Abstract
Telephone-Linked Care (TLC) technology has been developed and applied as an alternative to and a supplement for office visits as a means to deliver ambulatory care. TLC is used to monitor patients with chronic diseases, counsel patients on important health behaviors, and provide information and support to home caregivers of patients with disabling condtions. TLC speaks to patients over the telephone in their homes using computer-controlled digitized human speech. Patients use their telephone keypad to communicate. TLC conversations last 2-15 minutes per call and take place weekly for periods of at least 3 months. The conversations consist of a salutation, password verification, the core clinical part, and a closing. The structure of the clinical part is similar for each of the application groups: chronic disease, health behavior, and caregiver support. The system architecture consists of linked voice and database components and their subcomponents. Preliminary evaluation indicates that TLC is well accepted by patients and their providers and can improve clinical outcomes.
A visit to a physician's office is the principal source of health care for the majority of Americans, with more than 650 million physician office visits occurring in 1991.1 Despite the importance of the office visit, its content and structure have changed little over time. With the advent of managed care systems, however, there is now new pressure to improve the efficiency and outcomes of these visits. Thus, in many settings time scheduled for an office visit has been drastically reduced, enabling more patients to be seen in the course of the day and driving down unit costs. Although greater efficiency has been achieved, health care providers feel the stress of delivering high quality care in less time. In response, they are seeking new ways to care for patients that maximize both quality of patient care and practice efficiency.
The telephone has been used in health care for a century,2 and more advanced telecommunications technology has been in use for more than three decades.3 Despite this history and recent rapid developments in the telecommunications field,4 the use of telecommunications technology to deliver health care remains underdeveloped, although it offers great potential to improve ambulatory care practice. For some time, practitioners have used the telephone as an outreach mechanism to contact patients and for patients to contact them.5 In recent years automated telephone systems have been introduced to remind patients about their appointments,6,7 promote attendance in drug treatment programs,8 administer health questionaires,9 educate patients,10 and assess substance abuse.11 As the demands on ambulatory care practice increase, however, further innovative uses of telecommunications technology are needed to enhance both the quality and efficiency of ambulatory care practice.
Over the past decade, our unit has utilized telecommunications technology to develop a Telephone-Linked Care (TLC) system that carries out totally automated telephone encounters with patients. These virtual visits over the telephone have been designed for a variety of clinical situations, including the care of patients with chronic disease and individuals requiring health behavior change. The purpose of this paper is to discuss our work and highlight the ways in which telecommunications technology can be used to help clinicians establish new means of communicating with patients that enhance the provision of health care services.
Overview of the Telephone-Linked Care (TLC) System
Brief Description of TLC
TLC is a computer-based telecommunications system that converses with patients and other individuals in their homes over the telephone (Fig. 1).12 The system carries out automated, telephone-based health care encounters with patients that supplement and complement office visits between patients and their health care providers. Patients can begin using TLC on referral from their providers or on their own initiative. During TLC telephone encounters, the system speaks to patients using computer-controlled digitized human speech. The patients, in turn, communicate with TLC by depressing the keys on their telephone keypad or by speaking into the telephone receiver. During each conversation, TLC asks the patients clinical questions and comments on their responses; it also can provide information and counseling. Depending on the clinical domain of the particular TLC application and the patients' responses, a conversation can last between 2 and 15 minutes. Likewise, the number of TLC conversations per patient and their frequency can also vary. Typically, patients converse with TLC on a weekly schedule and continue for periods of at least 3 months. Some TLC applications allow the patients to call whenever they want. For most TLC systems, responsible health care providers receive routine reports at periodic intervals that summarize the patients' status. TLC also sends special alert reports to providers when the patients' clinical condition warrants immediate notification. In some applications, the patients receive regular reports that complement the content of the TLC conversations. Figure 1 illustrates the interconnections between TLC, the patient, and the physician or other provider.
Figure 1.
Overview of TLC functions. The patient initiates the process by telephoning TLC (A). TLC carries out a conversation with the patient and stores information provided by the patient in a database (B). TLC issues patient reports to the patient's physician or other provider (C) and to the patient (D). The physician reads the report, and it is placed in the patient's medical record (E), whether this is paper or electronic.
Types of TLC Applications
The clinical applications of TLC and their current status are shown on Table 1. These applications fall into three groups. One group assists clinicians who care for ambulatory patients with chronic illnesses (including high-risk pregnancy, which is a temporary “chronic” condition). These applications monitor the status of the patient's health condition and transmit important clinical information from the patient to the clinician. For example, in TLC-Hypertension,12 patients monitor their blood pressure weekly and report the values to TLC. TLC, in turn, provides the patients' clinicians with the blood pressure information, displayed in a graphical format. Depending upon the urgency of the information, the clinicians will receive it on alert reports sent immediately (electronically or by fax) or on standard monthly reports. The objective of TLC monitoring of patients with chronic illnesses is two-fold. First, by providing very complete and timely patient information to clinicians, we expect that they would adjust therapy better and consequently better control the patients' diseases. Second, for those chronic health conditions for which patients can and frequently do experience exacerbations, we expect that TLC would be able to detect deterioration early, and by notifying clinicians, facilitate interventions to abort the exacerbations. Chronic diseases in which exacerbations are common include asthma, chronic obstructive lung disease, congestive heart failure, angina pectoris, and high-risk pregnancy.
Table 1.
Clinical Applications of TLC
| Applications | Current Status |
|---|---|
| Chronic disease management | |
| Hypertension | Evaluated |
| Angina pectoris | Being evaluated |
| Congestive heart failure (CHF) | Designed |
| Chronic obstructive pulmonary disease (COPD) | Programmed |
| Being designed | |
| Childhood asthma | Programmed |
| Diabetes mellitus | Programmed |
| Chronic disability - Functional | Programmed |
| Impairment | |
| Hih-risk pregnancy | |
| Health behavior management | |
| Medication-taking | Evaluated |
| Physical activity | Pilot test evaluation completed & full evaluation in progress |
| Diet—general | Pilot test evaluation completed |
| Diet—low fat | Being evaluated |
| Diet—weight management | Designed |
| Cigarette smoking | Programmed |
| Mammography screening | Designed |
| Care-giver support | |
| Alzheimer's disease | Being evaluated |
A second group of TLC applications (Table 1) addresses changing or sustaining important health care behaviors.13,14 Many of these are lifestyle behaviors.
Thus, these TLC applications could be used by individuals who have a disease, such as diabetes mellitus, or by other individuals who are apparently free of disease but who are at risk for developing a health problem in the future because of an unhealthy lifestyle. The design of these applications utilizes both behavioral theory (i.e., the nature of the behavior and how it is sustained or changed) and the behavior change heuristics of expert clinicians.
A third group of applications (currently with one example) provides support, both informational and emotional, to individuals who care for a person at home with a serious health condition.15 The need for this type of application is likely to increase in the future as the American population ages and the burden of chronic disease and disability grows. For personal and financial reasons, families often wish to keep a disabled member out of a nursing home but need help in taking care of that person at home. The availability of service organizations to help these caregivers is limited in the United States. The TLC caregiver applications help the caregiver deal with specific issues that come up in the care at home of individuals with specific health conditions. For example, in the Alzheimer's disease application, TLC provides information on how to manage specific disruptive behaviors (e.g., having a tantrum) that frequently affect Alzheimer's disease patients.
The boundaries between the groups of TLC applications are not absolute. For example, many of the chronic disease applications contain behavioral sub-modules within them. In practice, a particular patient or group of patients can use one or more TLC applications during the same time period, and specific TLC applications can be “called” while a patient is using another application. For example, a person using TLC-Diabetes could choose to start using a physical activity promoting application as an option during a TLC-Diabetes conversation.
System Description
Structure of TLC Conversations
Table 2 shows the structure of a TLC conversation with a patient. The conversation begins with a salutation that announces to the patient that TLC is calling or has been reached. For example, a TLC application for promoting regular physical activity being tested at Harvard Pilgrim Health Care (HPHC) begins as follows: “Hello! You've reached Harvard Health Care's Telephone Linked Care or TLC.” The conversation goes on to request that the patient enter his or her password, which is a personal identifier number. Once this is confirmed, the clinical core of the TLC conversation can begin (Table 3). At the very end of the conversation, TLC makes a closing remark and then hangs up. In the HPHC physical activity application, for example, the system says: “Good-bye, [patient's name]. Before we end, if you have any difficulty or concerns about working with TLC, please call 1-800-XXXX and leave a message explaining what the problem is, and your name and phone number. A member of the TLC team will get back to you shortly.”
Table 2.
Structure of a TLC Conversation
| Salutation |
| Password (PIN) Verification |
| Conversation clinical core |
| Closing |
Table 3.
Conversation Clinical Core
| Chronic Disease Applications | Health Behavior Applications | Caregiver Support Applications |
|---|---|---|
| Assess disease | Assess health behavior | Assess caregiver needs & stress |
| Device results | Performance | Giving information & practical advice |
| Symptoms | Behavioral | Giving emotional support |
| Physical findings | Goal attainment | |
| Functioning | Intervention | |
| Assess use of prescribed treatments | Goal setting | |
| Knowledge | ||
| Adherence | ||
| Counsel adherence (if required) |
Content of the Clinical Core of a TLC Conversation
Chronic Disease Applications
The content of the clinical core of the conversation differs among the TLC applications. For each group of applications (see Table 1), however, there is a common general structure. The structure of the clinical core for the chronic disease applications, shown in Table 3, begins with an assessment of the disease. In this part, TLC asks the patient to provide information about the status of his or her disease. If patients are using an instrument to self-monitor themselves, TLC asks them to report the instrument's results. A common instrument used in self-monitoring is a bathroom scale. Patients using TLC in weight management, control of hypercholesterolemia, and congestive heart failure are asked to weigh themselves regularly, in a standardized way, and to report their weights to TLC. Some patients self-monitor using more specialized devices, such as a sphygmomanometer, blood glucose monitor, or peak flow meter. Before they begin using TLC, they are given a calibrated device and are taught a standardized protocol to use the device properly. Thereafter, they use the device regularly and report results to TLC. For example, in TLC-Diabetes, the system asks the patient to enter selected home blood glucose test values (the highest and the lowest during the previous week, and the number above and below certain thresholds). In TLC-Asthma, an application designed for children with asthma, TLC tells the user: “Now pick up your peak flow meter and check your peak flow three times. When you are done, enter the biggest number. I'll wait until you are ready.” As more patient self-monitoring devices and tests become available for home use, we expect to incorporate them into TLC chronic disease applications.
Asking patients with a chronic disease questions about key symptoms is a common way clinicians assess disease status. Similarly, much of the content of TLC chronic disease applications is devoted to collecting information on symptoms. In TLC-Angina, for example, the system queries the patient about the number of episodes of angina experienced during the previous week, the duration of the longest episode, the severity of the most severe episode, which activities and at what level of exertion brought on the angina, and whether the angina pain experienced was typical for the patient or different. If the angina is different, TLC inquires whether the patient experienced associated symptoms, such as shortness of breath.
For those diseases in which patients can observe important physical findings, TLC will ask patients to report these findings in its assessment of the disease. For example, in TLC-CHF, a TLC application for congestive heart failure, the system asks about ankle swelling (pedal edema), a common physical finding in this disease.
In most TLC chronic disease applications, there are questions that address the level of patient functioning. In both TLC-Angina and TLC-Chronic Lung Disease, for example, we have incorporated the Chronic Respiratory Disease Questionnaire (CRQ)16 into the questioning of the patients by TLC. At the time patients begin to use these two TLC systems, they identify the five most important activities they engage in that are most affected by their disease. During subsequent TLC conversations, the system asks them to identify which of the selected activities they engaged in during the previous week. If they did not do the activity, they are asked whether fear of symptoms stopped them from trying. If they did the activity, TLC asks them to rate the severity of symptoms experienced. From this information, the system calculates a CRQ score and reports it to the responsible clinicians.
In addition to monitoring the status of the disease, TLC chronic disease applications assess the patient's use of prescribed treatments (Table 3). The most important of these are medications. All TLC chronic disease applications contain a medication module with two parts. The first part assesses whether the patient understands which medications he or she should be taking and how to take them. It establishes agreement or disagreement between the patient's understanding of what the physician prescribed and the physician's actual prescription. The second part assesses the patient's adherence to the regimen. Some TLC chronic disease applications contain a third part that counsels nonadherent patients to take all of their prescribed medications.
The medication knowledge part begins with a question about whether the physician changed the medication regimen since the last TLC conversation. If so, TLC checks to see if its medication files for the patient have been updated since the last TLC call. If not, it skips the medication module, and a TLC Data Manager checks with the patient's physician to update the regimen. If there has been no change to the regimen, TLC verifies the patient's understanding of the regimen for each prescribed medication. The system first checks on the medication's name, then the unit dose amount, frequency of administration, and finally conditions of administration (route, time of day, with or without food, etc.). A TLC Data Manager would report all discrepancies to the patient's physician.
Next, TLC addresses the issue of medication adherence. It begins with the question shown by Haynes to elicit the most truthful responses: “Frequently, people don't take all of their medications. Did you miss taking any of your [medication name] during the past week?”17 If the patient answers in the affirmative, TLC determines the amount (usually number of pills) missed. From this, it calculates an adherence rate (amount taken/amount prescribed). At times, some patients take extra medicine in addition to their prescribed doses, so TLC inquires about these extra doses in a separate question.
In some TLC chronic disease applications, TLC offers to counsel patients who are not taking all of their prescribed medication. For example, in TLC-Hypertension,12 the medication adherence counseling part compares the patient's adherence to antihypertensive medications reported during the call with that reported previously (mean adherence over the previous 4 weeks). The system further links the adherence level and the change in adherence with the level of the patient's blood pressure. For example, the system might remark: “Today I see that you are taking all of your blood pressure medications, which is an improvement for you. Previously, you were taking your medications only 78% of the time. I also see that your blood pressure is much better controlled today. It is 134 over 86, an improvement over the recent past when the average was 162 over 94. Keep it up!” In TLC-Angina, we have gone one step farther to inquire from the patient why he or she has missed some medication doses. The system inquires whether the patient forgot to refill a prescription, forgot some doses, or thought the medication was causing side effects. Depending upon the patient's answer, TLC gives the patient particular advice for dealing with the reason(s) for medication non-adherence.
Health Behavior Applications
The organizational structure of the clinical core for the health behavior applications, shown in Table 3, shares some elements with the chronic disease applications; however, for the most part, it is quite different. Like the chronic disease applications, the health behavior applications entail multiple conversations over time, since behavior change takes time. Thus, the clinical core begins with an assessment of the health behavior, just as the chronic disease applications begin with an assessment of the disease. This assessment has both a performance component and a behavioral component (Table 3). For example, in TLC-ACT,14 an intervention for promoting regular physical activity, performance of the behavior is assessed by questioning whether the person engaged in any moderate or more strenuous physical activity during the previous week and, if so, on how many days and for how many minutes on average per day. Performance is also measured by a reading taken from a pedometer that the person wears on the day prior to each TLC call.
The behavioral component of the assessment deals with the person's intention to engage in the behavior at a goal level. For physical activity, the ultimate goal is for TLC users to do moderate-intensity physical activity (like a brisk walk) on at least 5 days per week for at least 30 minutes each day.18,19 Depending on the person's intention to be this active, he or she is channeled into a particular part of TLC-ACT. For example, for a person who is not active, an appropriate behavorial process would be for the person to learn about the positive health effects of regular exercise and the detrimental effects of a sedentary lifestyle.
For most of the health behavior applications, there is a third component of the assessment, a goal attainment component (Table 3). This entails a comparison of the person's current performance (using one or more measures of performance) and the goal the person set for himself during the previous conversation. This strategy of setting intermediate, small, easily achievable goals and then comparing later performance to the goals is derived from Social Learning Theory.20 Achievement of intermediate goals has been shown to promote the sense of self-efficacy, which in turn facilitates long-term behavior change. Individuals who use TLC-ACT, for example, establish their personal goal for physical activity for each upcoming week at the end of each TLC-ACT call. During each subsequent TLC call, the system compares the users' performance with the personal goals they set during that previous call.
Following assessment, the patient who uses a TLC health behavior application enters the intervention part of the core of the conversation (Table 3). Here, the patient receives information and counseling to affect behavior change. For each application, this section is modeled on the basis of specific health behavior theories, the results of health behavior research studies, and the judgment of expert clinicians. For example, in TLC-Mammography the intervention part is organized around 34 factors that women commonly identify as barriers to getting a mammogram, such as concerns about a painful procedure, cost, and/or concerns about losing a breast.21 These factors have been identified in studies of women who do not get mammograms. In TLC-Mammography we have organized these factors into seven groups. During TLC-Mammography conversations, the system first inquires whether a woman has issues in any of the seven groups. If so, the system probes further into the specific factors within the selected groups.
The last part of the clinical core for the TLC health behavior applications deals with goal setting. As discussed above, at the end of each TLC-ACT conversation, the user sets a personal goal for physical activity for the upcoming week. This goal may be less than, the same as, or more than the systems' ultimate goal for the person of 30 minutes of moderate-intensity exercise on at least 5 days a week.
Caregiver Support Applications
For the third set of applications, the caregiver support applications, the structure of the clinical core of the conversation is also shwon in Table 3. The conversation begins by assessing caregiver needs and stress, continues with giving information and advice, and in some cases, offering emotional support. Our examples are drawn from the first caregiver support application, TLC-Alzheimer's Disease (TLC-AD),15 an application for supporting the caregiver role of individuals, typically family members, who take care of Alzheimer's disease patients living at home.
Like the chronic disease and health behavior applications, the caregiver support applications begin with an assessment component. In TLC-AD, this is an assessment of the caregiver's needs in the care of the Alzheimer's patient, called the care recipient, and the resulting stress on the caregiver. At the beginning of each conversation with a caregiver, TLC-AD assesses which of 18 commonly manifested disruptive behaviors (e.g., tantrums) the care recipient is displaying. For each behavior identified, TLC asks the caregiver to describe the frequency and intensity of the behavior, the degree to which the disruptive behavior causes the caregiver stress, and the level of that stress.
Next, the caregiver can receive information and practical advice on how to deal with a specific disruptive behavior. TLC uses vignettes to communicate some of the information and advice. These vignettes describe how a hypothetical caregiver deals with a care recipient who exhibits the particular disruptive behavior in question. For example, if a caregiver reports that his or her Alzheimer's relative is wandering away from home, TLC-Ad explains to the caregiver how to make a footprint of the care recipient and how to store cotton balls with the person's scent to aid in a potential search. The system goes on to recommend that the care recipient wear an identification bracelet, and it relates a vignette about an Alzheimer's patient named John who “... refused to wear a bracelet, since he thought it was girlish, so everyone in the household got one and then he wanted to wear his!” If desired, the caregiver can choose other informational topics that explain how to identify triggers in the environment that provoke disruptive behaviors and receive advice on how to prevent such occurrences. They can also access a resource module, which provides information on how to contact regional and national Alzheimer's disease community services.
In subsequent conversations, TLC-AD assesses the usefulness of the information and advice it provided earlier. If the advice was not helpful, caregivers are asked if they would like additional information and advice on how to manage specific disruptive behaviors, in which case TLC-AD offers another tier of information and advice. If the advice was not useful, TLC-AD suggests that the caregivers post their specific problems on the TLC-AD community voice-mail bulletin board, which is linked electronically to the telecommunications system. This is the emotional support component. Here, users can get support from other Alzheimer's caregivers who can leave personal voice-mail messages that give emotional support and practical advice. The goal is to mimic a caregiver support group via the telephone to reduce the isolation felt by caregivers, especially those who cannot leave their homes to participate in traditional support groups.
TLC-AD also reassess the caregiver's level of stress related to managing disruptive behaviors; if the stress level consistently rises, an Alert Report is faxed to the provider who referred the caregiver. This report identifies the type(s) of disruptive behaviors occurring in the caregiving situation and the changes in the caregiver's stress level.
TLC Conversation Superstructure
For each TLC application, there is a superstructure operating above the structure of the individual TLC conversations, described above. This superstructure controls which parts of the basic conversation are used in a given conversation, and it employs two strategies: (1) parceling out the conversation content across multiple conversations, and (2) using contingencies to determine whether specific conversation content should be covered. These strategies serve to limit the duration of each conversation with a patient, and make the content of each conversation more relevant to a patient's clinical situation at a particular time.
An example of the first strategy of distributing content over multiple conversations is found in TLC-Low Fat, an application that educates and counsels individuals on how to reduce fat, especially saturated fat, in their diets. The conversation architecture in TLC-Low Fat is a cycle of six TLC conversations. Each conversation covers food consumption questions in one or two food groups, food selection at one type of restaurant (e.g., Italian), and selective questions on food purchasing, preparation, garnishing, and serving. Altogether, the six conversations cover all of TLC-Low Fat's content, with the material in each conversation covering part of the total.
TLC-Angina uses the second strategy of controlling the level of detail in the questioning by TLC, contingent on patient status at the time of the call. In this application, patients receive a full assessment of their angina once every 4 weeks. During the interim, TLC only asks four to six basic questions about the angina, with the principal question being whether the angina has worsened in terms of frequency, severity, or duration of episodes. A patient who indicates that it is worse will have a full angina assessment. A similar strategy is employed for the medication assessment and medication counseling parts. TLC-ACT also uses contingencies to control the conversation content. One such contingency is to relinquish control of the content and duration of the conversation to the patient.
Feedback and Reports to Patients and Providers
Much of the information, advice, support, and counseling by TLC is done in response to the answers patients give to TLC questions (Fig. 2). This TLC feedback also serves to maintain the human side of the conversation, supporting the “feel” of the conversation as a true dialogue. For example, in TLC-ACT, a patient who is not exercising is asked why and is presented with some common reasons why people do not exercise. If the person does not select any of the options presented, TLC responds by saying: “You haven't selected any reason. Perhaps none of these is relevant to you.” This response both acknowledges and legitimizes the patient's answer to a TLC-ACT question. At another point in the conversation, TLC addresses the benefits of exercise and asks the patient whether it has an effect on cholesterol levels. If the patient answers yes, TLC responds with, “That's right! HDL, or good cholesterol, goes up with physical activity. Higher levels of the good cholesterol carry away the bad cholesterol from your body, and this means your chance of getting a heart attack is much lower.” This response, in addition to acknowledging the person's answer to a TLC question, provides information. Later on in the TLC-ACT conversation, the system suggests that the patient look out for information on exercise in the media. The rationale for this advice (and the information provided on cholesterol, as well) is drawn from behavioral theory and is termed “consciousness raising.” Next, TLC-ACT asks the patient if he or she plans to adopt the suggestion. If the patient agrees, TLC says, “That's good! There's always some new information on exercise in the media. If it would be helpful, you could even write down what you have learned.” This feedback acknowledges the patient's answer, reinforces the advice given, and provides an additional suggestion that might increase the level of consciousness raising. Thus, TLC feedback to patients maintains the dialogue, acknowledges and legitimizes patients' responses, provides information, and motivates behavior change.
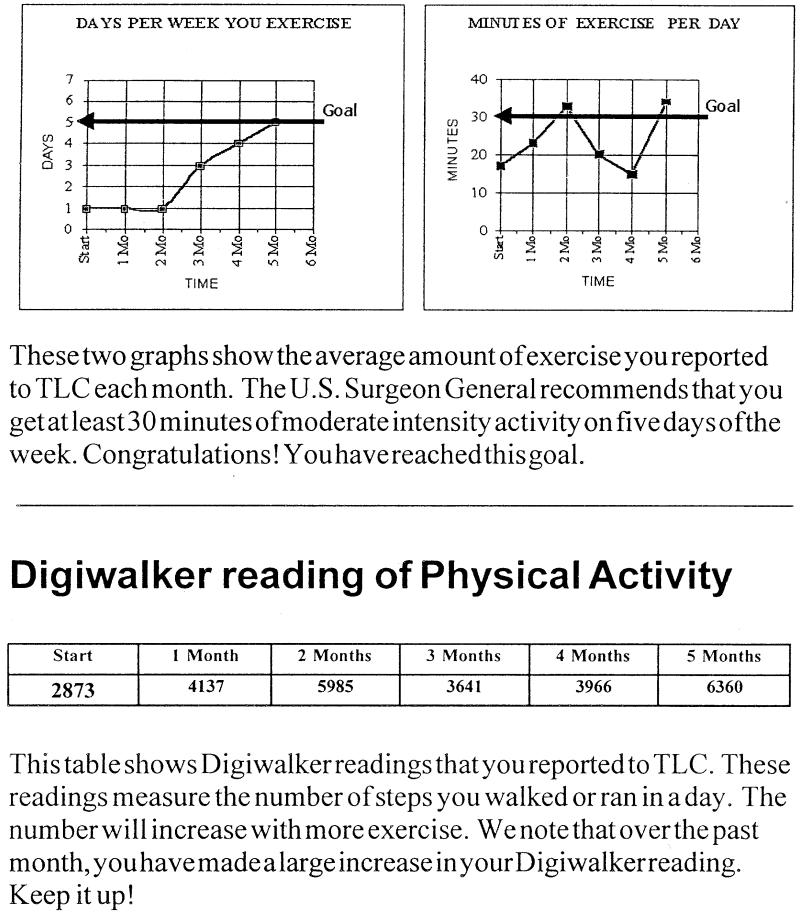
Figure 2.
Sample patient report for TLC-ACT. This is an example of a patient report for TLC-ACT, an application for promoting physical activity. The upper two graphs display the patient's average level of physical activity per month. The graph on the left plots the average number of days per week that the patient was active. The graph on the right depicts the average number of minutes of activity per active day. The graph at the bottom of the page displays the average pedometer readings reported by the patient.
Feedback to patients and their providers can also be in the form of written reports (both in printed and electronic formats). The purpose of the reports is to provide important information to the recipient and to affect the recipient's behavior.
For patients, the reports are a tangible record of their use of TLC. For example, in TLC-ACT, patients receive monthly reports that graphically display their pedometer readings reported to TLC over time, as well as changes over time in the number of days per week they exercise and the number of minutes they exercise per day (Fig. 2). Written text below each graph interprets the graph for the patient.
The goal of the Patient Report is to demonstrate how the patients are doing and to motivate them to be more active. In most TLC applications, physicians and other health providers also receive reports on individual patients.
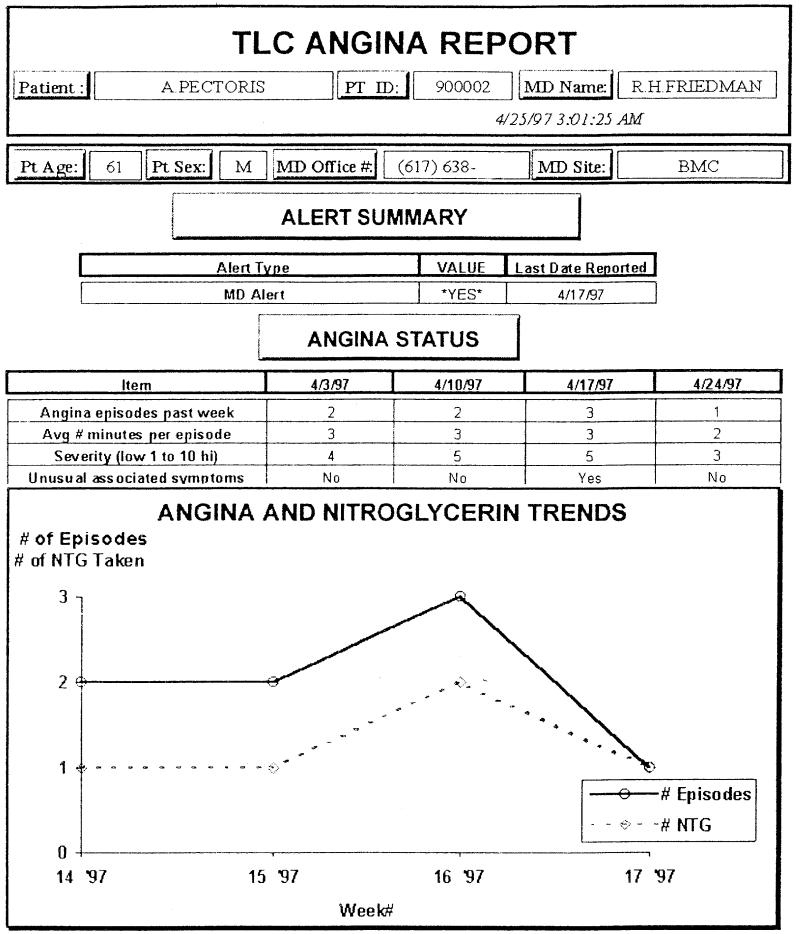
Figure 3 depicts a sample Physician Report that was generated by TLC-Angina. The report indicates the level of urgency and displays important information about the patient's condition. Similar reports are produced in other TLC applications. Like laboratory test reports, TLC Physician Reports communicate the patients' clinical status and, in some instances, would trigger physician action, such as contacting a patient to change medications.
Figure 3.
Sample physician report from TLC-Angina. This is a contrived example of a report to a physician who is caring for a patient with angina pectoris. The Alert Summary indicates if and when the patient last had an urgent problem for which an alert report was sent to the physician. Angina Status summarizes basic information about the patient's angina from the most recent four TLC calls. Angina and Nitroglycerin Trends display the number of the angina episodes and nitroglycerin tablets reported per week since the patient started using TLC. The numbers on the X-axis are the week numbers (1-52) for the year 1997. Thus, 14′ 97 means the 14th 1997.
TLC Computer System Architecture and Processing
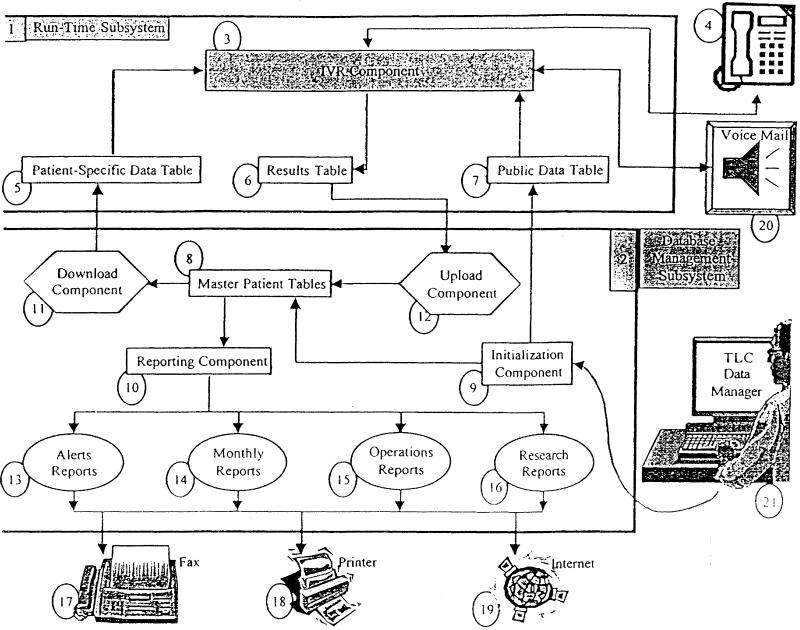
The TLC computer system consists of dual microprocessors; one microprocessor operates a Run-Time Subsystem, and a second microprocessor controls a Database Management Subsystem.26 The Run-Time Subsystem executes TLC conversations with patients, whereas the Database Management Subsystem stores and outputs TLC data. In designing TLC, we separated these two subsystems so that either part could be changed or replaced without affecting the other. This modular approach allows us to introduce and integrate with minimal effort new commercial or inhouse software and hardware products. In fact, during the past decade, we have changed both subsystems, independently of each other, and we expect to do so again in the near future. In the following discussion, we will demonstrate how the subsystems are currently configured and how they interface.
Figure 4 displays the TLC system architecture, with the Run-Time Subsystem shown at the top half of the figure and the Database Management Subsystem at the bottom half. Each component in the figure is assigned a unique number that is denoted in the text below in boldface. In the figure, the arrows between the components indicate their interconnections.
Figure 4.
Schematic Diagram of TLC System Architecture and Processing.
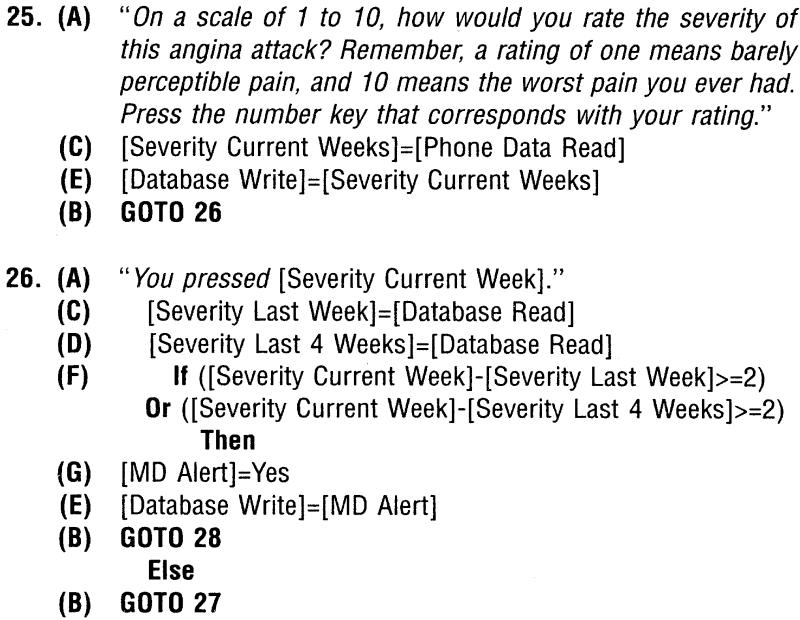
The Run-Time Subsystem (1) contains the Interactive Voice Response (IVR) Component (3) and three data tables: a Patient-Specific Data Table (5), a Public Data Table (6) and a Results Table (7). The heart of the Run-Time Subsystem is the IVR Component, which executes and speaks TLC conversations by integrating telephone hardware, touch-tone telephone decoding, and digital and analog voice translation. The TLC conversations spoken by the IVR Component are controlled by programmed scripts stored in the IVR Component. Figure 5 denotes part of a programmed script for TLC-Angina. In the figure, the spoken text is italicized and surrounded by quotation marks. The number to the left of the text is the segment number of the programmed script. The segments (or groups of lines) of the script are numbered sequentially, beginning with “1.” In addition to the italicized spoken text, the programmed script segments contain instructions for obtaining information from the patient user and the system's database—(C) and (D) in Figure 5, storing data in the database (E), manipulating this data (F), and controlling the flow of the conversation (B). The entire programmed script of a TLC application may contain hundreds of segments of English language text and the associated instructions. The IVR Component executes the programmed script beginning with the first script segment and proceeds to other segments by using data-driven logic embedded within the script segments.
Figure 5.
Part of the programmed script for TLC-Angina. This example represents “segments” 25-26 of a script that totals 120 “segments.” The material in quotations (A) is the English language script spoken by TLC. The numbers to the left of the script are labels to identify the “segment” location of each script segment. GOTO statements (B) control the flow of the conversation from segment to segment. Phrases surrounded by square brackets are system variables. Data are collected from a patient response (depressing a key on the telephone keypad) to a TLC question (C). Data can also be accessed from the TLC database (D) or stored in the database (E). Conditional statements are embedded within the script (E) and can control the flow of the conversation as well as determine what data are stored or retrieved from the database. Some data stored (G) trigger other actions: in this case, an immediate report to the patient's physician.
A TLC conversation is established between the patient (item 4 in Figure 4) and the IVR Component (3) when a patient makes a call to, or receives a call from, the TLC system. This initiates the operation of the Run-Time Subsystem (1), demonstrated at the top half of Figure 4. Once a telephone connection is established, the IVR Component executes the first segment of programmed script, which results in the salutation and password request being spoken. To produce the human speech, the IVR Component translates digitized voice data into speech. Next, the IVR Component waits for the patient to enter a password via the touch-tone keypad on the patient's telephone. Having received and decoded the touch-tones into their equivalent numerical values, the IVR Component authenticates the password entered by the patient by searching a list of valid passwords stored in the Patient-Specific Data Table (5). After accepting a valid password, the IVR Component executes the rest of the programmed script for a particular TLC application.
Evaluating the instructions in the programmed script segments requires data input into the IVR Component from patients using their telephones to generate touch-tones (4) and from data residing in two data tables in the Run-Time Subsystem: the Patient-Specific Data Table, mentioned above, and a Public Data Table (7). The Patient-Specific Data Table supplies data to the IVR Component on the patients' names, passwords, dates of birth, their physicians' names, and other patient attributes entered when patients are registered to use TLC. This table also provides the IVR component with selected information entered by patients during prior TLC calls. The Public Data Table (7), a second data table in the Run-Time Subsystem, has the special function of enabling the IVR Component to speak variable words or phrases, such as the patient's physician's name. Speech of this type is referred to as a “donut.” The Run-Time Subsystem contains a third table, the Results Table (6). It contains all information gathered from the patient's touch-tone input during a single TLC conversation and calculations made within the script (e.g., a patient's overall medication adherence). Data transfers from the Results Table to the Patient-Specific Data Table are discussed below. In certain TLC applications, the script requests a call transfer to or from an external Voice Mail system (20) through a PBX. This is used in TLC-AD to create both a community voice-mail bulletin board and a personal voice-mail system.
The Database Management Subsystem (2), displayed at the bottom half of Figure 4, contains the Master Patient Tables (8), which are the repository for all patient data, and four special components: an Initialization Component (9), a Reporting Component (10), a Download Component (11), and an Upload Component (12). The Database Management Subsystem collects, stores, transfers, and outputs data. It collects patient enrollment information from its Initialization Component (9). Using the initialization system, a TLC Data Manager (21) can enter patient-specific information, such as the patient's name, that is used by the IVR Component during TLC conversations. The Initialization Component, in turn, transfers this information to the Master Patient Tables (8), where it is stored, and to the Public Data Table, where it is also stored in the specific form of donuts. Whereas the Patient-Specific Data Table, resident in the Run-Time Subsystem described earlier, contains only patient data used in TLC conversations, the Master Patient Tables have all patient data that have been collected, whether used in TLC conversations or not.
The Upload Component (12) transfers data collected from patients during TLC conversations from the Results Table in the Run-Time Subsystem to the Master Patient Tables in the Database Management Subsystem. Following the execution of the Upload Component, the Download Component (11) updates the Patient-Specific Data Table's (5) records with information collected during the most recent TLC conversation. The Patient-Specific Data Table is then ready for the patient's next TLC call. The Master Patient Tables provide data for the Reporting Component (10), which generates the following four types of reports:
Alert Reports (13). The reporting system scans the Master Patient Tables for specific data elements that indicate an alert (or urgent condition) for the patient. The information is sent immediately to the patient's physician, either via fax (17), printer (18), the Internet (19), or a telephone call from the TLC Data Manager (21).
Monthly Reports (14). The reporting system sends the responsible physician a monthly Physician Report on the patient's status (Fig. 2), which can be transmitted like the Alert Reports. Patient Reports (Fig. 3) can also be sent regularly, typically by mail.
Operations Reports (15). The TLC Data Manager is notified about system problems when they occur. In addition, the status of the system is reported regularly, such as the number of times patients called in (or failed to call in) as scheduled or the number of times that the TLC system called out.
Research Reports (16). For research purposes, TLC operators can generate statistically-oriented summaries of selected data items that were gathered by TLC for any given time period. For example, one may wish to analyze the patients' blood pressures reported to TLC over a specific time period.
When the reporting system generates a report, it converts data in the Master Patient Tables into a format appropriate for visual display (such as tables and graphs). The Reporting System (10) that generates reports consists of forms, tables, queries, macros, and procedural code. Items (17), (18), and (19) at the bottom of Figure 4 represent the modes of communication available to the TLC System to transmit the data outputs. Any of the types of reports listed can be sent through any of these modes of communication. The Internet mode includes the transport of reports to remote FTP sites, attached to e-mail messages, or posted as Web pages.
Evaluation of TLC
Thus far, one chronic disease application (TLC-Hypertension) and one health behavior application (TLC-Medication Adherence) have been evaluated in a randomized clinical trial. The applications were combined and tested in a community-based clinical trial conducted in 29 communities in the Boston metropolitan area involving 267 elderly hypertensive patients cared for by 132 physicians.12 The subjects were randomly assigned to either a group that used TLC weekly as a supplement to their usual medical care or to a group that had their usual medical care alone. The study follow-up period was 6 months. The study hypotheses were that TLC users, in comparison with controls, would sustain greater improvements in medication adherence and blood pressure control.
TLC users had a mean medication adherence improvement of 18% compared with 12% for the usual care group (p =.03) (Table 1). For patients who were nonadherent with their antihypertensive medications at baseline, the effect of TLC on adherence was greater (36% vs. 26%, p =.03). Mean diastolic blood pressure (DBP) decreased 5.2 mmHg among TLC users compared with 0.8 mmHg for control group subjects (p =.02). Among nonadherent patients, mean DBP decreased 6.0 mmHg for TLC users but increased 2.8 mmHg in the usual care group (p =.01). The level of blood pressure improvement that resulted from TLC use is associated with an observed 40% reduction in stroke risk and a 10-15% reduction in coronary heart disease risk.23 Patient satisfaction with TLC in this study was high. Most patients found that it was easy to use (94%), made them more aware of their hypertension (95%), and relieved their worries about their disease (79%). Eighty-five percent of the 102 participating physicians whose patients were TLC users stated that they read TLC reports regularly, and 84% said they placed the reports in their patients' medical records. Forty percent claimed to discuss the information on the TLC reports regularly with their patients.
Two other TLC health behavior applications have been evaluated in randomized pilot studies: TLC-Low Fat and TLC-ACT. TLC-Low Fat, designed to modify dietary behavior in patients with hypercholesterolemia, was tested with 49 adults whose total cholesterol was ≥240 mg/dL.13 At the end of a 3-month intervention period, TLC-Low Fat users had a greater decrease in total cholesterol than non-users (mean = -21.3 mg/dL vs. +1.3 mg/dL, p < 0.01).
The second randomized pilot study evaluated the first version of TLC-ACT. The application targeted sedentary elders and was designed to motivate them to walk regularly for exercise.14 Sixty-eight individuals, aged 60 years and older, were randomly assigned to use TLC or not to use it. After 3 months of follow-up, TLC users walked more per week than control group subjects (mean = 120 minutes vs. 40 minutes, p =.065). TLC user satisfaction with both the Low Fat and ACT applications was high, similar to that reported by users of the hypertension application.
Patients who have used TLC have ranged in age from their 20s to their 90s; there has been a diversity of educational, socioeconomic, and racial/ethnic backgrounds, as well. A study of TLC use by elders showed that only cognitively impaired individuals were unable to use TLC without assistance.24 A person who is able to use a telephone unassisted can use TLC. Overall, we conclude that TLC use, thus far, is associated with positive changes in targeted health behaviors and improvement in disease control. Patients have been satisfied with their use of the system, and physicians integrate TLC reports into their medical practices.
Current Status and Future Plans
Table 1 shows the current status of TLC projects. We are currently applying the technology to more complex chronic diseases, to health behaviors that are more difficult to modify (cigarette smoking and mammography screening), and to new target populations such as children (asthma) and caregivers (Alzheimer's disease). We will also tackle the issue of how to “combine” applications—that is, how to monitor patients with multiple chronic diseases and health behavior needs without overwhelming them with too many separate TLC conversations. There is also the need to creatively explore the interplay between the TLC conversations, written materials sent to the patients and their providers (whether these are generated by TLC or not), the use of other communication vehicles (video and computer), and the role of human providers of health services. In the current model for using TLC in the health care delivery system, TLC functions as a combination of a test (it provides information to clinical decision makers) and also an independent provider of care (it helps modify patient health behavior).
Use of the system is not predicated on any change in how health care providers function. In fact, we expect this to change, and we plan to develop systems of care in which TLC applications interface with providers with redefined responsibilities. For example, caring for patients with high-risk pregnancy often entails the use of nurses who monitor these patients through office visits and over the telephone. Our TLC-High Risk Pregnancy application could be tailored to be used by these nurses as the “front end” of a monitoring system. This would change their work responsibilities, and would result in a redefinition of their role. Finally, we will be engaged in a number of technical developments, including the introduction of speech recognition and integration with the Internet. Over time we expect to change the platform of TLC applications to whatever home communication/information/entertainment device becomes established in the marketplace.
Conclusions
The telephone is and will remain in the near future the most common telecommunications link between health care providers and their patients.24 While most Americans have access to a telephone, access to computer networks still remains limited only to those with resources, knowledge, and computer skills.25 This has raised some concern among health care advocates who feel that the disadvantaged may be left off of the new telecommunications highway.26 For this reason, telephone-based information system interventions offer particular promise because they address the access problem and offer a reasonable cost alternative to computer hardware systems in patient's homes. The TLC system provides an example of the utility of this approach.
As the next millennium approaches, the virtual health care visit will become more commonplace. Telecommunications technology is undergoing rapid changes that will greatly affect the health care arena. We expect there will be devices available to patients in their homes that will integrate and improve upon the features of today's telephone, television, video, and computer technology.
Given the level of patient acceptance to date of the first wave of telecommunications technology, we speculate that the market demand for technology-based delivery systems used by patients in their homes will be strong.
Acknowledgments
The authors recognize their colleagues, past and present, who have contributed to the work presented, and give special recognition to Mary Beth Smith, Donald Belfer, Joseph Kennedy, Irina Arakelian, Kathleen Carey, Ramesh Farzanfar, Karla Jarvis, Barbara Tarlow, Lewis Kazis, Alan Jette, and Sharon Tennstedt. The authors thank Steven Pauker for his crucial support during the early days. They acknowledge the invaluable assistance of Sheilah Dorsey in the preparation of this manuscript, and Johnny Sandaire in the design of the tables and figures and in editing manuscript.
Supported by grants from the National Institutes of Health: HL 40076, HL 52528, HL 55664, NR 03318, AG 10798, and AG 13255. From the Agency for Health Care Policy and Research: HS 05135. The Medical Foundation. American Cancer Society, Massachusetts Division.
References
- 1.Schappert SM. National ambulatory medical care survey: 1991 summary. Vital Health Stat. 1994;116: 1-110. [PubMed] [Google Scholar]
- 2.Hallam L. You've got a lot to answer for, Mr. Bell: a review of the use of the telephone in primary care. Fam Pract. 1989;6: 47-57. [DOI] [PubMed] [Google Scholar]
- 3.Scannell KM, Perednia DA, Kissman HM. Telemedicine: past, present, future. Bethesda, MD: National Library of Medicine, National Institutes of Health, Public Health Service, USDHHS, 1995.
- 4.Detmer DE. The future of the IAIMS in a managed care environment: a call for private action and public investment. J Am Med Inform Assoc. 1997;4(2Suppl): S65-71. [PMC free article] [PubMed] [Google Scholar]
- 5.Spencer DC, Daugird AJ: The nature and content of physician telephone calls in a private practice. J Fam Pract. 1988;27: 201-5. [PubMed] [Google Scholar]
- 6.Tanke ED, Leirer VO. Automated telephone reminders in tuberculosis care. Med Care. 1994;32: 380-9. [DOI] [PubMed] [Google Scholar]
- 7.Alemi F, Alemagno SA, Goldhagen J, et al. Computer reminders improve on-time immunization rates. Med Care. 1996;34: OS45-OS51. [DOI] [PubMed] [Google Scholar]
- 8.Alemi F, Stephens RC, Javalghi RG, Dyches H, Butts J, Ghadiri A. A randomized trial of a telecommunications network for pregnant women who use cocaine. Med Care. 1996;34: OS10-OS20. [DOI] [PubMed] [Google Scholar]
- 9.Kobak KA, Greist JH, Jefferson JW, Katzelnick DJ. Computer-administered clinical rating scales. Psychopharmacology. 1996;127: 291-301. [DOI] [PubMed] [Google Scholar]
- 10.Alemi F, Stephens RC, Muise K, Dyches H, Mosavel M, Butts J. Educating patients at home: community health rap. Med Care. 1996;34: OS21-OS31. [DOI] [PubMed] [Google Scholar]
- 11.Searles JS, Perrine MW, Mundt JC, Helzer JE. Self-report of drinking using touch-tone telephone: extending the limits of reliable daily contact. J Stud Alcohol. 1995;56: 375-382. [DOI] [PubMed] [Google Scholar]
- 12.Friedman RH, Kazis LE, Jette A, et al. A telecommunications system for monitoring and counseling patients with hypertension: impact on medication adherence and blood pressure control. Am J Hyper. 1996;9: 285-292. [DOI] [PubMed] [Google Scholar]
- 13.Dutton JP, Posner BA, Smigelski C, Friedman RH. Lowering of total serum cholesterol through the use of DietAid: a telecommunications system for dietary counseling. Ann Beh Med. 1995;17(Suppl): S088. [Google Scholar]
- 14.Cullinane PM, Hyppolite K, Zastawney AL, Friedman RH. Telephone linked communication: activity counseling and tracking for older patients. J Gen Int Med. 1994;9(Suppl 2): 86A. [Google Scholar]
- 15.Mahoney DM. Reach for TLC: resources for enhancing Alzheimer's caregivers' health (reach project). National Institute on Aging/National Institute of Nursing Research Cooperative Study, 2000 1995.
- 16.Guyatt GH, Thompson PJ, Berman LB, et al. How should we measure function in patients with chronic heart and lung disease? J Chron Dis. 1985;6: 517-24. [DOI] [PubMed] [Google Scholar]
- 17.Haynes RB, Taylor DW, Sackett DL (eds), Compliance in Health Care. Baltimore: Johns Hopkins University Press, 1979.
- 18.Pate RR, Pratt M, Blair SN, et al. Physical activity and public health: a recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995;273: 402-7. [DOI] [PubMed] [Google Scholar]
- 19.US Department of Health and Human Services. Physical activity and health: a report of the surgeon general. Atlanta, GA: USDHHS, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, 1996.
- 20.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall, 1986.
- 21.Smith RA, Haynes S. Barriers to screening for breast cancer. Cancer 1992;69: 1967-78. [DOI] [PubMed] [Google Scholar]
- 22.Smith MB, Bruce KE, Torgerson JS, et al. Logical and efficient conversations between patients and the telephone-linked computer system. In: Greenes RS (ed): Proceedings: The Twelfth Annual Symposium on Computer Applications in Medical Care. Washington, DC: IEEE Society, 1988; 463-7.
- 23.Collins R, Peto R, MacMahon S, et al. Blood pressure, stroke, and coronary heart disease. Part 2. Short-term reductions in blood pressure: overview of randomized drug trials in an epidemiological context. Lancet. 1990;335: 827-38. [DOI] [PubMed] [Google Scholar]
- 24.Markson L, Friedman RH, Jette A, Kazis L. Computers as clinician extenders: monitoring chronic illness in elderly patients. Inter J Tech Aging. 1992;5: 153-65. [Google Scholar]
- 25.Johnson BE, Johnson CA. Telephone medicine: a general internal medicine experience. J Gen Intern Med. 1990;5: 234-9. [DOI] [PubMed] [Google Scholar]
- 26.Shalala D. Comments. Partnerships '97 Net Conference, May 7-9, 1997.
- 27.Pophal M. Do new technologies ignore the disadvantaged? American Nurse. 1997;2: 4. [PubMed] [Google Scholar]