Abstract
Objective
To investigate the potential dietary impact of the opening of new retailers of healthy foods.
Design
Systematic review of the peer-reviewed research literature.
Setting
References published before November 2015 were retrieved from MEDLINE, EMBASE and Web of Science databases using keyword searches.
Subjects
The outcome of the review was change in fruit and vegetable consumption among adults.
Results
Of 3514 references retrieved, ninety-two articles were reviewed in full text, and twenty-three articles representing fifteen studies were included. Studies used post-test only (n 4), repeated cross-sectional (n 4) and repeated measures designs (n 7) to evaluate the dietary impact of supermarket (n 7), farmers’ market (n 4), produce stand (n 2) or mobile market (n 2) openings. Evidence of increased fruit and vegetable consumption was most consistent among adults who began shopping at the new retailer. Three of four repeated measures studies found modest, albeit not always statistically significant, increases in fruit and vegetable consumption (range 0·23–0·54 servings/d) at 6–12 months after baseline. Dietary change among residents of the broader community where the new retailer opened was less consistent.
Conclusions
The methodological quality of studies, including research designs, sampling methods, follow-up intervals and outcome measures, ranged widely. Future research should align methodologically with previous work to facilitate meta-analytic synthesis of results. Opening a new retailer may result in modest short-term increases in fruit and vegetable consumption among adults who choose to shop there, but the potential longer-term dietary impact on customers and its impact on the broader community remain unclear.
Keywords: Diet, Food supply, Fruit and vegetable consumption, Health promotion, Systematic review
Social ecological models of health suggest that community food environments must be structured to support healthy eating behaviours to effectively prevent chronic disease( 1 – 4 ). However, a growing body of research has documented disparities in access to healthy foods throughout the USA( 5 , 6 ). Neighbourhoods with predominantly low-income and racial and ethnic minority residents tend to have limited access to retailers of healthier food options, such as full-service supermarkets( 7 , 8 ), and are instead disproportionately served by retailers of energy-dense processed foods, including fast-food outlets( 9 ).
A growing focus on increasing access to healthy foods by opening new retailers in underserved communities is reflected in both national public health objectives and large-scale healthy food financing initiatives. For example, Healthy People 2020 includes an objective to increase the proportion of Americans who have access to a food outlet that sells foods recommended by federal dietary guidelines(10). In 2010, the US Departments of Agriculture, Treasury, and Health and Human Services announced the Healthy Food Financing Initiative, which funds the development of new retailers of healthy foods in underserved communities throughout the country( 11 ). Additional public–private partnerships, such as the Pennsylvania Fresh Food Financing Initiative, the New York Fresh Retail Expansion to Support Health (FRESH) programme, the California FreshWorks Fund and the New Orleans Fresh Food Retailer Initiative( 12 – 15 ), are emerging as models for improving local food environments. Among other activities, these initiatives incentivize the development of supermarkets and grocery stores in limited-access neighbourhoods through zoning reforms, loans and grants.
Introducing new retailers of healthy foods into limited-access communities is an intuitively appealing intervention strategy, and although multiple evaluations of such initiatives have been published, no known systematic reviews have synthesized this body of research. The present systematic review aims to answer the following research questions:
-
1.
What types of retailers of fruits and vegetables have been evaluated and in what settings?
-
2.
What methods have been used to evaluate these initiatives?
-
3.
To what extent have these initiatives impacted fruit and vegetable consumption among adults?
Fruit and vegetable consumption among adults was identified as the outcome of interest because this was a commonly used outcome in relevant studies, as well as the broader epidemiological literature( 6 ).
Methods
References were retrieved from MEDLINE, EMBASE and Web of Science databases from inception through November 2015 using a search strategy adapted from a previous systematic review about spatial access to food retailers and diet( 6 ). English-language references that contained at least one keyword related to the following three domains were retrieved: (i) food retailers (food retail*, food store*, food outlet*, grocer*, supermarket*, farmers market*, farm stand); (ii) the environment (access*, availab*, afford*, environment*, loca*, neighborhood*, neighbourhood*, communit*, urban, or rural); and (iii) diet (diet, fruit*, vegetable*, nutriti*, consum*, intake).
Two investigators (R.C.W. and I.G.R.) identified candidate articles by independently reviewing the titles of all references for eligibility, referring to the abstracts for additional details when a decision could not be made based on the title alone. References were excluded if they: (i) were not about the general topic area of access to healthy foods as a determinant of dietary behaviour; (ii) were not about an initiative intended to increase access to healthy foods; or (iii) were not about the introduction of a new retailer of healthy foods into a community. Additional references were identified by hand-searching the bibliographies of the candidate articles and entering their bibliographic information into Google Scholar to identify more recent articles that had cited them.
Once the pool of candidate articles was finalized, all were reviewed in full text. In instances in which multiple publications resulted from the same parent study (e.g. a baseline paper describing the retailer and one or more outcome evaluations), we grouped articles by parent study and determined eligibility at the study level. Studies were excluded if they were found to meet the exclusion criteria described previously, if the evaluation did not include change in fruit and vegetable consumption as an outcome, or if it focused exclusively on dietary change among children. Studies that focused exclusively on children were excluded because the causal mechanism through which the opening of a new retailer of healthy foods would impact diet was expected to differ for this group.
The data abstraction form was developed based on the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) statement and piloted with a sample of articles. Two investigators (R.C.W. and I.G.R.) independently abstracted the following information from all articles included in the review: bibliographic information, key characteristics of the retailer described in the article (e.g. type, location, date opened, setting, population served, etc.), the methods used to evaluate the retailer (e.g. sampling methods, sample size, data collection procedures, outcome measures, etc.) and its impact on fruit and vegetable consumption; discrepancies were resolved by consensus. For studies that used repeated measures designs, mean differences in fruit and vegetable consumption were the principal summary measure. Nine corresponding authors were contacted by email for additional information about the methods or results (89 % response rate).
Studies were the unit of analysis for the present review. Due to the heterogeneity in methods used, meta-analysis was not possible. Analysis involved organizing studies according to the type of evaluation design used and using descriptive statistics, including frequencies and percentages, to describe the types of retailers that were assessed, the methods used to evaluate them and change in fruit and vegetable consumption. In many cases, the number of references exceeds the number of studies because multiple publications resulted from individual studies.
Results
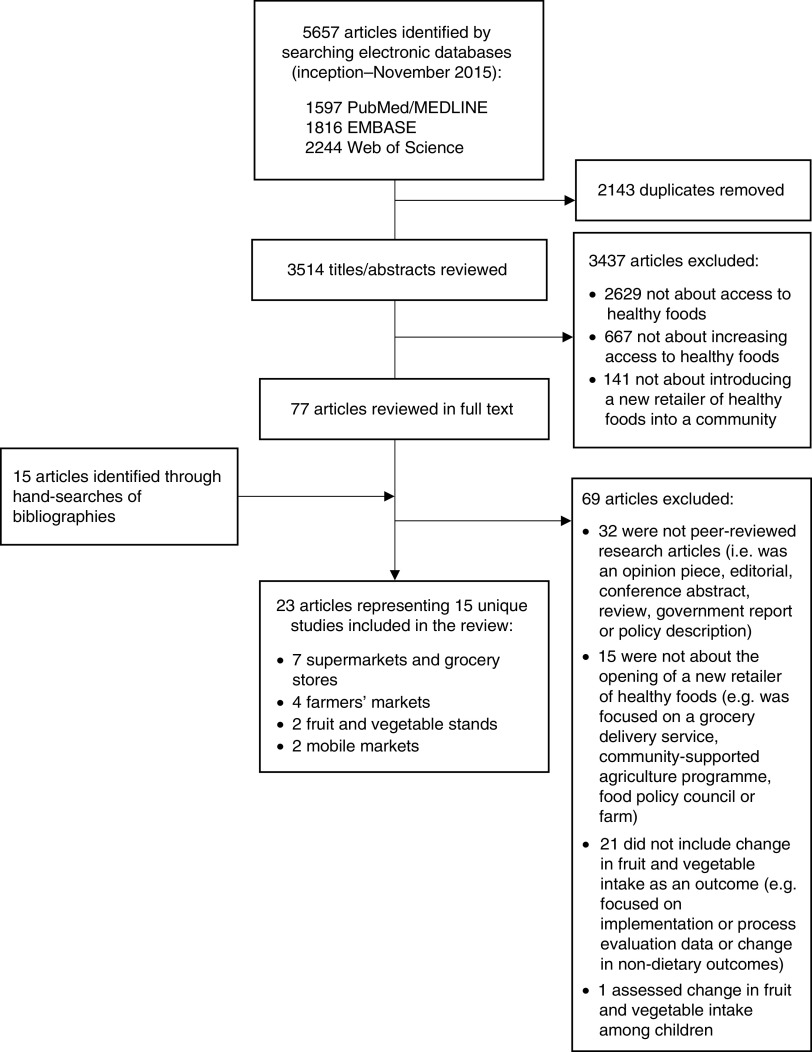
Of the 5657 references retrieved through keyword searches, 3514 were unique articles and 3437 were excluded based on the title/abstract review (Fig. 1). The remaining seventy-seven candidate articles and fifteen additional articles identified through hand-searching were reviewed in full text to assess eligibility. Of these, sixty-nine articles were excluded. The most common reasons for exclusion were that the article was not a peer-reviewed original research article (i.e. was an opinion piece, editorial, letter to the editor, conference abstract, review, government report or policy description; n 32); was not about the opening of a new retailer of healthy foods (e.g. was focused on a grocery delivery service, community-supported agriculture programme, food policy council or farm; n 15); or did not assess change in fruit and vegetable consumption among adults as part of the evaluation (n 22). The twenty-two articles in this latter category commonly reported implementation or process evaluation data (e.g. sales volume, demographic characteristics of shoppers, satisfaction with the retailer, etc.) or changes to other non-dietary outcomes (e.g. customers’ shopping patterns, access to healthy foods, etc.). The present review focuses on the remaining twenty-three articles, which represented fifteen unique studies.
Fig. 1.
Flow diagram depicting article selection for inclusion in the present systematic review on the dietary impact of introducing new retailers of fruits and vegetables into a community
Description of retailers and settings
As shown in Fig. 1, the types of retailers assessed included supermarkets and grocery stores (n 7)( 16 – 30 ), farmers’ markets (n 4)( 31 – 34 ), fruit and vegetable stands or markets (n 2)( 35 , 36 ), and mobile markets (n 2)( 37 , 38 ). Supermarkets and grocery stores tended to be subsidized through public–private partnerships, including the Healthy Food Financing Initiative (n 2)( 19 , 22 , 23 ) and the New York Food Retail Expansion to Support Health (FRESH) initiative (n 1)( 20 , 21 ), or were aligned with broader corporate initiatives to promote economic development or open supermarkets in deprived areas (n 2)( 24 – 27 , 29 , 30 ). The smaller retailers, such as farmers’ markets, fruit and vegetable stands or markets, and mobile markets, tended to report community involvement in planning or operating the retailer, including having a community advisory board, collaborating with other local organization to implement the retailer, or that the project used a community-based participatory approach (n 7)( 31 – 36 , 38 ).
Most of the retailers were located in low-income and/or economically deprived communities (n 13)( 16 – 30 , 32 , 33 , 35 – 38 ) that had limited access to healthy foods (n 12)( 16 – 31 , 33 – 36 ) in the USA (n 11)( 19 – 23 , 28 – 33 , 35 – 37 ), the UK (n 3)( 16 – 18 , 24 – 27 , 38 ) or Australia (n 1)( 34 ). Many studies also described the communities in which the new retailer opened as comprised of predominantly racial or ethnic minority residents (n 7)( 19 – 23 , 29 – 33 ). Most retailers were located in general community settings (n 11)( 16 – 31 , 33 , 34 , 38 ), although some farmers’ markets, fruit and vegetable stands, and mobile markets operated at local community organizations (n 3)( 35 – 37 ), residential housing complexes (n 2)( 35 , 37 ) and health centres (n 1)( 32 ).
Evaluation methods
A variety of methods were used to evaluate the impact of the retailer on fruit and vegetable intake. Retailers were evaluated using post-test only designs (n 4)( 28 , 33 – 35 ), repeated cross-sectional designs (n 4)( 20 , 21 , 29 – 31 , 38 ) and repeated measures designs (n 7; Table 1)( 16 – 19 , 22 – 27 , 32 , 36 , 37 ). Studies assessed the impact of the retailer on fruit and vegetable consumption approximately six months (n 7)( 24 – 28 , 31 , 32 , 35 – 37 ), one year (n 5)( 16 – 23 , 29 , 30 ) or two years (n 2)( 33 , 38 ) after the retailer opened, or at multiple follow-up intervals( 33 ).
Table 1.
Methodological summary of evaluations of the opening of a retailer of healthy foods on fruit and vegetable intake among adults (N 15)
| Study design | Reference(s) | Retailer, year opened, setting | Sample description (sample size, response rate) | Data collection | Outcome measure | Results |
|---|---|---|---|---|---|---|
| Post-test only (n 4) | Woodruff et al.( 35 ) | Fruit and vegetable stand 2014 Cobb County, Georgia, USA | Convenience sample of returning market shoppers aged ≥18 years (n 100, 99 %) | Self-administered surveys 4 months after market opening | Two-item retrospective measure | 65 % reported eating more vegetables, 55 % reported eating more fruit as a result of shopping at the market |
| Ruelas et al. ( 33 ) | Farmer’s markets 2007 Los Angeles, California, USA | Convenience sample of market shoppers aged ≥18 years (n 415 at one location, n 1375 at second location, NR) | Surveys administered 5 months after market opening at one location and 2 years after opening at second location | Single-item retrospective measure | 97–98 % agreed or strongly agreed that they eat more fruits and vegetables because of the market | |
| Payet et al. ( 34 ) | Farmers’ market 2001 Rural community near Carnarvon, Western Australia | Convenience sample of market shoppers aged ≥18 years (n 100, 80·6 %*) | Surveys administered 2 years and 4 months after market opening | Single-item retrospective measure | 71 % reported eating more fruits and vegetables since started shopping at the market | |
| Wang et al. ( 28 ) | Grocery store 2004 Northern California, USA | Convenience sample of adults aged ≥18 years who were the primary grocery shoppers for their homes and lived ~3·2 km (~2 miles) from the store (n 78, NR) | Surveys administered 6 months after store opening | Four-item measure assessing frequency of fruit and vegetable consumption currently and last year | 10 % reported an increase in fruit consumption, 9 % reported an increase in vegetable consumption over the previous year* | |
| Repeated cross-sectional (n 4) | Freedman( 31 ) | Farmers’ market 2006 Nashville, Tennessee, USA | Convenience sample of market shoppers | Surveys administered at baseline (n 29), mid-way through the season (n 15) and at the end of the season (n 16) | Two-item screener adapted from Youth Risk Behavior Surveillance System | Results are reported graphically, but suggest a pattern of greater fruit and vegetable consumption among follow-up sample relative to baseline sample |
| Jennings et al. ( 38 ) | Mobile fruit and vegetable market 2008 Great Yarmouth and Waverly, England, UK | Convenience sample of shoppers (n 255, 62 %) | Surveys administered at baseline and 2 years after market began operating | Two-item screener measuring portions consumed per day | 1·16-portion increase in mean fruit and vegetable consumption (95 % CI 0·83, 1·48, P<0·001) | |
| Sadler et al. ( 29 , 30 ) | Grocery store 2010 Flint, Michigan, USA | Probability sample of adults aged ≥18 years who were the primary grocery store for their homes and either lived within 2000 m of the store or in a nearby comparison neighbourhood (n 150–200 per time point, 15 % response rate) | Interviewer-administered surveys at baseline and 12 months after store opening | BRFSS screener | 0·0-serving change in fruit and vegetable consumption among intervention residents* 0·4-serving increase among comparison neighbourhood residents* | |
| Elbel et al. ( 20 , 21 ) | Supermarket 2011 South Bronx, New York, USA | Convenience sample of adults aged ≥18 years (approximately n 1300 per time point, NR) | Intercept surveys and dietary recalls administered at baseline, 1–5 months and 13–17 months after store opening | 24 h dietary recall and the Eating and Physical Activity Survey | 24 h dietary recall results: • 0·05-unit increase in fruit and 0·21-unit increase in vegetable consumption at final follow-up • Difference-in-differences: 0·10 for fruit and 0·32 for vegetable consumption Screener results: • 0·2-unit increase in fruit consumption and 0·1-unit increase in vegetable consumption at final follow-up • Difference-in-differences: 0·1 for fruit and 0·0 for vegetable consumption Note: No results reached statistical significance | |
| Repeated measures (n 7) | Abusabha et al. ( 37 ) | Mobile fruit and vegetable market 2007 Troy, New York, USA | Convenience sample of shoppers aged ≥55 years who lived at the senior housing complex served by the market (n 43, 54 % at follow-up*) | Surveys administered at baseline and 6 months after the market began serving the senior housing complex | Five-item screener adapted from BRFSS | 0·45-serving increase in total fruit and vegetable intake (95 % CI −0·23, 1·14; P=0·188) |
| Freedman et al. ( 32 ) | Farmers’ market 2001 Rural county in South Carolina, USA | Probability sample of adult patients at the health clinic where the farmers’ market operated who had a diagnosis of diabetes (n 44, NR) | Interviewer-administered surveys at baseline, 2 and 5 months after the market opening | Nineteen-item screener adapted from the NCI FVS | 0·54-serving increase in total fruit and vegetable intake at 5-month follow-up (95 % CI −1·14, 2·23; P=0·52) | |
| Evans et al. ( 36 ) | Fruit and vegetable stand 2010 Austin, Texas, USA | Probability sample of adults aged ≥18 years who lived within 0·8 km (0·5 miles) of market recruited through door-to-door household sampling (n 61, 66 % at follow-up) | Interviewer-administered surveys at baseline and 2 months after the market opened | Seven-item screener adapted from the NCI FVS | 0·42-serving increase in total fruit and vegetable intake among intervention community residents (sd=2·49; P=0·210) | |
| Wrigley et al. & Gill and Rudkin( 24 – 27 ) | Supermarket 2000 Leeds, England, UK | Sample of adults who were responsible for domestic food arrangements for the household and who lived in the neighbourhood where the supermarket opened (n 615, 61 % at follow-up) | Self-administered food consumption diary at baseline and 6–7 months after the store opening | 7 d food consumption diary | 0·23-serving increase in fruit and vegetable intake among residents who began shopping at the new retailer (P=0·034) 0·04-serving increase in fruit and vegetable intake in intervention community residents* | |
| Cummins et al. ( 16 – 18 ) | Supermarket 2001 Glasgow, Scotland, UK | Probability sample of adults aged ≥16 years who were the main food shopper for their homes and who lived in the neighbourhood where the supermarket opened or a comparison community (n 412, 68 % at follow-up) | Self-administered postal survey at baseline and 11 months after the store opening | Two-item screener assessing usual fruit and vegetable intake per day | 0·29-portion increase in fruit and vegetable intake in the intervention community (P=0·07) 0·44-portion increase in fruit and vegetable intake in the comparison community (P=0·003) | |
| Cummins et al. ( 19 ) | Supermarket 2009 Philadelphia, Pennsylvania, USA | Probability sample of adults aged ≥18 years who lived near the new supermarket or were residents of a neighbouring community recruited through random directory listings and random digit dialling (n 656, 46 % at follow-up) | Interviewer-administered surveys at baseline and 6 months after store opening | Twenty-two-item screener adapted from Block Food Frequency Questionnaire | −0·16-serving difference between neighbourhoods at baseline −0·21-serving difference between neighbourhoods at follow-up Difference-in-differences: −0·05 (NS) | |
| Dubowitz et al. ( 22 , 23 ) | Supermarket 2013 Pittsburgh, Pennsylvania, USA | Probability sample of adults aged ≥18 years who were the primary food shopper for their household and lived in the neighbourhood where the supermarket opened or a comparison neighbourhood, recruited through door-to-door sampling (n 831, 65 % at follow-up) | Interviewer-administered surveys at baseline and 7–14 months after the store opening | Two 24 h dietary recalls administered 7–14 d apart | −0·32-serving change among adopters of the new retailer (NS) −0·27-serving change among residents of intervention community (se=0·08, P<0·001) Difference-in-differences (intervention v. comparison neighbourhood residents): −0·14 (NS) |
NR, not reported; BRFSS, Behavioral Risk Factor Surveillance System; NCI FVS, National Cancer Institute Fruit and Vegetable Intake Screener.
Calculated by hand using information provided in the article.
Eight studies used convenience sampling( 20 , 21 , 28 , 31 , 33 – 35 , 37 , 38 ) and six used probability sampling methods( 16 – 19 , 22 , 23 , 29 , 30 , 32 , 36 ). The sampling method could not be determined for one study( 24 – 27 ). Six studies sampled shoppers at the new retailer( 31 , 33 – 35 , 37 , 38 ) and three sampled residents of the neighbourhood where the new retailer opened( 24 – 28 , 36 ). An additional five studies sampled from both residents of the neighbourhood where the new retailer opened and a comparison neighbourhood that did not receive a new retailer( 16 – 23 , 29 , 30 ). One study sampled patients at a health clinic where the retailer was located( 32 ). Sample sizes ranged widely.
Outcome measures included retrospective items asking participants to what extent their fruit and vegetable intake changed over time (n 4)( 28 , 33 – 35 ), two-item screeners assessing usual daily intake of fruits and vegetables (n 3)( 19 , 31 , 38 ), brief fruit and vegetable intake screeners or FFQ (n 6)( 16 – 18 , 20 , 21 , 29 , 30 , 32 , 36 , 37 ), or dietary recalls (n 3)( 20 – 27 ). One study used multiple methods of assessing fruit and vegetable intake( 20 , 21 ).
Post-test only designs
Methodological overview
Four studies used post-test only designs to assess the dietary impact of the new retailer (Table 1). In these studies, cross-sectional surveys were administered to participants four months to two-and-a-half years after the opening of the retailer( 28 , 33 – 35 ). All studies focused on dietary change among a convenience sample of adults who were either shoppers at the retailer( 33 – 35 ) or lived in the neighbourhood where the new retailer opened for business( 28 ). All of these studies used a retrospective approach to measure change in fruit and vegetable intake by asking participants to report changes in fruit or vegetable consumption as a result of shopping at the retailer( 33 – 35 ) or generally within the past year( 28 ).
Change in fruit and vegetable intake
Of the studies that surveyed shoppers at the retailer, most respondents reported that they were eating more fruits and/or vegetables at the time of the survey( 33 – 35 ). For example, of 100 shoppers at a farmers’ market in Carnarvon, Western Australia who were surveyed approximately two-and-a-half years after its opening, 71 % reported that they were eating more fruits and vegetables since they started shopping there( 34 ). A survey of 100 returning customers who were surveyed approximately four months after the opening of a fruit and vegetable stand in Cobb County, Georgia, USA reported that they were eating more vegetables (65 %) and fruit (55 %) as a result of the market( 35 ). Another survey administered to shoppers at two farmers’ markets in Los Angeles, California, USA between five months and two years after the markets opened reported that 97–98 % agreed or strongly agreed that they were eating more fruits and vegetables as a result of the market( 33 ). By contrast, the one study that assessed the impact of a new grocery store that opened in an unnamed city in California, USA on the dietary behaviours of residents of the neighbourhood where it opened (regardless of whether participants shopped there) found smaller changes in fruit and vegetable consumption. Relatively few respondents who lived 3·2 km (2 miles) from the new grocery store reported increased vegetable (10·3 %) or fruit (9 %, n 73) consumption over the previous year( 28 ).
Repeated cross-sectional designs
Methodological overview
Four studies used repeated cross-sectional surveys at baseline and follow-up to assess the dietary impact of the new retailer (Table 1). Two studies used a convenience sample of market shoppers( 31 , 38 ); one used a random sample of households with landlines located within 2000 m of the store site and a nearby comparison neighbourhood( 29 , 30 ); and another recruited participants from busy intersections in the neighbourhood where the retailer opened, as well as a nearby comparison neighbourhood( 20 , 21 ). Measurement approaches included using a two-item fruit and vegetable intake screener( 31 , 38 ); the Behavioral Risk Factor Surveillance System (BRFSS) screener( 29 , 30 ); or a combination of a brief screener and a single 24 h dietary recall( 20 , 21 ).
Change in fruit and vegetable intake
Results from studies in this category were difficult to summarize due to the heterogeneity in methodological approaches. For example, one evaluation of a farmers’ market in Nashville, Tennessee, USA found that shoppers sampled at 1- and 2-month follow-ups reported higher levels of fruit and vegetable consumption relative to a different sample of shoppers sampled at baseline( 31 ). However, these results were reported graphically, and no estimates of mean intake were presented to quantify the difference in mean intake between the samples over time( 31 ). A different study of a convenience sample of shoppers at a mobile market in the UK found that those sampled at follow-up reported higher mean fruit and vegetable intake at follow-up than the baseline sample (mean difference=1·16 portions, 95 % CI 0·83, 1·48, P<0·0001)( 38 ).
Two studies assessed community-level dietary change among residents of the neighbourhood that received the new retailer relative to those who lived in a comparison neighbourhood( 20 , 21 , 29 , 30 ). One of these studies conducted telephone surveys before and 12 months after a grocery store opened in Flint, Michigan, USA among a random sample of households located within 2000 m of the new store and those located in a comparison neighbourhood. That study found that mean intake of fruits and vegetables was the same among the baseline and follow-up samples in the intervention neighbourhood (mean intake=2·6 servings/d among samples at both time points), although mean intake was higher among the comparison neighbourhood residents in the follow-up sample relative to the baseline sample (mean intake=2·5 servings/d at baseline, mean intake=2·9 servings/d at follow-up)( 29 , 30 ). Information about the precision and statistical significance of these estimates is unavailable.
Another study conducted surveys among adults recruited from busy intersections located in a neighbourhood that received a new supermarket and a comparison neighbourhood in the Bronx, New York City, USA( 20 , 21 ). Surveys were administered at baseline, 1–5 months and 13–17 months after the supermarket opened, and included two different methods of assessing fruit and vegetable intake. Results from the brief fruit and vegetable intake screener indicated among both intervention and comparison neighbourhood residents that mean fruit and vegetable intake was highest at baseline relative to either follow-up time point (e.g. mean change in vegetable consumption=−0·1 daily servings among intervention neighbourhood sample v. 0·0 among comparison neighbourhood sample). Results from the 24 h dietary recalls showed a different pattern of higher fruit and vegetable consumption at follow-up relative to baseline in both groups, although greater improvements among those sampled from the comparison community (e.g. mean change in vegetable consumption of 0·21 daily servings among intervention neighbourhood sample v. 0·58 daily servings among comparison neighbourhood sample)( 20 , 21 ).
Repeated measures designs
Methodological overview
Seven studies used repeated measures to assess the dietary impact of the new retailer (Table 1). All of these studies collected data from participants at baseline and at either one (n 6)( 16 – 19 , 22 – 26 , 36 , 37 ) or two (n 1)( 32 ) follow-up time points. The majority of these studies used probability sampling methods to recruit participants( 16 – 19 , 22 , 23 , 32 , 36 ), although one used convenience sampling methods( 37 ) and the approach used by another could not be determined( 24 – 27 ). One study recruited shoppers at the new retailer( 37 ), two recruited residents of the neighbourhood where the new retailer opened( 24 – 26 , 36 ) and three recruited residents of both the intervention neighbourhood and a nearby comparison neighbourhood( 16 – 19 , 22 , 23 ). One study recruited patients from the clinic where the new retailer opened for business( 32 ). Studies in this category measured change in fruit and vegetable consumption using a two-item screener asking about usual intake of fruits and vegetables per day (n 1)( 19 ), brief screeners or FFQ (e.g. BRFSS( 37 ), the National Cancer Institute Fruit and Vegetable Screener( 32 , 36 ) or the Block Food Frequency Questionnaire( 16 – 18 ); n 4), a 7 d food diary (n 1)( 24 – 26 ) or multiple 24 h dietary recalls (n 1)( 22 , 23 ).
Change in fruit and vegetable intake
With one exception( 19 ), all studies in this category reported mean within-person change in fruit and vegetable intake from baseline to follow-up. Depending on the sampling strategy used, these results could be presented in three ways: (i) change in fruit and vegetable intake among shoppers at the new retailer; (ii) change in fruit and vegetable intake among residents of the neighbourhood where the new retailer opened; or (iii) the differencein-differences comparing mean change in fruit and vegetable intake among residents of the intervention v. comparison neighbourhood (Table 2).
Table 2.
Effect sizes of the impact of the opening of a new retailer of healthy foods on within-person change in fruit and vegetable consumption among adults (n 6)
| Reference(s) | Retailer | Country | Outcome measure | Sample | Mean difference | 95 % CI or statistical significance | Follow-up interval |
|---|---|---|---|---|---|---|---|
| Change in fruit and vegetable intake among adult shoppers at the retailer | |||||||
| Abusabha et al. ( 37 ) | Mobile market | USA | BRFSS screener | Forty-three adults aged ≥55 years | +0·45 servings | −0·23, 1·14 | 6 months |
| Freedman et al. ( 32 ) | Farmers’ market | USA | NCI FVS | Forty-one adults with diagnosis of diabetes | +0·54 servings | −1·14, 2·23 | 5 months |
| Wrigley et al. & Gill and Rudkin( 24 – 27 ) | Supermarket | UK | 7 d food diaries | 276 adults | +0·23 portions | P=0·034 | 6–7 months |
| Dubowitz et al. ( 22 , 23 ) | Supermarket | USA | Two 24 h dietary recalls | 368 adults | −0·32 servings | NS | 7–14 months |
| Change in fruit and vegetable intake among adult residents of neighbourhood that received new retailer | |||||||
| Evans et al. ( 36 ) | Fruit and vegetable stand/market | USA | NCI FVS | Sixty-one adults | +0·42 servings | sd=2·49, P=0·210 | 2 months |
| Wrigley et al. & Gill and Rudkin( 24 – 27 ) | Supermarket | UK | 7 d food diary | 615 adults who were responsible for domestic food arrangements for the household | +0·04 portions* | NS | 6–7 months |
| Cummins et al. ( 16 – 18 ) | Supermarket | UK | Two-item screener assessing usual daily intake | 191 adults who were the main food shopper for their homes | +0·29 portions | P=0·07 | 11 months |
| Dubowitz et al. ( 22 , 23 ) | Supermarket | USA | Two 24 h dietary recalls | 571 adults who were the primary food shopper for their homes | −0·27 servings | se=0·08, P<0·001 | 7–14 months |
| Difference-in-difference in fruit and vegetable intake comparing adult residents of intervention v. comparison neighbourhood | |||||||
| Cummins et al. ( 16 – 18 ) | Supermarket | UK | Two-item screener assessing usual daily intake | 412 adults | −0·15* | NR | 11 months |
| Dubowitz et al. ( 22 , 23 ) | Supermarket | USA | Two 24 h dietary recalls | 831 adults who were the primary food shopper for their homes | −0·14 | NS | 7–14 months |
BRFSS, Behavioral Risk Factor Surveillance System; NCI FVS, National Cancer Institute Fruit and Vegetable Intake Screener; NR, not reported.
Result was calculated by hand based on information provided in the article.
Of the five studies that reported change in fruit and vegetable intake among shoppers at the new retailer, most reported modest, albeit not always statistically significant, increases in mean intake (n 4)( 24 – 26 , 32 , 37 ), although one study reported a small decrease( 22 , 23 ). For example, one study of forty-three shoppers at a mobile market in Troy, New York, USA reported a statistically insignificant 0·45-serving increase in daily fruit and vegetable intake six months after the market expanded its route to serve additional stops (95 % CI −0·23, 1·14)( 37 ). Another study of forty-one diabetic adults who shopped at a farmers’ market in a health clinic in rural South Carolina, USA reported a statistically insignificant 0·54-serving increase in fruit and vegetable intake five months after it opened (95 % CI −1·14, 2·23)( 32 ). Another study of 276 shoppers at a new supermarket in Leeds, UK reported a statistically significant 0·23-portion increase in fruit and vegetable intake six to seven months after it opened (P=0·034)( 24 – 27 ). However, a study of 368 shoppers at a new supermarket in Philadelphia, Pennsylvania, USA reported a statistically insignificant −0·32-serving decrease in intake seven to fourteen months after it opened( 22 , 23 ).
Results were less consistent among the four studies that assessed change in intake among residents of the neighbourhood where the new retailer opened for business. For example, one study of 615 residents found essentially no change in fruit and vegetable consumption six to seven months after the opening of a new supermarket in their neighbourhood in Leeds, UK (mean difference=0·04 portions/d)( 24 – 27 ). However, two studies found evidence of modest, but not statistically significant, increases in fruit and vegetable intake. The first reported a statistically insignificant 0·42-serving increase in daily intake among a probability sample of sixty-one adults who lived within 0·8 km (0·5) miles of a new fruit and vegetable stand in Austin, Texas, USA two months after it opened( 36 ). The other study found a 0·29-portion increase among a probability sample of 191 adults who were the main food shoppers for their homes and lived in a Glasgow, UK neighbourhood where a new supermarket was opened at 11-month follow-up (P=0·07)( 16 – 18 ). In contrast to these results, a study that included a probability sample of 571 adults living in a neighbourhood in Philadelphia, Pennsylvania, USA where a new supermarket opened, reported a statistically significant 0·27-serving decrease in fruit and vegetable consumption at 6-month follow-up (se=0·08, P<0·001)( 22 , 23 ).
Two studies reported difference-in-differences comparing change among residents of the neighbourhood where the new retailer opened, relative to change among residents in a comparison neighbourhood. These studies evaluated supermarket openings in Pittsburgh, Pennsylvania, USA( 22 , 23 ) and Glasgow, UK( 16 – 18 ). In both instances, results were the opposite of what was expected and indicated either greater increases in fruit and vegetable intake among the comparison neighbourhood residents (difference-in-differences=−0·15)( 16 – 18 ) or smaller decreases in fruit and vegetable intake among comparison neighbourhood residents (difference-in-differences=−0·14)( 22 , 23 ).
Discussion
Most studies included in the present review focused on recent openings of healthy food retailers in low-income communities with limited access to healthy foods. The methodological approaches to evaluating these initiatives, including the research designs, sampling approaches, follow-up intervals and outcome measures, varied widely. Although all study designs were limited in their ability to causally attribute any observed change in fruit and vegetable consumption to the opening of the retailer itself, evaluations of supermarket and grocery store openings tended to use more rigorous study designs (e.g. two-group repeated measure or repeated cross-sectional designs with larger representative samples), while evaluations of farmers’ markets, fruit and vegetable stands, and mobile markets tended to use weaker designs (e.g. post-test only designs with smaller convenience samples).
Across study types, results suggest that the dietary impact of the new retailer may be greatest among adults who choose to shop there. For example, three out of four repeated measures studies of shoppers at the new retailer found modest increases in fruit and vegetable consumption, ranging from 0·23 to 0·54 daily servings at 6–12 months follow-up( 24 – 27 , 32 , 37 ). Although most of these effect sizes did not reach statistical significance, two reported small sample sizes, calling into question whether they were powered to detect dietary change of this magnitude. These effect sizes are similar in magnitude to those reported by a systematic review of behavioural interventions to increase fruit and vegetable intake( 39 ), and prior research has documented that even small increases in fruit and vegetable intake may be related to reductions in energy density( 40 ). Additionally, results from all three post-test only designs that surveyed shoppers at the new retailer found that relatively high proportions of shoppers reported they were eating more fruits and vegetables since starting to shop there (55–98 %)( 33 – 35 ).
The impact of the opening of a new retailer on fruit and vegetable consumption among the broader community of residents of the neighbourhood where the retailer opened was less clear. Studies that used either repeated measures or repeated cross-sectional designs found no evidence of change( 24 – 27 , 29 , 30 ), modest increases( 16 – 18 , 20 , 21 , 28 , 36 ) or decreases( 20 – 23 ) in fruit and vegetable consumption. The variability in results may be explained in part by the heterogeneity in methodological approaches used, including eligibility criteria and methods used to sample intervention neighbourhood residents. Those that also sampled from a comparison neighbourhood were unable to detect a significant difference in mean change in fruit and vegetable consumption between the two groups.
We are limited in our ability to comment on differential dietary impact by retailer type due to the methodological heterogeneity among studies included in the present review. However, evaluations of one category of retailer – supermarkets – tended to have the most methodological consistency, with four out of five studies employing a repeated measures design. These studies found mixed results regarding the impact of the new retailer on fruit and vegetable consumption among shoppers( 22 – 27 ), residents of the intervention community( 16 – 18 , 22 – 27 ), and differences between residents of intervention and comparison communities( 16 – 18 , 22 , 23 ). Although previous reviews have documented systematic disparities in access to supermarkets among many neighbourhoods throughout the USA( 5 ), research regarding the causal links between access to supermarkets and improved dietary intake is inconclusive( 6 ). In the light of the large-scale initiatives focused on policy, systems and environmental changes to improve community retail food environments, many of which focus on introducing supermarkets into low-income communities, more rigorous research with greater methodological consistency is needed regarding the impact of supermarkets on dietary behaviour( 12 – 15 , 41 ).
A strength of the present review is that it is the first to our knowledge to summarize the state of scientific knowledge regarding the potential dietary impact of opening new retailers of healthy foods within a community. Limitations of the review include potential publication bias and incomplete retrieval of relevant articles from the keyword search strategy. Additionally, most studies evaluated the dietary impact of the opening of new retailers within low-income neighbourhoods with limited access to healthy foods in the USA. The extent to which these findings would generalize to other geographic contexts (e.g. developing countries, non-Western contexts, etc.) is unknown. Additionally, the review focused exclusively on the impact of these retailers on fruit and vegetable intake among adults. The impact on fruit and vegetable intake among children or on other outcomes relevant to dietary behaviour or chronic disease prevention remains unknown. Many articles that were considered for( 42 , 43 ) or included in the present review( 20 – 23 ), or have been published since( 44 – 46 ), assessed other outcomes of interest, including area-level access to healthy foods, change in other dietary behaviours (e.g. change in total energy intake, dietary quality, consumption of specific food groups) or BMI. These may be outcomes of potential interest for future reviews.
Results from the present review suggest that opening a new retailer of healthy foods in limited-access communities may be an appropriate strategy to improve short-term fruit and vegetable intake among adults who choose to shop there, although more research is needed to confirm these findings and to understand the potential impact of this approach on the broader community and/or over longer periods of time. Interventions that focus on other structural interventions, such as improving the in-store environments of existing retailers, may be a more appropriate strategy for improving population-level dietary behaviour( 47 , 48 ). Limitations of this body of research include a reliance on pre-experimental or quasi-experimental designs with limited ability to establish causality, potentially underpowered studies reliant on small sample sizes, and the use of a range of outcome measures and follow-up intervals that prevents meta-analytic synthesis of results. Recommendations for future research include designing adequately powered studies that are methodologically aligned with those of previous work, to facilitate comparisons and summary of these initiatives and strengthen the evidence base regarding this potential dietary impact of this approach to improving community food environments.
Acknowledgements
Acknowledgements: The authors acknowledge with gratitude the contributions of Michael Goodman, MD, MPH for his assistance with developing the protocol for this review. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. Financial support: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. Conflict of interest: None. Authorship: R.C.W. designed the study, performed the study search, abstracted and analysed the data, and prepared the manuscript. I.G.R. abstracted the data and assisted with the preparation of the manuscript. D.M.H., J.A.G., M.K., R.H. and M.C.K. provided oversight of the project and assisted with the preparation of the manuscript. Ethics of human subject participation: Not applicable.
References
- 1. Brownson RC, Haire-Joshu D & Luke DA (2006) Shaping the context of health: a review of environmental and policy approaches in the prevention of chronic diseases. Annu Rev Public Health 27, 341–370. [DOI] [PubMed] [Google Scholar]
- 2. Glanz K, Sallis JF, Saelens BE et al. (2005) Healthy nutrition environments: concepts and measures. Am J Health Promot 19, 330–333. [DOI] [PubMed] [Google Scholar]
- 3. Story M, Kaphingst KM, Robinson-O’Brien R et al. (2008) Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health 29, 253–272. [DOI] [PubMed] [Google Scholar]
- 4. Frieden TR (2010) A framework for public health action: the health impact pyramid. Am J Public Health 100, 590–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Larson NI, Story MT & Nelson MC (2009) Neighborhood environments: disparities in access to healthy foods in the US. Am J Prev Med 36, 74–81. [DOI] [PubMed] [Google Scholar]
- 6. Caspi CE, Sorensen G, Subramanian SV et al. (2012) The local food environment and diet: a systematic review. Health Place 18, 1172–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moore LV & Diez Roux AV (2006) Associations of neighborhood characteristics with the location and type of food stores. Am J Public Health 96, 325–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zenk SN, Schulz AJ, Israel BA et al. (2005) Neighborhood racial composition, neighborhood poverty, and the spatial accessibility of supermarkets in metropolitan Detroit. Am J Public Health 95, 660–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fleischhacker SE, Evenson KR, Rodriguez DA et al. (2011) A systematic review of fast food access studies. Obes Rev 12, e460–e471. [DOI] [PubMed] [Google Scholar]
- 10. US Department of Health and Human Services (2016) Healthy People 2020 Objectives. https://www.healthypeople.gov/2020/topics-objectives/topic/nutrition-and-weight-status/objectives (accessed May 2011).
- 11. Office of Community Services (2017) Healthy Food Financing Initiative 2010. https://www.acf.hhs.gov/ocs/programs/community-economic-development/healthy-food-financing (accessed August 2017).
- 12. The Reinvestment Fund (2015) Pennsylvania Fresh Food Financing Initiative. http://www.trfund.com/pennsylvania-fresh-food-financing-initiative/ (accessed May 2015).
- 13. New York City Office of the Mayor (n.d.) Food Retail Expansion to Support Health (FRESH). http://www.nyc.gov/html/misc/html/2009/fresh.shtml (accessed May 2015).
- 14. California FreshWorks Fund (n.d.) Fresh Works. http://cafreshworks.com/ (accessed November 2016).
- 15. City of New Orleans (n.d.) Fresh Food Retailers Initiative. http://www.nola.gov/city/fresh-food-retailers-initiative/ (accessed November 2016).
- 16. Cummins S, Findlay A, Higgins C et al. (2008) Reducing inequalities in health and diet: findings from a study on the impact of a food retail development. Environ Plan A 40, 402–422. [Google Scholar]
- 17. Cummins S, Findlay A, Petticrew M et al. (2008) Retail-led regeneration and store-switching behaviour. J Retail Consum Serv 15, 288–295. [Google Scholar]
- 18. Cummins S, Petticrew M, Higgins C et al. (2005) Large scale food retailing as an intervention for diet and health: quasi-experimental evaluation of a natural experiment. J Epidemiol Community Health 59, 1035–1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cummins S, Flint E & Matthews SA (2014) New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff (Millwood) 33, 283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Elbel B, Mijanovich T, Kiszko K et al. (2015) The introduction of a supermarket via tax-credits in a low-income area: the influence on purchasing and consumption. Am J Health Promot 31, 59–66. [DOI] [PubMed] [Google Scholar]
- 21. Elbel B, Moran A, Dixon LB et al. (2015) Assessment of a government-subsidized supermarket in a high-need area on household food availability and children’s dietary intakes. Public Health Nutr 18, 2881–2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dubowitz T, Ghosh-Dastidar M, Cohen DA et al. (2015) Diet and perceptions change with supermarket introduction in a food desert, but not because of supermarket use. Health Aff (Millwood) 34, 1858–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dubowitz T, Ncube C, Leuschner K et al. (2015) A natural experiment opportunity in two low-income urban food desert communities: research design, community engagement methods, and baseline results. Health Educ Behav 42, 1 Suppl., 87S–96S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wrigley N, Warm D & Margetts B (2003) Deprivation, diet, and food-retail access: findings from the Leeds ‘food deserts’ study. Environ Plan A 35, 151–188. [Google Scholar]
- 25. Wrigley N, Warm D, Margetts B et al. (2004) The Leeds ‘food deserts’ intervention study: what the focus groups reveal. Int J Retail Distrib Manag 32, 123–136. [Google Scholar]
- 26. Wrigley N, Warm D, Margetts B et al. (2002) Assessing the impact of improved retail access on diet in a ‘food desert’: a preliminary report. Urban Stud 39, 2061–2082. [Google Scholar]
- 27. Gill L & Rudkin S (2014) Deconstructing supermarket intervention effects on fruit and vegetable consumption in areas of limited retail access: evidence from the Seacroft Study. Environ Plan A 46, 649–665. [Google Scholar]
- 28. Wang MC, MacLeod KE, Steadman C et al. (2007) Is the opening of a neighborhood full-service grocery store followed by a change in the food behavior of residents? J Hunger Environ Nutr 2, 3–18. [Google Scholar]
- 29. Sadler RC, Gilliland JA & Arku G (2013) A food retail-based intervention on food security and consumption. Int J Environ Res Public Health 10, 3325–3346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sadler RC, Gilliland JA & Arku G (2013) Community development and the influence of new food retail sources on the price and availability of nutritious food. J Urban Aff 35, 471–491. [Google Scholar]
- 31. Freedman D (2007) A community health case study: creating a food oasis in a food desert. Community Psychol 40, 67–70. [Google Scholar]
- 32. Freedman DA, Choi SK, Hurley T et al. (2013) A farmers’ market at a federally qualified health center improves fruit and vegetable intake among low-income diabetics. Prev Med 56, 288–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ruelas V, Iverson E, Kiekel P et al. (2012) The role of farmers’ markets in two low income, urban communities. J Community Health 37, 554–562. [DOI] [PubMed] [Google Scholar]
- 34. Payet J, Gilles M & Howat P (2005) Gascoyne Growers Market: a sustainable health promotion activity developed in partnership with the community. Aust J Rural Health 13, 309–314. [DOI] [PubMed] [Google Scholar]
- 35. Woodruff RC, Coleman AM, Hermstad AK et al. (2016) Increasing community access to fresh fruits and vegetables: a case study of the Farm Fresh Market pilot program in Cobb County, Georgia, 2014. Prev Chronic Dis 13, E36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Evans AE, Jennings R, Smiley AW et al. (2012) Introduction of farm stands in low-income communities increases fruit and vegetable among community residents. Health Place 18, 1137–1143. [DOI] [PubMed] [Google Scholar]
- 37. Abusabha R, Namjoshi D & Klein A (2011) Increasing access and affordability of produce improves perceived consumption of vegetables in low-income seniors. J Am Diet Assoc 111, 1549–1555. [DOI] [PubMed] [Google Scholar]
- 38. Jennings A, Cassidy A, Winters T et al. (2012) Positive effect of a targeted intervention to improve access and availability of fruit and vegetables in an area of deprivation. Health Place 18, 1074–1078. [DOI] [PubMed] [Google Scholar]
- 39. Ammerman AS, Lindquist CH, Lohr KN et al. (2002) The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence. Prev Med 35, 25–41. [DOI] [PubMed] [Google Scholar]
- 40. Williams RA, Roe LS & Rolls BJ (2013) Comparison of three methods to reduce energy density. Effects on daily energy intake. Appetite 66, 75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bunnell R, O’Neil D, Soler R et al. (2012) Fifty communities putting prevention to work: accelerating chronic disease prevention through policy, systems and environmental change. J Community Health 37, 1081–1090. [DOI] [PubMed] [Google Scholar]
- 42. Larsen K & Gilliland J (2009) A farmers’ market in a food desert: evaluating impacts on the price and availability of healthy food. Health Place 15, 1158–1162. [DOI] [PubMed] [Google Scholar]
- 43. Lucan SC, Maroko A, Shanker R et al. (2011) Green Carts (mobile produce vendors) in the Bronx – optimally positioned to meet neighborhood fruit and vegetable needs? J Urban Health 88, 977–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chrisinger B (2016) A mixed-method assessment of a new supermarket in a food desert: contributions to everyday life and health. J Urban Health 93, 425–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Engler-Stringer R, Muhajarine N, Ridalls T et al. (2016) The Good Food Junction: a community-based food store intervention to address nutritional health inequities. JMIR Res Protoc 5, e52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zhang YT, Laraia BA, Mujahid MS et al. (2016) Is a reduction in distance to nearest supermarket associated with BMI change among type 2 diabetes patients? Health Place 40, 15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Escaron AL, Meinen AM, Nitzke SA et al. (2013) Supermarket and grocery store-based interventions to promote healthful food choices and eating practices: a systematic review. Prev Chronic Dis 10, E50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Liberato SC, Bailie R & Brimblecombe J (2014) Nutrition interventions at point-of-sale to encourage healthier food purchasing: a systematic review. BMC Public Health 14, 919. [DOI] [PMC free article] [PubMed] [Google Scholar]