Abstract
Objectives
The objectives were to collect baseline data on the occurrence, testing and vaccination practices, and clinical outcomes of feline leukaemia virus (FeLV) and feline immunodeficiency virus (FIV) in New Zealand
Methods
A cross-sectional survey of 423 veterinary practices in New Zealand was performed to collect data on FeLV and FIV testing and vaccination during the 2015 calendar year. Clinical records from 572 cats tested using a point-of-care ELISA at a first-opinion veterinary practice between 7 April 2010 and 23 June 2016 were also obtained and multivariable logistic regression models were constructed to identify risk factors for test positivity. Survival times were estimated using Kaplan–Meier methods.
Results
The survey was completed by 112 clinics (26.4%) of which 72 performed in-house testing. Of the 2125 tests performed, 56 (2.6%) were positive for FeLV and 393 (18.5%) were positive for FIV. Fewer than 1% of cats were vaccinated for FeLV, with veterinarians citing low perceived prevalence as the primary reason for not vaccinating. Being male compared with being female and having clinical evidence of immunosuppression were significant risk factors for both FeLV and FIV test positivity. The median survival times of FeLV and FIV test-positive cats were 10 days (95% confidence interval [CI] 0–16) and 650 days (95% CI 431–993), respectively.
Conclusions and relevance
Testing and vaccination for FeLV and FIV in New Zealand appears targeted towards high-risk animals, which may bias prevalence estimates. Baseline data should be monitored for changes in FeLV epidemiology now commercial vaccines are no longer available.
Introduction
Feline leukaemia virus (FeLV) and feline immunodeficiency virus (FIV) are important pathogens causing clinical disease in domestic cats worldwide.1 The prevalences reported in the literature vary widely depending on the geographical location and clinical characteristics of the study populations,2 with infections less commonly reported in healthy cats and confined cats compared with clinically unwell cats and free-roaming cats.3–8 Both viruses spread directly through bite wounds.3,9,10 Sexual contact, vertical transmission and social interactions such as mutual grooming or shared food or water dishes are more important transmission pathways for FeLV than FIV.11,12 Unsurprisingly, cats that are aggressive, sexually intact, frequently in contact with other cats or observed fighting have been identified as being significantly more likely to test positive for either pathogen.8,13–15 Experimental studies have shown that susceptibility to FeLV decreases significantly with age, with almost 100% of newborn kittens developing persistent viraemia after inoculation vs only 15% of kittens over 4 months of age.16,17 Since there are currently no effective treatments for FeLV and FIV,18 the cornerstone of disease management in clinical practice is preventing new infections through vaccination or segregation.19 Many cats diagnosed with FeLV die or are euthanased within 2–3 years owing to clinical complications,20 while FIV-positive cats can remain asymptomatic for many years.21,22 Diagnostic testing is therefore important for determining the infection status of cats to inform clinical decisions,23 but may not be performed routinely in private practice.24
FeLV and FIV are both endemic in the New Zealand domestic cat population, yet relatively little is known about their epidemiology. Two studies published in the early 1980s reported the prevalence of FeLV in cattery populations at between 4.4% and 11%,25,26 while another more recent study from 2013 estimated the national prevalences of FeLV and FIV at 5.5% and 10%, respectively, based on 200 blood samples submitted to a commercial diagnostic laboratory for routine haematological testing.27 There has also been some recent work to characterise the molecular epidemiology of FIV in New Zealand to determine whether the commercially available vaccine is likely to be effective against the currently circulating subtypes.28,29 However, since vaccination against FIV is relatively uncommon in New Zealand,30 and the last commercially available vaccine for FeLV was removed from the domestic market in March 2016 owing to low sale volumes, these tools are not currently being utilised to protect patient populations. Gathering better baseline data on disease occurrence, risk factors and clinical outcomes will be important for guiding discussions on how we can better manage these diseases moving forward.
The objectives of this study were therefore: (1) to collect updated data on the occurrence of FeLV and FIV in New Zealand through a national survey of companion animal veterinary clinics; (2) to assess veterinarians’ opinions towards testing and vaccination for FeLV after the last commercially available FeLV vaccine was removed from the domestic market; and (3) to conduct a preliminary investigation into the risk factors and clinical outcomes for client-owned animals diagnosed with FeLV and/or FIV through point-of-care testing.
Materials and methods
National clinic survey data
A cross-sectional survey was emailed to the 423 registered veterinary practices in New Zealand on 25 May 2016 to collect quantitative data on in-house testing and vaccination for FeLV and FIV performed during the 2015 calendar year. Veterinarians were also asked to provide their opinions on the safety, efficacy and cost of FeLV vaccines using Likert-scale ratings and free-text comment fields. A reminder email was sent to all veterinary practices 1 month after the initial email and then a hard copy of the survey was mailed to the remaining non-responders 2 weeks later. The survey closed on 25 September 2016 with a total of 112 responses. A full copy of the survey is available from the corresponding author upon request.
First-opinion practice data
The electronic medical records from a first-opinion veterinary practice in Waimate, New Zealand, were searched for all invoiced in-house SNAP FIV/FeLV Combo tests (IDEXX Laboratories) performed between 7 April 2010 and 23 June 2016. This practice was selected for convenience since the authors had direct access to the clinical records. The search yielded 620 test records for 601 individual cats. Records from 29 cats with unrecorded test results were excluded leaving 572 cats in the final study sample. Basic descriptive data, including the name, client code, date of birth, date of testing, breed, sex, neutering status and postcode, were downloaded from the electronic records. The date of birth and date of testing were used to determine age at testing, which was subsequently categorised into four groups: under 1 year; 1–5 years; 5–10 years; and over 10 years of age. Cat breed was categorised into two groups: ‘domestic’ (including domestic shorthair, domestic mediumhair and domestic longhair breeds) and ‘purebred’ (including all other defined breeds).
The free-text field of the clinical records was then manually reviewed to collect data on the history and physical examination findings on the date of initial testing. The data were categorised into the following binary variables describing the presence or absence of lethargy, anorexia, chronic diarrhoea (based on the subjective reports of the owner), weight loss (if this was recorded as a presenting complaint or if the patient lost <10% of its body weight since the last recorded visit), pyrexia (if the body temperature was >39.3°C), anaemia (if the cat was described as have pale mucous membranes or consistent haematological parameters), inflammatory oral disease (if the cat had gingivitis that was more severe than the degree of dental disease warranted), lymphoma (based on histopathology or clinical signs such as generalised lymphadenopathy or consistent thoracic masses on radiography) and immunosuppression (based on the presence of leukopenia on haematology or the presence of chronic or refractory infections). Cats were classified as having clinical signs consistent with FeLV or FIV if at least one of these recorded clinical signs was present. Additionally, information was collected on the presumed reason for testing (presence of compatible clinical signs, known exposure to another infected cat or testing prior to vaccination) and the number of times the cat previously presented to the clinic for a suspected cat fight (categorised as either zero, one or more than one incident).
Records from subsequent visits were then examined to determine if any follow-up testing was performed to confirm the positive FeLV results. For cats that were euthanased or known to have died, the date of death was recorded. For all other cats, the most recent date the cat was known to be alive (either through a clinic consultation or other forms of client communication) was recorded.
Statistical analysis
The prevalence of positive FeLV and FIV test results was estimated at both the practice level and national level by taking the total number of positive tests divided by the total number of tests performed. Basic descriptive statistics were provided on the testing and vaccination practices reported by the veterinary clinics in the national survey, as well as the demographic characteristics of patients tested for FeLV and FIV at the first-opinion veterinary practice.
Separate multivariable logistic regression models were then constructed for FeLV and FIV to identify risk factors associated with test positivity. Univariable analyses were performed using a χ2 test (for variables with more than five observations in all cells) and Fisher’s exact test (for variables with fewer than five observations in at least one cell) to identify risk factors associated with the outcome of interest at a P value <0.2 for inclusion in the multivariable analysis.
A backwards stepwise process was then used to select variables for the final models. All variables with a P value <0.05 were retained. The results from the univariable and multivariable analyses were reported as odds ratios (ORs) and 95% confidence intervals (CIs). Survival curves for FIV-positive cats, FeLV-positive cats and FeLV/FIV-negative cats were estimated by the Kaplan–Meier product limit method. For cats with no recorded euthanasia or death event, the survival times were right-censored at the last recorded date the cat was seen at the practice or the last recorded phone conversation where the cat was known to be alive. The log-rank test for censored data was used to compare difference in survival times between FIV-positive vs FIV-negative and FeLV-positive vs FeLV-negative cats. All statistical analyses were performed using R statistical software.31
Results
National clinic survey
The national survey was completed by 112/423 (26.5%) registered veterinary practices in New Zealand. Of the 112 respondents, 72 (64.3%) performed point-of-care FeLV and FIV tests in their practice during the 2015 calendar year with 51 (70.8%) using the IDEXX SNAP FIV/FeLV Combo Test, 10 (13.9%) using the InSight FIV-FeLV Combi Rapid Diagnostic Test (Woodley Equipment), six (8.3%) using the FASTest FeLV-FIV test (Megacor Diagnostik) and five (6.9%) using the SensPERT FeLV Ag/FIV Ab Test (VetAll Laboratories). An estimated 2125 in-house tests were performed in a patient population of approximately 120,000 cats, meaning that <2% of cats were tested annually.
The overall prevalence of FIV-positive tests was 18.5%, whereas the overall prevalence of FeLV-positive tests was 2.6%. Most veterinary practices (67.3%) used the test to check for FIV only rather than to screen for both diseases (31.2%) or to screen for FeLV only (1.6%). The primary reason for running the in-house test was because the patient was showing compatible clinical signs (60.2% for FIV and 71.4% for FeLV). A smaller percentage of tests were run for routine screening (22.7% for FIV and 24.1% for FeLV) or because the cat was exposed to an infected individual (17.1% for FIV and 4.5% for FeLV). Only seven practices (9.7%) performed repeat and/or confirmatory testing for positive in-house results.
Most veterinary practices never (70/112; 62.5%) or rarely (29/112 or 25.9%) vaccinated against FeLV. Only an estimated 0.2% of cats were vaccinated during the 2015 calendar year with the most common reasons being requested by the owner (29.7%), exposure to infected cats (25.3%), routine vaccination (25.3%), cat at risk being outdoors (5.4%) and other reasons (21.3%). The low perceived prevalence of disease was highlighted as the main reason for not vaccinating against FeLV in the Likert-rating questions (Table 1) and free-text survey comments.
Table 1.
Level of veterinarian agreement with statements regarding reasons for not vaccinating against feline leukaemia virus (FeLV) based on data from 112 clinics participating in a national survey
| Question* | Strongly disagree | Disagree | Neither agree nor disagree | Agree | Strongly agree |
|---|---|---|---|---|---|
| The prevalence of FeLV in my practice area is too low | 3 (2.8) |
4 (3.8) |
14 (13.2) |
34 (32.1) | 51 (48.1) |
| The cost of vaccination is prohibitive to my clients | 10 (9.4) |
29 (27.4) |
50 (47.2) |
13 (12.3) |
4 (3.8) |
| The risks of adverse effects from the vaccine are not outweighed by the benefits | 5 (4.7) |
22 (20.8) |
38 (35.8) |
27 (25.5) |
14 (13.2) |
| The vaccine does not provide adequate protection against FeLV | 5 (4.7) |
24 (22.6) |
67 (63.2) |
7 (6.6) |
2 (1.9) |
Data are n (%)
Six survey respondents did not provide answers to these questions
First-opinion practice data
Of the 572 cats with recorded test results, 29 (5.1%) were positive for FeLV antigen only, 91 (15.9%) were positive for FIV antibody only and 12 (2.1%) were positive for both FIV and FeLV. The remaining 440 cats (76.9%) tested negative for both diseases. Descriptive statistics on the signalment and clinical variables stratified by test status are presented in Table 2 along with the results from the univariable analyses. Only 2/41 FeLV-positive cats (4.9%) were retested with a confirmatory FeLV PCR. One was PCR positive and the other was PCR negative. Two of the FIV-positive cats were retested with a repeat FIV antibody SNAP test, both of which remained positive.
Table 2.
Descriptive statistics on the signalment and clinical characteristics of 572 cats tested for feline leukaemia virus (FeLV) and feline immunodeficiency virus (FIV) using a commercially available point-of-care ELISA kit at a first-opinion veterinary practice in New Zealand between 7 April 2010 and 23 June 2016
| FeLV positive |
FIV positive |
|||||
|---|---|---|---|---|---|---|
| Variable | Levels | All cats | n (%) | P value* | n (%) | P value* |
| Age (years) | <1 | 52 | 2 (3.8) | – | 1 (1.9) | – |
| 1–5 | 210 | 16 (7.6) | 0.349 | 21 (10) | 0.094 | |
| 5–10 | 154 | 16 (10.3) | 0.172 | 41 (26.6) | 0.004 | |
| >10 | 126 | 4 (3.2) | 0.822 | 32 (25.4) | 0.006 | |
| Breed | Domestic | 509 | 38 (7.4) | – | 101 (19.8) | – |
| Purebred | 60 | 3 (5.0) | 0.494 | 2 (3.3) | 0.007 | |
| Sex | Female | 231 | 6 (2.6) | – | 24 (10.4) | – |
| Male | 321 | 31 (9.6) | 0.002 | 76 (23.7) | <0.001 | |
| Neutering status | Neutered | 455 | 30 (6.6) | – | 70 (15.4) | – |
| Entire | 25 | 1 (4.0) | 0.616 | 3 (12.0) | 0.647 | |
| Previous cat bites | 0 | 361 | 26 (7.2) | – | 56 (15.5) | – |
| 1 | 103 | 9 (8.8) | 0.598 | 21 (20.4) | 0.242 | |
| >2 | 103 | 6 (5.7) | 0.601 | 26 (25.2) | 0.024 | |
| Lethargy | Absent | 382 | 9 (2.4) | – | 62 (16.2) | – |
| Present | 158 | 27 (16.8) | <0.001 | 31 (19.6) | 0.343 | |
| Anorexia | Absent | 363 | 12 (3.3) | – | 59 (16.3) | – |
| Present | 184 | 25 (13.4) | <0.001 | 40 (21.7) | 0.117 | |
| Weight loss | Absent | 420 | 18 (4.3) | – | 62 (14.8) | – |
| Present | 135 | 20 (14.7) | <0.001 | 37 (27.4) | 0.001 | |
| Chronic diarrhoea | Absent | 554 | 40 (7.2) | – | 100 (18.1) | – |
| Present | 6 | 0 (0) | 0.989 | 1 (16.7) | 0.93 | |
| Pyrexia | Absent | 231 | 13 (5.6) | – | 38 (16.5) | – |
| Present | 72 | 16 (21.3) | <0.001 | 16 (22.2) | 0.266 | |
| Anaemia | Absent | 530 | 28 (5.3) | – | 92 (17.4) | – |
| Present | 33 | 13 (39.4) | <0.001 | 10 (30.3) | 0.066 | |
| Inflammatory oral disease | Absent | 496 | 34 (6.8) | – | 84 (16.9) | – |
| Present | 66 | 7 (10.6) | 0.269 | 18 (27.3) | 0.043 | |
| Lymphoma | Absent | 543 | 34 (6.2) | – | 98 (18.0) | – |
| Present | 18 | 6 (31.6) | <0.001 | 3 (16.7) | 0.881 | |
| Immunosuppression | Absent | 481 | 23 (4.8) | – | 74 (15.4) | – |
| Present | 79 | 16 (19.8) | <0.001 | 27 (34.2) | <0.001 | |
| Clinical signs of FeLV/FIV | Absent | 196 | 2 (1.0) | – | 20 (10.2) | – |
| Present | 373 | 39 (10.4) | 0.001 | 83 (22.3) | 0.001 | |
| Other systemic illness | Absent | 318 | 23 (7.2) | – | 54 (17.0) | – |
| Present | 247 | 17 (6.8) | 0.86 | 47 (19.0) | 0.529 | |
| Known FeLV/FIV exposure | No | 545 | 39 (7.1) | – | 98 (18.0) | NA |
| Yes | 24 | 2 (8.0) | 0.877 | 5 (20.8) | 0.723 | |
| Prior to FeLV/FIV vaccination | No | 467 | 40 (7.2) | – | 98 (21.0) | – |
| Yes | 102 | 1 (7.1) | 0.997 | 5 (4.9) | 0.001 | |
The P values are based on a χ2 test for variables with >5 observations in all cells and a Fisher’s exact test for variables with <5 observations in at least one cell
NA = not applicable
The majority of FeLV-positive cats (95.1%; n = 39/41) had at least one compatible clinical sign (mean 3.6, median 4, range 0–7). The most common clinical signs were lethargy (65.9%; n = 27/41), anorexia (61.0%; n = 25/41) and weight loss (48.8%; n = 20/41). Only 36.6% (n = 15/41) of FeLV-positive cats had a recorded history of treated cat bites. In the multivariable model (Table 3), the presence of anaemia, pyrexia and immunosuppression were significantly associated with FeLV positivity. Sex was also found to be significant, with male cats being 4.63 times more likely to be positive than females (95% CI 1.60–17.00).
Table 3.
Multivariable analysis of risk factors associated with feline leukaemia virus (FeLV) test positivity among 572 patients tested for FeLV and feline immunodeficiency virus using a commercially available point-of-care ELISA kit at a first-opinion veterinary practice in New Zealand between 7 April 2010 and 23 June 2016
| Variable | Levels | OR | 95% CI | P value |
|---|---|---|---|---|
| Sex | Female | Ref | – | – |
| Male | 4.63 | 1.60–17.0 | 0.009 | |
| Anaemia | Absent | Ref | – | – |
| Present | 3.61 | 1.19–10.36 | 0.019 | |
| Pyrexia | Absent | Ref | – | – |
| Present | 3.75 | 1.52–9.45 | 0.004 | |
| Immunosuppression | Absent | Ref | – | – |
| Present | 3.42 | 1.35–8.60 | 0.009 |
OR = odds ratio; CI = confidence interval
The majority of FIV-positive cats (80.6%; n = 83/103) had at least one compatible clinical sign (mean 2.2, median 2, range 0–7) and, similar to FeLV, the most common clinical signs were lethargy (31/103; n = 30.1%), anorexia (40/103; n = 38.8%) and weight loss (35.9%; n = 37/103). Only 45.6% (n = 47/103) of FIV-positive cats had a history of treated cat bites. The multivariable model (Table 4) showed that being >5 years of age was associated with increased risk of FIV test positivity. Additionally, male cats, domestic breeds and cats with the presence of immunosuppression were also at significantly increased risk. In contrast, cats that were specifically being tested for FIV prior to vaccination were significantly less likely to be seropositive than cats that were tested for other reasons (OR 0.26, 95% CI 0.08–0.67; P = 0.013).
Table 4.
Multivariable analysis of risk factors associated with feline immunodeficiency virus (FIV) test positivity among 572 patients tested for feline leukaemia virus and FIV using a commercially available point-of-care ELISA kit at a first-opinion veterinary practice in New Zealand between 7 April 2010 and 23 June 2016
| Variable | Levels | OR | 95% CI | P value |
|---|---|---|---|---|
| Age (years) | <1 | Ref | – | – |
| 1–5 | 5.55 | 1.08–102 | 0.102 | |
| 5–10 | 18.39 | 3.65–335 | 0.005 | |
| >10 | 14.09 | 2.77–258 | 0.011 | |
| Sex | Female | Ref | – | – |
| Male | 2.79 | 1.64–4.90 | <0.001 | |
| Breed | Domestic | Ref | – | – |
| Purebred | 0.07 | 0.004–0.33 | 0.009 | |
| Immunosuppression | Absent | Ref | – | – |
| Present | 2.51 | 1.33–4.62 | 0.003 | |
| Prior to vaccination | No | Ref | – | – |
| Yes | 0.26 | 0.08–0.67 | 0.013 |
OR = odds ratio; CI = confidence interval
The median survival times of FeLV-positive and FIV-positive cats were 10 days (95% CI 0–16) and 650 days (95% CI 431–993), respectively. Median survival time of negative cats could not be calculated in this study as 264/440 negative cats (60.0%) were still alive at the end of the observation period. The majority of FeLV-positive cats (n = 29/41; 70.7%) were euthanased within 14 days of diagnosis (Figure 1). In contrast, only 21/102 FIV-positive cats (20.6%) died or were euthanased within 14 days of diagnosis. Long-term survival of the remainder of the FIV-positive cats was lower than FIV-negative cats (Figure 1). The log-rank tests showed that there was a significant difference in survival times between FeLV test positive cats and cats that were test negative for both FeLV and FIV (P <0.001) and between FeLV antigen-positive cats and cats that were test positive for FIV only (P <0.001).
Figure 1.
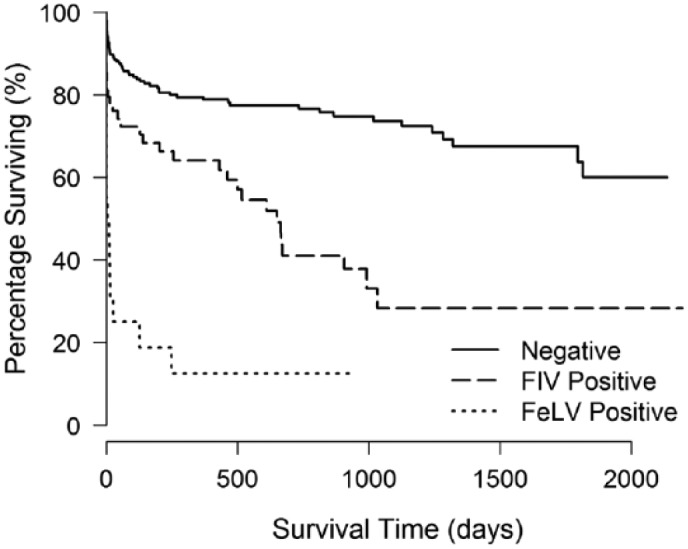
Kaplan–Meier curves for survival time of feline immunodeficiency virus (FIV) test positive, feline leukaemia virus (FeLV) test positive and FIV/FeLV-negative cats among 572 patients tested for FeLV and FIV using a commercially available point-of-care ELISA kit at a first-opinion veterinary practice in New Zealand between 7 April 2010 and 23 June 2016
Discussion
Our current study found that the occurrence of FeLV was 2.6% and the occurrence of FIV was 18.5% among predominantly client-owned cats across New Zealand. These results were markedly different from the 5.5% FeLV prevalence and 10% FIV prevalence reported in the previous cross-sectional study of random blood samples submitted to a diagnostic laboratory in New Zealand27 but broadly consistent with estimates from Australia, which were obtained from demographically similar populations.13,32
There are several possible reasons for our higher observed occurrence of FIV. First, veterinarians who responded to our survey indicated that the majority of cats were only tested because there was a high index of suspicion for disease, such as the presence of compatible clinical signs, known exposure to infected animals and presentation for bite wounds. These have previously been identified as risk factors for FIV,2,8,13 and we would therefore expect a higher occurrence of disease in this population compared with cats selected at random. Even though most cats were not retested for confirmation, previous research has demonstrated a good correlation between the presence of FIV antibodies on ELISA and the presence of proviral DNA on blood PCR, which is indicative of active infection.33 Second, false-positive reactions can occur on the FIV antibody tests used in practice owing to previous FIV vaccination or the presence of maternal antibodies.34–36 Although it is unlikely that veterinarians would have tested a known vaccinated cat, many patients present with an incomplete medical history and it is therefore possible that some of the tested cats were previously vaccinated. Third, in the free-text comments of our survey, several veterinarians indicated that they had stopped testing for FIV and FeLV in-house because clinical cases were rare in their practice regions. The study sample may therefore have been biased towards practices with higher clinical disease occurrence.
The occurrence of FeLV test positivity in cats from the first-opinion veterinary practice was marginally greater than expected at 7.2% vs the 2.6% observed in the general population across New Zealand. With FeLV antigen ELISA testing, there is no known interference from previous vaccination or maternal antibodies that could lead to false-positive reactions. However, the sensitivity and specificity have been reported at 92.3% (95% CI 79.7–97.3) and 97.3% (95% CI 95.5–98.4%), respectively.23 Given the relatively low occurrence of FeLV and the fact that <5% of positive cats were retested for confirmation, we cannot rule out the possibility that some of these cats were false-positive reactors on the in-house ELISA. Several respondents to the national clinic survey also anecdotally reported isolated incidents of particularly severe clinical FeLV, which suggests there could be regional differences in FeLV occurrence and epidemiology. A future prospective study with unbiased sampling methods is needed to explore this further.
In guidelines published by the American Association of Feline Practitioners (AAFP), it was recommended that all cats be routinely screened for FeLV and FIV when they are first acquired, when they have compatible clinical signs and when they have high-risk lifestyles, which include known exposures to infected cats, evidence of bite wounds and access to the outdoors.19 Previous research has documented that the majority of client-owned cats in New Zealand are free-roaming,37 and at least 36% of cats from our first-opinion practice data had a known history of medical treatment for cat bite wounds, which would place them in the high-risk category. However, <2% of client-owned cats across New Zealand were tested for FeLV and FIV over a single calendar year. Similar low levels of compliance with testing guidelines have been reported in the USA, even when testing was offered at no cost to the client.24 In the free-text comments of the national clinic survey, one veterinarian indicated that routine testing was not performed because a positive diagnosis was unlikely to change the management or clinical outcome for the patient, particularly since many clients were reluctant to confine their cats. To our knowledge, there has been little research to date in the field of FeLV and FIV epidemiology exploring client perceptions and responses to positive diagnoses. This could have significant implications on our ability to control these viruses at the population level and therefore warrants further investigation.
Cats that tested positive for FeLV and/or FIV on the in-house ELISA frequently presented with lethargy, anorexia, weight loss and immunosuppression, which may have indicated that their retroviral diseases had progressed to an advanced clinical stage. Given that relatively few cats were retested for confirmation, we cannot rule out the possibility that these clinical signs were associated with other underlying disease processes. However, we speculate within the limitations of reviewing historical medical records that many of these cats would have been euthansed anyway, regardless of confirmation, owing to the poor clinical prognosis. This likely explains why the survival times for positive cats were significantly lower in our study compared with the survival times reported in other studies where cats were still clinically healthy at the time of diagnosis.20–22,38 Other factors that may contribute to lower survival times could include coinfection with both FIV and FeLV,39 or other opportunistic pathogens,40,41 as well as differences in the potential virulence of common circulating strains in New Zealand compared with other countries.42
The preliminary investigation into risk factors for FeLV and FIV found no evidence that previous bite wounds, known exposure to infected cats or being sexually intact increased the risk of test positivity, despite these being identified in other studies as important risk factors.9,10,12 While we cannot rule out biases due to missing information in historical medical records or biases due to data only being obtained from a single practice, it is also possible that transmission dynamics in New Zealand are different from other populations owing to the majority of cats being free-roaming. For example, FeLV is traditionally considered a pathogen that requires prolonged close friendly contact like mutual grooming or shared water for transmission given the poor survivability of the virus in the environment.43,44 Housemates that are indoor–outdoor may have fewer close contacts. Similar to other studies from the USA,8 Australia32 and Germany,2 we found that being male significantly increased the risk of FeLV and FIV test positivity. From a behavioural perspective, male cats have been shown to have more aggressive tendencies, leading to a greater risk of bite wounds.24,45 The majority of cats in our study were also already neutered, which may explain why this was not found to be a significant risk factor.
The AAFP guidelines also advocate the use of vaccines in cats with high-risk lifestyles.19 This has become more complicated in New Zealand now that the FeLV vaccine is no longer commercially available. Although vaccination rates were still low prior to March 2016 when the vaccine was removed,30 our study found that FeLV vaccines were primarily administered to high-risk cats. It will be important to monitor how the epidemiology of the disease changes now that these cats can no longer be protected. Several practices declined to participate in the national survey because they were unable to easily query their practice data to obtain summary data on the number of feline patients and results from the diagnostic testing. New initiatives are currently underway in New Zealand to improve data capture from electronic medical records that will hopefully make these type of monitoring studies easier in the future.46,47
Conclusions
Our study findings suggest that the epidemiology of FeLV and FIV in New Zealand is different than other countries, which may be owing to the large percentage of client-owned cats that are free-roaming. Prevalence should continue to be monitored now that FeLV vaccination is no longer possible.
Acknowledgments
We thank the veterinary practices in New Zealand for generously contributing their testing data and the Veterinary Centre, Waimate for providing detailed access to their clinical records. We are grateful to Nick Cave for reviewing the clinic survey form.
Footnotes
Conflict of interest: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Partial funding for publication was provided by the Institute for Veterinary, Animal and Biomedical Sciences, Massey University.
Accepted: 28 July 2017
References
- 1. Levy J. Feline leukemia virus and feline immunodeficiency virus. In: Miller L, Hurley K, Hoboken F. (eds). Infectious disease management in animal shelters. Hoboken, NJ: Wiley-Blackwell, 2009, pp 307–317. [Google Scholar]
- 2. Gleich SE, Krieger S, Hartmann K. Prevalence of feline immunodeficiency virus and feline leukaemia virus among client-owned cats and risk factors for infection in Germany. J Feline Med Surg 2009; 11: 985–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yamamoto JK, Hansen H, Ho EW, et al. Epidemiologic and clinical aspects of feline immunodeficiency virus infection in cats from the continental United States and Canada and possible mode of transmission. J Am Vet Med Assoc 1989; 194: 213–220. [PubMed] [Google Scholar]
- 4. Ueland K, Lutz H. Prevalence of feline leukemia virus and antibodies to feline immunodeficiency virus in cats in Norway. Zoonoses Public Health 1992; 39: 53–58. [DOI] [PubMed] [Google Scholar]
- 5. Malik R, Kendall K, Cridland J, et al. Prevalences of feline leukaemia virus and feline immunodeficiency virus infections in cats in Sydney. Aust Vet J 1997; 75: 323–327. [DOI] [PubMed] [Google Scholar]
- 6. Hosie MJ, Robertson C, Jarrett O. Prevalence of feline leukaemia virus and antibodies to feline immunodeficiency virus in cats in the United Kingdom. Vet Rec 1989; 125: 293–297. [DOI] [PubMed] [Google Scholar]
- 7. Little S, Sears W, Lachtara J, et al. Seroprevalence of feline leukemia virus and feline immunodeficiency virus infection among cats in Canada. Can Vet J 2009; 50: 644–648. [PMC free article] [PubMed] [Google Scholar]
- 8. Levy JK, Scott HM, Lachtara JL, et al. Seroprevalence of feline leukemia virus and feline immunodeficiency virus infection among cats in North America and risk factors for seropositivity. J Am Vet Med Assoc 2006; 228: 371–376. [DOI] [PubMed] [Google Scholar]
- 9. Shelton GH, Waltier RM, Connor SC, et al. Prevalence of feline immunodeficiency virus and feline leukemia-virus infections in pet cats. J Am Anim Hosp Assoc 1989; 25: 7–12. [Google Scholar]
- 10. Yamamoto JK, Sparger E, Ho EW, et al. Pathogenesis of experimentally induced feline immunodeficiency virus infection in cats. Am J Vet Res 1988; 49: 1246–1258. [PubMed] [Google Scholar]
- 11. Hardy W, Old L, Hess P, et al. Horizontal transmission of feline leukaemia virus. Nature 1973; 244: 266–269. [DOI] [PubMed] [Google Scholar]
- 12. Caney S. Feline leukaemia virus: an update. In Pract 2000; 22: 397–404. [Google Scholar]
- 13. Westman ME, Paul A, Malik R, et al. Seroprevalence of feline immunodeficiency virus and feline leukaemia virus in Australia: risk factors for infection and geographical influences (2011–2013). J Feline Med Surg Open Rep 2016; 2. DOI: 2055116916646388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hellard E, Fouchet D, Santin-Janin H, et al. When cats’ ways of life interact with their viruses: a study in 15 natural populations of owned and unowned cats (Felis silvestris catus). Prev Vet Med 2011; 101: 250–264. [DOI] [PubMed] [Google Scholar]
- 15. Sparkes AH. Feline leukaemia virus and vaccination. J Feline Med Surg 2003; 5: 97–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hoover EA, Olsen RG, Hardy WD, et al. Feline leukemia virus infection: age-related variation in response of cats to experimental infection. J Natl Cancer Inst 1976; 57: 365–369. [DOI] [PubMed] [Google Scholar]
- 17. Hoover EA, Olsen RG, Hardy WD, et al. Biologic and immunologic response of cats to experimental infection with feline leukemia virus1.” Comp Leuk Res 1975; 43: 180–183. [DOI] [PubMed] [Google Scholar]
- 18. Dunham SP, Graham E. Retroviral infections of small animals. Vet Clin North Am Small Anim Pract 2008; 38: 879–901. [DOI] [PubMed] [Google Scholar]
- 19. Levy J, Crawford C, Hartmann K, et al. 2008. American Association of Feline Practitioners’ feline retrovirus management guidelines. J Feline Med Surg 2008; 10: 300–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hartmann K. Clinical aspects of feline retroviruses: a review. Viruses 2012; 4: 2684–2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ravi M, Wobeser GA, Taylor SM, et al. Naturally acquired feline immunodeficiency virus (FIV) infection in cats from western Canada: prevalence, disease associations, and survival analysis. Can Vet J 2010; 51: 271. [PMC free article] [PubMed] [Google Scholar]
- 22. Hartmann K. Clinical aspects of feline immunodeficiency and feline leukemia virus infection. Vet Immunol Immunopathol 2011; 143: 190–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hartmann K, Griessmayr P, Schulz B, et al. Quality of different in-clinic test systems for feline immunodeficiency virus and feline leukaemia virus infection. J Feline Med Surg 2007; 9: 439–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Goldkamp CE, Levy JK, Edinboro CH, et al. Seroprevalences of feline leukemia virus and feline immunodeficiency virus in cats with abscesses or bite wounds and rate of veterinarian compliance with current guidelines for retrovirus testing. J Am Vet Med Assoc 2008; 232: 1152–1158. [DOI] [PubMed] [Google Scholar]
- 25. Jones BR, Lee EA. Feline leukaemia virus testing. N Z Vet J 1981; 29: 188–189. [DOI] [PubMed] [Google Scholar]
- 26. Jones BR, Lee EA, Pauli JV. Feline leukaemia virus testing. N Z Vet J 1983; 31: 145–146. [DOI] [PubMed] [Google Scholar]
- 27. Jenkins KS, Dittmer KE, Marshall JC, et al. Prevalence and risk factor analysis of feline haemoplasma infection in New Zealand domestic cats using a real-time PCR assay. J Feline Med Surg 2013; 15: 1063–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kann R, Seddon J, Meers J, et al. Feline immunodeficiency virus subtypes in domestic cats in New Zealand. N Z Vet J 2007; 55: 358–360. [DOI] [PubMed] [Google Scholar]
- 29. Hayward JJ, Taylor J, Rodrigo AG. Phylogenetic analysis of feline immunodeficiency virus in feral and companion domestic cats of New Zealand. J Virol 2007; 81: 2999–3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cave NJ, Jackson R, Bridges JP. Policies for the vaccination of cats and dogs in New Zealand veterinary practices. N Z Vet J 2016; 64: 145–153. [DOI] [PubMed] [Google Scholar]
- 31. R Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2016. [Google Scholar]
- 32. Norris JM, Bell ET, Hales L, et al. Prevalence of feline immunodeficiency virus infection in domesticated and feral cats in eastern Australia. J Feline Med Surg 2007; 9: 300–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Arjona A, Barquero N, Doménech A, et al. Evaluation of a novel nested PCR for the routine diagnosis of feline leukemia virus (FeLV) and feline immunodeficiency virus (FIV). J Feline Med Surg 2007; 9: 14–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Uhl E, Heaton-Jones T, Pu R, et al. FIV vaccine development and its importance to veterinary and human medicine: a review: FIV vaccine 2002 update and review. Vet Immunol Immunopathol 2002; 90: 113–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Westman ME, Malik R, Hall E, et al. Determining the feline immunodeficiency virus (FIV) status of FIV-vaccinated cats using point-of-care antibody kits. Comp Immunol Microbiol Infect Dis 2015; 42: 43–52. [DOI] [PubMed] [Google Scholar]
- 36. Barr MC. FIV, FeLV, and FIPV: interpretation and misinterpretation of serological test results. Semin Vet Med Surg (Small Anim) 1996; 11: 144–153. [DOI] [PubMed] [Google Scholar]
- 37. Allan FJ, Pfeiffer DU, Jones BR, et al. A cross-sectional study of risk factors for obesity in cats in New Zealand. Prev Vet Med 2000; 46: 183–196. [DOI] [PubMed] [Google Scholar]
- 38. Liem BP, Dhand NK, Pepper AE, et al. Clinical findings and survival in cats naturally infected with feline immunodeficiency virus. J Vet Intern Med 2013; 27: 798–805. [DOI] [PubMed] [Google Scholar]
- 39. Pedersen NC, Torten M, Rideout B, et al. Feline leukemia virus infection as a potentiating cofactor for the primary and secondary stages of experimentally induced feline immunodeficiency virus infection. J Virol 1990; 64: 598–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Pedersen N, Yamamoto JK, Ishida T, et al. Feline immunodeficiency virus infection. Vet Immunol Immunopathol 1989; 21: 111–129. [DOI] [PubMed] [Google Scholar]
- 41. Tenorio AP, Franti CE, Madewell BR, et al. Chronic oral infections of cats and their relationship to persistent oral carriage of feline calici-, immunodeficiency, or leukemia viruses. Vet Immunol Immunopathol 1991; 29: 1–14. [DOI] [PubMed] [Google Scholar]
- 42. Pedersen NC, Leutenegger CM, Woo J, et al. Virulence differences between two field isolates of feline immunodeficiency virus (FIV-APetaluma and FIV-CPGammar) in young adult specific pathogen free cats. Vet Immunol Immunopathol 2001; 79: 53–67. [DOI] [PubMed] [Google Scholar]
- 43. Francis D, Essex M, Hardy W. Excretion of feline leukaemia virus by naturally infected pet cats. Nature 1977; 269: 252–254. [DOI] [PubMed] [Google Scholar]
- 44. Addie D, Dennis J, Toth S, et al. Long-term impact on a closed household of pet cats of natural infection with feline coronavirus, feline leukaemia virus and feline immunodeficiency virus. Vet Rec 2000; 146: 419–424. [DOI] [PubMed] [Google Scholar]
- 45. Hart B, Cooper L. Factors relating to urine spraying and fighting in prepubertally gonadectomized cats. J Am Vet Med Assoc 1984; 184: 1255–1258. [PubMed] [Google Scholar]
- 46. Muellner P, Muellner U, Gates MC, et al. Evidence in practice – a pilot study leveraging companion animal and equine health data from primary care veterinary clinics in New Zealand. Front Vet Sci 2016; 3: 116 DOI: 10.3389/fvets.2016.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. O’Neill D. VetCompass clinical data points the way forward. Vet Ireland J 2012; 2: 353–356. [Google Scholar]


