre-hypertensive 24% were normotensive at 12 months. In contrast, 13% of the pre-hypertensive group became hypertensive at 12 months. Our results support previous findings,20,25 that average changes for diastolic and systolic blood pressures of between –12 and –10 mmHg can be achieved through regular movement breaks. The implication for this finding is those who are suffering or at risk from suffering cardiovascular disease, but are unable or unwilling to participate in exercise to meet recommendation guidelines might be able to offset this through participation in regular low dose movement.
Second, the observed improvement in blood pressure was achieved by having individuals participate in frequent movement breaks during work hours. The goal of the intervention was not solely to reduce blood pressure, as other benefits stem from reducing prolonged sitting. Moreover, all participants, regardless of blood pressure categorization, eschewed additional participation in common forms of exercise-based activities for simple activities that could be incorporated into their work tasks (ie, standing while talking on the phone). The improvement in cardiovascular health provides evidence that mortality risk reductions associated with physical activity occur independently of how activity is accumulated, supporting recent findings reported by Pedro et al32 promoting bouts of physical activity of less than 5 minutes. We support the current physical activity recommendations, but, health benefits can only be achieved if people engage in activity. Thus, for those parts of the population who do not like, cannot physically do, or who have low confidence in performing exercise, our findings highlight an alternative that might be more palatable to the wider population.33,32 While rates of participation reduced over the time period, we have shown that it is feasible to implement a long-term e-health solution in the workplace.
Third, an issue that plagues all broad population interventions based on increased physical activity is ongoing compliance. Variable compliance over time is costly both in budgetary and human capital but more critically in the lost potential for improving the health status of those parts of the population who have pre-existing cardiac disease risk factors.34 Consistently participants’ levels of physical activity tend to decline over time even within an ongoing intervention.35 Based on the reduction in movement breaks over time, we presume that this trend was also evident in the current study and might explain the magnitude and the sustained effect of the intervention on blood pressure measures in these participants. Of interest, the decline in compliance to the intervention was largest in the normotensive group and accompanied mean increases in all blood pressure variables. As participants were aware of their blood pressure results it is possible that the improvements observed in the at-risk groups early in the intervention provided additional motivation to maintain their interrupted sitting behavior for the full 12-month intervention. It is also possible that participants with elevated blood pressures at baseline experienced greater perceptual health benefits which encouraged them to maintain compliance, nonetheless, these data were not collected. Although good research design mandates that participants are blinded to the dependent variable, in a field-based study such as this, awareness of findings might indicate to participants who are at-risk that the intervention is having a positive effect on their health and thus lead to greater adherence. We acknowledge that this might be a shortcoming to our study but would argue that the outcome justifies not blinding participants to the dependent variable. A challenge with translational research is to adequately control the experimental procedures. In an ideal situation a randomized control group would have been used as a comparator as used in our previous study.25 Nonetheless, this was not feasible as the primary aim of the DHHS was to improve the overall health of their all employees and not those specifically at risk of cardiovascular disease.
This study was feasible, maintaining a 41% participation rate over 12 months. Attrition is one of the major methodological problems in longitudinal, field-based studies with attrition rates of 30% to 70% often reported which can deteriorate the generalisability of the findings if participants who remain in a study differ from those who dropout.36 This study compares favorably to other workplace health interventions of shorter duration. This finding is encouraging for the use of e-health solutions designed to change health behavior in the workplace.
We cannot discount the possibility that participants chose to respond to the e-health solution cues by indicating they had performed a movement break without actually doing so. Despite this, the magnitude of change in blood pressure suggests that participants did perform some form of NEPA when prompted. Further, while participants were specifically instructed not to engage in any new exercise programmes or change their diet for the duration of the study, we did not collect information on these variables. Our study may also suffer from selection bias related to the level of motivation with regard to willingness to adopt a healthier lifestyle, similar to other lifestyle programme randomized controlled trials.37 Future research in this area is needed to place better control on these variables and include an objective measure of movement in the workplace.
CONCLUSION
There are several take home messages from our study. First, there is a willingness for people to use technology as a means of engaging in preventative health programmes. This acceptance presents a range of opportunities for health professionals to increase the breadth of activities and the population reach in delivering impactful solutions. Second, the use of free-choice but regular low intensity movements as the primary mechanism for health change is encouraging for interventions that target long-term sedentary populations. A change of focus towards promoting alternative types of physical movement such as the short breaks used in this study might alleviate the low participation rates observed in the general population or possibly offer a scaffold to help sedentary individuals into other types of movement such as exercise. Moreover, the acceptance of intrusive prompting mechanisms indicates that for some individuals, less control might be acceptable and hence equate to better compliance for them to health behavior change. This insight offers potential transference to other health interventions (ie, prescribed drug-taking, dietary, and physiotherapy rehabilitation).
Footnotes
C.M. and K.A. have contributed equally to this work.
Acknowledgments of financial support: This study was funded in part by a Tasmanian Government (Australia) Healthy@Work grant (www.healthyatwork.tas.gov.au).
The authors declare that there were no conflicts of interest in this experiment. Study design, data collection, analysis and interpretation, writing of the report, and submission of the results were not influenced by the funding source. While S.P. and D.C. designed the original e-health solution, none of the authors have an association with commercial entities or other financial interest relevant to this study.
REFERENCES
- 1.Healy GN, Lawler SP, Thorp AA, et al. Reducing prolonged sitting in the workplace (an evidence review: full report); 2012. Available at: http://www.vichealth.vic.gov.au/Publications/Economicparticipation/Creating_Healthy_Workplaces.aspx Accessed August 14, 2017. [Google Scholar]
- 2.Dunstan DW, Barr EL, Healy GN, et al. Television viewing time and mortality: the Australian diabetes, obesity and lifestyle study (AusDiab). Circulation 2010; 121:384–391. [DOI] [PubMed] [Google Scholar]
- 3.Thorp AA, Healy GN, Owen N, et al. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian diabetes, obesity and lifestyle (AusDiab) study 2004–2005. Diabetes Care 2010; 33:327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Toomingas A, Forsman M, Mathiassen SE, Heiden M, Nillson T. Variation between seated and standing/walking postures among male and female call centre operators. BMC Public Health 2012; 12:154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Evans RE, Fawole HO, Sheriff SA, Dall PM, Grant PM, Ryan CG. Point-of-choice prompts to reduce sitting time at work: a randomized trial. Am J Prev Med 2012; 43:293–297. [DOI] [PubMed] [Google Scholar]
- 6.Healy GN, Eakin EG, Lamontagne AD, et al. Reducing sitting time in office workers: short-term efficacy of a multicomponent intervention. Prev Med 2013; 57:43–48. [DOI] [PubMed] [Google Scholar]
- 7.Ryan CG, Dall PM, Granat MH, Grant PM. Sitting patterns at work: objective measurement of adherence to current recommendations. Ergonomics 2011; 54:531–538. [Google Scholar]
- 8.Katzmarzyk PT, Min-Lee I. Sedentary behaviour and life expectancy in the USA: a cause-deleted life table analysis. BMJ Open 2012; 2:e000828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koster A, Caserotti P, Patel KV, et al. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS One 2012; 7:e37696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviours and cause-specific mortality in US adults. Am J Clin Nutr 2012; 95:437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van der Ploeg HP, Chey T, Korda RJ, Banks E, Bauman A. Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med 2012; 172:494–500. [DOI] [PubMed] [Google Scholar]
- 12.Lee PH, Wong FKY. The association between time spent in sedentary behaviours and blood pressure: a systematic review and meta-analysis. Sports Med 2015; 45:867–880. [DOI] [PubMed] [Google Scholar]
- 13.Beunza JJ, Martinez-Gonzalez MA, Ebrahim S, et al. Sedentary behaviours and the risk of hypertension: the SUN cohort. Am J Hypertens 2007; 20:1156–1162. [DOI] [PubMed] [Google Scholar]
- 14.Ragland DR, Greiner BA, Holman BL, Fisher JM. Hypertension and years of driving in transit vehicle operators. Scand J Public Health 1997; 25:271–279. [DOI] [PubMed] [Google Scholar]
- 15.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016; 388:1302–1310. [DOI] [PubMed] [Google Scholar]
- 16.Cooley PD, Pedersen SJ. A pilot study of increasing nonpurposeful movement breaks as work as a means of reducing prolonged sitting. J Environ Public Health 2013; 2013:1–8. Article ID 128376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levine JA. Nonexercise activity thermogenesis (NEAT): environment and biology. Am J Physiol Endocrinol Metab 2004; 286:E675–E685. [DOI] [PubMed] [Google Scholar]
- 18.Ekblom-Bak E, Ekblom B, Vikström M, de Faire U, Hellenius ML. The importance of non-exercise physical activity for cardiovascular health and longevity. Br J Sports Med 2014; 48:233–238. [DOI] [PubMed] [Google Scholar]
- 19.Hamer M, de Oliveira C, Demakakos P. Non-exercise physical activity and survival: English longitudinal study of ageing. Am J Prev Med 2014; 47:452–460. [DOI] [PubMed] [Google Scholar]
- 20.Larsen RN, Kingwell BA, Sethi P, Cerin E, Owen N, Dunstan DW. Breaking up prolonged sitting reduces resting blood pressure in overweight/obese adults. Nutr Metab Cardiovasc Dis 2014; 24:976–982. [DOI] [PubMed] [Google Scholar]
- 21.Commissaris DA, Huysmans MA, Mathiassen SE, Srinivasan D, Koppes L, Hendriksen IJ. Interventions to reduce sedentary behavior and increase physical activity during productive work: a systematic review. Scand J Work Environ Health 2016; 42:181–191. [DOI] [PubMed] [Google Scholar]
- 22.Middleton KR, Anton SD, Perri MG. Long term adherence to health behavior change. Am J Lifestyle Med 2013; 7:395–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swartz AM, Rote AE, Welch WA, et al. Prompts to disrupt sitting time and increase physical activity at work, 2011–2012. Prev Chronic Dis 2014; 11:E73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pedersen SJ, Cooley PD, Mainsbridge CP. An e-health intervention designed to increase workday energy expenditure by reducing prolonged occupational sitting habits. Work 2014; 49:289–295. [DOI] [PubMed] [Google Scholar]
- 25.Mainsbridge CP, Cooley PD, Fraser SP, Pedersen SJ. The effect of an e-health intervention designed to reduce prolonged occupational sitting time on mean arterial pressure. J Occup Environ Med 2014; 56:1189–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cooley PD, Pedersen SJ, Mainsbridge CP. Assessment of the impact of a workplace health and wellbeing intervention: closing the loop. Qual Health Res 2014; 24:90–101. [DOI] [PubMed] [Google Scholar]
- 27.Perloff D, Grim C, Flack J, et al. Human blood pressure determination by sphygmomanometry. Circulation 1993; 88:2460–2470. [DOI] [PubMed] [Google Scholar]
- 28.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure: the JNC 7 report. JAMA 2003; 289:2560–2572. [DOI] [PubMed] [Google Scholar]
- 29.StataCorp. Stata Statistical Software: Release 14 2015. College Station, TX, USA. [Google Scholar]
- 30.Graphpad Prism. Version 7.00 for Windows, GraphPad Software 2017. La Jolla, California, USA. Available at: https://www.graphpad.com/guides/prism/7/userguide/index.htm?citing_graphpad_prism.htm Accessed August 14, 2017. [Google Scholar]
- 31.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: Part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005; 111:697–716. [DOI] [PubMed] [Google Scholar]
- 32.Pedro FS, Troiano RP, Matthews CE, Kraus WE. Moderate-to-vigorous physical activity and all-cause mortality: do bouts matter? J Am Heart Assoc 2018; 7:e007678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ekelund U, Steene-Johannessen J, Brown WJ, et al. Lancet Physical Activity Series 2 Executive Committee, Lancet Sedentary Behaviour Working Group. Does physical activity attenuate, or even eliminate, the detrimental associateion of sitting time with mortality? A harmonized meta-analysis of data from more than 1 million men and women. Lancet 2016; 388:1302–10. [DOI] [PubMed] [Google Scholar]
- 34.Reiner M, Niermann C, Jekauc D, Woll A. Long-term benefits of physical activity: a systematic review of longitudinal studies. BMC Public Health 2013; 13:813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zubala A, MacGillivray S, Frost H, et al. Promotion of physical activity interventions for community dwelling older adults: A systematic review of reviews. PLoS One 2017; 12:e0180902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gustavson K, von Soest T, Karvold E, Roysamb E. Attrition and generalizability in longitudinal studies: Findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Public Health 2012; 12:918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coffeng JK, van der Ploeg HP, Castellano MD, et al. A 30 month worksite-based lifestyle program to promote cardiovascular health in middle-aged bank employees: Design of the TRANSIP-PESA randomised controlled trial. Am Heart J 2016; 184:121–132. [DOI] [PubMed] [Google Scholar]


